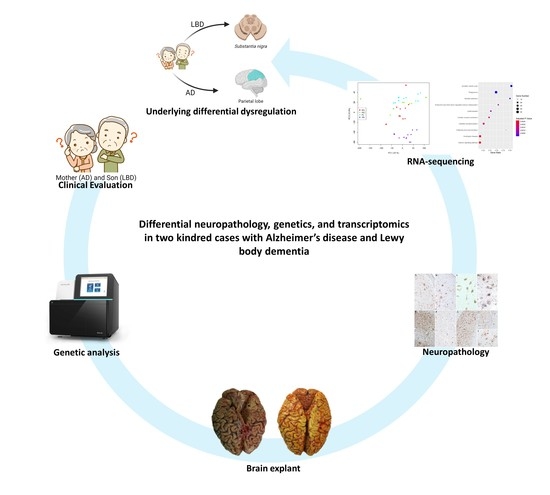
Differential Neuropathology, Genetics, and Transcriptomics in Two Kindred Cases with Alzheimer’s Disease and Lewy Body Dementia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Clinical Assessment
2.2. Tissue Collection, Preparation, and Immunohistochemistry
2.3. Genetic Analysis
2.3.1. DNA Preparation and Next-Generation Sequencing
2.3.2. Hereditary Hypothesis Analysis
2.4. RNA Extraction and Whole-Transcriptome Sequencing
2.5. Pathway and Gene Ontology Analysis
3. Results
3.1. Clinical Observation
3.2. Neuropathology and Immunohistochemistry
3.3. Genetic Analysis
3.4. Transcriptome Profile
3.5. KEGG Pathway and GO Term Analysis
3.5.1. Substantia Nigra
3.5.2. Parietal Lobe
3.5.3. Basal Ganglia
3.5.4. Hippocampus
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morris, J.C. Classification of Dementia and Alzheimer’s Disease. Acta Neurol. Scand. Suppl. 1996, 165, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Mirra, S.S.; Heyman, A.; McKeel, D.; Sumi, S.M.; Crain, B.J.; Brownlee, L.M.; Vogel, F.S.; Hughes, J.P.; van Belle, G.; Berg, L.; et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part II. Standardization of the Neuropathologic Assessment of Alzheimer’s Disease. Neurology 1991, 41, 479–486. [Google Scholar] [CrossRef]
- Braak, H.; Alafuzoff, I.; Arzberger, T.; Kretzschmar, H.; Tredici, K. Staging of Alzheimer Disease-Associated Neurofibrillary Pathology Using Paraffin Sections and Immunocytochemistry. Acta Neuropathol. 2006, 112, 389–404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montine, T.J.; Phelps, C.H.; Beach, T.G.; Bigio, E.H.; Cairns, N.J.; Dickson, D.W.; Duyckaerts, C.; Frosch, M.P.; Masliah, E.; Mirra, S.S.; et al. National Institute on Aging-Alzheimer’s Association Guidelines for the Neuropathologic Assessment of Alzheimer’s Disease: A Practical Approach. Acta Neuropathol. 2012, 123, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Thal, D.R.; Rüb, U.; Orantes, M.; Braak, H. Phases of A Beta-Deposition in the Human Brain and Its Relevance for the Development of AD. Neurology 2002, 58, 1791–1800. [Google Scholar] [CrossRef]
- Jellinger, K.A. Dementia with Lewy Bodies and Parkinson’s Disease-Dementia: Current Concepts and Controversies. J. Neural. Transm. 2018, 125, 615–650. [Google Scholar] [CrossRef]
- Heidebrink, J.L. Is Dementia with Lewy Bodies the Second Most Common Cause of Dementia? J. Geriatr. Psychiatry Neurol. 2002, 15, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Weisman, D.; McKeith, I. Dementia with Lewy Bodies. Semin. Neurol. 2007, 27, 42–47. [Google Scholar] [CrossRef]
- Hogan, D.B.; Jetté, N.; Fiest, K.M.; Roberts, J.I.; Pearson, D.; Smith, E.E.; Roach, P.; Kirk, A.; Pringsheim, T.; Maxwell, C.J. The Prevalence and Incidence of Frontotemporal Dementia: A Systematic Review. Can. J. Neurol. Sci. 2016, 43, S96–S109. [Google Scholar] [CrossRef] [Green Version]
- McKeith, I.G.; Boeve, B.F.; DIckson, D.W.; Halliday, G.; Taylor, J.P.; Weintraub, D.; Aarsland, D.; Galvin, J.; Attems, J.; Ballard, C.G.; et al. Diagnosis and Management of Dementia with Lewy Bodies. Neurology 2017, 89, 88–100. [Google Scholar] [CrossRef] [Green Version]
