Open Intraperitoneal Onlay Mesh (IPOM) Technique for Incisional Hernia Repair
- 1Department of Surgery and Center for Minimally Invasive Surgery, Academic Teaching Hospital of Charité Medical School, Vivantes Hospital, Berlin, Germany
- 2Department of Surgery I – Section Coloproctologie and Hernia Surgery, Lukas Hospital, Neuss, Germany
In an Expert Consensus Guided by Systematic Review the panel agreed that for open elective incisional hernia repair sublay mesh location is preferred, but open intraperitoneal onlay mesh (IPOM) may be useful in certain settings. Accordingly, the available literature on the open IPOM technique was searched and evaluated.
Material and Methods: A systematic search of the available literature was performed in July 2018 using Medline, PubMed, and the Cochrane Library. Forty-five publications were identified as relevant for the key question.
Results: Compared to laparoscopic IPOM, the open IPOM technique was associated with significantly higher postoperative complication rates and recurrence rates. For the open IPOM with a bridging situation the postoperative complication rate ranges between 3.3 and 72.0% with a mean value of 20.4% demonstrating high variance, as did the recurrence rate of between 0 and 61.0% with a mean value of 12.6%. Only on evaluation of the upward-deviating maximum values and registry data is a trend toward better outcomes for the sublay technique demonstrated. Through the use of a wide mesh overlap, avoidance of dissection in the abdominal wall and defect closure it appears possible to achieve better outcomes for the open IPOM technique.
Conclusion: Compared to the laparoscopic technique, open IPOM is associated with significantly poorer outcomes. For the sublay technique the outcomes are quite similar and only tendentially worse. Further studies using an optimized open IPOM technique are urgently needed.
Introduction
Two recently published systematic reviews and meta-analyses and a registry study once again impressively demonstrated that for incisional hernias mesh techniques compared with suture techniques resulted in significantly lower recurrence rates (1–3). However, which mesh technique assures the best outcomes for the respective patient is still under debate.
While meta-analyses have identified advantages for the laparoscopic compared with the open technique for repair of incisional hernia (4–7), in the guidelines the laparoscopic intraperitoneal onlay mesh (IPOM) technique is recommended only for a defect size of up to 10 cm (8–12).
In an Expert Consensus Guided by Systematic Review the panel agreed that for open elective incisional hernia repair sublay mesh location is preferred, but open intraperitoneal onlay mesh (IPOM) may be useful in certain settings (13). In systematic reviews the open IPOM technique is discussed, in particular, in the context of large incisional hernias (14, 15). Based on the expert consensus, this paper now explores and evaluates the available literature on open intraperitoneal onlay mesh (IPOM) in accordance with the Parker (16) nomenclature.
Materials and Methods
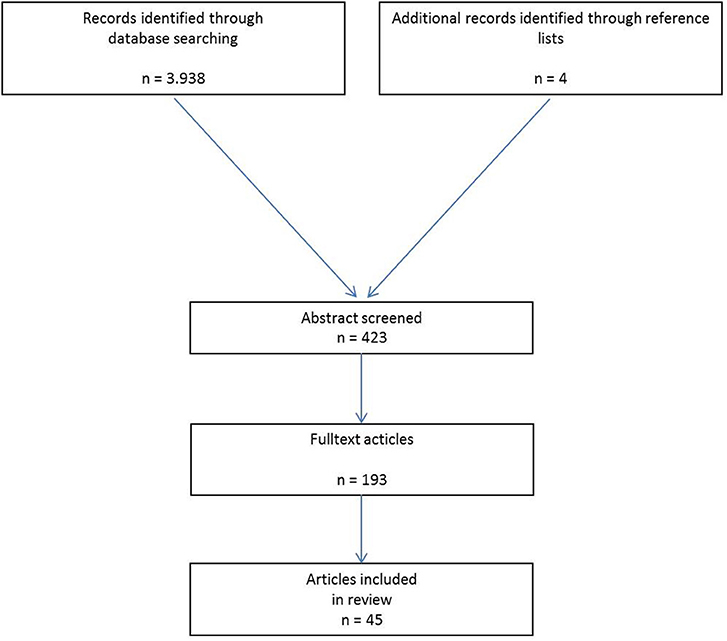
A systematic search of the available literature was performed in July 2018 using Medline, PubMed, and the Cochrane Library, as well as a search of relevant journals and reference lists. The following search terms were used: “Incisional hernia,” “Intraperitoneal mesh,” “Open intraperitoneal onlay mesh,” “Open IPOM,” and “IPOM.” The abstracts of 423 publications were checked. For the present analysis 45 publications were identified as relevant for the key question (Figure 1).
