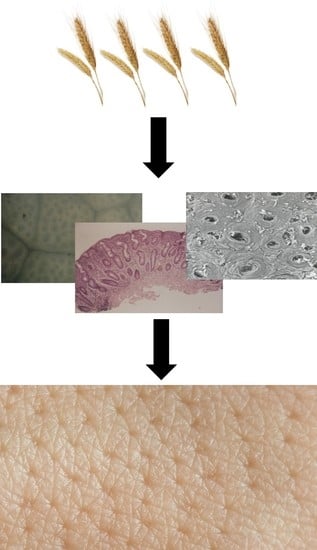
The Skin in Celiac Disease Patients: The Other Side of the Coin
Abstract
:1. Introduction
2. Blistering Diseases
2.1. Pemphigus
2.2. Dermatitis Herpetiformis
2.3. Linear IgA Bullous Dermatosis
3. Urticaria
4. Hereditary Angioneurotic Edema
5. Atopic Dermatitis
6. Cutaneous Vasculitis
7. Erythema Nodosum
8. Erythema Elevatum Diutinum
9. Necrolytic Migratory Erythema
10. Psoriasis
11. Vitiligo Disease
12. Behçet’s Disease
13. Aphthous Stomatitis
14. Oral Lichen Planus
15. Dermatomyositis
16. Porphyria
17. Alopecia Areata
18. Rosacea
19. Acquired Hypertrichosis Lanuginosa
20. Pyoderma Gangrenosum
21. Ichthyosiform Dermatoses
22. Pellagra
23. Generalized Acquired Cutis Laxa
24. Skin Malignancies
25. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lebwohl, B.; Sanders, D.S.; Green, P.H.R. Coeliac disease. Lancet 2018, 391, 70–81. [Google Scholar] [CrossRef]
- Leonard, M.M.; Sapone, A.; Catassi, C.; Fasano, A. Celiac disease and nonceliac gluten sensitivity: A review. JAMA 2017, 318, 647–656. [Google Scholar] [CrossRef] [PubMed]
- Abenavoli, L.; Proietti, I.; Zaccone, V. Celiac disease: From gluten to skin. Expert. Rev. Clin. Immunol. 2009, 5, 789–800. [Google Scholar] [CrossRef] [PubMed]
- Abenavoli, L.; Proietti, I.; Leggio, L. Cutaneous manifestations in celiac disease. World J. Gastroenterol. 2006, 12, 843–852. [Google Scholar] [CrossRef] [Green Version]
- Hujoel, I.A.; Reilly, N.R.; Rubio-Tapia, A. Celiac disease: Clinical features and diagnosis. Gastroenterol. Clin. North Am. 2019, 48, 19–37. [Google Scholar] [CrossRef] [PubMed]
- OCEBM Levels of Evidence. Available online: https://www.cebm.net/?o=1025 (accessed on 31 May 2019).
- Palleria, C.; Bennardo, L.; Dastoli, S.; Iannone, L.F.; Silvestri, M.; Manti, A.; Nisticò, S.P.; Russo, E.; De Sarro, G. Angiotensin-converting-enzyme inhibitors and angiotensin II receptor blockers induced pemphigus: A case series and literature review. Dermatol. Ther. 2018, 32, e12748. [Google Scholar] [CrossRef] [Green Version]
- Labidi, A.; Serghini, M.; Karoui, S.; Ben Mustapha, N.; Boubaker, J.; Filali, A. Epilepsy, pemphigus and celiac disease: An exceptional association. Tunis Med. 2014, 92, 585–586. [Google Scholar]
- Drago, F.; Cacciapuoti, M.; Basso, M.; Parodi, A.; Rebora, A. Pemphigus improving with gluten-free diet. Acta Derm. Venereol. 2005, 85, 84–85. [Google Scholar] [CrossRef]
- Antiga, E.; Caproni, M. The diagnosis and treatment of dermatitis herpetiformis. Clin. Cosmet. Investig. Dermatol. 2015, 13, 257–265. [Google Scholar] [CrossRef]
- Salmi, T.T.; Hervonen, K.; Kurppa, K.; Collin, P.; Kaukinen, K.; Reunala, T. Celiac disease evolving into dermatitis herpetiformis in patients adhering to normal or gluten-free diet. Scand. J. Gastroenterol. 2015, 50, 387–392. [Google Scholar] [CrossRef]
- Hull, C.M.; Liddle, M.; Hansen, N. Elevation of IgA anti-epidermal transglutaminase antibodies in dermatitis herpetiformis. Br. J. Dermatol. 2008, 159, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Reunala, T.; Salmi, T.T.; Hervonen, K.; Kaukinen, K.; Collin, P. Dermatitis herpetiformis: A common extraintestinal manifestation of coeliac disease. Nutrients 2018, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Husby, S.; Koletzko, S.; Korponay-Szabó, I.R.; Mearin, M.L.; Phillips, A.; Shamir, R.; Troncone, R.; Giersiepen, K.; Branski, D.; Catassi, C.; et al. European society for pediatric gastroenterology, hepatology, and nutrition guidelines for the diagnosis of coeliac disease. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 136–160. [Google Scholar] [CrossRef] [PubMed]
