Synthesis, Characterization, and Activity of Hydroxymethylnitrofurazone Nanocrystals against Trypanosoma cruzi and Leishmania spp.
Abstract
:1. Introduction
2. Results and Discussion
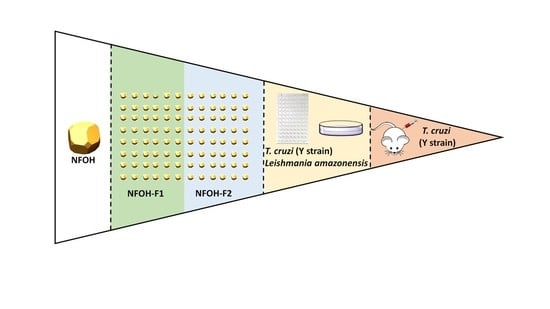
2.1. Screening for the Preparation of NFOH Nanocrystals
2.2. Factorial Design
2.3. X-ray Diffraction (XRD)
3. Biological Activity
3.1. Cytotoxicity on Macrophages (50.0% Cytotoxicity Concentrations [CC50])
3.2. Anti-T. cruzi Activity (In Vitro)
3.3. Anti-Leishmanial Activity (In Vitro)
3.4. Anti-T. cruzi Activity in Mice
4. Material and Methods
4.1. Chemistry
4.1.1. Preliminary Assay for Preparation of NFOH Nanocrystals
4.1.2. Factorial Design
4.1.3. MPS and PI Analysis
4.1.4. ZP
4.1.5. Lyophilization
4.1.6. XRD
4.2. Biology
4.2.1. Cytotoxicity on Macrophages (CC50)
4.2.2. In Vitro anti-T. cruzi Activity (IC50)
4.2.3. In Vitro Anti-Leishmania Activity (IC50)
4.2.4. Anti-T. cruzi Murine Assay
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO-World and Health Organization. Neglected Tropical Diseases. Available online: www.who.int/neglected_diseases/diseases/en/ (accessed on 6 December 2022).
- DNDi. Drugs for Neglected Diseases Initiative (DNDi), Neglected Tropical Diseases-Chagas Disease. 2020. Available online: https://www.dndi.org/diseases-projects/chagas/ (accessed on 6 December 2022).
- Alvar, J.; Croft, S.; Olliaro, P. Chemotherapy in the treatment and control of leishmaniasis. Adv. Parasitol. 2006, 61, 223–274. [Google Scholar] [PubMed]
- Andrade, M.C.; Oliveira, M.D.F.; Nagao-Dias, A.T.; Coêlho, I.C.B.; Cândido, D.D.S.; Freitas, E.C.; Bezerra, F.S.M. Clinical and serological evolution in chronic Chagas disease patients in a 4-year pharmacotherapy follow-up: A preliminary study. Rev. Soc. Bras. Med. Trop. 2013, 46, 776–778. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barrett, M.P.; Croft, S.L. Management of trypanosomiasis and leishmaniasis. Br. Med. Bull. 2012, 104, 175–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castro, J.A.; DeMecca, M.M.; Bartel, L.C. Toxic side effects of drugs used to treat chagas’ disease (american trypanosomiasis). Hum. Exp. Toxicol. 2006, 25, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.L.; Marson, M.E.; Ramirez, J.C.; Mastrantonio, G.; Schijman, A.G.; Altcheh, J.; Riarte, A.R.; Bournissen, F.G. Pharmacokinetic and pharmacodynamic responses in adult patients with Chagas disease treated with a new formulation of benznidazole. Memórias Do Inst. Oswaldo Cruz 2016, 111, 218–221. [Google Scholar] [CrossRef]
