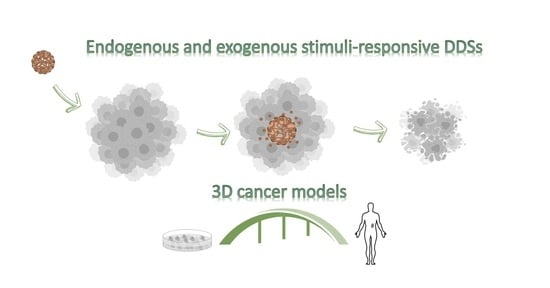
The Effective Combination between 3D Cancer Models and Stimuli-Responsive Nanoscale Drug Delivery Systems
Abstract
:1. Introduction
2. 3D In Vitro Platforms to Investigate Endogenous Stimuli-Responsive Drug-Delivery Systems
2.1. pH-Responsive Drug-Delivery Systems
2.2. Enzyme Responsive Drug Delivery Systems
2.3. Hypoxia-Responsive Drug Delivery System
2.4. ROS- and Redox-Responsive Drug Delivery Systems
3. 3D In Vitro Platforms for Investigating Exogenous Stimuli-Responsive Drug Delivery Systems
3.1. Light-Responsive Drug Delivery Systems
3.2. Temperature-Responsive Drug Delivery Systems
3.3. Ultrasound-Responsive Drug Delivery Systems
3.4. Magnetic Field-Responsive Drug Delivery Systems
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Lv, D.; Hu, Z.; Lu, L.; Lu, H.; Xu, X. Three-dimensional Cell Culture: A Powerful Tool in Tumor Research and Drug Discovery (Review). Oncol. Lett. 2017, 14, 6999–7010. [Google Scholar] [CrossRef] [Green Version]
- Foglietta, F.; Canaparo, R.; Muccioli, G.; Terreno, E.; Serpe, L. Methodological aspects and pharmacological applications of three-dimensional cancer cell cultures and organoids. Life Sci. 2020, 254, 117784. [Google Scholar] [CrossRef] [PubMed]
- Chaicharoenaudomrung, N.; Kunhorm, P.; Noisa, P. Three-dimensional cell culture systems as an in vitro platform for cancer and stem cell modeling. World J. Stem Cells 2019, 11, 1065–1083. [Google Scholar] [CrossRef]
- Breslin, S.; O’Driscoll, L. Three-dimensional cell culture: The missing link in drug discovery. Drug Discov. Today 2013, 18, 240–249. [Google Scholar] [CrossRef]
- Ryu, N.E.; Lee, S.H.; Park, H. Spheroid Culture System Methods and Applications for Mesenchymal Stem Cells. Cells 2019, 8, 1620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Low, L.A.; Mummery, C.; Berridge, B.R.; Austin, C.P.; Tagle, D.A. Organs-on-chips: Into the next decade. Nat. Rev. Drug Discov. 2021, 20, 345–361. [Google Scholar] [CrossRef] [PubMed]
- Nii, T.; Makino, K.; Tabata, Y. Three-Dimensional Culture System of Cancer Cells Combined with Biomaterials for Drug Screening. Cancers 2020, 12, 2754. [Google Scholar] [CrossRef]
- Crampton, A.L.; Cummins, K.A.; Wood, D.K. Correction to: A High-Throughput Workflow to Study Remodeling of Extracellular Matrix-Based Microtissues by Crampton AL, Cummins KA, and Wood DK. Tissue Eng. Part C Methods 2019, 25, 25–36. https://doi.org/10.1089/ten.tec.2018.0290. Tissue Eng. Part C Methods 2019, 25, 446. [Google Scholar] [CrossRef]
- Liu, C.; Mejia, D.L.; Chiang, B.; Luker, K.E.; Luker, G.D. Hybrid collagen alginate hydrogel as a platform for 3D tumor spheroid invasion. Acta Biomater. 2018, 75, 213–225. [Google Scholar] [CrossRef]
- Amorim, S.; da Costa, D.S.; Pashkuleva, I.; Reis, C.A.; Reis, R.L.; Pires, R.A. 3D hydrogel mimics of the tumor microenvironment: The interplay among hyaluronic acid, stem cells and cancer cells. Biomater. Sci. 2021, 9, 252–260. [Google Scholar] [CrossRef]
- Pinto, M.P.; Dye, W.W.; Jacobsen, B.M.; Horwitz, K.B. Malignant stroma increases luminal breast cancer cell proliferation and angiogenesis through platelet-derived growth factor signaling. BMC Cancer 2014, 14, 735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, C.; Liu, Y.; Xu, X.X.; Guo, X.; Sun, G.W.; Ma, X.J. Mesenchymal stem cells enhance the metastasis of 3D-cultured hepatocellular carcinoma cells. BMC Cancer 2016, 16, 566. [Google Scholar] [CrossRef] [Green Version]