- Mendes, F.B.; Hissa-Elian, A.; Abreu, M.A.; Gonçalves, V.S. Review: Dermatitis herpetiformis. Ann. Bras. Dermatol. 2013, 88, 594–599. [Google Scholar] [CrossRef] [PubMed]
- Egan, C.A.; Smith, E.P.; Taylor, T.B.; Meyer, L.J.; Samowitz, W.S.; Zone, J.J. Linear IgA bullous dermatosis responsive to a gluten-free diet. Am. J. Gastroenterol. 2001, 96, 1927–1929. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F.; Lindelöf, B.; Rashtak, S.; Rubio-Tapia, A.; Murray, J.A. Does urticaria risk increase in patients with celiac disease? A large population-based cohort study. Eur. J. Dermatol. 2013, 23, 681–687. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, B.; O’Neill, C.; Francis, D.; Niimi, N.; Barr, R.; Barlow, R.; Kobza, B.A.; Welsh, K.; Greaves, M. Human leucocyte antigen class II associations in chronic idiopathic urticaria. Br. J. Dermatol. 1999, 140, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Rodrigo, L.; Beteta-Gorriti, V.; Alvarez, N.; De Castro, C.G.; De Dios, A.; Palacios, L.; Santos-Juanes, J. Cutaneous and mucosal manifestations associated with celiac disease. Nutrients 2018, 21, 10. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.E., 3rd. Oedema: A current state-of-the-art review, III: Mechanisms of hereditary angioedema. Ann. Allergy Asthma Immunol. 2008, 100, S7–S12. [Google Scholar] [CrossRef]
- Farkas, H.; Visy, B.; Fekete, B.; Karádi, I.; Kovács, J.B.; Kovács, I.B.; Kalmár, L.; Tordai, A.; Varga, L. Association of celiac disease and hereditary angioneurotic edema. Am. J. Gastroenterol. 2002, 97, 2682–2683. [Google Scholar] [CrossRef]
- Henao, M.P.; Kraschnewski, J.L.; Kelbel, T.; Craig, T.J. Diagnosis and screening of patients with hereditary angioedema in primary care. Ther. Clin. Risk Manag. 2016, 12, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Boothe, D.W.; Tarbox, J.A.; Tarbox, M.B. Atopic dermatitis: Pathophysiology. Adv. Exp. Med. Biol. 2017, 1027, 21–37. [Google Scholar]
- Ress, K.; Annus, T.; Putnik, U.; Luts, K.; Uibo, R.; Uibo, O. Celiac disease in children with atopic dermatitis. Pediatr. Dermatol. 2014, 31, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.R.; Carlson, J.A. Clinical approach to cutaneous vasculitis. Am. J. Clin. Dermatol. 2008, 9, 71–92. [Google Scholar] [CrossRef] [PubMed]
- Baigrie, D.; Crane, J.S. Leukocytoclastic Vasculitis (Hypersensitivity Vasculitis); StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Meyers, S.; Dikman, S.; Spiera, H.; Schultz, N.; Janowitz, H. Cutaneous vasculitis complicating coeliac disease. Gut 1981, 22, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Caproni, M.; Bonciolini, V.; D’Errico, A.; Antiga, E.; Fabbri, P. Celiac disease and dermatologic manifestations: Many skin clue to unfold gluten-sensitive enteropathy. Gastroenterol. Res. Pract. 2012, 2012, 952753. [Google Scholar] [CrossRef]
- Spagnuolo, R.; Dastoli, S.; Silvestri, M. Anti interleukin 12/23 in the treatment of erythema nodosum and Crohn disease: A case report. Dermatol. Ther. 2019, 32, e12811. [Google Scholar] [CrossRef]
- Fretzayas, A.; Moustaki, M.; Liapi, O.; Nicolaidou, P. Erythema nodosum in a child with celiac disease. Case Rep. Pediatr. 2011, 2011, 935153. [Google Scholar] [CrossRef]
