- 1Department of Health and Social Work, University of Applied Sciences Emden/Leer, Emden, Germany
- 2Women’s Research Center, Brandeis University, Waltham, MA, United States
- 3Leibniz Institute for Prevention Research and Epidemiology–BIPS, Bremen, Germany
- 4Medical School, Vilnius University, Vilnius, Lithuania
- 5Countway Library of Medicine, Harvard Medical School, Boston, MA, United States
- 6Harvard Medical School, Boston, MA, United States
Objectives: We aimed at 1) collating and evaluating the current evidence on factors contributing to resilience of adult transnational migrants, 2) identifying methodological factors which contribute to the findings, 3) identifying and analyzing promotive and preventive factors contributing to the findings.
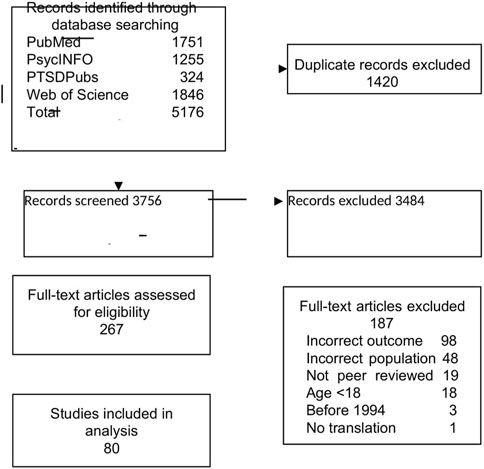
Methods: A systematic search for relevant studies published until 2021 was conducted in PubMed, PsycINFO, PTSDPubs, and Web of Science. Both, quantitative and qualitative peer-reviewed observational studies reporting on resilience and wellbeing, sense of coherence, or post-traumatic growth outcomes among transnational migrants (aged 18+). Risk of Bias was assessed using the Critical Appraisal Skills Program for qualitative studies and the Appraisal Tool for cross-sectional studies. Due to the heterogeneity of studies we did a narrative review.
Results: Database search yielded 3,756 unique records, of those n = 80 records, representing n = 76 studies met the inclusion criteria. The studies provided knowledge on resilience for n = 9,845 transnational migrants across 23 countries. All studies except two were cross sectional. N = 45 reported on resilience, n = 4 on Sense of Coherence and n = 15 on Post-Traumatic Growth. The study methods were not related to the findings. Future orientation, hope and religion/spirituality, caring for others and having opportunities were shown to be more pertinent to resilience outcomes than institutional care structures.
Conclusion: Our findings highlight that mental health professionals and policymakers should try to support positive perspectives for the future and encourage policies tailored towards giving refugees opportunities to work, learn and care and to help others.
Introduction
Mental health conditions of transnational migrants (migrants and refugees) is a serious and growing public health problem. Migrant, is defined as a person who moves away from his or her place of usual residence, whether within a country or across an international border, temporarily or permanently. A refugee is defined as a person who: “owing to well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group or political opinion, is outside the country of his nationality and is unable or, owing to such fear, is unwilling to avail himself of the protection of that country; or who, not having a nationality and being outside the country of his former habitual residence, is unable or, owing to such fear, is unwilling to return to it. In Africa, Article I (2) of the 1969 OAU Convention extends the refugee definition to: “every person who, owing to external aggression, occupation, foreign domination or events seriously disturbing public order in either part or the whole of his country of origin or nationality, is compelled to leave his place of habitual residence in order to seek refuge in another place outside his country of origin or nationality.” In Latin America, Conclusion III of the 1984 Cartagena Declaration, extends the refugee definition to: “persons who have fled their country because their lives, safety or freedom have been threatened by generalized violence, foreign aggression, internal conflicts, massive violation of human rights or other circumstances which have seriously disturbed public order.” [1, 2]. We use the term transnational migrants in this paper as an umbrella term including migrants, asylum seekers and refugees. According to the World Migration Report 2022 [3], in 2020, 3.6% of the world population, almost 281 million people, including 26.4 million refugees, lived outside their country of birth. Transnational migrants are often exposed during their journey to a range of risk factors for anxiety, depression, and posttraumatic stress (PTSD) (e.g., human rights violations, poverty, violence, travelling long distances under dangerous circumstances, discrimination in the host country). [4, 5] Pre-migration risk factors might include adversities such as violence and human rights violations, lack of basic needs such as food, water, housing and medical care, and separation from or loss of loved ones. Migration journey factors include exploitation and abuse [6]. Finally, resettlement factors include loss of important social roles, lack of employment, difficult living circumstances [7, 8] and discrimination. Yet, many transnational migrants display resilience [4, 9].
The negative effects of pre-migration, migration journey and resettlement adversities on mental health are well documented. Fazel et al. (2005) [10] conducted a systematic review of refugees resettled in high-income countries, and reported a prevalence of 9% for posttraumatic stress disorder (PTSD), 5% for depressive disorder, and 4% for generalized anxiety disorder, based on studies reporting on at least 200 participants. Another review covering studies published between 1987 and 2009, comprising 81,866 refugees and conflict-affected populations, reported an unadjusted weighted prevalence of 30% for PTSD and 30% for depression [4]. A recent systematic review of mental health conditions among refugees observed substantial heterogeneity of mental health outcomes [4, 11] (Kaade submitted). Some of the heterogeneity across the studies may be attributable to methodological differences (among others, measures used to assess outcomes), the changing nature of migrating populations (among others, different types of experiences), and the different coping strategies reported in the studies. While this literature contributes to knowledge on risk factors, less is known about factors that contribute to resilience and related conditions including posttraumatic growth and sense of coherence.
Without underestimating the exposure to a wide range of risk factors for mental health (e.g., poverty, violence, travelling long distances under dangerous circumstances, discrimination in the host country) [4, 5], transnational first-generation migrants show considerable levels of resilience, post-traumatic growth (PTG), and sense of coherence (SOC) [12–15] Resilience is a construct that has been conceptualized in diverse ways: as a trait, as an outcome and as a process, and is most commonly defined as “positive adaptation despite significant adversity” [9]. Accordingly, resilience refers to the dynamic process of a person successfully adapting to, or recovering from adversity [16, 17]. The resilience process may differ depending on the cultural, developmental, and historical context of individuals, and may vary across age and gender. Hence, it is a constantly changing interaction and adaption between an individual and his or her environment. Related to resilience are the concepts of Posttraumatic Growth (PTG) Sense of Coherence (SOC) and wellbeing. PTG as proposed by Tedeschi and Calhoun (1996) [18], is defined as a positive change in an individual’s life as a consequence of exposure to adversity. PTG goes beyond the absence of symptoms or return to a baseline function following adversity, and includes an adversity-induced increase in psychological benefits, such as a greater appreciation of life, improved interpersonal relationships, and re-evaluation of priorities in life [19–21]. PTG has been observed in survivors of different types of adversities [21], including the Holocaust [22], natural disasters, war and armed conflict [23]. Sense of coherence (SOC) is defined as a general orientation to life that represents the extent to which individuals (a) perceive events as structured, predictable and explicable, (b) feel able to deal with events, and (c) are willing and motivated to deal with these events [12]. According to Antonovsky, these three components are called comprehensibility, manageability, and meaningfulness, and together determine whether an individual has a strong or weak SOC. A further outcome is mental wellbeing [5], which includes a variety of facets such as self-acceptance, the establishment of close ties to other individuals, a sense of autonomy in thought and action, the ability to navigate complex environments and the pursuit of meaningful goals, and a sense of purpose in life and growth and development as a person [24].
Research on factors related to resilience, PTG, SOC and wellbeing has so far focused on factors deemed positive in Western population groups, such as openness to new experiences, optimism, extraversion [25] and social support [26, 27]. A systematic review investigating enablers of psychological wellbeing among refugees and asylum seekers (N = 16 articles with N = 1,352 participants) identified eight enablers of subjective wellbeing: social support; faith, religion and spirituality; cognitive strategies; education and training opportunities; employment and economic activities; behavioral strategies; political advocacy; and environmental conditions [28]. No systematic review so far investigated promotive and preventive factors contributing to resilience in transnational migrants, Going beyond the previous reviews, we include observational quantitative and qualitative studies investigating individual, family, and community factors associated with resilience and resilience related outcomes (PTG, SOC, and mental wellbeing). By providing a comprehensive synthesis of the current knowledge on promotive and preventive factors related to resilience in transnational migrants, our review provides empirical support for intervention programs and policy initiatives aimed at supporting and promoting resilience of transnational migrants. We expect this study to provide a suggestive direction for researchers, policymakers, and practitioners on developing strategies to promote and support resilience among transnational migrants and reduce mental health conditions. By drawing the evidence for multiple disciplines (e.g., public health, epidemiology, anthropology, sociology, medicine, psychology), it also draws attention to the importance of interdisciplinary collaboration including public health, anthropology, medicine and sociology.
