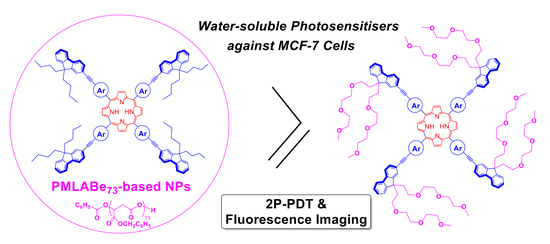
Encapsulation of Hydrophobic Porphyrins into Biocompatible Nanoparticles: An Easy Way to Benefit of Their Two-Photon Phototherapeutic Effect without Hydrophilic Functionalization
Abstract
:Simple Summary
Abstract
1. Introduction
2. Results and Discussion
2.1. Preparation and Characterization of Porphyrin-Loaded NPs Based on PMLABe73
2.2. Emission Properties of the Porphyrin-Loaded NPs
2.3. In Vitro PDT Assays Using Porphyrin-Loaded NPs
3. Materials and Methods
3.1. General
3.2. Preparation of Starting Polymer
3.3. Preparation of Porphyrin Stock Solutions
3.4. Preparation of PMLABe73-Based NPs
3.5. Cell Culture
3.6. Methods
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dabrowski, J.M.; Pucelik, B.; Regiel-Futyra, A.; Brindell, M.; Mazuryk, O.; Kyzioł, A.; Stochel, G.; Macyk, W.; Arnaut, L.G. Engineering of relevant photodynamic processes through structural modifications of metallotetrapyrrolic photosensitizers. Coord. Chem. Rev. 2016, 325, 67–101. [Google Scholar] [CrossRef]
- Figueira, F.; Pereira, P.M.R.; Silva, S.; Cavaleiro, J.A.S.; Tomé, J.P.C. Porphyrins and Phthalocyanines Decorated with Dendrimers: Synthesis and Biomedical Applications. Curr. Org. Synth. 2014, 11, 110–126. [Google Scholar] [CrossRef]
- Josefsen, L.B.; Boyle, R.W. Unique Diagnostic and Therapeutic Roles of Porphyrins and Phthalocyanines in Photodynamic Therapy, Imaging and Theranostics. Theranostics 2012, 2, 916–966. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandlanda, J.; Malatestic, N.; Boyle, R. Porphyrins and related macrocycles: Combining photosensitization withradio- or optical-imaging for next generation theranostic agents. Photodiagnosis Photodyn. Ther. 2018, 23, 281–294. [Google Scholar] [CrossRef]
- Zhang, Y.; Lovell, J.F. Recent applications of phthalocyanines and naphthalocyanines for imaging and therapy. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2018, 9, e1420. [Google Scholar] [CrossRef] [Green Version]
- Wong, R.C.H.; Lo, P.-C.; Ng, D.K.P. Stimuli responsive phthalocyanine-based fluorescent probes and photosensitizers. Coord. Chem. Rev. 2019, 379, 30–46. [Google Scholar] [CrossRef]
- Bonnett, R. Photosensitizers of the porphyrin and phthalocyanine series for photodynamic therapy. Chem. Soc. Rev. 1995, 24, 19–33. [Google Scholar] [CrossRef]
- Starkey, J.R.; Pascucci, E.M.; Drobizhev, M.A.; Elliott, A.; Rebane, A.K. Vascular targeting to the SST2 receptor improves the therapeutic response to near-IR two-photon activated PDT for deep-tissue cancer treatment. Biochim. Biophys. Acta 2013, 1830, 4594–4603. [Google Scholar] [CrossRef] [Green Version]
- Khurana, M.; Collins, H.A.; Karotki, A.; Anderson, H.L.; Cramb, D.T.; Wilson, B.C. Quantitative In Vitro Demonstration of Two-Photon Photodynamic Therapy Using Photofrin® and Visudyne®. Photochem. Photobiol. 2007, 83, 1441–1448. [Google Scholar] [CrossRef]