- Papadopoulos, K.I.; Sjoberg, K.; Lindgren, S.; Hallengren, B. Evidence of gastrointestinal immunoreactivity in patients with sarcoidosis. J. Int. Med. 1999, 245, 525–531. [Google Scholar] [CrossRef]
- Momen, S.E.; Jorizzo, J.; Al-Niaimi, F. Erythema elevatum diutinum: A review of presentation and treatment. J. Eur. Acad. Dermatol. Venereol. 2014, 28, 1594–1602. [Google Scholar] [CrossRef]
- Rodriguez-Serna, M.; Fortea, J.M.; Perez, A.; Febrer, I.; Ribes, C.; Aliaga, A. Erythema elevatum diutinum associated with celiac disease: Response to a gluten-free diet. Pediatr. Dermatol. 1993, 10, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Tasanen, K.; Raudasoja, R.; Kallioinen, M.; Ranki, A. Erythema elevatum diutinum in association with coeliac disease. Br. J. Dermatol. 1997, 136, 624–627. [Google Scholar] [CrossRef] [PubMed]
- Compton, N.L.; Chien, A.J. A rare but revealing sign: Necrolytic migratory erythema. Am. J. Med. 2013, 126, 387–389. [Google Scholar] [CrossRef]
- Tamura, A.; Ogasawara, T.; Fujii, Y.; Kanek, H.; Nakayama, A.; Higuchi, S.; Hashimoto, N.; Miyabayashi, Y.; Fujimoto, M.; Komai, E. Glucagonoma with necrolytic migratory erythema: Metabolic profile and detection of biallelic inactivation of DAXX gene. J. Clin. Endocrinol. Metab. 2018, 103, 2417–2423. [Google Scholar] [CrossRef] [PubMed]
- Bennardo, L.; Del Duca, E.; Dastoli, S.; Schipani, G.; Scali, E.; Silvestri, M.; Nisticò, S.P. Potential applications of topical oxygen therapy in dermatology. Dermatol. Pract. Concept. 2018, 8, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Dattola, A.; Silvestri, M.; Bennardo, L.; Del Duca, E.; Longo, C.; Bianchi, L.; Nisticò, S.P. Update of calcineurin inhibitors to treat inverse psoriasis: A systematic review. Dermatol. Ther. 2018, 31, e12728. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.J.; Nguyen, T.U.; Poon, K.Y.; Herrinton, L.J. The association of psoriasis with autoimmune diseases. J. Am. Acad. Dermatol. 2012, 67, 924–930. [Google Scholar] [CrossRef]
- Bhatia, B.K.; Millsop, J.W.; Debbaneh, M.; Koo, J.; Linos, E.; Liao, W. Diet and psoriasis, part II: Celiac disease and role of a gluten-free diet. J. Am. Acad. Dermatol. 2014, 71, 350–358. [Google Scholar] [CrossRef] [Green Version]
- Tsoi, L.C.; Spain, S.L.; Knight, J.; Ellinghaus, E.; Stuart, P.E.; Capon, F.; Ding, J.; Li, Y.; Tejasvi, T.; Gudjonsson, J.E.; et al. Identification of 15 new psoriasis susceptibility loci highlights the role of innate immunity. Nat. Genet. 2012, 44, 1341–1348. [Google Scholar] [CrossRef] [Green Version]
- Cianci, R.; Cammarota, G.; Frisullo, G.; Pagliari, D.; Ianiro, G.; Martini, M.; Frosali, S.; Plantone, D.; Damato, V.; Casciano, F.; et al. Tissue-infiltrating lymphocytes analysis reveals large modifications of the duodenal “immunological niche” in coeliac disease after gluten-free diet. Clin. Transl. Gastroenterol. 2012, 3, e28. [Google Scholar] [CrossRef]
- De Bastiani, R.; Gabrielli, M.; Lora, L.; Napoli, L.; Tosetti, C.; Pirrotta, E. Association between coeliac disease and psoriasis: Italian primary care multicentre study. Dermatology 2015, 230, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Magna, P.; Elbuluk, N.; Orlow, S.J. Recent advances in understanding vitiligo. F1000Research 2016, 5, pii:F1000 Faculty Rev-2234. [Google Scholar]
