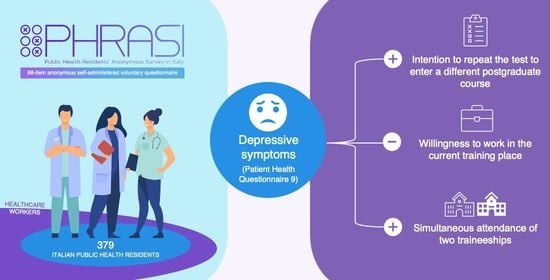
Depressive Symptoms of Public Health Medical Residents during the COVID-19 Pandemic, a Nation-Wide Survey: The PHRASI Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Variables of Interest
2.2. Depressive Symptoms
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Limitations and Strengths
4.2. Implications for Policy, Practice, and Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Mental Disorders. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 8 December 2022).
- World Health Organization (WHO). COVID-19 Pandemic Triggers 25% Increase in Prevalence of Anxiety and Depression Worldwide. Available online: https://www.who.int/news/item/02-03-2022-COVID-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide (accessed on 8 December 2022).
- EpiCentro Depressione—Passi. Available online: https://www.epicentro.iss.it/passi/dati/depressione?tab-container-1=tab1 (accessed on 20 November 2022).
- Amerio, A.; Aguglia, A.; Odone, A.; Gianfredi, V.; Serafini, G.; Signorelli, C.; Amore, M. COVID-19 Pandemic Impact on Mental Health of Vulnerable Populations. Acta Biomed. Atenei Parm. 2020, 91, 95–96. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, J.; Geng, Y.; Fang, Z.; Zhu, L.; Chen, Y.; Yao, Y. Meta-Analysis of the Prevalence of Anxiety and Depression among Frontline Healthcare Workers during the COVID-19 Pandemic. Front. Public Health 2022, 10, 984630. [Google Scholar] [CrossRef]
- Gianfredi, V.; Provenzano, S.; Santangelo, O.E. What Can Internet Users’ Behaviours Reveal about the Mental Health Impacts of the COVID-19 Pandemic? A Systematic Review. Public Health 2021, 198, 44–52. [Google Scholar] [CrossRef]
- Martínez, E.I.; García, J.R.; Arberas, E.J.; Llosa, J.A. Difference between Impacts of COVID-19 on Women and Men’s Psychological, Social, Vulnerable Work Situations, and Economic Well-Being. Int. J. Environ. Res. Public. Health 2022, 19, 8849. [Google Scholar] [CrossRef]
- Santomauro, D.F.; Mantilla Herrera, A.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global Prevalence and Burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 Due to the COVID-19 Pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, F.; Alshahrani, N.Z.; Abu Sabah, A.; Zarbah, A.; Abu Sabah, S.; Mamun, M.A. Prevalence and Factors Associated with Mental Health Problems in Saudi General Population during the Coronavirus Disease 2019 Pandemic: A Systematic Review and Meta-Analysis. PsyCh J. 2022, 11, 18–29. [Google Scholar] [CrossRef]
- Yuan, K.; Zheng, Y.-B.; Wang, Y.-J.; Sun, Y.-K.; Gong, Y.-M.; Huang, Y.-T.; Chen, X.; Liu, X.-X.; Zhong, Y.; Su, S.-Z.; et al. A Systematic Review and Meta-Analysis on Prevalence of and Risk Factors Associated with Depression, Anxiety and Insomnia in Infectious Diseases, Including COVID-19: A Call to Action. Mol. Psychiatry 2022, 27, 3214–3222. [Google Scholar] [CrossRef]
- Signorelli, C.; Odone, A.; Gianfredi, V.; Balzarini, F.; Bucci, D.; Croci, R.; Gaetti, G.; Stirparo, G.; Guerra, R. Epidemiological Assessment of the First COVID-19 Epidemic Wave in Lombardy. A Systematic Review: First COVID-19 Epidemic Wave in Lombardy. Acta Biomed. Atenei Parm. 2021, 92, E2021462. Available online: https://www.mattioli1885journals.com/index.php/actabiomedica/article/view/12340 (accessed on 30 December 2022).
- Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Wessely, S. Managing Mental Health Challenges Faced by Healthcare Workers during COVID-19 Pandemic. BMJ 2020, 368, m1211. [Google Scholar] [CrossRef] [PubMed]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental Health Problems Faced by Healthcare Workers Due to the COVID-19 Pandemic-A Review. Asian J. Psychiatry 2020, 51, 102119. [Google Scholar] [CrossRef]
- Penninx, B.W.J.H.; Benros, M.E.; Klein, R.S.; Vinkers, C.H. How COVID-19 Shaped Mental Health: From Infection to Pandemic Effects. Nat. Med. 2022, 28, 2027–2037. [Google Scholar] [CrossRef]
- Catalini, A.; Mazza, C.; Cosma, C.; Minutolo, G.; De Nicolò, V.; Gallinoro, V.; Caminiti, M.; Ancona, A.; Stacchini, L.; Berselli, N.; et al. Public Health Residents’ Anonymous Survey in Italy (PHRASI): Study Protocol for a Cross-Sectional Study for a Multidimensional Assessment of Mental Health and Its Determinants. Int. J. Environ. Res. Public. Health 2023, 20, 2003. [Google Scholar] [CrossRef] [PubMed]
- Charan, J.; Biswas, T. How to Calculate Sample Size for Different Study Designs in Medical Research? Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef]
- European Union. Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC (General Data Protection Regulation). Eur-Lex. Access to European Unione Law. 2016. Available online: https://eur-lex.europa.eu/eli/reg/2016/679/oj (accessed on 16 December 2022).
- Italia. Decreto Legislativo 10 Agosto 2018, n. 101. Disposizioni per L’adeguamento Della Normativa Nazionale Alle Disposizioni del Regolamento (UE) 2016/679 del Parlamento Europeo e del Consiglio, del 27 Aprile 2016, Relativo Alla Protezione Delle Persone Fisiche Con Riguardo al Trattamento dei Dati Personali, Nonché alla Libera Circolazione di Tali Dati e Che Abroga la Direttiva 95/46/CE (Regolamento Generale Sulla Protezione Dei Dati). Gazzetta Ufficiale Della Repubblica Italiana Serie Generale n. 159 del 4 September 2018. Available online: https://www.gazzettaufficiale.it/eli/id/2018/09/04/18G00129/sg (accessed on 19 April 2023).
- Italia. Decreto Legislativo 30 Giugno 2003, n. 196. Codice in Materia di Protezione dei Dati Personali. In Ministero della Giustizia—Ufficio Pubblicazioni Leggi e Decreti, Editor. Supplemento Ordinario alla “Gazzetta Ufficiale della Repubblica Italiana”; Serie Generale; Istituto Poligrafico e Zecca Dello Stato: Roma, Italy, 2003; Volume 123/L, pp. 11–207. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2003-07-29&atto.codiceRedazionale=003G0218 (accessed on 19 April 2023).
- Mazzotti, E.; Fassone, G.; Picardi, A.; Sagoni, E.; Ramieri, L.; Lega, I.; Camaioni, D.; Abeni, D.; Pasquini, P. II Patient Health Questionnaire (PHQ) per lo screening dei disturbi psichiatrici: Uno studio di validazione nei confronti della Intervista Clinica Strutturata per il DSM-IV asse I (SCID-I). Ital. J. Psychopathol. 2003, 9, 235–242. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef]
- Allen, M.P. (Ed.) The Problem of Multicollinearity. In Understanding Regression Analysis; Springer US: Boston, MA, USA, 1997; pp. 176–180. ISBN 978-0-585-25657-3. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-Project.Org/ (accessed on 16 December 2022).
