Postoperative Recovery Outcomes for Obese Patients Undergoing General Anesthesia: A Meta-Analysis of Randomized Controlled Trials
- Department of Anesthesiology, Henan Provincial People’s Hospital, Henan University, China
Purpose: This study was performed to assess the postoperative recovery outcomes in obese patients undergoing general anesthesia.
Methods: The eligible studies were identified from PubMed, EmBase, and the Cochrane library until December 2020. The standard mean differences (SMDs) with 95% confidence intervals (CIs) were used to calculate the role of desflurane, sevoflurane, and propofol on recovery outcomes, and the analyses using the random-effects model.
Results: Eleven randomized controlled trials involving 713 obese patients undergoing general anesthesia were selected for final meta-analysis. We noted desflurane was associated with a shorter time to eye-opening than sevoflurane (SMD: −0.86; 95% CI, −1.43 to −0.28; P = 0.003). The use of desflurane with shorter time to extubation as compared with propofol (SMD: −1.13; 95% CI, −1.52 to −0.73; P < 0.001) or sevoflurane (SMD: −1.19; 95% CI, −2.15 to −0.22; P = 0.016), while sevoflurane was associated with longer time to extubation as compared with propofol (SMD: 1.47; 95% CI, 1.03 to 1.91; P < 0.001). Desflurane were associated with shorter time to stating name as compared with propofol (SMD: −1.40; 95% CI, −2.32 to −0.48; P = 0.003) or sevoflurane (SMD: −2.09; 95% CI, −3.33 to −0.85; P = 0.001). In addition, desflurane was associated with a longer time for orientation to place as compared with propofol (SMD: 0.65; 95% CI, 0.22 to 1.07; P = 0.003), while desflurane with shorter time for orientation to place as compared with sevoflurane (SMD: −0.88; 95% CI, −1.46 to −0.30; P = 0.003).
Conclusions: The use of desflurane could provide better recovery outcomes in obese patients undergoing general anesthesia. Further large-scale trials should be comparison the long-term effectiveness of various anesthetics.
Introduction
Obesity is considered a major epidemiological problem and the number of obese persons reached over 600 million in 2014 (1). The treatment of obese patients and related complications remains a challenge, especially in anesthesiology. The potential complications of obesity, include insulin-resistance, diabetes, cardiovascular disease, hormonal imbalance, glomerulopathy or neoplasia, and other disorders, which play an important role in respiratory and hemodynamic nature (2–4). The potential adverse effects include obstructive sleep apnoea, hypoventilation syndrome, or postoperative atelectasis (5). Moreover, obese patients were associated with an increased risk of adverse respiratory events after general anesthesia (6). Therefore, obese patients required careful preoperative evaluation and intraoperative management to ensure better recovery outcomes and fewer adverse events (7).
Nowadays, a variety of anesthetics are already used for morbidly obese patients, while no single strategy has shown more beneficial effects than others. Desflurane, sevoflurane, and propofol are widely used for obese patients, and rapid postoperative recovery is related to earlier maintenance of airways and associated with effective protection against aspiration and greater oxygenation (8). However, the use of longer-acting opioids could bias the postoperative recovery outcomes. Numerous studies have already compared the postoperative recovery outcomes of desflurane, sevoflurane, and propofol for obese patients (9–19). We, therefore, performed a systematic review and meta-analysis to compare the effects of desflurane, sevoflurane, and propofol on recovery outcomes for obese patients.
Methods
Data Sources, Search Strategy, and Selection Criteria
The reporting and conducting of this study were in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Statement (20). The query task for systematic reviews was to collect randomized controlled trials (RCTs) that compared the role of desflurane, sevoflurane, and propofol on recovery outcomes for obese patients undergoing general anesthesia was eligible in this study, and the publication language was not restricted. The potentially relevant articles were searched in PubMed, EmBase, and the Cochrane Library from January 2000 to December 2020, and the following search terms were used through Medical Subject Heading to text words: (“obese” OR “overweight” OR “bariatric surgery” OR “body mass index”) AND (“anesthesia” OR “anesthetic” OR “desflurane” OR “sevoflurane” OR “propofol” OR “total intravenous anesthesia” OR “general anesthesia”). Meta-analyses were screened out if they did not meet the inclusion criteria listed later, first at the title/abstract level, and later at the methods section level if necessary. We also reviewed the reference lists in retrieved studies for any further eligible studies.
