- 1Department of Physical Therapy, University of Pittsburgh, Pittsburgh, PA, United States
- 2National Council on Aging Center for Healthy Aging, Arlington, VA, United States
- 3Department of Medicine and Biostatistics, University of Pittsburgh, Pittsburgh, PA, United States
- 4Administration for Community Living, Washington, DC, United States
Background: Using the RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) framework, we describe the implementation of evidence-based chronic disease self-management education (CDSME) programs by the Administration for Community Living CDSME Grantees during 2016–2022 and we also explore the impact of the COVID-19 pandemic on implementation.
Methods: Grantees collected data before and after the implementation of the CDSME programs and contributed to the national data repository. Data components included workshop information, participant information, and organizational data.
Results: The cohort consisted of 175,973 individuals who participated in 34 CDSME programs across 45 states. Participants had a mean ± SD age of 66.1 ± 14.8 years, were primarily female (65.9%) and had a mean ± SD of 2.6 ± 2.3 chronic conditions. Compared to the pre-COVID-19 strata, those who participated during COVID-19 were on average 1.5 years younger and had slightly less comorbidities. For individuals who had pre and post program self-reported health, 65.3% stayed the same, 24.4% improved, and 10.3% worsened (p < 0.001) after participating in CDSME programs.
Conclusion: CDSME offers a variety of programs across a broad geographic area to a diverse set of older adults in the US, underscoring the expansive reach of this public health initiative. COVID-19 appears to have shifted participant reach toward a slightly younger and healthier population. Finally, these programs appear to be effective in improving participants’ self-rated health. However, these results should be interpreted with caution, given limitations due to missing data and the observational nature of this study design.
Introduction
Chronic disease is a common and costly problem in the United States with more than half of the US population having at least one chronic condition, and up to one-third having more than one (1, 2). The prevalence of chronic disease increases with age and in those 60 years of age or older, virtually everyone has at least one chronic disease and 80% have two or more (i.e., multimorbidity) (3). The health consequences are dire, as chronic diseases often lead to a loss of functional independence, (4–6) social isolation, (7) cognitive decline, (3, 8) and mortality (5, 6). In addition, the cost associated with chronic disease is enormous (9), with more than two-thirds of all healthcare costs go toward treating patients with chronic illnesses, and 95% of all Medicare spending is associated with chronic conditions (10).
Optimal chronic disease management has become the holy grail for patients, providers, policymakers, population health experts, and the research community (10, 11). Though each chronic disease provides a unique experience, many overlap in the behavioral risk factors (i.e., physical inactivity, poor nutrition, tobacco-use, and excessive alcohol consumption) that contribute to the development and progression of these conditions. Evidence-based chronic disease self-management education (CDSME) programs are public health interventions that target known behavioral risk factors by promoting behavior change within community networks. Evidence-based CDSME programs differ in their specific focus and may include various elements, including exercise and skills training. These efficacious programs have been rigorously studied and translated into practice models for community-based implementation (12). Analyses of specific CDSME programs have also demonstrated economic benefits (13–16). For example, participation in Stanford Chronic Disease Self-Management Program™ resulted in net benefit of $364 per participant, which translates to $8.9 billion if just 10% of the population with chronic disease participated (13).
Since the early 2000s, the Administration on Aging (AoA) has been building a comprehensive infrastructure for the delivery and sustainability of various evidence-based health promotion programs to support healthy aging. Since 2012, the Administration for Community Living (ACL), an operating division of the U.S. Department of Health and Human Services, has received dedicated funding through the Affordable Care Act’s Prevention and Public Health Fund to support dissemination of evidence-based CDSME programs. The ACL awards competitive grants in the form of cooperative agreements to states, community-based organizations, tribal entities, and institutions of higher education to support capacity building, scaling, and sustainability of evidence-based CDSME programs. Since 2017, the ACL has awarded approximately $38 million in cooperative agreements to support CDSME program dissemination and implementation.
While specific evidence-based CDSME programs have been studied in detail, implementation has generally been evaluated on an individual program or single organization basis. Much can be learned about the collective implementation of evidence-based CDSME programs over time. Implementation evaluation can provide an overview of real-world success and identify targets to guide future efforts for communities and policymakers. Furthermore, evaluation of recent data can help illustrate the impact of the COVID-19 pandemic on the implementation of these programs. Early in the pandemic, community programming was suspended, but as the pandemic progressed the use of remote delivery options, such as video-conferencing, phone and mail, were implemented for some but not all programs (17). The return to in-person program delivery varied greatly by state and type of site. Documenting the impact of the pandemic on the reach of these programs may inform efforts to develop alternative delivery options that are acceptable and available to all individuals.
Using the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework, we examine the implementation of the ACL-approved evidence-based CDSME programs. The RE-AIM framework is a commonly accepted model to plan and examine implementation success for various health promotion and healthcare initiatives across clinical, community, and work settings (18). Our specific purpose for these secondary analyses was to describe the reach and explore the effectiveness of these programs over recent years. We also explored how the COVID-19 pandemic, which had a well-known impact on communities (e.g., restrictions on in-person gatherings), affected reach and effectiveness.
Findings from this work will inform the efforts of the national CDSME network of partners. National CDSME Resource Center data can be used to examine the number, proportion, and representativeness of people who participated in an evidence-based CDSME program that was supported by the ACL. Furthermore, while these programs have been rigorously studied to ensure there are benefits to participants, evaluating these data allows for quality assurance (e.g., correcting program drift). Ultimately, these data are also crucial in the justification of ongoing support from policymakers and their constituents, which ensures the continuation of necessary funds to support this critical public health endeavor.
Materials and methods
Study participants and procedures
These analyses used data from the National CDSME Resource Center’s data repository. All ACL grantees are required to use this national database as a condition of funding. These data reflect various program workshop, delivery site, and participant information. Program workshop leaders collected these data, and organizations that hosted the workshops coordinated data entry into the repository in a centralized or decentralized manner at the state, regional or local level. Grantees employed methods of data collection, including paper-based, interviewer-administered, and electronic capture, that worked best for their individual location. All participant-specific data were de-identified and aggregated. For this study, data were limited to participants who started and completed a CDSME program in either January 1, 2016–December 31, 2019, or January 1, 2021 – October 4, 2022 (i.e., the last day the repository was updated before starting these analyses). To form clear subgroups that represented pre- and post- COVID-19 epidemic onset, data from participants who started or finished within the 2020 timeframe were excluded, because the degree and timing of specific public health restrictions varied by region. Additionally, it is important to note that these data reflect programs implemented by ACL CDSME grantees and, as such, do not include other areas or organizations that offered CDSME programs, not required to use the repository. This study which involved secondary data analysis was deemed exempt by the University of Pittsburgh Institutional Review Board as it did not include identifiable data.
