Treatment of recurrent acute tonsillitis—a systematic review and clinical practice recommendations
- 1Department of Otorhinolaryngology, Jena University Hospital, Jena, Germany
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Research Program in Systems Oncology, University of Helsinki and Helsinki University Hospital, Helsinki, Finland
- 3Department of Otolaryngology, Head and Neck Surgery, Galilee Medical Center, Affiliated with Azrieli Faculty of Medicine, Bar-Ilan University, Safed, Israel
- 4Department Otorhinolaryngology, Head and Neck Surgery, Nottingham University Hospitals, Queens Medical Centre Campus, Nottingham, United Kingdom
- 5ENT Unit, Policlinico Città di Udine, Udine, Italy
- 6Department of Otolaryngology, Head and Neck Surgery, Radboud University Medical Center, Nijmegen, Netherlands
- 7International Head and Neck Scientific Group, Padua, Italy
Background: There is an ongoing debate on the indications for tonsil surgery in both children and adults with recurrent acute tonsillitis. The aim is to provide practical recommendations for diagnostics and treatment for recurrent acute tonsillitis including evidence-based decision making for tonsillectomy.
Methods: A systematic literature search in PubMed, Embase, Web of Science, and ScienceDirect from 2014 until April 2023 resulted in 68 articles. These were the basis for the review and a comprehensive series of consensus statements on the most important diagnostics and indications for both non-surgical and surgical therapy. A consensus paper was circulated among the authors and members of the International Head and Neck Scientific Group until a final agreement was reached for all recommendations.
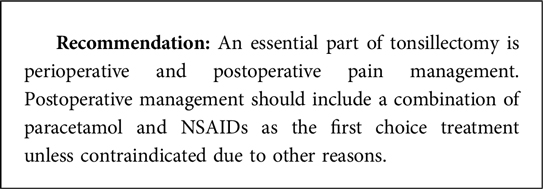
Results: The differentiation between sore throat and tonsillitis patient episodes is mostly not feasible and hence is not relevant for diagnostic decision making. Diagnostics of a tonsillitis/sore throat episode should always include a classification with a scoring system (Centor, McIssac, FeverPAIN score) to estimate the probability of a bacterial tonsillitis, mainly due to group A streptococcus (GAS). In ambiguous cases, a point-of-care test GAS swab test is helpful. Consecutive counting of the tonsillitis/sore throat episodes is important. In addition, a specific quality of life score (Tonsillectomy Outcome Inventory 14 or Tonsil and Adenoid Health Status Instrument) should be used for each episode. Conservative treatment includes a combination of paracetamol and/or non-steroidal anti-inflammatory drugs. In case of high probability of bacterial tonsillitis, and only in such cases, especially in patients at risk, standard antibiotic treatment is initiated directly or by delayed prescription. Tonsillectomy is indicated and is highly effective if the patient has had ≥7 adequately treated episodes in the preceding year, ≥5 such episodes in each of the preceding 2 years, or ≥3 such episodes in each of the preceding 3 years. An essential part of surgery is standardized pain management because severe postoperative pain can be expected in most patients.
Conclusion: It is necessary to follow a stringent treatment algorithm for an optimal and evidence-based treatment for patients with recurrent acute tonsillitis. This will help decrease worldwide treatment variability, antibiotic overuse, and avoid ineffective tonsillectomy.
Introduction
Group A β-hemolytic streptococcus (GAS) is responsible for 5%–15% of sore throat visits in adults and 20%–30% in children (1). Pediatric streptococcal pharyngitis (or tonsillitis) in the US costs an estimated $224–$539 million per year, including indirect costs related to parental work losses (2). Accurate diagnosis and appropriate antimicrobial therapy for streptococcal pharyngitis/tonsillitis are important to prevent acute rheumatic fever and suppurative complications, improve symptoms, decrease contagiousness, reduce transmission, and minimize the adverse effects of inappropriate antimicrobial therapy. However, the signs and symptoms of GAS and non-streptococcal pharyngitis and/or tonsillitis overlap, making clinical diagnosis impossible. Antimicrobial therapy is of no proven benefit for acute pharyngitis/tonsillitis caused by organisms other than GAS. Physicians must exclude the diagnosis of GAS pharyngitis to prevent inappropriate administration of antimicrobials and the development of antimicrobial resistance among common pathogens (3). If a patient has repeated GAS pharyngitis/tonsillitis, the treatment decision becomes even more difficult.
The debate on the optimal treatment and surgical indications for recurrent acute tonsillitis is still ongoing. An important parameter for decision making is the number of bacterial tonsillitis episodes the patient had in the preceding year or years, taking into account the social, work, or educational absence or alteration to life each episode has had. Here the questions start: How best to count these episodes? How do we know which episodes were caused by a bacterial infection or not? How do we know that it was a tonsillitis and not just an acute laryngopharyngitis? Hence, the indication for or against surgery is based on non-reliable criteria. On the other hand, hard outcome criteria are also difficult to define. There is no objective measurement that directly correlates with the severity of tonsil inflammation. Most clinical trials that have defined the indication for tonsil surgery based on tonsillitis episodes have used cumulated sore throat episodes over time after surgery as outcome criterion (4–6). Here, the problem is the same: When does a sore throat episode start? All these issues together might explain why it has been so difficult in the past to prove with a high level of evidence whether tonsil surgery is effective in severe cases of recurrent acute tonsillitis (5). These (unclear) benefits of surgery have to be balanced against the risk of surgery. Worldwide, the surgical standard for the treatment of recurrent acute tonsillitis is tonsillectomy. Tonsillectomy has a relevant postoperative complication risk, including bleeding. Overall, the frequency of readmission for post-tonsillectomy hemorrhage is about 2%–7%, and the reoperation rate for hemostasis is about 1%–2% (7–9). Although rare, some patients even die due to bleeding after tonsillectomy (three to seven deaths per 100,000 tonsillectomies) (10, 11). Furthermore, tonsillectomy is one of the most painful procedures, even more painful than large abdominal surgeries (12, 13). This is why it is currently investigated if tonsillotomy, i.e., a procedure with much less morbidity and only minor pain, is as effective to treat recurrent acute tonsillitis in children and adults (14).
The review presented here gives an overview about the current knowledge on recurrent acute tonsillitis and provides recommendations for optimal diagnostics and treatment of children and adult patients with recurrent acute tonsillitis.
Material and methods
Search and consensus strategy
As a starting point, a careful review was done on the current clinical guidelines (Supplementary Table S1). This was followed by a systematic review conducted in three steps in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guideline (15). We conducted a systematic literature search for the publications in English language since 2014 in PubMed, Embase, Web of Science, and ScienceDirect databases. The year 2014 was chosen, because all relevant literature older than 2014 were evaluated in the German clinical guideline on tonsillitis treatment in children and adults (16). The following MeSH terms were used: “tonsillitis”, “Recurrence”, “Humans”, “Tonsillitis* / surgery”, “Tonsillitis* / therapy”, “Tonsillectomy* / adverse effects”, “Tonsillitis* / epidemiology”, “Quality of life”, “Child”, “Adult”, “Palatine tonsil”, “Sore throat”, and “humans” (period: 2008–2022; last search on May 5, 2022). Our research retrieved 314 records. In agreement with the PRISMA guidelines (15), we reported the results using the PICOST-DS tool (17): Participants: all ages, recurrent acute tonsillitis; intervention: any kind of intervention: drug therapy, non-surgical therapy, and surgical therapy; comparator: not needed; outcomes: no restriction; time: no limits of the time; setting: outpatients and inpatients; and study design: all designs studies. Finally, a total of 68 studies were included in the present review based on relevance and scientific evidence. A flow diagram of the research is reported in the Supplementary Material (Supplementary Figure S1).
Recommendation assessment
The highest level of evidence reached the level of retrospective observational cohort studies (Oxford Centre for Evidence-based Medicine Level III–IV). Due to the lack of higher quality evidence, the presented recommendations reached the level of recommendation B, i.e., considerable benefit substantiated by non-first-class evidence, according to international standards and the Association of the Scientific Medical Societies guidelines (18). The most important diagnostic tests and treatment options were discussed in-depth and a consensus was proposed. Based on the evidence of the literature, a proposal for all recommendations was written by the first author. All authors made comments on each recommendation and were able to view the comments of all authors in the process. Based on the first round of comments, the recommendations were revised by the first authors. Again, the recommendations circulated among the authors to give another opportunity to comment. Based on the second round of comments, the recommendations were revised again by the first author. All authors finally agreed with the formulations. In total, the articles were circulated among all authors for three rounds until a consensus was reached for all recommendations. A strong consensus (100% of all eight authors) was reached for all recommendations based on the Delphi process.
