Engagement during a Mixed In-Person and Remotely Delivered Psychological Intervention for Youth with Functional Abdominal Pain Disorders and Anxiety
Abstract
:1. Introduction
2. Methods
2.1. Procedure and Sample
2.2. ADAPT Intervention
2.3. Outcome Measures
2.4. Data Analysis
2.4.1. Micro-Level Engagement
Quantitative Methods
Qualitative Methods
2.4.2. Macro-Level Engagement
Mixed Methods Approach
2.4.3. Engagement in Relation to ADAPT Outcomes
3. Results
3.1. Sample Characteristics
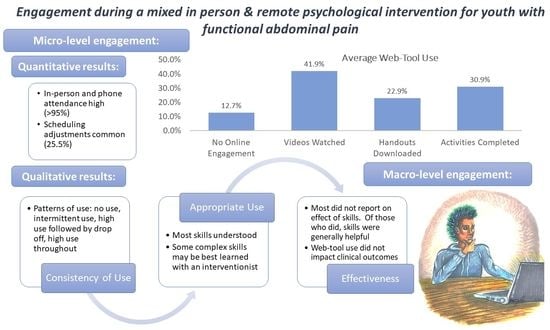
3.2. Micro-Level Engagement
3.2.1. Quantitative Results
3.2.2. Qualitative Results
3.3. Macro-Level Engagement
3.4. Web Tool Usage in Relation to ADAPT Outcomes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Korterink, J.J.; Diederen, K.; Benninga, M.A.; Tabbers, M.M. Epidemiology of pediatric functional abdominal pain disorders: A meta-analysis. PLoS ONE 2015, 10, e0126982. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef]
- Robin, S.G.; Keller, C.; Zwiener, R.; Hyman, P.E.; Nurko, S.; Saps, M.; Di Lorenzo, C.; Shulman, R.J.; Hyams, J.S.; Palsson, O.; et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the Rome IV Criteria. J. Pediatr. 2018, 195, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Mulvaney, S.; Lambert, E.W.; Garber, J.; Walker, L.S. Trajectories of symptoms and impairment for pediatric patients with functional abdominal pain: A 5-year longitudinal study. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 737–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Pub: Arlington, VA, USA, 2013. [Google Scholar]
- Dufton, L.M.; Dunn, M.J.; Compas, B.E. Anxiety and somatic complaints in children with recurrent abdominal pain and anxiety disorders. J. Pediatr. Psychol. 2009, 34, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Shelby, G.D.; Shirkey, K.C.; Sherman, A.L.; Beck, J.E.; Haman, K.; Shears, A.R.; Horst, S.N.; Smith, C.A.; Garber, J.; Walker, L.S. Functional abdominal pain in childhood and long-term vulnerability to anxiety disorders. Pediatrics 2013, 132, 475–482. [Google Scholar] [CrossRef] [Green Version]
- Cunningham, N.R.; Cohen, M.B.; Farrell, M.K.; Mezoff, A.G.; Lynch-Jordan, A.; Kashikar-Zuck, S. Concordant parent-child reports of anxiety predict impairment in youth with functional abdominal pain. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 312–317. [Google Scholar] [CrossRef] [Green Version]
- Dorn, L.D.; Campo, J.C.; Thato, S.; Dahl, R.E.; Lewin, D.; Chandra, R.; Di Lorenzo, C. Psychological comorbidity and stress reactivity in children and adolescents with recurrent abdominal pain and anxiety disorders. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 66–75. [Google Scholar] [CrossRef]
- Wendland, M.; Jackson, Y.; Stokes, L.D. Functional disability in paediatric patients with recurrent abdominal pain. Child Care Health Dev. 2010, 36, 516–523. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Jagpal, A.; Peugh, J.; Farrell, M.K.; Cohen, M.B.; Mezoff, A.G.; Lynch-Jordan, A.; Kashikar-Zuck, S. Risk Categorization predicts disability in pain-associated functional gastrointestinal disorders after 6 months. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 685–690. [Google Scholar] [CrossRef] [Green Version]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Varma, P.; Junge, M.; Meaklim, H.; Jackson, M.L. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 109, 110236. [Google Scholar] [CrossRef] [PubMed]
- Kazantzis, N.; Luong, H.K.; Usatoff, A.S.; Impala, T.; Yew, R.Y.; Hofmann, S.G. The processes of cognitive behavioral therapy: A review of meta-analyses. Cogn. Ther. Res. 2018, 42, 349–357. [Google Scholar] [CrossRef]
- Fisher, E.; Law, E.; Dudeney, J.; Eccleston, C.; Palermo, T.M. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst. Rev. 2019, 4, CD011118. [Google Scholar] [CrossRef]
