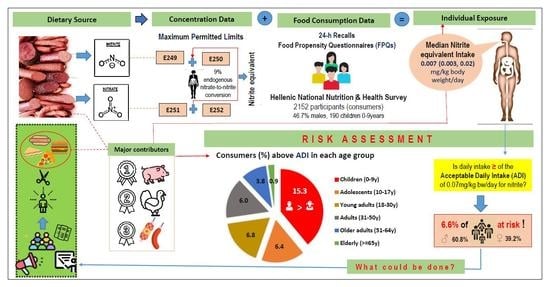
Risk Assessment of Nitrite and Nitrate Intake from Processed Meat Products: Results from the Hellenic National Nutrition and Health Survey (HNNHS)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. Exposure Assessment
2.2.1. Food Consumption Data
- Participants
- Processed meat consumption frequency
2.2.2. Occurrence Data
- Food groups classification
- Maximum Permitted Limits (MPLs)
- Estimated nitrite and nitrate intake
- Estimated food groups contribution to daily total nitrite intake
2.3. Risk Characterization
2.4. Other Parameters
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, Volume 114; Red Meat and Processed Meat; IARC monographs on the evaluation of carcinogenic risks to humans; IARC Press: Lyon, France, 2018; ISBN 978-92-832-0152-6.
- World Cancer Reserach Fund/American Institute for Cancer Recommendations and Public Health and Policy Implications. Available online: https://www.wcrf.org/wp-content/uploads/2021/01/Recommendations.pdf (accessed on 13 March 2022).
- Kastorini, C.-M.; Critselis, E.; Zota, D.; Coritsidis, A.L.; Nagarajan, M.K.; Papadimitriou, E.; Belogianni, K.; Benetou, V.; Linos, A.; on behalf of the Greek National Dietary Guidelines Scientific Team. National Dietary Guidelines of Greece for Children and Adolescents: A Tool for Promoting Healthy Eating Habits. Public Health Nutr. 2019, 22, 2688–2699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO Cancer: Carcinogenicity of the Consumption of Red Meat and Processed Meat. Available online: https://www.who.int/news-room/questions-and-answers/item/cancer-carcinogenicity-of-the-consumption-of-red-meat-and-processed-meat (accessed on 25 March 2022).
- European Commission Regulation (EC). No 1333/2008 of the European Parliament and of the Council of 16 December 2008 on Food Additives (OJ L 354 31.12.2008, p. 16). Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:02008R1333-20201223&from=EL (accessed on 8 August 2022).
- Sindelar, J.J.; Milkowski, A.L. Human Safety Controversies Surrounding Nitrate and Nitrite in the Diet. Nitric Oxide Biol. Chem. 2012, 26, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Kotopoulou, S.; Zampelas, A.; Magriplis, E. Dietary Nitrate and Nitrite and Human Health: A Narrative Review by Intake Source. Nutr. Rev. 2021, 4, 762–773. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global Nutrition Transition and the Pandemic of Obesity in Developing Countries. Nutr. Rev. 2012, 70, 3–21, PMCID:PMC3257829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, A.; Mathur, P. Evaluating Hazards Posed by Additives in Food: A Review of Studies Adopting a Risk Assessment Approach. Curr. Res. Nutr. Food Sci. J. 2015, 3, 243–255. [Google Scholar] [CrossRef]
- Jain, A.; Mathur, P. Estimation of Food Additive Intake—Overview of the Methodology. Food Rev. Int. 2015, 31, 355–384. [Google Scholar] [CrossRef]
- Moy, G.G. Risk Analysis: Risk Analysis of Hazards in Food: An Overview. Encycl. Food Saf. 2014. [Google Scholar] [CrossRef]
- EFSA Re-Evaluation of Potassium Nitrite (E 249) and Sodium Nitrite (E 250) as Food Additives. EFSA J. Eur. Food Saf. Auth. 2017, 15, e04786, PMCID:PMC7009987. [CrossRef] [PubMed]
- EFSA Re-Evaluation of Sodium Nitrate (E 251) and Potassium Nitrate (E 252) as Food Additives. EFSA J. Eur. Food Saf. Auth. 2017, 15, e04787. [CrossRef]
- Anyzewska, A.; Wawrzyniak, A. Evaluating Adult Dietary Intakes of Nitrate and Nitrite in Polish Households during 2006–2012. Rocz. Panstw. Zakl. Hig. 2014, 65, 107–111. [Google Scholar] [PubMed]
- European Commission Regulation (EC). No 178/2002 of the European Parliament and of the Council of 28 January 2002 Laying down the General Principles and Requirements of Food Law, Establishing the European Food Safety Authority and Laying down Procedures in Matters of Food Safety. Available online: https://eur-lex.europa.eu/legal-content/EL/TXT/?uri=CELEX%3A02002R0178-20190726 (accessed on 8 August 2022).