Methods
We conducted a systematic literature review of factors contributing to transnational migrants’ resilience. There is no universally agreed definition of the term “first-generation migrant.” In this review we include all those which are included in the United Nation’s definition of migrant as “an individual who is residing in a foreign country, irrespective of the causes, voluntary, or involuntary, and the means, regular or irregular; used to migrate” [29]. Additionally, we do not use any restriction on length of residence but include transnational migrants, independent of length of stay in the new country. Our systematic review is reported in accordance with the PRISMA guidelines [30]. Ethical approval was not required for this review as the data are publicly available.
Search Strategy and Information Sources
We identified studies that examined resilience in migrants and refugees by searching the electronic databases PubMed (NCBI), PsycINFO (EBSCO), PTSDPubs (ProQuest), and the Web of Science Core Collection. The search, developed by a subject expert (JL) and an experienced medical librarian (PAB), included terms for refugees and migrants, together with a range of terms intended to capture studies under a broad definition of resilience. Under the broad definition of resilience were included studies investigating resilience, PTG, SOC or mental wellbeing. Controlled vocabulary terms were included when available, and no date or language restrictions were applied (Supplementary Appendix S1). The search was last updated on 15 July 2021. The most recent update in 2021 might be a limitation of this paper, however, it provides evidence on this population group of transnational migrants during the time period up to July 2021. The reference lists of included articles were examined for further studies of interest.
Inclusion and Exclusion Criteria
Studies were eligible for inclusion in this review if they fulfilled the following criteria: (a) were peer-reviewed observational empirical studies, (b) involved first generation transnational migrants (including refugees and asylum seekers) aged 18 years and above, who lived in any country outside their home country, and (c) included one or more of the following as the main outcome: resilience, PTG, SOC or mental wellbeing. Studies were excluded if (a) they were intervention studies, (b) were conducted among (or included) children or adolescents younger than 18 years of age, (c) included seasonal or other specific groups of workers, (d) specifically focused on traumatized persons, and (e) investigated exclusively mental health or psychopathological (e.g., PTSD) and physical health outcomes. Studies focusing on coping strategies as a main outcome or resilience as a personal trait were also excluded. Further, studies using a single-case design (e.g., clinical case study) as well as books, book chapters, abstracts without full texts, conference proceedings, reviews, editorials, opinion statements, letters to the editor, reports, dissertations, theses and similar publications were excluded. We additionally excluded studies published before 1994 when the Diagnostic and Statistical Manual of Mental Disorders (DSM) was revised and updated.
Study Screening and Selection
JL, MJ and FSZ screened the titles and abstracts as well as the full texts independently using Covidence [31], an online software program that enables the creation and management of systematic reviews. Each record or article was screened by at least two individuals. Any conflicts were discussed by the three reviewers until consensus was reached. The publications selected after the full text screening were then subjected to a final in-depth review. To ensure the eligibility of publications, the research team discussed each article in detail before making the decision to include it in the data extraction stage.
Data Extraction and Coding
Data extraction was piloted on a small number of studies by the researchers independently. Data were extracted and managed in Excel spreadsheets. JL, MJ and FSZ extracted the following data from all included studies independently: authors, study design, participants (age, gender, type of population), outcome, outcome measure, confounders, confounder measures and results. The three authors then compared and discussed their outputs and thereby compiled the final data extraction tables. Where an included study was published in multiple articles, we used all outcome information. The unit of allocation remained the study, rather than the number of publications.
Risk of Bias
MJ, FSZ and Jl assessed the risk of bias of the studies, with each study being assessed by at least two researchers. Discrepancies were discussed and resolved in consensus. Due to the variation in study designs included in this review, two separate appraisal tools were used to assess risk of bias: the Critical Appraisal Skills Program (CASP) [32] for qualitative studies, and the Appraisal Tool for Cross-sectional Studies (AXIS) [33] for quantitative studies. The CASP checklist includes 10 aspects to be recorded with a “yes,” “cannot tell,” or “no.” The total number of “yes” responses indicates the risk of bias level of the study, which can range from 0–10. We rated as high risk of bias studies scoring 0–2 yes responses, moderate risk of bias studies scoring 2–5 yes and low risk of bias those studies with more than 5 yes responses. The AXIS consists of 20 components to be recorded with “yes,” “no,” “don’t know/comment.” We stratified the studies according to potential risk of bias. We rated as low risk of bias studies scoring 0–2 yes responses, moderate risk of bias studies scoring 2–5 yes and high risk of bias those studies with more than 5 yes responses.
Synthesis of Results
Due to the diversity across studies in relation to outcomes, settings, samples, methods, and measures, both qualitative and quantitative data were synthetized narratively. A thematic synthesis method was used. The authors coded the extracted text and identified descriptive themes. The latter were then collapsed into analytical themes through discussion within the research team.
Results
Characteristics of the Included Studies
A total of 3,756 unique records were identified through database searching, and 267 full-text articles were assessed for inclusion (Figure 1). Finally, we identified 80 articles, representing 77 studies, that met the inclusion criteria and were included in our analysis, providing data for n = 10,047 transnational adult migrants. Six of the studies included in the review were published before 2010, n = 30 studies used quantitative methods, N = 3 used mixed methods, and n = 44 were qualitative (Table 1). Out of the 30 quantitative studies, all except two were cross-sectional. Regarding outcomes, n = 45 studies reported on resilience, n = 4 on sense of coherence and n = 15 on post-traumatic growth and n = 20 on mental wellbeing, (Tables 2, 3).
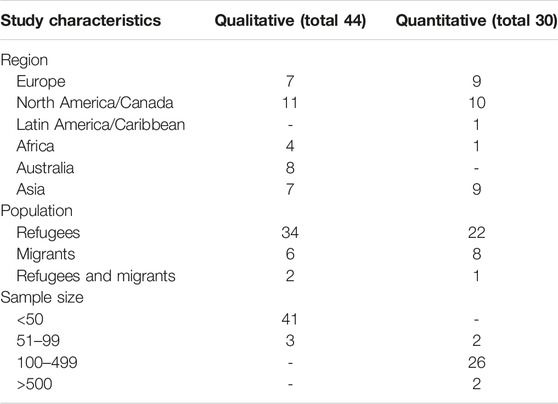
TABLE 1. Overview of included studies (n = 39 qualitative, n = 30 quantitative, n = 3 mixed methods, n = 1 action research) Global, 2021.
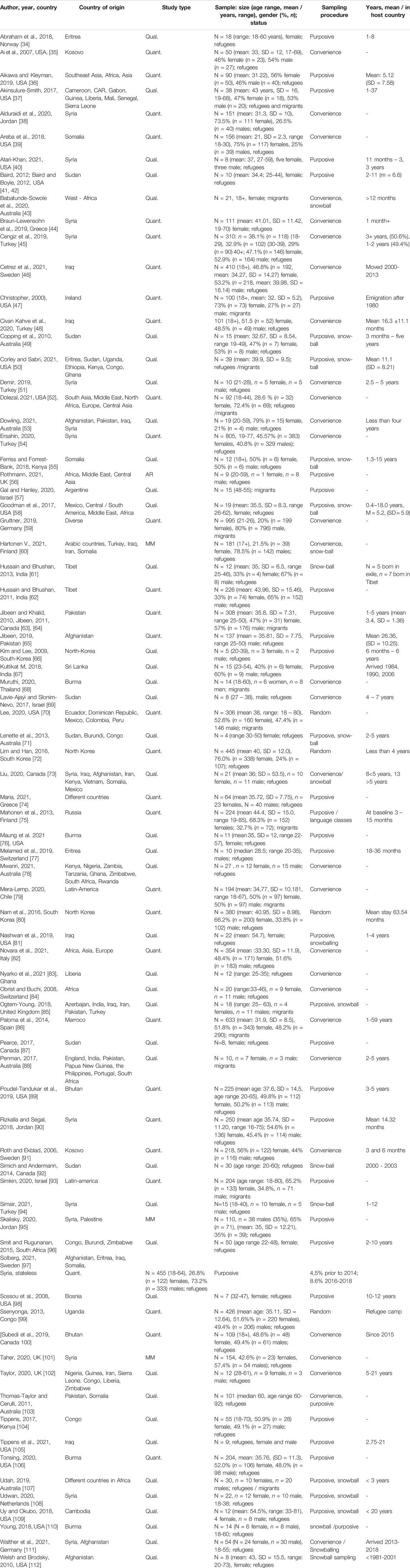
TABLE 2. Studies included in the review on resilience factors in transnational migrants (migrants, refugees) Global, 2021.