Results
Laparoscopic vs. Open Intraperitoneal Onlay Mesh (IPOM) With Bridging for Incisional Hernia Repair
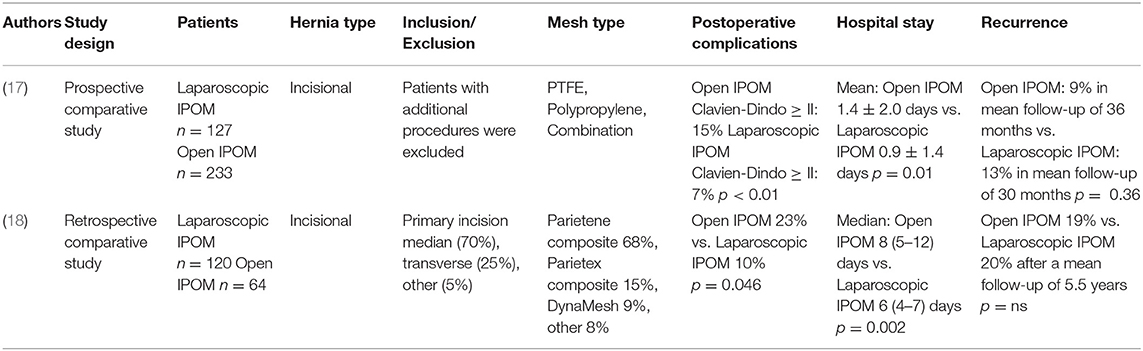
In a prospective (17) and a retrospective study (18) the outcomes of the laparoscopic and open IPOM techniques for incisional hernia were compared (Table 1). For the prospective study comparison of 127 laparoscopic and 233 open IPOM incisional hernias repairs showed a significantly lower postoperative complication rate (Clavien-Dindo ≥ II) of 7% for the laparoscopic and of 15% for the open IPOM technique (p < 0.01) (17).
Likewise, the hospital stay for the laparoscopic IPOM was significantly shorter (0.9 ± 1.4 days vs. 1.4 ± 2.0 days; p = 0.01) (17). No significant difference was seen in the recurrence rate (laparoscopic 13% vs. open 9%; p = 0.36) (17).
Similarly, the retrospective comparative study of 120 laparoscopic and 64 open IPOM operations showed comparable outcomes (18), with a significantly lower postoperative complication rate in favor of the laparoscopic technique (10 vs. 23%; p = 0.046) (18). Similarly, in this study the hospital stay after laparoscopic IPOM was significantly shorter [median 6 (4–7) days vs. 8 (5–12) days; p = 0.002] (18). Likewise, in this study no significant difference was found in the recurrence rate after laparoscopic vs. open IPOM for incisional hernia repairs (laparoscopic 20% vs. open 19%; p = ns) (18).
Hence, the laparoscopic compared with the open IPOM technique had a significantly lower postoperative complication rate and hospital stay and with a somewhat similar recurrence rate.
Accordingly, for defects up for 10 cm preference should in general be given to laparoscopic over open IPOM repair.
