Telemedicine and Telehealth in Urology: Uptake, Impact and Barriers to Clinical Adoption
- 1Department of Mechanical and Industrial Engineering, Manipal Institute of Technology, Manipal Academy of Higher Education, Manipal, Karnataka, India
- 2iTRUE (International Training and Research in Uro-oncology and Endourology) Group, Manipal, Karnataka, India
- 3Gandhi Medical College, Kaloji Narayana Rao University of Health Sciences, Secunderabad, Telangana, India
- 4Department of Computer Science and Engineering, Manipal Institute of Technology, Manipal Academy of Higher Education, Manipal, Karnataka, India
- 5Robotics and Urooncology, Max Hospital and Max Institute of Cancer Care, New Delhi, India
- 6Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India
- 7Department of Urology, Father Muller Medical College, Mangalore, Karnataka, India
- 8A.J. Institute of Medical Sciences and Research Centre, Mangalore, Karnataka, India
- 9Department of Urology, Freeman Hospital, Newcastle upon Tyne, United Kingdom
- 10Department of Urology, Government Medical College Hospital, Guwahati, India
- 11Department of Urology, University Hospital Southampton NHS Trust, Southampton, United Kingdom
- 12Department of Urology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India
- 13Department of Information and Communication Technology, Manipal Institute of Technology, Manipal Academy of Higher Education, Manipal, Karnataka, India
- 14Department of Urology, Jagiellonian University in Krakow, Kraków, Poland
Telemedicine has great potential in urology as a strong medium for providing patients with continuous high-quality urological care despite the hurdles involved in its implementation. Both clinicians and patients are crucial factors in determining the success of tele-consults in terms of simplicity of use and overall satisfaction. For it to be successfully incorporated into routine urological practice, rigorous training and evidence-based recommendations are lacking. If these issues are addressed, they can provide a significant impetus for future tele-consults in urology and their successful deployment, even beyond the pandemic, to assure safer and more environment-friendly patient management.
Introduction
The COVID-19 pandemic has nudged more surgeons and practitioners into inculcating telemedicine into their routine practice. Although used interchangeably, telehealth may strictly differ from telemedicine in that it encompasses a larger range of remote healthcare services than telemedicine. In addition to clinical services, telehealth can refer to remote non-clinical services such as provider training, administrative meetings, and continuing medical education. While there are still certain challenges in incorporating telemedicine into mainstream surgical practice, we wanted to explore the extent to which clinicians safely and effectively incorporate telemedicine. Also, the aspects of patient care that are best addressed via telemedicine and how this transition affects physician-patient relationships and issues such as its impact on climate and cost.
Telemedicine offers the advantage of being a practical, alternate solution, especially during times of pandemic, to significantly reduce the transmissibility of communicable disease, ensuring better protection for physicians and patients (1). According to a study from Borchert et al., urologists followed a triage mechanism concerning the implementation of telemedicine to both COVID-19 and non-COVID-19 patients, emphasising that consultations can be managed in a patient and physician safety-conscious manner, reducing transmissibility while ensuring satisfactory consults (2). Some urologists witnessed voluntary cancellation of in-person visits by patients themselves who opted for tele-consults (1). This emphasises the fact that telehealth has gained favourability among patients who are anxious about disease transmission, especially in the setting of the current pandemic.
A literature search was done for English language articles over the last two decades from 2020 to 2021, and present in Scopus, Pubmed, MEDLINE, Clinicaltrials.gov, Web of Science (WoS), and Google Scholar. A total of 38 articles were identified on the initial search. After screening, 17 articles were identified as related to uptake, impact, and barriers among the clinicians for the adoption of telemedicine in urology. The search was conducted by using a combination of the following terms: “telemedicine”, “clinicians”, “urology”, “telehealth”, “prostatic neoplasms”, “urinary bladder neoplasms”, “kidney neoplasms”, “testicular neoplasms”, “prostatic hyperplasia”, “urinary calculi”, “sexual dysfunction”, “physiological”, “erectile dysfunction”, “infertility”, “urinary tract infections”, “urinary incontinence”, “prostate cancer”, “bladder cancer”, “kidney cancer”, “testis cancer”, “benign prostatic hyperplasia”, “urinary stone”, “sexual dysfunction”, “erectile dysfunction”, “infertility”, and “genitourinary trauma”.