- Palermo, T.M.; Eccleston, C.; Lewandowski, A.S.; Williams, A.C.d.C.; Morley, S. Randomized controlled trials of psychological therapies for management of chronic pain in children and adolescents: An updated meta-analytic review. Pain 2010, 148, 387–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levy, R.L.; Langer, S.L.; Walker, L.S.; Romano, J.M.; Christie, D.L.; Youssef, N.; DuPen, M.M.; Feld, A.D.; Ballard, S.A.; Welsh, E.M.; et al. Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. Am. J. Gastroenterol. 2010, 105, 946–956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lalouni, M.; Ljótsson, B.; Bonnert, M.; Ssegonja, R.; Benninga, M.; Bjureberg, J.; Högström, J.; Sahlin, H.; Simrén, M.; Feldman, I.; et al. Clinical and cost effectiveness of online cognitive behavioral therapy in children with functional abdominal pain disorders. Clin. Gastroenterol. Hepatol. 2019, 17, 2236–2244.e2211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otte, C. Cognitive behavioral therapy in anxiety disorders: Current state of the evidence. Dialogues Clin. Neurosci. 2011, 13, 413–421. [Google Scholar] [CrossRef] [PubMed]
- James, A.C.; James, G.; Cowdrey, F.A.; Soler, A.; Choke, A. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst. Rev. 2015, CD004690. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Nelson, S.; Jagpal, A.; Moorman, E.; Farrell, M.; Pentiuk, S.; Kashikar-Zuck, S. Development of the aim to decrease anxiety and pain treatment for pediatric functional abdominal pain disorders. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 16–20. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Kalomiris, A.; Peugh, J.; Farrell, M.; Pentiuk, S.; Mallon, D.; Le, C.; Moorman, E.; Fussner, L.; Dutta, R.A.; et al. Cognitive behavior therapy tailored to anxiety symptoms improves pediatric functional abdominal pain outcomes: A randomized clinical trial. J. Pediatr. 2021, 230, 62–70.e63. [Google Scholar] [CrossRef]
- Kashikar-Zuck, S.; Ting, T.V.; Arnold, L.M.; Bean, J.; Powers, S.W.; Graham, T.B.; Passo, M.H.; Schikler, K.N.; Hashkes, P.J.; Spalding, S. Cognitive behavioral therapy for the treatment of juvenile fibromyalgia: A multisite, single-blind, randomized, controlled clinical trial. Arthritis Rheum 2012, 64, 297–305. [Google Scholar] [CrossRef]
- Rapee, R.M. Group treatment of children with anxiety disorders: Outcome and predictors of treatment response. Aust. J. Psychol. 2000, 52, 125–129. [Google Scholar] [CrossRef]
- Beatty, L.; Binnion, C. A Systematic Review of predictors of, and reasons for, adherence to online psychological interventions. Int. J. Behav. Med. 2016, 23, 776–794. [Google Scholar] [CrossRef] [PubMed]
- Palermo, T.M.; de la Vega, R.; Murray, C.; Law, E.; Zhou, C. A digital health psychological intervention (WebMAP Mobile) for children and adolescents with chronic pain: Results of a hybrid effectiveness-implementation stepped-wedge cluster randomized trial. Pain 2020, 161, 2763–2774. [Google Scholar] [CrossRef] [PubMed]
- Chien, I.; Enrique, A.; Palacios, J.; Regan, T.; Keegan, D.; Carter, D.; Tschiatschek, S.; Nori, A.; Thieme, A.; Richards, D.; et al. A machine learning approach to understanding patterns of engagement with internet-delivered mental health interventions. JAMA Netw. Open 2020, 3, e2010791. [Google Scholar] [CrossRef]
- Yardley, L.; Spring, B.J.; Riper, H.; Morrison, L.G.; Crane, D.H.; Curtis, K.; Merchant, G.C.; Naughton, F.; Blandford, A. Understanding and promoting effective engagement with digital behavior change interventions. Am. J. Prev. Med. 2016, 51, 833–842. [Google Scholar] [CrossRef] [Green Version]
- Using Fmri to Understand Response to An Integrative Treatment for Pain and Anxiety in Pediatric Functional Abdominal Pain Disorders (FAPD). Clinicaltrials.Gov Registration: NCT03518216. Available online: https://clinicaltrials.gov/ct2/show/NCT03518216 (accessed on 9 July 2021).