Results
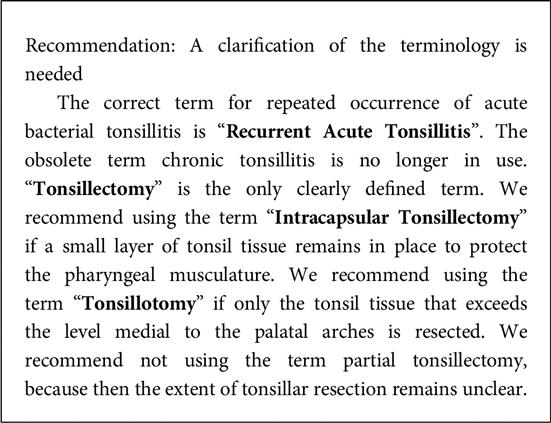
Definition of recurrent acute tonsillitis and tonsil surgery
“Recurrent acute tonsillitis” is the repeated distinct time period or episodes of acute bacterial infections of the palatine tonsils with symptom-free or symptom-poor intervals. It has to be emphasized that the term is restricted to the palatine tonsils and assumes a bacterial origin of the tonsillitis episodes. This has to be differentiated from the terms “sore throat” and “pharyngitis” which are frequently used interchangeably. Sore throat describes a painful irritation of the throat independent of an obvious etiology. In real life and for decision making, a differentiation between an episode of sore throat and an episode of tonsillitis is often not possible. Tonsillectomy is defined as complete removal of the palatine tonsils, including its capsule, by dissecting the peritonsillar space between the tonsil capsule and the muscular wall (19). In case of intracapsular or partial tonsillectomy, all tonsil tissue is removed, but a small remnant layer is retained (the “capsule”) to protect the underlying muscles. The term tonsillotomy is sometimes used synonymously to report the use of partial tonsillectomy. Alternatively, tonsillotomy is used to describe cutting through the tonsil at the level of the palatal arches, i.e., all tonsil tissue beyond this level is left in place.
Pathophysiology of recurrent acute tonsillitis
The palatine tonsils are part of Waldeyer's ring and belong to the mucosa-associated lymphoid tissue (MALT) (20). A pathologist reporting on an excised normal palatine tonsil, i.e., a tonsil of a person who never had problems with this organ, would find many inflammatory cells, different sets of leukocytes including neutrophils, or granulocytes. The pathologist would thus report an inflammation of the tonsil. This inflammation of the tonsil reflects its physiological function. This inflammatory process only becomes a disease, when this physiological—local—inflammation is accompanied by a viral or bacterial infection with clinical symptoms. The predominant reason for a bacterial infection is symptomatic cases of GAS tonsillitis (21). Depending on the region, bacteria like Streptococcus dysgalactiae subsp. equisimilis, Fusobacterium necrophorum, and others can also be found in adolescents and young adults with tonsillitis symptoms (22). The patient has recurrent acute tonsillitis when she/he develops further episodes of acute bacterial tonsillitis with symptom-free or symptom-poor intervals after the first bacterial tonsillitis.
Epidemiology of recurrent acute tonsillitis
Acute (and mainly viral) tonsillitis is a frequent disease, said to account for about one-third of all respiratory tract infections treated in primary care (23). Exact numbers are difficult to obtain, with all the previously mentioned difficulties of definition and unreliable diagnostic criteria. Despite these circumstances, it is estimated that 600 million symptomatic GAS cases are diagnosed worldwide each year (21). About one among 10 of these patients develop recurrent acute tonsillitis. Nevertheless, it affects hundreds of thousands of children and young adults every year. The prevalence of recurrent episodes is about 12% in patients with tonsillitis, i.e., about 12,000 per 100,000 individuals having had at least one tonsillitis episode before (24).
Risk factors for recurrent acute tonsillitis
A GAS infection as a cause of a tonsillitis episode is the only known hard risk factor for the development of recurrent acute tonsillitis (25). Recurrent acute tonsillitis could be a genetic immunosusceptibility disease because it is reported that patients younger than 12 years with recurrent acute tonsillitis show some (otherwise subclinical) antibody deficiency and aberrant T-cell function (26).
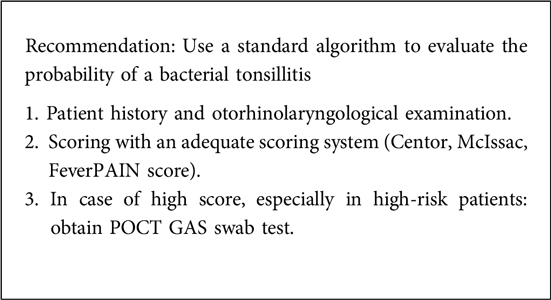
Clinical assessment of recurrent acute tonsillitis
Viral and bacterial infections have the same unspecific clinical symptoms like sore throat with or without fever. The clinical differentiation is often not possible. Furthermore, there is no examination that allows one to differentiate between a patient with acute tonsillitis, acute pharyngitis without tonsillitis (if this really exists), tonsillopharyngitis, or laryngopharyngitis. Therefore, many physicians prefer to ambiguously define it as “sore throat.” The number of bacterial tonsillitis episodes is currently the most important parameter to determine the indication for or against tonsillectomy. Therefore, the proof that the patient has another episode of bacterial tonsillitis is important. Empirically, about 70% of the cases are viral infections, and about 30% have a bacterial etiology (27). The probability in children is higher than in adults. As most of the bacterial infections are caused by GAS, the proof of a GAS-related tonsillitis is important.
The mostly used clinical scoring systems are only validated for GAS infections and patients with sore throat, i.e., not explicitly designed for patients with acute tonsillitis (Table 1). The scoring systems only allow a gross estimation of the probability of a bacterial tonsillitis. If the patients have a high score (Centor score 3–4 points; McIsaac score: 3–4 points; or FeverPAIN score: 3–5 points), the standard approach then, especially in high-risk patients, is to perform a fast point-of-care test (POCT) swab test. Modern POCTs have a high sensitivity and specificity comparable with time-consuming standard laboratory testing (28, 29). Nevertheless, one should be aware that children can be asymptomatic GAS carriers (30). Physicians who wish to ensure maximal sensitivity in diagnosis when the patient has a negative POCT test but relevant symptoms or even worsening symptoms may repeat the POCT test or continue to use conventional throat culture with standard laboratory testing (3). In any case, if the initial scoring indicated an uncomplicated tonsillitis and the patient's condition worsens, re-evaluation should be considered after 3 days.
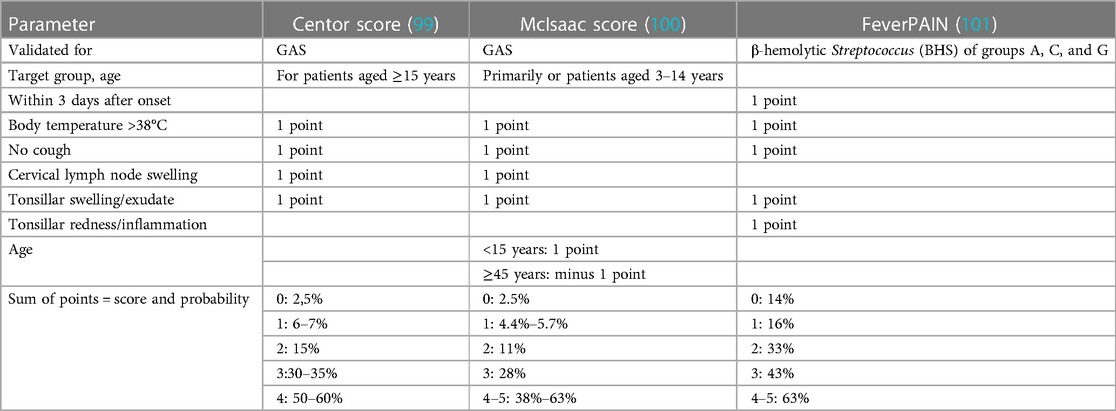
Table 1. Most important scores for prediction of a Streptococcus infection in patients with sore throat.
A newer optional but practical approach is to begin with symptomatic treatment, for instance, with adequate dose of rapid-acting paracetamol directly in the office/clinic (22). If this does not have an effect within 15–30 min, a fast POCT swab test should be used.
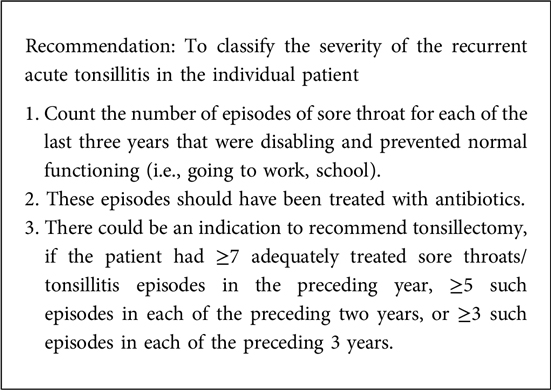
Classification of the severity of recurrent acute tonsillitis
It was unclear until recently if a tonsillectomy is effective in patients suffering from severe recurrent acute tonsillitis. The Cochrane review from 2014 based on seven trials (five in children and two in adults; Table 2) revealed that good information about the effectiveness of tonsillectomy (with/without adenoidectomy) was only available for the first year following surgery in children and for 5–6 months in adults (6). Children had a small benefit from surgery: children who had surgery had three episodes of sore throat on average compared to 3.6 episodes experienced by the other children, i.e., 0.6 episodes of any type of sore throat in the first year was avoided. In adults, conclusions on the effectivity could not be drawn: the two included trials suggested that the number of days with sore throat may be fewer in the first 6 months following tonsillectomy compared to a conservative management. This was the reason why the UK's National Institute for Health Research commissioned the NATTINA trial (6). NATTINA is so far the largest multicenter clinical trial (453 participants randomized) to assess the effectiveness of surgical intervention in adults compared to a conservative management (Table 2). NATTINA represents a new milestone on the importance of tonsillectomy in adults (31). The primary outcome measure was the total number of sore throat days, reported weekly over 24 months (32). It was shown that compared with conventional medical management, tonsillectomy is both clinically effective and cost-effective. Tonsillectomy reduces sore throat days by almost 53% in over 2 years.
