Human Copper-Containing Amine Oxidases in Drug Design and Development
Abstract
:1. Introduction
2. Catalytic Mechanism of Copper Amine Oxidases
3. Medical Relevance of Targeting hVAP-1
3.1. Basis for Clinical Targeting of VAP-1
3.2. Clinical Trials
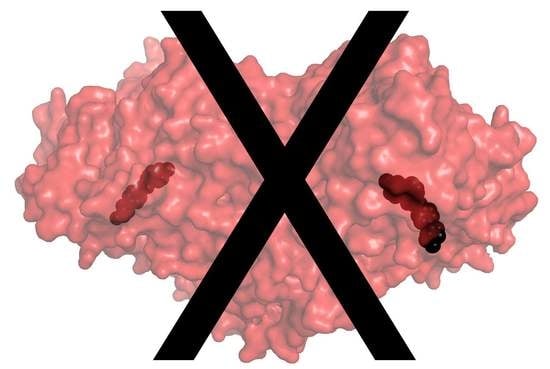
4. Structural Biology and Computer-Aided Drug Design in hVAP-1-Targeted Inhibitor Design
4.1. X-Ray Structures of hVAP-1 Complexes for Docking Studies and Inspiration for Drug Design
4.1.1. Irreversible Complex of 2HP with hVAP-1
4.1.2. Diverse Binding Modes Between Imidazole and hVAP-1
4.2. Mechanism-Based Inhibitors
4.2.1. Hydrazines
4.2.2. Thiazoles
4.2.3. Indanols
4.2.4. H-Imidazol-2-Amines
4.2.5. Allylamines
4.2.6. Glycine Amides
4.3. Reversible Inhibitors
4.3.1. Pyridazinones
4.3.2. Phenyl-Piperidinyl Amine
5. hDAO as an Off-Target
5.1. Biological Function
5.2. Off-Target Function
5.3. Unintended Drug–hDAO Interactions at the Atomic Level
6. Special Considerations in hVAP-1-Targeted Drug Design
6.1. Species-Specific Features in VAP-1 Ligand Recognition
6.2. The Risk for Interaction with Other CAO Sub-Family Members
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| 2HP | 2-hydrazinopyridine; |
| ADRs | adverse drug reactions; |
| AOC1 | hDAO human diamine oxidase; |
| AOC2 | hRAO retina-specific amine oxidase; |
| AOC3 | hVAP-1 vascular adhesion protein-1; |
| CAO | copper-containing amine oxidase; |
| DAO | diamine oxidase; |
| HTS | high-throughput screening; |
| MAO | monoamine oxidase; |
| mVAP-1 | murine ortholog of vascular adhesion protein-1; |
| PDB | Protein Data Bank; |
| PET | positron emission tomography; |
| rVAP-1 | rat ortholog of vascular adhesion protein-1; |
| TPQ | topaquinone. |
References
- Lopes de Carvalho, L.; Bligt-Lindén, E.; Ramaiah, A.; Johnson, M.S.; Salminen, T.A. Evolution and functional classification of mammalian copper amine oxidases. Mol. Phylogenet. Evol. 2019, 139, 106571. [Google Scholar] [CrossRef] [PubMed]
- Schwelberger, H. Diamine oxidase (DAO) enzyme and gene. In Histamine: Biology and Medical Aspects; Falus, A., Ed.; SpringMed Publishing: Budapest, Hungary, 2004; pp. 43–52. [Google Scholar]
- Kaitaniemi, S.; Elovaara, H.; Grön, K.; Kidron, H.; Liukkonen, J.; Salminen, T.; Salmi, M.; Jalkanen, S.; Elima, K. The unique substrate specificity of human AOC2, a semicarbazide-sensitive amine oxidase. Cell. Mol. Life Sci. 2009, 66, 2743–2757. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.; Salmi, M.; Bono, P.; Hellman, J.; Leu, T.; Jalkanen, S. Cloning of vascular adhesion protein 1 reveals a novel multifunctional adhesion molecule. J. Exp. Med. 1998, 188, 17–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dawkes, H.; Phillips, S. Copper amine oxidase: Cunning cofactor and controversial copper. Curr. Opin. Struct. Biol. 2001, 11, 666–673. [Google Scholar] [CrossRef]
- Nymalm, Y.; Kidron, H.; Söderholm, A.; Viitanen, L.; Kaukonen, K.; Pihlavisto, M.; Smith, D.; Veromaa, T.; Airenne, T.; Johnson, M.; et al. Crystallization and preliminary X-ray analysis of the human vascular adhesion protein-1. Acta Cryst. D Biol. Cryst. 2003, 59, 1288–1290. [Google Scholar] [CrossRef]
- Jakobsson, E.; Nilsson, J.; Ogg, D.; Kleywegt, G.J. Structure of human semicarbazide-sensitive amine oxidase/vascular adhesion protein-1. Acta Cryst. Sect. D Biol. Cryst. 2005, 61, 1550–1562. [Google Scholar] [CrossRef]
- Airenne, T.T.; Nymalm, Y.; Kidron, H.; Smith, D.J.; Pihlavisto, M.; Salmi, M.; Jalkanen, S.; Johnson, M.S.; Salminen, T.A. Crystal structure of the human vascular adhesion protein-1: Unique structural features with functional implications. Protein Sci. 2005, 14, 1964–1974. [Google Scholar] [CrossRef]
- Elovaara, H.; Kidron, H.; Parkash, V.; Nymalm, Y.; Bligt, E.; Ollikka, P.; Smith, D.J.; Pihlavisto, M.; Salmi, M.; Jalkanen, S.; et al. Identification of two imidazole binding sites and key residues for substrate specificity in human primary amine oxidase AOC3. Biochemistry 2011, 50, 5507–5520. [Google Scholar] [CrossRef]
- Bligt-Lindén, E.; Pihlavisto, M.; Szatmári, I.; Otwinowski, Z.; Smith, D.J.; Lázár, L.; Fülöp, F.; Salminen, T.A. Novel pyridazinone inhibitors for vascular adhesion protein-1 (VAP-1): Old target-new inhibition mode. J. Med. Chem. 2013, 56, 9837–9848. [Google Scholar] [CrossRef] [Green Version]
- McGrath, A.P.; Hilmer, K.M.; Collyer, C.A.; Shepard, E.M.; Elmore, B.O.; Brown, D.E.; Dooley, D.M.; Guss, J.M. Structure and inhibition of human diamine oxidase. Biochemistry 2009, 48, 9810–9822. [Google Scholar] [CrossRef] [Green Version]
- McGrath, A.; Caradoc-Davies, T.; Collyer, C.; Guss, J. Correlation of active site metal content in human diamine oxidase with trihydroxyphenylalanine quinone cofactor biogenesis. Biochemistry 2010, 49, 8316–8324. [Google Scholar] [CrossRef] [PubMed]
- McGrath, A.P.; Hilmer, K.M.; Collyer, C.A.; Dooley, D.M.; Guss, J.M. A new crystal form of human diamine oxidase. Acta Cryst. Sect. F Struct. Biol. Cryst. Commun. 2010, 66, 137–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salmi, M.; Jalkanen, S. Homing-associated molecules CD73 and VAP-1 as targets to prevent harmful inflammations and cancer spread. Febs Lett. 2011, 585, 1543–1550. [Google Scholar] [CrossRef] [PubMed]