- Dyrbye, L.N.; West, C.P.; Satele, D.; Boone, S.; Tan, L.; Sloan, J.; Shanafelt, T.D. Burnout among U.S. Medical Students, Residents, and Early Career Physicians Relative to the General U.S. Population. Acad. Med. J. Assoc. Am. Med. Coll. 2014, 89, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Joules, N.; Williams, D.M.; Thompson, A.W. Depression in Resident Physicians: A Systematic Review. Open J. Depress. 2014, 3, 89–100. [Google Scholar] [CrossRef]
- Han, R.; Hahn, E.; Done, S.J.; Pun, C.; Shivji, S.; Lu, F.-I. Resident Depression and Burnout during the COVID-19 Pandemic. Arch. Pathol. Lab. Med. 2022, 147, 368–375. [Google Scholar] [CrossRef]
- Mata, D.A.; Ramos, M.A.; Bansal, N.; Khan, R.; Guille, C.; Di Angelantonio, E.; Sen, S. Prevalence of Depression and Depressive Symptoms among Resident Physicians: A Systematic Review and Meta-Analysis. JAMA 2015, 314, 2373–2383. [Google Scholar] [CrossRef]
- Mendonça, V.S.; Steil, A.; Góis, A.F.T. Mental Health and the COVID-19 Pandemic: A Study of Medical Residency Training over the Years. Clin. Sao Paulo Braz. 2021, 76, e2907. [Google Scholar] [CrossRef]
- Allan, B.A.; Dexter, C.; Kinsey, R.; Parker, S. Meaningful Work and Mental Health: Job Satisfaction as a Moderator. J. Ment. Health Engl. 2018, 27, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Harvey, S.B.; Modini, M.; Joyce, S.; Milligan-Saville, J.S.; Tan, L.; Mykletun, A.; Bryant, R.A.; Christensen, H.; Mitchell, P.B. Can Work Make You Mentally Ill? A Systematic Meta-Review of Work-Related Risk Factors for Common Mental Health Problems. Occup. Environ. Med. 2017, 74, 301–310. [Google Scholar] [CrossRef]
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender Differences in Depression in Representative National Samples: Meta-Analyses of Diagnoses and Symptoms. Psychol. Bull. 2017, 143, 783–822. [Google Scholar] [CrossRef]
- Templeton, K.; Nilsen, K.M.; Walling, A. Issues Faced by Senior Women Physicians: A National Survey. J. Women’s Health 2020, 29, 980–988. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Abraham, A.; Chaabna, K.; Doraiswamy, S.; Bhagat, S.; Sheikh, J.; Mamtani, R.; Cheema, S. Depression among Healthcare Workers in the Eastern Mediterranean Region: A Systematic Review and Meta-Analysis. Hum. Resour. Health 2021, 19, 81. [Google Scholar] [CrossRef]
- Nomoto, M.; Hara, A.; Kikuchi, K. Effects of long-time commuting and long-hour working on lifestyle and mental health among school teachers in Tokyo, Japan. J. Hum. Ergol. 2015, 44, 1–9. [Google Scholar]
- Jensen, M.T.; Rundmo, T. Associations between Work Family Conflict, Emotional Exhaustion, Musculoskeletal Pain, and Gastrointestinal Problems in a Sample of Business Travelers. Scand. J. Psychol. 2015, 56, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Everson, S.A.; Maty, S.C.; Lynch, J.W.; Kaplan, G.A. Epidemiologic Evidence for the Relation between Socioeconomic Status and Depression, Obesity, and Diabetes. J. Psychosom. Res. 2002, 53, 891–895. [Google Scholar] [CrossRef]