Data and measures
Program characteristics
The national data repository includes more than 30 different evidence-based CDSME programs. The programs included in this analysis were those that were deployed by ACL grantees during the timeframe of interest (i.e., 2016–2019 or 2021–2022).
Delivery site characteristics
The organizational infrastructure where CDSME programs were offered was diverse, and grantees classified the delivery sites as one of the following setting types: senior center; residential facility; healthcare organization; faith-based organization; community center; parks and recreation/other recreational organization; Area Agency on Aging/multi-purpose social services/state unit on aging; library; county health department/municipal government/state health department; educational institution; tribal center; workplace; other. The state and county where each workshop was implemented was also reported. Most grantees offered more than one program and reached multiple implementation sites.
Participant characteristics and outcomes
Grantees collected participant information during an orientation session (if applicable) or the first program session, as well as upon program completion. Though encouraged by workshop leaders, individuals were not required to complete the participant survey to participate in the program. During the pre-program survey (i.e., baseline), participants reported their age, sex, race/ethnicity, education level, and living arrangements. Participants also reported the presence/absence of 16 different chronic conditions (e.g., heart disease, cancer), and whether they felt their activities were limited in any way due to physical, mental, or emotional problems.
Uniform outcome assessment is an evolving target for the National CDSME Resource Center, especially among CDSME programs, which have diverse structures and foci. Currently, participants are asked to answer the following questions (1) “in general, would you say that your health is excellent, very good, good, fair or poor?” (i.e., self-rated health) and (2) “how often do you feel lonely or isolated from those around? Always, often, sometimes, rarely, or never?.” Self-rated health was introduced to the pre- and post-program surveys in November 2016 and August 2017, respectively. Frequency of feeling lonely or isolated was introduced to both pre- and post-program surveys in February 2020. For these analyses, we considered self-rated health to be our primary exploratory outcome, given the longer history of its use in CDSME outcome assessment and its robust prognostic properties regarding future health events. We considered frequency of feeling lonely or isolated to be our secondary exploratory outcome.
Statistical analyses
Statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC). Descriptive analyses included means and standard deviations for continuous variables, as well as frequencies and proportions for categorical variables. Independent samples t test and chi-squared tests were used to compare those who participated pre-COVID (i.e., 2016–2019) and during COVID (i.e., 2021–2022) on all pre-program characteristics. To explore overall effectiveness of CDSME programs, we restricted our analytic cohort to those who completed pre- and post-program self-rated health, and we compared them to those who only completed pre-program self-rated health to assess any dropout bias. Among this restricted analytic cohort, we then used Bowker’s symmetry tests to compare pre- vs. post-program self-rated health and frequency of feeling lonely or isolated.
Results
Reach
Program level
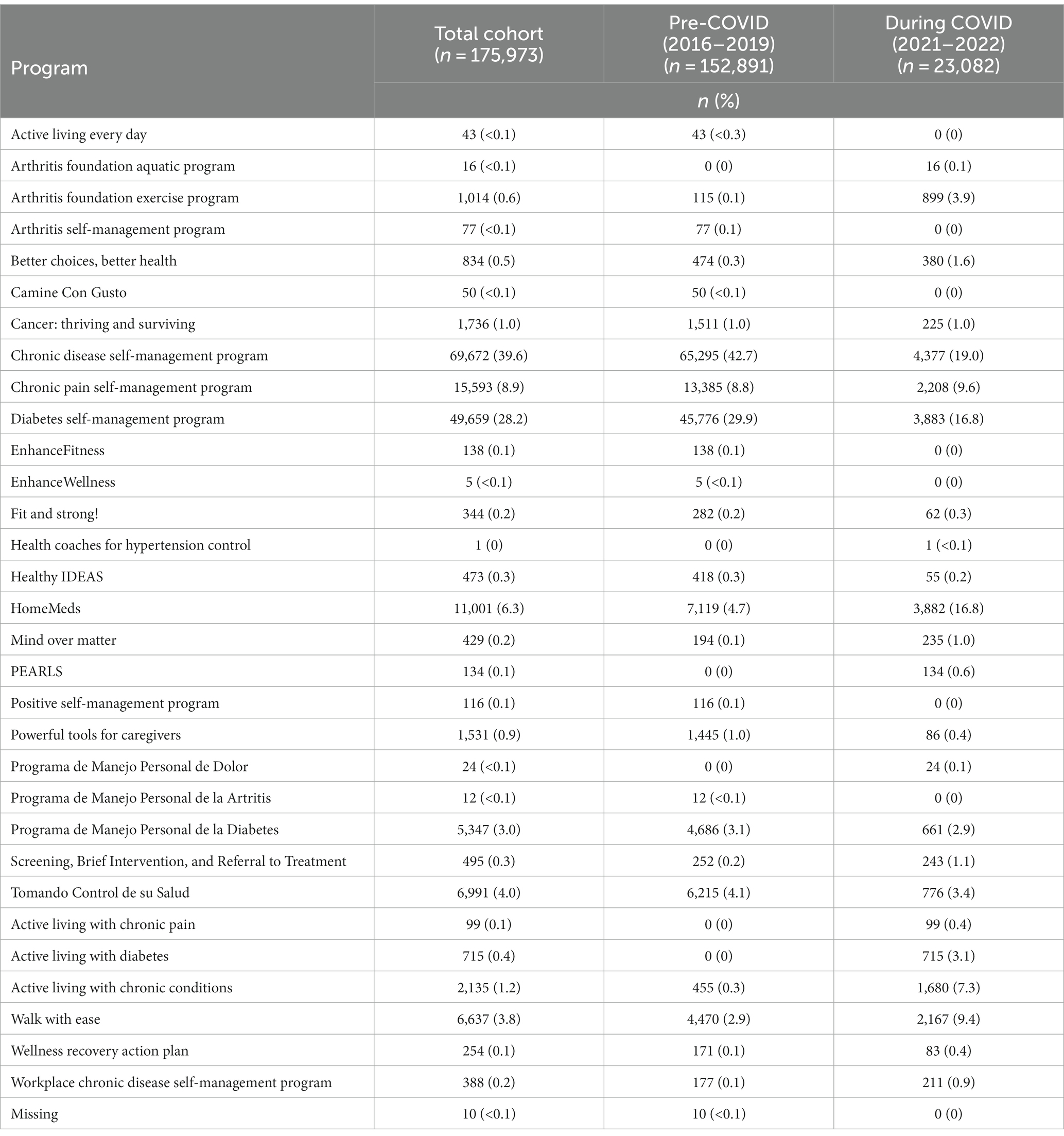
The number of participants by CDSME program is displayed in Table 1. The cohort consisted of 175,973 participants who participated in 34 CDSME programs. The programs with the most participation included the Chronic Disease Self-Management Program (39.6%), the Diabetes Self-Management Program (28.2%), and the Chronic Pain Self-Management Program (8.9%). We also examined how program participation changed from pre-COVID to during COVID. Descriptively, the proportion of individuals who participated in those three programs declined from pre-COVID to during COVID timeframes, while the proportion of individuals who participated in HomeMeds and Walk with Ease increased.