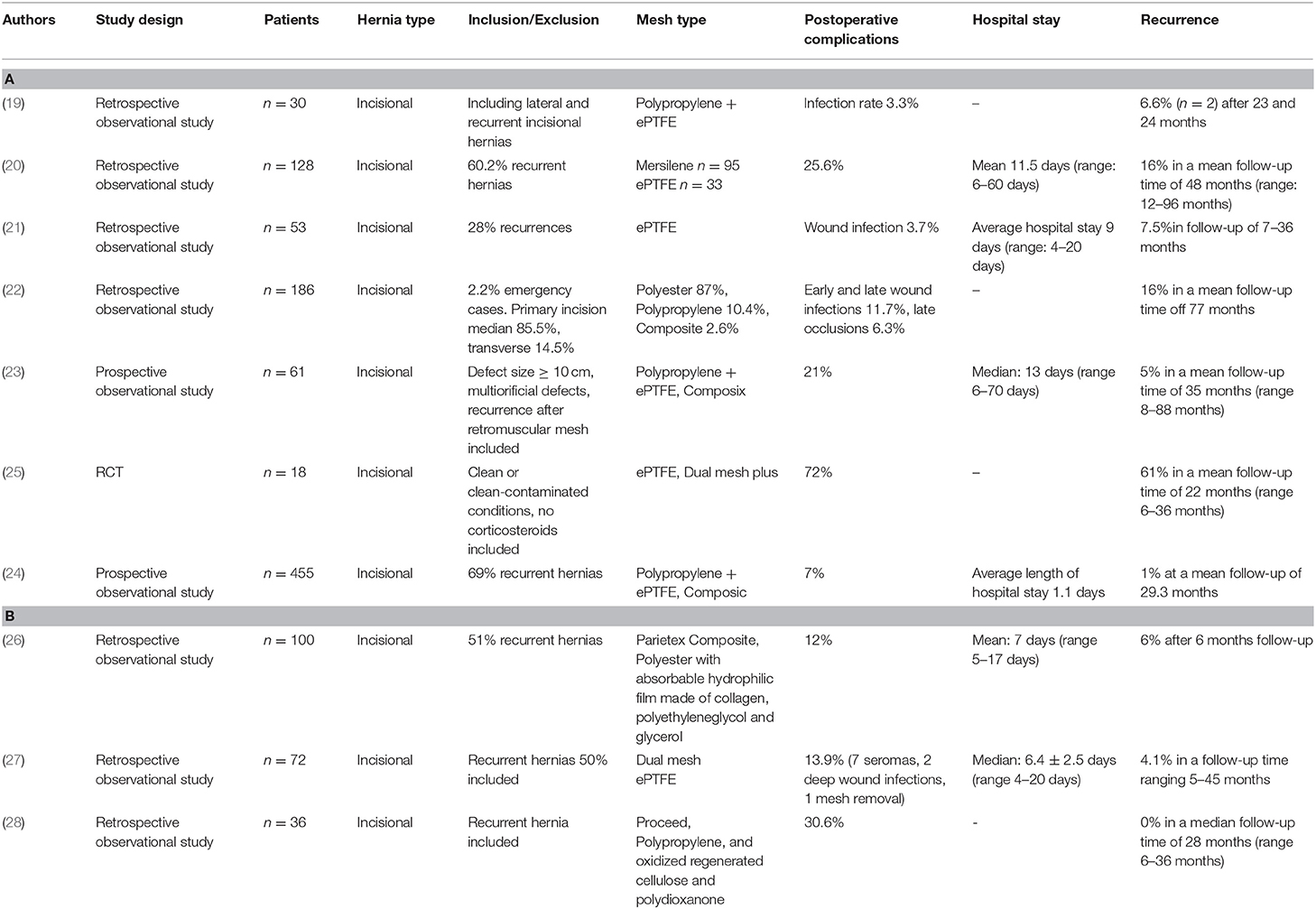
Open Intraperitoneal Onlay Mesh With Bridging in Incisional Hernia Repair
Since in general open IPOM is indicated for incisional hernia repair of large defects when a sublay technique is no longer feasible, this mainly involves a bridging situation. Accordingly, most of the studies published report on an open intraperitoneal onlay mesh technique with bridging (19–28) (Table 2). The outcomes demonstrated high variance (Table 2). The postoperative complication rates were in the range of 3.3–72% and the recurrence rates 0–61%. The mean value calculated for the open intraperitoneal onlay mesh technique in the studies featured in Table 2 was 20.4% (range: 3.3–72%) for the postoperative complication rates and the recurrence rates it was 12.6% (range: 0–61%). Some studies revealed extremely good (postoperative complication rate 7%, recurrence rate 10%) (24), others extremely poor (postoperative complication rate 72%, recurrence rate 61%), outcomes (25).The authors of the publication with the best outcomes attributed the good results to the use of a wide overlap, avoidance of dissection in the abdominal wall and coverage of the mesh with the peritoneal hernia sac or defect closure (24). Hence, no clear picture can be identified. Further studies are urgently needed to better ascertain the role of open IPOM with bridging. However, comparison of the literature data on the outcomes of the open IPOM vs. sublay technique did not reveal any essential difference (sublay: mean postoperative complication rate 18.6% (range 8.0–26%), mean recurrence rate 13.5% (range 1.6–32%)] (29). Only on evaluation of upward-deviating maximum values is a trend toward better outcomes for the sublay technique demonstrated (29).