- Weinberger, A.H.; Gbedemah, M.; Martinez, A.M.; Nash, D.; Galea, S.; Goodwin, R.D. Trends in Depression Prevalence in the USA from 2005 to 2015: Widening Disparities in Vulnerable Groups. Psychol. Med. 2018, 48, 1308–1315. [Google Scholar] [CrossRef] [PubMed]
- Shields-Zeeman, L.; Collin, D.F.; Batra, A.; Hamad, R. How Does Income Affect Mental Health and Health Behaviours? A Quasi-Experimental Study of the Earned Income Tax Credit. J. Epidemiol. Community Health 2021, 75, 929–935. [Google Scholar] [CrossRef] [PubMed]
- Economou, M.; Madianos, M.; Peppou, L.E.; Patelakis, A.; Stefanis, C.N. Major Depression in the Era of Economic Crisis: A Replication of a Cross-Sectional Study across Greece. J. Affect. Disord. 2013, 145, 308–314. [Google Scholar] [CrossRef]
- Ridley, M.; Rao, G.; Schilbach, F.; Patel, V. Poverty, Depression, and Anxiety: Causal Evidence and Mechanisms. Science 2020, 370, eaay0214. [Google Scholar] [CrossRef] [PubMed]
- Heinz, A.J.; Meffert, B.N.; Halvorson, M.A.; Blonigen, D.; Timko, C.; Cronkite, R. Employment Characteristics, Work Environment, and the Course of Depression over 23 Years: Does Employment Help Foster Resilience? Depress. Anxiety 2018, 35, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Bowling, J.; Simmons, M.; Dodge, B.; Sundarraman, V.; Lakshmi, B.; Dharuman, S.T.; Herbenick, D. Family Formation Goals Among Sexual and Gender Minority Individuals in Urban India. Stud. Fam. Plann. 2019, 50, 357–373. [Google Scholar] [CrossRef]
- MacDonald, M.M.; Rindfuss, R.R. Earnings, Relative Income, and Family Formation. Demography 1981, 18, 123–136. [Google Scholar] [CrossRef]
- Xu, J.; Zhang, L. The Effect of Living Alone on the Mental Health of the Economically Active Floating Population during the COVID-19 Pandemic. Front. Public Health 2022, 10, 931425. [Google Scholar] [CrossRef]
- Posel, D. Living Alone and Depression in a Developing Country Context: Longitudinal Evidence from South Africa. SSM Popul. Health 2021, 14, 100800. [Google Scholar] [CrossRef]
- Gianfredi, V.; Beran, M.; Koster, A.; Eussen, S.J.; Odone, A.; Signorelli, C.; Schaper, N.C.; Köhler, S.; Bosma, H.; Dagnelie, P.C.; et al. Association between Social Network Characteristics and Prevalent and Incident Depression: The Maastricht Study. J. Affect. Disord. 2021, 293, 338–346. [Google Scholar] [CrossRef]
- Honjo, K.; Tani, Y.; Saito, M.; Sasaki, Y.; Kondo, K.; Kawachi, I.; Kondo, N. Living Alone or With Others and Depressive Symptoms, and Effect Modification by Residential Social Cohesion Among Older Adults in Japan: The JAGES Longitudinal Study. J. Epidemiol. 2018, 28, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Mondal, H.; Mondal, S. Social Desirability Bias: A Confounding Factor to Consider in Survey by Self-Administered Questionnaire. Indian J. Pharmacol. 2018, 50, 143–144. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, C.A.; Hewitt, A.D. A Methodology for Assessing Sample Representativeness. Environ. Forensics 2005, 6, 71–75. [Google Scholar] [CrossRef]
