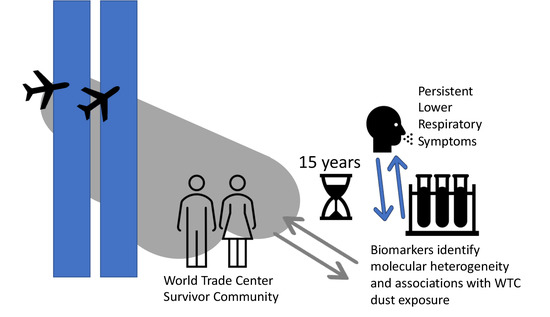
Molecular Clustering Analysis of Blood Biomarkers in World Trade Center Exposed Community Members with Persistent Lower Respiratory Symptoms
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Patients
2.3. Samples
2.4. Multiplex Assays
2.5. Statistical Analysis
3. Results
3.1. Demographic Characteristic of Study Populations
3.2. Biomarker Analysis and Hierarchical Clustering
3.3. Comparison of WTC Clusters 1 and 2 for Biomarker Levels
3.4. Comparison of WTC Clusters 1 and 2 for WTC Exposures
3.5. Comparison of WTC Exposure Categories for Biomarker Levels
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Prezant, D.J.; Weiden, M.; Banauch, G.I.; McGuinness, G.; Rom, W.N.; Aldrich, T.K.; Kelly, K.J. Cough and bronchial responsiveness in firefighters at the world trade center site. N. Engl. J. Med. 2002, 347, 806–815. [Google Scholar] [CrossRef] [PubMed]
- Oppenheimer, B.W.; Goldring, R.M.; Herberg, M.E.; Hofer, I.S.; Reyfman, P.A.; Liautaud, S.; Rom, W.N.; Reibman, J.; Berger, K.I. Distal airway function in symptomatic subjects with normal spirometry following world trade center dust exposure. Chest 2007, 132, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Reibman, J.; Liu, M.; Cheng, Q.; Liautaud, S.; Rogers, L.; Lau, S.; Berger, K.I.; Goldring, R.M.; Marmor, M.; Fernandez-Beros, M.E.; et al. Characteristics of a residential and working community with diverse exposure to world trade center dust, gas, and fumes. J. Occup. Environ. Med. 2009, 51, 534–541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiden, M.D.; Ferrier, N.; Nolan, A.; Rom, W.N.; Comfort, A.; Gustave, J.; Zeig-Owens, R.; Zheng, S.; Goldring, R.M.; Berger, K.I.; et al. Obstructive airways disease with air trapping among firefighters exposed to world trade center dust. Chest 2010, 137, 566–574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reibman, J.; Caplan-Shaw, C.; Wu, Y.; Liu, M.; Amin, M.R.; Berger, K.I.; Cotrina-Vidal, M.L.; Kazeros, A.; Durmus, N.; Fernandez-Beros, M.E.; et al. Characterization of persistent uncontrolled asthma symptoms in community members exposed to world trade center dust and fumes. Int. J. Environ. Res. Public Health 2020, 17, 6645. [Google Scholar] [CrossRef]
- Jordan, H.T.; Friedman, S.M.; Reibman, J.; Goldring, R.M.; Archie, S.A.M.; Ortega, F.; Alper, H.; Shao, Y.; Maslow, C.B.; Cone, J.E.; et al. Risk factors for persistence of lower respiratory symptoms among community members exposed to the 2001 world trade center terrorist attacks. Occup. Environ. Med. 2017, 74, 449–455. [Google Scholar] [CrossRef]
- Caplan-Shaw, C.; Kazeros, A.; Pradhan, D.; Berger, K.; Goldring, R.; Zhao, S.; Liu, M.; Shao, Y.; Fernandez-Beros, M.E.; Marmor, M.; et al. Improvement in severe lower respiratory symptoms and small airway function in world trade center dust exposed community members. Am. J. Ind. Med. 2016, 59, 777–787. [Google Scholar] [CrossRef]
- Kazeros, A.; Zhang, E.; Cheng, X.; Shao, Y.; Liu, M.; Qian, M.; Caplan-Shaw, C.; Berger, K.I.; Goldring, R.M.; Ghumman, M.; et al. Systemic inflammation associated with world trade center dust exposures and airway abnormalities in the local community. J. Occup. Environ. Med. 2015, 57, 610–616. [Google Scholar] [CrossRef]
- Lippmann, M.; Cohen, M.D.; Chen, L.C. Health effects of world trade center (wtc) dust: An unprecedented disaster’s inadequate risk management. Crit. Rev. Toxicol. 2015, 45, 492–530. [Google Scholar] [CrossRef]
- Takeda, N.; Maghni, K.; Daigle, S.; L’Archeveque, J.; Castellanos, L.; Al-Ramli, W.; Malo, J.L.; Hamid, Q. Long-term pathologic consequences of acute irritant-induced asthma. J. Allergy Clin. Immunol. 2009, 124, 975–981.e1. [Google Scholar] [CrossRef]
- Cormier, M.; Lemiere, C. Occupational asthma. Int. J. Tuberc. Lung Dis. 2020, 24, 8–21. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.M.; Bernstein, I.L. Irritant-induced airway disorders. Immunol. Allergy Clin. N. Am. 2011, 1, 747–768. [Google Scholar] [CrossRef] [PubMed]