Delivery site level
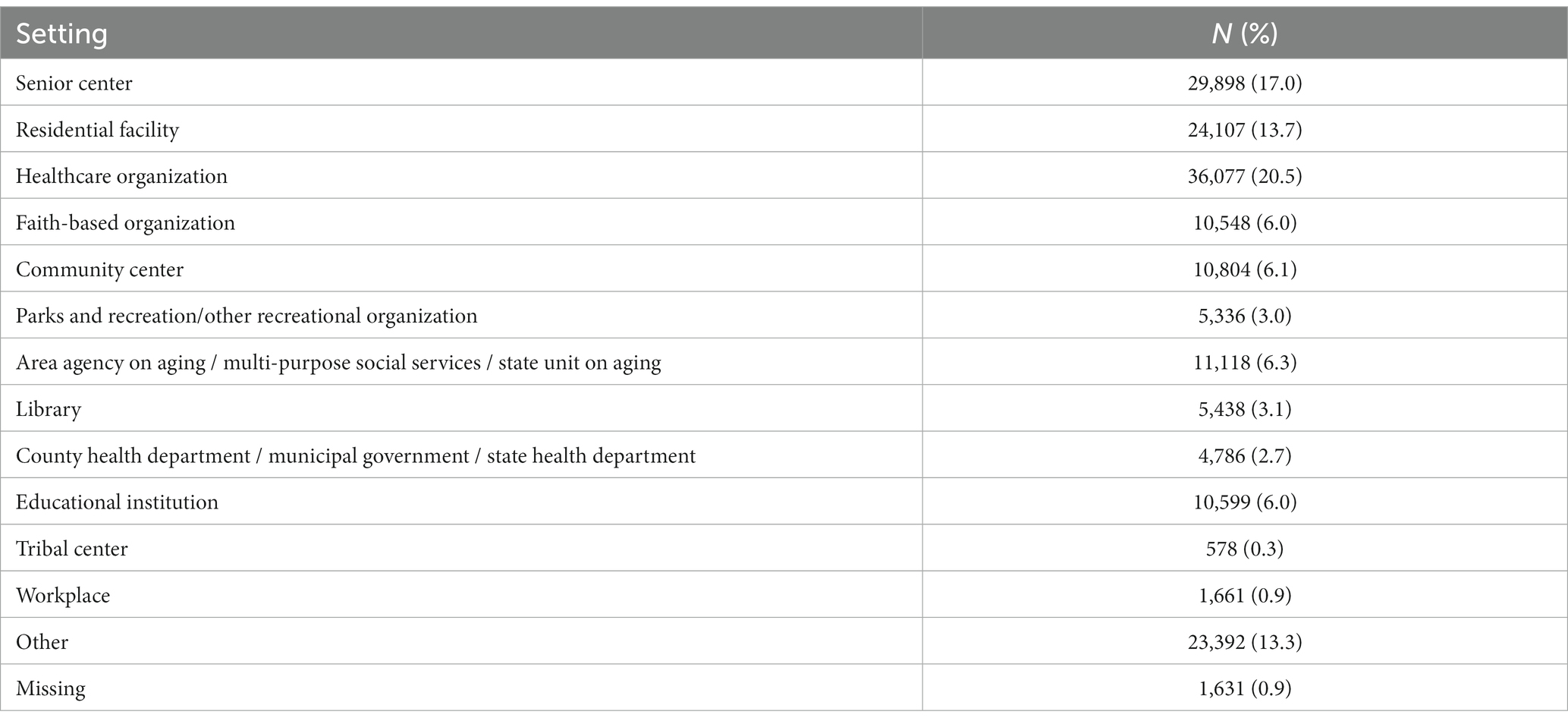
The number of individuals who participated in CDSME programs by state is illustrated in Figure 1. States with the greatest number of participants (>9,000) were Florida, New York, Virginia, California, Wisconsin, and Texas. Table 2 displays the number of individuals who participated by setting type, with the most common settings being healthcare organizations (20.5%), senior centers (17.0%), and residential facilities (13.7%).