- Salmi, M.; Jalkanen, S. Ectoenzymes controlling leukocyte traffic. Eur. J. Immunol. 2012, 42, 284–292. [Google Scholar] [CrossRef]
- Salmi, M.; Jalkanen, S. Ectoenzymes in leukocyte migration and their therapeutic potential. Semin. Immunopathol. 2014, 36, 163–176. [Google Scholar] [CrossRef]
- Salmi, M.; Jalkanen, S. Vascular adhesion protein-1: A cell surface amine oxidase in translation. Antioxid. Redox Signal. 2019, 30, 314–332. [Google Scholar] [CrossRef]
- Aalto, K.; Autio, A.; Kiss, E.A.; Elima, K.; Nymalm, Y.; Veres, T.Z.; Marttila-Ichihara, F.; Elovaara, H.; Saanijoki, T.; Crocker, P.R.; et al. Siglec-9 is a novel leukocyte ligand for vascular adhesion protein-1 and can be used in PET imaging of inflammation and cancer. Blood 2011, 118, 3725–3733. [Google Scholar] [CrossRef]
- Elovaara, H.; Parkash, V.; Fair-Mäkelä, R.; Salo-Ahen, O.M.H.; Guédez, G.; Bligt-Lindén, E.; Grönholm, J.; Jalkanen, S.; Salminen, T.A. Multivalent interactions of human primary amine oxidase with the v and C22 domains of sialic acid-binding immunoglobulin-like lectin-9 regulate its binding and amine oxidase activity. PLoS ONE 2016, 11, e0166935. [Google Scholar] [CrossRef] [Green Version]
- Koskinen, K.; Vainio, P.J.; Smith, D.J.; Pihlavisto, M.; Ylä-Herttuala, S.; Jalkanen, S.; Salmi, M. Granulocyte transmigration through the endothelium is regulated by the oxidase activity of vascular adhesion protein-1 (VAP-1). Blood 2004, 103, 3388–3395. [Google Scholar] [CrossRef] [Green Version]
- Merinen, M.; Irjala, H.; Salmi, M.; Jaakkola, I.; Hanninen, A.; Jalkanen, S. Vascular adhesion protein- 1 is involved in both acute and chronic inflammation in the mouse. Am. J. Pathol. 2005, 166, 793–800. [Google Scholar] [CrossRef] [Green Version]
- O’Rourke, A.; Wang, E.; Miller, A.; Podar, E.M.; Scheyhing, K.; Huang, L.; Kessler, C.; Gao, H.; Ton-Nu, H.-T.; Jones, S.D.; et al. Antiinflammatory effects of LJP 1586 [Z-3-fluoro-2-(4-methoxybenzyl)allylamine hydrochloride], an amine-based inhibitor of semicarbazide-sensitive amine oxidase activity. J. Pharm. Exp. 2008, 324, 867–875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noonan, T.; Lukas, S.; Peet, G.; Pelletier, J.; Panzenbeck, M.; Hanidu, A.; Mazurek, S.; Wasti, R.; Rybina, I.; Roma, T.; et al. The oxidase activity of vascular adhesion protein-1 (VAP-1) is essential for function. Am. J. Clin. Exp. Immunol. 2013, 2, 172–185. [Google Scholar] [PubMed]
- Jones, B.; Kearns, G. Histamine: New thoughts about a familiar mediator. Clin. Pharm. 2011, 89, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Elmore, B.; Bollinger, J.; Dooley, D. Human kidney diamine oxidase:heterologous expression, purification, and characterization. J. Biol. Inorg. Chem. 2002, 7, 565–579. [Google Scholar] [CrossRef] [PubMed]
- Maintz, L.; Novak, N. Histamine and histamine intolerance. Am. J. Clin. Nutr. 2007, 85, 1185–1196. [Google Scholar] [CrossRef] [PubMed]
- Sattler, J.; Häfner, D.; Klotter, H.; Lorenz, W.; Wagner, P. Food-induced histaminosis as an epidemiological problem: Plasma histamine elevation and haemodynamic alterations after oral histamine administration and blockade of diamine oxidase (DAO). Agents Actions 1988, 23, 361–365. [Google Scholar] [CrossRef]
- Maintz, L.; Schwarzer, V.; Bieber, T.; Van der Ven, K.; Novak, N. Effects of histamine and diamine oxidase activities on pregnancy: A critical review. Hum. Reprod. Update 2008, 14, 485–495. [Google Scholar] [CrossRef] [Green Version]
- Heuts, D.P.H.M.; Gummadova, J.O.; Pang, J.; Rigby, S.E.J.; Scrutton, N.S. Reaction of Vascular Adhesion Protein-1 (VAP-1) with primary amines: Mechanistic insights from isotope effects and quantitative structure-activity relationships. J. Biol. Chem. 2011, 286, 29584–29593. [Google Scholar] [CrossRef] [Green Version]
- Klinman, J.P. The multi-functional topa-quinone copper amine oxidases. Biochim. Biophys. Acta 2003, 1647, 131–137. [Google Scholar] [CrossRef]
- Shepard, E.M.; Dooley, D.M. Inhibition and oxygen activation in copper amine oxidases. Acc. Chem. Res. 2015, 48, 1218–1226. [Google Scholar] [CrossRef]
- Pannecoeck, R.; Serruys, D.; Benmeridja, L.; Delanghe, J.R.; Van Geel, N.; Speeckaert, R.; Speeckaert, M.M. Vascular adhesion protein-1: Role in human pathology and application as a biomarker. Crit. Rev. Clin. Lab. Sci. 2015, 52, 284–300. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.M.; Saysell, C.G.; Wilmot, C.M.; Tambyrajah, W.S.; Jaeger, J.; Knowles, P.; Phillips, S.E. The active site base controls cofactor reactivity in Escherichia coli amine oxidase: X-ray crystallographic studies with mutational variants. Biochemistry 1999, 38, 8217–8227. [Google Scholar] [CrossRef] [PubMed]
- Green, E.L.; Nakamura, N.; Dooley, D.M.; Klinman, J.P.; Sanders-Loehr, J. Rates of oxygen and hydrogen exchange as indicators of TPQ cofactor orientation in amine oxidases. Biochemistry 2002, 41, 687–696. [Google Scholar] [CrossRef] [PubMed]