- Sumi, Y.; Foley, S.; Daigle, S.; L’Archeveque, J.; Olivenstein, R.; Letuve, S.; Malo, J.L.; Hamid, Q. Structural changes and airway remodelling in occupational asthma at a mean interval of 14 years after cessation of exposure. Clin. Exp. Allergy 2007, 37, 1781–1787. [Google Scholar] [CrossRef]
- Gomez, J.L.; Yan, X.; Holm, C.T.; Grant, N.; Liu, Q.; Cohn, L.; Nezgovorova, V.; Meyers, D.A.; Bleecker, E.R.; Crisafi, G.M.; et al. Characterisation of asthma subgroups associated with circulating ykl-40 levels. Eur. Respir. J. 2017, 50, 1700800. [Google Scholar] [CrossRef] [Green Version]
- Reibman, J.; Marmor, M.; Filner, J.; Fernandez-Beros, M.E.; Rogers, L.; Perez-Perez, G.I.; Blaser, M.J. Asthma is inversely associated with helicobacter pylori status in an urban population. PLoS ONE 2008, 3, e4060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamura, Y.; Phan, C.; Tu, L.; le Hiress, M.; Thuillet, R.; Jutant, E.M.; Fadel, E.; Savale, L.; Huertas, A.; Humbert, M.; et al. Ectopic upregulation of membrane-bound il6r drives vascular remodeling in pulmonary arterial hypertension. J. Clin. Investig. 2018, 128, 1956–1970. [Google Scholar] [CrossRef] [Green Version]
- Chirinos, J.A.; Orlenko, A.; Zhao, L.; Basso, M.D.; Cvijic, M.E.; Li, Z.; Spires, T.E.; Yarde, M.; Wang, Z.; Seiffert, D.A.; et al. Multiple plasma biomarkers for risk stratification in patients with heart failure and preserved ejection fraction. J. Am. Coll. Cardiol. 2020, 75, 1281–1295. [Google Scholar] [CrossRef] [PubMed]
- Peeters, S.A.; Engelen, L.; Buijs, J.; Chaturvedi, N.; Fuller, J.H.; Schalkwijk, C.G.; Stehouwer, C.D.; EURODIAB Prospective Complications Study Group. Plasma levels of matrix metalloproteinase-2, -3, -10, and tissue inhibitor of metalloproteinase-1 are associated with vascular complications in patients with type 1 diabetes: The eurodiab prospective complications study. Cardiovas. Diabetol. 2015, 14, 31. [Google Scholar] [CrossRef] [Green Version]
- Todd, J.L.; Vinisko, R.; Liu, Y.; Neely, M.L.; Overton, R.; Flaherty, K.R.; Noth, I.; Newby, L.K.; Lasky, J.A.; Olman, M.A.; et al. Circulating matrix metalloproteinases and tissue metalloproteinase inhibitors in patients with idiopathic pulmonary fibrosis in the multicenter ipf-pro registry cohort. BMC Pulm. Med. 2020, 20, 64. [Google Scholar] [CrossRef] [Green Version]
- Crowley, G.; Kim, J.; Kwon, S.; Lam, R.; Prezant, D.J.; Liu, M.; Nolan, A. Pedf, a pleiotropic wtc-li biomarker: Machine learning biomarker identification and validation. PLoS Comput. Biol. 2021, 17, e1009144. [Google Scholar] [CrossRef]
- Cleven, K.L.; Rosenzvit, C.; Nolan, A.; Zeig-Owens, R.; Kwon, S.; Weiden, M.D.; Skerker, M.; Halpren, A.; Prezant, D.J. Twenty-year reflection on the impact of world trade center exposure on pulmonary outcomes in fire department of the city of new york (fdny) rescue and recovery workers. Lung 2021, 199, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Haider, S.H.; Veerappan, A.; Crowley, G.; Caraher, E.J.; Ostrofsky, D.; Mikhail, M.; Lam, R.; Wang, Y.; Sunseri, M.; Kwon, S.; et al. Multiomics of world trade center particulate matter-induced persistent airway hyperreactivity. Role of receptor for advanced glycation end products. Am. J. Respir. Cell Mol. Biol. 2020, 63, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Haider, S.H.; Oskuei, A.; Crowley, G.; Kwon, S.; Lam, R.; Riggs, J.; Mikhail, M.; Talusan, A.; Veerappan, A.; Kim, J.S.; et al. Receptor for advanced glycation end-products and environmental exposure related obstructive airways disease: A systematic review. Eur. Respir. Rev. 2019, 28, 180096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeig-Owens, R.; Singh, A.; Aldrich, T.K.; Hall, C.B.; Schwartz, T.; Webber, M.P.; Cohen, H.W.; Kelly, K.J.; Nolan, A.; Prezant, D.J.; et al. Blood leukocyte concentrations, fev1 decline, and airflow limitation. A 15-year longitudinal study of world trade center-exposed firefighters. Ann. Am. Thorac. Soc. 2018, 15, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Liu, C.; Putman, B.; Zeig-Owens, R.; Hall, C.B.; Schwartz, T.; Webber, M.P.; Cohen, H.W.; Berger, K.I.; Nolan, A.; et al. Predictors of asthma/copd overlap in fdny firefighters with world trade center dust exposure: A longitudinal study. Chest 2018, 154, 1301–1310. [Google Scholar] [CrossRef]