- Reinik, M.; Tamme, T.; Roasto, M.; Juhkam, K.; Jurtsenko, S.; Tenńo, T.; Kiis, A. Nitrites, Nitrates and N-Nitrosoamines in Estonian Cured Meat Products: Intake by Estonian Children and Adolescents. Food Addit. Contam. 2005, 22, 1098–1105. [Google Scholar] [CrossRef] [PubMed]
- Temme, E.H.M.; Vandevijvere, S.; Vinkx, C.; Huybrechts, I.; Goeyens, L.; Van Oyen, H. Average Daily Nitrate and Nitrite Intake in the Belgian Population Older than 15 Years. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2011, 28, 1193–1204. [Google Scholar] [CrossRef] [PubMed]
- Vin, K.; Connolly, A.; McCaffrey, T.; McKevitt, A.; O’Mahony, C.; Prieto, M.; Tennant, D.; Hearty, A.; Volatier, J.L. Estimation of the Dietary Intake of 13 Priority Additives in France, Italy, the UK and Ireland as Part of the FACET Project. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2013, 30, 2050–2080. [Google Scholar] [CrossRef] [PubMed]
- Merino, L.; Darnerud, P.O.; Toldrá, F.; Ilbäck, N.-G. Time-Dependent Depletion of Nitrite in Pork/Beef and Chicken Meat Products and Its Effect on Nitrite Intake Estimation. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2016, 33, 186–192, PMCID:PMC4784486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suomi, J.; Ranta, J.; Tuominen, P.; Putkonen, T.; Bäckman, C.; Ovaskainen, M.-L.; Virtanen, S.M.; Savela, K. Quantitative Risk Assessment on the Dietary Exposure of Finnish Children and Adults to Nitrite. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2016, 33, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Adam, A.H.B.; Mustafa, N.E.M.; Rietjens, I.M.C.M. Nitrite in Processed Meat Products in Khartoum, Sudan and Dietary Intake. Food Addit. Contam. Part B Surveill. 2017, 10, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S. Exposure Estimates of Nitrite and Nitrate from Consumption of Cured Meat Products by the U.S. Population. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2018, 35, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Milešević, J.; Vranić, D.; Gurinović, M.; Korićanac, V.; Borović, B.; Zeković, M.; Šarac, I.; Milićević, D.R.; Glibetić, M. The Intake of Phosphorus and Nitrites through Meat Products: A Health Risk Assessment of Children Aged 1 to 9 Years Old in Serbia. Nutrients 2022, 14, 242. [Google Scholar] [CrossRef]
- Elias, A.; Jalakas, S.; Roasto, M.; Reinik, M.; Nurk, E.; Kaart, T.; Tuvike, A.; Meremäe, K.; Nelis, K.; Elias, T. Nitrite and Nitrate Content in Meat Products and Estimated Nitrite Intake by the Estonian Children. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Smiliotopoulos, T.; Magriplis, E.; Zampelas, A. Validation of a Food Propensity Questionnaire for the Hellenic National Nutrition and Health Survey (HNNHS) and Results on This Population’s Adherence to Key Food-Group Nutritional Guidelines. Nutrients 2020, 12, 1808. [Google Scholar] [CrossRef]