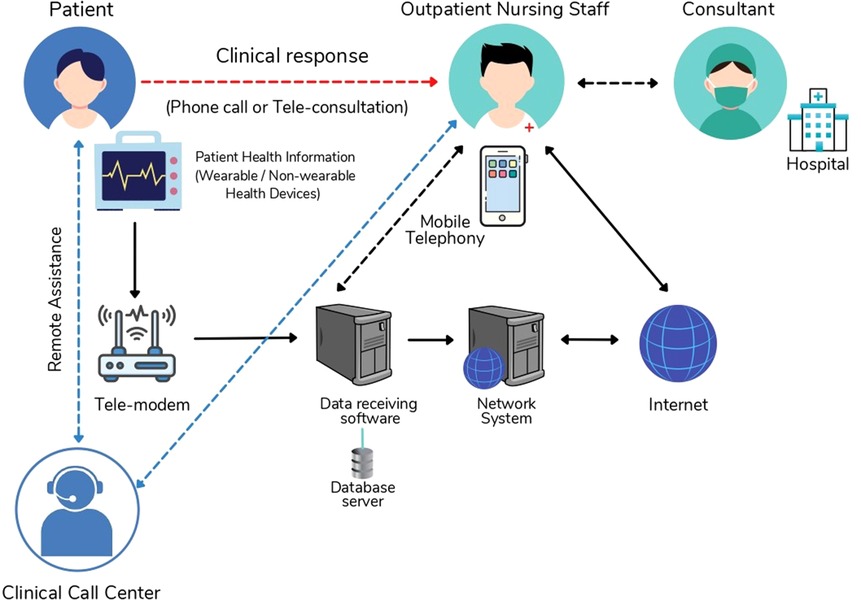
Telemedicine has also offered the chance to address sexual health-related urologic problems, in a manner that is comfortable to the patients (3). Urological cancer care and counseling were as effective as in-person visits in one study (4). Another major advantage of telemedicine compared to routine clinic visits was the reduction in carbon footprint attributed to such a transition, emphasising the fact that telemedicine can help contribute to a more environment-friendly clinical practice (5, 6). Figure 1 shows the network architecture to establish a connection between patient and consultant using a telehealth application.
Physicians are keen to incorporate telemedicine into routine urology practise, but there is still a need for more active support and active guidelines with formal training (7, 8). Barriers to accessing appropriate and adequate technology remain an important concern that needs to be addressed (9). Patients who were not English proficient and those that came from areas with an unstable Internet connection, were less likely to use telemedicine urology consults (3). Similarly, patients were keen at the outset to take up telemedicine due to an unclear understanding of indications and concerns related to reimbursement (7, 9). Among the users that adopted telemedicine, however, there was a significant degree of satisfaction with health information received via this medium.
Data security and breaches in confidential health information are key issues that were identified and need vigilance and improvements (3). Additionally, there might be some inaccuracies and loss of crucial clinical information during transmission of information via telephone consults (1). While there are challenges in implementation, there was a good response in adapting telemedicine into clinical practice. A cross-sectional study found that since the start of the pandemic, urologists' implementation of telemedicine has increased significantly, with one survey suggesting that it nearly tripled compared to pre-pandemic times (9). This exemplifies the need and urgency with which such practices were incorporated and might be a pointer to a similar response in future pandemic and non-pandemic times.
Through this review, we try to address the factors affecting the uptake of telemedicine and telehealth in routine urological practise, the impact it has had on the delivery of patient care, and the several challenges and concerns faced by urologists in its adoption.
Role in Preventing Transmission of Communicable Diseases
Before COVID-19, the role of telehealth consultations was minimal in routine urological practice. Several studies have therefore been undertaken to evaluate the suitability of incorporating telehealth in urology. A global cross-sectional study done during the pandemic tried to address urologists' perceptions of the utility of in-person clinic appointments, the feasibility of substituting traditional care with telemedicine, and the current barriers to its implementation. It found that close to 80% (n = 244) of urologists were keen on continuing the use of tele-consults in their practice after the pandemic (9). The study also found that globally telemedicine in urology tripled, compared to the pre-pandemic times. Urologists however identified three major barriers in the implementation of tele-consults, patients' inability to understand and effectively utilize this technology, lack of access to the required technology, and reimbursement concerns.