- Crowley, G.; Kwon, S.; Haider, S.H.; Caraher, E.J.; Lam, R.; St-Jules, D.E.; Liu, M.; Prezant, D.J.; Nolan, A. Metabolomics of world trade center-lung injury: A machine learning approach. BMJ Open. Respir. Res. 2018, 5, e000274. [Google Scholar] [CrossRef]
- Caraher, E.J.; Kwon, S.; Haider, S.H.; Crowley, G.; Lee, A.; Ebrahim, M.; Zhang, L.; Chen, L.C.; Gordon, T.; Liu, M.; et al. Receptor for advanced glycation end-products and world trade center particulate induced lung function loss: A case-cohort study and murine model of acute particulate exposure. PLoS ONE 2017, 12, e0184331. [Google Scholar] [CrossRef]
- Weiden, M.D.; Kwon, S.; Caraher, E.; Berger, K.I.; Reibman, J.; Rom, W.N.; Prezant, D.J.; Nolan, A. Biomarkers of world trade center particulate matter exposure: Physiology of distal airway and blood biomarkers that predict fev(1) decline. In Seminars in Respiratory and Critical Care Medicine; Thieme Medical Publisher: New York, NY, USA, 2015; Volume 36, pp. 323–333. [Google Scholar] [CrossRef] [Green Version]
- Kwon, S.; Weiden, M.D.; Echevarria, G.C.; Comfort, A.L.; Naveed, B.; Prezant, D.J.; Rom, W.N.; Nolan, A. Early elevation of serum mmp-3 and mmp-12 predicts protection from world trade center-lung injury in new york city firefighters: A nested case-control study. PLoS ONE 2013, 8, e76099. [Google Scholar] [CrossRef]
- Nolan, A.; Kwon, S.; Cho, S.J.; Naveed, B.; Comfort, A.L.; Prezant, D.J.; Rom, W.N.; Weiden, M.D. Mmp-2 and timp-1 predict healing of wtc-lung injury in new york city firefighters. Respir. Res. 2014, 15, 5. [Google Scholar] [CrossRef] [Green Version]
- Hankinson, J.L.; Odencrantz, J.R.; Fedan, K.B. Spirometric reference values from a sample of the general U.S. Population. Am. J. Respir. Crit. Care Med. 1999, 159, 179–187. [Google Scholar] [CrossRef] [Green Version]
- Defawe, O.D.; Fong, Y.; Vasilyeva, E.; Pickett, M.; Carter, D.K.; Gabriel, E.; Rerks-Ngarm, S.; Nitayaphan, S.; Frahm, N.; McElrath, M.J.; et al. Optimization and qualification of a multiplex bead array to assess cytokine and chemokine production by vaccine-specific cells. J. Immunol. Methods 2012, 382, 117–128. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Zhou, T.; Zhang, Y.; Yang, E.S.; Schramm, C.A.; Shi, W.; Pegu, A.; Oloniniyi, O.K.; Henry, A.R.; Darko, S.; et al. Ultrapotent antibodies against diverse and highly transmissible sars-cov-2 variants. Science 2021, 373, eabh1766. [Google Scholar] [CrossRef]
- Azadeh, M.; Gorovits, B.; Kamerud, J.; MacMannis, S.; Safavi, A.; Sailstad, J.; Sondag, P. Calibration curves in quantitative ligand binding assays: Recommendations and best practices for preparation, design, and editing of calibration curves. AAPS J. 2017, 20, 22. [Google Scholar] [CrossRef]
- Liu, M.; Qian, M.; Cheng, Q.; Berger, K.I.; Shao, Y.; Turetz, M.; Kazeros, A.; Parsia, S.; Goldring, R.M.; Caplan-Shaw, C.; et al. Longitudinal spirometry among patients in a treatment program for community members with world trade center-related illness. J. Occup. Environ. Med. 2012, 54, 1208–1213. [Google Scholar] [CrossRef] [Green Version]
- Arslan, A.A.; Tuminello, S.; Yang, L.; Zhang, Y.; Durmus, N.; Snuderl, M.; Heguy, A.; Zeleniuch-Jacquotte, A.; Shao, Y.; Reibman, J. Genome-wide DNA methylation profiles in community members exposed to the world trade center disaster. Int. J. Environ. Res. Public Health 2020, 17, 5493. [Google Scholar] [CrossRef]
- Shao, Y.; Durmus, N.; Zhang, Y.; Pehlivan, S.; Fernandez-Beros, M.E.; Umana, L.; Corona, R.; Addessi, A.; Abbott, S.A.; Smyth-Giambanco, S.; et al. The development of a wtc environmental health center pan-cancer database. Int. J. Environ. Res. Public Health 2021, 18, 1646. [Google Scholar] [CrossRef]
