Effects of remnant preservation in anterior cruciate ligament reconstruction: A systematic review and meta-analysis
- 1Health Science Center, Shenzhen University, Shenzhen, China
- 2Department of Sports Medicine, The First Affiliated Hospital of Shenzhen University, Shenzhen Second People's Hospital, Shenzhen, China
Background: Compared with standard anterior cruciate ligament (ACL) reconstruction, it is controversial whether anterior cruciate ligament reconstruction (ACLR) with remnant preservation can lead to better clinical outcomes. We conducted a systematic study and meta-analysis to assess the differences in clinical efficacy between the two.
Method: We searched for clinical randomized controlled studies and cohort studies included in the Cochrane library, PubMed, and Embase from March 2012 to March 2022 in English. The included studies were ACLR with or without remant preservation, and the data were extracted and the quality of the included studies was assessed by two authors, respectively. Revman 5.4 was used for statistical analysis and conclusions were presented.
Result: Ten articles containing a total of 777 patients were finally included. There was no significant difference in postoperative Lachman test [OR = 1.66, 95%CI (0.79, 3.49), P = 0.18 > 0.05], Tegner score [SMD = −0.13, 95%CI (−0.47, 0.22), P = 0.46 > 0.05], synovial coverage rate by second-look arthroscopy [OR = 1.55, 95%CI (0.66, 3.65), P = 0.32 > 0.05], the rate of cyclops lesion [OR = 3.92, 95%CI (0.53, 29.29), P = 0.18 > 0.05], joint range of motion [SMD = 0.27, 95%CI (−0.13, 0.68), P = 0.19 > 0.05] and re-injury rate [OR = 0.57, 95%CI (0.18, 1.74), P = 0.32 > 0.05] between the two groups. There were statistically significant differences in postoperative Lysholm score [SMD = 0.98, 95% CI (0.32, 1.64), P = 0.004 < 0.05], International Knee Documantation Committee grade (IKDC grade) [OR = 2.19, 95%CI (1.03, 4.65), P = 0.04 < 0.05], Pivot shift test [OR = 1.71, 95%CI (1.06, 2.77), P = 0.03 < 0.05], KT1000/2000 arthrometer side-to-side difference [SMD = −0.22, 95%CI (−0.42, −0.03), P = 0.02 < 0.05], operation time [SMD = 11.69, 95%CI (8.85, 14.54), P = 0.00001 < 0.05] and degree of tibial tunnel enlargement [SMD = −0.66, 95%CI (−1.08, −0.23), P = 0.002 < 0.05].
Conclusion: This meta-analysis concluded that remnant preservation significantly had better results in terms of patient functional score (Lysholm, IKDC), knee stability (Pivot shift test, postoperative side-to-side anterior laxity) and tibial tunnel enlargement. In terms of complications (incidence of Cyclops lesions, range of motion, re-injury rate), no significant differences were seen between the two groups. Although many studies concluded that remnant preservation could bring better synovial coverage, this meta-analysis indicated that there is insufficient evidence to support it, possibly due to different remnant preservation procedures.The potential risks associated with longer operation times are also worth considering.
Introduction
The anterior cruciate ligament (ACL) is one of the important structures to maintain the static and dynamic stability of the knee joint. It is located in the joint cavity and surrounded by synovial tissue. ACL injury is one of the most common sports injuries of the knee joint (1). After complete ACL rupture, the broken end of the ACL is gradually encapsulated by synovial tissue, coupled with the special environment in the knee joint, and the injured ligament is usually difficult to heal by itself (2). Anterior cruciate ligament reconstruction (ACLR) has become an effective surgical method for the treatment of ACL injury, which can restore the stability of the knee joint, accelerate the time of return to sport (RTS), and effectively prevent meniscus injury and reduce the risk of arthritis progression (3). However, the postoperative effect did not achieve the desired effect. For example, some patients still have knee instability after surgery, and the re-injury rate and the risk of osteoarthritis still exist (4, 5). In recent years, ACL remnant preservation has become a research hotspot in ACL reconstruction, but the clinical significance, surgical methods and indications of remnant preservation remain controversial.
After ACLR, ACL will go through three biological outcome periods: tissue necrosis, new tissue ingrowth and ligamentization, and then the histological morphology and biomechanical properties of the graft tend to be normal ACL (6). However, in the period of tissue necrosis and new tissue ingrowth, the graft failure load is significantly reduced and it is easy to damage again. A large number of biological and animal experiments have shown that the preservation of ACL remnant can accelerate the synovial coverage of the transplanted ligament, reduce synovial fluid invasion of the transplanted ligament and the inner wall of the bone tunnel, and promote revascularization, ligamentization, and tendon-bone healing (7–10). Beside, residual proprioceptors in the ACL remnant still play a role in stabilizing the knee after ACL injury (11). However, a large number of clinical studies have failed to produce consensus. Some believe that compared with standard reconstruction, ACLR with remnant preservation can bring better clinical efficacy. Some believe that the clinical prognosis of ACLR with remnant preservation is similar to that of standard ACLR, which does not bring better efficacy and may even bring the risk of some complications, such as residual contracture or hyperplasia leading to postoperative knee extension disorder (12).
Several previous reviews also summarized the relevant literature for analysis, but none of them reached a uniform conclusion (12–14). It may be due to insufficient strict literature screening criteria, and no systematic analysis of surgical indications, surgery, etc. Based on previous studies, this study included clinical studies with high grade evidence in the last decade and included all outcome measures available for systematic analysis for systematic studies and meta-analysis whenever possible.
The purpose of this meta-analysis was to compare the clinical outcome of standard ACLR and ACLR with remnant preservation, and provide a reference for clinicians. Our hypothesis is that ACLR with remnant preservation can result in better clinical outcomes.
Data and methods
Search strategy and selection criteria
Two authors independently completed a systematic search of three databases (PubMed, EMBASE, Cochrane Library). The base terms used included “anterior cruciate ligament,” “ACL reconstruction,” “remnant,” “preservation,” “remnant-preserved.” This search was limited for studies reporting outcomes in the last 10 years (from March 2012 to March 2022), and was limited to English studies. The included studies (LEVEL OF EVIDENCE: I and II.) were reviewed. According to the inclusion and exclusion criteria, two authors independently selected all articles by reviewing the full text. Any disagreements at the inclusion stage were resolved by discussion with the third author.
Inclusion and exclusion criteria
The Inclusion criteria for this article are as follows: Randomized controlled trial or cohort study; ACL reconstruction with remnant preservation performed on experimental group, while standard ACL reconstruction without remnant preservation performed on control group, and the surgical techniques were fully described; at least one of the following outcome measures should be reported (postoperative Lysholm score, IKDC score, Tegner score, Lachman test, Pivot-shift test, KT1000/2000 arthrometer side-to-side difference, bone tunnel enlargement, operation time, cyclops lesion, range of motion, re-injury rate, second-look arthroscopic examination); Only human subjects were used. The exclusion criteria are as follows: The full text can't be obtained, the literatures published repeatedly, non-clinical study, retrospective study, including the patients who suffer from postoperative re-injury to reoperation, who are combined with other ligament surgeries, who suffer from fracture combined with open fracture, nerve and blood vessel injury, as well as other knee joint disease history or systemic disease history.
Data extraction
The study authors, publication time, number of patients, age, gender, time from injury to surgery, postoperative Lysholm score, IKDC score, Tegner score, knee laxity measured by KT1000/2000, bone tunnel enlargement, operation time, re-injury rate and second-look arthroscopic examination were extracted.