Borchert et al. found that adopting a triage system with respect to the risk, stratifying patients in urgent need of urological care, COVID-19 positive and COVID-19 negative patients, could show promise in safely caring for patients, whilst preventing communicable disease transmission (2). Team members from urology care did not contract the virus and could safely attend to patients at the same time while employing this strategy.
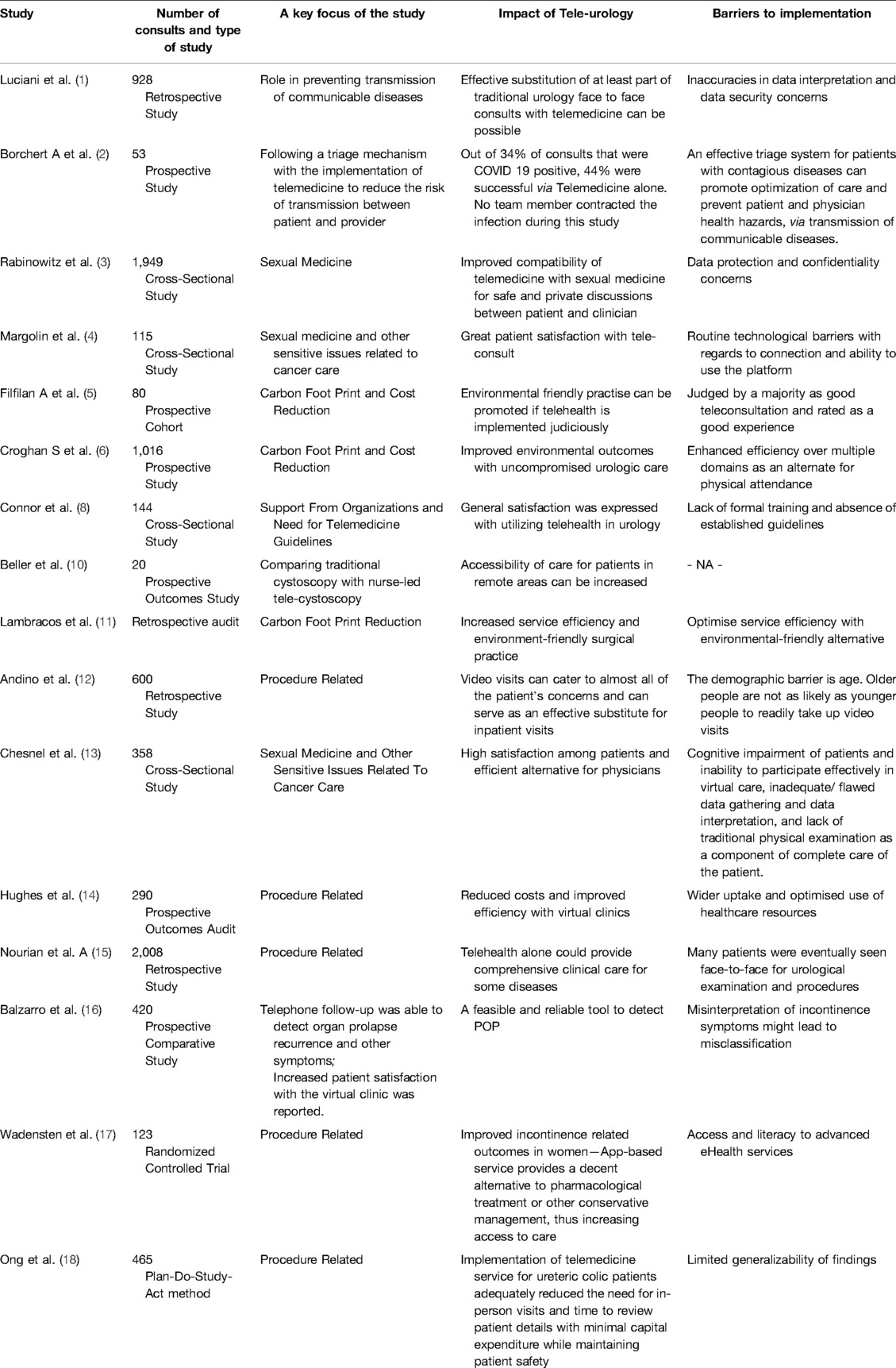
A study from Northern Italy concurred with the same observation, where Luciani et al. found that a “targeted virtual approach” would prove to be of greater benefit over the cancellation, especially in patients with advanced urological malignancies (1). The study also identified that inaccuracies might creep in during tele-consults and crucial data might be missed out on, and recommended that it was imperative to maintain robust electric health records and services from expert staff members to tackle this issue. Table 1 summarizes some of the key focus, findings of the studies discussed, and perspectives of urologists towards acceptance and implementation of telemedicine in their clinical and surgical practices.