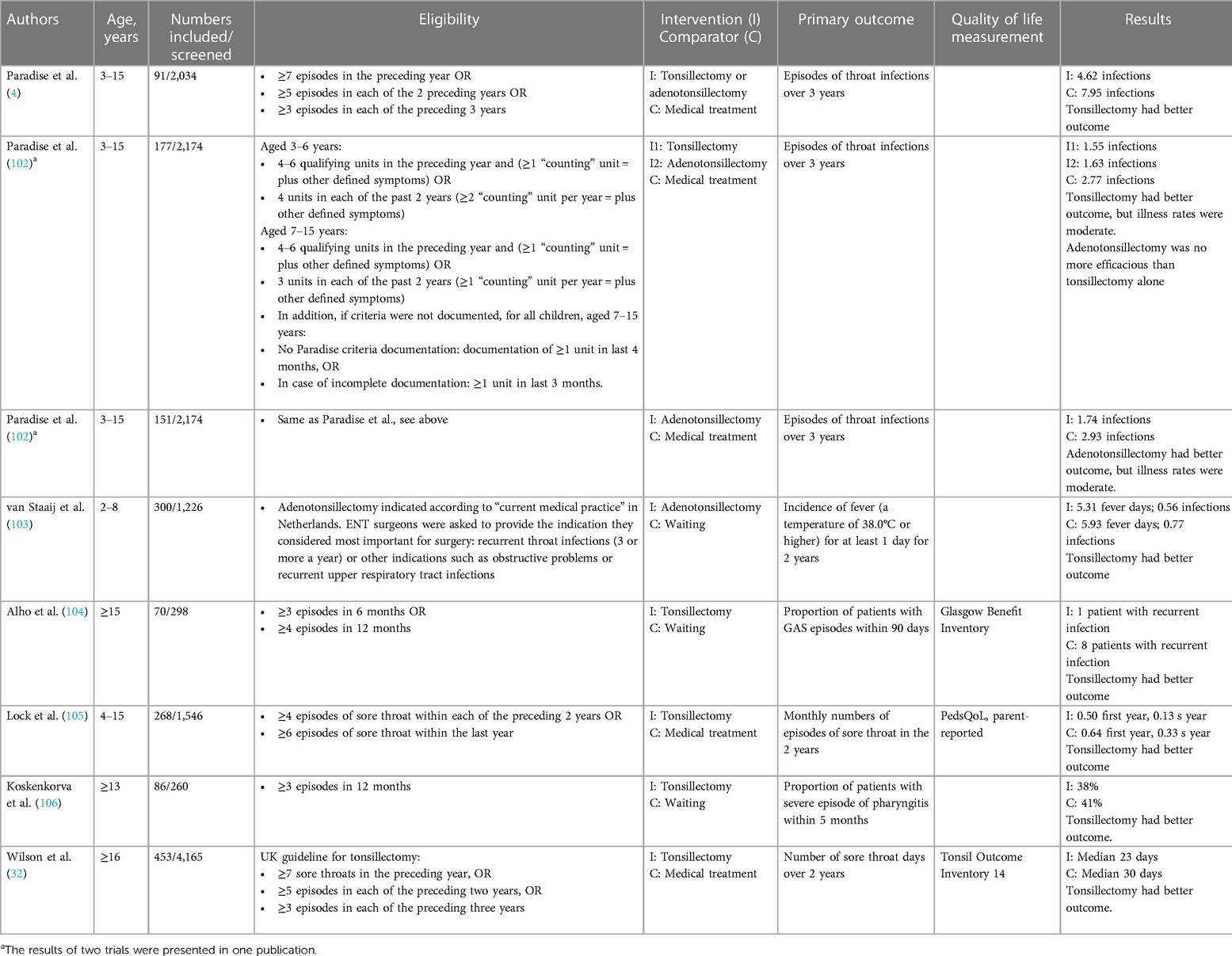
Table 2. Most important randomized controlled clinical trials analyzing the efficacy of tonsil surgery compared to a control group.
Based on the main NATTINA result that tonsillectomy is more beneficial mainly for severe cases of recurrent acute tonsillitis, current clinical guidelines recommend tonsillectomy if the patient experiences at least five to seven sore throat episodes within 1–2 years (Supplementary Table S2). For example, the German guideline explicitly requires episodes of acute tonsillitis. In addition to the number of episodes, nearly all guidelines require additional parameters to substantiate the severity and a high probability that the episodes were episodes of bacterial tonsillitis. The NATTINA trial probably will define the new standard to count the number of episodes, i.e., following the UK guideline (cf. Table 2 and Supplementary Table S2).
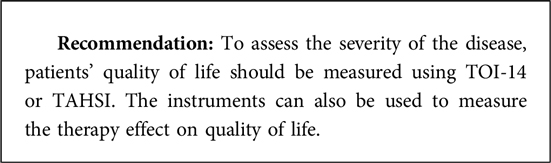
To allow a better estimation of the disease burden, a quality of life assessment should be performed. The most frequently used generic questionnaire is the Glasgow Benefit Inventory (GBI) (33). It is used to report change in quality of life after surgery. The PedsQL is another generic tool frequently especially used for children (34). Specific questionnaires are the Tonsillectomy Outcome Inventory 14 (TOI-14) and the Tonsil and Adenoid Health Status Instrument (TAHSI) (35, 36). Both the TOI-14 and the TAHSI were designed to assess the disease-specific quality of life for patients with recurrent or chronic tonsillitis. Both questionnaires are partly validated in several languages for adults and children (English, Spanish, German, Arabic, Finnish) (37–40). The benefit of tonsillectomy in gaining quality of life is higher in patients with higher number of tonsillitis episodes before surgery (41, 42).
Therapy of recurrent acute tonsillitis
There are three treatment options: watchful waiting, drug therapy, or tonsillectomy. A decision is made based on the evaluation of the severity of the recurrent acute tonsillitis. If the patient has an apparently uncomplicated episode, is immunocompetent, not comorbid, and has a low score (Centor, McIsaac, FeverPAIN, see above), waiting or symptomatic treatment is indicated. In comorbid or critically ill patients, one should lean toward recommending POCT for GAS (22). Identification of patients with risk for severe disease course is important. Conditions are severe immunosuppression, such as long-term use of systemic steroids, organ transplantation, stem cell transplantation, AIDS, neutropenia, and other congenital or acquired immune defects, or severe comorbidities (43).
Peritonsillar abscess, or quinsy, is a relevant complication of acute bacterial tonsillitis. The annual incidence rates are in the range of 9–41 cases in a population of 100,000 (44). Whether the risk for a peritonsillar abscess is higher in patients with recurrent acute tonsillitis is unclear. Some studies describe higher risks, and others report that patients with peritonsillar abscess have less likely a history of recurrent acute tonsillitis (44–46). This means that the risk of peritonsillar abscess cannot be considered a standalone argument for or against a particular therapy for recurrent acute tonsillitis.
If POCT is unavailable, antibiotic treatment is recommended in these subgroups of patients. In patients with high score and poor effect on fast-acting symptomatic analgesics (see above), one would consider antibiotics in the presence of GAS due to POCT. Finally, in case of severe recurrent tonsillitis based on the number of tonsillitis episodes, tonsil surgery should be recommended.
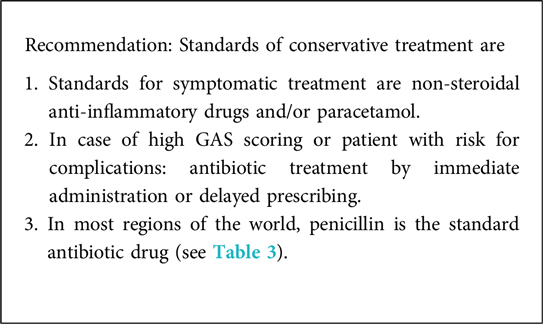
Conservative treatment
Standards for symptomatic treatment are non-steroidal anti-inflammatory drugs and paracetamol (43). If the situation worsens after 2 days or if there is no noticeable improvement over 8 days, the patient should come back for re-evaluation (22). Due to the limited effect of oral or intramuscular corticosteroids in reducing the pain, we do not recommend the use of corticosteroids (47). The US Food and Drug Administration (FDA) issued a black box warning for codeine and tramadol in children younger than 12 years and limited use in children between 12 and 18 years of age owing to difficulty breathing and death (48).