- Santos, I.; Tavares, B.; Munhoz, T.; Almeida, L.; Tessele Barreto da Silva, N.; Tams, B.; Patella, A.; Matijasevich, A. Sensitivity and Specificity of the Patient Health Questionnaire-9 (PHQ-9) among Adults from the General Population. Cad. Saúde Pública 2013, 29, 1533–1543. [Google Scholar] [CrossRef] [PubMed]
- Ogunnubi, O.P.; Ojo, T.M.; Oyelohunnu, M.A.; Olagunju, A.T.; Tshuma, N. Stress and Training Satisfaction among Resident Doctors in Nigeria: Any Justification for a Change in Training Policy? J. Clin. Sci. 2018, 15, 32–40. [Google Scholar] [CrossRef]
- Salari, N.; Khazaie, H.; Hosseinian-Far, A.; Khaledi-Paveh, B.; Kazeminia, M.; Mohammadi, M.; Shohaimi, S.; Daneshkhah, A.; Eskandari, S. The Prevalence of Stress, Anxiety and Depression within Front-Line Healthcare Workers Caring for COVID-19 Patients: A Systematic Review and Meta-Regression. Hum. Resour. Health 2020, 18, 100. [Google Scholar] [CrossRef]
- Krasner, M.S.; Epstein, R.M.; Beckman, H.; Suchman, A.L.; Chapman, B.; Mooney, C.J.; Quill, T.E. Association of an Educational Program in Mindful Communication with Burnout, Empathy, and Attitudes among Primary Care Physicians. JAMA 2009, 302, 1284–1293. [Google Scholar] [CrossRef]
- CLER Evaluation Committee. CLER Pathways to Excellence: Expectations for an Optimal Clinical Learning Environment to Achieve Safe and High-Quality Patient Care, Version 2.0; Accreditation Council for Graduate Medical Education: Chicago, IL, USA, 2019. [Google Scholar] [CrossRef]
- Aaronson, A.L.; Backes, K.; Agarwal, G.; Goldstein, J.L.; Anzia, J. Mental Health During Residency Training: Assessing the Barriers to Seeking Care. Acad. Psychiatry J. Am. Assoc. Dir. Psychiatr. Resid. Train. Assoc. Acad. Psychiatry 2018, 42, 469–472. [Google Scholar] [CrossRef]
- de Mélo Silva Júnior, M.L.; Valença, M.M.; Rocha-Filho, P.A.S. Individual and Residency Program Factors Related to Depression, Anxiety and Burnout in Physician Residents—A Brazilian Survey. BMC Psychiatry 2022, 22, 272. [Google Scholar] [CrossRef]
- Wu, A.; Roemer, E.C.; Kent, K.B.; Ballard, D.W.; Goetzel, R.Z. Organizational Best Practices Supporting Mental Health in the Workplace. J. Occup. Environ. Med. 2021, 63, e925–e931. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health Atlas 2020; World Health Organization: Geneva, Switzerland, 2021; ISBN 9789240036703. [Google Scholar]
- Chekroud, S.R.; Gueorguieva, R.; Zheutlin, A.B.; Paulus, M.; Krumholz, H.M.; Krystal, J.H.; Chekroud, A.M. Association between Physical Exercise and Mental Health in 1·2 Million Individuals in the USA between 2011 and 2015: A Cross-Sectional Study. Lancet Psychiatry 2018, 5, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Jorm, A.F.; Korten, A.E.; Jacomb, P.A.; Rodgers, B.; Pollitt, P.; Christensen, H.; Henderson, S. Helpfulness of Interventions for Mental Disorders: Beliefs of Health Professionals Compared with the General Public. Br. J. Psychiatry 1997, 171, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Spiegel, J.M. Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review. Int. J. Environ. Res. Public. Health 2019, 16, 4396. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Yang, L.; Zhang, C.; Xiang, Y.-T.; Liu, Z.; Hu, S.; Zhang, B. Online Mental Health Services in China during the COVID-19 Outbreak. Lancet Psychiatry 2020, 7, e17–e18. [Google Scholar] [CrossRef]