Carbon Footprint, Time and Cost Reduction
A reduction in inpatient time and cost as well as significant drops in CO2 emissions can be an impetus to adopting a more environmentally friendly practice. The impact of telehealth on reducing greenhouse gas emissions was studied and it was found that adopting tele-consults reduced transport to the tune of 52 miles per patient. This study alone saw a net decrease in CO2 emission by 1.1 tonnes (1). Croghan et al. in their study estimated that adopting tele-consults saved 1,257.8 h of patient travel time and a 6-tonne reduction in carbon emissions over 3 months (6). The study also evaluated the utility of virtual clinics across several other domains in terms of effectiveness and found that offering telehealth options to patients might prove just as valuable as in-person visits.
Beller et al., in their observational retrospective study of the National Hospital Response Framework Alert, found that virtual phone consults increased by 274% while saving each patient an estimated 22.7 km of travel on average. The study points toward how service efficiency can be optimised while providing an environmentally friendly alternative for routine clinical practice (10). Prospective audit of virtual clinic visits of patients was done over 6 years and found that virtual consults reduced the cost per clinic appointment by 93%, equating to a total saving of £12,006 during the study (11). This study also found that nurse-led virtual clinics provided a safe follow-up and also allowed to substantially reduce the cost of treatment by meticulously selecting between virtual discharge or an in-patient face-to-face visit, on a case-to-case basis (11).
The ureteric colic assessment was simplified by adapting tele-consults. Andino et al., in their study from a specialty center in Singapore, used telemedicine workflow as a quality improvement study using the PDSA method. They showed that ureteric colic telemedicine service reduced the number of face-to-face consultations and time to review patient data, without compromising patient safety. The wait time for patients was considerably reduced by adopting this approach. The study also found that patients saved on the cost and time spent on travel and follow-up clinic visits. At the same time, we're able to get earlier reviews at an average of 30.3 days, a significant improvement from the previous 60 to 90 days. This study also received great patient satisfaction (12).
Sexual Medicine and Other Sensitive Issues
Telemedicine in sexual health-related urologic concerns received positive appreciation from patients and urologists alike. There was a steady increase in the number of male sexual health-related consults during the COVID-19 pandemic. Telemedicine helps create a comfort zone for the clinician and patient to discuss sensitive topics, such as impotence and infertility. Croghan et al. in their study of 115 patients, found that 77% of patients and 70% of physicians reported being “extremely satisfied” with most of the components of telemedicine encounters including communication, the scope for shared decision making, time devoted to patient concerns and overall effectiveness and convenience (6). Almost 78% of patients and 85% of physicians “strongly agreed” that they were able to comprehensively discuss sensitive topics about cancer care, uncompromisingly as in an in-person visit (6). This study also identified technological barriers to be the key limiting factor to the successful implementation of such encounters.
Rabinowitz et al. (3) tried to establish patient satisfaction in tele-urology consults in the domain of neuro-urology in 358 patients, and found that the mean efficiency of the telephone consultation was 9.3/10 (±1.5) (3). The mean global satisfaction was 9.0/10 (±1.3). However, this study found that a sizeable number preferred an in-person consult is available to them. This study found that cognitive impairment, difficulty to obtain key patient details, and lack of the traditional physical examination were unfavorable to the efficiency of teleconsultation.
Guidelines for Successful Implementation
A German study from Chesnel et al. tried to ascertain the suitability and comfort of telemedicine consults among urologists and patients (13). This study found that patients largely favoured telemedicine consults and that users were more likely to implement telemedicine after the COVID-19 pandemic. However, the usage among German urologists remains low and they feel that there needs to be active support in the form of Societal guidelines for better implementation. Among patients that were offered tele-consults, nonusers were concerned with unclear indications for telemedicine and lesser reimbursements during telemedicine than in-person visitations.