- Sun, Z.; Zhang, L.-P.; Wu, F.; Zhao, Y. Photosensitizers for Two-Photon Excited Photodynamic Therapy. Adv. Funct. Mater. 2017, 27, 1704079. [Google Scholar] [CrossRef]
- Pawlicki, M.; Collins, H.A.; Denning, R.G.; Anderson, H.L. Two-Photon Absorption and the Design of Two-Photon Dyes. Angew. Chem. Int. Ed. 2009, 48, 3244–3266. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, P.; Patravale, V. The upcoming field of theranostic nanomedicine: An overview. J. Biomed. Nanotechnol. 2012, 8, 859–882. [Google Scholar] [CrossRef] [PubMed]
- Bhaumik, J.; Mittal, A.K.; Banerjee, A.; Chisti, Y.; Banerjee, U.C. Applications of phototheranostic nanoagents in photodynamic therapy. Nano Res. 2015, 8, 1373–1394. [Google Scholar] [CrossRef]
- Yao, D.; Zhang, X.; Mongin, O.; Paul, F.; Paul-Roth, C.O. Synthesis and Characterization of New Conjugated Fluorenyl-Porphyrin Dendrimers for Optics. Chem. Eur. J. 2016, 22, 5583–5597. [Google Scholar] [CrossRef]
- Yao, D.; Zhang, X.; Triadon, A.; Richy, N.; Mongin, O.; Blanchard-Desce, M.; Paul, F.; Paul-Roth, C.O. New Conjugated meso-Tetrafluorenylporphyrin-cored Derivatives as Fluorescent Two-photon Photosensitizers for Singlet Oxygen Generation. Chem. Eur. J. 2017, 23, 2635–2647. [Google Scholar] [CrossRef]
- Abid, S.; Ben Hassine, S.; Sun, Z.; Richy, N.; Camerel, F.; Jamoussi, B.; Blanchard-Desce, M.; Mongin, O.; Paul, F.; Paul-Roth, C.O. Impact of Changing the Core in Tetrapyrrolic Dendrimers designed for Oxygen Sensitization: New Fluorescent Phthalocyanines-based Dendrimers with high Two-photon Absorption Cross-sections. Macromolecules 2021, 54, 6726–6744. [Google Scholar] [CrossRef]
- Shi, L.; Nguyen, C.; Daurat, M.; Dhieb, A.C.; Smirani, W.; Blanchard-Desce, M.; Gary-Bobo, M.; Mongin, O.; Paul-Roth, C.; Paul, F. Biocompatible Conjugated Fluorenylporphyrins for Two-photon Photodynamic Therapy and Fluorescence Imaging. Chem. Commun. 2019, 55, 12231–12234. [Google Scholar] [CrossRef]
- Abid, S.; Nguyen, C.; Daurat, M.; Durand, D.; Jamoussi, B.; Blanchard-Desce, M.; Gary-Bobo, M.; Mongin, O.; Paul-Roth, C.O.; Paul, F. Biocompatible fluorenylphthalocyanines for one and two-photon photodynamic therapy and fluorescence imaging. Dyes Pigm. 2022, 197, 109840. [Google Scholar] [CrossRef]
- Huang, Z.W.; Laurent, V.; Chetouani, G.; Ljubimova, J.Y.; Holler, E.; Benvegnu, T.; Loyer, P.; Cammas-Marion, S. New functional degradable and bio-compatible nanoparticles based on poly(malic acid) derivatives for site-specific anti-cancer drug delivery. Int. J. Pharm. 2012, 423, 84–92. [Google Scholar] [CrossRef] [Green Version]
- Loyer, P.; Bedhouche, W.; Huang, Z.W.; Cammas-Marion, S. Degradable and Biocompatible Nanoparticles Decorated with Cyclic RGD Peptide for Efficient Drug Delivery to Hepatoma Cells In Vitro. Int. J. Pharm. 2013, 454, 727–737. [Google Scholar] [CrossRef] [Green Version]