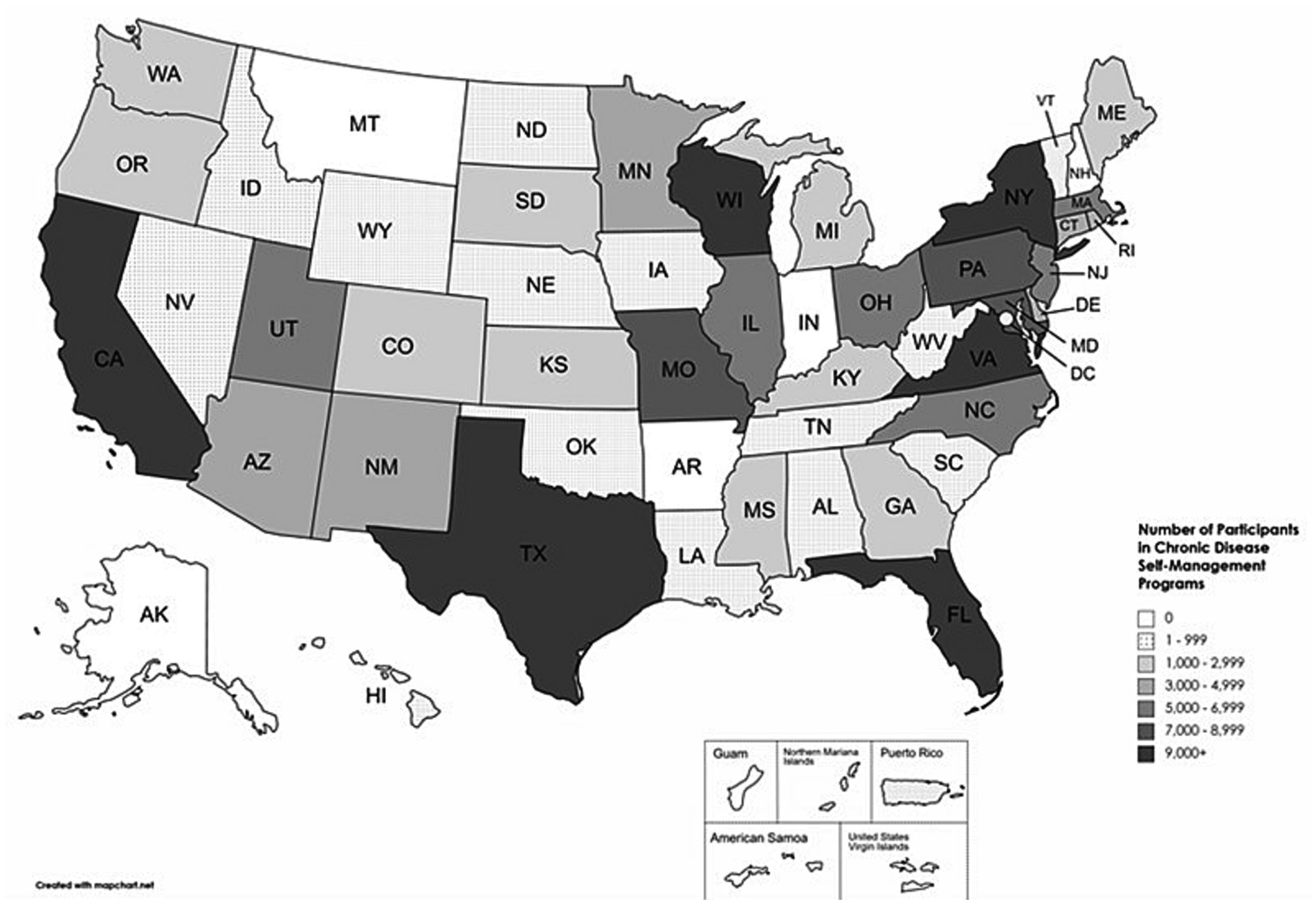
Figure 1. The number of individuals who participated in chronic disease self-management education programs by state.
Participant level
Participant characteristics for the total cohort (n = 175,973), pre-COVID strata (i.e., 2016–2019; n = 152,891), and during COVID strata (i.e., 2021–2022; n = 23,082) are displayed in Table 3. Participants had a mean ± SD age of 66.1 ± 14.8 years and were primarily female (65.9%). Individuals from various racial and ethnic groups participated, but the cohort was primarily White (55.1%) and not Hispanic or Latino (69.4%). Nearly half of the participants reported attending some college or vocational school, and approximately 10% of the sample did not complete high school. Participants had a mean ± SD of 2.6 ± 2.3 chronic conditions of the 16 assessed. The most commonly reported chronic conditions were hypertension (40.4%), arthritis (34.2%), and diabetes (33.7%). Nearly one quarter of the cohort reported being limited in activities because of physical, mental, or emotional problems. Approximately one third of the cohort rated their general overall health as good, very good, or excellent.
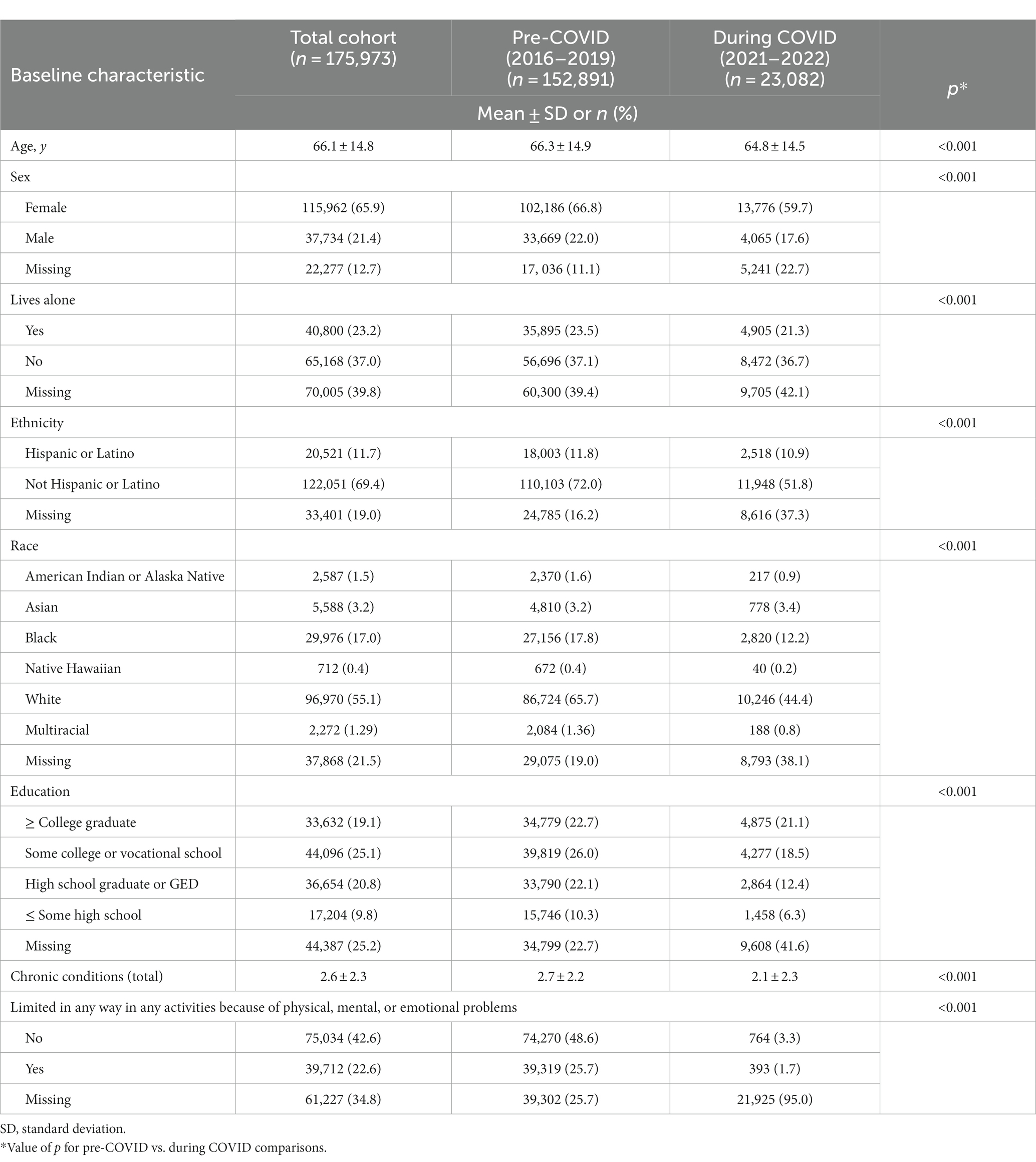
Table 3. Pre-program characteristics of the total sample, those who participated from pre-COVID pandemic (i.e., 2016–2019), and those who participated during the COVID pandemic (i.e., 2021–2022).