- Michas, G.; Karvelas, G.; Trikas, A. Cardiovascular Disease in Greece; the Latest Evidence on Risk Factors. Hellenic J. Cardiol. 2019, 60, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Karageorgou, D.; Magriplis, E.; Mitsopoulou, A.V.; Dimakopoulos, I.; Bakogianni, I.; Micha, R.; Michas, G.; Chourdakis, M.; Ntouroupi, T.; Tsaniklidou, S.M.; et al. Dietary Patterns and Lifestyle Characteristics in Adults: Results from the Hellenic National Nutrition and Health Survey (HNNHS). Public Health 2019, 171, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Magriplis, E.; Dimakopoulos, I.; Karageorgou, D.; Mitsopoulou, A.-V.; Bakogianni, I.; Micha, R.; Michas, G.; Ntouroupi, T.; Tsaniklidou, S.-M.; Argyri, K.; et al. Aims, Design and Preliminary Findings of the Hellenic National Nutrition and Health Survey (HNNHS). BMC Med. Res. Methodol. 2019, 19, 37. [Google Scholar] [CrossRef] [PubMed]
- EFSA Use of the EFSA Comprehensive European Food Consumption Database in Exposure Assessment. EFSA J. 2011, 9. [CrossRef]
- EFSA General Principles for the Collection of National Food Consumption Data in the View of a Pan-European Dietary Survey. EFSA J. 2009. [CrossRef]
- EFSA Guidance on the EU Menu Methodology. EFSA J. 2014, 12. [CrossRef] [Green Version]
- EFSA The Food Classification and Description System FoodEx 2 (Revision 2). EFSA Support. Publ. 2015, 12. [CrossRef] [Green Version]
- European Commission Report from the Commission on Dietary Food Additive Intake in the European Union. COM(2001) 0542 Final. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A52001DC0542 (accessed on 10 August 2022).
- EFSA Overview of the Procedures Currently Used at EFSA for the Assessment of Dietary Exposure to Different Chemical Substances. EFSA J. 2011. [CrossRef]
- Nikolic, M.; Ioannidou, S.; Tard, A.; Arcella, D. Mapping of FoodEx2 Exposure Hierarchy with the Food Categories of Annex II (Part D) of Regulation (EC) No 1333/2008 on Food Additives (Version 1) [Data set]. ZENODO 2021. [Google Scholar] [CrossRef]
- Kalaycıoğlu, Z.; Erim, F.B. Nitrate and Nitrites in Foods: Worldwide Regional Distribution in View of Their Risks and Benefits. J. Agric. Food Chem. 2019, 67, 7205–7222. [Google Scholar] [CrossRef]
- van den Brand, A.D.; Beukers, M.; Niekerk, M.; van Donkersgoed, G.; van der Aa, M.; van de Ven, B.; Bulder, A.; van der Voet, H.; Sprong, C.R. Assessment of the Combined Nitrate and Nitrite Exposure from Food and Drinking Water: Application of Uncertainty around the Nitrate to Nitrite Conversion Factor. Food Addit. Contam. Part A 2020, 37, 568–582. [Google Scholar] [CrossRef] [PubMed]
- Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). Revised on November 2005. Available online: https://sites.google.com/site/theipaq/scoring-protocol (accessed on 15 June 2022).