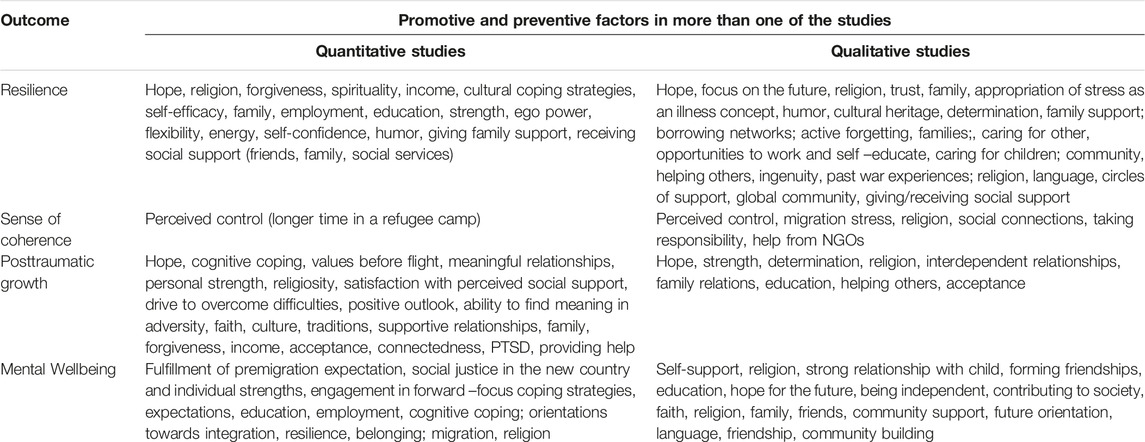
TABLE 3. Outcomes, studies, promotive and preventive factors in qualitative and in quantitative studies included in the review. Global, 2021.
Region of Study and Origin of Participants
In most of the studies (n = 60), the transnational migrants were defined as being refugees (Table 1). In the rest of the studies, participants were defined as migrants (n = 13), or as refugees (including asylum seekers) and migrants (n = 7).
Study Sample Characteristics
The study sample sizes ranged from n = 50 [35] to n = 995 [59] among quantitative studies, and from n = 4 [71] to n = 55 [104] among qualitative studies (Table 2). The majority of the participants were female (57.21%, n = 5,748) and the age range of the participants across all studies ranged from 18–68 years. The participants originated from more than 30 countries including Afghanistan [65, 111, 112], Congo [104], Eritrea [34, 113], Iran [73, 85], Iraq [60, 81, 85, 105, 114], Somalia [39, 115, 116], and Syria [38, 51, 53, 54, 73, 90, 94, 95, 101, 108, 111, 117] (Table 1).
Most of the studies were conducted in high income countries such as Australia [43, 53, 71, 78, 88, 107, 116, 118], Canada [63, 64, 87, 100], and the USA [35–37, 39, 40, 42, 47, 50, 52, 58, 70, 76, 81, 89, 98, 106, 109, 110, 112], with fewer being conducted in low and middle income countries: in Congo [99], Chile [79], Ghana [119], India [62], Jordan [38, 90, 95], Kenya [55, 104], South - Korea [66, 80, 120], Nepal [121], South Africa [96], Thailand [68], South-Africa [96] and Turkey [45, 48, 51, 54, 94]. Three studies reported that their participants were living in refugee camps [65, 69, 119], while the participants of the remaining studies were living in the community.
Study Sampling Methods
The quantitative studies generally used purposive sampling or convenience sampling methods, however, three studies used random sampling [70, 72, 99] (Table 2). The qualitative studies used the following sampling methods: purposive (n = 20), combined methods (n = 15). convenience (n = 9) or snowballing (n = 6). The review findings on determinants of resilience, PTG, SOC are presented separately according to study design (Supplementary Tables S1–S3).
Quantitative Studies Exploring Promotive and Preventive Factors of Resilience, SOC and Mental Wellbeing
The 30 quantitative studies included in the review constituted n = 8,651 participants. The sample sizes of the quantitative studies ranged from n = 50 [35] to n = 995 [59], with a mean size of n = 288 participants (Table 1). Resilience was measured using self-designed questionnaires [122] or versions of the Resilience Scale (RS-25, RS-11, RS-8) [89, 123], or the Connor-Davidson Resilience Scale (CD-RISC) [45]. PTG was measured using the Post-traumatic Growth Inventory (PTGI) [35, 62, 90], and SOC using the Sense of Coherence Scale [91]. Additionally, we identified studies investigating mental wellbeing. Mental wellbeing was measured using the BBC wellbeing scale [36], and the General Wellbeing Schedule [47, 100], among others (Supplementary Table S6).
Qualitative Studies Exploring Promotive and Preventive Factors of Resilience, SOC or Mental Wellbeing
The n = 39 qualitative studies identified in the review included n = 749 transnational migrants (Table 2). The study sample sizes ranged from n = 4 to n = 55. The following methods were applied in the studies: focus groups discussions [34, 37, 50, 55, 96, 124], individual interviews [40, 43, 50, 51, 53, 57, 58, 62, 68, 73, 76–78, 81, 83–85, 88, 94, 96, 104, 109, 116, 118, 125], participatory research [56, 87], and photovoice [42]. Additionally, some studies used ethnographic methods [42, 71], or direct observations [71, 77, 81, 84, 98].
Risk of Bias Assessment
Most of the studies were assigned a low risk of bias and determined to be of high quality. The main sources of potential risk of bias among quantitative studies were the lack of information on non-responders (all studies), or no justification of the sample size (n = 25) (Supplementary Table S5). Among the qualitative studies, a moderate rating was assigned to four studies that did not explicitly address the relationship between researcher and participants or ethical aspects [41] (Supplementary Table S5). No study was assigned a high risk of bias.
Measurement of Adversities
The measurement and definition of adversity exposure was heterogeneous across studies (Tables 2, 3). While some studies used a variety of self-report measures to assess adversity, others used standardized measures such as the Communal Traumatic Events Inventory, the Language, Identity and Behavioral Acculteration Scale (LIB), Harvard Trauma Questionnaire (HTQ), Refugee Trauma Experience Inventory (RTEI), Multidimensional Acculterative Stress Scale (MASS), Psychological Trauma Scale, Family the Adaptability and Cohesion Evaluation Scale (FACES-II), and the War Event Questionnaire (WEQ) (Supplementary Table S3).
Promotive and Preventive Factors
Results from the included studies are summarized in Table 3 and discussed hereafter according to the key categories of influencing factors identified by the studies. A variety of factors associated with resilience, PTG, SOC and wellbeing were identified in both quantitative and qualitative studies. Since some of the factors identified in both study types overlapped, the findings are summarized together. The main influencing factor at the individual level was hopefulness and future orientation. Hopefulness was described as desire accompanied by expectation to be able to fulfill the desire in the host country was identified in quantitative and in qualitative studies [35, 41, 69, 98, 109, 112, 126]. Future orientation was described as determination, and forward-oriented coping [35, 36, 86]. Further influencing factors at the individual level were religiousness [34, 37, 39, 58, 100], and spirituality [66, 71, 104, 127]. Support received by family [37, 55, 72, 80] and being able to support family members [96, 112, 116, 128] and friends [42, 55, 69, 129] were reported to be important factors at the relationship level, while financial resources [45, 65, 71, 90] and access to work [69, 75, 100] and education [65] played a role at the societal level (Table 3).