Several statistically significant differences existed between the pre-COVID and during COVID strata, but in many cases, statistical significance is likely due to the large sample size rather than material between-group differences. However, some differences do bear mentioning. Compared to the pre-COVID strata, those who participated during COVID were slightly younger (64.8 versus 66.3 years) and had slightly less comorbidities (2.1 versus 2.7) on average. Furthermore, we should also note that missing data were common among most factors, and missingness tended to be greater during COVID relative to pre-COVID.
Effectiveness
Table 4 illustrates the characteristics of the restricted cohort for exploring the effectiveness of CDSME programs. Of the 88,595 participants who completed pre-program self-rated health, 5,675 participants completed their post-program self-rated health (i.e., the restricted analytic cohort), while 82,920 participants did not. As noted above, post-program self-rated health was not introduced until August 2017, nearly 2 years after the start of the data collection. Thus, a certain degree of missingness for post-program self-rated health was to be expected by virtue of delayed deployment. Compared to those who only completed the pre-program self-rated health outcome, those who completed both pre- and post-program questions differed significantly on many characteristics. Like pre- and during COVID comparisons, however, many differences are likely due to large sample size rather than material between-group differences or differences in the degree of missingness (i.e., individuals who completed both pre- and post-program self-rated health tended to have more complete data). Of note, those who completed both pre- and post-program self-rated health were slightly younger than those who completed only pre-program self-rated health.
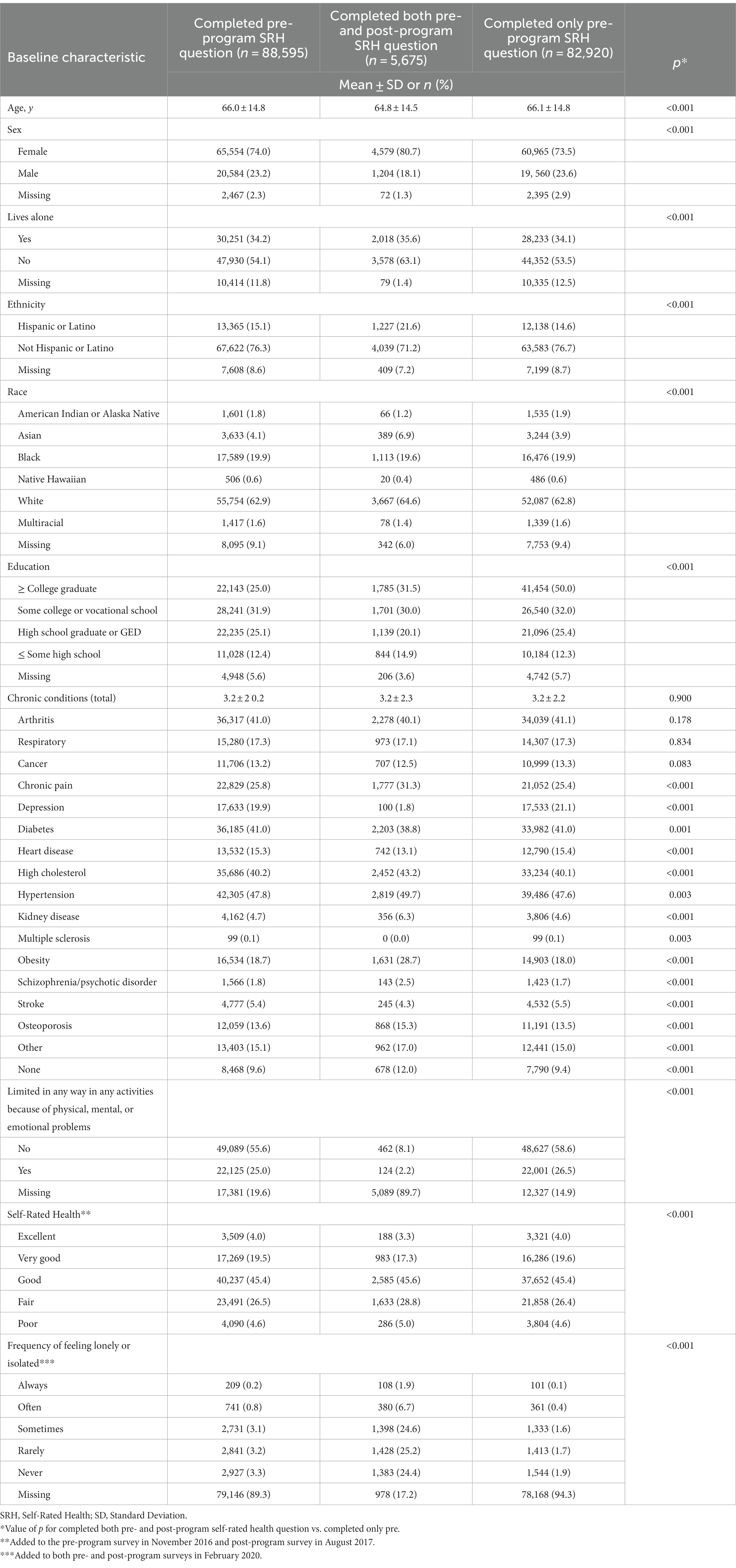
Table 4. Baseline characteristics for all participants who completed the preprogram self-rated health question, participants who completed both pre- and post-program self-rated health question, and those who only completed the pre-program self-rated health question (2016–2019, 2021–2022).