- Fuentes, B.R.; Maturana, A.M.; Cruz, M.R. Eficacia de nifurtimox para el tratamiento de pacientes con enfermedad de Chagas cronica. Rev. Chil. Infectol. 2012, 29, 82–86. [Google Scholar] [CrossRef] [Green Version]
- Maya, J.D.; Orellana, M.; Ferreira, J.; Kemmerling, U.; López-Muñoz, R.; Morello, A. Chagas disease: Present status of pathogenic mechanisms and chemotherapy. Biol. Res. 2010, 43, 323–331. [Google Scholar] [CrossRef] [Green Version]
- McGwire, B.S.; Satoskar, A.R. Leishmaniasis: Clinical syndromes and treatment. Mon. J. Assoc. Phys. 2014, 107, 7–14. [Google Scholar] [CrossRef] [Green Version]
- WHO-World and Health Organization. Control of Chagas disease: Second report of the WHO expert committee World Health Organization (2000: Brasilia, Brazil). Geneva World Health 2002, 905, 109. [Google Scholar]
- Scarim, C.B.; Chung, M.C. Current Approaches of Drug Discovery for Chagas Disease: Methodological Advances. Comb. Chem. High Throug. Screen. 2019, 22, 1–12. [Google Scholar] [CrossRef]
- Scarim, C.B.; Jornada, D.H.; Chelucci, R.C.; De Almeida, L.; Dos Santos, J.L.; Chung, M.C. Current advances in drug discovery for Chagas disease. Eur. J. Med. Chem. 2018, 5234, 30531. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.C.; Güido, R.V.C.; Martinelli, T.F.; Gonçalves, M.F.; Carneiro Poll, M.; Botelho, K.C.A.; Ferreira, E.I. Synthesis and in vitro evaluation of potential antichagasic hydroxymethylnitrofurazone (NFOH-121): A new nitrofurazone prodrug. Bioorg. Med. Chem. 2003, 11, 4779–4783. [Google Scholar] [CrossRef] [PubMed]
- Scarim, C.B.; Olmo, F.; Ferreira, E.I.; Chung, M.C.; Kelly, J.M.; Francisco, A.F. Image-Based In vitro Screening Reveals the Trypanostatic Activity of Hydroxymethylnitrofurazone against Trypanosoma cruzi. Int. J. Mol. Sci. 2021, 22, 6930. [Google Scholar] [CrossRef] [PubMed]
- Davies, C.; Cardozo, R.M.; Negrette, O.S.; Mora, M.C.; Chung, M.C.; Basombrío, M.A. Hydroxymethylnitrofurazone is active in a murine model of Chagas’ disease. Antimicrob. Agents Chemother. 2010, 54, 3584–3589. [Google Scholar] [CrossRef] [Green Version]
- Scarim, C.B.; de Andrade, C.R.; da Rosa, J.A.; dos Santos, J.L.; Chung, M.C. Hydroxymethylnitrofurazone treatment in indeterminate form of chronic Chagas disease: Reduced intensity of tissue parasitism and inflammation—A histopathological study. Int. J. Exp. Pathol. 2018, 99, 236–248. [Google Scholar] [CrossRef] [PubMed]
- Davies, C.; Dey Negrett, O.S.; Parada, L.A.; Basombrio, M.A.; Garg, N.J. Hepatotoxicity in Mice of a Novel Anti-parasite Drug Candidate Hydroxymethylnitrofurazone: A Comparison with Benznidazole. PLoS Negl. Trop. Dis. 2014, 8, e3231. [Google Scholar] [CrossRef] [Green Version]