- Walker, L.S.; Greene, J.W. The functional disability inventory: Measuring a neglected dimension of child health status. J. Pediatr. Psychol. 1991, 16, 39–58. [Google Scholar] [CrossRef] [PubMed]
- Kashikar-Zuck, S.; Flowers, S.R.; Claar, R.L.; Guite, J.W.; Logan, D.E.; Lynch-Jordan, A.M.; Palermo, T.M.; Wilson, A.C. Clinical utility and validity of the Functional Disability Inventory among a multicenter sample of youth with chronic pain. Pain 2011, 152, 1600–1607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGrath, P.J.; Walco, G.A.; Turk, D.C.; Dworkin, R.H.; Brown, M.T.; Davidson, K.; Eccleston, C.; Finley, G.A.; Goldschneider, K.; Haverkos, L.; et al. Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. J. Pain 2008, 9, 771–783. [Google Scholar] [CrossRef] [PubMed]
- Birmaher, B.; Khetarpal, S.; Brent, D.; Cully, M.; Balach, L.; Kaufman, J.; Neer, S.M. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 545–553. [Google Scholar] [CrossRef]
- Van der Veek, S.M.; de Haan, E.; Derkx, H.; Benninga, M.A.; Boer, F. Psychological factors addressed in cognitive behaviour therapy for paediatric functional abdominal pain: Which are most important to target? J. Health Psychol. 2019, 24, 1282–1292. [Google Scholar] [CrossRef]
- Walker, L.S.; Smith, C.A.; Garber, J.; Claar, R.L. Testing a model of pain appraisal and coping in children with chronic abdominal pain. Health Psychol. 2005, 24, 364–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holloway, I.; Todres, L. The status of method: Flexibility, consistency and coherence. Qual. Res. 2003, 3, 345–357. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Fussner, L.M.; Moorman, E.; Avar Aydin, P.O.; Brunner, H.I.; Kashikar-Zuck, S. Development and pilot testing of the treatment and education approach for childhood-onset lupus (TEACH): A cognitive behavioral treatment. Pediatr. Rheumatol. Online J. 2019, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, C.J., Jr.; Kashikar-Zuck, S.; Farrell, J.; Barnett, K.; Goldschneider, K.; Dampier, C.; Cunningham, N.R.; Crosby, L.; DeWitt, E.M. Qualitative evaluation of pediatric pain behavior, quality, and intensity item candidates and the PROMIS pain domain framework in children with chronic pain. J. Pain 2015, 16, 1243–1255. [Google Scholar] [CrossRef] [Green Version]
- Richardson, P.A.; Harrison, L.E.; Heathcote, L.C.; Rush, G.; Shear, D.; Lalloo, C.; Hood, K.; Wicksell, R.K.; Stinson, J.; Simons, L.E. Mhealth for pediatric chronic pain: State of the art and future directions. Expert. Rev. Neurother. 2020, 20, 1177–1187. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Ely, S.L.; Garcia, B.N.B.; Bowden, J. Addressing pediatric mental health using telehealth during COVID-19 and beyond: A narrative review. Acad. Pediatr. 2021. [Google Scholar] [CrossRef]
- Bradley, L.E.; Smith-Mason, C.E.; Corsica, J.A.; Kelly, M.C.; Hood, M.M. Remotely delivered interventions for obesity treatment. Curr. Obes. Rep. 2019, 8, 354–362. [Google Scholar] [CrossRef]
- McLay, L.; Sutherland, D.; Machalicek, W.; Sigafoos, J. Systematic review of telehealth interventions for the treatment of sleep problems in children and adolescents. J. Behav. Educ. 2020, 29, 222–245. [Google Scholar] [CrossRef] [Green Version]
- Pruitt, L.D.; Luxton, D.D.; Shore, P. Additional clinical benefits of home-based telemental health treatments. Prof. Psychol. Res. Pract. 2014, 45, 340–346. [Google Scholar] [CrossRef]
- Chatoor, I.; Krupnick, J. The role of non-specific factors in treatment outcome of psychotherapy studies. Eur. Child Adolesc. Psychiatry 2001, 10 (Suppl. 1), I19–I25. [Google Scholar] [CrossRef] [PubMed]
- Garrido, S.; Millington, C.; Cheers, D.; Boydell, K.; Schubert, E.; Meade, T.; Nguyen, Q.V. What works and what doesn’t work? a systematic review of digital mental health interventions for depression and anxiety in young people. Front. Psychiatry 2019, 10, 759. [Google Scholar] [CrossRef] [PubMed]