- McKeith, I.G.; Dickson, D.W.; Lowe, J.; Emre, M.; O’Brien, J.T.; Feldman, H.; Cummings, J.; Duda, J.E.; Lippa, C.; Perry, E.K.; et al. Diagnosis and Management of Dementia with Lewy Bodies: Third Report of the DLB Consortium. Neurology 2005, 65, 1863–1872. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beach, T.G.; Adler, C.H.; Lue, L.F.; Sue, L.I.; Bachalakuri, J.; Henry-Watson, J.; Sasse, J.; Boyer, S.; Shirohi, S.; Brooks, R.; et al. Unified Staging System for Lewy Body Disorders: Correlation with Nigrostriatal Degeneration, Cognitive Impairment and Motor Dysfunction. Acta Neuropathol. 2009, 117, 613–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansen, L.; Salmon, D.; Galasko, D.; Masliah, E.; Katzman, R.; Deteresa, R.; Thal, L.; Pay, M.M.; Hofstetter, R.; Klauber, M.; et al. The Lewy Body Variant of Alzheimer’s Disease: A Clinical and Pathologic Entity. Neurology 1990, 40, 1–8. [Google Scholar] [CrossRef]
- Walker, L.; Attems, J. Relationship Between Tau, β Amyloid and α-Synuclein Pathologies. Adv. Exp. Med. Biol. 2019, 1184, 169–176. [Google Scholar] [CrossRef]
- Nelson, P.T.; Dickson, D.W.; Trojanowski, J.Q.; Jack, C.R.; Boyle, P.A.; Arfanakis, K.; Rademakers, R.; Alafuzoff, I.; Attems, J.; Brayne, C.; et al. Limbic-Predominant Age-Related TDP-43 Encephalopathy (LATE): Consensus Working Group Report. Brain 2019, 142, 1503–1527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marsh, S.E.; Blurton-Jones, M. Examining the Mechanisms That Link β-Amyloid and α-Synuclein Pathologies. Alzheimer’s Res. Ther. 2012, 4, 11. [Google Scholar] [CrossRef]
- Spires-Jones, T.; Knafo, S. Spines, Plasticity, and Cognition in Alzheimer’s Model Mice. Neural Plast. 2012, 2012, 319836. [Google Scholar] [CrossRef]
- Gomperts, S.N.; Rentz, D.M.; Moran, E.; Becker, J.A.; Locascio, J.J.; Klunk, W.E.; Mathis, C.A.; Elmaleh, D.R.; Shoup, T.; Fischman, A.J.; et al. Imaging Amyloid Deposition in Lewy Body Diseases. Neurology 2008, 71, 903–910. [Google Scholar] [CrossRef]
- Thal, D.R.; von Arnim, C.A.F.; Griffin, W.S.T.; Mrak, R.E.; Walker, L.; Attems, J.; Arzberger, T. Frontotemporal Lobar Degeneration FTLD-Tau: Preclinical Lesions, Vascular, and Alzheimer-Related Co-Pathologies. J. Neural Transm. 2015, 122, 1007–1018. [Google Scholar] [CrossRef]
- Ossenkoppele, R.; Pijnenburg, Y.A.L.; Perry, D.C.; Cohn-Sheehy, B.I.; Scheltens, N.M.E.; Vogel, J.W.; Kramer, J.H.; van der Vlies, A.E.; La Joie, R.; Rosen, H.J.; et al. The Behavioural/Dysexecutive Variant of Alzheimer’s Disease: Clinical, Neuroimaging and Pathological Features. Brain 2015, 138, 2732–2749. [Google Scholar] [CrossRef] [Green Version]
- Perry, D.C.; Brown, J.A.; Possin, K.L.; Datta, S.; Trujillo, A.; Radke, A.; Karydas, A.; Kornak, J.; Sias, A.C.; Rabinovici, G.D.; et al. Clinicopathological Correlations in Behavioural Variant Frontotemporal Dementia. Brain 2017, 140, 3329–3345. [Google Scholar] [CrossRef] [PubMed]
- Carmona, S.; Zahs, K.; Wu, E.; Dakin, K.; Bras, J.; Guerreiro, R. The Role of TREM2 in Alzheimer’s Disease and Other Neurodegenerative Disorders. Lancet Neurol. 2018, 17, 721–730. [Google Scholar] [CrossRef]