The details of inclusion criteria were: (1) Participants: obese patients undergoing general anesthesia; (2) Intervention and control: any 2 of desflurane, sevoflurane, and propofol; (3) Outcome: time to eye opening, time to extubation, time to stating name, time for orientation to place, and time required for hand squeezing; and (4) Study design: the study had to have RCT design. The relevance of studies was assessed by reviewing the title and abstracts, and the full-text evaluations were evaluated to obtain whether potentially relevant trials reported an outcome of interest. The study selection was independently double-checked the inclusion and exclusion criteria by two reviewers, and the conflicts between reviewers were resolved by group discussion until a consensus was reached.
Data Collection and Quality Assessment
The following data items in each included study were independently extracted by two reviewers: first author’s name, publication year, region, sample size, mean age, male proportion, body mass index (BMI), anesthesia technique, surgical technique, and reported outcomes. Then the quality of each trial was assessed using the Jadad scale by the same two reviewers, which was based on randomization, blinding, allocation concealment, withdrawals and dropouts, and use of intention-to-treat analysis (21). Any disagreement between the two reviewers were settled by an additional reviewer referring to the full text of the articles.
Statistical Analysis
The effectiveness of a treatment on postoperative recovery outcomes was assigned as a continuous variable, and the standard mean difference (SMD) with a 95% confidence interval (CI) was calculated before data pooling. Then the random-effects model was used to calculate pooled SMD and 95% CI for comparison of the postoperative recovery outcomes after using desflurane, sevoflurane, or propofol (22, 23). Heterogeneity across included trials was evaluated using the I2 and Q statistic, and the significant heterogeneity was defined as I2 > 50.0% or P < 0.10 (24, 25). Subgroup analyses were also conducted for the postoperative recovery outcomes of desflurane versus sevoflurane according to mean age, male proportion, BMI, and surgical technique, and the difference between subgroup analyses was assessed by using the interaction t-test, which assumed the distribution of effect estimates were normal (26). Publication bias for investigated outcomes was assessed by using the funnel plot, Egger, and Begg tests (27, 28). The P-value for pooled conclusions is 2-sided, and the inspection level was 0.05. All of the analyses in this study were conducted by using the software STATA (version 10.0; Stata Corporation, College Station, TX, USA).
Results
Literature Search
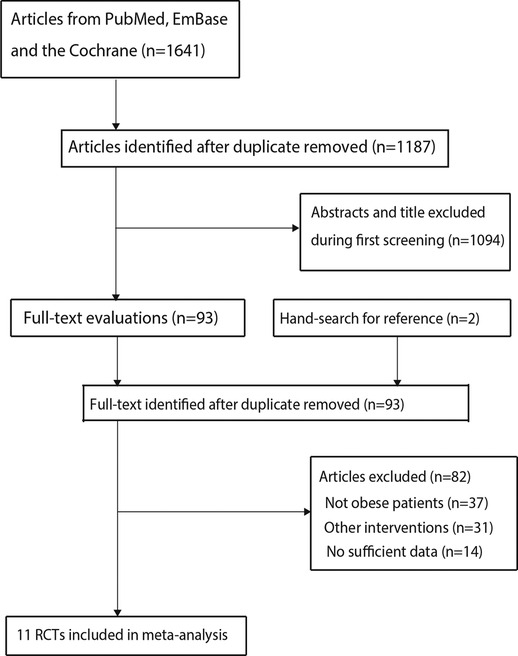
The electronic searches yielded 1,641 articles, and the 1,187 articles were retained after duplicate articles were removed. A total of 1,094 studies were excluded by reviewing their titles and abstracts because they reported irrelevant. The remaining 93 potentially eligible studies were retrieved, and 82 studies were removed after detailed evaluations: patients not obese (n = 37), other interventions (n = 31), and lacking sufficient data (n = 14). Reviewing the reference lists of the remaining studies did not find any new eligible studies. Finally, 11 RCTs were selected for meta-analysis (9–19), and the details of the study selection process are shown in Figure 1.