- MacDonell, K.W.; Prinz, R.J. A review of technology-based youth and family-focused interventions. Clin. Child Fam. Psychol. Rev. 2017, 20, 185–200. [Google Scholar] [CrossRef]
- Eysenbach, G. The law of attrition. J. Med. Internet Res. 2005, 7, e11. [Google Scholar] [CrossRef]
- Cugelman, B. Gamification: What it is and why it matters to digital health behavior change developers. JMIR Serious Games 2013, 1, e3. [Google Scholar] [CrossRef]
- Patel, A.; Schieble, T.; Davidson, M.; Tran, M.C.; Schoenberg, C.; Delphin, E.; Bennett, H. Distraction with a hand-held video game reduces pediatric preoperative anxiety. Paediatr. Anaesth. 2006, 16, 1019–1027. [Google Scholar] [CrossRef] [PubMed]
- Simons, L.E.; Smith, A.; Ibagon, C.; Coakley, R.; Logan, D.E.; Schechter, N.; Borsook, D.; Hill, J.C. Pediatric pain screening tool: Rapid identification of risk in youth with pain complaints. Pain 2015, 156, 1511–1518. [Google Scholar] [CrossRef] [Green Version]
- Fisher, E.; Law, E.; Dudeney, J.; Palermo, T.M.; Stewart, G.; Eccleston, C. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst. Rev. 2018, 9, CD003968. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [Green Version]
- Boyatzis, R.E. Transforming Qualitative Information: Thematic Analysis and Code Development; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1998; pp. 1–174. [Google Scholar]
- American Psychological Association. Psychologists Report Large Increase in Demand for Anxiety, Depression Treatment. Available online: http://www.apa.org/news/press/releases/2020/11/anxiety-depression-treatment (accessed on 12 July 2021).
- Perry, K.; Gold, S.; Shearer, E.M. Identifying and addressing mental health providers’ perceived barriers to clinical video telehealth utilization. J. Clin. Psychol. 2020, 76, 1125–1134. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, S.; Cortright, K.; Crawford, A.; Mizuno, Y.; Yoshida, K.; Hilty, D.; Guinart, D.; Torous, J.; Correll, C.U.; Castle, D.J.; et al. Changes in telepsychiatry regulations during the COVID-19 pandemic: 17 countries and regions’ approaches to an evolving healthcare landscape. Psychol. Med. 2020, 1–8. [Google Scholar] [CrossRef]
- Provenzi, L.; Grumi, S.; Gardani, A.; Aramini, V.; Dargenio, E.; Naboni, C.; Vacchini, V.; Borgatti, R. Italian parents welcomed a telehealth family-centred rehabilitation programme for children with disability during COVID-19 lockdown. Acta Paediatr. 2021, 110, 194–196. [Google Scholar] [CrossRef]
- Taddei, M.; Bulgheroni, S. Facing the real time challenges of the COVID-19 emergency for child neuropsychology service in Milan. Res. Dev. Disabil. 2020, 107, 103786. [Google Scholar] [CrossRef] [PubMed]

| Session | Platform * | Skill/Module | Target |
|---|---|---|---|
| 1 | In person | Psychoeducation | Pain & Anxiety |
| Relaxation: Deep Breathing & Guided Imagery | Pain | ||
| 2 | In person | Progressive Muscle Relaxation | Pain |
| Calming Statements | Pain | ||
| Activity Pacing | Pain | ||
| 3 | Web & phone | Pleasant Activity Scheduling | Pain |
| Problem Solving | Pain | ||
| 4 † | Web & phone | Detective Thinking | Anxiety |
| 5 † | Web & phone | Stepladders | Anxiety |
| Assertiveness Training | Anxiety | ||
| 6 | Web & phone | Maintenance Planning | Pain & Anxiety |
| Passive Use | Interactive Use | |||||
|---|---|---|---|---|---|---|
| Videos | Handout | Forms | ||||
| Skill Name | M (SD) | Range | M (SD) | Range | M (SD) | Range |
| Overall (n = 55) | ||||||
| Pleasant Activities & Problem Solving | 43.0% (39.4%) | 0–100% | 29.6% (40.6%) | 0–100% | 32.3% (22.9%) | 0–50% |
| Detective Thinking | 43.3% (43.4%) | 0–100% | 21.1% (36.1%) | 0–100% | 29.6% (28.6%) | 0–67% |