- Chen, M.L.; John, M.; Lee, S.L.; Tyner, K.M. Development Considerations for Nanocrystal Drug Products. AAPS J. 2017, 19, 642–651. [Google Scholar] [CrossRef]
- Müller, R.H.; Gohla, S.; Keck, C.M. State of the art of nanocrystals-Special features, production, nanotoxicology aspects and intracellular delivery. Eur. J. Pharm. Biopharm. 2011, 78, 1–9. [Google Scholar] [CrossRef]
- Noyes, A.A.; Whitney, W.R. The rate of solution of solid substances in their own solutions. J. Amer. Chem. Soc. 1897, 19, 930–934. [Google Scholar] [CrossRef] [Green Version]
- Doriguetto, A.C.; de Paula Silva, C.H.; Ellena, J.; Trossini, G.H.; Chin, C.M.; Ferreira, E.I. 5-Nitro-2-furaldehyde N-(hydroxymethyl) semicarbazone. Acta Crystallogr. Sect. E Struct. Rep. Online 2005, 61, 2099–2101. [Google Scholar] [CrossRef] [Green Version]
- Varshosaz, J.A.; Talari, R.; Mostafavi, S.A.; Nokhodchi, A. Dissolution enhancement of gliclazide using in situ micronization by solvent change method. Powder Technol. 2008, 187, 222–230. [Google Scholar] [CrossRef]
- De Souza, A.; Marin, D.S.S.; Mathias, S.L.; Monteiro, L.M.; Yukuyama, M.N.; Scarim, C.B.; Bou-Chacra, N.A. Promising nanotherapy in treating leishmaniasis. Intern. J. Pharm. 2018, 547, 421–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morilla, M.J.; Romero, E.L. Nanomedicines against Chagas disease: An update on therapeutics, prophylaxis and diagnosis. Nanomedicine 2015, 10, 465–481. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, L.M.; Löbenberg, R.; Ferreira, E.I.; Cotrim, P.C.; Kanashiro, E.; Rocha, M.; Chung, C.M.; Bou-Chacra, N.A. Targeting Leishmania amazonensis amastigotes through macrophage internalisation of a hydroxymethylnitrofurazone nanostructured polymeric system. Int. J. Antimicrob. Agents 2017, 50, 88–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romero, G.B.; Keck, C.M.; Muller, R.H.; Bou-Chacra, N.A. Development of cationic nanocrystals for ocular delivery. Eur. J. Pharmac. Biopharmac. 2016, 107, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Mosmann, T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxic assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef]
- Rolón, M.; Vega, C.; Escario, J.A.; Gómez-Barrio, A. Development of resazurin microtiter assay for drug sensibility testing of Trypanosoma cruzi epimastigotes. Parasitol. Res. 2006, 99, 103–107. [Google Scholar] [CrossRef]