- Van Zundert, I.; Fortuni, B.; Rocha, S. From 2D to 3D Cancer Cell Models-The Enigmas of Drug Delivery Research. Nanomaterials 2020, 10, 2236. [Google Scholar] [CrossRef] [PubMed]
- Cabral, H. Drug Delivery Systems. Methods in Molecular Biology. 437. Edited by Kewal K. Jain. Angew. Chem. Int. Ed. 2009, 48, 1718. [Google Scholar] [CrossRef]
- Maiti, S.; Sen, K.K. Introductory chapter: Drug delivery concepts. In Advanced Technology for Delivering Therapeutics; InTech: London, UK, 2017; ISBN 978-953-51-3121-2. [Google Scholar]
- Perrin, J.H. Sustained and controlled release drug delivery systems. J. Pharm. Sci. 1980, 6, 485. [Google Scholar] [CrossRef]
- Park, K. Controlled drug delivery systems: Past forward and future back. J. Control Release 2014, 190, 3–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, K. Facing the truth about nanotechnology in drug delivery. ACS Nano 2013, 7, 7442–7447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Attia, M.F.; Anton, N.; Wallyn, J.; Omran, Z.; Vandamme, T.F. An overview of active and passive targeting strategies to improve the nanocarriers efficiency to tumour sites. J. Pharm. Pharmacol. 2019, 71, 1185–1198. [Google Scholar] [CrossRef] [Green Version]
- Sledge, G.W., Jr.; Miller, K.D. Exploiting the hallmarks of cancer: The future conquest of breast cancer. Eur. J. Cancer 2003, 39, 1668–1675. [Google Scholar] [CrossRef]
- Bamrungsap, S.; Zhao, Z.; Chen, T.; Wang, L.; Li, C.; Fu, T.; Tan, W. Nanotechnology in therapeutics: A focus on nanoparticles as a drug delivery system. Nanomedicine (Lond.) 2012, 7, 1253–1271. [Google Scholar] [CrossRef]
- Knight, A. Systematic reviews of animal experiments demonstrate poor contributions toward human healthcare. Rev. Recent Clin. Trials 2008, 3, 89–96. [Google Scholar] [CrossRef] [Green Version]
- Roy, A.; Li, S.D. Modifying the tumor microenvironment using nanoparticle therapeutics. Wiley Interdiscip. Rev. Nanomed. 2016, 8, 891–908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, J.; Lane, L.A.; Nie, S. Stimuli-responsive nanoparticles for targeting the tumor microenvironment. J. Control Release 2015, 219, 205–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, R.K. Normalizing tumor microenvironment to treat cancer: Bench to bedside to biomarkers. J. Clin. Oncol. 2013, 31, 2205–2218. [Google Scholar] [CrossRef] [Green Version]
- Quail, D.F.; Joyce, J.A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med. 2013, 19, 1423–1437. [Google Scholar] [CrossRef] [PubMed]
- Huai, Y.; Hossen, M.N.; Wilhelm, S.; Bhattacharya, R.; Mukherjee, P. Nanoparticle Interactions with the Tumor Microenvironment. Bioconjug. Chem. 2019, 30, 2247–2263. [Google Scholar] [CrossRef]
- Fernandes, C.; Suares, D.; Yergeri, M.C. Tumor Microenvironment Targeted Nanotherapy. Front. Pharmacol. 2018, 9, 1230. [Google Scholar] [CrossRef]
- Mei, J.; Hong, Y.; Lam, J.W.; Qin, A.; Tang, Y.; Tang, B.Z. Aggregation-induced emission: The whole is more brilliant than the parts. Adv. Mater. 2014, 26, 5429–5479. [Google Scholar] [CrossRef]