- Meeus, B.; Verstraeten, A.; Crosiers, D.; Engelborghs, S.; van den Broeck, M.; Mattheijssens, M.; Peeters, K.; Corsmit, E.; Elinck, E.; Pickut, B.; et al. DLB and PDD: A Role for Mutations in Dementia and Parkinson Disease Genes? Neurobiol. Aging 2012, 33, 629.e5–629.e18. [Google Scholar] [CrossRef]
- Geiger, J.T.; Ding, J.; Crain, B.; Pletnikova, O.; Letson, C.; Dawson, T.M.; Rosenthal, L.S.; Pantelyat, A.; Gibbs, J.R.; Albert, M.S.; et al. Next-Generation Sequencing Reveals Substantial Genetic Contribution to Dementia with Lewy Bodies. Neurobiol. Dis. 2016, 94, 55–62. [Google Scholar] [CrossRef] [Green Version]
- Keogh, M.J.; Kurzawa-Akanbi, M.; Griffin, H.; Douroudis, K.; Ayers, K.L.; Hussein, R.I.; Hudson, G.; Pyle, A.; Cordell, H.J.; Attems, J.; et al. Exome Sequencing in Dementia with Lewy Bodies. Transl. Psychiatry 2016, 6, e728. [Google Scholar] [CrossRef] [Green Version]
- Orme, T.; Hernandez, D.; Ross, O.A.; Kun-rodrigues, C.; Darwent, L.; Shepherd, C.E.; Parkkinen, L.; Ansorge, O.; Clark, L.; Honig, L.S.; et al. Analysis of Neurodegenerative Disease- Causing Genes in Dementia with Lewy Bodies. Acta Neuropathol. Commun. 2020, 8, 5. [Google Scholar] [CrossRef] [PubMed]
- Clarimon, J.; Moreno-Grau, S.; Cervera-Carles, L.; Dols-Icardo, O.; Sánchez-Juan, P.; Ruiz, A. Genetic Architecture of Neurodegenerative Dementias. Neuropharmacology 2020, 168, 108014. [Google Scholar] [CrossRef] [PubMed]
- Saunders, A.M.; Roses, A.D.; Pericak-Vance, M.A.; Dole, K.C.; Strittmatter, W.J.; Schmechel, D.E.; Szymanski, M.H.; McCown, N.; Manwaring, M.G.; Schmader, K.; et al. Apolipoprotein E Epsilon 4 Allele Distributions in Late-Onset Alzheimer’s Disease and in Other Amyloid-Forming Diseases. Lancet 1993, 342, 710–711. [Google Scholar] [CrossRef]
- Rongve, A.; Witoelar, A.; Ruiz, A.; Athanasiu, L.; Abdelnour, C.; Clarimon, J.; Heilmann-Heimbach, S.; Hernández, I.; Moreno-Grau, S.; de Rojas, I.; et al. GBA and APOE Ε4 Associate with Sporadic Dementia with Lewy Bodies in European Genome Wide Association Study. Sci. Rep. 2019, 9, 7013. [Google Scholar] [CrossRef]
- Guerreiro, R.; Ross, O.A.; Kun-Rodrigues, C.; Hernandez, D.G.; Orme, T.; Eicher, J.D.; Shepherd, C.E.; Parkkinen, L.; Darwent, L.; Heckman, M.G.; et al. Investigating the Genetic Architecture of Dementia with Lewy Bodies: A Two-Stage Genome-Wide Association Study. Lancet Neurol. 2018, 17, 64–74. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Qin, Z.H. Molecular and Cellular Mechanisms of Excitotoxic Neuronal Death. Apoptosis 2010, 15, 1382–1402. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, D.; Sandor, C.; Volpato, V.; Caffrey, T.M.; Monzón-Sandoval, J.; Bowden, R.; Alegre-Abarrategui, J.; Wade-Martins, R.; Webber, C. A Single-Cell Atlas of the Human Substantia Nigra Reveals Cell-Specific Pathways Associated with Neurological Disorders. Nat. Commun. 2020, 11, 4183. [Google Scholar] [CrossRef] [PubMed]
- Phung, D.M.; Lee, J.; Hong, S.K.; Kim, Y.E.; Yoon, J.; Kim, Y.J. Meta-Analysis of Differentially Expressed Genes in the Substantia Nigra in Parkinson’s Disease Supports Phenotype-Specific Transcriptome Changes. Front. Neurosci. 2020, 14, 596105. [Google Scholar] [CrossRef]