- Brancaglion, G.A.; Toyota, A.E.; Cardoso Machado, J.V.; Fernandes Júnior, A.Á.; Silveira, A.T.; Vilas Boas, D.F.; Carvalho, D.T. In vitro and in vivo trypanocidal activities of 8-methoxy-3-(4-nitrobenzoyl)-6-propyl-2H-cromen-2-one, a new synthetic coumarin of low cytotoxicity against mammalian cells. Chem. Biol. Drug Des. 2018, 92, 1888–1898. [Google Scholar] [CrossRef]
- Espuri, P.F.; Dos Reis, L.L.; Peloso, E.F.; Gontijo, V.S.; Colombo, F.A.; Nunes, J.B.; de Oliveira, C.E.; de Almeida, E.T.; Silva, D.E.S.; Bortoletto, J.; et al. Synthesis and evaluation of the antileishmanial activity of silver compounds containing imidazolidine-2-thione. J. Biol. Inorg. Chem. 2019, 24, 419–432. [Google Scholar] [CrossRef]




| Formula | Order | Central Point | Time (hours) | NFOH (%w/w) | P407 (%w/w) | MPS | PI | ZP |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 1 | 48 | 3.0 | 1.0 | 248.2 ± 1.2 | 0.39 ± 0.01 | −26.2 ± 0.5 |
| 2 | 2 | 0 | 84 | 2.0 | 2.0 | 271.0 ± 1.8 | 0.28 ± 0.02 | −27.4 ± 0.2 |
| 3 | 3 | 1 | 120 | 3.0 | 1.0 | 191.3 ± 2.1 | 0.32 ± 0.04 | −28.1 ± 1.4 |
| 4 | 4 | 0 | 84 | 2.0 | 2.0 | 278.3 ± 2.4 | 0.24 ± 0.01 | −32.1 ± 2.3 |
| 5 | 5 | 1 | 48 | 3.0 | 3.0 | 254.1 ± 6.7 | 0.41 ± 0.06 | −25.5 ± 1.5 |
| 6 | 6 | 1 | 120 | 1.0 | 1.0 | 197.2 ± 0.5 | 0.25 ± 0.01 | −30.8 ± 2.2 |
| 7 | 7 | 1 | 120 | 1.0 | 3.0 | 214.4 ± 1.4 | 0.24 ± 0.02 | −23.9 ± 0.7 |
| 8 | 8 | 0 | 84 | 2.0 | 2.0 | 264.0 ± 1.1 | 0.28 ± 0.01 | −27.7 ± 0.2 |
| 9 | 9 | 1 | 120 | 3.0 | 3.0 | 284.6 ± 1.9 | 0.21 ± 0.01 | −28.0 ± 1.2 |
| 10 | 10 | 1 | 48 | 1.0 | 1.0 | 326.8 ± 4.3 | 0.21 ± 0.01 | −29.1 ± 0.9 |
| 11 | 11 | 1 | 48 | 1.0 | 3.0 | 258.6 ± 2.8 | 0.50 ± 0.01 | −27.2 ± 0.8 |
| DF | SS (adj) | MS (adj) | F Value | p Value | ||
|---|---|---|---|---|---|---|
| Model | 7 | 15,890.7 | 2270.10 | 66.27 | 0.003 | |
| Linear | 3 | 5344.6 | 1781.53 | 52.01 | 0.004 | |
| NFOH %w/w | 1 | 44.2 | 44.18 | 1.29 | 0.330 | |
| P407 %w/w | 1 | 290.4 | 290.41 | 8.48 | 0.062 | |
| Stirring Time (h) | 1 | 5010.0 | 5010.00 | 146.26 | 0.001 | |
| Interaction | 3 | 92,268.3 | 3089.44 | 90.19 | 0.002 | |
| NFOH %w/w × P407 %w/w | 1 | 2820.0 | 2820.00 | 82.33 | 0.003 | |
| NFOH %w/w × Stirring Time (h) | 1 | 2715.8 | 2715.85 | 79.29 | 0.003 | |
| P407 %w/w × Stirring Time (h) | 1 | 3732.5 | 3732.48 | 108.97 | 0.002 | |
| Curve | 1 | 1277.8 | 1277.76 | 37.30 | 0.009 | |
| Error | 3 | 102.8 | 4.25 | |||
| Lack of adjustment | 1 | 0.5 | 0.50 | 0.01 | 0.930 | |
| Pure Error | 2 | 102.3 | 51.13 | |||
| Total | 10 | 15,993.4 | ||||
| SD = 5.85263 | R2 = 99.36% | R2 (adj) = 97.86% | R2 (pred) = 98.36% | |||
| Formula | Predicted MPS (nm) | Observed MPS (nm) | PI |