- Dooley, D.M.; McGuirl, M.A.; Brown, D.E.; Turowski, P.N.; McIntire, W.S.; Knowles, P.F. A Cu(I)-semiquinone state in substrate-reduced amine oxidases. Nature 1991, 349, 262–264. [Google Scholar] [CrossRef] [PubMed]
- Mure, M.; Mills, S.A.; Klinman, J.P. Catalytic mechanism of the topa quinone containing copper amine oxidases. Biochemistry 2002, 41, 9269–9278. [Google Scholar] [CrossRef]
- Shepard, E.M.; Okonski, K.M.; Dooley, D.M. Kinetics and spectroscopic evidence that the Cu(I)-semiquinone intermediate reduces molecular oxygen in the oxidative half-reaction of Arthrobacter globiformis amine oxidase. Biochemistry 2008, 47, 13907–13920. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Mukherjee, A.; Nahumi, N.; Ozbil, M.; Brown, D.; Angeles-Boza, A.M.; Dooley, D.M.; Prabhakar, R.; Roth, J.P. Experimental and computational evidence of metal-O2 activation and rate-limiting proton-coupled electron transfer in a copper amine oxidase. J. Phys. Chem. B 2013, 117, 218–229. [Google Scholar] [CrossRef]
- Roth, J.P.; Klinman, J.P. Catalysis of electron transfer during activation of O2 by the flavoprotein glucose oxidase. Proc. Natl. Acad. Sci. USA 2003, 100, 62–67. [Google Scholar] [CrossRef] [Green Version]
- Kivi, E.; Elima, K.; Aalto, K.; Nymalm, Y.; Auvinen, K.; Koivunen, E.; Otto, D.M.; Crocker, P.R.; Salminen, T.A.; Salmi, M.; et al. Human Siglec-10 can bind to vascular adhesion protein-1 and serves as its substrate. Blood 2009, 114, 5385–5392. [Google Scholar] [CrossRef]
- Virtanen, H.; Autio, A.; Siitonen, R.; Liljenbäck, H.; Saanijoki, T.; Lankinen, P.; Mäkilä, J.; Käkelä, M.; Teuho, J.; Savisto, N.; et al. 68Ga-DOTA-Siglec-9—A new imaging tool to detect synovitis. Arthritis Res. 2015, 17, 305. [Google Scholar] [CrossRef] [Green Version]
- Roivainen, A. Identifier NCT03755245. Biodistribution, Dosimetry and Performance of [68Ga]Ga-DOTA-Siglec-9 in Healthy and Patients With Rheumatoid Arthritis (SIGLEC). Available online: https://clinicaltrials.gov/ct2/show/NCT03755245?term=VAP-1&cntry=FI&draw=2 (accessed on 20 January 2020).
- Arndtz, K.; Corrigan, M.; Rowe, A.; Kirkham, A.; Barton, D.; Fox, R.; Llewellyn, L.; Athwal, A.; Wilkhu, M.; Chen, Y.; et al. Investigating the safety and activity of the use of BTT1023 (Timolumab), in the treatment of patients with primary sclerosing cholangitis (BUTEO): A single-arm, two-stage, open-label, multi-centre, phase II clinical trial protocol. BMJ Open 2016. [Google Scholar] [CrossRef] [PubMed]
- De Zeeuw, D.; Renfurm, R.W.; Bakris, G.; Rossing, P.; Perkovic, V.; Hou, F.F.; Nangaku, M.; Sharma, K.; Heerspink, H.J.L.; Garcia-Hernandez, A.; et al. Efficacy of a novel inhibitor of vascular adhesion protein-1 in reducing albuminuria in patients with diabetic kidney disease (ALBUM): A randomised, placebo-controlled, phase 2 trial. Lancet Diabetes Endocrinol. 2018, 6, 925–933. [Google Scholar] [CrossRef]
- Nguyen, Q.D.; Sepah, Y.J.; Berger, B.; Brown, D.; Do, D.V.; Garcia-Hernandez, A.; Patel, S.; Rahhal, F.M.; Shildkrot, Y.; Renfurm, R.W. Primary outcomes of the VIDI study: Phase 2, double-masked, randomized, active-controlled study of ASP8232 for diabetic macular edema. Int. J. Retin. Vitr. 2019, 5, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pharmaxis Ltd. Boehringer Ingelheim Discontinues Development of BI 1467335 for NASH. Available online: https://www.boehringer-ingelheim.us/press-release/boehringer-ingelheim-discontinues-development-bi-1467335-nash (accessed on 20 January 2020).
- Aeddula, N.; Pathireddy, S.; Ansari, A.; Juran, P. Hydralazine-associated antineutrophil cytoplasmic antibody vasculitis with pulmonary-renal syndrome. BMJ Case Rep. 2018. [Google Scholar] [CrossRef] [Green Version]
- Novartis Products on NDA 008303. Available online: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=008303 (accessed on 20 January 2020).
- Énzsöly, A.; Markó, K.; Tábi, T.; Szökő, É.; Zelkó, R.; Tóth, M.; Petrash, J.; Mátyus, P.; Németh, J. Lack of association between VAP-1/SSAO activity and corneal neovascularization in a rabbit model. J. Neural Transm. 2013, 120, 969–975. [Google Scholar] [CrossRef] [Green Version]
- Yang, W.; Li, H.; Luo, H.; Luo, W. Inhibition of semicarbazide-sensitive amine oxidase attenuates myocardial ischemia-reperfusion injury in an in vivo rat model. Life Sci. 2011, 88, 302–306. [Google Scholar] [CrossRef]
- Wang, E.Y.; Gao, H.; Salter-Cid, L.; Zhang, J.; Huang, L.; Podar, E.M.; Miller, A.; Zhao, J.; O’Rourke, A.; Linnik, M.D. Design, synthesis, and biological evaluation of semicarbazide-sensitive amine oxidase (SSAO) inhibitors with anti-inflammatory activity. J. Med. Chem. 2006, 49, 2166–2173. [Google Scholar] [CrossRef]
- O’Rourke, A.; Wang, E.; Salter-Cid, L.; Huang, L.; Miller, A.; Podar, E.; Gao, H.; Jones, D.; Linnik, M. Benefit of inhibiting SSAO in relapsing experimental autoimmune encephalomyelitis. J. Neural Transm. 2007, 114, 845–849. [Google Scholar] [CrossRef]
- Salter-Cid, L.; Wang, E.; O’Rourke, A.; Miller, A.; Gao, H.; Huang, L.; Garcia, A.; Linnik, M. Anti-inflammatory effects of inhibiting the amine oxidase activity of semicarbazide-sensitive amine oxidase. J. Pharm. Exp. 2005, 315, 553–562. [Google Scholar] [CrossRef] [Green Version]