- Cole, T.J.; Lobstein, T. Extended International (IOTF) Body Mass Index Cut-Offs for Thinness, Overweight and Obesity: Extended International BMI Cut-Offs. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Magriplis, E.; Marakis, G.; Kotopoulou, S.; Naska, A.; Michas, G.; Micha, R.; Panagiotakos, D.; Zampelas, A. Trans Fatty Acid Intake Increases Likelihood of Dyslipidemia Especially among Individuals with Higher Saturated Fat Consumption. Rev. Cardiovasc. Med. 2022, 23, 130. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary Patterns: A Mediterranean Diet Score and Its Relation to Clinical and Biological Markers of Cardiovascular Disease Risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Magriplis, E.; Panagiotakos, D.; Mitsopoulou, A.-V.; Karageorgou, D.; Bakogianni, I.; Dimakopoulos, I.; Micha, R.; Michas, G.; Chourdakis, M.; Chrousos, G.P.; et al. Prevalence of Hyperlipidaemia in Adults and Its Relation to the Mediterranean Diet: The Hellenic National Nutrition and Health Survey (HNNHS). Eur. J. Prev. Cardiol. 2019, 26, 1957–1967. [Google Scholar] [CrossRef] [PubMed]
- Hellenic Statistical Authority Greece in Figures. Available online: https://www.statistics.gr/documents/20181/17831637/GreeceInFigures_2022Q2_EN.pdf/752939fa-ddfa-7b03-3b75-29b8bd0ee105 (accessed on 31 August 2022).
- Larsson, K.; Darnerud, P.O.; Ilbäck, N.-G.; Merino, L. Estimated Dietary Intake of Nitrite and Nitrate in Swedish Children. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2011, 28, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Vlachou, C.; Hofstädter, D.; Rauscher - Gabernig, E.; Griesbacher, A.; Fuchs, K.; König, J. Risk Assessment of Nitrites for the Austrian Adult Population with Probabilistic Modelling of the Dietary Exposure. Food Chem. Toxicol. 2020, 143, 111480. [Google Scholar] [CrossRef] [PubMed]
- Thomson, B.M.; Nokes, C.J.; Cressey, P.J. Intake and Risk Assessment of Nitrate and Nitrite from New Zealand Foods and Drinking Water. Food Addit. Contam. 2007, 24, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Menard, C.; Heraud, F.; Volatier, J.-L.; Leblanc, J.-C. Assessment of Dietary Exposure of Nitrate and Nitrite in France. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2008, 25, 971–988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ΕFSA Opinion of the Scientific Committee Related to Uncertainties in Dietary Exposure Assessment. EFSA J. 2007. [CrossRef]
- Bemrah, N.; Vin, K.; Sirot, V.; Aguilar, F.; Ladrat, A.-C.; Ducasse, C.; Gey, J.-L.; Rétho, C.; Nougadere, A.; Leblanc, J.-C. Assessment of Dietary Exposure to Annatto (E160b), Nitrites (E249-250), Sulphites (E220-228) and Tartaric Acid (E334) in the French Population: The Second French Total Diet Study. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2012, 29, 875–885. [Google Scholar] [CrossRef] [PubMed]