- Mei, J.; Leung, N.L.; Kwok, R.T.; Lam, J.W.; Tang, B.Z. Aggregation-Induced Emission: Together We Shine, United We Soar! Chem. Rev. 2015, 115, 11718–11940. [Google Scholar] [CrossRef]
- Li, D.; Zhang, Y.; Zhou, B. pH-responsive drug delivery system based on AIE luminogen functionalized layered zirconium phosphate nano-platelets. J. Solid State Chem. 2015, 25, 427–430. [Google Scholar] [CrossRef]
- Lai, W.F. Non-conjugated polymers with intrinsic luminescence for drug delivery. J. Drug Deliv. Sci. Technol. 2020, 59, 101916. [Google Scholar] [CrossRef]
- Lai, W.F.; Deng, R.; He, T.; Wong, W.T. A Bioinspired, Sustained-Release Material in Response to Internal Signals for Biphasic Chemical Sensing in Wound Therapy. Adv. Healthc. Mater. 2021, 10, e2001267. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Mun, H.; Sung, C.O.; Cho, E.J.; Jeon, H.J.; Chun, S.M.; Shin, T.H.; Jeong, G.S.; Kim, D.K.; Choi, E.K.; et al. Patient-derived lung cancer organoids as in vitro cancer models for therapeutic screening. Nat. Commun. 2019, 10, 3991. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, G.; Bertotti, A.; Leto, S.M.; Vetrano, S. Patient-derived tumor models: A more suitable tool for pre-clinical studies in colorectal cancer. J. Exp. Clin. Cancer Res. 2021, 40, 178. [Google Scholar] [CrossRef]
- Helmlinger, G.; Sckell, A.; Dellian, M.; Forbes, N.S.; Jain, R.K. Acid production in glycolysis-impaired tumors provides new insights into tumor metabolism. Clin. Cancer Res. 2002, 8, 1284–1291. [Google Scholar]
- Vaupel, P.; Kallinowski, F.; Okunieff, P. Blood flow, oxygen and nutrient supply, and metabolic microenvironment of human tumors: A review. Cancer Res. 1989, 49, 6449–6465. [Google Scholar]
- Zhu, Y.J.; Chen, F. pH-responsive drug-delivery systems. Chem. Asian J. 2015, 10, 284–305. [Google Scholar] [CrossRef]
- Crucho, C.I. Stimuli-responsive polymeric nanoparticles for nanomedicine. ChemMedChem 2015, 10, 24–38. [Google Scholar] [CrossRef]
- Jeong, H.; Kim, S.; Hong, B.J.; Lee, C.J.; Kim, Y.E.; Bok, S.; Oh, J.M.; Gwak, S.H.; Yoo, M.Y.; Lee, M.S.; et al. Tumor-Associated Macrophages Enhance Tumor Hypoxia and Aerobic Glycolysis. Cancer Res. 2019, 79, 795–806. [Google Scholar] [CrossRef] [Green Version]
- Bregenzer, M.E.; Horst, E.N.; Mehta, P.; Novak, C.M.; Raghavan, S.; Snyder, C.S.; Mehta, G. Integrated cancer tissue engineering models for precision medicine. PLoS ONE 2019, 14, e0216564. [Google Scholar] [CrossRef] [Green Version]
- Bhattacharya, S.; Calar, K.; de la Puente, P. Mimicking tumor hypoxia and tumor-immune interactions employing three-dimensional in vitro models. J. Exp. Clin. Cancer Res. 2020, 39, 75. [Google Scholar] [CrossRef]
- Shirmanova, M.V.; Druzhkova, I.N.; Lukina, M.M.; Matlashov, M.E.; Belousov, V.V.; Snopova, L.B.; Prodanetz, N.N.; Dudenkova, V.V.; Lukyanov, S.A.; Zagaynova, E.V. Intracellular pH imaging in cancer cells in vitro and tumors in vivo using the new genetically encoded sensor SypHer2. Biochim. Biophys. Acta 2015, 1850, 1905–1911. [Google Scholar] [CrossRef] [PubMed]
