The Performance of Paralleling Technique and Bisecting Angle Technique for Taking Periapical Radiographs: A Systematic Review
Abstract
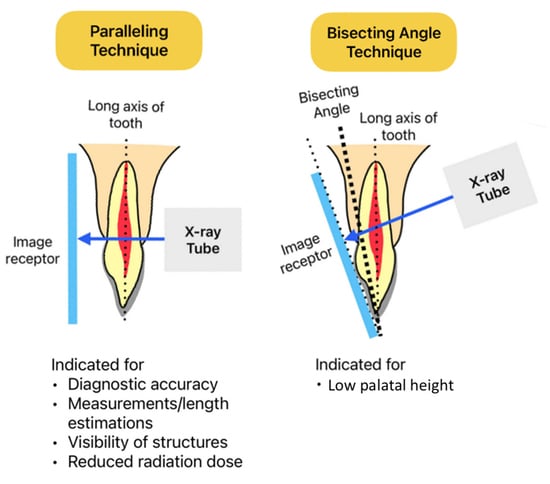
:1. Introduction
2. Materials and Methods
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grillon, M.; Yeung, A.W.K. Content Analysis of YouTube Videos That Demonstrate Periapical Radiography. Appl. Sci. 2022, 12, 9602. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Wong, N.S.M. Reject Rates of Radiographic Images in Dentomaxillofacial Radiology: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 8076. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Tanaka, R.; Jacobs, R.; Bornstein, M.M. Awareness and practice of 2D and 3D diagnostic imaging among dentists in Hong Kong. Br. Dent. J. 2020, 228, 701–709. [Google Scholar] [CrossRef]
- Biggerstaff, R.H.; Phillips, J.R. A quantitative comparison of paralleling long-cone and bisection-of-angle periapical radiography. Oral Surg. Oral Med. Oral Pathol. 1976, 41, 673–677. [Google Scholar] [CrossRef]
- Taguchi, M.; Wamasing, P.; Watanabe, H.; Sakamoto, J.; Kurabayashi, T. Applying the paralleling technique in intraoral periapical radiographs for Japanese patients by analyzing CT images. Oral Radiol. 2021, 37, 311–320. [Google Scholar] [CrossRef]
- Gupta, A.; Devi, P.; Srivastava, R.; Jyoti, B. Intra oral periapical radiography-basics yet intrigue: A review. Bangladesh J. Dent. Res. Educ. 2014, 4, 83–87. [Google Scholar] [CrossRef] [Green Version]
- Veena, K.; Razak, R.; Chatra, L.; Shenoy, P.; Prabhu, R.V. Appreciation of Incisive Foramen in Intraoral Periapical Radiographs-A Comparative Radiographic Study. J. Morphol. Sci. 2021, 38, 127–129. [Google Scholar] [CrossRef]
- Anand, A.; Sharma, S.; Shahi, A.K.; Rims, R. Comparative assessment of the opinion regarding usage of bisecting-angle technique and the paralleling techniques among dental professionals—A questionnaire based study. Eur. J. Mol. Clin. Med. 2020, 7, 7987–7993. [Google Scholar]
- Ahmad Satmi, A.S.; Fadilah, N.H.; Mohd Yusof, M.Y.P.; Adull Manan, N.F.; Mahmud, J.; Abdullah, S.A. Effectiveness and comfort assessment of the novel intra-oral bisecting angle bisector© and paralleling rinn® digital imaging receptor holders in low palatal height patients. Arch. Orofac. Sci. 2019, 15, 1–10. [Google Scholar] [CrossRef]
- Reddy, K.R.; Tatapudi, R.; Reddy, R.S.; Kumar, C.N.; Teja, T.N.; Swathi, G. Assessment of linear measurements with intra oral grid on intra oral periapical image—A comparison of digital and conventional film images using bisecting angle and paralleling techniques. J. Indian Acad. Oral Med. Radiol. 2019, 31, 339–345. [Google Scholar] [CrossRef]
- Darós, P.; Carneiro, V.C.; Siqueira, A.P.; de-Azevedo-Vaz, S.L. Diagnostic accuracy of 4 intraoral radiographic techniques for misfit detection at the implant abutment joint. J. Prosthet. Dent. 2018, 120, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Sanghvi, S.; Rao, A.; Karuna, Y.; Shetty, K.; Nayak, A. Image distortion of the roots of maxillary deciduous molars on Iopa’s recorded with bisecting angle or a modified paralleling technique. Biomed. Pharmacol. J. 2018, 11, 1039–1042. [Google Scholar] [CrossRef]
- Azizah, A.; Muhamad, A.; Mohd, A.; Atika, A. External Marker in Bisecting-Angle-Technique: A New Approach to Minimize Dental Radiographic Error. Med. Health 2017, 12, 304–311. [Google Scholar]