Quality assessment
Data were extracted independently by two arthors, evaluated for quality and reconciled, cross-checked, and in case of discrepancies resolved by discussion or a third investigator decided on their inclusion. Cohort studies used the Newcastle-Ottawa Scale (NOS) score to assess the quality of the literature, and randomized controlled trials were evaluated for the quality of the included studies according to the risk of bias assessment criteria recommended by the Cochrane Handbook for Systematic Reviews.
Statistical analysis
We used Revman 5.4 for all statistical analyses. Odds ratio (OR or RR) was used for dichotomous data, and weighted mean difference (WMD or SMD) was used for continuous variable data. Both types of indicators were expressed as 95% confidence interval (CI). In terms of heterogeneity test, the studies with good homogeneity (P > 0.1 or I2 < 50%) used the fixed-effect model for Meta analysis. If there was significant heterogeneity among the studies, the random model was used for Meta analysis. We also performed a subgroup analysis to identify potential differences between remnant preservation with and without tensioning.
Results
Literature search
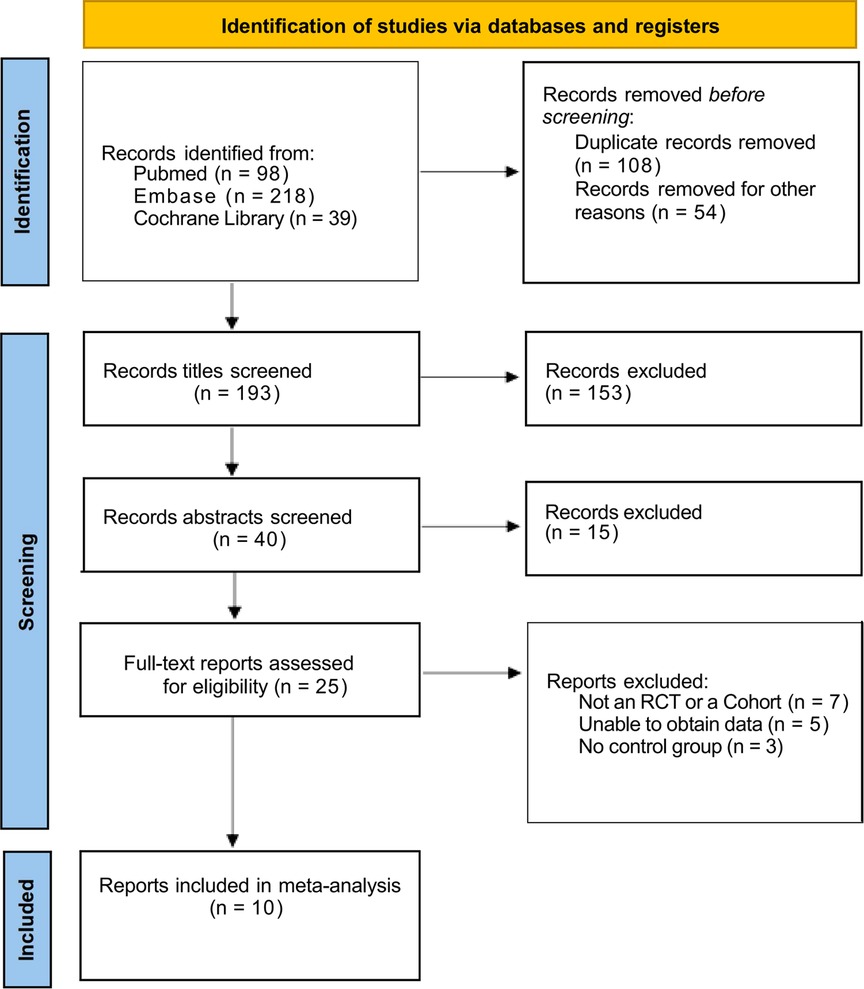
A total of 355 literatures were obtained by searching keywords, including PubMed (n = 98), EBSCO (n = 218) and Cochrane Library (n = 39). After layer-by-layer screening, 10 literatures were finally included (15–24). The literature screening process and results are shown in Figure 1.
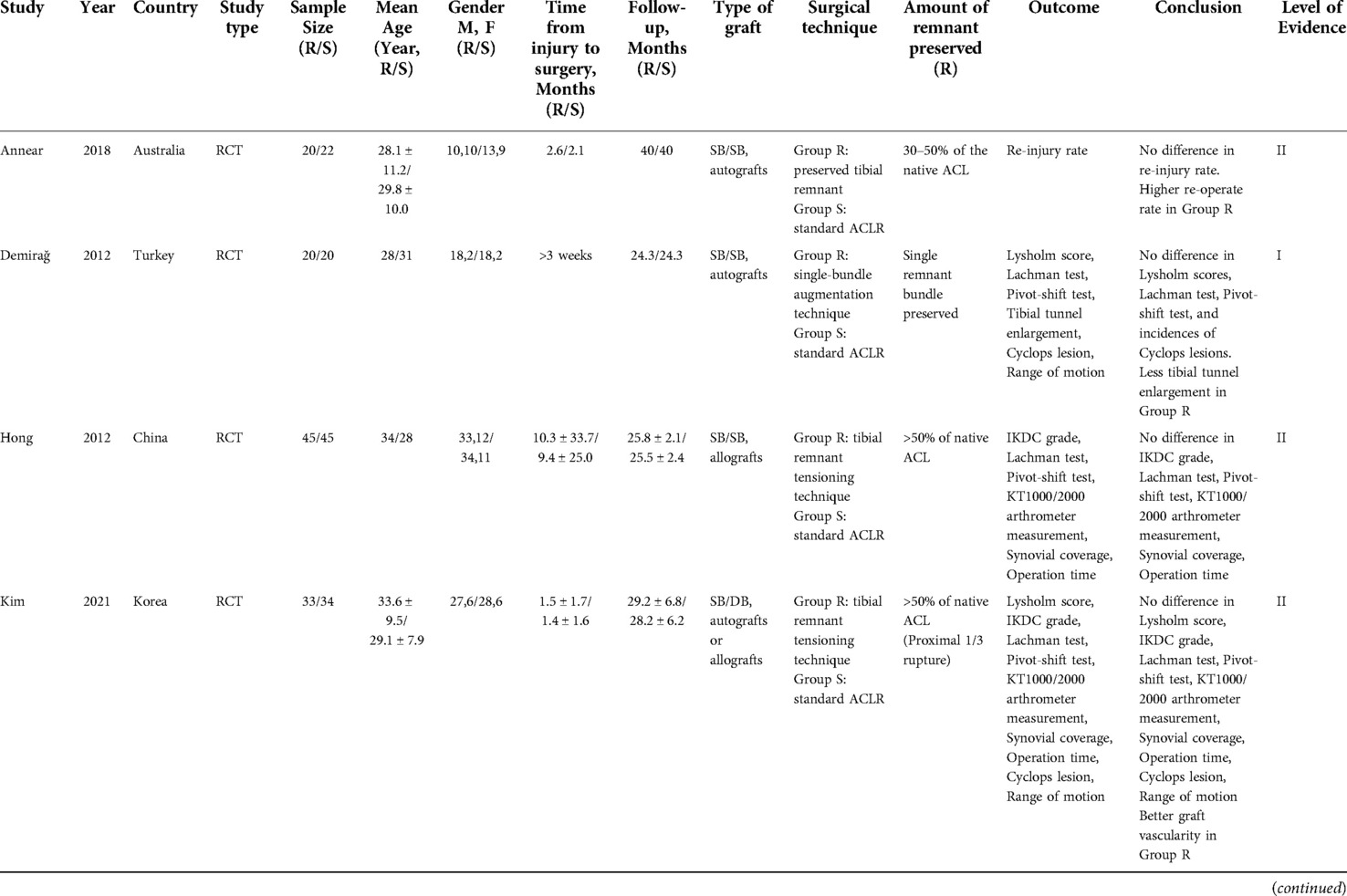
Among the 10 included literatures, all were published by English, including 777 patients, 370 cases in the experimental group (ACLR with remnant preservation, ACLR-R) and 407 cases in the control group (standard ACLR, ACLR-S). Table 1 summarized the details of included literatures in this meta-analysis.