- Casajus, H.; Saba, S.; Vlach, M.; Vène, E.; Ribault, C.; Tranchimand, S.; Nugier-Chauvin, C.; Dubreucq, E.; Loyer, P.; Cammas-Marion, S.; et al. Cell Uptake and Biocompatibility of Nanoparticles Prepared from Poly(benzyl malate) (Co)polymers Obtained through Chemical and Enzymatic Polymerization in Human HepaRG Cells and Primary Macrophages. Polymers 2018, 10, 1244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brossard, C.; Vlach, M.; Vène, E.; Ribault, C.; Dorcet, V.; Noiret, N.; Loyer, P.; Lepareur, N.; Cammas-Marion, S. Synthesis of Poly(Malic Acid) Derivatives End-Functionalized with Peptides and Preparation of Biocompatible Nanoparticles to Target Hepatoma Cells. Nanomaterials 2021, 11, 958. [Google Scholar] [CrossRef] [PubMed]
- Cammas, S.; Renard, I.; Langlois, V.; Guérin, P. Poly(beta-malic acid): Obtaining of high molecular weights by improvement of the synthesis route. Polymer 1996, 37, 4215–4220. [Google Scholar] [CrossRef]
- Thioune, O.; Fessi, H.; Devissaguet, J.P.; Puisieux, F. Preparation of pseudolatex by nanoprecipitation: Influence of the solvent nature on intrinsic viscosity and interaction constant. Int. J. Pharm. 1997, 146, 233–238. [Google Scholar] [CrossRef]
- Vargas-Guerreo, M.G.; Pluta, J.B.; Bellec, N.; Cammas-Marion, S.; Camerel, F. Nanoprecipitation of Biocompatible Poly(malic acid) Derivative, Its Ability to Encapsulate a Molecular Photothermal Agent and Photothermal Properties of the Resulting Nanoparticles. Molecules 2021, 26, 7703. [Google Scholar] [CrossRef] [PubMed]
- Gehlen, M.H.; De Schryver, F.C. Time-resolved fluorescence quenching in micellar assemblies. Chem. Rev. 1993, 93, 199–221. [Google Scholar] [CrossRef]
- Cepraga, C.; Gallavardin, T.; Marotte, S.; Lanoë, P.-H.; Mulatier, J.-C.; Lerouge, F.; Parola, S.; Lindgren, M.; Baldeck, P.L.; Marvel, J.; et al. Biocompatible well-defined chromophore–polymer conjugates for photodynamic therapy and two-photon imaging. Polym. Chem. 2013, 4, 61–67. [Google Scholar] [CrossRef]
- Monnereau, C.; Marotte, S.; Lanoë, P.-H.; Maury, O.; Baldeck, P.L.; Kreher, D.; Favier, A.; Charreyre, M.-T.; Marvel, J.; Leverrier, Y.; et al. Water-soluble chromophores with star-shaped oligomeric arms: Synthesis, spectroscopic studies and first results in bio-imaging and cell death induction. New J. Chem. 2012, 36, 2328–2333. [Google Scholar] [CrossRef]
- Eaton, D.F. Reference materials for fluorescence measurement. Pure Appl. Chem. 1988, 60, 1107–1114. [Google Scholar] [CrossRef]
- Demas, J.N.; Crosby, G.A. The Measurement of Photoluminescence Quantum Yields. A Review. J. Phys. Chem. 1971, 75, 991–1024. [Google Scholar]
- Brouwer, A.M. Standards for photoluminescence quantum yield measurements in solution (IUPAC Technical Report). Pure Appl. Chem. 2011, 83, 2213–2228. [Google Scholar] [CrossRef] [Green Version]