- Forés-Martos, J.; Boullosa, C.; Rodrigo-Domínguez, D.; Sánchez-Valle, J.; Suay-García, B.; Climent, J.; Falcó, A.; Valencia, A.; Puig-butillé, J.A.; Puig, S.; et al. Transcriptomic and Genetic Associations between Alzheimer’s Disease, Parkinson’s Disease, and Cancer. Cancers 2021, 13, 2990. [Google Scholar] [CrossRef] [PubMed]
- Kwok, J.B.; Loy, C.T.; Dobson-Stone, C.; Halliday, G.M. The Complex Relationship between Genotype, Pathology and Phenotype in Familial Dementia. Neurobiol. Dis. 2020, 145, 105082. [Google Scholar] [CrossRef] [PubMed]
- Poloni, T.E.; Medici, V.; Carlos, A.F.; Davin, A.; Ceretti, A.; Mangieri, M.; Cassini, P.; Vaccaro, R.; Zaccaria, D.; Abbondanza, S.; et al. Abbiategrasso Brain Bank Protocol for Collecting, Processing and Characterizing Aging Brains. J. Vis. Exp. 2020, e60296. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.C. Clinical Dementia Rating: A Reliable and Valid Diagnostic and Staging Measure for Dementia of the Alzheimer Type. Int. Psychogeriatr. 1997, 9, 173–176. [Google Scholar] [CrossRef]
- Palmieri, I.; Valente, M.; Farina, L.M.; Gana, S.; Minafra, B.; Zangaglia, R.; Pansarasa, O.; Sproviero, D.; Costa, A.; Pacchetti, C.; et al. PSEN1 Compound Heterozygous Mutations Associated with Cerebral Amyloid Angiopathy and Cognitive Decline Phenotype. Int. J. Mol. Sci. 2021, 22, 3870. [Google Scholar] [CrossRef]
- Kopanos, C.; Tsiolkas, V.; Kouris, A.; Chapple, C.E.; Albarca Aguilera, M.; Meyer, R.; Massouras, A. VarSome: The Human Genomic Variant Search Engine. Bioinformatics 2019, 35, 1978–1980. [Google Scholar] [CrossRef]
- Zucca, S.; Gagliardi, S.; Pandini, C.; Diamanti, L.; Bordoni, M.; Sproviero, D.; Arigoni, M.; Olivero, M.; Pansarasa, O. Data Descriptor: RNA-Seq pro Fi Ling in Peripheral Blood Mononuclear Cells of Amyotrophic Lateral Sclerosis Patients and Controls. Nature 2019, 6, 190006. [Google Scholar] [CrossRef]
- Leng, N.; Dawson, J.A.; Thomson, J.A.; Ruotti, V.; Rissman, A.I.; Smits, B.M.G.; Haag, J.D.; Gould, M.N.; Stewart, R.M.; Kendziorski, C. Gene Expression EBSeq: An Empirical Bayes Hierarchical Model for Inference in RNA-Seq Experiments. Bioinformatics 2013, 29, 1035–1043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuleshov, M.V.; Jones, M.R.; Rouillard, A.D.; Fernandez, N.F.; Duan, Q.; Wang, Z.; Koplev, S.; Jenkins, S.L.; Jagodnik, K.M.; Lachmann, A.; et al. Enrichr: A Comprehensive Gene Set Enrichment Analysis Web Server 2016 Update. Nucleic Acids Res. 2016, 44, W90–W97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanehisa, M.; Goto, S. KEGG: Kyoto Encyclopedia of Genes and Genomes. Nucleic Acids Res. 2000, 28, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Gagliardi, S.; Zucca, S.; Pandini, C.; Diamanti, L.; Bordoni, M.; Sproviero, D.; Arigoni, M.; Olivero, M.; Pansarasa, O.; Ceroni, M.; et al. Long Non-Coding and Coding RNAs Characterization in Peripheral Blood Mononuclear Cells and Spinal Cord from Amyotrophic Lateral Sclerosis Patients. Sci. Rep. 2018, 8, 2378. [Google Scholar] [CrossRef] [PubMed]
- Hong, G.; Zhang, W.; Li, H.; Shen, X.; Guo, Z. Separate Enrichment Analysis of Pathways for Up- and Downregulated Genes. J. R. Soc. Interface 2014, 11, 20130950. [Google Scholar] [CrossRef] [Green Version]