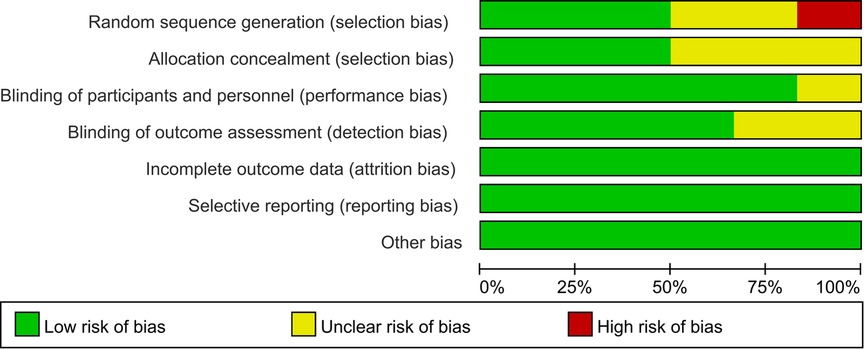
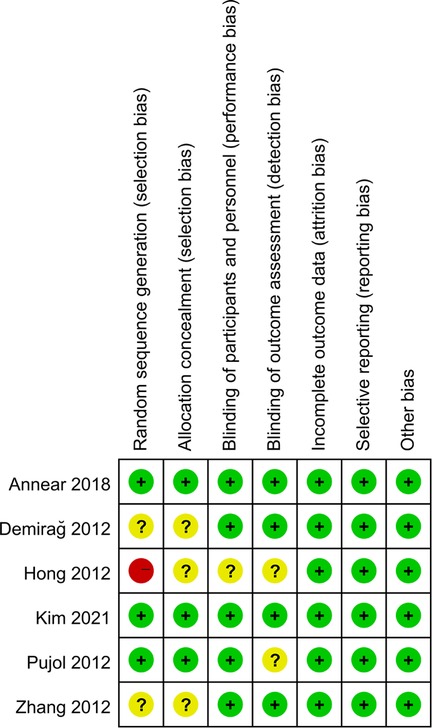
6 included articles were randomized controlled trials (15–20), and 4 were cohort studies (21–24). One of the four cohort studies scored 8 (22), one study scored 7 (23), and two scored 6 (21, 24). Randomized controlled trials evaluated the quality of included studies according to the risk of bias assessment criteria recommended by the Cochrane Handbook for Systematic Reviews, as shown in Figure 2, 3.
Patient subjective score
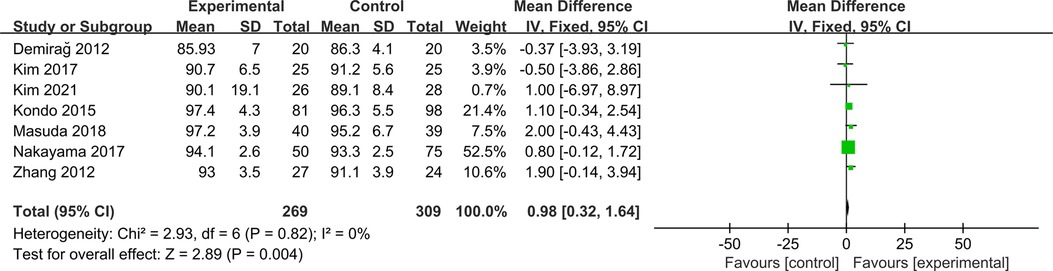
Lysholm score
Seven studies were included to compare postoperative Lysholm scores between ACLR-R and ACLR-S (16, 18, 20–24). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.82, I2 = 0%). The postoperative Lysholm score in the ACLR-R group was better than that in the ACLR-S group, and the difference was statistically significant [SMD = 0.98, 95% CI (0.32, 1.64), P = 0.004 < 0.05], as shown in Figure 4.
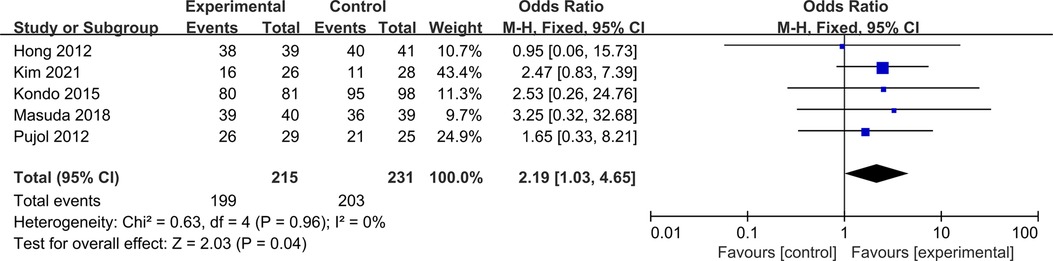
IKDC grade
Five studies were included to compare postoperative IKDC grade between ACLR-R and ACLR-S (17–19, 22, 23). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.96, I2 = 0%). The postoperative IKDC grade A/B probability in the ACLR-R group was better than that in the ACLR-S group, and the difference was statistically significant [OR = 2.19, 95%CI (1.03, 4.65), P = 0.04 < 0.05], as shown in Figure 5.
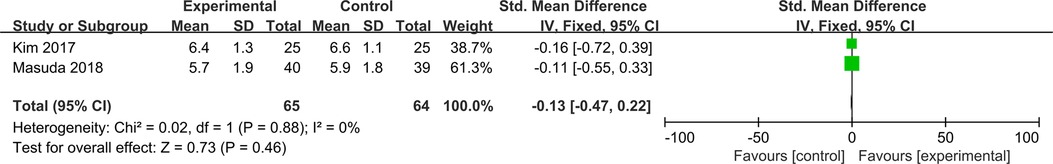
Tegner score
Two studies were included to compare postoperative Tegner score between ACLR-R and ACLR-S (21, 23). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.88, I2 = 0%). There was no significant difference in postoperative Tegner scores between the two groups [SMD = −0.13, 95%CI (−0.47, 0.22), P = 0.46 > 0.05], as shown in Figure 6.
Knee stability
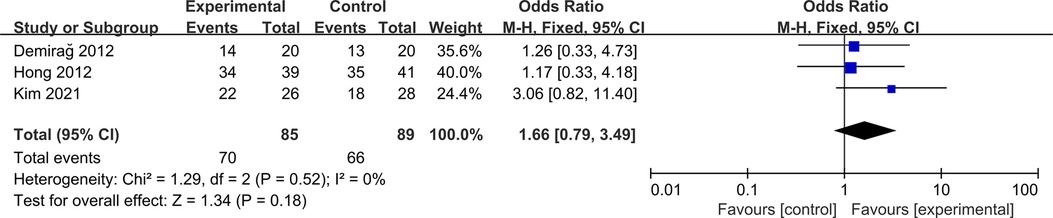
Lachman test
Three studies were included to compare postoperative Lachman test between ACLR-R and ACLR-S (16–18). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.52, I2 = 0%). There was no significant difference in postoperative Lachman test between the two groups [OR = 1.66, 95%CI (0.79, 3.49), P = 0.18 > 0.05], as shown in Figure 7.