Rodler et al. identified training in telemedicine among urologists as a key determinant of the success of tele-consults. Experience with telemedicine was assessed in 2 categories: technical determinants and patient communication. Variables were rated using a 5-point Likert Scale. Providers were more concerned about lack of adequate training in billing, rather than deficits in communication and equipment use (7). 87% of providers felt at ease while discussing sensitive topics using telehealth, while only 55% felt comfortable using telehealth (p < 0.001). Therefore, this study identifies that the providers would benefit from focused training in telemedicine for a successful implementation.
Procedure-Related Concerns
Connor et al. conducted a study to evaluate the feasibility of using nurse-led cystoscopy services and virtual patient consults via telemedicine, where urologic advanced practitioners performed cystoscopies that were interpreted virtually by urologists. This study found that such a model can improve access to urology consults for patients in remote locations and may lead to greater acceptance of nurse-led procedures (8).
Lambracos et al. did a study to determine the feasibility, reliability, and overall patient satisfaction of telephonic follow-up in women treated for stress urinary incontinence and pelvic organ prolapse. The study found that there might be a misinterpretation of initial symptoms and arriving at these diagnoses to start with, but the overall follow-up was feasible and reliable in women not reporting incontinence. This highlights a limitation of such tele-consults while dealing with incontinence-related problems (11).
Hughes et al. (14) in their study established the feasibility of video visits by patients as opposed to in-person visits and used the metric of “revisit” rates to determine success. They found that revisit rates were more when the initial visit was in an in-patient setting as compared to a virtual clinic approach. This can be attributed to previously scheduled in-patient appointments. Revisit rates due to medical concerns were similar across telehealth and in-person visits.
Patients with urological benign diseases whose clinic visits had been cancelled due to the COVID-19 pandemic were evaluated by Checcucci et al. (19) using telemedicine with phone-call visits as a feasible method for follow-up care. A telephone call was made to 607 of the individuals on the list. Many instances (531/607) revealed no need for in-person or emergency appointments since the symptoms were stable. 81.5 percent of patients (495/607) were more concerned about the possibility of infection than their urological disease. When it came to patient satisfaction with the utility of phone visits (rated at 4/5), the median score was 5/5 for the comprehensibility as well as ease of communication of exams, while only 53% of interviewees had access to the basic tools needed to conduct a real telemedicine consultation in accordance with the guidelines. For infectious disorders like COVID-19, the use of telemedicine reduces the frequency of needless visits to healthcare facilities and is a significant strategy in limiting the risk of transmission. A digitalization process must be pursued by infrastructures, health care providers, and patients in order to make televisit more widely available.
The clinical pathways for urology patients during the COVID-19 pandemic were discussed in a study by Simonato et al. (20). Since the outbreak of the COVID-19 pandemic, several urology centres have had to reorganise their clinical operations due to the massive reallocation of health resources. Preoperative, intraoperative, and postoperative care pathways have been established by an Italian group of urologists for the treatment of COVID-19 pandemic patients undergoing urgent urological surgeries or non-deferrable oncological interventions in Italy. In order to reduce the number of hospitalizations and thus the risk of infection, the diagnostic and staging process must be simplified. The recommendation suggested is that an accurate triage for COVID-19 symptoms be undertaken by telephone both before and during hospitalisation, as nasopharyngeal swabs are not mandated by tight laws. To make it easier for patients to return home and remain there after their hospital stay, we recommend that as many instructions as possible be given to them. Patients should be discharged from the hospital in a stable and healthy state in order to reduce the likelihood of a return visit. Post-discharge checks should be scaled back or rescheduled, and a reliable communication mechanism for telemonitoring patients should be put in place.
Challenges of Telemedicine and Future Perspectives
Telemedicine holds great promise in changing the way urology consults are carried out. There seems to be time and cost reduction, with satisfactory patient and clinician outcomes, suggesting that adopting such a practice holds a great scope in a future way beyond the pandemic. Carbon emission reduction and a greener surgical practice are added advantages of adopting such a practice. On the same token there exist challenges and barriers in the form of miscommunication, data privacy, security concerns, and lack of adequate training and guidelines, all of which needs to be addressed to ensure the success of such novel clinical practice (9).
In low-resource settings, in particular, wherein individuals lack sufficient diagnostic opportunities, have limited access to medical services due to financial conditions, a general lack of interest in healthcare, and their incapacity to get to the hospital on their own—particularly in the case of seniors living alone—along with a dire need for preventative measures and ongoing medical care in this group, telemedicine-based services has been a welcome change to address the constraints.