Discussion
This paper examined factors influencing resilience, PTG, SOC and mental wellbeing among transnational migrants. Studies identified by the search varied widely regarding population samples, context, study design, measurements, approach to data analysis, and whether the primary study focus was on resilience or mental health. Therefore, a narrative synthesis approach was adopted to capture this heterogeneity. In both quantitative and qualitative studies, individual (forward-orientation and hope, spirituality and religiousness), relationship (caring and belonging), as well as societal factors (opportunities for education and employment, opportunities for advocacy and activism) were reported to contribute towards resilience, PTG, SOC and mental wellbeing. The findings across the included studies were relatively consistent, despite the studies being set in diverse and varied contexts across different countries and with participants of diverse cultural backgrounds and migration experiences. Taken together resilience in transnational migrants was influenced by individual factors (e.g., forward orientation and hope. religiousness), family factors (e.g., caring and belonging), community factors (e.g., peer support) and society factors opportunities for education, work, advocacy and activism.
Methdological Factors
Methodological factors in both quantitative and qualitative studies were not related to the outcome.
Promotive and Preventive Factors
Forward-Orientation and Hope
The individual factors were mainly future oriented, such as hope and forward-orientation. Hope has been conceptualized as state, as trait and as process. Hope as positive motivational cognitive-emotional process is activated during times of difficulty and is a component of individual adaptability and agency. As such hope is a multidimensional process which has emotional, cognitive, motivational, social and identity related components. Hope can be understood in a more individualist way or as context dependent. People with high hope are more likely to perceive a situation as controllable and manageable; they usually find solutions more quickly compared to individuals with low hope [130]. Synder portrayed hope as a goal-oriented cognitive construct with affective and behavioral implications [130]. Hence, hope predicts progress towards goal attainment and functions as an important resource to enhance resilience. Hope, accordingly, includes planning and motivation and the expectation that positive outcomes will occur through a person`s agency. Hope has been linked to positive moods, wellbeing, adjustment, resilience and trust. One of the studies including refugees from South Sudan who had resettled in Uganda indicated that the refugees would not have left their home countries had circumstances not forced them to do so, because of the distant hope of peace and security (Meyer 2019). In another study, hope was found to be related to positive outcome perspectives in the life of migrants (Stone 2018). In line with this research, hope and accomplishment of goals reciprocally affect each other. Conversely, when people sense that they are not making progress, their tendency to engage in agency thinking might be reduced.
Spirituality and Religiousness
Positive religious coping includes religious forgiveness, seeking spiritual support, and reappraising God as benevolent. Religiousness might constitute engaging in religious activities, which was observed to provide a sense of normality to participants in the studies. This suggests that attempting to generate a state that feels normal, comfortable, or predictable, as perceived by the individual, may also be a strategy that some transnational migrants adopt.
Caring and Belonging
Social connectedness - where people experience a sense of belonging, is a well-established protective factor for mental health. Consistent with our findings, family bonding was listed as one of the most commonly reported factors in a recent systematic review [131]. This emphasis on the importance of family relationships is in line with the idea that transnational migrants’ resilience encompasses a more communal notion of resilience than the Western, more individualized concept.
Opportunities for Education and Employment
A further factor identified in the quantitative and qualitative studies concerns opportunities to learn and work. Education and employment opportunities have been shown to influence the integration process of transnational migrants in their new societies [132]. Accordingly, the post-migration situation, including discrimination and inability to work and study due to restrictions, may negatively impact resilience. The findings regarding perceived opportunities are in line with prior research demonstrating the effects of post-migration, e.g., stress on migrants’ mental health due to poor employment opportunities. Income is a powerful determinant of health and affects mental health in every age group. A meta-analysis of 59 studies comparing refugee mental health to that of resident populations revealed a linear relationship between refugees’ mental health and the right to work, access to employment, and socioeconomic status. Though studies included in the meta-analysis did not assess visa type or authorized legal status, the findings indicate that economic opportunities are a critical factor for resilience.
Opportunities for Prosociality (Advocacy and Caring)
Furthermore, prosocial behavior and the perception of being able to contribute, care and to be active in the host country was observed to be critical for resilience in the studies included in our review. This finding indicates that the social determinants of mental health apply to international migrants’ resilience and post-traumatic growth, and the impact of social inclusion and exclusion on resilience can be measured in quantitative studies and is likewise perceived in qualitative studies. Further, the findings suggest that psychosocial services for migrants should address these factors of providing opportunities for advocacy or activisms. Giving transnational migrants opportunities for prosociality might contribute to the feeling of belonging to the host society.
Strengths and Limitations
The strength of this review is that, to our knowledge, it is the first to bring together and synthesize studies on factors contributing to resilience, PTG, SOC and mental wellbeing. Despite these strengths, this review is not without limitations. Studies were excluded if the migration status of the participants was unclear or not reported. Therefore, potentially relevant studies may have been excluded. Overall, the current evidence base is limited mostly to cross-sectional studies, making it difficult to draw causal relationships between the factors identified and the outcomes. Further, the qualitative findings are based on self-reported narratives and are subject to common limitations across all the studies such as social desirability, under reporting, and relying on memory. The evidence base would benefit from longitudinal studies to better understand factors that promote positive outcomes during migration.
The different study designs and methods applied, especially the diverse sampling, restrict the cross-applicability of findings and makes generalizations difficult. Conducting research with transnational migrant populations is associated with many challenges, one of which is sampling. While restricting the inclusion criteria to studies that incorporated multi-stage representative sampling might have further improved the quality of the review, this would have greatly reduced the number of studies fitting the criteria. A further limitation might be related to the tools used to measure the outcomes of interest. Although most of the tools had been widely used in different cultural contexts, none had been specifically developed for migrants.
Conclusion
To conclude, this review provides evidence on the positive role of hope and prosociality on transnational migrants’ resilience trajectories. One of the implications of this study is that rather than perceiving refugees as ‘passive victims’ suffering from mental health problems, attention should be given to the resilience of transnational migrants and the factors contributing to resilience. Based on the results of this study, we can conclude that there are modifiable factors which can contribute to resilience. Focusing on resilience and PTG rather than trauma is crucial in shifting the portrayal of victimized transnational migrants and instead encourages policies and psychosocial services tailored towards giving transnational migrants, especially forced migrants opportunities and higher autonomy.
The focus on a purely psychological model of impact of migration may be an obstacle to adopting a more cultural appropriate Public health approach towards migration, that includes resilience and responding to adversities with hope and prosociality. Concepts of responding to adversities that focus on dealing with the past are not necessarily applicable to the livelihood of transnational migrants in their search for making peace with the past. By shifting the focus to the strengths and capacities of individuals who migrate, this form of research can promote a view of these individuals as capable, resourceful, motivated persons, who persevere amidst adversities. Such research is also crucial as a basis for the creation of new policies, programs, and interventions that can benefit migrants in general. Research, policy, and practice are often focused on documenting vulnerabilities rather than strengths. Findings from this review suggest that programs and resource allocation should be directed to areas that encourage or facilitate hope and opportunities for migrants to enable a future-orientated focus.
Author Contributions
JL desigend the study. JL and PB conducted the systematic search. JL, FS-Z, and MJ screened the papers and analysed the results. JL wrote the first draft of the manuscript. RM read the manuscript and contributed to revising the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2023.1606406/full#supplementary-material
References
1. The UN Refugee Agency (2003). United Nations High Commissioner for Refugees. Available at: https://emergency.unhcr.org/protection/legal-framework/refugee-definition.
2. Sironi, A, Bauloz, C, and Emmanuel, M. Glossary on Migration - International Organisation of Migration Law, No. 34. Geneva: International Organisation of Migration (2019). p. 248.
3. International Organisation of Migration IOM. World Migration Report 2020. Geneva: International Organisation of Migration Press (2020). p. 498.