- Li, H.J.; Du, J.Z.; Du, X.J.; Xu, C.F.; Sun, C.Y.; Wang, H.X.; Cao, Z.T.; Yang, X.Z.; Zhu, Y.H.; Nie, S.; et al. Stimuli-responsive clustered nanoparticles for improved tumor penetration and therapeutic efficacy. Proc. Natl. Acad. Sci. USA 2016, 113, 4164–4169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swetha, K.L.; Maravajjala, K.S.; Sharma, S.; Chowdhury, R.; Roy, A. Development of a tumor extracellular pH-responsive nanocarrier by terminal histidine conjugation in a star shaped poly(lactic-co-glycolic acid). Eur. Polym. J. 2021, 147, 110337. [Google Scholar] [CrossRef]
- Cho, H.; Jammalamadaka, U.; Tappa, K. Nanogels for Pharmaceutical and Biomedical Applications and Their Fabrication Using 3D Printing Technologies. Materials 2018, 11, 302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stawicki, B.; Schacher, T.; Cho, H. Nanogels as a Versatile Drug Delivery System for Brain Cancer. Gels 2021, 7, 63. [Google Scholar] [CrossRef]
- Yang, G.; Fu, S.; Yao, W.; Wang, X.; Zha, Q.; Tang, R. Hyaluronic acid nanogels prepared via ortho ester linkages show pH-triggered behavior, enhanced penetration and antitumor efficacy in 3-D tumor spheroids. J. Colloid Interface Sci. 2017, 504, 25–38. [Google Scholar] [CrossRef]
- Mura, S.; Nicolas, J.; Couvreur, P. Stimuli-responsive nanocarriers for drug delivery. Nat. Mater. 2013, 12, 991–1003. [Google Scholar] [CrossRef]
- Lagies, S.; Schlimpert, M.; Neumann, S.; Waldin, A.; Kammerer, B.; Borner, C.; Peintner, L. Cells grown in three-dimensional spheroids mirror in vivo metabolic response of epithelial cells. Commun. Biol. 2020, 3, 246. [Google Scholar] [CrossRef]
- Shahriari, M.; Zahiri, M.; Abnous, K.; Taghdisi, S.M.; Ramezani, M.; Alibolandi, M. Enzyme responsive drug delivery systems in cancer treatment. J. Control Release 2019, 308, 172–189. [Google Scholar] [CrossRef]
- Breslin, S.; O’Driscoll, L. The Relevance of Using 3D Cell Cultures, in Addition to 2D Monolayer Cultures, When Evaluating Breast Cancer Drug Sensitivity and Resistance. Oncotarget 2016, 7, 45745–45756. [Google Scholar] [CrossRef] [Green Version]
- Kulkarni, P.S.; Haldar, M.K.; Nahire, R.R.; Katti, P.; Ambre, A.H.; Muhonen, W.W.; Shabb, J.B.; Padi, S.K.; Singh, R.K.; Borowicz, P.P.; et al. Mmp-9 responsive PEG cleavable nanovesicles for efficient delivery of chemotherapeutics to pancreatic cancer. Mol. Pharm. 2014, 11, 2390–2399. [Google Scholar] [CrossRef] [Green Version]
- Liu, R.; Hu, C.; Yang, Y.; Zhang, J.; Gao, H. Theranostic nanoparticles with tumor-specific enzyme-triggered size reduction and drug release to perform photothermal therapy for breast cancer treatment. Acta Pharm. Sin. B 2019, 9, 410–420. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Yang, X.; Yin, Q.; Cai, K.; Wang, H.; Chaudhury, I.; Yao, C.; Zhou, Q.; Kwon, M.; Hartman, J.A.; et al. Investigating the optimal size of anticancer nanomedicine. Proc. Natl. Acad. Sci. USA 2014, 111, 15344–153449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McAtee, C.O.; Barycki, J.J.; Simpson, M.A. Emerging roles for hyaluronidase in cancer metastasis and therapy. Adv. Cancer Res. 2014, 123, 1–34. [Google Scholar]
- Hu, C.; Cun, X.; Ruan, S.; Liu, R.; Xiao, W.; Yang, X.; Yang, Y.; Yang, C.; Gao, H. Enzyme-triggered size shrink and laser-enhanced NO release nanoparticles for deep tumor penetration and combination therapy. Biomaterials 2018, 168, 64–75. [Google Scholar] [CrossRef]