Figure 2 displays participants’ pre- and post-program self-rated health and frequency of feeling lonely or isolated for the analytic cohort. Cells highlighted in green indicate participants who improved from pre- to post-program, the white cells indicate those who stayed the same, and the red cells indicate those who worsened. For self-rated health, 65.3% stayed the same, 24.4% improved, and 10.3% worsened (p < 0.001). For frequency of feeling lonely or isolated, 51.3% stayed the same, 14.8% improved, 14.6% worsened, and 19.3% were missing either pre- or post-program data (p < 0.001).
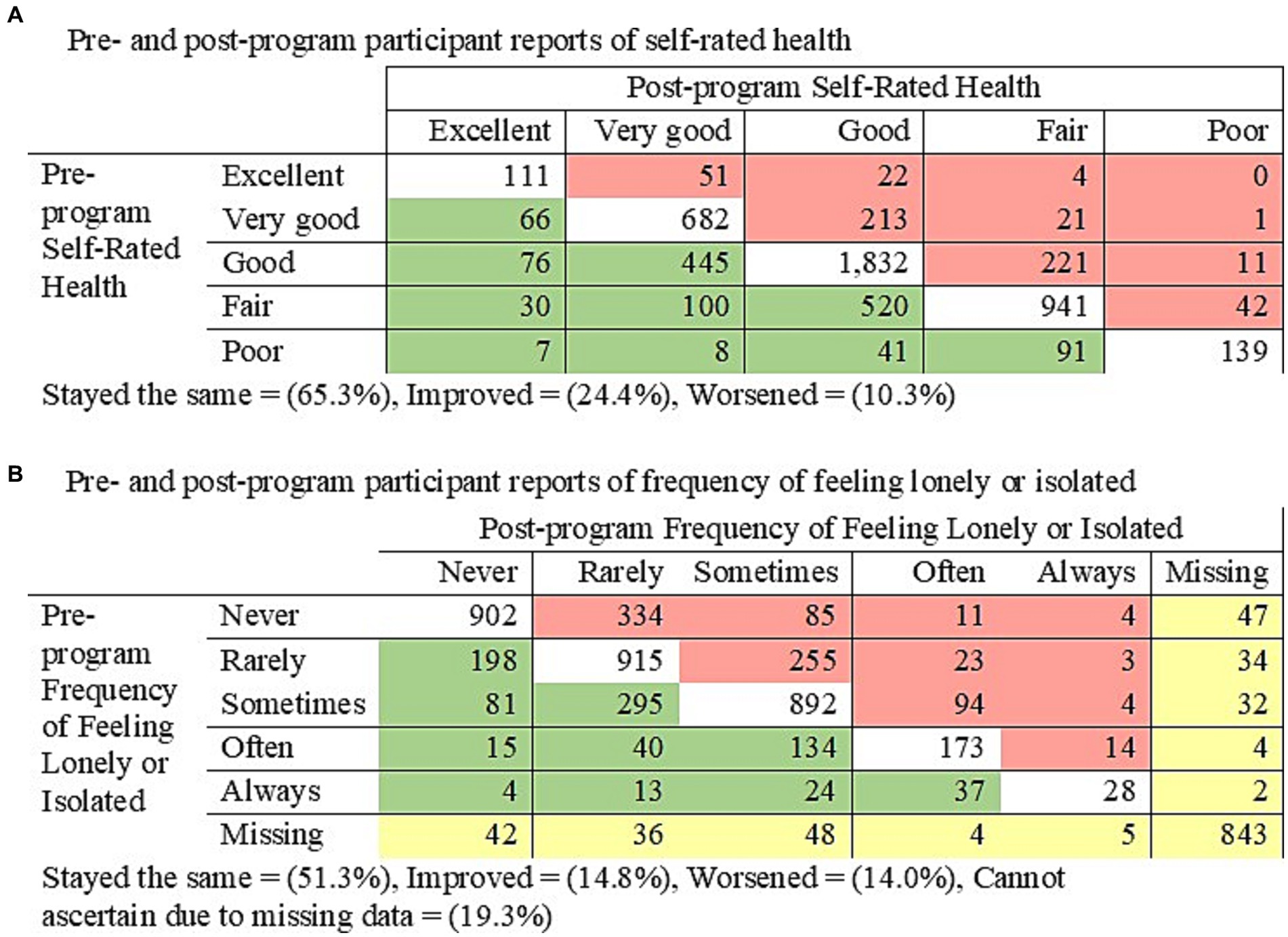
Figure 2. Symmetry tests for pre- to post-program (A) self-rated health (p < 0.001) and (B) frequency of feeling lonely or isolated (p < 0.001).
Discussion
During the nearly 6 years of CDSME program participation observed, the CDSME evidence-based programs reached over 175,000 older adults and adults with disabilities in 45 states, in addition to Washington D.C. and Puerto Rico. The CDSME programs were offered in numerous settings, including senior centers, residential facilities, and healthcare organizations. Though missing data on demographic variables prevent us from drawing definitive comparisons to the broader US older adult population, the sample contains participants of varying racial, ethnic, educational, and health backgrounds.
This dataset also allowed us to examine the impact COVID-19 had on CDSME reach. Shifts in program popularity from pre-COVID-19 to during COVID-19 was observed. For example, there was a decline in the proportion of people who participated in the Chronic Disease Self-Management Program (pre-COVID-19 = 42.7% vs. during COVID-19 = 19.0%), while the proportion of people who participated in the HomeMeds program increased (pre-COVID-19 = 4.7% vs. during COVID-19 = 16.8%). These shifts are unsurprising given the nature of program format, wherein some programs (e.g., Chronic Disease Self-Management Program) were often delivered in-person to groups of participants and others (e.g., HomeMeds) were delivered one-on-one or virtual (12). It should be noted that the COVID-19 pandemic led to innovations in program formatting (e.g., shifting to virtual models) (17). However, creating uniform data collection methods often lags behind changes in program implementation, and data reflecting program format were not consistently reported.