- Guo, T.; Hou, D.; Yu, D. Bioinformatics Analysis of Gene Expression Profile Data to Screen Key Genes Involved in Intracranial Aneurysms. Mol. Med. Rep. 2019, 20, 4415–4424. [Google Scholar] [CrossRef] [Green Version]
- Corder, E.H.; Saunders, A.M.; Strittmatter, W.J.; Schmechel, D.E.; Gaskell, P.C.; Small, G.W.; Roses, A.D.; Haines, J.L.; Pericak-Vance, M.A. Gene Dose of Apolipoprotein E Type 4 Allele and the Risk of Alzheimer’s Disease in Late Onset Families. Science 1993, 261, 921–923. [Google Scholar] [CrossRef]
- Neu, S.C.; Pa, J.; Kukull, W.; Beekly, D.; Kuzma, A.; Gangadharan, P.; Wang, L.S.; Romero, K.; Arneric, S.P.; Redolfi, A.; et al. Apolipoprotein E Genotype and Sex Risk Factors for Alzheimer Disease: A Meta-Analysis. JAMA Neurol. 2017, 74, 1178–1189. [Google Scholar] [CrossRef]
- Chai, A.B.; Lam, H.H.J.; Kockx, M.; Gelissen, I.C. Apolipoprotein E Isoform-Dependent Effects on the Processing of Alzheimer’s Amyloid-β. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2021, 1866, 158980. [Google Scholar] [CrossRef]
- de Luca, V.; Spalletta, G.; Souza, R.P.; Graff, A.; Bastos-Rodrigues, L.; Camargos Bicalho, M.A. Definition of Late Onset Alzheimer’s Disease and Anticipation Effect of Genome-Wide Significant Risk Variants: Pilot Study of the APOE E4 Allele. Neuropsychobiology 2019, 77, 8–12. [Google Scholar] [CrossRef]
- Giannini, G.; Conti, A.; Mammarella, S.; Scrobogna, M.; Sorrentino, V. The Ryanodine Receptor/Calcium Channel Genes Are Widely and Differentially Expressed in Murine Brain and Peripheral Tissues. J. Cell Biol. 1995, 128, 893–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanner, J.T.; Georgiou, D.K.; Joshi, A.D.; Hamilton, S.L. Ryanodine Receptors: Structure, Expression, Molecular Details, and Function in Calcium Release. Cold Spring Harb. Perspect. Biol. 2010, 2, a003996. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bussiere, R.; Lacampagne, A.; Reiken, S.; Liu, X.; Scheuerman, V.; Zalk, R.; Martin, C.; Checler, F.; Marks, A.R.; Chami, M. Amyloid β Production Is Regulated by Β2-Adrenergic Signaling-Mediated Post-Translational Modifications of the Ryanodine Receptor. J. Biol. Chem. 2017, 292, 10153–10168. [Google Scholar] [CrossRef] [Green Version]
- Lacampagne, A.; Liu, X.; Reiken, S.; Bussiere, R.; Meli, A.C.; Lauritzen, I.; Teich, A.F.; Zalk, R.; Saint, N.; Arancio, O.; et al. Post-Translational Remodeling of Ryanodine Receptor Induces Calcium Leak Leading to Alzheimer’s Disease-like Pathologies and Cognitive Deficits. Acta Neuropathol. 2017, 134, 749–767. [Google Scholar] [CrossRef]
- Emptage, N.J.; Reid, C.A.; Fine, A. Calcium Stores in Hippocampal Synaptic Boutons Mediate Short-Term Plasticity, Store-Operated Ca2+ Entry, and Spontaneous Transmitter Release. Neuron 2001, 29, 197–208. [Google Scholar] [CrossRef] [Green Version]
- Yao, J.; Liu, Y.; Sun, B.; Zhan, X.; Estillore, J.P.; Turner, R.W.; Chen, S.R.W. Increased RyR2 Open Probability Induces Neuronal Hyperactivity and Memory Loss with or without Alzheimer’s Disease-Causing Gene Mutations. Alzheimer’s Dement 2022, in press. [Google Scholar] [CrossRef]