|---|---|---|---|
| A | 248.39 | 245.2 ± 1.4 | 0.29 ± 0.01 |
| B | 204.67 | 199.4 ± 2.3 | 0.26 ± 0.03 |
| C | 213.6 ± 2.0 | 215.46 | 0.34 ± 0.01 |
| D | 219.1± 2.3 | 222.33 | 0.28 ± 0.03 |
| Formula | Order | Central | Time (hours) | NFOH (%w/w) | P188 (%w/w) | MPS (nm) | PI | PZ (mV) |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 1 | 48 | 3.0 | 1.0 | 285.9 ± 3.3 | 0.43 ± 0.02 | −33.2 ± 0.5 |
| 2 | 2 | 0 | 84 | 2.0 | 2.0 | 304.0 ± 2.1 | 0.29 ± 0.03 | −33.4 ± 0.7 |
| 3 | 3 | 1 | 120 | 3.0 | 1.0 | 184.8 ± 0.5 | 0.34 ± 0.04 | −33.3 ± 1.1 |
| 4 | 4 | 0 | 84 | 2.0 | 2.0 | 298.3 ± 2.1 | 0.21 ± 0.01 | −40.3 ± 0.6 |
| 5 | 5 | 1 | 48 | 3.0 | 3.0 | 274.8 ± 3.1 | 0.57 ± 0.01 | −34.6 ± 1.1 |
| 6 | 6 | 1 | 120 | 1.0 | 1.0 | 193.5 ± 3.2 | 0.23 ± 0.01 | −34.5 ± 1.1 |
| 7 | 7 | 1 | 120 | 1.0 | 3.0 | 203.0 ± 0.1 | 0.26 ± 0.01 | −34.8 ± 1.5 |
| 8 | 8 | 0 | 84 | 2.0 | 2.0 | 310.1 ± 3.3 | 0.24 ± 0.02 | −36.6 ± 0.7 |
| 9 | 9 | 1 | 120 | 3.0 | 3.0 | 194.3 ± 2.1 | 0.31 ± 0.03 | −31.7 ± 1.1 |
| 10 | 10 | 1 | 48 | 1.0 | 1.0 | 296.5 ± 2.5 | 0.22 ± 0.01 | −38.7 ± 0.6 |
| 11 | 11 | 1 | 48 | 1.0 | 3.0 | 311.8 ± 2.2 | 0.39 ± 0.02 | −38.2 ± 1.2 |
| 12 | 12 | −1 | 120 | 2.0 | 2.0 | 198.5 ± 1.4 | 0.24 ± 0.04 | −34.5 ± 1.4 |
| 13 | 13 | 0 | 84 | 2.0 | 2.0 | 298.3 ± 2.1 | 0.37 ± 0.07 | −34.5 ± 0.6 |
| 14 | 14 | −1 | 120 | 2.0 | 1.0 | 171.0 ± 0.7 | 0.22 ± 0.01 | −36.3 ± 0.7 |
| 15 | 15 | −1 | 84 | 3.0 | 1.0 | 194.4 ± 1.6 | 0.25 ± 0.01 | −36.1 ± 0.6 |
| 16 | 16 | 0 | 84 | 2.0 | 2.0 | 299.3 ± 1.9 | 0.28 ± 0.02 | −39.2 ± 0.9 |
| 17 | 17 | 1 | 48 | 2.0 | 1.0 | 256.1 ± 1.4 | 0.22 ± 0.03 | −32.5 ± 0.2 |
| 18 | 18 | −1 | 84 | 3.0 | 2.0 | 261.9 ± 2.1 | 0.29 ± 0.01 | −31.7 ± 1.3 |
| 19 | 19 | 0 | 84 | 2.0 | 2.0 | 301.2 ± 2.7 | 0.32 ± 0.01 | −38.1 ± 1.2 |
| 20 | 20 | −1 | 84 | 1.0 | 1.0 | 217.9 ± 3.3 | 0.21 ± 0.02 | −31.5 ± 1.8 |
| DF | SS (adj) | MS (adj) | F-Value | p-Value | ||
|---|---|---|---|---|---|---|
| Model | 5 | 48,894.5 | 9778.9 | 137.46 | 0.001 | |
| Blocks | 1 | 4318.6 | 4318.6 | 60.70 | 0.001 | |
| Linear | 3 | 26,702.8 | 8900.9 | 125.12 | 0.001 | |
| NFOH % w/w | 1 | 746.1 | 746.1 | 10.49 | 0.006 | |
| P188 % w/w | 1 | 19.1 | 19.1 | 0.27 | 0.612 | |
| Stirring time (h) | 1 | 26,149.6 | 26,149.6 | 367.57 | 0.001 | |
| Quadradic | 1 | 14,030.0 | 14,030.0 | 197.21 | 0.001 | |
| P188 % w/w*P188 % | 1 | 14,030.0 | 14,030.0 | 197.21 | 0.001 | |
| Error | 14 | 996.0 | 71.1 | |||
| Lack of adjustment | 9 | 891.2 | 99.0 | 4.72 | 0.051 | |
| Pure Error | 5 | 104.8 | 21.0 | * | * | |
| Total | 19 | 49,890.5 | ||||
| SD = 8.43456 | R2= 98.00% | R2 (adj) = 97.29% | R2 (pred) = 95.30% | |||