Study Characteristics
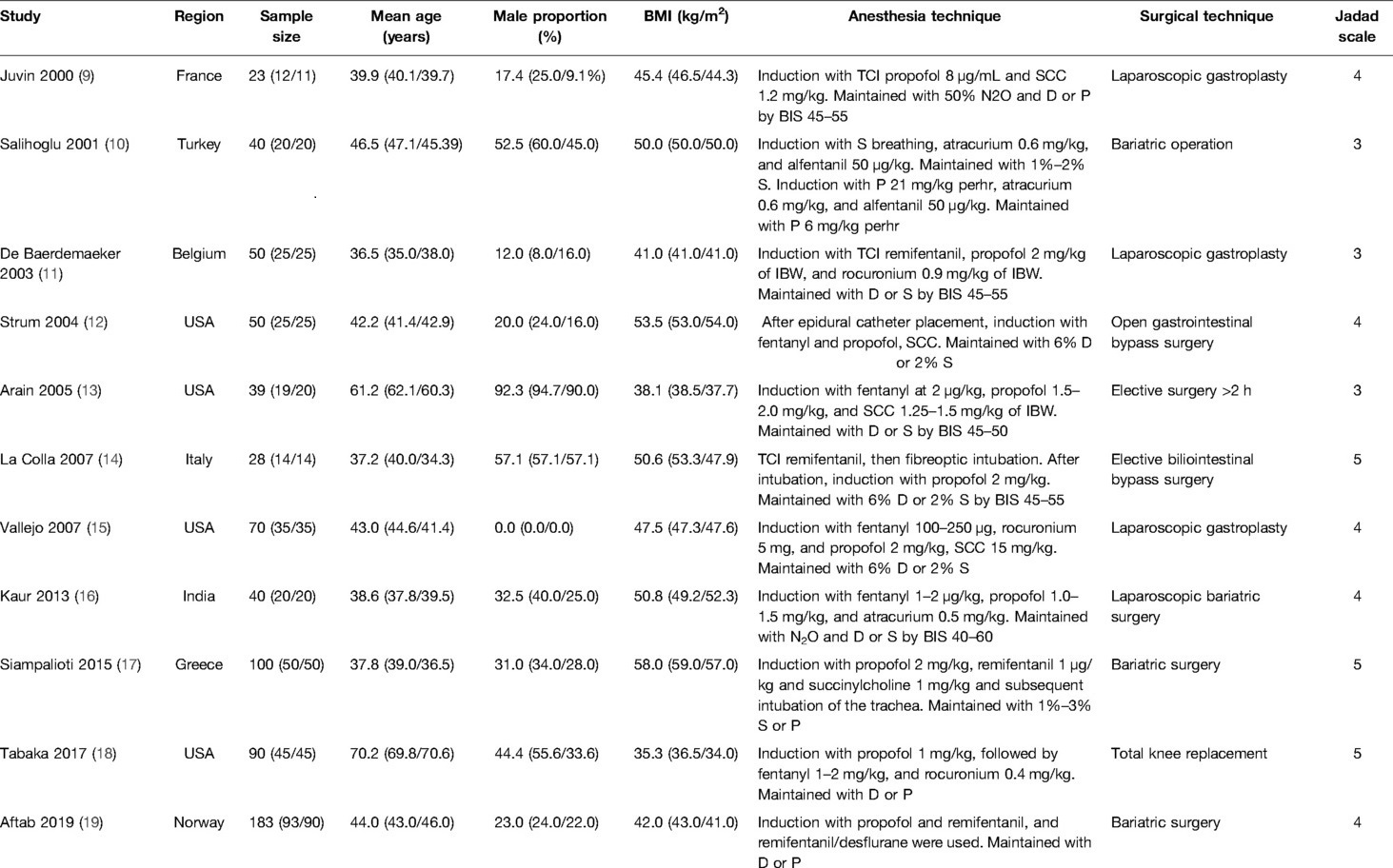
The characteristics of included studies are summarized in Table 1, and 713 obese patients undergoing general anesthesia were involved. Six studies compared desflurane with sevoflurane, three trials compared desflurane with propofol, and the remaining two trials compared sevoflurane with propofol. The BMI for each trial ranged from 35.3 to 58.0 kg/m2, and the sample size ranged from 23 to 183. Eight trials with high quality (three trials had five scores, five trials had four scores), and the remaining three trials with low quality (three trials had three scores).
Meta-Analysis
The number of trials for time to eye opening when comparing desflurane with propofol, desflurane with sevoflurane, and sevoflurane with propofol were three, six, and two trials, respectively. We noted desflurane was associated with a shorter time to eye opening as compared with sevoflurane (SMD: −0.86; 95% CI, −1.43 to −0.28; P = 0.003; Figure 2A). However, desflurane (SMD: 0.05; 95% CI, −0.71 to 0.80; P = 0.906) or sevoflurane (SMD: 1.13; 95% CI, −0.00 to 2.27; P = 0.050) were not associated with the time to eye opening when compared with propofol (Figure 2A). There was significant heterogeneity in the comparisons of desflurane with propofol (I2 = 86.6%; P = 0.001), desflurane with sevoflurane (I2 = 79.7%; P < 0.001), and sevoflurane with propofol (I2 = 89.3%; P < 0.001).