Open Intraperitoneal Onlay Mesh With Defect Closure by a Myoaponeurotic Flap in Incisional Hernia Repair
To avoid a bridging situation in the open IPOM operation, techniques were introduced for defect closure in open IPOM (30). Arnaud et al. (30) first reported on an open IPOM technique with defect closure by means of a myoaponeurotic flap according to Welti and Eudel: “After excision of the scar, the herniated sac is exposed and the adjacent anterior fascia is cleared of subcutaneous tissue up to 10–15 cm from the ring of the hernia sac. The sac is then excised and intestinal adhesions dissected free to facilitate the placement of the mesh at least 10 cm from the edge of the hernia neck. The mesh is secured to the musculofascial wall by through-and-through-non absorbable sutures” (30). “The anterior lamina of the rectus sheath is incised longitudinally 4 cm back from its medial edge bilaterally. Both aponeurotic flaps are then reflected inward and sutured by interrupted absorbable stitches” (30). The publications addressing this technique report much lower postoperative complication rates and recurrence rates (30, 31, 32) (Table 3). It appears that defect closure results in both fewer postoperative complications and recurrences. This concords with the existing data showing that defect closure in incisional hernia repair assures better outcomes (13).

Table 3. Open intraperitoneal onlay mesh with defect closure by a myoaponeurotic flap for incisional hernia repair.
Open Intraperitoneal Onlay Mesh With Defect Closure in Modified Sublay Technique for Incisional Hernia Repair
Another variant of the open IPOM technique aimed at defect closure involves a modification with the sublay technique (33). “Skin and subcutaneous flaps are then developed on both sides to allow for medialization of the rectus muscles and fascia over the mesh” (33). “The mesh is placed within the abdomen and secured with u-sutures” (33). The fascia and excess hernia is then closed over the mesh” (33). “This also allows for return of the rectus muscles to the midline thus restoring the normal architecture of the abdominal wall” (33). The outcomes with this technique (Table 4) are also highly variable and no better than those achieved with the modification involving the myoaponeurotic flap (33, 34).
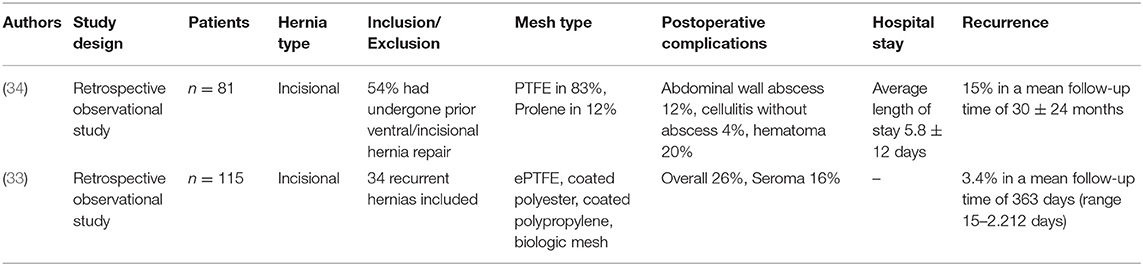
Table 4. Open intraperitoneal onlay mesh with defect closure by sublay-technique for incisional hernia repair.
Open Intraperitoneal Onlay Biological Mesh With Defect Closure by a Component Separation Technique in Contaminated Ventral and Incisional Hernias
In a prospective multicenter study on repair of contaminated ventral hernias, 26 patients were treated by means of a component separation technique and intraperitoneal placement of a biological mesh (Strattice) (35). All patients had a defect closure and reinforcement of the repair with an appropriately sized piece of a biologic mesh with at least 3–5 cm of fascial overlap (35). The rate of wound infection was 30%, wound dehiscence 15%, seroma 15% and hematoma 8% (35). The recurrence rate after 1 year was 30%. No significant differences were noted vs. positioning of the biological mesh in the retrorectus layer (35).
Outcome Data for Open Intraperitoneal Onlay Mesh in Registries
Of the 1,495 open incisional hernia repairs registered in the Danish Hernia Database, 258 (22.9%) were performed in the open IPOM technique (36). During the same period of time 1,763 incisional hernia laparoscopic repairs were carried out. Multivariate analysis revealed that younger age, open repair, hernia defects >7 cm, and onlay or intraperitoneal mesh positioning in open repair were significant risk factors for poor late outcomes (p < 0.05) (36). Sublay mesh position reduced the risk of reoperation for recurrence after open repairs (36).