- Tan, P.; Cai, H.; Wei, Q.; Tang, X.; Zhang, Q.; Kopytynski, M.; Yang, J.; Yi, Y.; Zhang, H.; Gong, Q.; et al. Enhanced chemo-photodynamic therapy of an enzyme-responsive prodrug in bladder cancer patient-derived xenograft models. Biomaterials 2021, 277, 121061. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, N.; Sloane, B.F. Cathepsin B: Multiple roles in cancer. Proteom. Clin. Appl. 2014, 8, 427–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hong, S.H.; Larocque, K.; Jaunky, D.B.; Piekny, A.; Oh, J.K. Dual disassembly and biological evaluation of enzyme/oxidation-responsive polyester-based nanoparticulates for tumor-targeting delivery. Colloids Surf B Biointerfaces 2018, 172, 608–617. [Google Scholar] [CrossRef]
- Brown, J.M.; Wilson, W.R. Exploiting tumour hypoxia in cancer treatment. Nat. Rev. Cancer 2004, 4, 437–447. [Google Scholar] [CrossRef]
- Leek, R.; Grimes, D.R.; Harris, A.L.; McIntyre, A. Methods: Using Three-Dimensional Culture (Spheroids) as an In Vitro Model of Tumour Hypoxia. Adv. Exp. Med. Biol. 2016, 899, 167–196. [Google Scholar] [PubMed]
- Riffle, S.; Hegde, R.S. Modeling tumor cell adaptations to hypoxia in multicellular tumor spheroids. J. Exp. Clin. Cancer Res. 2017, 36, 102. [Google Scholar] [CrossRef]
- Kulkarni, P.; Haldar, M.K.; You, S.; Choi, Y.; Mallik, S. Hypoxia-Responsive Polymersomes for Drug Delivery to Hypoxic Pancreatic Cancer Cells. Biomacromolecules 2016, 17, 2507–2513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mamnoon, B.; Feng, L.; Froberg, J.; Choi, Y.; Sathish, V.; Mallik, S. Hypoxia-Responsive, Polymeric Nanocarriers for Targeted Drug Delivery to Estrogen Receptor-Positive Breast Cancer Cell Spheroids. Mol. Pharm. 2020, 17, 4312–4322. [Google Scholar] [CrossRef]
- Xu, Q.; He, C.; Xiao, C.; Chen, X. Reactive Oxygen Species (ROS) Responsive Polymers for Biomedical Applications. Macromol. Biosci. 2016, 16, 635–646. [Google Scholar] [CrossRef] [Green Version]
- Ballance, W.C.; Qin, E.C.; Chung, H.J.; Gillette, M.U.; Kong, H. Reactive oxygen species-responsive drug delivery systems for the treatment of neurodegenerative diseases. Biomaterials 2019, 217, 119292. [Google Scholar] [CrossRef]
- Tao, W.; He, Z. ROS-responsive drug delivery systems for biomedical applications. Asian J. Pharm. Sci. 2018, 13, 101–112. [Google Scholar] [CrossRef]
- Argenziano, M.; Foglietta, F.; Canaparo, R.; Spagnolo, R.; Della Pepa, C.; Caldera, F.; Trotta, F.; Serpe, L.; Cavalli, R. Biological Effect Evaluation of Glutathione-Responsive Cyclodextrin-Based Nanosponges: 2D and 3D Studies. Molecules 2020, 25, 2775. [Google Scholar] [CrossRef] [PubMed]
- Niculescu, A.G.; Grumezescu, A.M. Photodynamic Therapy—An Up-to-Date Review. Appl. Sci. 2021, 11, 3626. [Google Scholar] [CrossRef]
- Evans, C.L. Three-Dimensional in Vitro Cancer Spheroid Models for Photodynamic Therapy: Strengths and Opportunities. Front. Phys. 2015, 3, 15. [Google Scholar] [CrossRef] [Green Version]
- Calixto, G.M.; Bernegossi, J.; De Freitas, L.M.; Fontana, C.R.; Chorilli, M. Nanotechnology-Based Drug Delivery Systems for Photodynamic Therapy of Cancer: A Review. Molecules 2016, 21, 342. [Google Scholar] [CrossRef] [PubMed]
- Mozhi, A.; Sunil, V.; Zhan, W.; Ghode, P.B.; Thakor, N.V.; Wang, C.H. Enhanced penetration of pro-apoptotic and anti-angiogenic micellar nanoprobe in 3D multicellular spheroids for chemophototherapy. J. Control Release 2020, 323, 502–518. [Google Scholar] [CrossRef] [PubMed]