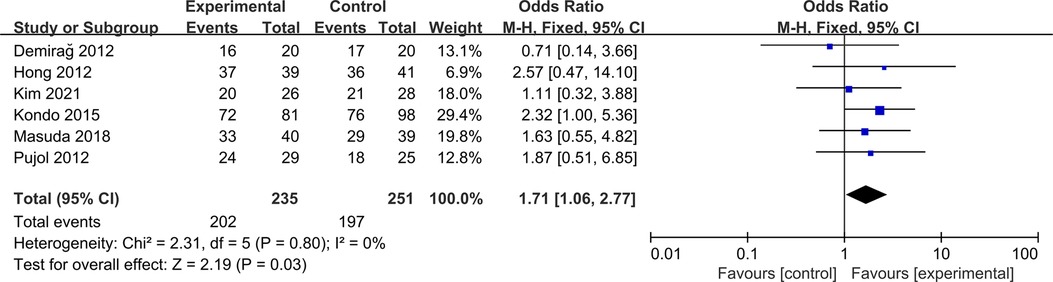
Pivot-shift test
Six studies were included to compare postoperative Pivot-shift test between ACLR-R and ACLR-S (16–19, 22, 23). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.80, I2 = 0%). The negative rate of postoperative Pivot shift test in ACLR-R group was more than that in ACLR-S group, and the difference was statistically significant [OR = 1.71, 95%CI (1.06, 2.77), P = 0.03 < 0.05], as shown in Figure 8.
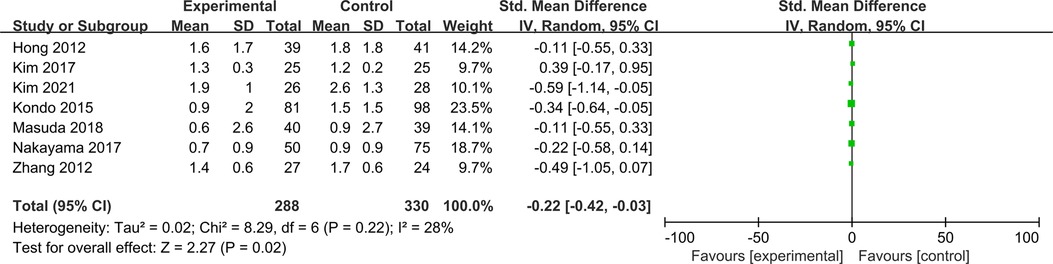
KT1000/2000 arthrometer measurement
Seven studies were included to compare postoperative side-to-side anterior laxity measured by KT1000/2000 arthrometer between ACLR-R and ACLR-S (17, 18, 20–24). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.22, I2 = 28%). The postoperative side-to-side anterior laxity measured by KT1000/2000 arthrometer in the ACLR-R group was less than that in the ACLR-S group, and the difference was statistically significant [SMD = −0.22, 95%CI (−0.42, −0.03), P = 0.02 < 0.05], as shown in Figure 9.
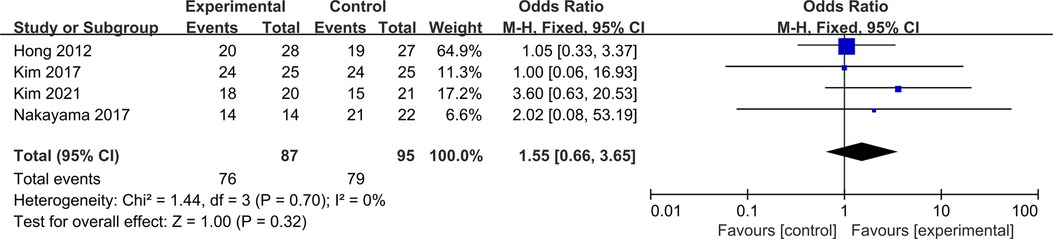
Synovial coverage
Four studies were included to compare postoperative synovial coverage between ACLR-R and ACLR-S (17, 18, 21, 24). Four studies were included to compare postoperative synovial coverage between ACLR-R and ACLR-S. The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.70, I2 = 0%). The probability of patients with postoperative synovial coverage >50% was similar between the two groups, and the difference was not statistically significant [OR = 1.55, 95%CI (0.66, 3.65), P = 0.32 > 0.05], as shown in Figure 10.
Operation time
Four studies were included to compare operation time between ACLR-R and ACLR-S (17, 18, 21, 22). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.34, I2 = 10%). The operation time in the ACLR-R group was more than that in the ACLR-S group, and the difference was statistically significant [SMD = 11.69, 95%CI (8.85, 14.54), P = 0.00001 < 0.05], as shown in Figure 11.
Complications
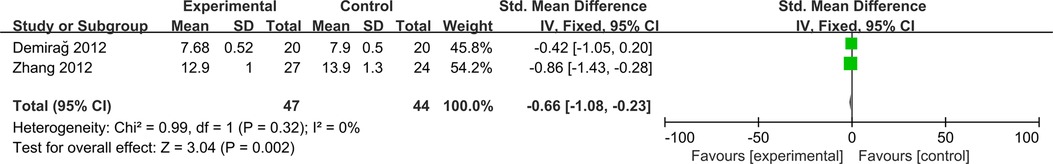
Tibial tunnel enlargement
Two studies were included to compare tibial tunnel enlargement between ACLR-R and ACLR-S (16, 20). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.32, I2 = 0%). The tibial tunnel enlargement in the ACLR-R group was less than that in the ACLR-S group, and the difference was statistically significant [SMD = −0.66, 95%CI (−1.08, −0.23), P = 0.002 < 0.05], as shown in Figure 12.
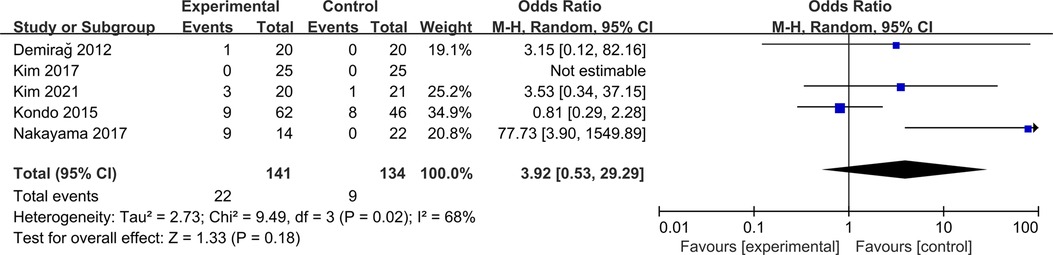
Cyclops lesion
Five studies were included to compare cyclops lesion between ACLR-R and ACLR-S (16, 18, 21, 22, 24). The Random-effect model was selected for analysis based on the heterogeneity test results (P = 0.02, I2 = 68%). The cyclops lesion was similar between the two groups, and the difference was not statistically significant [OR = 3.92, 95%CI (0.53, 29.29), P = 0.18 > 0.05], as shown in Figure 13.
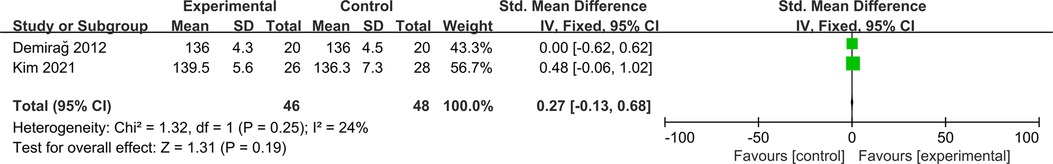
Range of motion
Two studies were included to compare postoperative range of motion (ROM) between ACLR-R and ACLR-S (16, 18). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.25, I2 = 24%). The postoperative ROM was similar between the two groups, and the difference was not statistically significant [SMD = 0.27, 95%CI (−0.13, 0.68), P = 0.19 > 0.05], as shown in Figure 14.