- Durmus, N.; Pehlivan, S.; Zhang, Y.; Shao, Y.; Arslan, A.A.; Corona, R.; Henderson, I.; Sterman, D.H.; Reibman, J. Lung cancer characteristics in the world trade center environmental health center. Int. J. Environ. Res. Public Health 2021, 18, 2689. [Google Scholar] [CrossRef]
- Arslan, A.A.; Zhang, Y.; Durmus, N.; Pehlivan, S.; Addessi, A.; Schnabel, F.; Shao, Y.; Reibman, J. Breast cancer characteristics in the population of survivors participating in the world trade center environmental health center program 2002–2019. Int. J. Environ. Res. Public Health 2021, 18, 7555. [Google Scholar] [CrossRef]
- Durmus, N.; Shao, Y.; Arslan, A.A.; Zhang, Y.; Pehlivan, S.; Fernandez-Beros, M.E.; Umana, L.; Corona, R.; Smyth-Giambanco, S.; Abbott, S.A.; et al. Characteristics of cancer patients in the world trade center environmental health center. Int. J. Environ. Res. Public Health 2020, 17, 7190. [Google Scholar] [CrossRef]
- Rosen, R.; Shao, Y.; Zhang, Q.; Bao, J.; Zhang, Y.; Masurkar, A.; Wisniewski, T.; Urban, N.; Reibman, J. Cognitive function among world trade center-exposed community members with mental health symptoms. Int. J. Environ. Res. Public Health 2022, 19, 3440. [Google Scholar] [CrossRef]
- Clouston, S.A.P.; Hall, C.B.; Kritikos, M.; Bennett, D.A.; DeKosky, S.; Edwards, J.; Finch, C.; Kreisl, W.C.; Mielke, M.; Peskind, E.R.; et al. Cognitive impairment and world trade centre-related exposures. Nat. Rev. Neurol. 2022, 18, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Baba, R.Y.; Zhang, Y.; Shao, Y.; Berger, K.I.; Goldring, R.M.; Liu, M.; Kazeros, A.; Rosen, R.; Reibman, J. Copd in smoking and non-smoking community members exposed to the world trade center dust and fumes. Int. J. Environ. Res. Public Health 2022, 19, 4249. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R.; Zhu, Z.; Shao, Y.; Liu, M.; Bao, J.; Levy-Carrick, N.; Reibman, J. Longitudinal change of ptsd symptoms in community members after the world trade center destruction. Int. J. Environ. Res. Public Health 2019, 16, 1215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosen, R.L.; Levy-Carrick, N.; Reibman, J.; Xu, N.; Shao, Y.; Liu, M.; Ferri, L.; Kazeros, A.; Caplan-Shaw, C.E.; Pradhan, D.R.; et al. Elevated c-reactive protein and posttraumatic stress pathology among survivors of the 9/11 world trade center attacks. J. Psychiatr. Res. 2017, 89, 14–21. [Google Scholar] [CrossRef]
- Marmor, M.; Shao, Y.; Bhatt, D.H.; Stecker, M.M.; Berger, K.I.; Goldring, R.M.; Rosen, R.L.; Caplan-Shaw, C.; Kazeros, A.; Pradhan, D.; et al. Paresthesias among community members exposed to the world trade center disaster. J. Occup. Environ. Med. 2017, 59, 389–396. [Google Scholar] [CrossRef] [Green Version]
- Ait-Oufella, H.; Yu, M.; Kotti, S.; Georges, A.; Vandestienne, M.; Joffre, J.; Roubille, F.; Angoulvant, D.; Santos-Zas, I.; Tedgui, A.; et al. Plasma and genetic determinants of soluble trem-1 and major adverse cardiovascular events in a prospective cohort of acute myocardial infarction patients. Results from the fast-mi 2010 study. Int. J. Cardiol. 2021, 344, 213–219. [Google Scholar] [CrossRef]
- Jonsson, A.; Hjalmarsson, C.; Falk, P.; Ivarsson, M.L. Levels of matrix metalloproteinases differ in plasma and serum—aspects regarding analysis of biological markers in cancer. Br. J. Cancer 2016, 115, 703–706. [Google Scholar] [CrossRef] [Green Version]
- Mannello, F. Serum or plasma samples? The “Cinderella” role of blood collection procedures: Preanalytical methodological issues influence the release and activity of circulating matrix metalloproteinases and their tissue inhibitors, hampering diagnostic trueness and leading to misinterpretation. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 611–614. [Google Scholar] [CrossRef] [Green Version]
- Thrailkill, K.; Cockrell, G.; Simpson, P.; Moreau, C.; Fowlkes, J.; Bunn, R.C. Physiological matrix metalloproteinase (mmp) concentrations: Comparison of serum and plasma specimens. Clin. Chem. Lab. Med. 2006, 44, 503–504. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Qin, L.; Zhang, P.; Li, K.; Liang, L.; Sun, J.; Xu, B.; Dai, Y.; Li, X.; Zhang, C.; et al. Longitudinal COVID-19 profiling associates il-1ra and il-10 with disease severity and rantes with mild disease. JCI Insight 2020, 5, e139834. [Google Scholar] [CrossRef]