4. Blackmore, R, Boyle, JA, Fazel, M, Ranasinha, S, Gray, KM, Fitzgerald, G, et al. The Prevalence of Mental Illness in Refugees and Asylum Seekers: A Systematic Review and Meta-Analysis. PLOS Med (2020) 17:e1003337. doi:10.1371/journal.pmed.1003337
5. Lindert, J. Psychological Resilience in Refugees - a Systematic Review. Eur J Public Health (2017) 27:1. doi:10.1093/eurpub/ckx187.473
6. Scoglio, AAJ, and Salhi, C. Violence Exposure and Mental Health Among Resettled Refugees: A Systematic Review. Trauma, Violence & Abuse (2020) 22:1192–208. doi:10.1177/1524838020915584
7. Walther, L, Fuchs, LM, Schupp, J, and von Scheve, C. Living Conditions and the Mental Health and Well-Being of Refugees: Evidence From a Large-Scale German Survey. J Immigrant Minor Health (2020) 22:903–13. doi:10.1007/s10903-019-00968-5
8. Wu, S, Renzaho, AMN, Hall, BJ, Shi, L, Ling, L, and Chen, W. Time-Varying Associations of Pre-Migration and Post-Migration Stressors in Refugees' Mental Health During Resettlement: A Longitudinal Study in Australia. Lancet Psychiatry (2020) 8:36–47. doi:10.1016/S2215-0366(20)30422-3
9. Ungar, M. The Social Ecology of Resilience. In: A Handbook of Theory and Practice. New York: Springer Science press (2012). doi:10.1007/978-1-4614-0586-3
10. Fazel, M, Wheeler, J, and Danesh, J. Prevalence of Serious Mental Disorder in 7000 Refugees Resettled in Western Countries: A Systematic Review. Lancet (2005) 365:1309–14. doi:10.1016/S0140-6736(05)61027-6
11. Bogic, M, Njoku, A, and Priebe, S. Long-Term Mental Health of War-Refugees: A Systematic Literature Review. BMC Int Health Hum Rights (2015) 15:29. doi:10.1186/s12914-015-0064-9
12. Kelner, M. Unraveling the Mystery of Health: How People Manage Stress and Stay Well. Aaron Antonovsky. Jossey-Bass Publishers, San Francisco. Can J Aging (1987) 7:1. doi:10.1017/S0714980800007133
13. Bonanno, GA. Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive After Extremely Aversive Events? Am Psychol (2004) 59:20–8. doi:10.1037/0003-066X.59.1.20
14. Keyes, CL. The Mental Health Continuum: From Languishing to Flourishing in Life. J Health Soc Behav (2002) 43:207–22. doi:10.2307/3090197
15. Patel, V, Saxena, S, Lund, C, Thornicroft, G, Baingana, F, Bolton, P, et al. The Lancet Commission on Global Mental Health and Sustainable Development. Lancet (2018) 392:1553–98. doi:10.1016/S0140-6736(18)31612-X
16. Lines, RLJ, Crane, M, Ducker, KJ, Ntoumanis, N, Thogersen-Ntoumani, C, Fletcher, D, et al. Profiles of Adversity and Resilience Resources: A Latent Class Analysis of Two Samples. Br J Psychol (2020) 111:174–99. doi:10.1111/bjop.12397
17. Masten, AS. Resilience from a Developmental Systems Perspective. World Psychiatry (2019) 18:101–2. doi:10.1002/wps.20591
18. Tedeschi, RG, and Calhoun, LG. The Posttraumatic Growth Inventory: Measuring the Positive Legacy of Trauma. J Traumatic Stress (1996) 9:455–71. doi:10.1007/BF02103658
19. Tedeschi, RG, and Calhoun, LG. Handbook of Posttraumatic Growth: Research and Practice. New York: Psychology Press (2014). p. 402.
20. Powell, S, Rosner, R, Butollo, W, Tedeschi, RG, and Calhoun, LG. Posttraumatic Growth After War: A Study With Former Refugees and Displaced People in Sarajevo. J Clin Psychol (2003) 59:71–83. doi:10.1002/jclp.10117
21. Calhoun, LG, and Tedeschi, RG. Handbook of Posttraumatic Growth: Research and Practice. New York: Routledge (2014). p. 402.
22. Dekel, S, Mandl, C, and Solomon, Z. Is the Holocaust Implicated in Posttraumatic Growth in Second-Generation Holocaust Survivors? A Prospective Study. J Traumatic Stress (2013) 26:530–3. doi:10.1002/jts.21836
23. Kroo, A, and Nagy, H. Posttraumatic Growth Among Traumatized Somali Refugees in Hungary. J Loss Trauma (2011) 16:440–58. doi:10.1080/15325024.2011.575705
24. Lindert, J, Bain, PA, Kubzansky, LD, and Stein, C. Well-Being Measurement and the WHO Health Policy Health 2010: Systematic Review of Measurement Scales. Eur J Public Health (2015) 25:731–40. doi:10.1093/eurpub/cku193
25. Jaksic, N, Brajkovic, L, Ivezic, E, Topic, R, and Jakovljevic, M. The Role of Personality Traits in Posttraumatic Stress Disorder (PTSD). Psychiatria Danubina (2012) 24:256–66. PMID: 23013628.
26. Benetato, BB. Posttraumatic Growth Among Operation Enduring Freedom and Operation Iraqi Freedom Amputees. J Nurs Scholarship (2011) 43:412–20. doi:10.1111/j.1547-5069.2011.01421.x
27. Schroevers, MJ, Helgeson, VS, Sanderman, R, and Ranchor, AV. Type of Social Support Matters for Prediction of Posttraumatic Growth Among Cancer Survivors. Psychooncology (2010) 19:46–53. doi:10.1002/pon.1501
28. Posselt, M, Eaton, H, Ferguson, M, Keegan, D, and Procter, N. Enablers of Psychological Well-Being for Refugees and Asylum Seekers Living in Transitional Countries: A Systematic Review. Health Soc Care Community (2019) 27:808–23. doi:10.1111/hsc.12680
29. Internationla Organisation of Migration. Glossary on Migration. Geneva: Internationla Organisation of Migration press (2011). p. 118.
30. Moher, D, Liberati, A, Tetzlaff, J, Altman, DG, and Group, P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med (2009) 151:264. doi:10.7326/0003-4819-151-4-200908180-00135
31. Covidence systematic review software. Veritas Health Innovation (2021). Available at: www.covidence.org (Accessed November, 2021).