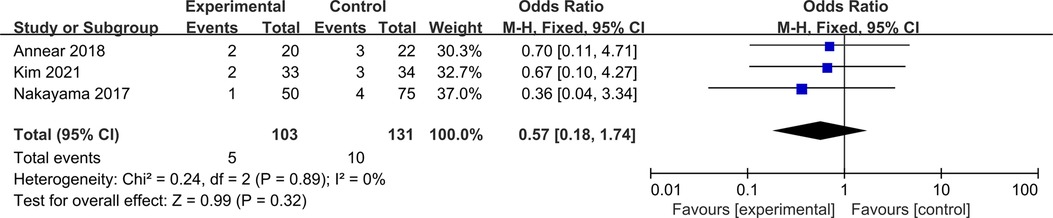
Re-injury rate
Three studies were included to compare re-injury rate between ACLR-R and ACLR-S (15, 18, 24). The fixed-effect model was selected for analysis based on the heterogeneity test results (P = 0.89, I2 = 0%). The rate of re-injury was similar between the two groups, and the difference was not statistically significant [OR = 0.57, 95%CI (0.18, 1.74), P = 0.32 > 0.05], as shown in Figure 15.
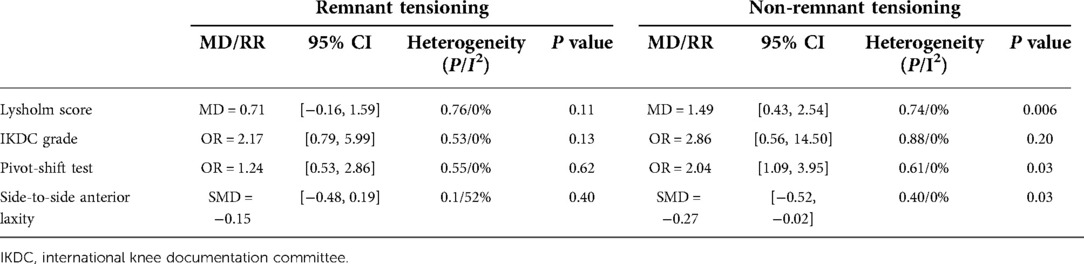
Subgroup analysis
Subgroup analysis was performed according to technique of remnant preservation (remnant preservation with and without remnant tensioning), as shown in Table 2. In the subgroup of Non-remnant tensioning, significant differences were found in Lysholm score, Pivot-shift test and side-to-side difference between ACLR-P and ACLR-S. In the subgroup of remnant tensioning, we could see high heterogeneity of postoperative side-to-side difference between ACLR-P and ACLR-S due to the study of Kim (21). In this trial, the ACLR-P used allograft tendons, while the ACLR-S used autologous tendons. Exclusion of this trial altered the result of the side-to-side difference [SMD = −0.26, 95%CI (−0.51, −0.02), P = 0.04 < 0.05] (P = 0.39 and I2 = 0% for heterogeneity) between ACLR-P and ACLR-S.
Discussion
Our results suggest that compared with standard ACLR, ACLR with remnant preservation had better results in terms of Lysholm scores, IKDC grade, Pivot shift test, postoperative side-to-side anterior laxity, operation time and degree of tibial tunnel enlargement. However, there was no significant difference between the two groups in terms of Lachman test, Tegner score, synovial coverage rate, complications (incidence of Cyclops lesions, range of motion), and re-injury rate. These results suggest that the ACLR with remnant preservation can promote graft healing, increase knee stability, prevent tibial tunnel widening, and have similar or even better clinical outcomes than standard ACLR.
Knee stability includes both static and dynamic stability. Static stability mainly refers to the mechanical traction of ligaments, while dynamic stability refers to the perception and control of the knee during movement. ACL is not only a static stability device for the knee joint, but also has a role in maintaining the dynamic stability of the knee joint because of proprioceptors (25). Patients with ACL injury will have knee instability, swelling and pain. Without timely treatment, patients will have secondary meniscus and articular cartilage injury, and even the risk of progression of arthritis will be increased, which will seriously affect the function of the patient's knee joint. It can be seen that restoring knee stability is the most important therapeutic aim of ACL reconstruction. After ACLR, both graft ligament healing and proprioceptive recovery affect knee stability.
After ACLR, the graft ligament is incompetent and undergoes four stages: ischemia, necrosis, proliferation, and ligamentization in the joint cavity, followed by a tendency to normal ACL (26). Synovialization and vascularization of the graft are important stages of the biological healing process. Good synovial coverage can promote the reconstruction of blood supply of the ACL graft and bring better knee function and stability. Synovialization and vascularization of the graft are important stages of the biological healing process. Good synovial coverage can promote the reconstruction of blood supply of the ACL graft and bring better knee function and stability (27). Animal studies had showed that after ACL complete injury, preserving the ACL remnant, which has a vascular-rich synovium, a large number of fibroblasts, myofibroblasts, and vascular-derived stem cells, can promote the ability of vascular regeneration by promoting the expression of vasoactive factors around the graft, and eventually promote synovialization and ligamentization of the graft (28, 29). Many follow-up studies had also demonstrated that preserving the remnant results in better synovial coverage, and that good synovial coverage may contribute to knee stability (30, 31). However, our study concluded that there is no significant difference between the two groups in terms of the probability of patients with postoperative synovial coverage > 50%. This result may be due to the differences in surgical procedures of remnant preservation and ACLR among the four included articles. In the study by Nakayama et al, both groups performed double-bundle ACLR using autograft (24). In the study by Kim et al, both groups used single-bundle ACLR, while the ACLR-P group used allograft and ACLR-S group used autograft (21). Kim et al performed single-bundle ACLR for ACLR-P, and double-bundle for ACLR-S group, and both of the groups used allograft or autograft (18). Hong et al performed single-bundle ACLR using allograft (17). Only Nakayama et al placed the remnant between the AM and PL bundle grafts (24), the others passed the graft through the center of the tibial remnant (17, 18, 21). So we supposed that our result due to the following reasons: (1) Synovialization of allograft is worse than autograft, (2) The graft passes through the center of the tibial remnant, which means more contact area with the remnant, resulting in the remnant wrapping the graft tendon and sealing of the tibial tunnel adequately (32). At the same time, not only these four articles, but all the included literature do not have a uniform standard for the quality of remnant preservation. Kim et al found that only preserving the remnants fully covered with synovium can have better synovial coverage at the second microscopy than non-remnant preservation (33). It meant that a remnant with poor synovial coverage cannot contribute to postoperative synovial coverage. Meanwhile, the small sample size is also a factor that affects the result.
Besides the second-look arthroscopic examination, MRI is also commonly used to evaluate ligamentization of the graft. Signal/noise quatient (SNQ) is a common indicator for assessing the degree of graft ligamentization after ACLR. Lower SNQ represents lower graft water content, more ligamentization, and better biomechanical properties (34). Remnant preservation is an independent associated factors of graft SNQ (35). Takahashi et al. performed a retrospective analysis and showed that SNQ values of ACL grafted tendon at 2 years after surgery in ACLR-R Group were better than those in ACLR-S Group (30). In our Meta analysis, only one study evaluated the SNQ value, and the results showed that the mean SNQ values were compared and showed no signifificant intergroup differences at 1 year (18). In this study, they performed remnant-tensioning single-bundle and double-bundle ACLR, and . But when they used DCE-MRI to assess graft vascularity, the results showed that the ACL-R group had a richer graft vascularity than the ACLR-S group.