- Langarizadeh, M.; Tabatabaei, M.S.; Tavakol, K.; Naghipour, M.; Rostami, A.; Moghbeli, F. Telemental Health Care, an Effective Alternative to Conventional Mental Care: A Systematic Review. Acta Inform. Med. AIM J. Soc. Med. Inform. Bosnia Herzeg. Cas. Drus. Za Med. Inform. BiH 2017, 25, 240–246. [Google Scholar] [CrossRef]
- O’Connor, E.; Rossom, R.C.; Henninger, M.; Groom, H.C.; Burda, B.U.; Henderson, J.T.; Bigler, K.D.; Whitlock, E.P. Screening for Depression in Adults: An Updated Systematic Evidence Review for the U.S. Preventive Services Task Force; U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2016. [Google Scholar]
- Akincigil, A.; Matthews, E.B. National Rates and Patterns of Depression Screening in Primary Care: Results from 2012 and 2013. Psychiatr. Serv. 2017, 68, 660–666. [Google Scholar] [CrossRef]
- Alosaimi, F.D.; Kazim, S.N.; Almufleh, A.S.; Aladwani, B.S.; Alsubaie, A.S. Prevalence of Stress and Its Determinants among Residents in Saudi Arabia. Saudi Med. J. 2015, 36, 605–612. [Google Scholar] [CrossRef]
| Characteristic | n, % (N = 379) | No Clinically Relevant Depressive Symptoms (PHQ-9 < 10) N = 282 1 | Clinically Relevant Depressive Symptoms (PHQ-9 ≥ 10) N = 97 1 | p-Value 2 |
|---|---|---|---|---|
| Age [median, (IQR)] | 30.0 (29.0, 34.0) | 30 (28.00, 34) | 31 (29.00, 33) | 0.13 |
| Sex | ||||
| Female | 219 (58%) | 164 (58.16%) | 55 (56.70%) | 0.8 |
| Male | 160 (42%) | 118 (41.84%) | 42 (43.30%) | |
| Region of residence | ||||
| Center | 96 (25%) | 75 (26.60%) | 21 (21.65%) | 0.3 |
| North | 157 (41%) | 119 (42.20%) | 38 (39.18%) | |
| South and islands | 126 (33%) | 88 (31.21%) | 38 (39.18%) | |
| Cohabitation | ||||
| Alone | 98 (26%) | 70 (24.82%) | 28 (28.87%) | 0.4 |
| With Others | 281 (74%) | 212 (75.18%) | 69 (71.13%) | |
| Number of children | ||||
| 0 | 327 (86%) | 241 (85.46%) | 86 (88.66%) | 0.3 |
| 1 | 32 (8%) | 23 (8.16%) | 9 (9.28%) | |
| >1 | 20 (5%) | 18 (6.38%) | 2 (2.06%) | |
| Region of traineeship | ||||
| Center | 113 (30%) | 84 (29.79%) | 29 (29.90%) | 0.6 |
| North | 178 (47%) | 136 (48.23%) | 42 (43.30%) | |
| South and islands | 88 (23%) | 62 (21.99%) | 26 (26.80%) | |
| Course year in the postgraduate school | ||||
| 1st biennium | 292 (77%) | 218 (77.30%) | 74 (76.29%) | 0.8 |
| 2nd biennium | 87 (23%) | 64 (22.70%) | 23 (23.71%) | |
| Off-site | ||||
| No | 211 (56%) | 159 (56.38%) | 52 (53.61%) | 0.6 |
| Yes | 168 (44%) | 123 (43.62%) | 45 (46.39%) | |
| Commuter | ||||
| No | 258 (68%) | 197 (69.86%) | 61 (62.89%) | 0.2 |
| Yes | 121 (32%) | 85 (30.14%) | 36 (37.11%) | |
| Willingness to work in the current work/training place after completion of the postgraduate course | ||||
| No | 125 (33%) | 80 (28.37%) | 45 (46.39%) | 0.001 |
| Yes | 254 (67%) | 202 (71.63%) | 52 (53.61%) | |
| Simultaneous attendance of two traineeships | ||||
| No | 321 (85%) | 245 (86.88%) | 76 (78.35%) | 0.044 |