Assessment of the Open Intraperitoneal Onlay Mesh Technique in Systematic Reviews and Meta-Analyses
In a Cochrane database systematic review comparison of onlay vs. intraperitoneal mesh position in open incisional hernia repair revealed that there were non-significantly fewer hernia recurrences, less seroma formation and more postoperative pain in the intraperitoneal group (37).
The findings of three further systematic reviews and meta-analyses must be analyzed in a critical light with respect to the key question addressed here since they included studies with primary abdominal wall hernias and incisional hernias, i.e., mixed patient collectives, as well as the laparoscopic technique (38–40). Numerous studies have demonstrated that the outcomes for repair of primary abdominal wall hernias and incisional hernias differ highly significantly and therefore should not be combined (41–45). Moreover, the mesh position as underlay was not defined exactly. These may also have included preperitoneal mesh placements (16). Studies with biological meshes were also included (38).
Mean Values of Postoperative Complications and Recurrence Rate
Under consideration of all analyzed studies the mean value for the postoperative complications is 20.4% with a range of 3.3 and 72% and for the recurrence rate 12.6% with a range of 0–61%.
Discussion
While in an Expert Consensus Guided by Systematic Review preference is given to the sublay mesh position for repair of incisional hernia, the open intraperitoneal onlay mesh (IPOM) technique is, nonetheless, deemed useful in certain clinical situations (13). Therefore, this present review of the literature collates and analyzes the data available on the open IPOM technique. Comparison of the open with the laparoscopic technique reveals significant advantages for the laparoscopic procedure. Since in the guidelines the use of the laparoscopic IPOM technique is recommended only for a defect size of up to 10 cm (8–12), laparoscopic repair should be given preference for defects up to that size. Accordingly, the open IPOM technique in addition to other procedures tends to be used for large incisional hernias (14, 15). In general defect closure of large incisional hernias is not possible, thus creating a bridging situation as reported on in the majority of studies on the open IPOM. The outcomes demonstrate high variance. For example, for open IPOM with bridging situation postoperative complication rates of between 3.3 and 72.0% and mean value of 20.4% are identified, and for the recurrence rate of between 0 and 61.0% with mean value of 12.6%.The outcomes are very diverging. These inconsistent outcomes are probably explained by the fact that the open IPOM technique represents a very heterogeneous group. In some cases, the results derive from centers and surgeons dedicated to refining the technique, using it as the first-hand choice with great volume and awareness of the anatomical circumstances [e.g., (19–24, 26, 28, 30–32)]. In other cases, the open IPOM is applied as a desperate solution to solve a complex problem when there is no other alternative due to anatomical conditions after previous surgery [presumably references (2, 4, 17, 18, 36, 39)].
Comparison of these findings with the outcomes reported in the literature for sublay repair of incisional hernia reveals that in the case of the sublay technique the postoperative complication rates are between 8.0 and 26.0%, with a mean value of 18.6%, and recurrence rates of between 1.6 and 32.0%, with a mean value of 13.5% (29). Hence, only in respect of the extreme values are the outcomes better for the sublay technique. Likewise, registry data demonstrate somewhat more favorable outcomes for the sublay technique.
Therefore, further comparative studies are urgently needed to ascertain the role of the open IPOM technique in incisional hernia repair. That is borne out in particular in the study by Iannitti et al. (24) with a large sample size (n = 455) and a low postoperative complication rate of 7% and recurrence rate of 1% at a mean follow-up of 29.3 months. In the technique described by Iannitti et al. (24) dissection in the abdominal wall was avoided and attention paid to the provision of an appropriately large mesh overlap. Furthermore, the mesh was covered with at least the peritoneal hernia sac (24).
Attention should be paid to these technical aspects when implementing the open IPOM technique.
Modifications of the open IPOM technique are aimed at mesh-based defect closure through a combination with a myoaponeurotic flap or closure of the anterior lamina of the rectus sheath as used in the sublay technique. However, both techniques require dissection in the abdominal wall, albeit to a lesser degree when using myoaponeurotic flaps. That also no doubt explains the more favorable outcomes of open IPOM repair by means of a myoaponeurotic flap compared with closure of the anterior lamina of the rectus sheath. Likewise, comparison of outcomes of open IPOM technique with bridging reveals lower postoperative complication and recurrence rates for the modification with myoaponeurotic flaps. However, to date that technique has only been used and extensively reported by a French working group.