In addition to static stability, dynamic stability is also particularly important. ACL is also a proprioceptive organ, included a large number of proprioceptors, which are mainly distributed near the femoral and tibial insertion of the ligament and are particularly important for maintaining the dynamic stability of the knee joint (36). During knee flexion, extension, rotation and other movements, ACL receives the corresponding mechanical traction. The proprioceptor receives the signal and generates nerve impulses, which are transmitted to the central nervous system, forming reflexes and proprioception. Then muscles adjacent to the joints contract to complete the role of protecting and controlling the knee joint (37). After ACL injury, mechanoreceptors and conduction pathways are injured, resulting in affected neuromuscular reflexes and ultimately, and affecting knee proprioception and stability (38). Studies have shown that after ACL injury, proprioceptors still exist at ACL remnant, which are involved in completing part of the proprioceptive function, and the number of receptors is positively correlated with the proprioceptive level of the knee joint (39, 40). Animal experiments showed that the number and density of proprioceptors were significantly higher after ACLR-R, comparing to standard ACLR (41). Angle reproduction and angle thresholds are commonly used clinically to assess patient proprioception. Two literatures were included in this study to evaluate the patient's postoperative proprioception, and both concluded that remnant preservation was beneficial to the recovery of proprioception. However, due to the differences in the measurement method and data recording method in detail, it is impossible to make a comprehensive analysis.
Knee stability was primarily assessed by physical examination (Lachman test and Pivot shift test) and KT1000/KT2000 arthrometer. Anteroposterior knee stability was assessed by the Lachman test and KT1000/KT2000 arthrometer, while rotational stability was assessed by the pivot shift test. Eight articles were included in this meta-analysis to assess knee stability, with three assess the Lachman test, six assess the pivot shift test, and seven assess the side-to-side anterior laxity by KT1000/KT2000 arthrometer. In this meta-analysis, it was concluded that remnant preservation could improve knee stability, but there was no significant change in postoperative subjective function scores. Some scholars have previously proposed that there is no relationship between objective measurement results and patients' subjective feelings, but objective measurements are superior in assessing patient knee stability (42).
Bone tunnel enlargement is one of the important indicators affecting the prognosis of ACLR. After ACLR, the bone is absorbed or dissolved under the combined stimulation of biological and mechanical factors (inflammatory factors, immune response, bone quality, bone tunnel position, graft fixation method, graft material, etc.), resulting in tibial tunnel enlargement. From a physical point of view, the tibial remnant preservation can seal the graft, separate the bone tunnel and joint cavity and reduce synovial fluid penetration into the bone tunnel (43). Tight wrapping of the graft by the remnant tissue reduces micromotion of the graft in the bone tunnel. From a biological healing point of view, the blood supply of the remnant can help the graft to revascularization and crawl instead, promotes the biological healing between the graft and the bone tunnel, and also reduces the micromotion between the graft and the bone tunnel (41). our meta-analysis shows a similar conclusion that the tibial tunnel enlargement in ACLR-R group was significantly lower than that in ACLR-S group. In addition, some scholars have proposed that poor bone tunnel positioning is also one of the reasons affecting bone tunnel enlargement. In the past, it was believed that preserving the remnant tissue could affect the localization of the bone tunnel. With improvements in surgical techniques, several studies have demonstrated that remnant does not affect bone tunnel positioning.
Cyclops lesions refers to the formation of a fibrovascular tissue nodule in the front of ACL graft. most of which are asymptomatic (44, 45). Cyclops syndrome is an important cause of reoperation after ACLR due to symptomatic extension dysfunction caused by cyclops impingement in the intercondylar fossa, with an overall incidence of about 2%–47% (22). Some scholars believe that preservation of ACL remnant increases the incidence of cyclops lesions after ACL reconstruction. However, the pathogenesis of cyclops lesions produced by ACL remnant is inconclusive and may be due to the development of fibers or inflammatory hyperplasia due to remnant stimulation. Also, there is no study could clearly demonstrate the association between remnant preservation and cyclops syndrome. Recent studies have shown that remnant preservation does not lead to an increased incidence of cyclops lesions, and even if it produces intercondylar notch hyperplasia, it does not affect the patient's postoperative clinical manifestations. A cohort study suggests that remnant preservation is not associated with symptomatic cyclops lesions, possibly because hypervascular scar tissue may also be generated after removal of the remnant (46). Removal of the remnant can cause increased bleeding, which can lead to scar tissue, and eventual cyclops lesions. But remnant preservation does not debride a large amount of remnant tissue, so reduced bleeding. It has even been shown that cyclops lesions do not lead to early postoperative extension dysfunction, but extension dysfunction will promote the proliferation of intercondylar notch nodules and ultimately form cyclops lesions. The amount of remnant preserved also had no effect on the generation of cyclops lesions. The results of this study also shows similar conclusions, at the second-look arthroscopy, remnant preservation did not cause an increase in cyclops lesions, and there was no significant difference in postoperative range of motion.
Four literatures analyzed the operation time and our analysis showed that the operation time was significantly longer in group A than in group B. Only one study showed no significant difference in operative time between the two groups, probably due to the fact that group ACLR-R performed remnant-tensioning single-bundle ACLR while group underwent double-bundle ACLR (18). The increase in surgery time may put the knee at increased risk of infection. Besides, the longer operation time means that the use of tourniquets is longer, and it is worth considering whether there is an impact on the recovery of muscle strength of the quadriceps muscle postoperatively.
Remnant preservation with tenision is believed to promote biological healing of the graft, as well as bring better preservation of mechanoreceptors due to residual mechanoreceptors receiving constant mechanical stimulation (47). Also, tenisioning the tibial remnant can avoid impingement, because it can prevent the loose injury ACL from curling up on the tibial footprint (47). Depending on whether tension was applied to the tibial remnant, we performed a subgroup analysis. The results showed that preservation without remnant tensioning had significant advantages in terms of Lysholm score, IKDC grade, Pivot-shift test and side-to-side difference, but group preservation with remnant tensioning does not show the significant superiority, comparing to Group ACLR-S. The results may be due to the points mentioned above, the differences in ACLR procedures, remnant placement, and amount and quality of remnant preservation (33, 40, 48, 49).
This study has some limitations. First, previous studies have shown that ACLR-R can preserve proprioceptions in the ACL remnant, and in this study, only two of the included articles underwent proprioception assessment, but we were not able to perform analyses and comparisons because of the inconsistent measurement method and data processing method. 2, The follow-up time of the studies included in this study was less than 3 years. 3, The technique of remnant preservation of the included articles was not uniform.
Despite these limitations, this study included eleven articles with a high level of evidence, and all were RCT and cohort studies, in the past 10 years. Although the techniques of remnant preservation are not uniform, this study is the first to provide the subgroup analysis of surgical techniques.