- Boissy, R.E.; Manga, P. On the etiology of contact/occupational vitiligo. Pigment Cell Res. 2004, 17, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Ezzedine, K.; Lim, H.W.; Suzuki, T.; Katayama, I.; Hamzavi, I.; Lan, C.C.; Goh, B.K.; Anbar, T.; De Castro, S.C.; Lee, A.Y. Revised classification/nomenclature of vitiligo and related issues: The Vitiligo Global Issues Consensus Conference. Pigment Cell Melanoma Res. 2012, 25, E1–E13. [Google Scholar] [CrossRef] [PubMed]
- Shahmoradi, Z.; Najafian, J.; Naeini, F.F.; Fahimipour, F. Vitiligo and autoantibodies of celiac disease. Int. J. Prev. Med. 2013, 4, 200–203. [Google Scholar] [PubMed]
- Abenavoli, L. Behçet’s disease and celiac disease: A rare association or a possible link? Rheumatol. Int. 2010, 30, 1405–1406. [Google Scholar] [CrossRef] [PubMed]
- Abenavoli, L.; Proietti, I.; Vonghia, L.; Leggio, L.; Ferrulli, A.; Capizzi, R.; Mirijello, A.; Cardone, S.; Malandrino, N.; Leso, V.; et al. Intestinal malabsorption and skin diseases. Dig. Dis. 2008, 26, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Malahias, T.; Brar, P.; Minaya, M.T.; Green, P.H. The association between celiac disease, dental enamel defects, and aphthous ulcers in a United States cohort. J. Clin. Gastroenterol. 2010, 44, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Caldas, C.A.M.; Verderame, L.L.; De Carvalho, J.F. Behçet’s disease associated with celiac disease: A very rare association. Rheumatol. Int. 2010, 30, 523–525. [Google Scholar] [CrossRef] [PubMed]
- Nieri, M.; Tofani, E.; Defraia, E.; Giuntini, V.; Franchi, L. Enamel defects and aphthous stomatitis in celiac and healthy subjects: Systematic review and meta-analysis of controlled studies. J. Dent. 2017, 65, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Pastore, L.; Carroccio, A.; Compilato, D.; Panzarella, V.; Serpico, R.; Lo Muzio, L. Oral manifestations of celiac disease. J. Clin. Gastroenterol. 2008, 42, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Cigic, L.; Gavic, L.; Simunic, M.; Ardalic, Z.; Biocina-Lukenda, D. Increased prevalence of celiac disease in patients with oral lichen planus. Clin. Oral Investig. 2015, 19, 627–635. [Google Scholar] [CrossRef] [PubMed]
- Compilato, D.; Carroccio, A.; Campisi, G. Hidden coeliac disease in patients suffering from oral lichen planus. J. Eur. Acad. Dermatol. Venereol. 2012, 26, 390–391. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, A.P. Connective tissue disease: Current Concepts. Dermatol. Clin. 2019, 37, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Song, M.S.; Farber, D.; Bitton, A.; Jass, J.; Singer, M.; Karpati, G. Dermatomyositis associated with celiac disease: Response to a gluten-free diet. Can. J. Gastroenterol. 2006, 20, 433–435. [Google Scholar] [CrossRef] [PubMed]
- Kao, L.; Chung, L.; Fiorentino, D.F. Pathogenesis of dermatomyositis: Role of cytokines and interferon. Curr. Rheumatol. Rep. 2011, 13, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Dalakas, M.C.; Hohlfeld, R. Polymyositis and dermatomyositis. Lancet 2003, 362, 971–982. [Google Scholar] [CrossRef]
- Caproni, M.; Torchia, D.; Cardinali, C.; Volpi, W.; Del Bianco, E.; D’Agata, A.; Fabbri, P. Infiltrating cells, related cytokines and chemokine receptors in lesional skin of patients with dermatomyositis. Br. J. Dermatol. 2004, 151, 784–791. [Google Scholar] [CrossRef] [PubMed]