- Iikubo, M.; Kamio, T.; Hashimoto, N.; Nishioka, T.; Wakoh, M.; Sano, T.; Igarashi, C.; Kobayashi, K.; Seki, K.; Katsumata, A. Comparison of bisecting and parallel intraoral radiography and cone-beam computed tomography for detecting various horizontal angle root fractures. Oral Radiol. 2015, 31, 173–180. [Google Scholar] [CrossRef]
- Ibrahim, M.F.; Aziz, M.S.; Maxood, A.; Khan, W.U. Comparison of paralleling and bisecting angle techniques in endodontic working length radiography. Pakistan Oral Dent. J. 2013, 33, 160–164. [Google Scholar]
- Kanchan-Talreja, P.; Acharya, A.B.; Naikmasur, V.G. An assessment of the versatility of Kvaal’s method of adult dental age estimation in Indians. Arch. Oral Biol. 2012, 57, 277–284. [Google Scholar] [CrossRef]
- Aps, J. Flemish general dental practitioners’ knowledge of dental radiology. Dentomaxillofac. Radiol. 2010, 39, 113–118. [Google Scholar] [CrossRef] [Green Version]
- Kazzi, D.; Horner, K.; Qualtrough, A.; Martinez-Beneyto, Y.; Rushton, V. A comparative study of three periapical radiographic techniques for endodontic working length estimation. Int. Endod. J. 2007, 40, 526–531. [Google Scholar] [CrossRef]
- Rush, E.; Thompson, N. Dental radiography technique and equipment: How they influence the radiation dose received at the level of the thyroid gland. Radiography 2007, 13, 214–220. [Google Scholar] [CrossRef]
- Huh, K.-H.; Lee, S.-S.; Jeon, I.-S.; Yi, W.-J.; Heo, M.-S.; Choi, S.-C. Quantitative analysis of errors in alveolar crest level caused by discrepant projection geometry in digital subtraction radiography: An in vivo study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 100, 750–755. [Google Scholar] [CrossRef]
- Tugnait, A.; Clerehugh, V.; Hirschmann, P. Radiographic equipment and techniques used in general dental practice. A survey of general dental practitioners in England and Wales. J. Dent. 2003, 31, 197–203. [Google Scholar] [CrossRef]
- Chandler, N.; Koshy, S. Radiographic practices of dentists undertaking endodontics in New Zealand. Dentomaxillofac. Radiol. 2002, 31, 317–321. [Google Scholar] [CrossRef]
- Forsberg, J.; Halse, A. Periapical radiolucencies as evaluated by bisecting-angle and paralleling radiographic techniques. Int. Endod. J. 1997, 30, 115–123. [Google Scholar] [CrossRef]
- Forsberg, J.; Halse, A. Radiographic simulation of a periapieal lesion comparing the paralleling and the bisecting-angle techniques. Int. Endod. J. 1994, 27, 133–138. [Google Scholar] [CrossRef]
- Lecomber, A.; Faulkner, K. Organ absorbed doses in intraoral dental radiography. Br. J. Radiol. 1993, 66, 1035–1041. [Google Scholar] [CrossRef]
- Wood, R.; Bristow, R.; Clark, G.; Nussbaum, C.; Taylor, K. Technique-dependent decrease in thyroid absorbed dose for dental radiography. Health Phys. 1989, 56, 893–901. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, J. A comparison of the paralleling and bisecting-angle radiographic techniques in endodontics. Int. Endod. J. 1987, 20, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, J. Estimation of the root filling length with the paralleling and bisecting-angle techniques performed by undergraduate students. Int. Endod. J. 1987, 20, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, J. Radiographic reproduction of endodontic “working length” comparing the paralleling and the bisecting-angle techniques. Oral Surg. Oral Med. Oral Pathol. 1987, 64, 353–360. [Google Scholar] [CrossRef]
- Abdul Razak, A.A.; Abdul Razak, I. Accuracy of tooth length measurements from periapical radiographs. Dent. J. Malays. 1985, 8, 27–32. [Google Scholar]
- Mourshed, F.; McKinney, A.L. A comparison of paralleling and bisecting radiographic techniques as experienced by dental students. Oral Surg. Oral Med. Oral Pathol. 1972, 33, 284–296. [Google Scholar] [CrossRef] [PubMed]