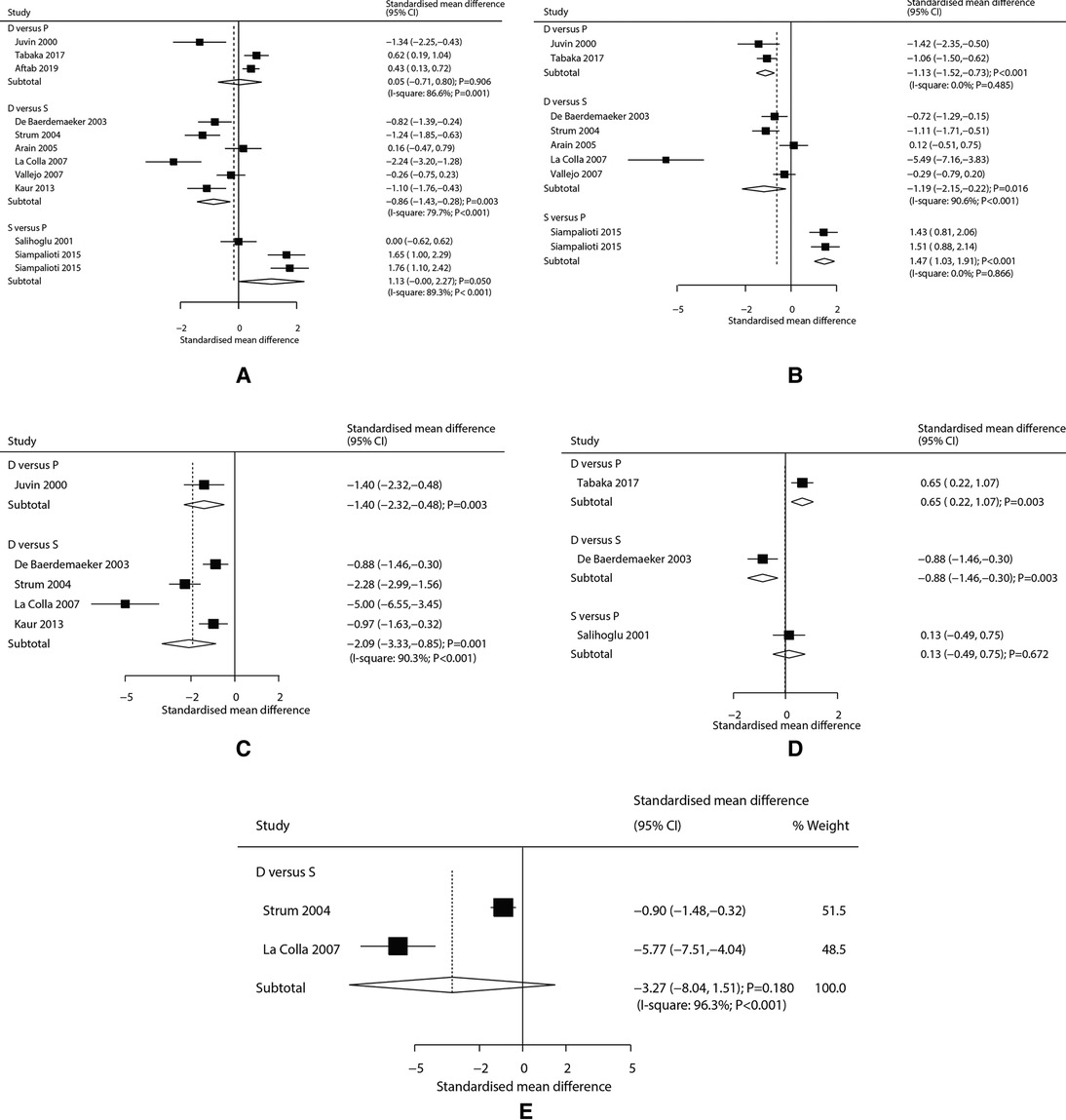
Figure 2. (A) Effects of various anesthetics on time to eye opening, (B) Effects of varies anesthetics on time to extubation, (C) Effects of various anesthetics on time to stating name, (D) Effects of various anesthetics on time for orientation to place, (E) Effects of varies anesthetics on time required for hand squeezing.