In case of a high score (Centor, McIsaac, FeverPAIN; see Table 1 and above) and a positive GAS POCT when required (see above), antibiotic treatment can be considered. The patient or the caregivers should know that the primary goal of antibiotic treatment is to shorten the duration of the disease rather than to prevent complications (43, 49). Several studies show that antibiotics reduce acute symptoms more frequently in patients if GAS was present (22). The patient or the caregivers should also know that these benefits have to be balanced against drug reactions like diarrhea, anaphylaxis, and mycoses occurring in up to 10% of the patients (43). In patients with an intermediate score, a delayed prescribing can be performed, i.e., issuing of the prescription is only redeemed by the patient if symptoms worsen or do not improve after 3–5 days (50). The recommended antibiotics, either by immediate administration or delayed prescribing, are listed in Table 3. Penicillin is the antibiotic of choice. There is no clear evidence that other antibiotics are more effective than penicillin in the treatment of an episode of recurrent GAS-related tonsillitis (51–53).
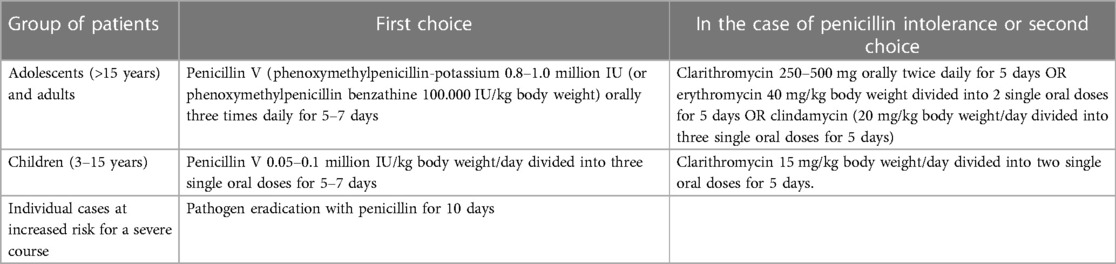
Table 3. Examples for antibiotic treatment of an acute tonsillitis episode probably related to a GAS infection.
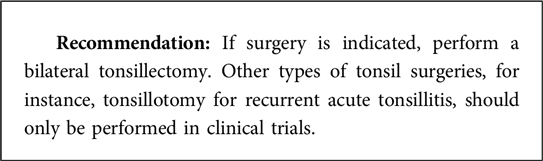
Surgical treatment
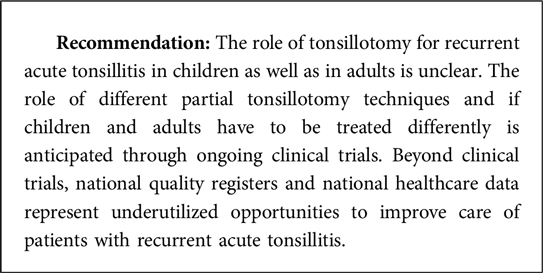
Surgery is indicated for severe cases of recurrent acute tonsillitis. The severity has to be classified as described above. Surgery is indicated based on a clear cut-off number of acute tonsillitis episodes (see above). Standard surgery is bilateral tonsillectomy. The recently published NATTINA trial has confirmed the efficacy and also the cost-effectiveness of tonsillectomy in adults with severe recurrent acute tonsillitis (32). Only the German guideline offers as alternative a tonsillotomy in case of tonsil with a size >Brodsky grade 1 (16, 54). We do not recommend performing tonsillotomy or any other kind of partial tonsillectomy outside from clinical trials. So far, the evidence that tonsillotomy is as effective as tonsillectomy for recurrent acute tonsillitis is unproven (55). In the treatment of sleep-related disorders, this is different for children. Here, partial tonsillectomy/tonsillotomy is recommended as an alternative to tonsillectomy in many countries. It is important to distinguish between the two indications, sleep-related disorders and recurrent acute tonsillitis.
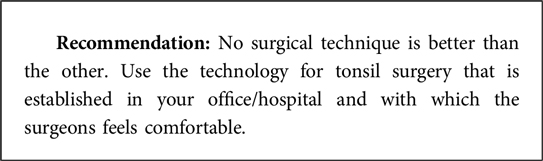
Surgical techniques
The most frequent and traditional method of tonsillectomy is with metal surgical instruments (cold steel tonsillectomy; tonsillectomy by cold dissection or with a snare/guillotine). Due to the relevant risk of primary and secondary postoperative bleeding and because of moderate to severe pain for up to weeks after surgery, other techniques are being used for decades with the aim to reduce the risk of postoperative bleeding and severe pain (56). Alternative techniques are bipolar radiofrequency ablation (coblation), bipolar electrodissection (electrocauterization, electrocautery), harmonic scalpel, microdebrider-assisted partial tonsillectomy, diathermy, laser surgery, and cryosurgery. Tonsillectomy by cold dissection and also the alternative techniques are more or less used for total tonsillectomy as well as for partial tonsil surgery. The current evidence remains low regarding any of the alternative techniques having advantages over traditional tonsillectomy (56). Most trials do not differentiate clearly between the indications (recurrent acute tonsillitis vs. tonsillar hypertrophy) and the extent of tonsil surgery (56). Population-based data do not report an advantage for alternative techniques (7, 57, 58). It is important to separate the question of the best technique from the extent of surgery. There is a consensus that any partial type of tonsil surgery, especially tonsillotomy, has a lower postoperative bleeding rate and produces less postoperative pain (8, 59, 60). Hence, any technique used for partial tonsillectomy and tonsillotomy has a lower risk of postoperative bleeding and severe pain.
Postoperative pain management
Tonsillectomy is ranked among the top 25 procedures with highest pain intensities (12, 61). It is more painful than a number of so-called major abdominal surgeries. Median pain scores are about 5–6 on a 11-part numeric rating scale (NRS 0–10). Typically, a planned pain management is recommended if an NRS >3 can be expected. Nevertheless, there is no consensus for optimal pain management. Moreover, some clinicians still are underestimating the degree of pain associated with tonsillectomy, as they consider it be a minimally invasive surgical procedure. Patients with preoperative chronic pain due to other diseases, females, and young adults are associated with higher postoperative pain intensity (13).
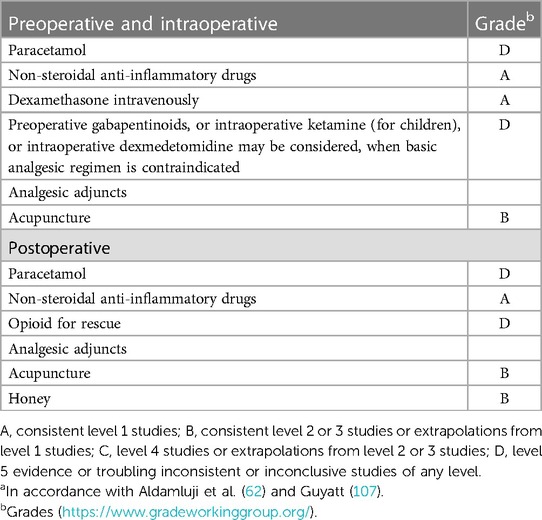
A recent systematic review analyzed preoperative and intraoperative interventions to reduce postoperative pain. Paracetamol (acetaminophen), non-steroidal anti-inflammatory drugs (NSAIDs), intravenous dexamethasone, ketamine (only assessed in children), gabapentinoids, dexmedetomidine, honey, and acupuncture improved postoperative pain. Inconsistent evidence was found for local anesthetic infiltration, antibiotics, and magnesium sulfate. Limited evidence was found for clonidine (62). Mouthwash gargle with benzydamine hydrochloride was not found to be superior to placebo in a recent randomized control trial (63). Evidence-based recommendations for pain management are listed in Table 4. Pain management should be initiated during tonsillectomy. Non-opioid analgesics should be administered intraoperatively. The administration should be continued in the postoperative period, unless contraindications are present (64). Intravenous dexamethasone should be given intraoperatively. The patient can have high pain scores typically for 3–5 days after surgery.
In general, mono-analgesics only have a limited analgesic efficacy in the postoperative setting after tonsillectomy. Therefore, it is recommended to use analgesic in combination (e.g., paracetamol plus NSAIDs). Ibuprofen is widely used as a first choice NSAID (65). There is no evidence that NSAIDs increase the risk of postoperative bleeding (66, 67). The value of intravenous dexamethasone in the postoperative phase is controversial and it is not frequently used (68, 69). Opioids are only recommended as rescue analgesics. Codeine is forbidden in many countries for children and tramadol in some countries too. Especially in the United States, strategies are searched to avoid opioids in consequence of the opioid epidemic (70). Optimal combination of paracetamol plus NSAID might decrease the probability to need opioids as rescue analgesics (71).
The analgesic effect of intraoperative and postoperative acupuncture as well as postoperative honey was investigated (72–74). Acupuncture is rarely provided as it requires specific training. The optimal acupuncture regime has not been defined, yet. More randomized controlled trials are needed to define the risk and combination of most effective drugs for postoperative pain relief after tonsillectomy.