- Kühnisch, J.; Anttonen, V.; Duggal, M.; Spyridonos, M.L.; Rajasekharan, S.; Sobczak, M.; Stratigaki, E.; van Acker, J.; Aps, J.; Horner, K. Best clinical practice guidance for prescribing dental radiographs in children and adolescents: An EAPD policy document. Eur. Arch. Paediatr. Dent. 2020, 21, 375–386. [Google Scholar] [CrossRef] [PubMed]


| Study | Journal | Country | Indication/Study Purpose | Dental Specialty | Sample Size | Statistical Tests | Key Findings |
|---|---|---|---|---|---|---|---|
| Veena et al., 2021 [7] | Journal of Morphological Sciences | India | Visibility of incisive foramen | Implantology | 60 B tech/60 P tech | Chi-square test | Percentage of visibility on incisive foramen was higher in P tech than B tech (76.7% vs. 40.0%, p = 0.000) |
| Anand et al., 2020 [8] | European Journal of Molecular and Clinical Medicine | India | Opinion of techniques among dental professionals | General | 250 dental students and dentists | N/A | B tech was chosen by most dental professionals (p < 0.05); equal preference for operator and patient comfort; P tech was favored for exposure parameters and image accuracy (p < 0.05) |
| Ahmad Satmi et al., 2020 [9] | Archives of Orofacial Sciences | Malaysia | Effectiveness and comfort of techniques in low palatal height patients | General | 30 B tech/30 P tech | Mann–Whitney U test (for repeat rate) | Image repeat rate was higher in P tech than B tech (18.6% vs. 8.9%, p = 0.0251). Comfort was at medium range for both techniques |
| Reddy et al., 2019 [10] | Journal of Indian Academy of Oral Medicine and Radiology | India | Linear measurements with techniques, with conventional and digital film images, with the use of Intra Oral Grid | Endodontics, Periodontics | 80/80/40/40 (conventional B tech, conventional P tech, digital B tech, digital P tech) | N/A | P tech showed a significant difference compared to B tech in conventional and digital methods with grid usage (p < 0.05) |
| Darós et al., 2018 [11] | Journal of Prosthetic Dentistry | Brazil | Diagnostic accuracy of techniques on misfit detection at the implant-abutment joint (IAJ) | Implantology | 60 B tech/60 P tech/60 P tech with custom-made holder/60 bitewing | ROC curves (Az) and Fisher tests | P tech had significantly higher diagnostic values than B tech (p < 0.05) for 50- and 150-micron misfits |
| Sanghvi et al., 2018 [12] | Biomedical and Pharmacology Journal | India | Root length distortion of maxillary deciduous molar roots | Pediatrics | 33 B tech/27 P tech | Chi-square test | No significant difference between techniques (p < 0.05) |
| Azizah et al., 2017 [13] | Medicine and Health | Malaysia | Radiographic error rate | General | 80/80/80 (B tech, B tech with external marker and P tech) | Chi-square test | Number of radiographic errors was least in B tech with external marker (31), less in P tech (37) and highest in B tech (45) (B tech vs. P tech, p = 0.206; B tech vs. B tech with marker, p = 0.027) |
| Likubo et al., 2015 [14] | Oral Radiology | Japan | Diagnostic accuracy for root fractures | Endodontics | 81 B tech/81 P tech | Kruskal–Wallis test | P tech had greater sensitivity for groove/fracture that were right-angles (p < 0.01) and 75-degrees to the long axis of the tooth (p < 0.05) than B tech, but B tech had greater sensitivity for the 55-degree groove (p < 0.01) |
| Ibrahim et al., 2013 [15] | Pakistan Oral | Pakistan | Reject rate in endodontic working length radiography | Endodontics | 120 B tech/120 P tech | Chi-square test | B tech had a higher retake rate than P tech (24.2% vs. 10.2%, p = 0.01) |