From the available meta-analyses and systematic reviews it is almost impossible to generate further data on open IPOM outcomes since they include joint evaluation of primary abdominal wall hernias and incisional hernias, open and laparoscopic techniques as well as synthetic and biological meshes. Hence, interpretation of outcomes is very difficult.
In summary, it can be stated that the open IPOM is clearly inferior to the laparoscopic technique but achieves quite acceptable outcomes compared with the open sublay technique. It appears that outcomes can be further improved through the use of a wide overlap, avoidance of dissection in the abdominal wall and defect closure. Further studies using a standardized open IPOM technique are urgently needed.
Author Contributions
FK: literature search, literature analyses, publication concept, and publication draft; BL: literature search, literature analyses, publication concept, and critical review of the publication draft.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Mathes T, Walgenbach M, Siegel R. Suture versus mesh repair in primary and incisional ventral hernias: a systematic review and meta-analysis. World J Surg. (2016) 40:826–35. doi: 10.1007/s00268-015-3311-2
2. López-Cano M, Martin-Dominguez LA, Pereira JA, Armengo-Carrasco M, Garcia-Alamino JM. Balancing mesh-related complications and benefits in primary ventral and incisional hernia surgery. A meta-analysis and trial sequential analysis. PLoS ONE (2018) 13:e0197813. doi: 10.1371/journal.pone.0197813
3. Koktotovic D, Bisgaard T, Helgstrand F. Long-term recurrence and complications associated with elective incisional hernia repair. JAMA (2016) 316:1575–82. doi: 10.1001/jama.2016.15217
4. Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, et al. Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia (2015) 19:449–63. doi: 10.1007/s10029-015-1351-z
5. Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, et al. Reply to comment to Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia Hernia (2015) 19:1027–9. doi: 10.1007/s10029-015-1432-z
6. Jensen KK, Jorgensen LN. Comment to: meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Awaiz et al. Hernia 19:449-463. Hernia (2015) 19:1025–6. doi: 10.1007/s10029-015-1412-3
7. Al Chalabi H, Larkin J, Mehigan B, McCormick P. A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials International. J Surg. (2015) 20:65–74. doi: 10.1016/j.ijsu.2015.05.050
8. Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc. (2014) 28:2–29. doi: 10.1007/s00464-013-3170-6
9. Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. (Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS])-part 2. Surg Endosc. (2014) 28:353–79. doi: 10.1007/s00464-013-3171-5
10. Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS])-Part III. Surg Endosc. (2016) 28:380–404. doi: 10.1007/s00464-013-3172-4
11. Earle D, Roth JS, Saber A, Haggerty S, Bradley JF, Fanelli R, et al. SAGES guidelines for laparoscopic ventral hernia repair. Surg Endosc. (2016) 30:3163–83. doi: 10.1007/s00464-016-5072-x
12. Silecchia G, Campanile FC, Sanchez L, Ceccarelli G, Antinori A, Ansaloni L, et al. Laparoscopic ventral/incisional hernia repair: updated Consensus Development Conference based guidelines [corrected]. Surg Endosc. (2015) 29:2463–84. doi: 10.1007/s00464-015-4293-8
13. Liang MK, Holihan JL, Itani K, Alawadi ZM, Flores Gonzales JR, Askenasy EP, et al. Verntral hernia management: expert consensus guided by systematic review. Ann Surg. (2017) 265:80–9. doi: 10.1097/SLA.0000000000001701
14. Eriksson A, Rosenberg J, Bisgaard T. Surgical treatment for giant incisional hernia: a qualitative systematic review. Hernia (2014) 18:31–8. doi: 10.1007/s10029-013-1066-y
15. Deerenberg EB, Timmermans L, Hogerzeil DP, Slieker JC, Eilers PHC, Jeelkel J, et al. A systematic review of the surgical treatment of large incisional hernia. Hernia (2015)19:89–101. doi: 10.1007/s10029-014-1321-x
16. Parker SG, Wood CPJ, Sanders DL, Windsor ACJ. Nomenclature in abdominal wall hernias: is it time for consensus? World J Surg. (2017) 41:2488–91. doi: 10.1007/s00268-017-4037-0
17. Bingener J, Buck L, Richards M, Michlek J, Schwesinger W, Sirinek K. Long-term outcomes in laparoscopic vs open ventral hernia repair. Arch Surg. (2007)142:562–7 doi: 10.1001/archsurg.142.6.562
18. Lavanchy JL, Buff SE, Kohler A, Candinas D, Beldi G. Long-term results of laparoscopic versus open intraperitoneal onlay mesh incisional hernia repair: a propensity score-matched analysis. Surg Endosch. (2018). doi: 10.1007/s00464-018-6298-6. [Epub ahead of print].