- Moreira, A.F.; Dias, D.R.; Costa, E.C.; Correia, I.J. Thermo- and pH-responsive nano-in-micro particles for combinatorial drug delivery to cancer cells. Eur. J. Pharm. Sci. 2017, 104, 42–51. [Google Scholar] [CrossRef]
- Senavirathna, L.K.; Fernando, R.; Maples, D.; Zheng, Y.; Polf, J.C.; Ranjan, A. Tumor Spheroids as an In Vitro Model for Determining the Therapeutic Response to Proton Beam Radiotherapy and Thermally Sensitive Nanocarriers. Theranostics 2013, 3, 687–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serpe, L.; Foglietta, F.; Canaparo, R. Nanosonotechnology: The next challenge in cancer sonodynamic therapy. Nanotechnol. Rev. 2012, 1, 173–182. [Google Scholar] [CrossRef]
- Zhao, Y.Z.; Du, L.N.; Lu, C.T.; Jin, Y.G.; Ge, S.P. Potential and problems in ultrasound-responsive drug delivery systems. Int. J. Nanomed. 2013, 8, 1621–1633. [Google Scholar]
- Schroeder, A.; Honen, R.; Turjeman, K.; Gabizon, A.; Kost, J.; Barenholz, Y. Ultrasound triggered release of cisplatin from liposomes in murine tumors. J. Control Release 2009, 137, 63–68. [Google Scholar] [CrossRef]
- Kheirolomoom, A.; Mahakian, L.M.; Lai, C.Y.; Lindfors, H.A.; Seo, J.W.; Paoli, E.E.; Watson, K.D.; Haynam, E.M.; Ingham, E.S.; Xing, L.; et al. Copper−Doxorubicin as a Nanoparticle Cargo Retains Efficacy with Minimal Toxicity. Mol. Pharm. 2010, 7, 1948–1958. [Google Scholar] [CrossRef] [Green Version]
- Logan, K.; Foglietta, F.; Nesbitt, H.; Sheng, Y.; McKaig, T.; Kamila, S.; Gao, J.; Nomikou, N.; Callan, B.; McHale, A.P.; et al. Targeted chemo-sonodynamic therapy treatment of breast tumours using ultrasound responsive microbubbles loaded with paclitaxel, doxorubicin and Rose Bengal. Eur. J. Pharm. Biopharm. 2019, 139, 224–231. [Google Scholar] [CrossRef]
- Foglietta, F.; Pinnelli, V.; Giuntini, F.; Barbero, N.; Panzanelli, P.; Durando, G.; Terreno, E.; Serpe, L.; Canaparo, R. Sonodynamic Treatment Induces Selective Killing of Cancer Cells in an In Vitro Co-Culture Model. Cancers 2021, 13, 3852. [Google Scholar] [CrossRef]
- Logan, K.A.; Nesbitt, H.; Callan, B.; Gao, J.; McKaig, T.; Taylor, M.; Love, M.; McHale, A.P.; Callan, J.F. Synthesis of a gemcitabine-modified phospholipid and its subsequent incorporation into a single microbubble formulation loaded with paclitaxel for the treatment of pancreatic cancer using ultrasound-targeted microbubble destruction. Eur. J. Pharm. Biopharm. 2021, 165, 374–382. [Google Scholar] [CrossRef]
- Grainger, S.J.; Serna, J.V.; Sunny, S.; Zhou, Y.; Deng, C.X.; El-Sayed, M.E. Pulsed ultrasound enhances nanoparticle penetration into breast cancer spheroids. Mol. Pharm. 2010, 7, 2006–2019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tran, B.C.; Seo, J.; Fowlkes, J.B.; Cain, C.A. Microbubble enhanced threshold reductions for tissue damage using high intensity ultrasound. In Proceedings of the 2001 Ultrasonics Symposium, Atlanta, GA, USA, 7–10 October 2001. [Google Scholar]
- Benhal, P.; Broda, A.; Najafali, D.; Malik, P.; Mohammed, A.; Ramaswamy, B.; Depireux, D.A.; Shimoji, M.; Shukoor, M.; Shapiro, B. On-chip testing of the speed of magnetic nano- and micro-particles under a calibrated magnetic gradient. J. Magn. Magn. Mater. 2019, 474, 187–198. [Google Scholar] [CrossRef]