- Urpi-Sarda, M.; Casas, R.; Chiva-Blanch, G.; Romero-Mamani, E.S.; Valderas-Martinez, P.; Salas-Salvado, J.; Covas, M.I.; Toledo, E.; Andres-Lacueva, C.; Llorach, R.; et al. The mediterranean diet pattern and its main components are associated with lower plasma concentrations of tumor necrosis factor receptor 60 in patients at high risk for cardiovascular disease. J. Nutr. 2012, 142, 1019–1025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, S.C.; Yang, K.C.; Hu, C.J.; Chiou, H.Y.; Wu, C.C.; Jeng, J.S. Elevated plasma level of soluble form of rage in ischemic stroke patients with dementia. Neuromol. Med. 2017, 19, 579–583. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bennett, P.C.; Gill, P.S.; Silverman, S.; Blann, A.D.; Balakrishnan, B.; Lip, G.Y. Ethnic/racial differences in circulating markers of angiogenesis and their association with cardiovascular risk factors and cardiovascular disease. Int. J. Cardiol. 2013, 167, 1247–1250. [Google Scholar] [CrossRef]
- Hachim, M.Y.; Elemam, N.M.; Ramakrishnan, R.K.; Hachim, I.Y.; Salameh, L.; Mahboub, B.; Al Heialy, S.; Halwani, R.; Hamoudi, R.; Hamid, Q. Confounding patient factors affecting the proper interpretation of the periostin level as a biomarker in asthma development. J. Asthma Allergy 2020, 13, 23–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wenzel, S.; Ford, L.; Pearlman, D.; Spector, S.; Sher, L.; Skobieranda, F.; Wang, L.; Kirkesseli, S.; Rocklin, R.; Bock, B.; et al. Dupilumab in persistent asthma with elevated eosinophil levels. N. Engl. J. Med. 2013, 368, 2455–2466. [Google Scholar] [CrossRef]
- Lam, R.; Haider, S.H.; Crowley, G.; Caraher, E.J.; Ostrofsky, D.F.; Talusan, A.; Kwon, S.; Prezant, D.J.; Wang, Y.; Liu, M.; et al. Synergistic effect of wtc-particulate matter and lysophosphatidic acid exposure and the role of rage: In-vitro and translational assessment. Int. J. Environ. Res. Public Health 2020, 17, 4318. [Google Scholar] [CrossRef]
- Cho, S.J.; Echevarria, G.C.; Lee, Y.I.; Kwon, S.; Park, K.Y.; Tsukiji, J.; Rom, W.N.; Prezant, D.J.; Nolan, A.; Weiden, M.D. Ykl-40 is a protective biomarker for fatty liver in world trade center particulate matter-exposed firefighters. J. Mol. Biomark. Diagn. 2014, 5, 1000174. [Google Scholar] [CrossRef]
- Cho, S.J.; Nolan, A.; Echevarria, G.C.; Kwon, S.; Naveed, B.; Schenck, E.; Tsukiji, J.; Prezant, D.J.; Rom, W.N.; Weiden, M.D. Chitotriosidase is a biomarker for the resistance to world trade center lung injury in new york city firefighters. J. Clin. Immunol. 2013, 33, 1134–1142. [Google Scholar] [CrossRef] [Green Version]
- Cho, S.J.; Echevarria, G.C.; Kwon, S.; Naveed, B.; Schenck, E.J.; Tsukiji, J.; Rom, W.N.; Prezant, D.J.; Nolan, A.; Weiden, M.D. One airway: Biomarkers of protection from upper and lower airway injury after world trade center exposure. Respir. Med. 2014, 108, 162–170. [Google Scholar] [CrossRef] [Green Version]
- Haider, S.H.; Kwon, S.; Lam, R.; Lee, A.K.; Caraher, E.J.; Crowley, G.; Zhang, L.; Schwartz, T.M.; Zeig-Owens, R.; Liu, M.; et al. Predictive biomarkers of gastroesophageal reflux disease and barrett’s esophagus in world trade center exposed firefighters: A 15 year longitudinal study. Sci. Rep. 2018, 8, 3106. [Google Scholar] [CrossRef] [Green Version]
- Lam, R.; Kwon, S.; Riggs, J.; Sunseri, M.; Crowley, G.; Schwartz, T.; Zeig-Owens, R.; Colbeth, H.; Halpren, A.; Liu, M.; et al. Dietary phenotype and advanced glycation end-products predict wtc-obstructive airways disease: A longitudinal observational study. Respir. Res. 2021, 22, 19. [Google Scholar] [CrossRef]