33. Downes, MJBM, Williams, HC, and Dean, RS. Development of a Critical Appraisal Tool to Assess the Quality of Cross-Sectional Studies (AXIS). BMJ Open (2016) 6:12. doi:10.1136/bmjopen-2016-011458
34. Abraham, R, Lien, L, and Hanssen, I. Coping, Resilience and Posttraumatic Growth Among Eritrean Female Refugees Living in Norwegian Asylum Reception Centres: A Qualitative Study. Int J Soc Psychiatry (2018) 64:359–66. doi:10.1177/0020764018765237
35. Ai, AL, Tice, TN, Whitsett, DD, Ishisaka, T, and Chim, MX. Posttraumatic Symptoms and Growth of Kosovar War Refugees: The Influence of hope and Cognitive Coping. J Positive Psychol (2018) 2:55–65. doi:10.1080/17439760601069341
36. Aikawa, M, and Kleyman, K. Immigration, Coping, and Well-Being: Implications for Communities' Roles in Promoting the Well-Being of Immigrants and Refugees. J Prev Intervention Community (2021) 49:81–92. doi:10.1080/10852352.2019.1633066
37. Akinsulure-Smith, AM. Resilience in the Face of Adversity: African Immigrants' Mental Health Needs and the American Transition. J Immigrant Refugees Stud (2017) 15:428–48. doi:10.1080/15562948.2016.1238989
38. Alduraidi, H, Dardas, LA, and Price, MM. Social Determinants of Resilience Among Syrian Refugees in Jordan. J Psychosocial Nurs Ment Health Serv (2020) 58:31–8. doi:10.3928/00989134-20200624-04
39. Areba, EM, Duckett, L, Robertson, C, and Savik, K. Religious Coping, Symptoms of Depression and Anxiety, and Well-Being Among Somali College Students. J Religion Health (2018) 57:94–109. doi:10.1007/s10943-017-0359-3
40. Atari-Khan, , Covington, AH, Gerstein, LH, Herz, H, Varner, BR, Brasfield, C, et al. Concepts of Resilience Among Trauma-Exposed Syrian Refugees. Couns Psychol (2021) 49:233–68. doi:10.1177/0011000020970522
41. Baird, MB. Well-Being in Refugee Women Experiencing Cultural Transition. ANS Adv Nurs Sci (2012) 35:249–63. doi:10.1097/ANS.0b013e31826260c0
42. Baird, MB, and Boyle, JS. Well-Being in Dinka Refugee Women of Southern Sudan. J Transcultural Nurs (2012) 23:14–21. doi:10.1177/1043659611423833
43. Babatunde-Sowole, OO, DiGiacomo, M, Power, T, Davidson, PM, and Jackson, . Resilience of African Migrant Women: Implications for Mental Health Practice. Int J Ment Health Nurs D (2020) 29:92–101. doi:10.1111/inm.12663
44. Braun-Lewensohn, O, Abu-Kaf, S, and Al-Said, K. Women in Refugee Camps: Which Coping Resources Help Them to Adapt? Int J Environ Res Public Health (2019) 16:3990. doi:10.3390/ijerph16203990
45. Cengiz, I, Ergun, D, and Cakici, E. Posttraumatic Stress Disorder, Posttraumatic Growth and Psychological Resilience in Syrian Refugees: Hatay, Turkey. Anadolu Psikiyatr Derg (2019) 20:3. doi:10.5455/apd.4862
46. Cetrez, OA, DeMarinis, V, Sundvall, M, Fernandez-Gonzalez, M, Borisova, L, and Titelman, D. A Public Mental Health Study Among Iraqi Refugees in Sweden: Social Determinants, Resilience, Gender, and Cultural Context. Front Sociol (2021) 6:551105. doi:10.3389/fsoc.2021.551105
47. Christopher, KA. Determinants of Psychological Well-Being in Irish Immigrants. West J Nurs Res (2000) 22:123–40. doi:10.1177/019394590002200203
48. Civan, KA, Aydemir, MC, Yuksel, RN, Kaya, H, Unverdi, BE, and Goka, E. Evaluating the Relationship Between Post Traumatic Stress Disorder Symptoms and Psychological Resilience in a Sample of Turkoman Refugees in Turkey. J Immigrant Minor Health (2020) 23:3. doi:10.1007/s10903-020-01122-2
49. Copping, A, Shakespeare-Finch, J, and Paton, D. Towards a Culturally Appropriate Mental Health System: Sudanese-Australians' Experiences With Trauma. J Pac Rim Psychol (2010) 4:53–60. doi:10.1375/prp.4.1.53
50. Corley, A, and Sabri, B. Exploring African Immigrant Women's Pre- and Post-Migration Exposures to Stress and Violence, Sources of Resilience, and Psychosocial Outcomes. Issues Ment Health Nurs (2021) 42:484–94. doi:10.1080/01612840.2020.1814912
51. Demir Ooa, R. Resilience Among Syrian University Students in Turkey. Turkish J Edu (2019) 8:1. doi:10.19128/turje.454138
52. Dolezal, ML, Alsubaien, MK, Sheikh, I, Rosencrans, P, Walker, RS, Zoellner, LA, et al. Differences in Posttraumatic and Psychosocial Outcomes Among Refugees, Asylum Seekers, and Internally Displaced Persons. J Nervous Ment Disord (2021) 209:28–34. doi:10.1097/NMD.0000000000001248
53. Dowling, AK, and Russell, G. The Impact of Migration Upon the Perceived Health of Adult Refugees Resettling in Australia: A Phenomenological Study. J Ethnic Migration Stud (2021) 48:3. doi:10.1080/1369183x.2020.1771173
54. Ersahin, Z. Post-Traumatic Growth Among Syrian Refugees in Turkey: The Role of Coping Strategies and Religiosity. Curr Psychol A J Diverse Perspect Diverse Psychol Issues (2022) 41:2398–407. doi:10.1007/s12144-020-00763-8
55. Ferriss, SS, and Forrest-Bank, SS. Perspectives of Somali Refugees on Post-Traumatic Growth After Resettlement. J Refugee Stud (2018) 31:626–46. doi:10.1093/jrs/fey006
56. Flothmann, C, and Daphne, J. Seeking Asylum in Bristol: Insights Into Psychological Needs and Resilience. Int J Migration Health Soc Care (2021) 17:2. doi:10.1108/IJMHSC-05-2020-0054
57. Gal, S, and Hanley, J. The Long-Term Impact of Political Activism on Mental Wellbeing in the Context of Adult Immigrants Who Experienced Childhood Political Trauma. J Immigrant Minor Health (2020) 22:982–7. doi:10.1007/s10903-019-00962-x
58. Goodman, RD, Vesely, CK, Letiecq, B, and Cleaveland, CL. Trauma and Resilience Among Refugee and Undocumented Immigrant Women. J Couns Dev (2017) 95:309–21. doi:10.1002/jcad.12145
59. Gruttner, M. Belonging as a Resource of Resilience: Psychological Wellbeing of International and Refugee Students in Study Preparation at German Higher Education Institutions. Student Success (2019) 10:36–44. doi:10.5204/ssj.v10i3.1275
60. Hartonen, VR, Väisänen, P, Karlsson, L, and Pöllänen, S. ‘Between Heaven and Hell’: Subjective Well-Being of Asylum Seekers. Int J Soc Welfare (2021) 30:30–45. doi:10.1111/ijsw.12435
61. Hussain, D, and Bhushan, B. Posttraumatic Growth Experiences Among Tibetan Refugees: A Qualitative Investigation. Qual Res Psychol (2013) 10:204–16. doi:10.1080/14780887.2011.616623
62. Hussain, D, and Bhushan, B. Posttraumatic Stress and Growth Among Tibetan Refugees: The Mediating Role of Cognitive-Emotional Regulation Strategies. J Clin Psychol (2011) 67:720–35. doi:10.1002/jclp.20801
63. Jibeen, T, and Khalid, R. Predictors of Psychological Well-Being of Pakistani Immigrants in Toronto, Canada. Int J Intercultural Relations (2010) 34:452–64. doi:10.1016/j.ijintrel.2010.04.010
64. Jibeen, T. Moderators of Acculturative Stress in Pakistani Immigrants: The Role of Personal and Social Resources. Int J Intercultural Relations (2011) 35:523–33. doi:10.1016/j.ijintrel.2011.04.002
65. Jibeen, T. Subjective Well-Being of Afghan Refugees in Pakistan: The Moderating Role of Perceived Control in Married Men. Community Ment Health J (2019) 55:144–55. doi:10.1007/s10597-018-0342-9
66. Kim, HK, and Lee, OJ. A Phenomenological Study on the Experience of North Korean Refugees. Nurs Sci Q (2009) 22:85–8. doi:10.1177/0894318408329242
67. Kuttikat, M, Vaillancourt, A, and Massey, M. Battered But Bold: Sri Lankan Tamil Refugee War Experiences, Camp Challenges and Resilience. Int J Migration Health Soc Care (2018) 14:245–59. doi:10.1108/IJMHSC-04-2017-0013