- Diouf, F.; Berg, K.; Ptok, S.; Lindtner, O.; Heinemeyer, G.; Heseker, H. German Database on the Occurrence of Food Additives: Application for Intake Estimation of Five Food Colours for Toddlers and Children. Food Addit. Contam. Part Chem. Anal. Control Expo. Risk Assess. 2014, 31, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Honikel, K.-O. The Use and Control of Nitrate and Nitrite for the Processing of Meat Products. Meat Sci. 2008, 78, 68–76. [Google Scholar] [CrossRef] [PubMed]



| Age Group | Dietary Exposure to Nitrite | |||||
|---|---|---|---|---|---|---|
| Median | Mean | 95th Percentile | ||||
| mg/kg bw/day | % ADI 1 | mg/kg bw/day | % ADI | mg/kg bw/day | % ADI | |
| Minors (<18 years) 2 | 0.014 | 14.3 | 0.030 | 42.9 | 0.126 | 180.0 |
| Children 0–9 years | 0.02 | 28.6 | 0.038 | 54.3 | 0.173 | 247.1 |
| Adolescents 10–17 years | 0.01 | 14.3 | 0.022 | 31.4 | 0.076 | 108.6 |
| Adults (≥18 years) 3 | 0.007 | 10.0 | 0.021 | 30.0 | 0.078 | 111.4 |
| Young adults 18–30 years | 0.008 | 11.4 | 0.025 | 35.7 | 0.087 | 124.3 |
| Adults 31–50 years | 0.007 | 10 | 0.020 | 28.6 | 0.079 | 112.9 |
| Older adults 51–64 years | 0.004 | 5.7 | 0.014 | 20.0 | 0.056 | 80 |
| The elderly ≥65 years | 0.003 | 4.3 | 0.008 | 11.4 | 0.048 | 68.6 |
| Total | 0.007 | 10 | 0.022 | 31.4 | 0.173 | 118.6 |
| Variable 1 | Total N = 2152 | Below ADI N = 2009 (93.4%) | Above ADI N = 143 (6.6%) | p-Value (by Intake Level) 2 |
|---|---|---|---|---|
| Age(years), median (IQR) | 29 (21, 42) | 29 (21, 42) | 26 (15, 36) | <0.001 |
| Age group (years), n (%) | <0.001 | |||
| Children (0–9) | 190 (8.8) | 161 (8.0) | 29 (20.3) | |
| Adolescents (10–17) | 188 (8.7) | 176 (8.8) | 12 (8.4) | |
| Young adults (18–30) | 782 (36.4) | 729 (36.3) | 53 (37.0) | |
| Adults (31–50) | 664 (30.9) | 624 (31.0) | 40 (28.0) | |
| Older adults (51–64) | 211 (9.8) | 203 (10.1) | 8 (5.6) | |
| Elderly (>=65) | 117 (5.4) | 116 (5.8) | 1 (0.7) | |
| Sex, n (%) | <0.001 | |||
| Females | 1144 (53.3) | 1088 (54.4) | 56 (39.2) | |
| Males | 1001 (46.7) | 914 (45.6) | 87 (60.8) | |
| Weight (kg), mean (sd) | 67.9 (20.7) | 68.2 (20.4) | 62.9 (24.2) | <0.05 |
| Area of residence, n (%) | 0.215 | |||
| Attiki and Thessaloniki | 1429 (67.0) | 1335 (67.1) | 94 (66.7) | |
| Islands (including Crete) | 219 (10.3) | 199 (10.0) | 20 (14.2) | |
| Mainland | 483 (22.7) | 456 (22.9) | 27 (19.1) | |
| Marital status 3, n (%) | 0.165 | |||
| Divorced/Separated/Widowed/Single | 1044 (62.0) | 980 (61.6) | 64 (68.8) | |
| Married/Cohabiting | 639 (38.0) | 610 (38.4) | 29 (31.2) | |
| Education level 3, n (%) | 0.146 | |||
| Up to 6 years of school | 88 (5.1) | 87 (5.3) | 1 (1.1) | |
| 12 years of school | 661 (38.4) | 626 (38.5) | 35 (36.8) | |
| Higher education (including colleges) | 974 (56.5) | 915 (56.2) | 59 (62.1) | |
| Employment status 3, n (%) | 0.034 | |||
| Unemployed | 535 (31.0) | 507 (31.1) | 28 (29.2) | |
| Employed | 1009 (58.5) | 944 (58.0) | 65 (67.7) | |
| Pension | 180 (10.5) | 177 (10.9) | 3 (3.1) | |
| Smoking status 3, n (%) | 0.119 | |||