- Kwon, S.; Lee, M.; Crowley, G.; Schwartz, T.; Zeig-Owens, R.; Prezant, D.J.; Liu, M.; Nolan, A. Dynamic metabolic risk profiling of world trade center lung disease: A longitudinal cohort study. Am. J. Respir. Crit. Care Med. 2021, 204, 1035–1047. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.; Crowley, G.; Mikhail, M.; Lam, R.; Clementi, E.; Zeig-Owens, R.; Schwartz, T.M.; Liu, M.; Prezant, D.J.; Nolan, A. Metabolic syndrome biomarkers of world trade center airway hyperreactivity: A 16-year prospective cohort study. Int. J. Environ. Res. Public Health 2019, 16, 1486. [Google Scholar] [CrossRef] [Green Version]
- Kwon, S.; Crowley, G.; Caraher, E.J.; Haider, S.H.; Lam, R.; Veerappan, A.; Yang, L.; Liu, M.; Zeig-Owens, R.; Schwartz, T.M.; et al. Validation of predictive metabolic syndrome biomarkers of world trade center lung injury: A 16-year longitudinal study. Chest 2019, 156, 486–496. [Google Scholar] [CrossRef]
- Crowley, G.; Kwon, S.; Ostrofsky, D.F.; Clementi, E.A.; Haider, S.H.; Caraher, E.J.; Lam, R.; St-Jules, D.E.; Liu, M.; Prezant, D.J.; et al. Assessing the protective metabolome using machine learning in world trade center particulate exposed firefighters at risk for lung injury. Sci. Rep. 2019, 9, 11939. [Google Scholar] [CrossRef] [Green Version]
- Clementi, E.A.; Talusan, A.; Vaidyanathan, S.; Veerappan, A.; Mikhail, M.; Ostrofsky, D.; Crowley, G.; Kim, J.S.; Kwon, S.; Nolan, A. Metabolic syndrome and air pollution: A narrative review of their cardiopulmonary effects. Toxics 2019, 7, 6. [Google Scholar] [CrossRef] [Green Version]
- Carbone, F.; Elia, E.; Casula, M.; Bonaventura, A.; Liberale, L.; Bertolotto, M.; Artom, N.; Minetti, S.; Dallegri, F.; Contini, P.; et al. Baseline hs-crp predicts hypertension remission in metabolic syndrome. Eur. J. Clin. Investig. 2019, 49, e13128. [Google Scholar] [CrossRef]
- Sherman, R.M.; Forman, J.; Antonescu, V.; Puiu, D.; Daya, M.; Rafaels, N.; Boorgula, M.P.; Chavan, S.; Vergara, C.; Ortega, V.E.; et al. Assembly of a pan-genome from deep sequencing of 910 humans of african descent. Nat. Genet. 2019, 51, 30–35. [Google Scholar] [CrossRef]
- Katz, D.H.; Tahir, U.A.; Bick, A.G.; Pampana, A.; Ngo, D.; Benson, M.D.; Yu, Z.; Robbins, J.M.; Chen, Z.Z.; Cruz, D.E.; et al. Whole genome sequence analysis of the plasma proteome in black adults provides novel insights into cardiovascular disease. Circulation 2022, 145, 357–370. [Google Scholar] [CrossRef]
- Ujfaludi, Z.; Tuzesi, A.; Majoros, H.; Rothler, B.; Pankotai, T.; Boros, I.M. Coordinated activation of a cluster of mmp genes in response to uvb radiation. Sci. Rep. 2018, 8, 2660. [Google Scholar] [CrossRef]
- Jackson, B.C.; Nebert, D.W.; Vasiliou, V. Update of human and mouse matrix metalloproteinase families. Hum. Genom. 2010, 4, 194–201. [Google Scholar] [CrossRef] [Green Version]
- Kahn, L.G.; Han, X.; Koshy, T.T.; Shao, Y.; Chu, D.B.; Kannan, K.; Trasande, L. Adolescents exposed to the world trade center collapse have elevated serum dioxin and furan concentrations more than 12years later. Environ. Int. 2018, 111, 268–278. [Google Scholar] [CrossRef]
- Edelman, P.; Osterloh, J.; Pirkle, J.; Caudill, S.P.; Grainger, J.; Jones, R.; Blount, B.; Calafat, A.; Turner, W.; Feldman, D.; et al. Biomonitoring of chemical exposure among new york city firefighters responding to the world trade center fire and collapse. Environ. Health Perspect. 2003, 111, 1906–1911. [Google Scholar] [CrossRef]
- Horii, Y.; Jiang, Q.; Hanari, N.; Lam, P.K.; Yamashita, N.; Jansing, R.; Aldous, K.M.; Mauer, M.P.; Eadon, G.A.; Kannan, K. Polychlorinated dibenzo-p-dioxins, dibenzofurans, biphenyls, and naphthalenes in plasma of workers deployed at the world trade center after the collapse. Environ. Sci. Technol. 2010, 44, 5188–5194. [Google Scholar] [CrossRef]
- Wolff, M.S.; Teitelbaum, S.L.; Lioy, P.J.; Santella, R.M.; Wang, R.Y.; Jones, R.L.; Caldwell, K.L.; Sjodin, A.; Turner, W.E.; Li, W.; et al. Exposures among pregnant women near the world trade center site on 11 september 2001. Environ. Health Perspect. 2005, 113, 739–748. [Google Scholar] [CrossRef] [Green Version]