| NP | Composition | Dh (nm) a,b | PDI b,c |
|---|---|---|---|
| NP1 | PMLABe73[1b] (10 wt%) | 213 ± 1 | 0.20 ± 0.03 |
| NP2 | PMLABe73[1b] (1 wt%) | 232 ± 6 | 0.17 ± 0.01 |
| NP3 | PMLABe73[2b] (10 wt%) | 226 ± 2 | 0.14 ± 0.12 |
| NP4 | PMLABe73[2b] (1 wt%) | 260 ± 2 | 0.13 ± 0.05 |
| NP5 | PMLABe73 | 238 ± 1 | 0.17 ± 0.03 |
| NP | Composition | Dh (nm) a,b | PDI b,c |
|---|---|---|---|
| NP1 | PMLABe73[1b] (10 wt%) | 175 ± 2 | 0.23 ± 0.02 |
| NP2 | PMLABe73[1b] (1 wt%) | 204 ± 7 | 0.16 ± 0.02 |
| NP3 | PMLABe73[2b] (10 wt%) | 140 ± 2 | 0.30 ± 0.07 |
| NP4 | PMLABe73[2b] (1 wt%) | 207 ± 2 | 0.24 ± 0.04 |
| NP5 | PMLABe73 | 199 ± 2 | 0.23 ± 0.02 |
| Compound | λabs (nm) a | λem (nm) b | ϕF (%) c |
|---|---|---|---|
| NP1 | 430 | 661, 726 | 3 |
| NP2 | 429 | 661, 725 | 6 |
| NP3 | 435 | 666, 730 | 6 |
| NP4 | 432 | 663, 728 | 15 |
| 1a | 427 | 660, 724 | 3 |
| 2a | 432 | 664, 731 | 3 |
| 1b d | 426 | 657, 722 | 20 |
| 2b a | 432 | 660, 726 | 23 |
| NP | Composition | wt% (Exp) a | %exp/%theo Ratio b |
|---|---|---|---|
| NP1 | PMLABe73[1b] (10 wt%) | 4.6 | 46% |
| NP2 | PMLABe73[1b] (1 wt%) | 0.77 | 77% |
| NP3 | PMLABe73[2b] (10 wt%) | 7.0 | 70% |
| NP4 | PMLABe73[2b] (1 wt%) | 0.69 | 69% |
| Sample | Porphyrin | NP Concentration (µg·mL−1) | Actual Porphyrin Concentration (µg·mL−1) |
|---|---|---|---|
| NP1 | 1b | 25 | 1.15 |
| NP2 | 1b | 25 | 0.19 |
| NP3 | 2b | 25 | 1.75 |
| NP4 | 2b | 25 | 0.17 |
| NP5 | - | 25 | 0 |
| - | 1a | - | 1.15 |
| - | 1a | - | 0.19 |
| - | 2a | - | 1.75 |
| - | 2a | - | 0.17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shi, L.; Nguyen, C.; Daurat, M.; Richy, N.; Gauthier, C.; Rebecq, E.; Gary-Bobo, M.; Cammas-Marion, S.; Mongin, O.; Paul-Roth, C.O.; et al. Encapsulation of Hydrophobic Porphyrins into Biocompatible Nanoparticles: An Easy Way to Benefit of Their Two-Photon Phototherapeutic Effect without Hydrophilic Functionalization. Cancers 2022, 14, 2358. https://doi.org/10.3390/cancers14102358
Shi L, Nguyen C, Daurat M, Richy N, Gauthier C, Rebecq E, Gary-Bobo M, Cammas-Marion S, Mongin O, Paul-Roth CO, et al. Encapsulation of Hydrophobic Porphyrins into Biocompatible Nanoparticles: An Easy Way to Benefit of Their Two-Photon Phototherapeutic Effect without Hydrophilic Functionalization. Cancers. 2022; 14(10):2358. https://doi.org/10.3390/cancers14102358
Chicago/Turabian StyleShi, Limiao, Christophe Nguyen, Morgane Daurat, Nicolas Richy, Corentin Gauthier, Estelle Rebecq, Magali Gary-Bobo, Sandrine Cammas-Marion, Olivier Mongin, Christine O. Paul-Roth, and et al. 2022. "Encapsulation of Hydrophobic Porphyrins into Biocompatible Nanoparticles: An Easy Way to Benefit of Their Two-Photon Phototherapeutic Effect without Hydrophilic Functionalization" Cancers 14, no. 10: 2358. https://doi.org/10.3390/cancers14102358