Shifts in participant demographics were also observed pre-COVID-19 vs. during COVID-19. Statistically significant differences were common across several participant characteristics (e.g., sex, living situation, ethnicity, and race). However, large sample sizes offer great statistical power, and many of these differences may not be material in nature. Furthermore, missing data prevents us from drawing definitive conclusions about shifts in participant demographics, and missing data appears to be more common since the COVID-19 pandemic. One notable difference, however, occurred with respect to age and number of chronic conditions. Compared to pre-COVID-19, those who participated during COVID-19 appear to be slightly younger and healthier. Though some programs provided alternative delivery formats that allowed for social distancing others did not. Thus, it is possible that older and less healthy adults may avoid in-person participation due to the potential COVID-19 exposure. In addition, alternative delivery formats that require technology may be a barrier to some older adults who do not have access to technology or are less comfortable using technology (17).
Of the approximately 175,000 participants in our sample, only 5,675 completed both the pre- and post-program assessments of self-rated health, our primary outcome of CDSME effectiveness. As mentioned before, post-program self-rated health assessment was not introduced into the data collection process until August 2017, thus, some missing data are to be expected. Nevertheless, our data indicate that there were significantly more improvements (24.4%) in self-rated health following program participation, compared to declines (10.3%). These findings are notable given the robust predictive nature of self-rated health (19–21). For example, in one cohort study, self-rated health had similar predictive capability of 10-year mortality rates compared to a comprehensive measure of objective health, which included assessments of the presence of various diseases, ability to perform specific activities of daily living, and psychological wellbeing (21). Self-rated health is a subjective indicator of health status that reflects various domains of health and wellbeing (e.g., biological, mental, social, and functional), which allows a person to weigh the importance of each underlying factor according to their own individual and cultural beliefs relative to health and health behaviors. Thus, this seemingly simple outcome measure should be an essential aspect of program effectiveness evaluation.
An ACL-approved “evidence-based program,” must have demonstrated efficacy using either an experimental or quasi-experimental design (22). Thus, the CDSME programs included in these analyses were shown to be effective in previous research studies across a variety of health outcomes. However, uniform outcome assessment that applies to all CDSME programs is difficult to obtain. Each CDSME program has a unique disease focus, approach, and goals. Given its independence from any one disease or condition, self-rated health is an attractive tool for assessing the effectiveness of CDSME programs without focusing on any specific disease or condition. Future efforts should be dedicated to identifying a comprehensive but parsimonious collection of meaningful outcomes that apply to all CDSME programs, which supplement self-rated health.
Of note, we found the proportion of people who improved (14.8%) and declined (14.6%) relative to how often they felt lonely or isolated. Feelings of loneliness and isolation are a serious health concern linked to chronic disease, (23) and we felt it important to include this as a possible outcome relative to program effectiveness. Moreover, many CDSME programs include a group and/or in-person component, which may lead to an expansion of social networks and thereby combat feelings of loneliness or isolation. The lack of clear improvements in this important outcome may have occurred for a variety of reasons. First, this measure was introduced in CDSME program data collection process in February 2020; in our analyses, only those who participated during COVID (i.e., 2021–2022) had data on this outcome measure. Second, feelings of social isolation may be only partially related to chronic disease status, and thus the impact of CDSME programs may be too small as to be discernable or material.
We should also note the significant limitations to our study and findings. First and foremost, the degree of missing data limits the ability to generalize and draw definitive conclusions from our results. Thus, we considered some of our analyses (i.e., effectiveness evaluation) to be exploratory in nature. Internal tracking by the National CDSME Resource Center staff (data not shown) indicate that grantees had challenges with several aspects of the data collection process. For example, grantees expressed concerns over the inefficient means of data collection (i.e., paper surveys), the time required to enter data into the database, program leaders’ compliance with reporting data in a timely manner, and staff turnover. These issues identify clear opportunities for process improvement, which may include streamlining data collection through virtual data capture (e.g., providing tablets to complete surveys), incentivizing data collection for program leaders and participants, and developing internal reporting processes for monitoring quality and completeness of collection. Such improvements could lead to more robust analyses that help determine for whom specific programs are most effective (i.e., precision public health).
In addition to missing data, we should also note limitations concerning our study design and analytical approach. From the perspective of reach, we examined geographical distribution at the state-level to ascertain a broad definition of reach. However, there is opportunity to examine geography precisely at the county and zip-code level of program delivery sites. These analyses may offer a more nuanced understanding of whether these programs are reaching under-resourced areas, where there is potentially a more urgent need for public health interventions. Also, our study design was observational in nature, and therefore causality cannot be definitively determined when evaluating effectiveness. Future research may consider quasi-experimental designs, if possible, to strengthen study conclusions.
Despite these limitations, there are notable strengths to our study. To our knowledge, this dataset is the only one of its kind, offering a unique ability to answer our research questions. Despite missing data, our findings were also robust, particularly with respect to exploring CDSME program impact on self-rated health. In addition, this dataset is diverse from a sociodemographic perspective, containing data from thousands of participants from traditionally underrepresented backgrounds. Thus, the findings from this study may be more generalizable to populations not traditionally captured in conventional research studies.
In conclusion, CDSME offers a variety of programs across a broad geographic area to a diverse set of older adults in the US, underscoring the expansive reach of this public health initiative. COVID-19 appears to have shifted CDSME program offerings toward those with formats that limit group exposure, and to have shifted participant reach toward a slightly younger and healthier population. Finally, these programs appear to be effective in improving participants’ self-rated health.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by University of Pittsburgh Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. This study which involved secondary data analysis was deemed exempt by the University of Pittsburgh Institutional Review Board as it did not contain identifiable data.
Author contributions
PC: Conceptualization, Writing – original draft, Writing – review & editing. JT: Conceptualization, Writing – review & editing. SP: Conceptualization, Formal analysis, Methodology, Writing – review & editing. GJ: Writing – review & editing. LS-B: Writing – review & editing. KC: Conceptualization, Supervision, Writing – review & editing. JB: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported in part by the National Institute on Aging at the National Institutes of Health (K24 AG057728 to JB and P30 AG024827). This project was supported by the Administration for Community Living (ACL), U.S. Department of Health and Human Services (HHS). The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by ACL/HHS, or the U.S. Government.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Buttorff, C , Teague, R , and Bauman, M . Multiple chronic conditions in the United States. Santa Monica, CA: RAND Corporation; (2017).