There is a paucity of literature concerning the use of telemedicine before the COVID-19 pandemic, which is a major limitation of his study. There is also inadequacy stemming from a lack of long-term follow-up in patients who were shifted to receive telehealth consultations and would require longitudinal studies to better study the potential benefits of telemedicine.
Conclusion
The review identifies that telemedicine in urology holds promise as a powerful medium for the delivery of uninterrupted high-quality urological care to patients. Patients play an important role as a determinant in the success of tele-consults with regards to ease of use and ultimate patient satisfaction. The primary limiting factors for the effective implementation among urologists lie in the fact that there is inadequate formal training and evidence-based guidelines to support its successful implementation. These concerns if addressed can prove to have a great impetus for future tele-consults in urology and its effective deployment, even after the pandemic, to ensure safer and more environment-friendly clinical and surgical practices.
Author Contributions
BH, NN, AP, and BS contributed to the conception and design of the study. EK, ¸ST, AP, PJ-J, and DM organized the database and wrote the first draft of the manuscript. NN, SK, ¸ST, RB, SM, and BH wrote sections of the manuscript. PC, AP, EK, and BS critically reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Luciani LG, Mattevi D, Cai T, Giusti G, Proietti S, Malossini G. Teleurology in the time of COVID-19 pandemic: here to stay? Urology. (2020) 140:4–6. doi: 10.1016/j.urology.2020.04.004
2. Borchert A, Baumgarten L, Dalela D, Jamil M, Budzyn J, Kovacevic N, et al. Managing urology consultations during COVID-19 pandemic: application of a structured care pathway. Urology. (2020) 141:7–11. doi: 10.1016/j.urology.2020.04.059
3. Rabinowitz MJ, Kohn TP, Ellimoottil C, Alam R, Liu JL, Herati AS. The impact of telemedicine on sexual medicine at a major academic center during the COVID-19 pandemic. Sex Med. (2021) 9:100366. doi: 10.1016/j.esxm.2021.100366
4. Margolin EJ, Pina Martina LA, Miles CH, Wenske S, McKiernan JM, DeCastro GJ, et al. Telemedicine in management of genitourinary malignancies: patient and physician perspectives. Urol Oncol: Semin Orig Invest. (2021) 39:480–6. doi: 10.1016/j.urolonc.2021.04.003
5. Filfilan A, Anract J, Chartier-Kastler E, Parra J, Vaessen C, de La Taille A, et al. Positive environmental impact of remote teleconsultation in urology during the COVID-19 pandemic in a highly populated area. Prog Urol. (2021) 31:1133–8. doi: 10.1016/j.purol.2021.08.036
6. Croghan SM, Rohan P, Considine S, Salloum A, Smyth L, Ahmad I, et al. Time, cost and carbon-efficiency: a silver lining of COVID era virtual urology clinics? Ann R Coll Surg Engl. (2021) 103(8):599–603. doi: 10.1308/rcsann.2021.0097
7. Rodler S, Schütz JM, Styn A, Weinhold P, Casucelli J, Eismann L, et al. Mapping telemedicine in German Private Practice Urological Care: implications for transitioning beyond the COVID-19 pandemic. Urol Int. (2021) 105:650–6. doi: 10.1159/000515982
8. Connor J, Zheng Y, Houle K, Cox L. Adopting telehealth during the COVID-19 ERA: the urologist’s perspective. Urology. (2021) 156:289–95. doi: 10.1016/j.urology.2021.03.051
9. Dubin JM, Wyant WA, Balaji NC, Ong WLK, Kettache RH, Haffaf M, et al. Telemedicine usage among urologists during the COVID-19 pandemic: cross-sectional study. J Med Internet Res. (2020) 22:1–12. doi: 10.2196/21875
10. Beller H, Lobo JM, Horton BJ, Sims T, Corey T, Tyson T, et al. Adapting nurse-led cystoscopy experience to the United States: tele-cystoscopy a possible compromise? Int J Urol Nurs. (2019) 13:81–6. doi: 10.1111/ijun.12197