| Formula | NFOH (%w/w) | Poloxamer 188 (%w/w) | Poloxamer 407 (%w/w) | Stirring Time (h) |
|---|---|---|---|---|
| NFOH-1 | 2.0 | 1.0 | - | 120 |
| NFOH-2 | 3.0 | - | 1.0 | 120 |
| NTA | MPS (nm) | ||
|---|---|---|---|
| NFOH-F1 | NFOH-F2 | ||
| d (0,1) | 91.3 ± 3.9 | 89.2 ± 0.1 | |
| d (0,5) | 136.7 ± 2.7 | 132.6 ± 6.4 | |
| d (0,9) | 188.2 ± 6.5 | 188.7 ± 4.5 | |
| Mean | 141.9 ± 0.6 | 138.2 ± 1.7 | |
| PCS | MPS | 193.5 ± 3.2 | 197.2 ± 0.5 |
| T. cruzi Y Strain | Cytotoxicity | Epimastigotes | Trypomastigotes | Amastigotes | |
|---|---|---|---|---|---|
| SI | SI | SI | |||
| CC50 | IC50 | IC50 | IC50 | ||
| Compounds | |||||
| NFOH-F1 | 1194.7 | 11.02 +/− 2.4 108 | 8.9 +/− 0.3 | 134 2.29 +/− 0.95 | 521 |
| NFOH-F2 | 885.5 | 18.83 +/− 4.06 47 | 10.5 +/− 0.56 | 84 4.85 +/− 3.91 | 182 |
| Benznidazole | >300.0 | 8.01 +/− 1.31 >37 | 4.21 +/− 0.23 | >71 4.8 +/− 1.7 | >62 |
| Leishmania | |||||
|---|---|---|---|---|---|
| Cytotoxicity | |||||
| amazonensis/ | Promastigotes | SI | Amastigotes | SI | |
| CC50 | |||||
| Compounds | |||||
| NFOH-F1 | 1194.7 | 101.97 +/− 2.41 | 11.72 | 90.35 +/− 6.58 | 7.71 |
| NFOH-F2 | 885.5 | 98.65 +/− 7.25 | 8.97 | 143.64 +/− 1.09 | 16.01 |
| Amphotericin B | 27.05 | 5.10 +/− 0.002 | 5.3 | 1.30 +/− 0.001 | 20.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarim, C.B.; de Souza, A.; Marins, D.S.S.; Santos, E.G.d.; de Figueiredo Diniz Castro, L.; Caldas, I.S.; Espuri, P.F.; Marques, M.J.; Ferreira, E.I.; Bou-Chacra, N.A.; et al. Synthesis, Characterization, and Activity of Hydroxymethylnitrofurazone Nanocrystals against Trypanosoma cruzi and Leishmania spp. Drugs Drug Candidates 2022, 1, 43-55. https://doi.org/10.3390/ddc1010005
Scarim CB, de Souza A, Marins DSS, Santos EGd, de Figueiredo Diniz Castro L, Caldas IS, Espuri PF, Marques MJ, Ferreira EI, Bou-Chacra NA, et al. Synthesis, Characterization, and Activity of Hydroxymethylnitrofurazone Nanocrystals against Trypanosoma cruzi and Leishmania spp. Drugs and Drug Candidates. 2022; 1(1):43-55. https://doi.org/10.3390/ddc1010005
Chicago/Turabian StyleScarim, Cauê Benito, Aline de Souza, Débora Soares Souza Marins, Elda Gonçalves dos Santos, Lívia de Figueiredo Diniz Castro, Ivo Santana Caldas, Patrícia Ferreira Espuri, Marcos José Marques, Elizabeth Igne Ferreira, Nadia Araci Bou-Chacra, and et al. 2022. "Synthesis, Characterization, and Activity of Hydroxymethylnitrofurazone Nanocrystals against Trypanosoma cruzi and Leishmania spp." Drugs and Drug Candidates 1, no. 1: 43-55. https://doi.org/10.3390/ddc1010005