| Kanchan-Talreja et al., 2012 [16] | Archives of Oral Biology | India | Accuracy of Kvaal formulae in Indian population for radiographic dental age estimation | Forensics | 53 B tech/47 P tech | N/A | Average error of age estimation, for standard formula: P tech = ±18–20 years; B tech = ±19–21 years; for Indian-specific formula: both techs = ±11–14 years |
| Aps 2010 [17] | Dentomaxillofacial Radiology | Belgium | Practice and knowledge of dental radiography by Flemish general dentists | General | 374 dentists | N/A | 81% used P tech, 14% used B tech, 5% unclear |
| Kazzi et al., 2007 [18] | International Endodontic Journal | UK | Subjective image quality and radiographic errors of endodontic working length estimation films | Endodontics | 37 B tech/60 P tech | Mann–Whitney U test | P tech had a significantly lower diagnostic unacceptability rate (16.7% vs. 48.6%, p < 0.001), incorrect vertical angulation rate (5.0% vs. 48.6%, p < 0.001) and cone cutting rate (20.0% vs. 62.2%, p < 0.001) |
| Rush and Thompson 2007 [19] | Radiography | UK | Radiation dose received at thyroid gland | General | 32 B tech/32 P tech | ANOVA | Radiation dose received at thyroid gland was significantly lower in P tech than B tech (1.617 μGy vs. 4.863 μGy, p < 0.01) |
| Huh et al., 2005 [20] | Oral Surg, Oral Med, Oral Pathol, Oral Radiol, and Endo | Korea | Amount of error in alveolar crest level for digital subtraction radiography | Periodontics | 360 B tech/360 P tech + biteblock/360 P tech | ANOVA | Amount of error was least in P tech with biteblock (0.108 mm), less in P tech (0.210 mm) and highest in B tech (0.277 mm) (p < 0.05). Error more severe in the molar region than in the anterior region |
| Tugnait et al., 2003 [21] | Journal of Dentistry | UK | Practice and knowledge of dental radiography by dentists in England and Wales | General | 800 questionnaires (592 valid responses) | Chi-square test | 31% used P tech, 22% used B tech; P tech was used more by younger dentists (p < 0.001) |
| Chandler and Koshy 2002 [22] | Dentomaxillofacial Radiology | New Zealand | Practice and knowledge of dental radiography for root canal treatment by New Zealand dentists | General | 1200 questionnaires (931 valid responses) | N/A | 26.3% used P tech, 22.4% used B tech; both techniques were in regular use |
| Forsberg and Halse 1997 [23] | International Endodontic Journal | Norway | Periapical radiolucencies’ lesion size | Endodontics | 168 B tech/168 P tech | McNemar test | Detection of presence of lesions was same between techniques. Size of lesions was not significantly different (p > 0.05) |
| Forsberg and Halse 1994 [24] | International Endodontic Journal | Norway | Periapical radiolucencies’ lesion size | Endodontics | 60 extracted teeth repeatedly imaged with multiple vertical angulations | N/A | P tech had lower ratio of cases with reduced lesion size than B tech (2% vs. 10–20%). Increased error as vertical angulation of central beam increased for both techs |
| Lecomber and Faulkner 1993 [25] | British Journal of Radiology | UK | Radiation dose absorbed by organs | General | 14 B tech/4 P tech | N/A | P tech had lower radiation dose than B tech (e.g., upper molar: P tech = 1.51 μSv, B tech = 3.18 μSv) |
| Wood et al., 1989 [26] | Health Physics | Canada | Radiation dose absorbed by thyroid gland | General | 20 B tech/20 P tech | T-test | P tech had lower absorbed dose at thyroid than B tech for 70-kVP beam (p < 0.05). However, P tech had higher dose at thyroid than B tech for 90-kVp beam (p < 0.05) |