11. Lambracos S, Yuan L, Kennedy-Smith A. COVID-19 and the impact on urology service provision at Capital & Coast District Health Board. N Z Med J. (2021) 134(1538):111–9.34239150
12. Andino JJ, Lingaya M-A, Daignault-Newton S, Shah PK, Ellimoottil C. Video visits as a substitute for urological clinic visits. Urology. (2020) 144:46–51. doi: 10.1016/j.urology.2020.05.080
13. Chesnel C, Hentzen C, Le Breton F, Turmel N, Tan E, Haddad R, et al. Efficiency and satisfaction with telephone consultation of follow-up patients in neuro-urology: experience of the COVID-19 pandemic. Neurourol Urodyn. (2021) 40:929–37. doi: 10.1002/nau.24651
14. Hughes T, Pietropaolo A, Archer M, Davis T, Tear L, Somani BK. Lessons learnt (clinical outcomes and cost savings) from Virtual Stone Clinic and their application in the era post-COVID-19: prospective outcomes over a 6-year period from a University Teaching Hospital. J Endourol. (2021) 35:200–5. doi: 10.1089/end.2020.0708
15. Nourian A, Smith N, Kleinman L, Boxer R, Shelton JB. A 5-year single-institution experience integrating telehealth into Urologic Care Delivery. Telemed e-Health. (2021) 27:997–1002. doi: 10.1089/tmj.2020.0267
16. Balzarro M, Rubilotta E, Trabacchin N, Mancini V, Costantini E, Artibani W, et al. A prospective comparative study of the feasibility and reliability of telephone follow-up in female urology: the patient home office novel evaluation (phone) study. Urology. (2020) 136:82–7. doi: 10.1016/j.urology.2019.10.021
17. Wadensten T, Nyström E, Franzén K, Lindam A, Wasteson E, Samuelsson E. A mobile app for self-management of urgency and mixed urinary incontinence in women: randomized controlled trial. J Med Internet Res. (2021) 23(4):e19439. doi: 10.2196/19439
18. Ong CS, Lu J, Tan YQ, Tan LG, Tiong HY. Implementation of a ureteric colic telemedicine service: a mixed methods quality improvement study. Urology. (2021) 147:14–20. doi: 10.1016/j.urology.2020.10.010
19. Checcucci E, De Luca S, Alessio P, Verri P, Granato S, De Cillis S, et al. Implementing telemedicine for the management of benign urologic conditions: a single centre experience in Italy. World J Urol. (2021) 39(8):3109–15. doi: 10.1007/s00345-020-03536-x
Keywords: telemedicine, urology, telehealth, COVID-19, patient satisfaction
Citation: Naik N, Nandyal SR, Nayak SG, Shah M, Ibrahim S, Hameed BMZ, Patil A, Suresh G, Shetty PA, Rai BP, TP R, Rice P, Reddy SJ, Bhat N, Garg D, Chlosta P and Somani BK (2022) Telemedicine and Telehealth in Urology: Uptake, Impact and Barriers to Clinical Adoption. Front. Surg. 9:911206. doi: 10.3389/fsurg.2022.911206
Received: 2 April 2022; Accepted: 13 June 2022;
Published: 30 June 2022.
Edited by:
Nicola Pavan, University of Trieste, ItalyReviewed by:
Richard Boxer, University of California, Los Angeles, United StatesMatteo Manfredi, University of Turin, Italy
Alchiede Simonato, University of Palermo, Italy
Copyright © 2022 Naik, Nandyal, Nayak, Shah, Ibrahim, Hameed, Patil, Suresh, Shetty, Rai, TP, Rice, Reddy, Bhat, Garg, Chłosta and Somani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: B. M. Zeeshan Hameed zeeshanhameedbm@gmail.com
Specialty section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
 Nithesh Naik
Nithesh Naik Shreyas Raghavan Nandyal
Shreyas Raghavan Nandyal Sanjana Ganesh Nayak
Sanjana Ganesh Nayak Milap Shah
Milap Shah Sufyan Ibrahim
Sufyan Ibrahim B. M. Zeeshan Hameed
B. M. Zeeshan Hameed Ananth Patil8
Ananth Patil8  Pritam A. Shetty
Pritam A. Shetty Bhavan Prasad Rai
Bhavan Prasad Rai Patrick Rice
Patrick Rice Suraj Jayadeva Reddy
Suraj Jayadeva Reddy Bhaskar K. Somani
Bhaskar K. Somani