2. Boersma, P , Black, LI , and Ward, BW . Prevalence of multiple chronic conditions among US adults, 2018. Prev Chronic Dis. (2020) 17:E106. doi: 10.5888/pcd17.200130
3. Tavaraes, JC , Silberman, M , and Popham, S , Chronic inequities: Measuring disease cost burden among older adults in the U.S. Available at: https://ncoa.org/article/the-inequities-in-the-cost-of-chronic-disease-why-it-matters-for-older-adults. (2022). Accessed June 23, 2023.
4. Ryan, A , Wallace, E , O'Hara, P , and Smith, SM . Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. (2015) 13:168. doi: 10.1186/s12955-015-0355-9
5. Wei, MY , Kabeto, MU , Galecki, AT , and Langa, KM . Physical functioning decline and mortality in older adults with multimorbidity: joint modeling of longitudinal and survival data. J Gerontol A Biol Sci Med Sci. (2019) 74:226–32. doi: 10.1093/gerona/gly038
6. Wei, MY , and Mukamal, KJ . Multimorbidity, mortality, and long-term physical functioning in 3 prospective cohorts of community-dwelling adults. Am J Epidemiol. (2018) 187:103–12. doi: 10.1093/aje/kwx198
7. Theis, KA , and Furner, SE . Shut-in? Impact of chronic conditions on community participation restriction among older adults. J Aging Res. (2011) 2011:759158. doi: 10.4061/2011/759158
8. Centers for Disease Control and Prevention . Chronic diseases and cognitive decline - - a public health issue. Available at: https://www.cdc.gov/aging/publications/chronic-diseases-brief.html#print. Accessed June 23, 2023.
9. Waters, HG M . The costs of chronic disease in the U.S. Milken institute. Available at: https://milkeninstitute.org/report/costs-chronic-disease-us?gclid=CjwKCAjwhdWkBhBZEiwA1ibLmBiDcqG4ryt3-lEfdM94ZVSu5A8W7qyqIYQyPqslVfoMUbaQ4QfObRoC3wYQAvD_BwE. (2018). Accessed June 23, 2023.
10. Centers for Disease Control and Prevention . The state of aging and health in America 2013. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Helath and Human Services (2013).
11. Grover, A , and Joshi, A . An overview of chronic disease models: a systematic literature review. Glob J Health Sci. (2014) 7:210–27. doi: 10.5539/gjhs.v7n2p210
12. The National Council on Aging . Evidence-Based Chronic Disease Self-Management Education Programs. Available at: https://ncoa.org/article/evidence-based-chronic-disease-self-management-education-programs. (2021). Accessed June 20, 2023.
13. Ahn, S , Basu, R , Smith, ML , Jiang, L , Lorig, K , Whitelaw, N, et al. The impact of chronic disease self-management programs: healthcare savings through a community-based intervention. BMC Public Health. (2013) 13:1141. doi: 10.1186/1471-2458-13-1141
14. Basu, R , Ory, MG , Towne, SD Jr, Smith, ML , Hochhalter, AK , and Ahn, S . Cost-effectiveness of the chronic disease self-management program: implications for community-based organizations. Front Public Health. (2015) 3:27. doi: 10.3389/fpubh.2015.00027
15. Ackermann, RT , Williams, B , Nguyen, HQ , Berke, EM , Maciejewski, ML , and LoGerfo, JP . Healthcare cost differences with participation in a community-based group physical activity benefit for medicare managed care health plan members. J Am Geriatr Soc. (2008) 56:1459–65. doi: 10.1111/j.1532-5415.2008.01804.x
16. Nguyen, HQ , Ackermann, RT , Berke, EM , Cheadle, A , Williams, B , Lin, E, et al. Impact of a managed-Medicare physical activity benefit on health care utilization and costs in older adults with diabetes. Diabetes Care. (2007) 30:43–8. doi: 10.2337/dc06-1013
17. Steinman, L , Chavez Santos, E , Chadwick, K , Mayotte, C , Johnson, S(S) , Kohn, M, et al. Remote evidence-based health promotion programs during COVID: a National Evaluation of reach and implementation for older adult health equity. Health Promot Pract. (2023) 15248399231175843:152483992311758. doi: 10.1177/15248399231175843
18. Glasgow, RE , Vogt, TM , and Boles, SM . Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. (1999) 89:1322–7. doi: 10.2105/AJPH.89.9.1322
19. DeSalvo, KB , Bloser, N , Reynolds, K , He, J , and Muntner, P . Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. (2006) 21:267–75. doi: 10.1111/j.1525-1497.2005.00291.x
20. DeSalvo, KB , Fan, VS , McDonell, MB , and Fihn, SD . Predicting mortality and healthcare utilization with a single question. Health Serv Res. (2005) 40:1234–46. doi: 10.1111/j.1475-6773.2005.00404.x
21. Wuorela, M , Lavonius, S , Salminen, M , Vahlberg, T , Viitanen, M , and Viikari, L . Self-rated health and objective health status as predictors of all-cause mortality among older people: a prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatr. (2020) 20:120. doi: 10.1186/s12877-020-01516-9
22. Administration for Community Living . Health Promotion (2023). Available at: https://acl.gov/programs/health-wellness/disease-prevention. Accessed June 23, 2023.
Keywords: implementation, chronic disease management, community programs, COVID-19, aging
Citation: Coyle P, Tripken J, Perera S, Juarez GA, Spencer-Brown L, Cameron K and Brach JS (2024) Dissemination and implementation of evidence-based programs for people with chronic disease: the impact of the COVID-19 pandemic. Front. Public Health. 11:1276387. doi: 10.3389/fpubh.2023.1276387
Edited by:
Margareta Rämgård, Malmö University, SwedenReviewed by:
Sumarni Mohd Ghazali, Ministry of Health (Malasiya), MalaysiaZia Ul Mustafa, University of Science Malaysia, Malaysia
Lakshmy Ramakrishnan, All India Institute of Medical Sciences, India
Angela M. Goins, University of Houston–Downtown, United States
Copyright © 2024 Coyle, Tripken, Perera, Juarez, Spencer-Brown, Cameron and Brach. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer S. Brach, jbrach@pitt.edu
 Peter Coyle
Peter Coyle Jennifer Tripken2
Jennifer Tripken2 Jennifer S. Brach
Jennifer S. Brach