- Liu, Y.; Yao, J.; Song, Z.; Guo, W.; Sun, B.; Wei, J.; Estillore, J.P.; Back, T.G.; Chen, S.R.W. Limiting RyR2 Open Time Prevents Alzheimer’s Disease-Related Deficits in the 3xTG-AD Mouse Model. J. Neurosci. Res. 2021, 99, 2906–2921. [Google Scholar] [CrossRef] [PubMed]
- Serratos, I.N.; Hernández-Pérez, E.; Campos, C.; Aschner, M.; Santamaría, A. An Update on the Critical Role of α-Synuclein in Parkinson’s Disease and Other Synucleinopathies: From Tissue to Cellular and Molecular Levels. Mol. Neurobiol. 2021, 2021, 620–642. [Google Scholar] [CrossRef]
- Opattova, A.; Cente, M.; Novak, M.; Filipcik, P. The Ubiquitin Proteasome System as a Potential Therapeutic Target for Treatment of Neurodegenerative Diseases. Gen. Physiol. Biophys 2015, 34, 337–352. [Google Scholar] [CrossRef]
- Oliveira, S.A.; Li, Y.J.; Noureddine, M.A.; Züchner, S.; Qin, X.; Pericak-Vance, M.A.; Vance, J.M. Identification of Risk and Age-at-Onset Genes on Chromosome 1p in Parkinson Disease. Am. J. Hum. Genet. 2005, 77, 252–264. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Schrodi, S.; Rowland, C.; Tacey, K.; Catanese, J.; Grupe, A. Genetic Evidence for Ubiquitin-Specific Proteases USP24 and USP40 as Candidate Genes for Late-Onset Parkinson Disease. Hum. Mutat. 2006, 27, 1017–1023. [Google Scholar] [CrossRef]
- Esposito, G.; Ana Clara, F.; Verstreken, P. Synaptic Vesicle Trafficking and Parkinson’s Disease. Dev. Neurobiol. 2012, 72, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Dong, B.H.; Niu, Z.Q.; Zhang, J.T.; Zhou, Y.J.; Meng, F.M.; Dong, A.Q. Complementary Transcriptomic and Proteomic Analysis in the Substantia Nigra of Parkinson’s Disease. Dis. Markers 2021, 2021, 2148820. [Google Scholar] [CrossRef] [PubMed]
- Kurvits, L.; Lättekivi, F.; Reimann, E.; Kadastik-Eerme, L.; Kasterpalu, K.M.; Kõks, S.; Taba, P.; Planken, A. Transcriptomic Profiles in Parkinson’s Disease. Exp. Biol. Med. 2021, 246, 584–595. [Google Scholar] [CrossRef] [PubMed]
- Ossenkoppele, R.; Zwan, M.D.; Tolboom, N.; van Assema, D.M.E.; Adriaanse, S.F.; Kloet, R.W.; Boellaard, R.; Windhorst, A.D.; Barkhof, F.; Lammertsma, A.A.; et al. Amyloid Burden and Metabolic Function in Early-Onset Alzheimer’s Disease: Parietal Lobe Involvement. Brain 2012, 135, 2115–2125. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, H.I.L.; van Boxtel, M.P.J.; Jolles, J.; Verhey, F.R.J.; Uylings, H.B.M. Parietal Cortex Matters in Alzheimer’s Disease: An Overview of Structural, Functional and Metabolic Findings. Neurosci. Biobehav. Rev. 2012, 36, 297–309. [Google Scholar] [CrossRef]
- Bruner, E.; Jacobs, H.I.L. Alzheimer’s Disease: The Downside of a Highly Evolved Parietal Lobe? J. Alzheimer’s Dis. 2013, 35, 227–240. [Google Scholar] [CrossRef]
- Marquer, C.; Devauges, V.; Cossec, J.C.; Liot, G.; Lécart, S.; Saudou, F.; Duyckaerts, C.; Lévêque-Fort, S.; Potier, M.C. Local Cholesterol Increase Triggers Amyloid Precursor Protein-Bace1 Clustering in Lipid Rafts and Rapid Endocytosis. FASEB J. 2011, 25, 1295–1305. [Google Scholar] [CrossRef]