- Foot, J.S.; Deodhar, M.; Turner, C.I.; Yin, P.; Van Dam, E.M.; Silva, D.G.; Olivieri, A.; Holt, A.; McDonald, I.A. The discovery and development of selective 3-fluoro-4-aryloxyallylamine inhibitors of the amine oxidase activity of semicarbazide-sensitive amine oxidase/vascular adhesion protein-1 (SSAO/VAP-1). Bioorg. Med. Chem. Lett. 2012, 22, 3935–3940. [Google Scholar] [CrossRef]
- Schilter, H.; Collison, A.; Russo, R.; Foot, J.; Yow, T.; Vieira, A.; Tavares, L.; Mattes, J.; Teixeira, M.; Jarolimek, W. Effects of an anti-inflammatory VAP-1/SSAO inhibitor, PXS-4728A, on pulmonary neutrophil migration. Respir. Res. 2015, 16, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarnicki, A.; Schilter, H.; Liu, G.; Wheeldon, K.; Essilfie, A.; Foot, J.; Yow, T.; Jarolimek, W.; Hansbro, P. The inhibitor of semicarbazide-sensitive amine oxidase, PXS-4728A, ameliorates key features of chronic obstructive pulmonary disease in a mouse model. Br. J. Pharm. 2016, 173, 3161–3175. [Google Scholar] [CrossRef] [PubMed]
- Katagiri, D.; Hamasaki, Y.; Doi, K.; Negishi, K.; Sugaya, T.; Nangaku, M.; Noiri, E. Interstitial renal fibrosis due to multiple cisplatin treatments is ameliorated by semicarbazide-sensitive amine oxidase inhibition. Kidney Int. 2016, 89, 374–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foot, J.S.; Yow, T.T.; Schilter, H.; Buson, A.; Deodhar, M.; Findlay, A.D.; Guo, L.; McDonald, I.A.; Turner, C.I.; Zhou, W.; et al. PXS-4681A, a potent and selective mechanism-based inhibitor of SSAO/VAP-1 with anti-inflammatory effects in vivo. J. Pharm. Exp. 2013, 347, 365–374. [Google Scholar] [CrossRef] [Green Version]
- Becchi, S.; Buson, A.; Foot, J.; Jarolimek, W.; Balleine, B.W. Inhibition of semicarbazide-sensitive amine oxidase/vascular adhesion protein-1 reduces lipopolysaccharide-induced neuroinflammation. Br. J. Pharm. 2017, 174, 2302–2317. [Google Scholar] [CrossRef] [Green Version]
- Elo, P.; Tadayon, S.; Liljenbäck, H.; Teuho, J.; Käkelä, M.; Koskensalo, K.; Saunavaara, V.; Virta, J.; Veres, T.; Kiviniemi, A.; et al. Vascular adhesion protein-1 is actively involved in the development of inflammatory lesions in rat models of multiple sclerosis. J. Neuroinflamm. 2018, 15, 128. [Google Scholar] [CrossRef]
- Ma, Q.; Manaenko, A.; Khatibi, N.; Chen, W.; Zhang, J.; Tang, J. Vascular adhesion protein-1 inhibition provides antiinflammatory protection after an intracerebral hemorrhagic stroke in mice. J. Cereb. Blood Flow Metab. 2011, 31, 881–893. [Google Scholar] [CrossRef] [Green Version]
- Silvola, J.M.U.; Virtanen, H.; Siitonen, R.; Hellberg, S.; Liljenbäck, H.; Metsälä, O.; Ståhle, M.; Saanijoki, T.; Käkelä, M.; Hakovirta, H.; et al. Leukocyte trafficking-associated vascular adhesion protein 1 is expressed and functionally active in atherosclerotic plaques. Sci. Rep. 2016, 6, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Xu, H.; Testai, F.; Valyi-Nagy, T.; Pavuluri, M.; Zhai, F.; Nanegrungsunk, D.; Paisansathan, C.; Pelligrino, D. VAP-1 blockade prevents subarachnoid hemorrhage-associated cerebrovascular dilating dysfunction via repression of a neutrophil recruitment-related mechanism. Brain Res. 2015, 1603, 141–149. [Google Scholar] [CrossRef]
- Watcharotayangul, J.; Mao, L.; Xu, H.; Vetri, F.; Baughman, V.; Paisansathan, C.; Pelligrino, D. Post-ischemic vascular adhesion protein-1 inhibition provides neuroprotection in a rat temporary middle cerebral artery occlusion model. J. Neurochem. 2012, 123, 116–124. [Google Scholar] [CrossRef]
- Klucher, K.; Wang, Y.; Xu, Y.; Halcomb, R.; Fenaux, M. A novel semicarbazide-sensitive amine oxidase inhibitor, TERN-201, reduces NAS and fibrosis in rodent models of non-alcoholic steatohepatitis. In Proceedings of the The International Liver Congress 2019 Abstract Book, Vienna, Austria, 10–14 April 2019; pp. e534–e535. [Google Scholar]
- Horváth, Á.; Menghis, A.; Botz, B.; Borbély, É.; Kemény, Á.; Tékus, V.; Csepregi, J.; Mócsai, A.; Juhász, T.; Zákány, R.; et al. Analgesic and anti-inflammatory effects of the novel semicarbazide-sensitive amine-oxidase inhibitor SzV-1287 in chronic arthritis models of the mouse. Sci. Rep. 2017, 7, 39863. [Google Scholar] [CrossRef] [PubMed]
- Horváth, H.; Tékus, V.; Bencze, N.; Szentes, N.; Scheich, B.; Bölcskei, K.; Szoke, E.; Mócsai, A.; Tóth-Sarudy, E.; Mátyus, P.; et al. Analgesic effects of the novel semicarbazide-sensitive amine oxidase inhibitor SZV 1287 in mouse pain models with neuropathic mechanisms: Involvement of transient receptor potential vanilloid 1 and ankyrin 1 receptors. Pharm. Res. 2018, 131, 231–243. [Google Scholar] [CrossRef] [PubMed]
- Payrits, M.; Saghy, E.; Matyus, P.; Czompa, Z.; Helyes, Z.; Szoke, E. A novel 3-(4,5-diphenyl-1,3-oxazol-2-yl)propanal oxime compound is a potent Transient Receptor Potential Ankyrin 1 and Vanilloid 1 (TRPA1 and V1) receptor antagonist. Neuroscience 2016, 324, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Tabi, T.; Szoko, E.; Mérey, A.; Tóth, V.; Mátyus, P.; Gyires, K. Study on SSAO enzyme activity and anti-inflammatory effect of SSAO inhibitors in animal model of inflammation. J. Neural Transm. 2013, 120, 963–967. [Google Scholar] [CrossRef]