- Trasande, L.; Koshy, T.T.; Gilbert, J.; Burdine, L.K.; Attina, T.M.; Ghassabian, A.; Honda, M.; Marmor, M.; Chu, D.B.; Han, X.; et al. Serum perfluoroalkyl substances in children exposed to the world trade center disaster. Environ. Res. 2017, 154, 212–221. [Google Scholar] [CrossRef] [Green Version]
- Koshy, T.T.; Attina, T.M.; Ghassabian, A.; Gilbert, J.; Burdine, L.K.; Marmor, M.; Honda, M.; Chu, D.B.; Han, X.; Shao, Y.; et al. Serum perfluoroalkyl substances and cardiometabolic consequences in adolescents exposed to the world trade center disaster and a matched comparison group. Environ. Int. 2017, 109, 128–135. [Google Scholar] [CrossRef]
- Spratlen, M.J.; Perera, F.P.; Sjodin, A.; Wang, Y.; Herbstman, J.B.; Trasande, L. Understanding the role of persistent organic pollutants and stress in the association between proximity to the world trade center disaster and birth outcomes. Int. J. Environ. Res. Public Health 2022, 19, 2008. [Google Scholar] [CrossRef]
- Spratlen, M.J.; Perera, F.P.; Lederman, S.A.; Rauh, V.A.; Robinson, M.; Kannan, K.; Trasande, L.; Herbstman, J. The association between prenatal exposure to perfluoroalkyl substances and childhood neurodevelopment. Environ. Pollut. 2020, 263, 114444. [Google Scholar] [CrossRef]
- Spratlen, M.J.; Perera, F.P.; Lederman, S.A.; Robinson, M.; Kannan, K.; Trasande, L.; Herbstman, J. Cord blood perfluoroalkyl substances in mothers exposed to the world trade center disaster during pregnancy. Environ. Pollut. 2019, 246, 482–490. [Google Scholar] [CrossRef]
- Trye, A.; Berger, K.I.; Naidu, M.; Attina, T.M.; Gilbert, J.; Koshy, T.T.; Han, X.; Marmor, M.; Shao, Y.; Giusti, R.; et al. Respiratory health and lung function in children exposed to the world trade center disaster. J. Pediatr. 2018, 201, 134–140.e6. [Google Scholar] [CrossRef]
- Trasande, L.; Koshy, T.T.; Gilbert, J.; Burdine, L.K.; Marmor, M.; Han, X.; Shao, Y.; Chemtob, C.; Attina, T.M.; Urbina, E.M. Cardiometabolic profiles of adolescents and young adults exposed to the world trade center disaster. Environ. Res. 2018, 160, 107–114. [Google Scholar] [CrossRef]
- Trasande, L.; Fiorino, E.K.; Attina, T.; Berger, K.; Goldring, R.; Chemtob, C.; Levy-Carrick, N.; Shao, Y.; Liu, M.; Urbina, E.; et al. Associations of world trade center exposures with pulmonary and cardiometabolic outcomes among children seeking care for health concerns. Sci. Total Environ. 2013, 444, 320–326. [Google Scholar] [CrossRef] [Green Version]
- Szema, A.M.; Savary, K.W.; Ying, B.L.; Lai, K. Post 9/11: High asthma rates among children in chinatown, new york. Allergy Asthma Proc. 2009, 30, 605–611. [Google Scholar] [CrossRef]
- Caruana, D.L.; Huang, P.H.; Li, J.C.; Cheslack-Postava, K.; Szema, A.M. Allergy and lung injury among rescue workers exposed to the world trade center disaster assessed 17 years after exposure to ground zero. J. Occup. Environ. Med. 2020, 62, e378–e383. [Google Scholar] [CrossRef]
- Thurston, G.D.; Balmes, J.R.; Garcia, E.; Gilliland, F.D.; Rice, M.B.; Schikowski, T.; van Winkle, L.S.; Annesi-Maesano, I.; Burchard, E.G.; Carlsten, C.; et al. Outdoor air pollution and new-onset airway disease. An official american thoracic society workshop report. Ann. Am. Thorac. Soc. 2020, 17, 387–398. [Google Scholar] [CrossRef]
- Lloyd, C.M.; Rankin, S.M. Chemokines in allergic airway disease. Curr. Opin. Pharmacol. 2003, 3, 443–448. [Google Scholar] [CrossRef] [Green Version]
- Makino, A.; Shibata, T.; Nagayasu, M.; Hosoya, I.; Nishimura, T.; Nakano, C.; Nagata, K.; Ito, T.; Takahashi, Y.; Nakamura, S. Rsv infection-elicited high mmp-12-producing macrophages exacerbate allergic airway inflammation with neutrophil infiltration. iScience 2021, 24, 103201. [Google Scholar] [CrossRef]
- Kong, D.H.; Kim, Y.K.; Kim, M.R.; Jang, J.H.; Lee, S. Emerging roles of vascular cell adhesion molecule-1 (vcam-1) in immunological disorders and cancer. Int. J. Mol. Sci. 2018, 19, 1057. [Google Scholar] [CrossRef] [Green Version]