- De Paepe, B.; Creus, K.K.; De Bleecker, J.L. Role of cytokines and chemokines in idiopathic inflammatory myopathies. Curr. Opin. Rheumatol. 2009, 21, 610–616. [Google Scholar] [CrossRef]
- Molnár, K.; Torma, K.; Siklós, K.; Csanády, K.; Korponay-Szabó, I.; Szalai, Z. Juvenile dermatomyositis and celiac disease. A rare association. Eur. J. Pediatr. Dermatol. 2006, 16, 153–157. [Google Scholar]
- Marie, I.; Lecomte, F.; Hachulla, E. An uncommon association: Celiac disease and dermatomyositis in adults. Clin. Exp. Rheumatol. 2001, 19, 201–203. [Google Scholar] [PubMed]
- Iannone, F.; Lapadula, G. Dermatomyositis and celiac disease association: A further case. Clin. Exp. Rheumatol. 2001, 19, 757–758. [Google Scholar] [PubMed]
- Ramanujam, V.M.; Anderson, K.E. Porphyria diagnostics-part 1: A brief overview of the porphyrias. Curr. Protoc. Hum. Genet. 2015, 86, 1–26. [Google Scholar]
- Ducamp, S.; Schneider-Yin, X.; De Rooij, F.; Clayton, J.; Fratz, E.J.; Rudd, A.; Ostapowicz, G.; Varigos, G.; Lefebvre, T.; Deybach, J.C.; et al. Molecular and functional analysis of the C-terminal region of human erythroid-specific 5-aminolevulinic synthase associated with X-linked dominant protoporphyria (XLDPP). Hum. Mol. Genet. 2013, 22, 1280–1288. [Google Scholar] [CrossRef]
- Anderson, K.E. Handbook of Porphyrin Science with Applications in Chemistry, Physics, Materials Science, Engineering, Biology, and Medicine, Vol. 29: Porphyrias and Sideroblastic Anemias; World Scientific Publishing Co.: Hackensack, NJ, USA, 2014; pp. 370–406. [Google Scholar]
- Twaddle, S.; Wassif, W.S.; Deacon, A.C.; Peters, T.J. Celiac disease in patients with variegate porphyria. Dig. Dis. Sci. 2001, 46, 1506–1508. [Google Scholar] [CrossRef] [PubMed]
- Urban-Kowalczyk, M.; Œmigielski, J.; Gmitrowicz, A. Neuropsychiatric symptoms and celiac disease. Neuropsychiatr. Dis. Treat. 2014, 10, 1961–1964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pratt, H.; King, L.; Messenger, A.; Christiano, A.; Sundberg, J. Alopecia areata. Nat. Rev. Dis. Primers. 2017, 3, 17011. [Google Scholar] [CrossRef] [PubMed]
- Hietikko, M.; Hervonen, K.; Salmi, T.; Ilus, T.; Zone, J.J.; Kaukinen, K.; Reunala, T.; Lindfors, K. Disappearance of epidermal transglutaminase and IgA deposits from the papillary dermis of patients with dermatitis herpetiformis after a long-term gluten-free diet. Br. J. Dermatol. 2018, 178, e198–e201. [Google Scholar] [CrossRef] [PubMed]
- Barahmani, N.; De Andrade, M.; Slusser, J.P.; Wei, Q.; Hordinsky, M.; Prezzo, V.H.; Christiano, A.; Norris, D.; Reveille, J.; Duvic, M. Human leukocyte antigen class II alleles are associated with risk of alopecia areata. J. Invest. Dermatol. 2008, 128, 240–243. [Google Scholar] [CrossRef]
- Betz, R.C.; Petukhova, L.; Ripke, S. Genome-wide meta-analysis in alopecia areata resolves HLA associations and reveals two new susceptibility loci. Nature Commun. 2015, 6, 5966. [Google Scholar] [CrossRef]
- Carroll, J.; McElwee, K.J.; King, L.E.; Byrne, M.C.; Sundberg, J.P. Gene array profiling and immunomodulation studies define a cell mediated immune response underlying the pathogenesis of alopecia areata in a mouse model and humans. J. Invest. Dermatol. 2002, 119, 392–402. [Google Scholar] [CrossRef] [PubMed]
- Fricke, A.C.V.; Miteva, M. Epidemiology and burden of alopecia areata: A systematic review. Clin. Cosmet. Investig. Dermatol. 2015, 8, 397–403. [Google Scholar]