| Forsberg 1987 [27] | International Endodontic Journal | Norway | Root filling length estimation | Endodontics | 433 B tech/433 P tech | N/A | P tech (4%) had less images with >1 mm measurement deviation from the gold standard image for working length and root filling images than B tech (13–19%) when used with specially-constructed or Eggen film holder |
| Forsberg 1987 [28] | International Endodontic Journal | Norway | Root filling length estimation | Endodontics | 200 B tech/200 P tech | N/A | With P tech as gold standard, B tech had >1 mm measurement deviation in 15% of cases (mostly shortened) |
| Forsberg 1987 [29] | Oral Surgery, Oral Medicine, Oral Pathology | Norway | Radiographic reproduction of working length | Endodontics | 90 B tech/ 90 P tech | Chi-square test | P tech had >1 mm measurement deviation in 3–7% of cases; P tech was significantly more accurate at measuring the apical position of the metal indicator than B tech (p < 0.05) |
| Abdul Razak and Abdul Razak 1985 [30] | Dental Journal of Malaysia | Malaysia | Accuracy in measuring tooth length | Endodontics | 120 B tech/120 P tech | N/A | The mean difference with the actual length was +1.4 mm for P tech and +2.2 mm for B tech (p < 0.001); B tech had a greater deviation range and was more magnified than P tech |
| Biggerstaff and Phillips 1976 [4] | Oral Surgery | US | Variability of measured crown–root ratio | Orthodontics | 5 B tech/5 P tech | N/A | Variance of radiographic of crown–root ratio was less for P tech than B tech (0.000019 vs. 0.000894) (p = 0.0005) |
| Mourshed and McKinney 1972 [31] | Oral Surgery, Oral Medicine, Oral Pathology | US | Radiographic error rate | General | 3236 P tech with XCP/2582 P tech with Precision/ 2670 B tech with Snap-A-Ray holder | N/A | B tech had greater retake rate (27.5% vs. 23.1–22.8%), incorrect vertical angulation (11.8% vs. 1.1–2.6%), and cone cutting (10.2% vs. 1.0–0.7%) than P tech; P tech had greater improper film positioning (25.6–28.4% vs. 18.5%) |
| Key Practical Considerations/Clinical Indications | Preferred Technique | Supporting Studies |
|---|---|---|
| Diagnostic accuracy (e.g., root fractures, implant misfits) | P tech | [11,14] |
| Bone level measurement for digital subtraction radiography | P tech | [20] |
| Tooth length/root length/crown–root ratio estimation | P tech | [4,10,27,29,30] |
| No difference | [12] | |
| Periapical lesion size measurement | P tech | [24] |
| No difference | [23] | |
| Visibility of incisive foramen | P tech | [7] |
| Radiation dose absorbed by thyroid and other organs | P tech | [19,25,26] |
| Practice preference (from four survey studies) | P tech | [17,21,22] |
| B tech | [8] | |
| Radiographic error rate/reject rate | P tech | [13,15,18,31] |
| B tech (for low palatal height) | [9] |
| Study | 1. Was the Study Question or Objective Clearly Stated? | 2. Was the Study Population Clearly and Fully Described, including a Case Definition? | 3. Were the Cases Consecutive? | 4. Were the Subjects Comparable? | 5. Was the Intervention Clearly Described? | 6. Were the Outcome Measures Clearly Defined, Valid, Reliable, and Implemented Consistently across all Study Participants? | 7. Was the Length of Follow-Up Adequate? | 8. Were the Statistical Methods Well Described? | 9. Were the Results Well Described? | Quality Rating (Good, Fair, or Poor) |
|---|---|---|---|---|---|---|---|---|---|---|