- Hyder, L.A.; Gonzalez, J.; Harden, J.L.; Johnson-Huang, L.M.; Zaba, L.C.; Pierson, K.C.; Eungdamrong, N.J.; Lentini, T.; Gulati, N.; Fuentes-Duculan, J.; et al. Trem-1 as a potential therapeutic target in psoriasis. J. Investig. Dermatol. 2013, 133, 1742–1751. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, H.; Kawakita, A.; Okazaki, S.; Yasutomi, M.; Murai, H.; Ohshima, Y. Il-17a/f modulates fibrocyte functions in cooperation with cd40-mediated signaling. Inflammation 2013, 36, 830–838. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Liu, S.; Verma, M.; Zafar, I.; Good, J.T.; Rollins, D.; Groshong, S.; Gorska, M.M.; Martin, R.J.; Alam, R. Mechanism of th2/th17-predominant and neutrophilic th2/th17-low subtypes of asthma. J. Allergy Clin. Immunol. 2017, 139, 1548–1558.e4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, F.; Liu, P.; Li, J.; Zhang, Y. Eotaxin-1 promotes prostate cancer cell invasion via activation of the ccr3-erk pathway and upregulation of mmp-3 expression. Oncol. Rep. 2014, 31, 2049–2054. [Google Scholar] [CrossRef] [Green Version]
- Yan, S.F.; Ramasamy, R.; Naka, Y.; Schmidt, A.M. Glycation, inflammation, and rage: A scaffold for the macrovascular complications of diabetes and beyond. Circ. Res. 2003, 93, 1159–1169. [Google Scholar] [CrossRef] [Green Version]
- Brigham, E.P.; Woo, H.; McCormack, M.; Rice, J.; Koehler, K.; Vulcain, T.; Wu, T.; Koch, A.; Sharma, S.; Kolahdooz, F.; et al. Omega-3 and omega-6 intake modifies asthma severity and response to indoor air pollution in children. Am. J. Respir. Crit. Care Med. 2019, 199, 1478–1486. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Level | NYUBAR Control 1 | WTCS | p | Test | Missing (%) | |
|---|---|---|---|---|---|---|
| Age, mean (SD) | 40.2 (11.4) | 55.6 (10.2) | <0.001 | 0 | ||
| Gender, n (%) | F | 35 (63.6) | 51 (69.9) | 0.581 | 0 | |
| M | 20 (36.4) | 22 (30.1) | ||||
| BMI, mean (SD) | 28.9 (6.8) | 30.3 (5.4) | 0.219 | 0 | ||
| Ethnicity, n (%) | Black | 9 (16.4) | 20 (27.4) | 0.046 | exact | 0 |
| Latino | 36 (65.5) | 33 (45.2) | ||||
| White | 10 (18.2) | 15 (20.5) | ||||
| White Other | 0 (0) | 5 (6.8) | ||||
| Education, n (%) | Grade school (up to 6th grade) | 2 (3.6) | 3 (4.2) | 0.903 | 0.8 | |
| High school (12th grade) | 18 (32.7) | 26 (36.1) | ||||
| More than high school | 35 (63.6) | 43 (59.7) | ||||
| PrePre BD FVC % pred 2 (mean (SD)) | 93.1 (11.3) | 95.4 (15.5) | 0.352 | 0.8 | ||
| Post BD FVC % pred 2 (mean (SD)) | 92.1 (11.7) | 97.0 (14.9) | 0.047 | 2.3 | ||
| Pre BD FEV1 % pred 3 (mean (SD)) | 93.1 (11.3) | 93.1 (13.7) | 0.981 | 0.8 | ||
| Post BD FEV1 % pred 3 (mean (SD)) | 94.1 (12.0) | 96.3 (13.9) | 0.363 | 2.3 | ||
| IgE (IU/mL), mean (SD) | 147.3 (212.3) | 106.3 (201.3) | 0.268 | 0 | ||
| WTC Exposure | WTC dust cloud | 0/55 | 73/73 | |||
| Data 4, n/N | Workplace with ash | 0/55 | 58/73 | |||
| Participant Category | 0/55 | 73/73 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grunig, G.; Durmus, N.; Zhang, Y.; Lu, Y.; Pehlivan, S.; Wang, Y.; Doo, K.; Cotrina-Vidal, M.L.; Goldring, R.; Berger, K.I.; et al. Molecular Clustering Analysis of Blood Biomarkers in World Trade Center Exposed Community Members with Persistent Lower Respiratory Symptoms. Int. J. Environ. Res. Public Health 2022, 19, 8102. https://doi.org/10.3390/ijerph19138102
Grunig G, Durmus N, Zhang Y, Lu Y, Pehlivan S, Wang Y, Doo K, Cotrina-Vidal ML, Goldring R, Berger KI, et al. Molecular Clustering Analysis of Blood Biomarkers in World Trade Center Exposed Community Members with Persistent Lower Respiratory Symptoms. International Journal of Environmental Research and Public Health. 2022; 19(13):8102. https://doi.org/10.3390/ijerph19138102
Chicago/Turabian StyleGrunig, Gabriele, Nedim Durmus, Yian Zhang, Yuting Lu, Sultan Pehlivan, Yuyan Wang, Kathleen Doo, Maria L. Cotrina-Vidal, Roberta Goldring, Kenneth I. Berger, and et al. 2022. "Molecular Clustering Analysis of Blood Biomarkers in World Trade Center Exposed Community Members with Persistent Lower Respiratory Symptoms" International Journal of Environmental Research and Public Health 19, no. 13: 8102. https://doi.org/10.3390/ijerph19138102