- Hallaji, Z.; Akhyani, M.; Ehsani, A.H.; Noormohammadpour, P.; Gholamali, F.; Bagheri, M.; Jahromi, J. Prevalence of anti-gliadin antibody in patients with alopecia areata: A case-control study. Tehran Univ. Med. J. 2011, 68, 738–742. [Google Scholar]
- Collin, P.; Reunala, T. Recognition and management of the cutaneous manifestations of Celiac disease. Am J. Clin. Dermatol. 2003, 4, 13–20. [Google Scholar] [CrossRef]
- Naveh, Y.; Rosenthal, E.; Ben-Arieh, Y.; Etzioni, A. Celiac disease-associated alopecia in childhood. J. Pediatr. 1999, 134, 362–364. [Google Scholar] [CrossRef]
- Mokhtari, F.; Panjehpour, T.; Naeini, F.; Hosseini, S.; Nilforoushzadeh, M.; Matin, M. The frequency distribution of celiac autoantibodies in alopecia areata. Int. J Prev. Med. 2016, 7, 109. [Google Scholar] [CrossRef] [PubMed]
- Van Zuuren, E.J. Rosacea. Nat. Engl. J. Med. 2017, 377, 1754–1764. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.L.S.; Raber, I.; Xu, J.; Li, R.; Spitale, R.; Chen, J.; Kiefer, A.K.; Tian, C.; Eriksson, N.K.; Hinds, D.A.; et al. Assessment of the genetic basis of rosacea by genome-wide association study. J. Invest. Dermatol. 2015, 135, 1548–1555. [Google Scholar] [CrossRef]
- Egeberg, A.; Weinstock, L.B.; Thyssen, E.P.; Gislason, G.H.; Thyssen, J.P. Rosacea and gastrointestinal disorders: A population-based cohort study. Br. J. Dermatol. 2017, 176, 100–106. [Google Scholar] [CrossRef]
- Sánchez-Estella, J.; Yuste, M.; Santos, J.C.; Alonso, M.T. Acquired paraneoplastic hypertrichosis lanuginose. Actas Dermosifiliogr. 2005, 96, 459–461. [Google Scholar] [CrossRef]
- Corazza, G.R.; Masina, M.; Passarini, B.; Neri, I.; Varotti, C. Ipertricosi lanuginosa acquisita associata a sindrome celiaca. G. Ital. Dermatol. Venereol. 1988, 123, 611–612. [Google Scholar] [PubMed]
- Braswell, S.F.; Kostopoulos, T.C.; Ortega-Loayza, A.G. Pathophysiology of pyoderma gangrenosum (PG): An updated review. J. Am. Acad. Dermatol. 2015, 73, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Hindryckx, P.; Novak, G.; Costanzo, A.; Danese, S. Disease-related and drug-induced skin manifestations in inflammatory bowel disease. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 203–214. [Google Scholar] [CrossRef] [PubMed]
- Weizman, A.V.; Huang, B.; Targan, S.; Dubinsky, M.; Fleshner, P.; Kaur, M.; Ippoliti, A.; Panikkath, D.; Vasiliauskas, E.; Shih, D.; et al. Pyoderma gangrenosum among patients with inflammatory bowel disease: A descriptive cohort study. J. Cutan. Med. Surg. 2014, 19, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Ampuero, J.; Rojas-Feria, M.; Castro-Fernández, M.; Cano, C.; Romero-Gómez, M. Predictive factors for erythema nodosum and pyoderma gangrenosum in inflammatory bowel disease. J. Gastroenterol. Hepatol. 2014, 29, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Sedda, S.; Caruso, R.; Marafini, I. Pyoderma gangrenosum in refractory celiac disease: A case report. BMC Gastroenterol. 2013, 13, 162. [Google Scholar] [CrossRef] [PubMed]
- Oji, V. Clinical presentation and etiology of ichthyoses. Overview of the new nomenclature and classification. Hautarzt 2010, 61, 891–902. [Google Scholar] [CrossRef] [PubMed]
- Menni, S.; Boccardi, D.; Brusasco, A. Ichthyosis revealing coeliac disease. Eur. J. Dermatol. 2000, 10, 398–399. [Google Scholar]
- Nenna, R.; D’Eufemia, P.; Celli, M.; Mennini, M.; Petrarca, L.; Zambrano, A.; Montuori, M.; La Pietra, M.; Bonamico, M. Celiac disease and lamellar ichthyosis. Case study analysis and review of the literature. Acta Dermatovenerol. Croat. 2011, 19, 268–270. [Google Scholar]