- Noda, K.; Miyahara, S.; Nakazawa, T.; Almulki, L.; Nakao, S.; Hisatomi, T.; She, H.; Thomas, K.; Garland, R.; Miller, J.; et al. Inhibition of vascular adhesion protein-1 suppresses endotoxin-induced uveitis. FASEB J. 2008, 22, 1094–1103. [Google Scholar] [CrossRef] [Green Version]
- Noda, K.; She, H.; Nakazawa, T.; Hisatomi, T.; Nakao, S.; Almulki, L.; Zandi, S.; Miyahara, S.; Ito, Y.; Thomas, K.L.; et al. Vascular adhesion protein-1 blockade suppresses choroidal neovascularization. FASEB J. 2008, 22, 2928–2935. [Google Scholar] [CrossRef] [Green Version]
- Noda, K.; Nakao, S.; Zandi, S.; Engelstädter, V.; Mashima, Y.; Hafezi-Moghadam, A. Vascular adhesion protein-1 regulates leukocyte transmigration rate in the retina during diabetes. Exp. Eye Res. 2009, 89, 774–781. [Google Scholar] [CrossRef] [Green Version]
- Yoshikawa, N.; Noda, K.; Ozawa, Y.; Tsubota, K.; Mashima, Y.; Ishida, S. Blockade of vascular adhesion protein-1 attenuates choroidal neovascularization. Mol. Vis. 2012, 18, 593–600. [Google Scholar]
- Marttila-Ichihara, F.; Smith, D.J.; Stolen, C.; Yegutkin, G.G.; Elima, K.; Mercier, N.; Kiviranta, R.; Pihlavisto, M.; Alaranta, S.; Pentikäinen, U.; et al. Vascular amine oxidases are needed for leukocyte extravasation into inflamed joints in vivo. Arthritis Rheum. 2006, 54, 2852–2862. [Google Scholar] [CrossRef]
- McDonald, I.; Foot, J.; Yin, P.; Fleming, E.; Van Dam, E. Semicarbazide-sensitive amine oxidase and vascular adhesion protein-1: One protein being validated as a therapeutic target for inflammatory diseases. Annu. Rep. Med. Chem. 2007, 42, 229–243. [Google Scholar]
- Dunkel, P.; Balogh, B.; Meleddu, R.; Maccioni, E.; Gyires, K.; Matyus, P. Semicarbazide-sensitive amine oxidase/vascular adhesion protein-1: A patent survey. Expert Opin. Ther. Pat. 2011, 21, 1453–1471. [Google Scholar] [CrossRef] [PubMed]
- Palfreyman, M.G.; McDonald, I.A.; Bey, P.; Danzin, C.; Zreika, M.; Cremer, G. Haloallylamine inhibitors of MAO and SSAO and their therapeutic potential. J. Neural Transm. Suppl. 1994, 41, 407–414. [Google Scholar] [PubMed]
- Nurminen, E.M.; Pihlavisto, M.; Lázár, L.; Pentikäinen, U.; Fülöp, F.; Pentikäinen, O.T. Novel hydrazine molecules as tools to understand the flexibility of vascular adhesion protein-1 ligand-binding site: Toward more selective inhibitors. J. Med. Chem. 2011, 54, 2143–2154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inoue, T.; Morita, M.; Tojo, T.; Yoshihara, K.; Nagashima, A.; Moritomo, A.; Ohkubo, M.; Miyake, H. Synthesis and SAR study of new thiazole derivatives as vascular adhesion protein-1 (VAP-1) inhibitors for the treatment of diabetic macular edema. Bioorg. Med. Chem. 2013, 21, 1219–1233. [Google Scholar] [CrossRef] [PubMed]
- Inoue, T.; Morita, M.; Tojo, T.; Nagashima, A.; Moritomo, A.; Imai, K.; Miyake, H. Synthesis and SAR study of new thiazole derivatives as vascular adhesion protein-1 (VAP-1) inhibitors for the treatment of diabetic macular edema: Part 2. Bioorg. Med. Chem. 2013, 21, 2478–2494. [Google Scholar] [CrossRef]
- Inoue, T.; Morita, M.; Tojo, T.; Nagashima, A.; Moritomo, A.; Miyake, H. Novel 1H-imidazol-2-amine derivatives as potent and orally active vascular adhesion protein-1 (VAP-1) inhibitors for diabetic macular edema treatment. Bioorg. Med. Chem. 2013, 21, 3873–3881. [Google Scholar] [CrossRef] [Green Version]
- Emanuela, B.; Minarini, A.; Tumiatti, V.; Milelli, A.; Lunelli, M.; Pegoraro, M.; Rizzoli, V.; Di Paolo, M.L. Synthetic polyamines as potential amine oxidase inhibitors: A preliminary study. Amino Acids 2012, 42, 913–928. [Google Scholar] [CrossRef]
- Yamaki, S.; Suzuki, D.; Fujiyasu, J.; Neya, M.; Nagashima, A.; Kondo, M.; Akabane, T.; Kadono, K.; Moritomo, A.; Yoshihara, K. Synthesis and structure activity relationships of glycine amide derivatives as novel Vascular Adhesion Protein-1 inhibitors. Bioorg. Med. Chem. 2017, 25, 187–201. [Google Scholar] [CrossRef]
- Yamaki, S.; Koga, Y.; Nagashima, A.; Kondo, M.; Shimada, Y.; Kadono, K.; Moritomo, A.; Yoshihara, K. Synthesis and pharmacological evaluation of glycine amide derivatives as novel vascular adhesion protein-1 inhibitors without CYP3A4 and CYP2C19 inhibition. Bioorg. Med. Chem. 2017, 25, 4110–4122. [Google Scholar] [CrossRef]
- Ernberg, K.; McGrath, A.P.; Peat, T.S.; Adams, T.E.; Xiao, X.; Pham, T.; Newman, J.; McDonald, I.A.; Collyer, C.A.; Guss, J.M. A new crystal form of human vascular adhesion protein 1. Acta Cryst. Sect. F Struct. Biol. Cryst. Commun. 2010, 66, 1572–1578. [Google Scholar] [CrossRef]
- Xu, H.; Salter-Cid, L.; Linnik, M.; Wang, E.; Paisansathan, C.; Pelligrino, D. Vascular adhesion protein-1 plays an important role in postischemic inflammation and neuropathology in diabetic, estrogen-treated ovariectomized female rats subjected to transient forebrain ischemia. J. Pharm. Exp. 2006, 317, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Li, H.; Luo, H.; Lin, Z.; Jiang, Z.; Luo, W. SSAO inhibitors suppress hepatocellular tumor growth in mice. Cell Immunol. 2013, 283, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Bligt-Lindén, E.; Arunachalam, R.; Parkash, V.; Salminen, T.A. Structural comparison of the active site channels in rodent and primate vascular adhesion protein-1. J. Neural Transm. 2013, 120, 947–950. [Google Scholar] [CrossRef]