| Yes | 58 (15%) | 37 (13.12%) | 21 (21.65%) | |
| Intention to repeat the test to enter a different postgraduate school/general practitioner course | ||||
| No | 315 (83%) | 251 (89.01%) | 64 (65.98%) | <0.001 |
| Maybe | 46 (12%) | 23 (8.16%) | 23 (23.71%) | |
| Yes | 18 (4.7%) | 8 (2.84%) | 10 (10.31%) | |
| Having a contract of employment compatible with the postgraduate school | ||||
| No | 242 (64%) | 182 (64.54%) | 60 (61.86%) | 0.6 |
| Yes | 137 (36%) | 100 (35.46%) | 37 (38.14%) | |
| Possibility to make ends meet with their own income | ||||
| Easily | 162 (43%) | 123 (43.62%) | 39 (40.21%) | 0.6 |
| Hardly | 217 (57%) | 159 (56.38%) | 58 (59.79%) |
| Variable | aOR Related to Depressive Symptoms (PHQ-9 ≥ 10) | 95% CI | p-Value |
|---|---|---|---|
| Cohabitation (ref. Alone) | |||
| With Others | 0.816 | 0.486–1.371 | 0.443 |
| Region of traineeship (ref. Center) | |||
| North | 0.912 | 0.527–1.577 | 0.741 |
| South and islands | 1.213 | 0.650–2.263 | 0.544 |
| Off-site (ref. No) | |||
| Yes | 1.171 | 0.731–1.877 | 0.512 |
| Commuter (ref. No) | |||
| Yes | 1.329 | 0.813–2.172 | 0.256 |
| Willingness to work in the current work/training place after completion of the postgraduate course (ref. No) | |||
| Yes | 0.456 | 0.283–0.734 | 0.001 |
| Simultaneous attendance of two traineeships (ref. No) | |||
| Yes | 1.832 | 1.010–3.324 | 0.046 |
| Intention to repeat the test to enter a different postgraduate school/general practitioner course (ref. No) | |||
| Maybe | 3.925 | 2.067–7.452 | <0.001 |
| Yes | 4.949 | 1.872–13.086 | 0.001 |
| Having a contract of employment compatible with the postgraduate school (ref. No) | |||
| Yes | 1.142 | 0.705–1.848 | 0.589 |
| Possibility to make ends meet with their own income (ref. Easily) | |||
| Hardly | 1.123 | 0.696–1.811 | 0.634 |
| Characteristic | Female | Male | ||||
|---|---|---|---|---|---|---|
| No Clinically Relevant Depressive Symptoms (PHQ-9 < 10) N = 164 1 | Clinically Relevant Depressive Symptoms (PHQ-9 ≥ 10) N = 55 1 | p-Value 2 | No Clinically Relevant Depressive Symptoms (PHQ-9 < 10) N = 118 1 | Clinically Relevant Depressive Symptoms (PHQ-9 ≥ 10) N = 42 1 | p-Value 2 | |
| Age [median, (IQR)] | 30 (28.00, 34) | 31 (29.00, 34) | 0.10 | 30 (28.00, 34) | 31 (29.00, 33) | 0.7 |
| Region of residence | ||||||
| Center | 44 (26.83%) | 9 (16.36%) | 0.3 | 31 (26.27%) | 12 (28.57%) | 0.4 |
| North | 72 (43.90%) | 26 (47.27%) | 47 (39.83%) | 12 (28.57%) | ||
| South and islands | 48 (29.27%) | 20 (36.36%) | 40 (33.90%) | 18 (42.86%) | ||
| Cohabitation | ||||||
| Alone | 34 (20.73%) | 15 (27.27%) | 0.3 | 36 (30.51%) | 13 (30.95%) | >0.9 |
| With Others | 130 (79.27%) | 40 (72.73%) | 82 (69.49%) | 29 (69.05%) | ||
| Number of children | ||||||
| 0 | 135 (82.32%) | 46 (83.64%) | 0.5 | 106 (89.83%) | 40 (95.24%) | 0.6 |
| 1 | 16 (9.76%) | 7 (12.73%) | 7 (5.93%) | 2 (4.76%) | ||
| >1 | 13 (7.93%) | 2 (3.64%) | 5 (4.24%) | 0 (0.00%) | ||
| Region of traineeship | ||||||
| Center | 48 (29.27%) | 14 (25.45%) | 0.9 | 36 (30.51%) | 15 (35.71%) | 0.3 |
| North | 80 (48.78%) | 28 (50.91%) | 56 (47.46%) | 14 (33.33%) | ||