19. Bendavid R. Composite mesh (polypropylene – e-PTFE) in the intraperitoneal position A report of 30 cases. Hernia (1997) 1:5–8. doi: 10.1007/BF02426380
20. Marchal F, Brunaud L, Sebbag H, Bresler L, Tortuyaux JM, Boissel P. Treatment of incisional hernias by placement of an intraperitoneal prosthesis: a series of 128 patients. Hernia (1999) 3:141–7. doi: 10.1007/BF01195314
21. Martinez DA, Vazquez JL, Pellicer E, Aguayo JL, Morales G, Moreno-Egea A. Results of expanded polytetrafluoroethylene patches in moderate and large incisional hernias. Hernia (1999) 3:149–52. doi: 10.1007/BF01195316
22. Oussoultzoglou E, Baulieux J, De la Roche E, Peregne V, Adham M, Berthoux N, et al. Long-term results of 186 patients with large incisional abdominal wall hernia treated by intraperitoneal mesh. Ann Chir. (1999) 53:33–40.
23. Bernard C, Polliand C, Mutelica L, Champault G. Repair of giant incisional abdominal wall hernias using open intraperitoneal mesh. Hernia (2007)11:315–20. doi: 10.1007/s10029-007-0222-7
24. Iannitti DA, Hope WW, Norton HJ, Lincourt AE, Millikan K, Fenoglio ME, et al. Technique and outcomes of abdominal incisional hernia repair using a synthetic composite mesh: a report of 455 cases. J AM Coll Surg. (2008) 206:83–8. doi: 10.1016/j.jamcollsurg.2007.07.030
25. De Vriesa Reilingh TS, van Goor H, Charbon JA, Rosman C, Hesseling EJ, van der Wilt GJ, et al. Repair of giant midline abdominal wall hernias: “Components Separation Technique” versus prosthetic repair interim analysis of a randomized controlled trial. World J Surg. (2007) 31:756–63. doi: 10.1007/s00268-006-0502-x
26. Ammaturo C, Bassi UA, Bassi G. Outcomes of the open mesh repair of large incisional hernias using an intraperitoneal composite mesh: our experience with 100 cases. Updates Surg. (2010) 62:55–61. doi: 10.1007/s13304-010-0002-2
27. Lo Monte AI, Damiano G, Plumbo VD, Zumbino C, Spelli G, Sammatono A, et al. Eight-point compass rose underlay technique in 72 consecutive elderly patients with large incisional hernia international. J Gerontol. (2011) 5:161–5. doi: 10.1016/j.ijge.2011.09.032
28. Liu F, Li J. Repair of large abdominal wall defects using the Proceed surgical mesh with open intra-peritoneum onlay method. Saudi Med J. (2011) 32:504–9.
29. Köckerling F, Schug-Pass C, Scheuerlein H. What is he current knowledge about sublay/retro-rectus repair of incisional hernias? Front Surg. (2018) 5:47. doi: 10.3389/fsurg.2018.00047
30. Arnaud JP, Tuech JJ, Pessaux P, Hadchity Y. Surgical Treatment of Postoperative Incisional Hernias by Intraperiotneal Insertion of Dacron Mesh and an aponeurotic graft. Arch Surg. (1999) 134:1260–2.
31. Hamy A, Pessaux P, Mucci-Hennekinne S, Radriamananjo S, Regenet N, Arnaud JP. Surgical Treatment of Large Incisional Hernias by an intraperitoneal dacron mesh and an aponeurotic graft. J Am Coll Surg. (2003) 196:531–4.