68. Muruthi, BA, Savannah, YS, Chou, JL, Ibrahim, EM, and Janes, EE. 'We Pray as a Family': The Role of Religion for Resettled Karen Refugees. J Fam Issues (2020) 41:3. doi:10.1177/0192513X20911068
69. Lavie-Ajayi, M, and Slonim-Nevo, V. A Qualitative Study of Resilience Among Asylum Seekers From Darfur in Israel. Qual Soc Work: Res Pract (2017) 16:825–41. doi:10.1177/1473325016649256
70. Lee, J, Hong, J, Zhou, Y, and Robles, G. The Relationships between Loneliness, Social Support, and Resilience Among Latinx Immigrants in the United States. Clin Soc Work (2020) 48:99–109. doi:10.1007/s10615-019-00728-w
71. Lenette, C, Brough, M, and Cox, L. Everyday Resilience: Narratives of Single Refugee Women With Children. Qual Soc Work: Res Pract (2013) 12:637–53. doi:10.1177/1473325012449684
72. Lim, SH, and Han, SS. A Predictive Model on North Korean Refugees' Adaptation to South Korean Society: Resilience in Response to Psychological Trauma. Asian Nurs Res (2016) 10:164–72. doi:10.1016/j.anr.2016.04.003
73. Liu, J, Mansoor, Y, Johar, J, Kim, S, Sidiqi, A, and Kapoor, V. Strengths-Based Inquiry of Resiliency Factors Among Refugees in Metro Vancouver: A Comparison of Newly-Arrived and Settled Refugees. Soc Sci Med (2020) 263:113243. doi:10.1016/j.socscimed.2020.113243
74. Maria, M, Dimitra, T, Mary, G, Stella, K, Athanasios, N, and Sarafis, P. Depression, Resilience and Post Traumatic Stress Disorder (PTSD) in Asylum-Seeker War Refugees. Mater Sociomed (2021) 33:26–9. doi:10.5455/msm.2021.33.26-29
75. Mahonen, TA, Leinonen, E, and Jasinskaja-Lahti, I. Met Expectations and the Wellbeing of Diaspora Immigrants: A Longitudinal Study. Int J Psychol : J Int de Psychol (2013) 48:324–33. doi:10.1080/00207594.2012.662278
76. Maung, JN, Johanna, E, Jeevanba, SB, Molitoris, A, Raziuddin, A, and Soheilian, SS. Burmese Refugee Women in the Midwest: Narratives of Resilience and Posttraumatic Growth. Couns Psychol (2021) 49:2. doi:10.1177/0011000020971635
77. Melamed, S, Chernet, A, Labhardt, ND, Probst-Hensch, N, and Pfeiffer, C. Social Resilience and Mental Health Among Eritrean Asylum-Seekers in Switzerland. Qual Health Res (2019) 29:222–36. doi:10.1177/1049732318800004
78. Mwanri, L, Anderson, L, and Gatwiri, K. Telling Our Stories: Resilience During Resettlement for African Skilled Migrants in Australia. Int J Environ Res Public Health (2021) 18:3954. doi:10.3390/ijerph18083954
79. Mera-Lemp, , Maria, J, Martinez-zelaya, G, Orellana, A, and Smith-castro, V. Acculturation Orientations, Acculturative Stress and Psychological Well-Being on Latin American Immigrants Settled in Santiago, Chile. Acta Colombiana de Psicologia (2020) 23:1. doi:10.14718/acp.2020.23.1.11
80. Nam, B, Kim, JY, Devylder, JE, and Song, A. Family Functioning, Resilience, and Depression Among North Korean Refugees. Psychiatry Res (2016) 245:451–7. doi:10.1016/j.psychres.2016.08.063
81. Nashwan, A, Cummings, SM, and Gagnon, K. Older Female Iraqi Refugees in the United States: Voices of Struggle and Strength. Int Soc Work (2019) 62:653–68. doi:10.1177/0020872817742699
82. Novara, C, Scaffidi Abbate, C, Garro, M, and Lavanco, G. The Welfare of Immigrants: Resilience and Sense of Community. J Prev Intervention Community (2021) 50:391–405. doi:10.1080/10852352.2021.1935197
83. Nyarko, F, and Punamäki, RL. The Content and Meaning of War Experiences: A Qualitative Study of Trauma and Resilience Among Liberian Young Refugees in Ghana. Transcultural Psychiatry (2021) 58:1363461520901636. doi:10.1177/1363461520901636
84. Obrist, B, and Buchi, S. Stress as an Idiom for Resilience: Health and Migration Among Sub-Saharan Africans in Switzerland. Anthropol Med (2008) 15:251–61. doi:10.1080/13648470802357596
85. Ogtem-Young, O. Faith Resilience: Everyday Experiences. Societies (2018) 8:10. doi:10.3390/soc8010010
86. Paloma, V, Garcia-Ramirez, M, and Camacho, C. Well-Being and Social Justice Among Moroccan Migrants in Southern Spain. Am J Community Psychol (2014) 54(1-2):1–11. doi:10.1007/s10464-014-9663-1
87. Pearce, EM, Walsh, CA, and Malek, L. Searching for Tomorrow-South Sudanese Women Reconstructing Resilience Through Photovoice. J Int Migration Integration (2017) 18:2. doi:10.1007/s12134-016-0500-2
88. Penman, J, and Goel, K. Coping and Resilience of Rural and Regional Australian Immigrants: Imperatives for Successful Settlement. Rural Soc (2017) 26:178–93. doi:10.1080/10371656.2017.1339406
89. Poudel-Tandukar, K, Chandler, GE, Jacelon, CS, Gautam, B, Bertone-Johnson, ER, and Hollon, SD. Resilience and Anxiety or Depression Among Resettled Bhutanese Adults in the United States. Int J Soc Psychiatry (2019) 65:496–506. doi:10.1177/0020764019862312
90. Rizkalla, N, and Segal, SP. Well-Being and Posttraumatic Growth Among Syrian Refugees in Jordan. J Traumatic Stress (2018) 31:213–22. doi:10.1002/jts.22281
91. Roth, G, and Ekblad, S. A Longitudinal Perspective on Depression and Sense of Coherence in a Sample of Mass-Evacuated Adults From Kosovo. J Nervous Ment Dis (2006) 194:378–81. doi:10.1097/01.nmd.0000217882.70120.38
92. Simich, L, and Andermann, L. Refuge and Resilience: Promoting Resilience and Mental Health Among Resettled Refugees and Forced Migrants. New York: Springer Dordrecht (2014). p. 226.
93. Simkin, H. The Centrality of Events, Religion, Spirituality, and Subjective Well-Being in Latin American Jewish Immigrants in Israel. Front Psychol (2020) 11:576402. doi:10.3389/fpsyg.2020.576402
94. Simsir Zd, B, and Kozan, HIO. Posttraumatic Growth Experiences of Syrian Refugees After War. J Humanistic Psychol (2021) 61:1. doi:10.1177/0022167818801090
95. Skalisky, J, Wanner, S, Howe, B, and Mauseth, K. Religious Coping, Resilience, and Involuntary Displacement: A Mixed-Methods Analysis of the Experience of Syrian and Palestinian Refugees in Jordan. Psychol Religion Spirituality (2020) 14:539–47. doi:10.1037/rel0000390
96. Smit, R, and Rugunanan, P. Transnational Forced Migration and Negotiating Emotional Well-Being: The Case of Women Refugees in South Africa. Soc Dyn (2015) 41:184–203. doi:10.1080/02533952.2015.1029749
97. Solberg, Ø, Sengoelge, M, Nissen, A, and Saboonchi, F. Coping in Limbo? The Moderating Role of Coping Strategies in the Relationship Between Post-Migration Stress and Well-Being During the Asylum-Seeking Process. Int J Environ Res Public Health (2021) 18:1004. doi:10.3390/ijerph18031004
98. Sossou, M-A, Craig, CD, Ogren, H, and Schnak, M. A Qualitative Study of Resilience Factors of Bosnian Refugee Women Resettled in the Southern United States. J Ethnic Cult Divers Soc Work: Innovation Theor Res Pract (2008) 17(4):365–85. doi:10.1080/15313200802467908
99. Ssenyonga, J, Olema, DK, and Owens, V. Posttraumatic Growth, Resilience, and Posttraumatic Stress Disorder (PTSD) Among Refugees. World Conf Psychol Sociol (2013) 82:144–8. doi:10.1016/j.sbspro.2013.06.238
100. Subedi, A, Edge, DS, Goldie, CL, and Sawhney, M. Resettled Bhutanese Refugees in Ottawa: What Coping Strategies Promote Psychological Well-Being? Can J Nurs Res (2019) 51:168–78. doi:10.1177/0844562119828905
101. Taher, R, and Allan, T. Posttraumatic Growth in Displaced Syrians in the UK: A Mixed-Methods Approach. J Loss Trauma (2020) 25:333–47. doi:10.1080/15325024.2019.1688022