The number of trials for time to extubation when comparing desflurane with propofol, desflurane with sevoflurane, and sevoflurane with propofol were two, five, and one trial(s), respectively. We noted desflurane was associated with shorter time to extubation when compared with propofol (SMD: −1.13; 95% CI, −1.52 to −0.73; P < 0.001) or sevoflurane (SMD: −1.19; 95% CI, −2.15 to −0.22; P = 0.016). However, sevoflurane versus propofol show a longer time to extubation (SMD: 1.47; 95% CI, 1.03 to 1.91; P < 0.001) (Figure 2B). There was significant heterogeneity for the comparison of desflurane with sevoflurane (I2 = 90.6; P < 0.001), while no evidence of heterogeneity for the comparisons of desflurane with propofol (I2 = 0.0%; P = 0.485), and sevoflurane with propofol (I2 = 0.0%; P = 0.866).
The number of trials for time to stating name when comparing desflurane with propofol, and desflurane with sevoflurane were one and four trial(s), respectively. We noted desflurane was associated with a shorter time to stating name when compared with propofol (SMD: −1.40; 95% CI, −2.32 to −0.48; P = 0.003) or sevoflurane (SMD: −2.09; 95% CI, −3.33 to −0.85; P = 0.001) (Figure 2C), and significant heterogeneity for the comparison of desflurane with sevoflurane was observed (I2 = 90.3; P < 0.001).
Time for orientation to place when comparing desflurane with propofol, desflurane with sevoflurane, and sevoflurane with propofol each had one trial. We noted desflurane was associated with a longer time for orientation to place as compared with propofol (SMD: 0.65; 95% CI, 0.22 to 1.07; P = 0.003), while desflurane versus sevoflurane show shorter time for orientation to place (SMD: −0.88; 95% CI, −1.46 to −0.30; P = 0.003). However, there was no significant difference between sevoflurane and propofol for the time for orientation to place (SMD: 0.13; 95% CI, −0.49 to 0.75; P = 0.672) (Figure 2D). Finally, we noted desflurane was not associated with the time required for hand squeezing as compared with sevoflurane (SMD: −3.27; 95% CI, −8.04 to 1.51; P = 0.180; Figure 2E), and significant heterogeneity was observed across included trials (I2 = 96.3; P < 0.001).
Subgroup Analysis
Subgroup analyses for the time to eye opening, time to extubation, and time to stating name when comparing desflurane with sevoflurane are shown in Table 2. We noted desflurane versus sevoflurane was associated with a shorter time to eye opening if the mean age of patients <40.0 years, proportion of men <50.0%, BMI ≥ 50.0 kg/m2, or patients were treated with gastroplasty. Moreover, desflurane versus sevoflurane was associated with a shorter time to extubation when the proportion of men <50.0%, or patients were treated with gastroplasty. Finally, desflurane versus sevoflurane was associated with a shorter time to stating name in all subgroups.
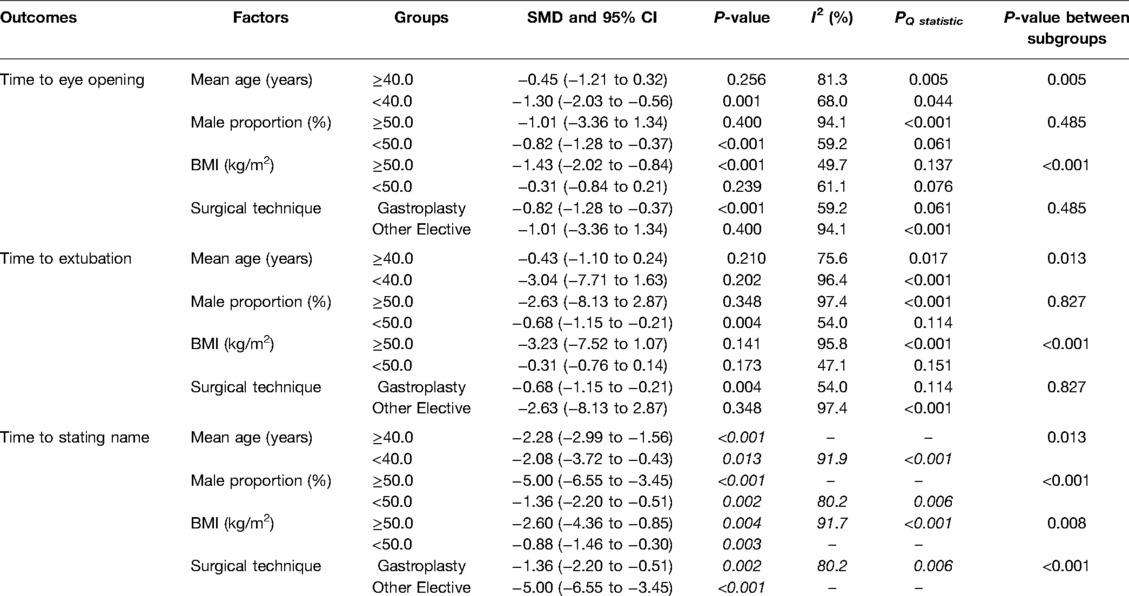
Table 2. Subgroup analyses of desflurane vs sevoflurane for time to eye opening, time to extubation, and time to stating name.