Ongoing clinical trials and clinical registers
After decades without important trials, the NATTINA trial was the start of a series of studies that are still ongoing (Supplementary Table S3). The German TOTO trial is a multicenter, 1:1 two-arm, randomized non-blinded non-inferiority trial (14). The non-inferiority of tonsillotomy compared to tonsillectomy is investigated. Patients ≥3 years of age are randomly allocated to undergo either tonsillotomy or tonsillectomy as surgical treatment of recurrent acute tonsillitis. The primary outcome is the number of sore throat days experienced over the 24-month follow-up. The Finnish FINITE trial investigates the hypothesis that the recovery time from tonsil surgery can be reduced with intracapsular tonsillectomy (75). Adult patients suffering from recurrent or “chronic” tonsillitis are included into a randomized, controlled, three-arm clinical trial. It is designed to compare three different surgical techniques: extracapsular monopolar tonsillectomy, intracapsular microdebrider tonsillectomy, and intracapsular coblation tonsillectomy. The primary endpoint is the recovery time from postoperative pain. Another Finnish multicenter trial compared tonsillectomy, tonsillotomy, and watchful waiting in adult patients with recurrent or “chronic” tonsillitis (76). The primary outcome will be tonsillitis-specific quality of life at 6 months. These trials will give important answers on the efficacy of tonsil surgery in adults and especially if less than total tonsillectomy will be effective.
Concerning clinical registers, the Nordic countries present good examples. In Sweden, the National Tonsil Surgery Register (https://ton.registercentrum.se/) is used since 1997 (77). Such quality registers have also been established in Norway and Denmark since 2016 (78). With the aim to improve the care of patients needing tonsil surgery, these registers allow an ongoing investigation of indications, surgical methods, and complications. In addition, national healthcare data form an important source for quality control of tonsil surgery. For instance, using a national cohort of children from the US American Pediatric Health Information System allowed an analysis of 96,415 children undergoing tonsillectomy between 2016 and 2021 (58). Important variables associated with postoperative bleeding were revealed including a probability model for future quality initiatives.
Discussion
The data of actual clinical trials on a high evidence-based level allowed us to define clear recommendations for the treatment of patients with recurrent acute tonsillitis, most important for the indication of antibiotic treatment and for tonsillectomy. If the patient presents a history of ≤7 sore throats in the preceding year, <5 episodes in each of the preceding 2 years, or <3 episodes in each of the preceding 3 years, and the new episode has a high score (Centor, McIsaac, FeverPAIN), especially when presenting with a positive GAS POCT, antibiotic treatment can be considered. If the patient experiences more episodes, i.e., at least five to seven sore throat episodes within 1–2 years, bilateral tonsillectomy can be recommended as the patient will profit much more from surgery than from another conservative treatment.
Nevertheless, the literature research clearly showed that there are many areas of uncertainty with an urgent need for more objective criteria to define the severity of a recurrent acute tonsillitis. The number of tonsillitis episodes per year cannot be exactly established and, therefore, is a non-reliable inclusion criterion. Furthermore, no reliable preoperative biomarkers are available to predict the outcome of tonsillectomy (45, 79). Machine learning algorithms to classify the clinical optical appearance of the tonsil might suggest or add an alternative solution, but with the number of tonsillitis episodes to train such algorithms, their meaningfulness will be limited (80). Innovative tools allowing a non-invasive cellular and molecular imaging and severity classifying of the tonsils are warranted. This might be a way to classify the severity without removing the tonsils and could spare some unneeded surgeries (81, 82).
The worldwide decline of tonsillectomy is associated with more acute admissions for tonsillitis in some countries (83). There seems to be a correlation between social deprivation and both tonsillectomy and tonsillitis; hence, lower socioeconomic groups are more effected. The reasons for this appear to be multifactorial. We also might need criteria reflecting the burden of the disease on socioeconomic factors, i.e., beyond the current approach of counting of tonsillitis episodes (83).
Finally, there is an ongoing debate on the long-term effects of tonsillectomy, i.e., the removal of a secondary immune organ. Tonsillectomy does not seem to have a negative effect on the immune system, when humoral and cellular immunity is measured after surgery (84–86). During the COVID-19 pandemic, it was speculated that patients who underwent a tonsillectomy might have a higher risk for a more severe course of the SARS-CoV2 infections (87, 88). This has remained so far unproven (89). Several population-based studies have been performed to study the effects of tonsillectomy on later occurrences of other diseases. The risk of pneumonia after tonsillectomy in adults seems not to be increased (90), whereas the risk for later development of an autoimmune disease seems to be slightly increased (91, 92). The list of studies investigating the risk of cancer after prior tonsillectomy seems to be larger: there is a slightly increased risk for breast cancer (93, 94) and Hodgkin’s disease (95). Of interest is a (self-explanatory) lower risk of oropharyngeal cancer (96). However, the causal relation remains unclear. It might be that factors that led to recurrent acute tonsillitis are responsible for this relation and not the tonsillectomy itself (97, 98). Hence, due to several reasons, more long-term studies after tonsillectomy are needed. Register studies might be the best option to harvest long-term data after tonsil surgery.
Conclusion
Recurrent acute tonsillitis worldwide has a high prevalence in children and adults. Each sore throat/tonsillitis episode should be classified by one of the three international scoring systems. In addition, a tonsillitis-specific quality of life score should be used. It is important both to classify the severity of the disease of each new episode and to further guide the need for an additional GAS POCT. These estimations are important requirements to decide for the optimal analgesic regime and, if the probability of a bacterial infection is high, to recommend for an antibiotic treatment. There is high evidence that tonsillectomy decreases the rate of sore throats in the severely affected cases with a high frequency of episodes. It still remains unclear whether or not partial tonsillectomy strategies are as effective, and this will be investigated in the ongoing clinical trials. In case of tonsillectomy, standardized perioperative and postoperative pain management is mandatory.
Author contributions
OG-L: conceptualization and literature review. OG-L and KG: literature analysis and first draft preparation. All authors: Delphi rounds to find a consensus on the recommendations. OG-L, KG, and AF: writing, review, and editing. AF: supervision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2023.1221932/full#supplementary-material
References
1. Ebell MH, Smith MA, Barry HC, Ives K, Carey M. The rational clinical examination. Does this patient have strep throat? JAMA. (2000) 284(22):2912–8. doi: 10.1001/jama.284.22.2912
2. Pfoh E, Wessels MR, Goldmann D, Lee GM. Burden and economic cost of group A streptococcal pharyngitis. Pediatrics. (2008) 121(2):229–34. doi: 10.1542/peds.2007-0484
3. Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. (2012) 55(10):1279–82. doi: 10.1093/cid/cis847
4. Paradise JL, Bluestone CD, Bachman RZ, Colborn DK, Bernard BS, Taylor FH, et al. Efficacy of tonsillectomy for recurrent throat infection in severely affected children. Results of parallel randomized and nonrandomized clinical trials. N Engl J Med. (1984) 310(11):674–83. doi: 10.1056/NEJM198403153101102
5. Burton MJ, Glasziou PP, Chong LY, Venekamp RP. Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database System Rev. (2014) 11:CD001802. doi: 10.1002/14651858.CD001802.pub3
6. Rubie I, Haighton C, O’Hara J, Rousseau N, Steen N, Stocken DD, et al. The NAtional randomised controlled Trial of Tonsillectomy IN Adults (NATTINA): a clinical and cost-effectiveness study: study protocol for a randomised control trial. Trials. (2015) 16:263. doi: 10.1186/s13063-015-0768-0
7. Mueller J, Boeger D, Buentzel J, Esser D, Hoffmann K, Jecker P, et al. Population-based analysis of tonsil surgery and postoperative hemorrhage. Eur Arch Otorhinolaryngol. (2015) 272(12):3769–77. doi: 10.1007/s00405-014-3431-6
8. Ostvoll E, Sunnergren O, Stalfors J. Increasing readmission rates for hemorrhage after tonsil surgery: a longitudinal (26 years) national study. Otolaryngol Head Neck Surg. (2018) 158(1):167–76. doi: 10.1177/0194599817725680
9. Li JC, Forer M, Veivers D. Reference rate for post-tonsillectomy haemorrhage in Australia—a 2000–2020 national hospital morbidity database analysis. PLoS One. (2022) 17(8):e0273320. doi: 10.1371/journal.pone.0273320
10. Ostvoll E, Sunnergren O, Ericsson E, Hemlin C, Hultcrantz E, Odhagen E, et al. Mortality after tonsil surgery, a population study, covering eight years and 82,527 operations in Sweden. Eur Arch Otorhinolaryngol. (2015) 272(3):737–43. doi: 10.1007/s00405-014-3312-z
11. Edmonson MB, Zhao Q, Francis DO, Kelly MM, Sklansky DJ, Shadman KA, et al. Association of patient characteristics with postoperative mortality in children undergoing tonsillectomy in 5 US States. JAMA. (2022) 327(23):2317–25. doi: 10.1001/jama.2022.8679
12. Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiol. (2013) 118(4):934–44. doi: 10.1097/ALN.0b013e31828866b3
13. Guntinas-Lichius O, Geissler K, Komann M, Schlattmann P, Meissner W. Inter-Hospital variability of postoperative pain after tonsillectomy: prospective registry-based multicentre cohort study. PloS One. (2016) 11(4):e0154155. doi: 10.1371/journal.pone.0154155
14. Guntinas-Lichius O, Geissler K, Asendorf T, Tostmann R, Lohler J. Tonsillectomy versus tonsillotomy for recurrent acute tonsillitis in children and adults (TOTO): study protocol for a randomized non-inferiority trial. Trials. (2021) 22(1):479. doi: 10.1186/s13063-021-05434-y
15. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
16. AWMF leitlinie: therapie entzündlicher erkrankungen der gaumenmandeln—tonsillitis (2015). Nr. 017/024. Available at: https://register.awmf.org/de/leitlinien/detail/017-024 (Accessed May 5, 2023).
17. Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. (2014) 14:579. doi: 10.1186/s12913-014-0579-0
18. AWMF-regelwerk leitlinien (2023). Available at: https://www.awmf.org/regelwerk/ (Accessed May 5, 2023).
19. Mitchell RB, Archer SM, Ishman SL, Rosenfeld RM, Coles S, Finestone SA, et al. Clinical practice guideline: tonsillectomy in children (update)—executive summary. Otolaryngol Head Neck Surg. (2019) 160(2):187–205. doi: 10.1177/0194599818807917
20. Brandtzaeg P, Pabst R. Let’s go mucosal: communication on slippery ground. Trends Immunol. (2004) 25(11):570–7. doi: 10.1016/j.it.2004.09.005
21. Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis. (2005) 5(11):685–94. doi: 10.1016/S1473-3099(05)70267-X
22. Gunnarsson RK, Ebell M, Centor R, Little P, Verheij T, Lindbaek M, et al. Best management of patients with an acute sore throat—a critical analysis of current evidence and a consensus of experts from different countries and traditions. Infect Dis (Lond). (2023) 55(6):384–95. doi: 10.1080/23744235.2023.2191714
23. Petersen I, Johnson AM, Islam A, Duckworth G, Livermore DM, Hayward AC. Protective effect of antibiotics against serious complications of common respiratory tract infections: retrospective cohort study with the UK general practice research database. Br Med J. (2007) 335(7627):982. doi: 10.1136/bmj.39345.405243.BE
24. Kvestad E, Kvaerner KJ, Roysamb E, Tambs K, Harris JR, Magnus P. Heritability of recurrent tonsillitis. Arch Otolaryngol Head Neck Surg. (2005) 131(5):383–7. doi: 10.1001/archotol.131.5.383
25. Roberts AL, Connolly KL, Kirse DJ, Evans AK, Poehling KA, Peters TR, et al. Detection of group A Streptococcus in tonsils from pediatric patients reveals high rate of asymptomatic streptococcal carriage. BMC Pediatr. (2012) 12:3. doi: 10.1186/1471-2431-12-3
26. Dan JM, Havenar-Daughton C, Kendric K, Al-Kolla R, Kaushik K, Rosales SL, et al. Recurrent group A Streptococcus tonsillitis is an immunosusceptibility disease involving antibody deficiency and aberrant T(FH) cells. Sci Transl Med. (2019) 11(478):eaau3776. doi: 10.1126/scitranslmed.aau3776
27. Putto A. Febrile exudative tonsillitis: viral or streptococcal? Pediatrics. (1987) 80(1):6–12. doi: 10.1542/peds.80.1.6
28. Gunnarsson R, Orda U, Elliott B, Heal C, Del Mar C. What is the optimal strategy for managing primary care patients with an uncomplicated acute sore throat? Comparing the consequences of nine different strategies using a compilation of previous studies. BMJ Open. (2022) 12(4):e059069. doi: 10.1136/bmjopen-2021-059069
29. Mantzourani E, Wasag D, Cannings-John R, Ahmed H, Evans A. Characteristics of the sore throat test and treat service in community pharmacies (STREP) in Wales: cross-sectional analysis of 11,304 consultations using anonymized electronic pharmacy records. J Antimicrob Chemother. (2022) 78(1):84–92. doi: 10.1093/jac/dkac358
30. McGuire E, Li A, Collin SM, Decraene V, Cook M, Padfield S, et al. Time to negative throat culture following initiation of antibiotics for pharyngeal group A Streptococcus: a systematic review and meta-analysis up to October 2021 to inform public health control measures. Euro Surveill. (2023) 28(15):2200573. doi: 10.2807/1560-7917.ES.2023.28.15.2200573
31. Guntinas-Lichius O. Tonsillectomy in adults—to do or not to do. Lancet (2023) 401(10393):2015–7. doi: 10.1016/S0140-6736(23)00673-6
32. Wilson JA, O’Hara J, Fouweather T, Stocken DD, Luke V, Haighton C, et al. Conservative management versus tonsillectomy in adults with recurrent acute tonsillitis in the UK (NATTINA): a multicentre, open-label, randomised controlled trial. Lancet. (2023) 401(10393):2051–9. doi: 10.1016/S0140-6736(23)00519-6
33. Hendry J, Chin A, Swan IR, Akeroyd MA, Browning GG. The Glasgow benefit inventory: a systematic review of the use and value of an otorhinolaryngological generic patient-recorded outcome measure. Clin Otolaryngol. (2016) 41(3):259–75. doi: 10.1111/coa.12518
34. Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care. (1999) 37(2):126–39. doi: 10.1097/00005650-199902000-00003
35. Stewart MG, Friedman EM, Sulek M, deJong A, Hulka GF, Bautista MH, et al. Validation of an outcomes instrument for tonsil and adenoid disease. Arch Otolaryngolg Head Neck Surg. (2001) 127(1):29–35. doi: 10.1001/archotol.127.1.29
36. Skevas T, Klingmann C, Plinkert PK, Baumann I. Development and validation of the tonsillectomy outcome inventory 14. HNO. (2012) 60(9):801–6. doi: 10.1007/s00106-012-2545-7
37. Witsell DL, Orvidas LJ, Stewart MG, Hannley MT, Weaver EM, Yueh B, et al. Quality of life after tonsillectomy in adults with recurrent or chronic tonsillitis. Otolaryngol Head Neck Surg (2008) 138(1 Suppl):S1–8. doi: 10.1016/j.otohns.2007.08.015
38. Steinbichler T, Bender B, Blassnigg E, Riechelmann H. Evaluation of a German version of the tonsil and adenoid health status instrument. J Otolaryngol. (2014) 43(1):41. doi: 10.1186/s40463-014-0041-7
39. Laajala A, Autio TJ, Ohtonen P, Alho OP, Koskenkorva TJ. Interpretation of tonsillectomy outcome inventory-14 scores: a prospective matched cohort study. Eur Arch Otorhinolaryngol. (2020) 277(5):1499–505. doi: 10.1007/s00405-020-05832-z
40. Samara L, Esteller E, Dura MJ, Guirao M, Cardesin A, Stewart M, et al. Adaptation and validation of the Spanish version of the tonsil and adenoid health status instrument. Laryngoscope. (2018) 128(6):1469–75. doi: 10.1002/lary.26923
41. Houborg HI, Klug TE. Quality of life after tonsillectomy in adult patients with recurrent acute tonsillitis: a systematic review. Eur Arch Otorhinolaryngol. (2022) 279(6):2753–64. doi: 10.1007/s00405-022-07260-7
42. Plath M, Sand M, Behnen K, Plath K, Baumann I. Does a tonsillectomy indicated according to the German S2k guideline affect short-term quality of life in adults? Eur Arch Otorhinolaryngol. (2023) 280(4):1963–71. doi: 10.1007/s00405-022-07758-0
43. Kruger K, Topfner N, Berner R, Windfuhr J, Oltrogge JH, Guideline Group. Clinical practice guideline: sore throat. Dt Arztebl Int (2021) 118(11):188–94. doi: 10.3238/arztebl.m2021.0121
44. Klug TE, Rusan M, Fuursted K, Ovesen T. Peritonsillar abscess: complication of acute tonsillitis or Weber’s glands infection? Otolaryngol Head Neck Surg. (2016) 155(2):199–207. doi: 10.1177/0194599816639551
45. Bohne S, Siggel R, Sachse S, Kiehntopf M, Bauer M, Straube E, et al. Clinical significance and diagnostic usefulness of serologic markers for improvement of outcome of tonsillectomy in adults with chronic tonsillitis. J Negat Results Biomed. (2013) 12(1):11. doi: 10.1186/1477-5751-12-11
46. Sanmark E, Wiksten J, Valimaa H, Aaltonen LM, Ilmarinen T, Blomgren K. Peritonsillar abscess may not always be a complication of acute tonsillitis: a prospective cohort study. PLoS One. (2020) 15(4):e0228122. doi: 10.1371/journal.pone.0228122
47. de Cassan S, Thompson MJ, Perera R, Glasziou PP, Del Mar CB, Heneghan CJ, et al. Corticosteroids as standalone or add on treatment for sore throat. Emergencias. (2022) 34(4):308–9.35833771
48. Food and Drug Administration. FDA drug safety communication: FDA requires labeling changes for prescription opioid cough and cold medicines to limit their use to adults 18 years and older (2018). Available at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-requires-labeling-changes-prescription-opioid-cough-and-cold (Accessed May 10, 2023).