| Never smoker | 847 (48.1) | 801 (48.3) | 46 (45.1) | |
| Current smoker | 656 (37.3) | 622 (37.5) | 34 (33.3) | |
| Ex-smoker | 257 (14.6) | 235 (14.2) | 22 (21.6) | |
| Physical activity status 3,4, n (%) | 0.930 | |||
| Low | 255 (15.5) | 239 (15.3) | 16 (17.2) | |
| Moderate | 624 (37.8) | 588 (37.8) | 36 (38.7) | |
| Sedentary | 101 (6.1) | 95 (6.1) | 6 (6.5) | |
| Very | 670 (40.6) | 635 (40.8) | 35 (37.6) | |
| Total energy intake (kcal/day), median (IQR) | 1917.8 (1443.1, 2518.5) | 1894.4 (1433.7, 2493.3) | 2249.9 (1639.6, 3357.4) | <0.001 |
| Total fat intake (%energy) 3, mean (sd) | 38.1 (9.5) | 38.0 (9.5) | 39.6 (9.5) | 0.1246 |
| Total TFA intake (%energy) 3, median (IQR) | 0.6 (0.4, 0.8) | 0.5 (0.4, 0.8) | 0.6 (0.4, 0.8) | 0.3107 |
| Total SFA intake (%energy) 3, mean (sd) | 13.4 (4.0) | 13.4 (4.0) | 13.9 (4.0) | 0.2235 |
| Total sodium intake (mg), mean (sd) | 2303 (690.1) | 2276.3 (666.2) | 2770.3 (906.1) | <0.001 |
| Sodium intake 3, n (%) | <0.001 | |||
| <1500 | 104 (6.4) | 103 (6.7) | 1 (1.1) | |
| >=1500 and <2300 | 851 (52.3) | 816 (53.1) | 35 (38.5) | |
| >=2300 | 673 (41.3) | 618 (40.2) | 55 (60.4) | |
| BMI adults(kg/m2) 3,5 mean (sd) | 24.0 (5.2) | 24.0 (5.2) | 23.0 (5.1) | 0.020 |
| BMI adults categories 3,5, n (%) | 0.488 | |||
| Healthy weight | 977 (56.6) | 921 (56.6) | 56 (57.1) | |
| Overweight | 507 (29.4) | 475 (29.2) | 32 (32.7) | |
| Obese | 241 (14.0) | 231 (14.2) | 10 (10.2) | |
| BMI children 6, mean (sd) | 18.8 (4.2) | 18.9 (4.3) | 18.1 (3.8) | 0.2680 |
| BMI children categories 5,6, n (%) | 0.602 | |||
| Healthy weight | 332 (92.2) | 293 (91.8) | 39 (95.1) | |
| Overweight | 21 (5.8) | 19 (6.0) | 2 (4.9) | |
| Obese | 7 (2.0) | 7 (2.2) | 0 (0) | |
| MedDiet score 3, mean (sd) | 27.0 (6.4) | 27.1 (6.3) | 25.0 (6.5) | <0.05 |
| MedDiet category 3, n (%) | <0.05 | |||
| MD < 23 | 373 (22.9) | 341 (22.2) | 32 (35.2) | |
| MD >= 23 | 1255 (77.1) | 1196 (77.8) | 59 (64.8) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotopoulou, S.; Zampelas, A.; Magriplis, E. Risk Assessment of Nitrite and Nitrate Intake from Processed Meat Products: Results from the Hellenic National Nutrition and Health Survey (HNNHS). Int. J. Environ. Res. Public Health 2022, 19, 12800. https://doi.org/10.3390/ijerph191912800
Kotopoulou S, Zampelas A, Magriplis E. Risk Assessment of Nitrite and Nitrate Intake from Processed Meat Products: Results from the Hellenic National Nutrition and Health Survey (HNNHS). International Journal of Environmental Research and Public Health. 2022; 19(19):12800. https://doi.org/10.3390/ijerph191912800
Chicago/Turabian StyleKotopoulou, Sotiria, Antonis Zampelas, and Emmanuella Magriplis. 2022. "Risk Assessment of Nitrite and Nitrate Intake from Processed Meat Products: Results from the Hellenic National Nutrition and Health Survey (HNNHS)" International Journal of Environmental Research and Public Health 19, no. 19: 12800. https://doi.org/10.3390/ijerph191912800