Publication Bias
The publication bias for time to eye opening, time to extubation, and time to stating name were also evaluated and presented in Supplementary Figures S1–S3. There was no significant publication bias for time to eye opening (P-value for Egger: 0.170; P value for Begg: 0.373), time to extubation (P-value for Egger: 0.417; P value for Begg: 0.917), and time to stating name (P-value for Egger: 0.073; P value for Begg: 0.086).
Discussion
In this meta-analysis of published RCTs, a total of 713 obese patients undergoing general anesthesia from 11 RCTs were recruited, and the characteristics across included trials were broad. This study found desflurane versus sevoflurane was associated with shorter time to eye opening, time to extubation, time to stating name, and time for orientation to place. Moreover, desflurane versus propofol was associated with a shorter time to extubation or time to stating name, and a longer time for orientation to place. Furthermore, sevoflurane was associated with a longer time to extubation than propofol. Finally, the effectiveness between desflurane and sevoflurane could affect by mean age, male proportion, BMI, and surgical technique.
A prior meta-analysis conducted by Liu et al identified 11 RCTs and found desflurane significantly reduced the time required eye opening, time required for hand squeezing, time required for extubation, and time required for name stating as compared with sevoflurane. Moreover, sevoflurane was associated with a shorter time required for extubation as compared with isoflurane, while no significant difference between sevoflurane and isoflurane for postanesthesia care unit discharge time (29). However, this study did not assess the treatment effectiveness between desflurane and sevoflurane according to patients’ characteristics. The potential heterogeneity across included trials was not explored. We, therefore, conducted a systematic review and meta-analysis to assess the effectiveness of desflurane, sevoflurane, and propofol on postoperative recovery outcomes for obese patients undergoing general anesthesia.
The summary results found desflurane shows better recovery outcomes than sevoflurane, and these results were consistent with prior meta-analyses (30). Although the recovery outcome might be related to the duration of surgery, this impact could be balanced by the duration of surgery being similar between the desflurane and sevoflurane groups. The potential reason for this could be desflurane was associated with a lower solubility in blood, lean tissue, and fat than sevoflurane (31). Moreover, the low blood/gas partition coefficient in desflurane could induce rapid and consistent recovery outcomes in obese patients (32). Subgroup analyses found the beneficial effects of desflurane are more evident in the subgroups of mean age <40.0 years, proportio of men ≥50.0%, BMI ≥ 50.0 kg/m2, and patients treated with other elective surgery. The potential reason for this could be the duration of wake in younger patients was more sensitive, and the male patients had stronger restorative ability. Moreover, there was a significant association between sevoflurane use with longer airway reflex recovery time could affect by BMI (33). Finally, the elective surgical are significantly related to the duration of surgery, which might affect the recovery time, and contribute to the significant heterogeneity among included trials.
We noted desflurane was associated with a shorter time to extubation, or time to stating name than propofol, while a longer time for orientation to place for patients who used desflurane was observed. The low solubility of desflurane could explain these results, which suggested less desflurane needs to be released from the tissues and eliminated from the body (34). Moreover, propofol as a lipid-soluble anesthetic and associated with a prolonged effect in obese patients because the proportion of fat in obese patients was high. The longer time for orientation to place could be explained by the fact that only one trial reported this effect, which needed further verification by large-scale RCT (18). In addition, we noted sevoflurane was associated with a longer time to extubation than propofol, which is based on the trial conducted by Siampalioti et al. (17). They point out that the time to eye opening and extubation was shorter when using propofol, while the postoperative recovery was rapid for patients who used sevoflurane.
Several shortcomings of this study should be acknowledged. First, mostly included trials compared the treatment effectiveness of desflurane with sevoflurane, and whether comparing desflurane or sevoflurane with propofol could affect patients’ characteristics needs to be further explored. Second, the heterogeneity across included trials is substantial, and not fully explained by subgroup analyses. Third, patients underwent various surgical techniques, and the duration of surgery was not available in most trials. Fourth is the inherent limitations of meta-analysis based on published articles, including inevitable publication bias, and restricted details analyses.