- Geczy, R.; Agnoletti, M.; Hansen, M.F.; Kutter, J.P.; Saatchi, K.; Häfeli, U.O. Microfluidic approaches for the production of monodisperse, superparamagnetic microspheres in the low micrometer size range. J. Magn. Magn. Mater. 2019, 471, 286–293. [Google Scholar] [CrossRef]


| Model | Advantages | Disadvantages |
|---|---|---|
| 2D in vitro models |
|
|
| 3D in vitro models |
|
|
| In vivo models |
|
|
| Endogenous | Stimuli | 3D Model | Drug-Delivery Systems (DDSs) | Main Results | References |
|---|---|---|---|---|---|
| pH | Polymeric cluster NPs (iCluster) | Polymeric cluster NPs (iCluster) | The pH-mediated release of the dendrimers promoted their penetration into the spheroid, facilitating the increased cellular drug internalization | [44] | |
| Histidine modified star-shaped PLGA (sPLGA-His NPs) loaded with docetaxel and disulfiram | Histidine modified star-shaped PLGA (sPLGA-His NPs) loaded with docetaxel and disulfiram | Docetaxel and disulfiram exhibited more rapid drug release by sPLGA-His NPs at pH 6.5 than at pH 7.4 in a 3D colon cancer model | [45] | ||
| Human liver (HepG2) and human neuroblastoma (SH-SY5Y) spheroids | pH-triggered hyaluronic acid nanogel system by copolymerizing methacrylate hyaluronic acid with a cross linker that contains ortho ester groups that can deliver doxorubicin (DOX@HA-NGs) | Doxorubicin showed excellent cancer cell uptake when delivered as DOX@HA-NGs, along with enhanced anticancer activity | [48] | ||
| Enzyme | Human pancreatic ductal (MIAPaCa-2 and PANC-1) carcinoma spheroids | Pegylated nanovesicles loaded with gemcitabine | Gemcitabine release is promoted by the destabilization of the pegylated nanovesicles under glutathione and metalloproteinase-9 action | [53] | |
| Human breast cancer (4T1) spheroids | Large NPs loaded with indocyanine green (ICG) and hyaluronic acid (HA) (AuNC@CBSA- ICG@HA) | Tumor overexpression of hyaluronidase allows a better penetration of NPs into 4T1 spheroids | [54] | ||
| Human bladder (T24) spheroids | A cathepsin B-sensitive polymer-paclitaxel (PTX) prodrug and the photosensitizer chlorin e6 (Ce6) loaded into NPs (poly(OEGMA)-PTX@Ce6) | Ce6 released into T24 spheroids and then light irradiated produced ROS. The PTX was also released by cathepsin B, determining anticancer effect | [58] | ||
| Human cervical adenocarcinoma (HeLa cells) and human alveolar adenocarcinoma (A549 cells) spheroids | Polyester-based nanoparticles loaded with doxorubicin (Dox-NPs) | Spheroids incubated with Dox-NPs and then exposed to esterase and hydrogen peroxide, underwent to increased Dox penetration and fluorescence intensity | [60] | ||
| Hypoxia | Human pancreatic (BxPC-3) spheroids | Polymersomes loaded with gemcitabine and erlotinib | Gemcitabine and erlotinib, entrapped into polymersomes, were released under spheroid hypoxic condition up to 90% | [64] | |
| Human breast cancer (MCF-7) spheroids | Polymersomes with an estrogen receptor (ER) ligand incorporated onto the surface of the carrier to deliver doxorubicin (E2-Dox-HRPS) | Targeted polymersomes showed a difference in cell viability in normoxic and hypoxic condition | [65] | ||