- Best, C. The disappearance of histamine from autolysing lung tissue. J. Physiol. 1929, 67, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Bieganski, T.; Kusche, J.; Lorenz, W.; Hesterberg, R.; Stahlknecht, C.; Feussner, K. Distribution and properties of human intestinal diamine oxidase and its relevance for the histamine catabolism. Biochim. Biophys. Acta 1983, 756, 196–203. [Google Scholar] [CrossRef]
- Schwelberger, H.G. The origin of mammalian plasma amine oxidases. J. Neural Transm. 2007, 114, 757–762. [Google Scholar] [CrossRef]
- Kovacova-Hanuskova, E.; Buday, T.; Gavliakova, S.; Plevkova, J. Histamine, histamine intoxication and intolerance. Allergol. Immunopathol. (Madr.) 2015, 43, 498–506. [Google Scholar] [CrossRef]
- Schwelberger, H.G. Origins of plasma amine oxidases in different mammalian species. Inflamm. Res. 2006, 55, 57–58. [Google Scholar] [CrossRef]
- Honzawa, Y.; Nakase, H.; Matsuura, M.; Chiba, T. Clinical significance of serum diamine oxidase activity in inflammatory bowel disease: Importance of evaluation of small intestinal permeability. Inflamm. Bowel Dis. 2011, 17, E23–E25. [Google Scholar] [CrossRef]
- Rosell-Camps, A.; Zibetti, S.; Pérez-Esteban, G.; Vila-Vidal, M.; Ferrés-Ramis, L.; García-Teresa-García, E. Histamine intolerance as a cause of chronic digestive complaints in pediatric patients. Rev. Esp. Enferm. Dig. 2013, 105, 201–206. [Google Scholar] [CrossRef]
- Maintz, L.; Benfadal, S.; Allam, J.-P.; Hagemann, T.; Fimmers, R.; Novak, N. Evidence for a reduced histamine degradation capacity in a subgroup of patients with atopic eczema. J. Allergy Clin. Immunol. 2006, 117, 1106–1112. [Google Scholar] [CrossRef] [PubMed]
- Wagner, N.; Peveling-Oberhag, A.; Reese, I.; Rady-Pizarro, U.; Mitzel, H.; Staubach, P. A popular Myth—low-histamine diet improves chronic spontaneous urticaria—Fact or fiction? J. Eur. Acad. Derm. Venereol. 2016, 31, 650–655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Izquierdo-Casas, J.; Comas-Basté, O.; Latorre-Moratalla, M.; Lorente-Gascón, M.; Duelo, A.; Vidal-Carou, M.; Soler-Singla, L. Low Serum Diamine Oxidase (DAO) activity levels in patients with migraine. J. Physiol. Biochem. 2018, 74, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Anvari, S.; Vyhlidal, C.; Dai, H.; Jones, B. Genetic variation along the histamine pathway in children with allergic versus nonallergic asthma. Am. J. Respir. Cell Mol. Biol. 2015, 53, 802–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Igaz, P.; Fitzimons, C.P.; Szalai, C.; Falus, A. Histamine genomics in silico: Polymorphisms of the human genes involved in the synthesis, action and degradation of histamine. Am. J. Pharm. 2002, 2, 67–72. [Google Scholar] [CrossRef]
- Bytautiene, E.; Vedernikov, Y.P.; Saade, G.R.; Romero, R.; Garfield, R.E. Effect of histamine on phasic and tonic contractions of isolated uterine tissue from pregnant women. Am. J. Obs. Gynecol. 2003, 188, 774–778. [Google Scholar] [CrossRef]
- Dale, H.; Laidlaw, P. The physiological action of β-iminazolylethylamine. J. Physiol. 1910, 41, 318–344. [Google Scholar] [CrossRef]
- Gahl, W.; Raubertas, R.; Vale, A.; Golubjatnikov, R. Maternal serum diamine oxidase in fetal death and low-birth-weight infants. Int. J. Obs. Gynaecol. 1982, 89, 202–207. [Google Scholar] [CrossRef]
- Myatt, L.; Roberts, J. Preeclampsia: Syndrome or disease? Curr. Hypertens. Rep. 2015, 17, 83. [Google Scholar] [CrossRef]
- Velicky, P.; Windsperger, K.; Petroczi, K.; Pils, S.; Reiter, B.; Weiss, T.; Vondra, S.; Ristl, R.; Dekan, S.; Fiala, C.; et al. Pregnancy-associated diamine oxidase originates from extravillous trophoblasts and is decreased in early-onset preeclampsia. Sci. Rep. 2018, 8, 6342. [Google Scholar] [CrossRef]
- Liang, X.; Zhao, Z.; Deng, W.; Tian, Z.; Lei, W.; Xu, X.; Zhang, X.; Su, R.; Yang, Z. Estrogen regulates amiloride-binding protein 1 through CCAAT/enhancer-binding protein-β in mouse uterus during embryo implantation and decidualization. Endocrinology 2010, 151, 5007–5016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mezher, M. Regulatory Affairs Professionals Society. Available online: https://www.raps.org/regulatory-focus™/news-articles/2015/4/who-makes-drug-side-effects-easier-to-find-with-new-database (accessed on 20 January 2020).
- Chartier, M.; Morency, L.P.; Zylber, M.I.; Najmanovich, R.J. Large-scale detection of drug off-targets: Hypotheses for drug repurposing and understanding side-effects. BMC Pharm. Toxicol. 2017, 18, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sjaastad, O. Potentiation by aminoguanidine of the sensitivity of sheep to histamine given by mouth. Effect of amino-guanidine on the urinary excretion of endogenous histamine. Q. J. Exp. Physiol. Cogn. Med. Sci. 1967, 52, 319–330. [Google Scholar] [PubMed]
- EFSA Panel on Biological Hazards. 2011. Available online: https://www.efsa.europa.eu/en/panels/biohaz (accessed on 20 January 2020).