49. Spinks A, Glasziou PP, Del Mar CB. Antibiotics for treatment of sore throat in children and adults. Cochrane Database Syst Rev. (2021) 12(12):CD000023. doi: 10.1002/14651858.CD000023.pub5
50. Spurling GK, Del Mar CB, Dooley L, Foxlee R, Farley R. Delayed antibiotic prescriptions for respiratory infections. Cochrane Database Syst Rev. (2017) 9(9):CD004417. doi: 10.1002/14651858.CD004417.pub5
51. Munck H, Jorgensen AW, Klug TE. Antibiotics for recurrent acute pharyngo-tonsillitis: systematic review. Eur J Clin Microniol Inf Dis. (2018) 37(7):1221–30. doi: 10.1007/s10096-018-3245-3
52. van Driel ML, De Sutter AI, Thorning S, Christiaens T. Different antibiotic treatments for group A streptococcal pharyngitis. Cochrane Database Syst Rev. (2021) 3(3):CD004406. doi: 10.1002/14651858.CD004406.pub5
53. Bar-Yishay M, Yehoshua I, Bilitzky A, Press Y. Treatment outcomes of acute streptococcal tonsillitis according to antibiotic treatment. A retrospective analysis of 242,366 cases treated in the community. Eur J Gen Pract. (2022) 28(1):142–9. doi: 10.1080/13814788.2022.2083105
54. Brodsky L. Modern assessment of tonsils and adenoids. Ped Clin North Am. (1989) 36(6):1551–69. doi: 10.1016/s0031-3955(16)36806-7
55. Kisser U, Lill C, Adderson-Kisser C, Patscheider M, Stelter K. Total versus subtotal tonsillectomy for recurrent tonsillitis—a prospective randomized noninferiority clinical trial. Acta Otolaryngol. (2020) 140(6):514–20. doi: 10.1080/00016489.2020.1725112
56. Pynnonen M, Brinkmeier JV, Thorne MC, Chong LY, Burton MJ. Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev. (2017) 8(8):CD004619. doi: 10.1002/14651858.CD004619.pub3
57. Sunnergren O, Hemlin C, Ericsson E, Hessen-Soderman AC, Hultcrantz E, Odhagen E, et al. Radiofrequency tonsillotomy in Sweden 2009–2012. Eur Arch Otorhinolaryngol. (2014) 271(6):1823–7. doi: 10.1007/s00405-013-2867-4
58. Johnson RF, Beams DR, Zaniletti I, Chorney SR, Kou YF, Lenes-Voit F, et al. Estimated probability distribution of bleeding after pediatric tonsillectomy: a retrospective national cohort study of US children. JAMA Otolaryngol Head Neck Surg. (2023) 149(5):431–8. doi: 10.1001/jamaoto.2023.0268
59. Wong Chung J, van Benthem PPG, Blom HM. Tonsillotomy versus tonsillectomy in adults suffering from tonsil-related afflictions: a systematic review. Acta Otolaryngol (2018) 138(5):492–501. doi: 10.1080/00016489.2017.1412500
60. Lundstrom F, Stalfors J, Ostvoll E, Sunnergren O. Practice, complications and outcome in Swedish tonsil surgery 2009–2018. An observational longitudinal national cohort study. Acta Otolaryngol. (2020) 140(7):589–96. doi: 10.1080/00016489.2020.1746396
61. Guntinas-Lichius O, Volk GF, Zaslansky R, Meissner W. The first postoperative day: prospective evaluation of pain in adult otorhinolaryngologic surgery. Clin J Pain. (2014) 30(11):978–86. doi: 10.1097/AJP.0000000000000050
62. Aldamluji N, Burgess A, Pogatzki-Zahn E, Raeder J, Beloeil H, PROSPECT Working Group collaborators. PROSPECT guideline for tonsillectomy: systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia (2021) 76(7):947–61. doi: 10.1111/anae.15299
63. Hanani T, Gadban H, Jahshan F, Ronen O. Tantum verde mouthwash for tonsillectomy: a prospective, double-blind, randomized control trial. Int J Ped Otorhinolaryngol. (2019) 121:173–8. doi: 10.1016/j.ijporl.2019.03.020
64. AWMF Leitlinien. Behandlung akuter perioperativer und posttraumatischer schmerzen. 2021;001/025. Available at: https://register.awmf.org/de/leitlinien/detail/001-025 (Accessed May 10, 2023).
65. Jensen DR. Pharmacologic management of post-tonsillectomy pain in children. World J Otorhinolaryngol Head Neck Surg. (2021) 7(3):186–93. doi: 10.1016/j.wjorl.2021.03.004
66. Sheth KR, Bernthal NM, Ho HS, Bergese SD, Apfel CC, Stoicea N, et al. Perioperative bleeding and non-steroidal anti-inflammatory drugs: an evidence-based literature review, and current clinical appraisal. Medicine (Baltimore). (2020) 99(31):e20042. doi: 10.1097/MD.0000000000020042
67. Losorelli SD, Scheffler P, Qian ZJ, Lin HC, Truong MT. Post-tonsillectomy ibuprofen: is there a dose-dependent bleeding risk? Laryngoscope. (2022) 132(7):1473–81. doi: 10.1002/lary.29876
68. Redmann AJ, Maksimoski M, Brumbaugh C, Ishman SL. The effect of postoperative steroids on post-tonsillectomy pain and need for postoperative physician contact. Laryngoscope. (2018) 128(9):2187–92. doi: 10.1002/lary.27167
69. Tolska HK, Hamunen K, Takala A, Kontinen VK. Systematic review of analgesics and dexamethasone for post-tonsillectomy pain in adults. Br J Anaesthesia. (2019) 123(2):e397–411. doi: 10.1016/j.bja.2019.04.063
70. Choo S, Nogan S, Matrka L. Postoperative opioid prescribing and consumption patterns after tonsillectomy. Otolaryngol Head Neck Surg. (2019) 161(6):960–6. doi: 10.1177/0194599819866823
71. Lammers CR, Schwinghammer AJ, Hall B, Kriss RS, Aizenberg DA, Funamura JL, et al. Comparison of oral loading dose to intravenous acetaminophen in children for analgesia after tonsillectomy and adenoidectomy: a randomized clinical trial. Anesth Analg. (2021) 133(6):1568–76. doi: 10.1213/ANE.0000000000005678
72. Cho HK, Park IJ, Jeong YM, Lee YJ, Hwang SH. Can perioperative acupuncture reduce the pain and vomiting experienced after tonsillectomy? A meta-analysis. Laryngoscope. (2016) 126(3):608–15. doi: 10.1002/lary.25721
73. Lal A, Chohan K, Chohan A, Chakravarti A. Role of honey after tonsillectomy: a systematic review and meta-analysis of randomised controlled trials. Clin Otolaryngol. (2017) 42(3):651–60. doi: 10.1111/coa.12792
74. Geissler K, Schulze M, Inhestern J, Meissner W, Guntinas-Lichius O. The effect of adjuvant oral application of honey in the management of postoperative pain after tonsillectomy in adults: a pilot study. PLoS One. (2020) 15(2):e0228481. doi: 10.1371/journal.pone.0228481
75. Piitulainen JM, Uusitalo T, Sjoblom HM, Ivaska LE, Jegoroff H, Kauko T, et al. Intracapsular tonsillectomy in the treatment of recurrent and chronic tonsillitis in adults: a protocol of a prospective, single-blinded, randomised study with a 5-year follow-up (the FINITE trial). BMJ Open. (2022) 12(9):e062722. doi: 10.1136/bmjopen-2022-062722
76. Laajala A, Tokola P, Autio TJ, Koskenkorva T, Tastula M, Ohtonen P, et al. Total or partial tonsillar resection (tonsillectomy or tonsillotomy) to change the quality of life for adults with recurrent or chronic tonsillitis: study protocol for a randomised controlled trial. Trials. (2021) 22(1):617. doi: 10.1186/s13063-021-05539-4
77. Hessen Soderman AC, Ericsson E, Hemlin C, Hultcrantz E, Mansson I, Roos K, et al. Reduced risk of primary postoperative hemorrhage after tonsil surgery in Sweden: results from the National Tonsil Surgery Register in Sweden covering more than 10 years and 54,696 operations. Laryngoscope. (2011) 121(11):2322–6. doi: 10.1002/lary.22179
78. Stalfors J, Ovesen T, Bertelsen JB, Bugten V, Wennberg S, Sunnergren O. Comparison of clinical practice of tonsil surgery from quality register data from Sweden and Norway and one clinic in Denmark. BMJ Open. (2022) 12(4):e056551. doi: 10.1136/bmjopen-2021-056551
79. Geissler K, Bohne S, Siggel R, Sachse S, Kiehntopf M, Bauer M, et al. Preoperative serum pattern analysis to predict the outcome of tonsillectomy in adults with chronic tonsillitis. Eur Arch Otorhinolaryngol. (2014) 271(10):2803–11. doi: 10.1007/s00405-014-3084-5
80. Yoo TK, Choi JY, Jang Y, Oh E, Ryu IH. Toward automated severe pharyngitis detection with smartphone camera using deep learning networks. Comput Biol Med. (2020) 125:103980. doi: 10.1016/j.compbiomed.2020.103980