| ROS | Human cervical adenocarcinoma (HeLa cells) and human alveolar adenocarcinoma (A549 cells) spheroids | Polyester-based nanoparticles loaded with doxorubicin (Dox-NPs) | Spheroids incubated with Dox-NPs and then exposed to esterase and hydrogen peroxide incubation, underwent to increased Dox penetration and fluorescence intensity | [60] |
| Exogenous | Stimuli | 3D Model | Drug Delivery Systems (DDSs) | Main Results | References |
|---|---|---|---|---|---|
| Light | Human bladder (T24) spheroids | A cathepsin B-sensitive polymer-paclitaxel (PTX) prodrug and the photosensitizer chlorin e6 (Ce6) loaded into NPs (poly(OEGMA)-PTX@Ce6) | Ce6 released into the T24 spheroids and then light irradiated produced ROS. The PTX was also released by cathepsin B, determining anticancer effect | [58] | |
| Rat C6 glioma cell line (C6 MCS) | Targeted Micellar Nanoprobe (TMNP) with exceptionally high encapsulation efficiencies of a hydrophobic drug simvastatin (SV) and a photosensitizer protoporphyrin IX (PpIX) | TMNP under light irradiation showed huge amount of ROS production and induction in apoptotic and necrotic pathways | [73] | ||
| Temperature | Human cervical (HeLa) spheroids | Doxorubicin-loaded gold-core silica-shell nanorods with salicylic acid-loaded poly (lactic-co-glycolic acid)-based microparticles (NIMPS) | Uniform doxorubicin distribution under NIR irradiation along with spheroid surface disorganization | [74] | |
| Adenocarcinomic human alveolar basal epithelial (A549) spheroids | Low temperature-sensitive liposomes (LTSLs) loaded with doxorubicin | Combination between LTSLs and mild hyperthermia induced reduction in spheroid viability | [75] | ||
| Ultrasound | Human breast cancer spheroids (MCF-7) | Microbubbles loaded with rose bengal, paclitaxel, and doxorubicin (O2MB-PTX-Dox/O2MB-PTX-RB) | MCF-7 spheroid volume reduction and increase in necrotic cells under sonodynamic exposure of O2MB-PTX-Dox/O2MB-PTX-RB | [80] | |
| Human pancreatic (BxPC-3) spheroids | Gemcitabine-modified phospholipid incorporated into a single microbubble formulation loaded with PTX (Lipid-Gem-PTX MB) | A statistically significant reduction in BxPC-3 spheroid volume was observed when spheroids underwent to US exposure of Lipid-Gem-PTX MB | [82] | ||
| Magnetic | On-chip system | Magnetic NPs (MNPs) | Particles with a diameter size between 10 and 100 μm displayed the similar trend | [85] | |
| Microfluidic chip | Magnetic NPs (MNPs) | MNPs showed highly spherical shape and superparamagnetic properties in the system | [86] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foglietta, F.; Serpe, L.; Canaparo, R. The Effective Combination between 3D Cancer Models and Stimuli-Responsive Nanoscale Drug Delivery Systems. Cells 2021, 10, 3295. https://doi.org/10.3390/cells10123295
Foglietta F, Serpe L, Canaparo R. The Effective Combination between 3D Cancer Models and Stimuli-Responsive Nanoscale Drug Delivery Systems. Cells. 2021; 10(12):3295. https://doi.org/10.3390/cells10123295
Chicago/Turabian StyleFoglietta, Federica, Loredana Serpe, and Roberto Canaparo. 2021. "The Effective Combination between 3D Cancer Models and Stimuli-Responsive Nanoscale Drug Delivery Systems" Cells 10, no. 12: 3295. https://doi.org/10.3390/cells10123295