| Stepladders | 43.3% (44.7%) | 0–100% | 13.9% (31.8%) | 0–100% | 33.3% (47.7%) | 0–100% |
| Assertiveness Training | 38.9% (43.8%) | 0–100% | 13.3% (34.4%) | 0–100% | 28.2% (27.5%) | 0–67% |
| Maintenance Planning | 37.3% (45.4%) | 0–100% | 26.4% (43.9%) | 0–100% | N/A | N/A |
| Effective (n, %) | Prompt | Participant Response |
| Problem Solving (n = 20/48, 41.7% completed) | ||
| Effective (20/20, 100%) | Identify your problem: | I get extreme belly pain when I swim causing me to want to sit out with my friends |
| Identify your thoughts, feelings, and behavior: | Thought: My friends will be mad at me if I don’t keep playing in the pool Feelings: Worry that the pain will worsen and Sad if I choose to sit out | |
| List coping skills you have learned so far: | Activity pacing, Progressive muscle relaxation, Positive statements, Mini relaxation, Deep breathing, Guided imagery | |
| Pick several coping skills to use to deal with this problem: | Activity Pacing, Positive Statements, Deep Breathing, Mini Relaxation | |
| Predict what will happen when you try the solution(s): | When I do activity pacing I think this will allow me to take some smaller breaks causing my belly to have time to stop hurting… When I do positive statements I would expect that the worry would decrease or stop …when I do deep breathing and mini relaxation I would expect to clear some of the negative thoughts and focus more on the swimming and fun than my pain | |
| What actually did happen when you tried the solution(s): | the activity pacing extremely helped with the pain to the point there almost was no pain the positive statements reminded me that I had gotten though the same pain before so it was not going to control me this time The deep breathing helped because it feels refreshing to my stomach to take a deep breath and release almost what feels like tension The mini relaxation reminded me that I was trying to have fun and would distract me from the pain | |
| What, if anything would you do differently next time: | try to stay in the pool longer and try guided imagery on the pool float | |
| Effective (n, %) | Prompt | Participant Response |
| Detective Thinking (n = 12/48, 25.0% completed) | ||
| Effective (10/12, 83.3%) | Event: | I am going somewhere new and don’t know where |
| Thoughts: | What if I am late or way to early? Am I sure this is where I’m going? Did I wear the appropriate thing? Was I supposed to bring something? | |
| Worry rating before: | 9 out of 10 | |
| What is the evidence? | I think this every time and I never am late… I could ask someone and see if I am going the right way. Don’t worry about what your wearing you look fine. …Plus people are late to things all the time. | |
| What is a realistic thought? | You won’t be late and even if you are its not like it’ll be a big deal. | |
| New worry rating: | 6 out of 10 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miller, A.K.; Ely, S.L.; Barber Garcia, B.N.; Richardson, P.; Cunningham, N.R. Engagement during a Mixed In-Person and Remotely Delivered Psychological Intervention for Youth with Functional Abdominal Pain Disorders and Anxiety. Children 2021, 8, 775. https://doi.org/10.3390/children8090775
Miller AK, Ely SL, Barber Garcia BN, Richardson P, Cunningham NR. Engagement during a Mixed In-Person and Remotely Delivered Psychological Intervention for Youth with Functional Abdominal Pain Disorders and Anxiety. Children. 2021; 8(9):775. https://doi.org/10.3390/children8090775
Chicago/Turabian StyleMiller, Alaina K., Samantha L. Ely, Brittany N. Barber Garcia, Patricia Richardson, and Natoshia R. Cunningham. 2021. "Engagement during a Mixed In-Person and Remotely Delivered Psychological Intervention for Youth with Functional Abdominal Pain Disorders and Anxiety" Children 8, no. 9: 775. https://doi.org/10.3390/children8090775