- Mills, J.D.; Nalpathamkalam, T.; Jacobs, H.I.L.; Janitz, C.; Merico, D.; Hu, P.; Janitz, M. RNA-Seq Analysis of the Parietal Cortex in Alzheimer’s Disease Reveals Alternatively Spliced Isoforms Related to Lipid Metabolism. Neurosci. Lett. 2013, 536, 90–95. [Google Scholar] [CrossRef]
- Wollmer, M.A. Cholesterol-Related Genes in Alzheimer’s Disease. Biochim. Biophys. Acta 2010, 1801, 762–773. [Google Scholar] [CrossRef]
- Heneka, M.T.; Carson, M.J.; el Khoury, J.; Landreth, G.E.; Brosseron, F.; Feinstein, D.L.; Jacobs, A.H.; Wyss-Coray, T.; Vitorica, J.; Ransohoff, R.M.; et al. Neuroinflammation in Alzheimer’s Disease. Lancet Neurol. 2015, 14, 388–405. [Google Scholar] [CrossRef] [Green Version]
- Hoozemans, J.J.M.; Veerhuis, R.; Rozemuller, J.M.; Eikelenboom, P. Neuroinflammation and Regeneration in the Early Stages of Alzheimer’s Disease Pathology. Int. J. Dev. Neurosci. 2006, 24, 157–165. [Google Scholar] [CrossRef] [PubMed]






| Gene | HGSV (Coding) | HGSV (Protein) | In Silico Prediction (SIFT; Polyphen2) | ACMG Classification | |
|---|---|---|---|---|---|
| Variants in common | RYR2 | c.12948_12950dupAAG | p.Gly4316_Ser4317insArg | NA; NA | LP |
| HTT | c.1403-4T>A | p.?? | NA; NA | VUS | |
| CTNNA3 | c.1133G>T | p.Arg378Leu | D; D | VUS | |
| CNTN6 | c.1585A>C | p.Ile529Leu | T; T | LB | |
| SYNPO | c.2507C>A | p.Thr836Asn | NA; T | LB | |
| KCNT1 | c.522G>A | p.Met174Ile | T; T | B | |
| HOMER2 | c.181A>G | p.Ile61Val | T; T | B | |
| Variants not in common (son-specific) | USP24 | c.2926G>A | p.Glu976Lys | T; T | LP |
| OBSCN | c.184G>C | p.Gly62Arg | D; D | VUS | |
| MTPAP | c.-33A>G | p.?? | NA; NA | VUS | |
| GALC | c.328 + 6A>G | p.?? | NA; NA | VUS | |
| DAPK1 | c.3287G>A | p.Ser1096Asn | T; T | LB | |
| HDAC4 | c.2990T>C | p.Leu997Pro | T; T | LB |
| n° DEGs Upregulated * | n° DEGs Downregulated ** | Total n° of DEGs | ||
|---|---|---|---|---|
| Substantia Nigra | mother | 181 | 116 | 297 |
| son | 1567 | 1166 | 2733 | |
| Parietal Lobe | mother | 156 | 195 | 351 |
| son | 68 | 100 | 168 | |
| Hippocampus | mother | 41 | 10 | 51 |
| son | 5 | 1 | 6 | |
| Basal Ganglia | mother | 103 | 159 | 262 |
| son | 109 | 101 | 210 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palmieri, I.; Poloni, T.E.; Medici, V.; Zucca, S.; Davin, A.; Pansarasa, O.; Ceroni, M.; Tronconi, L.; Guaita, A.; Gagliardi, S.; et al. Differential Neuropathology, Genetics, and Transcriptomics in Two Kindred Cases with Alzheimer’s Disease and Lewy Body Dementia. Biomedicines 2022, 10, 1687. https://doi.org/10.3390/biomedicines10071687
Palmieri I, Poloni TE, Medici V, Zucca S, Davin A, Pansarasa O, Ceroni M, Tronconi L, Guaita A, Gagliardi S, et al. Differential Neuropathology, Genetics, and Transcriptomics in Two Kindred Cases with Alzheimer’s Disease and Lewy Body Dementia. Biomedicines. 2022; 10(7):1687. https://doi.org/10.3390/biomedicines10071687
Chicago/Turabian StylePalmieri, Ilaria, Tino Emanuele Poloni, Valentina Medici, Susanna Zucca, Annalisa Davin, Orietta Pansarasa, Mauro Ceroni, Livio Tronconi, Antonio Guaita, Stella Gagliardi, and et al. 2022. "Differential Neuropathology, Genetics, and Transcriptomics in Two Kindred Cases with Alzheimer’s Disease and Lewy Body Dementia" Biomedicines 10, no. 7: 1687. https://doi.org/10.3390/biomedicines10071687