Conclusion
This meta-analysis concluded that remnant preservation significantly had better results in terms of patient functional score (Lysholm, IKDC), knee stability (Pivot shift test, postoperative side-to-side anterior laxity) and tibial tunnel enlargement. In terms of complications (incidence of Cyclops lesions, range of motion, re-injury rate), no significant differences were seen between the two groups. Although many studies concluded that remnant preservation could bring better synovial coverage, this meta-analysis indicated that there is insufficient evidence to support it, possibly due to different remnant preservation procedures.The potential risks associated with longer operation times are also worth considering.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
XH, FZ, ZW and ZM contributed to conception and design of the study; XH, FZ organized the database. XH, FZ performed the statistical analysis. XH wrote the first draft of the manuscript. XH, DZ, WC and SY wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Shenzhen Science and Technology Project (JCYJ20210324102607021), Shenzhen Double Chain Project for Innovation and Development Industry supported by Bureau of Industry and Information Technology of Shenzhen (201806081524201510), Shenzhen High-level Hospital Construction Fund (4004019); Human Resources and Social Security Bureau of Shenzhen, Postdoctoral Sustentation Fund (1040007), and Clinical Research Project of Shezhen Second People's Hospital (20200601027-FS01).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Prentice HA, Lind M, Mouton C, Persson A, Magnusson H, Gabr A, et al. Patient demographic and surgical characteristics in anterior cruciate ligament reconstruction: a description of registries from six countries. Br J Sports Med. (2018) 52(11):716–22. doi: 10.1136/bjsports-2017-098674
2. Murray MM, Fleming BC. Biology of anterior cruciate ligament injury and repair: kappa delta ann doner vaughn award paper 2013. J Orthop Res. (2013) 31(10):1501–6. doi: 10.1002/jor.22420
3. Mihelic R, Jurdana H, Jotanovic Z, Madjarevic T, Tudor A. Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17-20 years. Int Orthop. (2011) 35(7):1093–7. doi: 10.1007/s00264-011-1206-x
4. Ahn JH, Wang JH, Lee YS, Kim JG, Kang JH, Koh KH. Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: clinical and magnetic resonance imaging results. Arthroscopy. (2011) 27(8):1079–89. doi: 10.1016/j.arthro.2011.03.002
5. Leiter JR, Gourlay R, McRae S, de Korompay N, MacDonald PB. Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc. (2014) 22(5):1061–9. doi: 10.1007/s00167-013-2466-3
6. Amiel D, Kleiner JB, Akeson WH. The natural history of the anterior cruciate ligament autograft of patellar tendon origin. Am J Sports Med. (1986) 14(6):449–62. doi: 10.1177/036354658601400603
7. Mifune Y, Matsumoto T, Ota S, Nishimori M, Usas A, Kopf S, et al. Therapeutic potential of anterior cruciate ligament-derived stem cells for anterior cruciate ligament reconstruction. Cell Transplant. (2012) 21(8):1651–65. doi: 10.3727/096368912X647234
8. Matsumoto T, Kubo S, Sasaki K, Kawakami Y, Oka S, Sasaki H, et al. Acceleration of tendon-bone healing of anterior cruciate ligament graft using autologous ruptured tissue. Am J Sports Med. (2012) 40(6):1296–302. doi: 10.1177/0363546512439026
9. Choi S, Kim MK, Kwon YS, Kang H. Clinical and arthroscopic outcome of single bundle anterior cruciate ligament reconstruction: comparison of remnant preservation versus conventional technique. Knee. (2017) 24(5):1025–32. doi: 10.1016/j.knee.2017.05.012
10. Butt U, Khan ZA, Zahir N, Khan Z, Vuletic F, Shah I, et al. Histological and cellular evaluation of anterior cruciate ligament. Knee. (2020) 27(5):1510–8. doi: 10.1016/j.knee.2020.08.002
11. Li B, Wang YT, Bai LH, Wen Y. Changes of mechanoreceptors in different-state remnants of ruptured anterior cruciate ligament. Int Orthop. (2018) 42(11):2613–8. doi: 10.1007/s00264-018-3933-8
12. Delaloye JR, Murar J, Vieira TD, Franck F, Pioger C, Helfer L, et al. Knee extension deficit in the early postoperative period predisposes to cyclops syndrome after anterior cruciate ligament reconstruction: a risk factor analysis in 3633 patients from the SANTI study group database. Am J Sports Med. (2020) 48(3):565–72. doi: 10.1177/0363546519897064
13. Tie K, Chen L, Hu D, Wang H. The difference in clinical outcome of single-bundle anterior cruciate ligament reconstructions with and without remnant preservation: a meta-analysis. Knee. (2016) 23(4):566–74. doi: 10.1016/j.knee.2015.07.010
14. Ma T, Zeng C, Pan J, Zhao C, Fang H, Cai D. Remnant preservation in anterior cruciate ligament reconstruction versus standard techniques: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. (2017) 57(7-8):1014–22. doi: 10.23736/S0022-4707.16.06832-8
15. Annear PT, Rohr EJ, Hille DM, Gohil S, Ebert JR. No clinical difference in 10-year outcomes between standard and minimal graft debridement techniques in patients undergoing anterior cruciate ligament reconstruction using autologous hamstrings: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. (2019) 27(2):516–23. doi: 10.1007/s00167-018-5146-5
16. Demirağ B, Ermutlu C, Aydemir F, Durak K. A comparison of clinical outcome of augmentation and standard reconstruction techniques for partial anterior cruciate ligament tears. Eklem Hastalik Cerrahisi. (2012) 23(3):140–4. PMID: 23145756
17. Hong L, Li X, Zhang H, Liu X, Zhang J, Shen JW, et al. Anterior cruciate ligament reconstruction with remnant preservation: a prospective, randomized controlled study. Am J Sports Med. (2012) 40(12):2747–55. doi: 10.1177/0363546512461481
18. Kim JH, Oh E, Yoon YC, Lee DK, Lee SS, Wang JH. Remnant-Tensioning single-bundle anterior cruciate ligament reconstruction provides comparable stability to and better graft vascularity than double-bundle anterior cruciate ligament reconstruction in acute or subacute injury: a prospective randomized controlled study using dynamic contrast-enhanced magnetic resonance imaging. Arthroscopy. (2021) 37(1):209–21. doi: 10.1016/j.arthro.2020.08.035
19. Pujol N, Colombet P, Potel JF, Cucurulo T, Graveleau N, Hulet C, et al. Anterior cruciate ligament reconstruction in partial tear: selective anteromedial bundle reconstruction conserving the posterolateral remnant versus single-bundle anatomic ACL reconstruction: preliminary 1-year results of a prospective randomized study. Orthop Traumatol Surg Res. (2012) 98(8 Suppl):S171–7. doi: 10.1016/j.otsr.2012.09.007
20. Zhang Q, Zhang S, Cao X, Liu L, Liu Y, Li R. The effect of remnant preservation on tibial tunnel enlargement in ACL reconstruction with hamstring autograft: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. (2014) 22(1):166–73. doi: 10.1007/s00167-012-2341-7
21. Kim YK, Ahn JH, Yoo JD. A comparative study of clinical outcomes and second-Look arthroscopic findings between remnant-preserving Tibialis tendon allograft and hamstring tendon autograft in anterior cruciate ligament reconstruction: matched-pair design. Clin Orthop Surg. (2017) 9(4):424–31. doi: 10.4055/cios.2017.9.4.424
22. Kondo E, Yasuda K, Onodera J, Kawaguchi Y, Kitamura N. Effects of remnant tissue preservation on clinical and arthroscopic results after anatomic double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. (2015) 43(8):1882–92. doi: 10.1177/0363546515587713