In conclusion, we noted desflurane was associated with better postoperative recovery outcomes than sevoflurane or propofol for obese patients. Moreover, the effectiveness of sevoflurane versus propofol needs to be further assessed. Furthermore, the treatment effectiveness of desflurane versus sevoflurane on recovery outcome could affect by mean age, proportion of men, BMI, and surgical technique.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
Z-HH contributed to conceptualization. ZL and G-FZ contributed to document retrieval. Z-WL contributed to the formal analysis and investigation. S-QL contributed to the review and editing of the manuscript. All authors contributed to the article and approved the submitted version.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.862632/full#supplementary-material.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organisation. Health Topics-Obesity. Available from: http://www.who.int/topics/obesity/en/
2. Oberg B, Poulsen TD. Obesity: an anaesthetic challenge. Acta Anaesthesiol Scand. (1996) 40:191–200. doi: 10.1111/j.1399-6576.1996.tb04419.x
3. Shenkman Z, Shir Y, Brodsky JB. Perioperative management of the obese patient. Br J Anaesth. (1993) 70:349–59. doi: 10.1093/bja/70.3.349
4. Pelosi P, Croci M, Ravagnan I, Cerisara M, Vicardi P, Lissoni A, et al. Respiratory system mechanics in sedated, paralyzed, morbidly obese patients. J Appl Physiol (1985). (1997) 82:811–8. doi: 10.1152/jappl.1997.82.3.811
5. Gaszyński T, Gaszyński W. Postępowanie anestezjologiczne u pacjentów z otyłością znacznego stopnia. Anestezjol Intens Ter. (2002) 34:291–6. https://www.czytelniamedyczna.pl/94,postepowanie-anestezjologiczne-u-pacjentow-z-otyloscia-znacznego-stopnia.html
6. Gaszyński T, Gaszyński W, Strzelczyk J. Ostra niewydolność oddechowa u pacjentów otyłych. Twój Magazyn Medyczny - Chirurgia. (2003) 3:55–8.
7. Drenick EJ, Bale GS, Seltzer F, Johnson DG. Excessive mortality and causes of death in morbidly obese men. JAMA. (1980) 243:443–5. doi: 10.1001/jama.1980.03300310031018
8. Eger EI 2nd Age, minimum alveolar anesthetic concentration, and minimum alveolar anesthetic concentration-awake. Anesth Analg. (2001) 93:947–53. doi: 10.1097/00000539-200110000-00029
9. Juvin P, Vadam C, Malek L, Dupont H, Marmuse JP, Desmonts JM. Postoperative recovery after desflurane, propofol, or isoflurane anesthesia among morbidly obese patients: a prospective, randomized study. Anesth Analg. (2000) 91:714–9. doi: 10.1097/00000539-200009000-00041
10. Salihoglu Z, Karaca S, Kose Y, Zengin K, Taskin M. Total intravenous anesthesia versus single breath technique and anesthesia maintenance with sevoflurane for bariatric operations. Obes Surg. (2001) 11:496–501. doi: 10.1381/096089201321209413
11. De Baerdemaeker LE, Struys MM, Jacobs S, Den Blauwen NM, Bossuyt GR, Pattyn P, et al. Optimization of desflurane administration in morbidly obese patients: a comparison with sevoflurane using an ‘inhalation bolus’ technique. Br J Anaesth. (2003) 91:638–50. doi: 10.1093/bja/aeg236
12. Strum EM, Szenohradszki J, Kaufman WA, Anthone GJ, Manz IL, Lumb PD. Emergence and recovery characteristics of desflurane versus sevoflurane in morbidly obese adult surgical patients: a prospective, randomized study. Anesth Analg. (2004) 99:1848–53, table of contents. doi: 10.1213/01.ANE.0000136472.01079.95
13. Arain SR, Barth CD, Shankar H, Ebert TJ. Choice of volatile anesthetic for the morbidly obese patient: sevoflurane or desflurane. J Clin Anesth. (2005) 17:413–9. doi: 10.1016/j.jclinane.2004.12.015
14. La Colla L, Albertin A, La Colla G, Mangano A. Faster wash-out and recovery for desflurane vs sevoflurane in morbidly obese patients when no premedication is used. Br J Anaesth. (2007) 99:353–8. doi: 10.1093/bja/aem197
15. Vallejo MC, Sah N, Phelps AL, O’Donnell J, Romeo RC. Desflurane versus sevoflurane for laparoscopic gastroplasty in morbidly obese patients. J Clin Anesth. (2007) 19:3–8. doi: 10.1016/j.jclinane.2006.04.003
16. Kaur A, Jain AK, Sehgal R, Sood J. Hemodynamics and early recovery characteristics of desflurane versus sevoflurane in bariatric surgery. J Anaesthesiol Clin Pharmacol. (2013) 29:36–40. doi: 10.4103/0970-9185.105792