| Veena et al., 2021 [7] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Ahmad Satmi et al., 2020 [9] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Reddy et al., 2019 [10] | Yes | Yes | NR | Yes | Yes | Yes | NA | No | Yes | Good |
| Darós et al., 2018 [11] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Sanghvi et al., 2018 [12] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Azizah et al., 2017 [13] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Likubo et al., 2015 [14] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Ibrahim et al., 2013 [15] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Kanchan-Talreja et al., 2012 [16] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Kazzi et al., 2007 [18] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Rush and Thompson 2007 [19] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Huh et al., 2005 [20] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Forsberg and Halse 1997 [23] | Yes | Yes | NR | Yes | Yes | Yes | Yes | Yes | Yes | Good |
| Forsberg and Halse 1994 [24] | Yes | Yes | NR | Yes | Yes | Yes | NA | No | Yes | Good |
| Lecomber and Faulkner 1993 [25] | Yes | Yes | NR | Yes | Yes | Yes | NA | No | Yes | Good |
| Wood et al., 1989 [26] | Yes | Yes | NR | Yes | Yes | Yes | NA | Yes | Yes | Good |
| Forsberg 1987 [27] | Yes | Yes | Yes | Yes | Yes | Yes | NA | No | Yes | Good |
| Forsberg 1987 [28] | Yes | Yes | NR | Yes | Yes | Yes | NA | No | Yes | Good |
| Forsberg 1987 [29] | Yes | Yes | NR | Yes | Yes | Yes | NA | No | Yes | Good |
| Abdul Razak and Abdul Razak 1985 [30] | Yes | Yes | NR | Yes | Yes | Yes | NA | No | Yes | Good |
| Biggerstaff and Phillips 1976 [4] | Yes | Yes | NR | Yes | Yes | Yes | NA | No | Yes | Good |
| Mourshed and McKinney 1972 [31] | Yes | Yes | NR | Yes | Yes | Yes | NA | No | Yes | Good |
| Study | 1. Was the Study Question or Objective Clearly Stated? | 2. Was the Study Population Clearly Specified and Defined? | 3. Was the Participation Rate of Eligible Persons at Least 50%? | Were all Subjects Recruited from the Same or Similar Populations? Were the Inclusion and Exclusion Criteria Applied Uniformly? | 5. Was a Sample Size Justification, Power Description, or Variance and Effect Estimates Provided? | 6. Were the Exposures of Interest Measured Prior to the Outcomes Being Measured? | 7. Were the Outcome Measures Clearly Defined, Valid, Reliable, and Implemented Consistently? | 8. Were Key Potential Confounding Variables Measured and Adjusted Statistically? | Quality Rating (Good, Fair, or Poor) |
|---|---|---|---|---|---|---|---|---|---|
| Anand et al., 2020 [8] | Yes | No | NR | Yes | No | Yes | Yes | No | Fair |
| Aps 2010 [17] | Yes | Yes | NR | Yes | No | Yes | Yes | Yes | Fair |
| Tugnait et al., 2003 [21] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Good |
| Chandler and Koshy 2002 [22] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Good |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yen, M.; Yeung, A.W.K. The Performance of Paralleling Technique and Bisecting Angle Technique for Taking Periapical Radiographs: A Systematic Review. Dent. J. 2023, 11, 155. https://doi.org/10.3390/dj11070155
Yen M, Yeung AWK. The Performance of Paralleling Technique and Bisecting Angle Technique for Taking Periapical Radiographs: A Systematic Review. Dentistry Journal. 2023; 11(7):155. https://doi.org/10.3390/dj11070155
Chicago/Turabian StyleYen, Matthew, and Andy Wai Kan Yeung. 2023. "The Performance of Paralleling Technique and Bisecting Angle Technique for Taking Periapical Radiographs: A Systematic Review" Dentistry Journal 11, no. 7: 155. https://doi.org/10.3390/dj11070155