- Kusche, J.; Izbicki, J.; Mennigen, R.; Curt, A.; Parkin, J. The effect of experimental carcinogenesis on intestinal diamine oxidase, a polyamine deaminating enzyme. Cancer Detect. Prev. 1986, 9, 17–29. [Google Scholar] [PubMed]
- Sattler, J.; Lorenz, W. Intestinal diamine oxidases and enteral-induced histaminosis: Studies on three prognostic variables in an epidemiological model. J. Neural Transm. Suppl. 1990, 32, 291–314. [Google Scholar]
- Yee, S.; Lin, L.; Mersk, M.; Keiser, M.; Gupta, A.; Zhang, Y.; Chien, H.; Shoichet, B.; Giacomini, K. Prediction and validation of enzyme and transporter off-targets for metformin. J. Pharm. Pharm. 2015, 42, 463–475. [Google Scholar] [CrossRef] [Green Version]
- Brown, D.G.; Sanderson, M.R.; Garman, E.; Neidle, S. Crystal-structure of a berenil-d(CGCAAATTTGCG) complex: An example of drug DNA recognition based on sequence-dependent structural features. J. Mol. Biol. 1992, 226, 481–490. [Google Scholar] [CrossRef]
- Edwards, K.J.; Jenkins, T.C.; Neidle, S. Crystal structure of a pentamidine-oligonucleotide complex: Implications for DNA-binding properties. Biochemistry 1992, 31, 7104–7109. [Google Scholar] [CrossRef]
- Holt, A. Membrane-bound copper amine oxidases. In Copper Amine Oxidases: Structures, Catalytic Mechanisms and Role in Pathophysiology; Floris, G., Mondovi, B., Eds.; Taylor and Francis: Boca Raton, FL, USA, 2009; pp. 69–101. [Google Scholar]
- Thornalley, P.J. Use of aminoguanidine (Pimagedine) to prevent the formation of advanced glycation endproducts. Arch. Biochem. Biophys. 2003, 419, 31–40. [Google Scholar] [CrossRef]
- Abdel-Rahman, E.; Bolton, W.K. Pimagedine: A novel therapy for diabetic nephropathy. Expert Opin. Investig. Drugs. 2002, 11, 565–574. [Google Scholar]
- Freedman, B.I.; Wuerth, J.P.; Cartwright, K.; Bain, R.P.; Dippe, S.; Hershon, K.; Mooradian, A.D.; Spinowitz, B.S. Design and baseline characteristics for the aminoguanidine clinical trial in overt type 2 diabetic nephropathy (ACTION II). Control. Clin. Trials 1999, 20, 493–510. [Google Scholar] [CrossRef]
- Kubota, R.; Reid, M.J.; Lieu, K.L.; Orme, M.; Diamond, C.; Tulberg, N.; Henry, S.H. Comparison of inhibitor and substrate selectivity between rodent and human vascular adhesion protein-1. Mediat. Inflamm. 2020, 2020, 3270513. [Google Scholar] [CrossRef]
- Lyles, G.A. Mammalian plasma and tissue-bound semicarba ide-sensitive amine oxidases: Biochemical, pharmacological and toxicological aspects. Int. J. Biochem. Cell Biol. 1996, 28, 259–274. [Google Scholar] [CrossRef]
- Yu, P.H.; Zuo, D.M.; Davis, B.A. Characterization of human serum and umbilical artery semicarbazide-sensitive amine oxidase (SSAO). Species heterogeneity and stereoisomeric specificity. Biochem. Pharm. 1994, 47, 1055–1059. [Google Scholar] [CrossRef]
- Marti, L.; Abella, A.; De La Cruz, X.; García-Vicente, S.; Unzeta, M.; Carpéné, C.; Palacín, M.; Testar, X.; Orozco, M.; Zorzano, A. Exploring the binding mode of semicarbazide-sensitive amine oxidase/VAP-1: Identification of novel substrates with insulin-like activity. J. Med. Chem. 2004, 47, 4865–4874. [Google Scholar] [CrossRef] [PubMed]







| Name and Structure | Type of Inhibition | Company | Current Status | Ref. |
|---|---|---|---|---|
Hydralazine | Mechanism-based | Novartis International AG, Switzerland | FDA Approved in 15.01.1953 for the treatment of hypertension; later discontinued due to the development of newer medications. | [47,48] |
LJP1207 | Mechanism-based | La Jolla Pharmaceutical Company, USA | Discontinued; not appropriate for drug development due to its potentially toxic allylhydrazine structure | [49,50,51,52,53] |
| ASP8232 Undisclosed Structure | Unknown | R Tech Ueno Ltd., Japan; Astellas Pharma Europe BV, The Netherlands | Discontinued on Phase2 trials (NCT02302079, NCT02218099) due to strategic prioritization | [44,45] |
PXS-4159A (R10) | Mechanism-based | Pharmaxis Ltd., Australia | In preclinical toxicology evaluation | [54] |
PXS 4728A (BI 1467335) | Mechanism-based | Pharmaxis Ltd., Australia | Completed Phase II clinical trials for the treatment of non-alcoholic steatohepatitis (NCT03166735) | [55,56,57] |
PXS-4681A | Mechanism-based | Pharmaxis Ltd., Australia | Discontinued | [58,59] |
LJP1586 | Mechanism-based | La Jolla Pharmaceutical Company, USA | Discontinued | [22,60,61,62,63,64] |
| TERN-201 Undisclosed Structure | Mechanism-based | Eli Lilly and Company; Terns Pharmaceuticals | Phase I clinical trials for the treatment of non-alcoholic steatohepatitis | [65] |
| PRX167700 Undisclosed Structure | Unknown | Cambridge Biotechnology, UK; Proximagen, UK; Roche, Switzerland | Completed Phase II clinical trials for the treatment of osteoarthritis (NCT01945346) | |
SzV-1287 | Mechanism-based | Semmelweis University, Hungary | In preclinical studies; patented as a mean to treat hyperalgesia and allodynia in traumatic neuropathy or neurogenic inflammation | [66,67,68,69] |
U-V002 (R7) | Mechanism-based | R Tech Ueno Ltd., Japan; | Unknown | [70,71,72,73] |
BTT-2027 | Mechanism-based | Biotie Therapies Corp. | Discontinued | [20] |
BTT2052 | Mechanism-based | Biotie Therapies Corp. | Discontinued | [74] |
| Inhibitor | Type of Inhibitor, IC50 | Used VAP-1 Structure | Docking Tool | Ref. |
|---|---|---|---|---|
| Hydrazine Alcohols | ||||
R1: Compound 2a,b | Mechanism-based, 0.04–0.15 µM | 2C11 | GOLD 3.1.1 | [78] |
| Interacting residues: Covalent bond between hydrazine nitrogen and TPQ; H-bonds between hydrazine nitrogen and the hydroxyl group of R1 with TPQ and D386; hydrophobic interactions with Y384, F389, Y394, L468, L469. | ||||
R2: Compound 8 | Mechanism-based, 1.2 µM | 2C11 | GOLD 3.1.1 | [78] |
| Interacting residues: Covalent bond between hydrazine nitrogen and TPQ; H-bonds between nitrogen and TPQ and D386, and between the hydroxyl group and D386; hydrophobic interactions with Y384, Y394, F389. | ||||
R3: Compound 12 | Mechanism-based, 0.26 µM | 2C11 | GOLD 3.1.1 | [78] |
| Interacting residues: Covalent bond between hydrazine nitrogen and TPQ; H-bonds between the hydroxyl group and D386; hydrophobic interactions with Y384, Y394, F389. | ||||
R4: Compound 11a–d | Mechanism-based, 0.28–1.18 µM | 2C11 | GOLD 3.1.1 | [78] |
| Interacting residues: Covalent bond between hydrazine nitrogen and TPQ; 11a,b form H-bond with TPQ, while 11c,d with D386; hydrophobic interactions with A370, Y384, F389, Y394, L468, L469; 11c,d form π–π interaction with Y372 or Y384. | ||||