17. Siampalioti A, Karavias D, Zotou A, Kalfarentzos F, Filos K. Anesthesia management for the super obese: is sevoflurane superior to propofol as a sole anesthetic agent? A double-blind randomized controlled trial. Eur Rev Med Pharmacol Sci. (2015) 19:2493–500. https://www.europeanreview.org/article/918026214787
18. Tanaka P, Goodman S, Sommer BR, Maloney W, Huddleston J, Lemmens HJ. The effect of desflurane versus propofol anesthesia on postoperative delirium in elderly obese patients undergoing total knee replacement: a randomized, controlled, double-blinded clinical trial. J Clin Anesth. (2017) 39:17–22. doi: 10.1016/j.jclinane.2017.03.015
19. Aftab H, Fagerland MW, Gondal G, Ghanima W, Olsen MK, Nordby T. Pain and nausea after bariatric surgery with total intravenous anesthesia versus desflurane anesthesia: a double blind, randomized, controlled trial. Surg Obes Relat Dis. (2019) 15:1505–12. doi: 10.1016/j.soard.2019.05.010
20. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
21. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. (1996) 17:1–12. doi: 10.1016/0197-2456(95)00134-4
22. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
23. Ades AE, Lu G, Higgins JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Making. (2005) 25:646–54. doi: 10.1177/0272989X05282643
24. Deeks JJ, Higgins JPT, Altman DG. Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration. (2008). p. 243–96.
25. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
26. Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. (2003) 326:219. doi: 10.1136/bmj.326.7382.219
27. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
28. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
29. Liu FL, Cherng YG, Chen SY, Su YH, Huang SY, Lo PH, et al. Postoperative recovery after anesthesia in morbidly obese patients: a systematic review and meta-analysis of randomized controlled trials. Can J Anaesth. (2015) 62:907–17. doi: 10.1007/s12630-015-0405-0
30. Macario A, Dexter F, Lubarsky D. Meta-analysis of trials comparing postoperative recovery after anesthesia with sevoflurane or desflurane. Am J Health Syst Pharm. (2005) 62:63–8. doi: 10.1093/ajhp/62.1.63
31. Eger EI 2nd, Gong D, Koblin DD, Bowland T, Ionescu P, Laster MJ, et al. The effect of anesthetic duration on kinetic and recovery characteristics of desflurane versus sevoflurane, and on the kinetic characteristics of compound A, in volunteers. Anesth Analg. (1998) 86:414–21. doi: 10.1097/00000539-199802000-00037
32. Ogunnaike BO, Jones SB, Jones DB, Provost D, Whitten CW. Anesthetic considerations for bariatric surgery. Anesth Analg. (2002) 95:1793–805. doi: 10.1097/00000539-200212000-00061
33. McKay RE, Malhotra A, Cakmakkaya OS, Hall KT, McKay WR, Apfel CC. Effect of increased body mass index and anaesthetic duration on recovery of protective airway reflexes after sevoflurane vs desflurane. Br J Anaesth. (2010) 104:175–82. doi: 10.1093/bja/aep374
34. Eger EI 2nd, Johnson BH. Rates of awakening from anesthesia with I-653, halothane, isoflurane, and sevoflurane: a test of the effect of anesthetic concentration and duration in rats. Anesth Analg. (1987) 66:977–82. https://journals.lww.com/anesthesia-analgesia/Abstract/1987/10000/Rates_of_Awakening_from_Anesthesia_with_I_653,.10.aspx3631595
Keywords: obese, general anesthesia, postoperative recovery, meta-analysis, patient
Citation: Hu Z, Liu Z, Zheng G, Li Z and Liu S (2022) Postoperative Recovery Outcomes for Obese Patients Undergoing General Anesthesia: A Meta-Analysis of Randomized Controlled Trials. Front. Surg. 9:862632. doi: 10.3389/fsurg.2022.862632
Received: 26 January 2022; Accepted: 25 April 2022;
Published: 28 July 2022.
Edited by:
Hubert Scheuerlein, Klinik für Allgemein- und Viszeralchirurgie, St. Vincenz-Krankenhaus Gmb, GermanyReviewed by:
Carolina Isabella Alexandra Pape-Köhler, Witten/Herdecke University, GermanyCopyright © 2022 Hu, Liu, Zheng, Li and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sheng-Qun Liu suju666666@126.com
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Zhen-Hua Hu
Zhen-Hua Hu Zhe Liu
Zhe Liu  Sheng-Qun Liu
Sheng-Qun Liu