| South and islands | 36 (21.95%) | 13 (23.64%) | 26 (22.03%) | 13 (30.95%) | ||
| Course year in the postgraduate school | ||||||
| 1st biennium | 123 (75.00%) | 42 (76.36%) | 0.8 | 95 (80.51%) | 32 (76.19%) | 0.6 |
| 2nd biennium | 41 (25.00%) | 13 (23.64%) | 23 (19.49%) | 10 (23.81%) | ||
| Off-site | ||||||
| No | 86 (52.44%) | 31 (56.36%) | 0.6 | 73 (61.86%) | 21 (50.00%) | 0.2 |
| Yes | 78 (47.56%) | 24 (43.64%) | 45 (38.14%) | 21 (50.00%) | ||
| Commuter | ||||||
| No | 114 (69.51%) | 33 (60.00%) | 0.2 | 83 (70.34%) | 28 (66.67%) | 0.7 |
| Yes | 50 (30.49%) | 22 (40.00%) | 35 (29.66%) | 14 (33.33%) | ||
| Willingness to work in the current work/training place after completion of the postgraduate course | ||||||
| No | 47 (28.66%) | 29 (52.73%) | 0.001 | 33 (27.97%) | 16 (38.10%) | 0.2 |
| Yes | 117 (71.34%) | 26 (47.27%) | 85 (72.03%) | 26 (61.90%) | ||
| Simultaneous attendance of two traineeships | ||||||
| No | 142 (86.59%) | 46 (83.64%) | 0.6 | 103 (87.29%) | 30 (71.43%) | 0.018 |
| Yes | 22 (13.41%) | 9 (16.36%) | 15 (12.71%) | 12 (28.57%) | ||
| Intention to repeat the test to enter a different postgraduate school/general practitioner course | ||||||
| No | 146 (89.02%) | 39 (70.91%) | 0.005 | 105 (88.98%) | 25 (59.52%) | <0.001 |
| Maybe | 13 (7.93%) | 12 (21.82%) | 10 (8.47%) | 11 (26.19%) | ||
| Yes | 5 (3.05%) | 4 (7.27%) | 3 (2.54%) | 6 (14.29%) | ||
| Having a contract of employment compatible with the postgraduate school | ||||||
| No | 110 (67.07%) | 38 (69.09%) | 0.8 | 72 (61.02%) | 22 (52.38%) | 0.3 |
| Yes | 54 (32.93%) | 17 (30.91%) | 46 (38.98%) | 20 (47.62%) | ||
| Possibility to make ends meet with their own income | ||||||
| Easily | 67 (40.85%) | 17 (30.91%) | 0.2 | 56 (47.46%) | 22 (52.38%) | 0.6 |
| Hardly | 97 (59.15%) | 38 (69.09%) | 62 (52.54%) | 20 (47.62%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cedrone, F.; Berselli, N.; Stacchini, L.; De Nicolò, V.; Caminiti, M.; Ancona, A.; Minutolo, G.; Mazza, C.; Cosma, C.; Gallinoro, V.; et al. Depressive Symptoms of Public Health Medical Residents during the COVID-19 Pandemic, a Nation-Wide Survey: The PHRASI Study. Int. J. Environ. Res. Public Health 2023, 20, 5620. https://doi.org/10.3390/ijerph20095620
Cedrone F, Berselli N, Stacchini L, De Nicolò V, Caminiti M, Ancona A, Minutolo G, Mazza C, Cosma C, Gallinoro V, et al. Depressive Symptoms of Public Health Medical Residents during the COVID-19 Pandemic, a Nation-Wide Survey: The PHRASI Study. International Journal of Environmental Research and Public Health. 2023; 20(9):5620. https://doi.org/10.3390/ijerph20095620
Chicago/Turabian StyleCedrone, Fabrizio, Nausicaa Berselli, Lorenzo Stacchini, Valentina De Nicolò, Marta Caminiti, Angela Ancona, Giuseppa Minutolo, Clara Mazza, Claudia Cosma, Veronica Gallinoro, and et al. 2023. "Depressive Symptoms of Public Health Medical Residents during the COVID-19 Pandemic, a Nation-Wide Survey: The PHRASI Study" International Journal of Environmental Research and Public Health 20, no. 9: 5620. https://doi.org/10.3390/ijerph20095620