32. Briennon X, Lerite E, Meunier K, Besbois E, Hamy A, Arnaud JP. Surgical treatment of large incisional hernias by intraperitoneal insertion of Parietex® composite mesh with an associated aponeurotic graft (280 cases). J Visc Surg. (2011) 148:54–8. doi: 10.1016/j.jviscsurg.2010.12.007
33. Williams RF, Martin DF, Mulroony MT, Voeller GR. Intraperitoneal modification of the Rives-Stoppa repair for large incisional hernias Hernia (2008)12:141–5. doi: 10.1007/s10029-007-0300-x
34. Heartsill L, Richards ML, Arfai N, Lee A, Bingener-Casey J, Schwesinger WH, et al. Open rives-stoppa ventral hernia repair made simple and successful but not for everyone. Hernia (2005) 9:162–6. doi: 10.1007/s10029-005-0319-9
35. Rosen MJ, DeNoto G, Itani KMF, Butler C, Vargo D, Smiell J, et al. Evaluation of surgical outcomes of retro-rectus versus intraperitoneal reinforcement with bio-prosthetic mesh in the repair of contaminated ventral hernias. Hernia (2013)17:31–5. doi: 10.1007/s10029-012-0909-2
36. Helgstrand F, Rosenberg J, Kehlet H, Jorgensen LN, Bisgaard T. Nationwide prospective study of outcomes after elective incisional hernia repair. J Am Coll Surg. (2013) 216:217–28. doi: 10.1016/j.jamcollsurg.2012.10.013
37. Den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW. Open surgical procedures for incisional hernias cochrane database. Syst Rev (2008) 16:CD006438. doi: 10.1002/14651858.CD006438.pub2
38. Albino FP, Patel KM, Nahabendian MY, Sosin M, Attinger CE, Bhanot P. Does Mesh location matter in abdominal wall reconstruction? a systematic review of the literature and a summary of recommendations. Plast Reconstr Surg. (2013) 132:1295–304. doi: 10.1097/PRS.0b013e3182a4c393.
39. Holihan JL, Nguyen DH, Nguyen MT, Mo J, Kao LS, Liang MK. Mesh location on open ventral hernia repair: a systematic review and network meta-analysis. World J Surg. (2015) 40:89–99. doi: 10.1007/s00268-015-3252-9.
40. Holihan JL, Hannon C, Goodenough C, Flores-Gonzales JR, Itani KM, Olavarria O, et al. Ventral hernia repair: a meta-analysis of randomized controlled trials. Surg Infect. (2017) 18:647–58. doi: 10.1089/sur.2017.029
41. Kurian A, Gallagher S, Cheeyandira A, Josloff R. Laparoscopic repair of primary versus incisional ventral hernias: time to recognize the differences? Hernia (2010) 14:383–7. doi: 10.1007/s10029-010-0649-0
42. Subramanian A, Clapp ML, Hicks SC, Awad SS, Liang MK. Laparoscopic ventral hernia repair: primary versus secondary hernias. J Surg Res. (2013) 181:e1–5. doi: 10.1016/j.jss.2012.06.028
43. Stirler VMA, Schoenmaeckers EJP, de Haas RJ, Raymakers JTFJ, Rakic S. Laparoscopic repair of primary and incisional ventral hernias: the differences must be acknowledged. Surg Endosc. (2013) 28:891–5. doi: 10.1007/s00464-013-3243-6
44. Köckerling F, Schug-Paß C, Adolf D, Reinpold W, Stechemesser B. Is pooled data analysis of ventral and incisional hernia repair acceptable? Front Surg. (2015) 2:15. doi: 10.3389/fsurg.2015.00015
45. Kroese LF, Gillion JF, Jeekel J, Kleinrensind GJ, Lange JF. Hernia-Club members primary and incisional ventral hernias are different in terms of patient characteristics and postoperative complications – A prospective cohort study of 4,565 patients. Int J Surg. (2018) 51:114–9. doi: 10.1016/j.ijsu.2018.01.010
Keywords: incisional hernia, open intraperitoneal onlay, IPOM, surgical site infection, seroma, wound complication
Citation: Köckerling F and Lammers B (2018) Open Intraperitoneal Onlay Mesh (IPOM) Technique for Incisional Hernia Repair. Front. Surg. 5:66. doi: 10.3389/fsurg.2018.00066
Received: 27 August 2018; Accepted: 01 October 2018;
Published: 23 October 2018.
Edited by:
Hakan Kulacoglu, Recep Tayyip Erdogan University, TurkeyCopyright © 2018 Köckerling and Lammers. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ferdinand Köckerling, ferdinand.koeckerling@vivantes.de
 Ferdinand Köckerling
Ferdinand Köckerling Bernhard Lammers2
Bernhard Lammers2