- De Oliveira, A.A.; Bortolato, T.; Bernardes, F.F. Pellagra. J. Emerg. Med. 2018, 54, 238–240. [Google Scholar] [CrossRef]
- Lightwood, R.; Smallpeice, V. Coeliac disease with a conditioned vitamin deficiency resembling, but not typical of Pellagra. Proc. R. Soc. Med. 1937, 31, 71–73. [Google Scholar] [CrossRef] [PubMed]
- Schattner, A. 70-year-old man with isolated weight loss and a pellagra-like syndrome due to celiac disease. Yale J. Biol. Med. 1999, 72, 15–18. [Google Scholar] [PubMed]
- Paulsen, I.F.; Bredgaard, R.; Hesse, B.; Steiniche, T.; Henriksen, T.F. Acquired cutis laxa: Diagnostic and therapeutic considerations. J. Plast. Reconstr. Aesthet. Surg. 2014, 67, e242–e243. [Google Scholar] [CrossRef] [PubMed]
- Berk, D.R.; Bentley, D.D.; Bayliss, S.J.; Lind, A.; Urban, Z. Cutis laxa: A review. J. Am. Acad. Dermatol. 2012, 66, 842-e1–842-e17. [Google Scholar] [CrossRef] [PubMed]
- García-Patos, V.; Pujol, R.M.; Barnadas, M.A.; Pérez, M.; Moreno, A.; Condomines, J.; Gelpi, C.; Rodríguez, J.L.; De Moragas, J.M. Generalized acquired cutis laxa ssociated with coeliac disease: Evidence of immunoglobulin A deposits on the dermal elastic fibers. Br. J. Dermatol. 1996, 135, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Ilus, T.; Kaukinen, K.; Virta, L.J.; Pukkala, E.; Collin, P. Incidence of malignancies in diagnosed celiac patients: A population-based estimate. Am. J. Gastroenterol. 2014, 109, 1471–1477. [Google Scholar] [CrossRef] [PubMed]
- Porter, W.M.; Dawe, S.A.; Bunker, C.B. Dermatitis herpetiformis and cutaneous T-cell lymphoma. Clin. Exp. Dermatol. 2001, 26, 304–305. [Google Scholar] [CrossRef] [PubMed]

| Disorders Associated | Level of Evidence |
|---|---|
| Pemphigus | 4 |
| Dermatitis herpetiformis | 1A |
| Linear IgA bullous dermatosis | 4 |
| Urticaria | 2B |
| Hereditary angioneurotic edema | 4 |
| Atopic dermatitis | 4 |
| Cutaneous vasculitis | 4 |
| Erythema nodosum | 4 |
| Erythema elevatum diutinum | 4 |
| Necrolytic migratory erythema | 4 |
| Psoriasis | 1A |
| Vitiligo disease | 3B |
| Stomatous Aphtitis | 2A |
| Behçet’s disease | 4 |
| Oral lichen planus | 3B |
| Dermatomyositis | 4 |
| Porphyria | 4 |
| Rosacea | 2B |
| Alopecia areata | 3B |
| Acquired hypertrichosis lanuginosa | 5 |
| Pyoderma gangrenosum | 4 |
| Ichthyosiform dermatoses | 4 |
| Pellagra | 5 |
| Generalized acquired cutis laxa | 5 |
| Skin malignancies | 2B |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abenavoli, L.; Dastoli, S.; Bennardo, L.; Boccuto, L.; Passante, M.; Silvestri, M.; Proietti, I.; Potenza, C.; Luzza, F.; Nisticò, S.P. The Skin in Celiac Disease Patients: The Other Side of the Coin. Medicina 2019, 55, 578. https://doi.org/10.3390/medicina55090578
Abenavoli L, Dastoli S, Bennardo L, Boccuto L, Passante M, Silvestri M, Proietti I, Potenza C, Luzza F, Nisticò SP. The Skin in Celiac Disease Patients: The Other Side of the Coin. Medicina. 2019; 55(9):578. https://doi.org/10.3390/medicina55090578
Chicago/Turabian StyleAbenavoli, Ludovico, Stefano Dastoli, Luigi Bennardo, Luigi Boccuto, Maria Passante, Martina Silvestri, Ilaria Proietti, Concetta Potenza, Francesco Luzza, and Steven Paul Nisticò. 2019. "The Skin in Celiac Disease Patients: The Other Side of the Coin" Medicina 55, no. 9: 578. https://doi.org/10.3390/medicina55090578