102. Taylor, S, Charura, D, Cohen, E, Meth, F, Allan, J, Williams, G, et al. Loss, Grief, and Growth: An Interpretative Phenomenological Analysis of Experiences of Trauma in Asylum Seekers and Refugees. Traumatology (2020). doi:10.1037/trm0000250
103. Thomas-Taylor, D, and Cerulli, C. Use of Nonmedical and Pediatric Primary Care Medical Services by Families Who Call Police for Domestic Violence-Related Issues. Violence against Women (2011) 17:1409–20. doi:10.1177/1077801211428901
104. Tippens, JA. Urban Congolese Refugees in Kenya: The Contingencies of Coping and Resilience in a Context Marked by Structural Vulnerability. Qual Health Res (2017) 27:1090–103. doi:10.1177/1049732316665348
105. Tippens, JA, Roselius, K, Padasas, I, Khalaf, G, Kohel, K, Mollard, E, et al. Cultural Bereavement and Resilience in Refugee Resettlement: A Photovoice Study With Yazidi Women in the Midwest United States. Qual Health Res (2021) 31:1486–503. doi:10.1177/10497323211003059
106. Tonsing, KN. Exploratory Study of Personal Wellbeing of Burmese Refugees in the United States. J Ethnic Cult Divers Soc Work: Innovation Theor Res Pract (2020) 31:329–40. doi:10.1080/15313204.2020.1827335
107. Udah, H, Singh, P, Hölscher, D, and Cartmel, J. Experiences of Vulnerability and Sources of Resilience Among Immigrants and Refugees. Australas Rev Afr Stud (2019) 40:81–100. doi:10.22160/22035184/ARAS-2019-40-1/81-100
108. Udwan, G, Leurs, KHA, and Alencar, A. Digital Resilience Tactics of Syrian Refugees in the Netherlands: Social Media for Social Support, Health, and Identity. Soc Media + Soc (2020) 6:205630512091558. doi:10.1177/2056305120915587
109. Uy, KK, and Okubo, Y. Reassembling a Shattered Life: A Study of Posttraumatic Growth in Displaced Cambodian Community Leaders. Asian Am J Psychol (2018) 9:47–61. doi:10.1037/aap0000111
110. Young, SS, Muruthi, BA, Chou, JL, and Chevalier, M. Feminist Borderland Theory and Karen Refugees: Finding Place in the Family. J Feminist Fam Ther Int Forum (2018) 30:155–69. doi:10.1080/08952833.2017.1391031
111. Walther, L, Amann, J, Flick, U, Ta, TMT, Bajbouj, M, and Hahn, E. A Qualitative Study on Resilience in Adult Refugees in Germany. BMC Public Health (2021) 21:828. doi:10.1186/s12889-021-10817-6
112. Welsh, EA, and Brodsky, AE. After Every Darkness Is Light: Resilient Afghan Women Coping With Violence and Immigration. Asian Am J Psychol (2010) 13:163–74. doi:10.1037/a0020922
113. Kira, IA, Lewandowski, L, Templin, T, Ramaswamy, V, Ozkan, B, Hammad, A, et al. The Mental Health Effects of Retributive Justice: The Case of Iraqi Refugees. J Muslim Ment Health (2006) 1:145–69. doi:10.1080/15564900600980756
114. Thomas, FC, Roberts, B, Luitel, NP, Upadhaya, N, and Tol, WA. Resilience of Refugees Displaced in the Developing World: A Qualitative Analysis of Strengths and Struggles of Urban Refugees in Nepal. Conflict and Health (2011) 5:20. doi:10.1186/1752-1505-5-20
115. Copping, A, and Shakespeare-Finch, J. Trauma and Survival in African Humanitarian Entrants to Australia. In: K Gow, and M Celinski, editors. Mass Trauma: Impact and Recovery Issues. Natural Disaster Research, Prediction and Mitigation. NY: Nova Science Publishers (2013). p. 331–47.
116. Ochu, AC, Davis, EB, Magyar-Russell, G, O'Grady, KA, and Aten, JD. Religious Coping, Dispositional Forgiveness, and Posttraumatic Outcomes in Adult Survivors of the Liberian Civil War. Spirituality Clin Pract (2018) 5:104–19. doi:10.1037/scp0000163
117. Lim, MS, Carrotte, ER, and Hellard, ME. The Impact of Pornography on Gender-Based Violence, Sexual Health and Well-Being: What Do We Know? J Epidemiol Community Health (2016) 70:3–5. doi:10.1136/jech-2015-205453
118. Lewis, SE. Trauma and the Making of Flexible Minds in the Tibetan Exile Community. Ethos (2013) 41:313–36. doi:10.1111/etho.12024
119. Araya, M, Chotai, J, Komproe, IH, and Jong, JT. Quality of Life After Postconflict Displacement in Ethiopia: Comparing Placement in a Community Setting With That in Shelters. Soc Psychiatry Psychiatr Epidemiol (2011) 46:585–93. doi:10.1007/s00127-010-0223-1
120. Arnetz, J, Rofa, Y, Arnetz, B, Ventimiglia, M, and Jamil, H. Resilience as a Protective Factor Against the Development of Psychopathology Among Refugees. J Nervous Ment Dis (2013) 201:167–72. doi:10.1097/NMD.0b013e3182848afe
122. Thomas, T. Stress, Coping, and the Mental Health of Older Vietnamese Migrants. Aust Psychol (1999) 34:82–6. doi:10.1080/00050069908257433
123. Simich, L, Este, D, and Hamilton, H. Meanings of Home and Mental Well-Being Among Sudanese Refugees in Canada. Ethn Health (2010) 15:199–212. doi:10.1080/13557851003615560
124. Sossou, MA. Refugees' Life Transitions From Displacement to Durable Resettlement. In: TW Miller, editor. Handbook of Stressful Transitions across the Lifespan. NY: Springer (2010). p. 465–84.
125. Hussain, D, and Bhushan, B. Cultural Factors Promoting Coping Among Tibetan Refugees: A Qualitative Investigation. Ment Health Religion Cult (2011) 14:575–87. doi:10.1080/13674676.2010.497131
126. Birman, D, Simon, CD, Chan, WY, and Tran, N. A Life Domains Perspective on Acculturation and Psychological Adjustment: A Study of Refugees From the Former Soviet Union. Am J Community Psychol (2014) 53:60–72. doi:10.1007/s10464-013-9614-2
127. Snyder, CR. The Psychology of Hope: You Can Get There From Here. New York: Free Press (1994). p. 409.
128. Seguin, M, and Roberts, B. Coping Strategies Among Conflict-Affected Adults in Low and Middle-Income Countries: A Systematic Literature Review. Glob Public Health (2017) 12:811–29. doi:10.1080/17441692.2015.1107117
129. Zimmerman, C, Kiss, L, and Hossain, M. Migration and Health: A Framework for 21st Century Policy-Making. PLOS Med (2011) 8:e1001034. doi:10.1371/journal.pmed.1001034
130. Porter, M, and Haslam, N. Predisplacement and Postdisplacement Factors Associated With Mental Health of Refugees and Internally Displaced Persons: A Meta-Analysis. J Am Med Assoc (2005) 294:602–12. doi:10.1001/jama.294.5.602
131. Chen, W, Hall, BJ, Ling, L, and Renzaho, AM. Pre-Migration and Post-Migration Factors Associated With Mental Health in Humanitarian Migrants in Australia and the Moderation Effect of Post-Migration Stressors: Findings From the First Wave Data of the BNLA Cohort Study. Lancet Psychiatry (2017) 4:218–29. doi:10.1016/S2215-0366(17)30032-9
Keywords: resilience, hope, opportunities, transnational migrants, refugees
Citation: Lindert J, Samkange-Zeeb F, Jakubauskiene M, Bain PA and Mollica R (2023) Factors Contributing to Resilience Among First Generation Migrants, Refugees and Asylum Seekers: A Systematic Review. Int J Public Health 68:1606406. doi: 10.3389/ijph.2023.1606406
Received: 17 July 2023; Accepted: 07 November 2023;
Published: 11 December 2023.
Edited by:
Sonja Merten, Swiss Tropical and Public Health Institute, SwitzerlandReviewed by:
Afona Chernet, Swiss Tropical and Public Health Institute, SwitzerlandCopyright © 2023 Lindert, Samkange-Zeeb, Jakubauskiene, Bain and Mollica. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jutta Lindert, jutta.lindert@hs-emden-leer.de
This Review is part of the IJPH Special Issue “Migration Health Around the Globe—A Construction Site With Many Challenges.”
 Jutta Lindert
Jutta Lindert Florence Samkange-Zeeb3
Florence Samkange-Zeeb3