| Thiazoles | ||||
R5: Compound 10 | Mechanism-based, 0.23 µM | 2C11 | GOLD 5.0 | [79] |
| Interacting residues: Covalent bond between guanidine group and TPQ; H-bond between guanidine group and D386; S–O interaction of sulfur atom in the thiazole ring with T210 backbone carbonyl oxygen; proton–π interaction of amide moiety with Y176. | ||||
R6: Compound 35a | Mechanism-based, 34 nM | 2C11 | GOLD 5.0 | [80] |
| Interacting residues: Covalent bond between guanidine group and TPQ; π–proton interactions of sulfonyl moiety with L447, amide nitrogen with Y176, and guanidine nitrogen with Y384. | ||||
R7: Compound 35c | Mechanism-based, 20 nM | 2C11 | GOLD 5.0 | [80] |
| Interacting residues: Covalent bond between guanidine group and TPQ; H-bonds between sulfonyl moiety with L447 and D446, π–proton interactions of sulfonyl moiety with L447, amide nitrogen with Y176, and guanidine nitrogen with Y384. | ||||
| Indanols | ||||
BTT2052 | Mechanism-based, 0.06 µM | 1US1 | Manual docking | [74] |
| Interacting residues: Covalent bond between hydrazine nitrogen and TPQ; H-bond between the hydroxyl group and D386; hydrophobic interactions with M211, Y384, F389, L469. | ||||
| 1H-imidazol-2-amines | ||||
R8: Compound 19 | Mechanism-based, 32 µM | 2C11 | GOLD 5.1 | [81] |
| Interacting residues: Covalent bond between the amine group and TPQ; H-bond between NH of the imidazole ring with N470; π–π interaction between imidazole ring and Y384; π–proton interaction of benzene ring with L469. | ||||
R9: Compound 37b | Mechanism-based, 19 nM | 2C11 | GOLD 5.1 | [81] |
| Interacting residues: Covalent bond between the amine group and TPQ; π–proton interactions of thiazole group with T212 and L447; S-O interaction of thiazole sulfur with T210 backbone carbonyl oxygen; proton–π interaction between amide moiety and Y176; CH–O interaction of acetyl moiety and D180. | ||||
| Allylamines | ||||
R10: Compound 28 | Mechanism-based, 10 nM | ? | MOE 2011.10 | [54] |
| Interacting residues: Covalent bond between the amine group and TPQ; Hydrophobic interactions with F173 and Y394. | ||||
| Phenyl-piperidinyl amine | ||||
R11: ELP12 | Reversible, Ki(EI)111 µM/Ki(ESI) = 163 µM | 2C10 | AutoDock 4.2 | [82] |
| Interacting residues: Salt bridges between amino groups of R11 with the carboxylates of D180 and D446 and H-bonds with the side-chain of Y448 and with the backbone carbonyl of T424; an aromatic ring is stacked to the ring of Y176; hydrophobic interactions with F173, Y394, P397, I425, and L447; H-bond with Y394. | ||||
| Glycine amides | ||||
R12: Compound 4a | Mechanism-based, 0.80 µM | 2C11 | GOLD 5.2 | [83] |
| Interacting residues: Covalent bond between the primary amine group and TPQ; CH–p interaction with L447, CH–O interaction with the L468 backbone carbonyl oxygen, arene--H interaction with L447. | ||||
R13: Compound 4g | Mechanism-based, 0.34 µM | 2C11 | GOLD 5.2 | [83] |
| Interacting residues: Covalent bond between the primary amine group and TPQ; CH–O interaction with the L468 backbone carbonyl oxygen, arene–H interaction with L447. | ||||
R14: Compound 17h | Mechanism-based, 25 nM | 2C11 | GOLD 5.2 | [84] |
| Interacting residues: Covalent bond between primary amine group and TPQ; Three CH–p interactions: central phenyl ring with L469, pyrimidine ring with L447, and the hydrogen in the piperazine with Y394; two CH–O interactions: the oxygen in the glycine amide moiety with L468, and the hydrogen of the carbonyl group in the glycine amide moiety with the carbonyl oxygen of the L468 backbone; chloro group formed a halogen–O interaction with the carbonyl oxygen of the D446 backbone. | ||||
| PDB ID | Resolution, Å | Expression System | Date Deposited | Ligands | Inhibition Type, IC50/Ki | Ref. |
|---|---|---|---|---|---|---|
| Vascular Adhesion Protein 1 | ||||||
| 1PU4 | 3.20 | Cricetulus griseus (CHO cells) | 24.06.03 | — | n.a.1 | [8] |
| 1US1 | 2.90 | Cricetulus griseus (CHO cells) | 17.11.03 | — | n.a. | [8] |
| 2C10 | 2.50 | Homo sapiens (HEK293 cells) | 09.09.05 | — | n.a. | [7] |
| 2C11 | 2.90 | H. sapiens (HEK293 cells) | 09.09.05 | 2-Hydrazinopyridine | Mechanism- based, n.d.2 | [7] |
| 2Y73 | 2.60 | H. sapiens (human serum) | 28.01.11 | Imidazole | Mechanism- based, n.d.2 | [9] |
| 2Y74 | 2.95 | H. sapiens (human serum) | 28.01.11 | Imidazole | Mechanism- based, n.d.2 | [9] |
| 3ALA | 2.90 | Cricetulus griseus (CHO cells) | 29.07.10 | — | n.a. | [85] |
| 4BTW | 2.80 | H. sapiens (human serum) | 19.06.13 | R15: 5-(cyclohexylamino)-2-phenyl-6-(1H-1,2,4-triazol-5-yl)-3(2H)-pyridazinone | Reversible IC50 = 71 nM | [10] |
| 4BTX | 2.78 | H. sapiens (human serum) | 19.06.13 | R16: 5-isopropylamino-2-phenyl-6-(1H-1,2,4-triazol-5-yl)-3(2H)-pyridazinone | Reversible IC50 = 290 nM | [10] |
| 4BTY | 3.10 | H. sapiens (human serum) | 19.06.13 | R17: 5-[4-(4-methylpiperazin-1-yl)phenylamino]-2-(4-chlorophenyl)-6-(1H-1,2,4-triazol-5-yl)-3(2H)-pyridazinone | Reversible IC50 = 20 nM | [10] |
| Diamine Oxidase | ||||||
| 3HI7 | 1.80 | Drosophila melanogaster (S2 cells) | 19.05.09 | — | n.a. | [11] |
| 3HIG | 2.09 | Drosophila melanogaster (S2 cells) | 19.05.09 | Berenil (4-[(2E)-3-(4-carbamimidoylphenyl)triaz-2-en-1-yl]benzene-1-carboximidamide) | Reversible Ki = 13 nM | [11] |
| 3HII | 2.15 | Drosophila melanogaster (S2 cells) | 20.05.09 | Pentamidine (1,5-bis(4-amidinophenoxy)pentane) | Reversible Ki = 290 nM | [11] |
| 3K5T | 2.11 | Drosophila melanogaster (S2 cells) | 08.10.09 | — | n.a. | [13] |
| 3MPH | 2.05 | Drosophila melanogaster (S2 cells) | 27.04.10 | Aminoguanidine | Mechanism- based, Ki = 140 nM | [12] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vakal, S.; Jalkanen, S.; Dahlström, K.M.; Salminen, T.A. Human Copper-Containing Amine Oxidases in Drug Design and Development. Molecules 2020, 25, 1293. https://doi.org/10.3390/molecules25061293
Vakal S, Jalkanen S, Dahlström KM, Salminen TA. Human Copper-Containing Amine Oxidases in Drug Design and Development. Molecules. 2020; 25(6):1293. https://doi.org/10.3390/molecules25061293
Chicago/Turabian StyleVakal, Serhii, Sirpa Jalkanen, Käthe M. Dahlström, and Tiina A. Salminen. 2020. "Human Copper-Containing Amine Oxidases in Drug Design and Development" Molecules 25, no. 6: 1293. https://doi.org/10.3390/molecules25061293