23. Masuda T, Kondo E, Onodera J, Kitamura N, Inoue M, Nakamura E, et al. Effects of remnant tissue preservation on tunnel enlargement after anatomic double-bundle anterior cruciate ligament reconstruction using the hamstring tendon. Orthop J Sports Med. (2018) 6(12):1809858717. doi: 10.1177/2325967118811293
24. Nakayama H, Kambara S, Iseki T, Kanto R, Kurosaka K, Yoshiya S. Double-bundle anterior cruciate ligament reconstruction with and without remnant preservation - comparison of early postoperative outcomes and complications. KNEE. (2017) 24(5):1039–46. doi: 10.1016/j.knee.2017.05.008
25. Schenk S, Landsiedl F, Enenkel M. Arthroscopic single-stranded semitendinosus tendon- versus PDS-augmentation of reinserted acute femoral anterior cruciate ligament tears: 7 year follow-up study. Knee Surg Sports Traumatol Arthrosc. (2006) 14(4):318–24. doi: 10.1007/s00167-005-0669-y
26. Amiel D, Kleiner JB, Roux RD, Harwood FL, Akeson WH. The phenomenon of “ligamentization": anterior cruciate ligament reconstruction with autogenous patellar tendon. J Orthop Res. (1986) 4(2):162–72. doi: 10.1002/jor.1100040204
27. Lee JH, Bae DK, Song SJ, Cho SM, Yoon KH. Comparison of clinical results and second-look arthroscopy findings after arthroscopic anterior cruciate ligament reconstruction using 3 different types of grafts. Arthroscopy. (2010) 26(1):41–9. doi: 10.1016/j.arthro.2009.06.026
28. Sun L, Wu B, Tian M, Liu B, Luo Y. Comparison of graft healing in anterior cruciate ligament reconstruction with and without a preserved remnant in rabbits. Knee. (2013) 20(6):537–44. doi: 10.1016/j.knee.2013.09.004
29. Wu B, Zhao Z, Li S, Sun L. Preservation of remnant attachment improves graft healing in a rabbit model of anterior cruciate ligament reconstruction. Arthroscopy. (2013) 29(8):1362–71. doi: 10.1016/j.arthro.2013.05.010
30. Takahashi T, Kimura M, Hagiwara K, Ohsawa T, Takeshita K. The effect of remnant tissue preservation in anatomic double-bundle ACL reconstruction on knee stability and graft maturation. J Knee Surg. (2019) 32(6):565–76. doi: 10.1055/s-0038-1660513
31. Kim MK, Lee SR, Ha JK, Ra HJ, Kim SB, Kim JG. Comparison of second-look arthroscopic findings and clinical results according to the amount of preserved remnant in anterior cruciate ligament reconstruction. Knee. (2014) 21(3):774–8. doi: 10.1016/j.knee.2014.02.011
32. Yoo SH, Song EK, Shin YR, Kim SK, Seon JK. Comparison of clinical outcomes and second-look arthroscopic findings after ACL reconstruction using a hamstring autograft or a tibialis allograft. Knee Surg Sports Traumatol Arthrosc. (2017) 25(4):1290–7. doi: 10.1007/s00167-015-3955-3
33. Kim BH, Kim JI, Lee O, Lee KW, Lee MC, Han HS. Preservation of remnant with poor synovial coverage has no beneficial effect over remnant sacrifice in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. (2018) 26(8):2345–52. doi: 10.1007/s00167-017-4683-7
34. Gohil S, Annear PO, Breidahl W. Anterior cruciate ligament reconstruction using autologous double hamstrings: a comparison of standard versus minimal debridement techniques using MRI to assess revascularisation. A randomised prospective study with a one-year follow-up. J Bone Joint Surg Br. (2007) 89(9):1165–71. doi: 10.1302/0301-620X.89B9.19339
35. Okutan AE, Kalkisim M, Gurun E, Ayas MS, Aynaci O. Tibial slope, remnant preservation, and graft size are the most important factors affecting graft healing after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. (2022) 30(5):1584–93. doi: 10.1007/s00167-021-06660-2
36. Kruse LM, Gray B, Wright RW. Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. (2012) 94(19):1737–48. doi: 10.2106/JBJS.K.01246
37. Johansson H, Sjolander P, Sojka P. Receptors in the knee joint ligaments and their role in the biomechanics of the joint. Crit Rev Biomed Eng. (1991) 18(5):341–68. PMID: 2036801
38. Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. (2002) 73(3):330–4. doi: 10.1080/000164702320155356
39. Bali K, Dhillon MS, Vasistha RK, Kakkar N, Chana R, Prabhakar S. Efficacy of immunohistological methods in detecting functionally viable mechanoreceptors in the remnant stumps of injured anterior cruciate ligaments and its clinical importance. Knee Surg Sports Traumatol Arthrosc. (2012) 20(1):75–80. doi: 10.1007/s00167-011-1526-9
40. Kirizuki S, Matsumoto T, Ueha T, Uefuji A, Inokuchi T, Takayama K, et al. The influence of ruptured scar pattern on the healing potential of anterior cruciate ligament remnant cells. Am J Sports Med. (2018) 46(6):1382–8. doi: 10.1177/0363546518755753
41. Takahashi T, Kondo E, Yasuda K, Miyatake S, Kawaguchi Y, Onodera J, et al. Effects of remnant tissue preservation on the tendon graft in anterior cruciate ligament reconstruction: a biomechanical and histological study. Am J Sports Med. (2016) 44(7):1708–16. doi: 10.1177/0363546516643809
42. Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. (2004) 32(3):629–34. doi: 10.1177/0363546503261722
43. L'Insalata JC, Klatt B, Fu FH, Harner CD. Tunnel expansion following anterior cruciate ligament reconstruction: a comparison of hamstring and patellar tendon autografts. Knee Surg Sports Traumatol Arthrosc. (1997) 5(4):234–8. doi: 10.1007/s001670050056
44. Wang J, Ao Y. Analysis of different kinds of cyclops lesions with or without extension loss. Arthroscopy. (2009) 25(6):626–31. doi: 10.1016/j.arthro.2008.12.006
45. Cha J, Choi SH, Kwon JW, Lee SH, Ahn JH. Analysis of cyclops lesions after different anterior cruciate ligament reconstructions: a comparison of the single-bundle and remnant bundle preservation techniques. Skeletal Radiol. (2012) 41(8):997–1002. doi: 10.1007/s00256-011-1347-4
46. Webster KE, Murgier J, Feller JA, Klemm HJ, Devitt BM, Whitehead TS. Preservation of the tibial stump during anterior cruciate ligament reconstruction surgery did not increase the rate of surgery for symptomatic Cyclops lesions. Orthop J Sports Med. (2021) 9(4):1813039941. doi: 10.1177/2325967121992517
47. Jung YB, Jung HJ, Siti HT, Lee YS, Lee HJ, Lee SH, et al. Comparison of anterior cruciate ligament reconstruction with preservation only versus remnant tensioning technique. Arthroscopy. (2011) 27(9):1252–8. doi: 10.1016/j.arthro.2011.05.013
48. Franciozi CE, Minami FK, Ambra LF, Galvao P, Schumacher FC, Kubota MS. Remnant preserving ACL reconstruction with a functional remnant is related to improved laxity but not to improved clinical outcomes in comparison to a nonfunctional remnant. Knee Surg Sports Traumatol Arthrosc. (2022) 30(5):1543–51. doi: 10.1007/s00167-021-06572-1
Keywords: anterior cruciate ligament reconstruction, remnant preservation, meta-analysis, systematic review, anterior cruciate ligament
Citation: Xie H, Fu Z, Zhong M, Deng Z, Wang C, Sun Y and Zhu W (2022) Effects of remnant preservation in anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Front. Surg. 9:952930. doi: 10.3389/fsurg.2022.952930
Received: 27 May 2022; Accepted: 15 August 2022;
Published: 1 September 2022.
Edited by:
Rocco Papalia, Campus Bio-Medico University, ItalyReviewed by:
Guglielmo Torre, Campus Bio-Medico University, ItalyZhenxing Shao, Peking University Third Hospital, China
© 2022 Xie, Fu, Zhong, Deng, Wang, Sun and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weimin Zhu szhzwm@email.szu.edu.cn
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Huanyu Xie1
Huanyu Xie1  Mingjin Zhong
Mingjin Zhong Zhenhan Deng
Zhenhan Deng Weimin Zhu
Weimin Zhu