81. Piqueras S, Krafft C, Beleites C, Egodage K, von Eggeling F, Guntinas-Lichius O, et al. Combining multiset resolution and segmentation for hyperspectral image analysis of biological tissues. Analytica Chim Acta. (2015) 881:24–36. doi: 10.1016/j.aca.2015.04.053
82. Sharma G, Parmar A, Hoffmann F, Geißler K, von Eggeling F, Guntinas-Lichius O, et al. A proposal to perform high contrast imaging of human palatine tonsil with cross polarized optical coherence tomography. Photonics. (2022) 9(4):259. doi: 10.3390/photonics9040259
83. Hulse K, Lindsay E, Rogers A, Young D, Kunanandam T, Douglas CM. Twenty-year observational study of paediatric tonsillitis and tonsillectomy. Arch Dis Childhood. (2022) 107(12):1106–10. doi: 10.1136/archdischild-2022-323910
84. Bitar MA, Dowli A, Mourad M. The effect of tonsillectomy on the immune system: a systematic review and meta-analysis. Int J Ped Otorhinolaryngol. (2015) 79(8):1184–91. doi: 10.1016/j.ijporl.2015.05.016
85. Yan Y, Song Y, Liu Y, Su J, Cui L, Wang J, et al. Short- and long-term impacts of adenoidectomy with/without tonsillectomy on immune function of young children <3 years of age: a cohort study. Medicine (Baltimore). (2019) 98(19):e15530. doi: 10.1097/MD.0000000000015530
86. Altwairqi RG, Aljuaid SM, Alqahtani AS. Effect of tonsillectomy on humeral and cellular immunity: a systematic review of published studies from 2009 to 2019. Eur Arch Otorhinolaryngol. (2020) 277(1):1–7. doi: 10.1007/s00405-019-05672-6
87. Onal M, Onal O, Turan A. Can secondary lymphoid organs exert a favorable effect on the mild course of COVID-19 in children? Acta Otolaryngol. (2021) 141(1):83–4. doi: 10.1080/00016489.2020.1814965
88. Capriotti V, Mattioli F, Guida F, Marcuzzo AV, Lo Manto A, Martone A, et al. COVID-19 in the tonsillectomised population. Acta Otorhinolaryngol Ital. (2021) 41(3):197–205. doi: 10.14639/0392-100X-N1436
89. Kara A, Elden H, Okur E, Yilmaz MS, Mutlu F, Guven M, et al. Impact of tonsillectomy on COVID-19 pandemic: an observational study of the incidence and prognosis. Acta Otolaryngol. (2021) 141(9):857–9. doi: 10.1080/00016489.2021.1970803
90. Park SJ, Min C, Yoo DM, Lee SY, Choi HG. Tonsillectomy in adults over 40 years of age does not increase the risk of pneumonia: a three-year longitudinal follow-up study. Int J Environ Res Public Health. (2021) 18(24):13059. doi: 10.3390/ijerph182413059
91. Ji J, Sundquist J, Sundquist K. Tonsillectomy associated with an increased risk of autoimmune diseases: a national cohort study. J Autoimmun. (2016) 72:1–7. doi: 10.1016/j.jaut.2016.06.007
92. Kim JS, Lee MG, Lee SK, Yeom SW, Kang MG, Lee JH, et al. Association of adenotonsillar disease and adenotonsillectomy with the development of vitiligo: a nationwide population-based cohort study. Front Med. (2022) 9:1004218. doi: 10.3389/fmed.2022.1004218
93. Kacimi SEO, Elgenidy A, Cheema HA, Ould Setti M, Khosla AA, Benmelouka AY, et al. Prior tonsillectomy and the risk of breast cancer in females: a systematic review and meta-analysis. Front Oncol. (2022) 12:925596. doi: 10.3389/fonc.2022.925596
94. Sun LM, Chen HJ, Li TC, Sung FC, Kao CH. A nationwide population-based cohort study on tonsillectomy and subsequent cancer incidence. Laryngoscope. (2015) 125(1):134–9. doi: 10.1002/lary.24864
95. Liaw KL, Adami J, Gridley G, Nyren O, Linet MS. Risk of Hodgkin’s disease subsequent to tonsillectomy: a population-based cohort study in Sweden. Int J Cancer. (1997) 72(5):711–3. doi: 10.1002/(sici)1097-0215(19970904)72:5%3C711::aid-ijc1%3E3.0.co;2-v
96. Combes JD, Voisin N, Perie S, Malard O, Jegoux F, Nadjingar R, et al. History of tonsillectomy and risk of oropharyngeal cancer. Oral Oncol. (2021) 117:105302. doi: 10.1016/j.oraloncology.2021.105302
97. Vestergaard H, Westergaard T, Wohlfahrt J, Hjalgrim H, Melbye M. Tonsillitis, tonsillectomy and Hodgkin’s lymphoma. Int J Cancer. (2010) 127(3):633–7. doi: 10.1002/ijc.24973
98. Hollo G. Tonsillectomy and the incidence of various types of cancer. Immunol Res. (2021) 69(6):467–70. doi: 10.1007/s12026-021-09230-3
99. Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room. Med Decis Making. (1981) 1(3):239–46. doi: 10.1177/0272989x8100100304
100. McIsaac WJ, White D, Tannenbaum D, Low DE. A clinical score to reduce unnecessary antibiotic use in patients with sore throat. CMAJ. (1998) 158(1):75–83.9475915
101. Little P, Moore M, Hobbs FD, Mant D, McNulty C, Williamson I, et al. PRImary care Streptococcal Management (PRISM) study: identifying clinical variables associated with Lancefield group A beta-haemolytic streptococci and Lancefield non-group A streptococcal throat infections from two cohorts of patients presenting with an acute sore throat. BMJ Open. (2013) 3(10):e003943. doi: 10.1136/bmjopen-2013-003943
102. Paradise JL, Bluestone CD, Colborn DK, Bernard BS, Rockette HE, Kurs-Lasky M. Tonsillectomy and adenotonsillectomy for recurrent throat infection in moderately affected children. Pediatrics (2002) 110(1 Pt 1):7–15. doi: 10.1542/peds.110.1.7
103. van Staaij BK, van den Akker EH, Rovers MM, Hordijk GJ, Hoes AW, Schilder AG. Effectiveness of adenotonsillectomy in children with mild symptoms of throat infections or adenotonsillar hypertrophy: open, randomised controlled trial. Br Med J. (2004) 329(7467):651. doi: 10.1136/bmj.38210.827917.7C
104. Alho OP, Koivunen P, Penna T, Teppo H, Koskela M, Luotonen J. Tonsillectomy versus watchful waiting in recurrent streptococcal pharyngitis in adults: randomised controlled trial. Br Med J. (2007) 334(7600):939. doi: 10.1136/bmj.39140.632604.55
105. Lock C, Wilson J, Steen N, Eccles M, Mason H, Carrie S, et al. North of England and Scotland study of tonsillectomy and adeno-tonsillectomy in children (NESSTAC): a pragmatic randomised controlled trial with a parallel non-randomised preference study. Health Techno Assess (2010) 14(13):1–164, iii–iv. doi: 10.3310/hta14130
106. Koskenkorva T, Koivunen P, Koskela M, Niemela O, Kristo A, Alho OP. Short-term outcomes of tonsillectomy in adult patients with recurrent pharyngitis: a randomized controlled trial. CMAJ. (2013) 185(8):E331–6. doi: 10.1503/cmaj.121852
Keywords: tonsillitis, sore throat, pharyngitis, quality of life, outcome, treatment, tonsillectomy, tonsillotomy
Citation: Guntinas-Lichius O, Geißler K, Mäkitie AA, Ronen O, Bradley PJ, Rinaldo A, Takes RP and Ferlito A (2023) Treatment of recurrent acute tonsillitis—a systematic review and clinical practice recommendations. Front. Surg. 10:1221932. doi: 10.3389/fsurg.2023.1221932
Received: 13 May 2023; Accepted: 11 September 2023;
Published: 10 October 2023.
Edited by:
Haralampos Gouveris, Johannes Gutenberg University Mainz, GermanyReviewed by:
Norhafiza Mat Lazim, Universiti Sains Malaysia (USM), MalaysiaJoanna Jackowska, Poznan University of Medical Sciences, Poland
© 2023 Guntinas-Lichius, Geißler, Mäkitie, Ronen, Bradley, Rinaldo, Takes and Ferlito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Orlando Guntinas-Lichius orlando.guntinas@med.uni-jena.de
This paper was written by members and invitees of the International Head and Neck Scientific Group (www.IHNSG.com)
†ORCID Orlando Guntinas-Lichius orcid.org/0000-0001-9671-0784 Antti A. Mäkitie orcid.org/0000-0002-0451-2404 Ohad Ronen orcid.org/0000-0001-7084-0695 Patrick J. Bradley orcid.org/0000-0003-2810-5709 Alessandra Rinaldo orcid.org/0000-0001-7956-6709 Robert P. Takes orcid.org/0000-0003-4784-0499 Alfio Ferlito orcid.org/0000-0002-8247-8002
 Orlando Guntinas-Lichius
Orlando Guntinas-Lichius Katharina Geißler
Katharina Geißler Antti A. Mäkitie
Antti A. Mäkitie Ohad Ronen
Ohad Ronen Patrick J. Bradley
Patrick J. Bradley Alessandra Rinaldo5,†
Alessandra Rinaldo5,†  Robert P. Takes
Robert P. Takes Alfio Ferlito
Alfio Ferlito