- 1Department of Health Education and Behavioural Sciences, Faculty of Public Health, Mahidol University, Bangkok, Thailand
- 2Department of Public Health, Sefako Makgatho Health Sciences University, Pretoria, South Africa
- 3Department of Healthcare Administration, College of Medical and Health Science, Asia University, Taichung, Taiwan
- 4Department of Psychology, University of the Free State, Bloemfontein, South Africa
- 5Department of Psychology, College of Medical and Health Science, Asia University, Taichung, Taiwan
Background: Understanding national trends in risk factors of noncommunicable diseases (NCDs) may have health policy implications. The aim of the study was to assess the prevalence and social and demographic factors associated with risk factors of NCDs in adults from 2008 to 2019 in Sao Tome and Principe.
Methods: In repeat cross-sectional national STEPS surveys 2,457 adults (median age 37 years) in 2008 and 1,893 adults (median age 38 years) in 2019 in Sao Tome and Principe responded to structured interviews, physical and biochemical measures. Logistic regressions were applied to estimate predictors of NCD risk factors.
Results: Having three to seven NCD risk factors significantly decreased among men but not women from 36.6% in 2008 to 26.8% in 2019. The proportion of specific risk factors of NCD increased significantly for low physical activity from 17.4% in 2008 to 30.9% in 2019, and overweight/obesity from 37.3% in 2008 to 51.0% in 2019. Insufficient fruit/vegetable consumption decreased from 83.1% in 2008 to 53.3% in 2019, frequent alcohol use from 32.6% in 2008 to 24.8% in 2019, and diabetes from 3.1% in 2008 to 1.2% in 2019, while the proportion of current tobacco use and hypertension remained unchanged from 2008 to 2019. Men engaged more often than women in current tobacco use and frequent alcohol use, and women had higher rates of low physical activity and overweight/obesity than men. Higher educational levels were positively associated with overweight/obesity, and inversely associated with frequent alcohol use and inadequate fruit/vegetable intake.
Conclusion: Between 2008 and 2019, the prevalence of seven risk factors for NCDs in Sao Tome and Principe declined among men, but not among women. Several associated variables have been identified for each individual risk factor of NCD that may help guide interventions.
Introduction
Most deaths from non-communicable diseases (NCDs) occur in lower resourced countries (>85%) (1). In the lower-middle-income island of Central Africa, Sao Tome and Principe, 55% of people died from NCDs in 2016 (2). Cardiovascular disease, diabetes, cancer, and respiratory disease, account for more than 80% of NCD premature deaths (1). In the general population of Sao Tome and Principe, 20% had high blood pressure and 6% hypoglycaemia (2). The ill-healthy diet, tobacco, alcohol consumption and low physical activity increase the risk of death from NCDs (1). In Sao Tome and Principe, 7% of adults engaged in harmful alcohol use and 15% were physically inactive (2). Among recent mothers in Sao Tome and Principe, more than 30% were overweight or obese (3). As the number of NCDs grows rapidly in the sub-Saharan region of Africa, including in Sao Tome and Principe (4), due to multiple factors, such as the adoption of an unhealthy lifestyle, and the increase in the average life expectancy of the population (4), it is important to understand the local factors affecting NCDs to monitor changes in burden, measure the progress of the NCD programme, and plan new activities (5). In this regard, data from national communities on single and multiple risk factors for NCDs among adults in Sao Tome and Principe are needed in planning health programmes.
In another island country in Africa in Comoros, among adults (25–64 years) the prevalence of diabetes was 8.5% (6), and overweight and obesity was 28.6 and 22.2%, respectively (7). In other African countries, for example, in Malawi, 16.5% had 3–7 risk factors of NCD (ranging from 5.6% raised blood glucose to 32.9% raised blood pressure) (8), and in Zambia, 26.7% had 3–10 risk factors of NCD (ranging from 6.2% diabetes to 90.4% insufficient fruit and vegetable intake = IFVI) (9).
Social and demographic factors associated with NCD risk factors include older age (10–13), male sex (10, 14), educational level (10, 14), and residing in urban areas (13, 14). The aim of the investigation was to estimate the prevalence and sociodemographic factors associated with seven risk factors of NCDs in adults from 2008 to 2019 in Sao Tome and Principe.
Methods
Secondary data from two cross-sectional STEPS surveys conducted in 2008 and 2019 in Sao Tome and Principe were analyzed, with a total response rate of 95.5% in 2008 and 91.5 percent in 2019 (15). Multi-step stratified sampling was conducted to select one person at random of the target age (25–64 years in 2008, and 18–69 years in 2019; the 2019 survey was restricted to 25–64 years for this analysis) per household (15).
SaoTome and Principe has a population of 228,000 in 2022 (16), a literacy rate of 92.8%, an urbanization rate of 76.4% (17), a gross domestic product (GDP) per capita in 2019 of $ 1961; the life expectancy (at birth) increased from 63.5 years in 2000 to 70.4 years in 2019 (18). The NCD programme in Sao Tome and Principe includes implementing the NCD programme and promotion of healthy lifestyles (19). Regarding integration of the NCD programme into primary health care (PHC) in Sao Tome and Principe, partial implementation includes having NCD guidelines, generally available medicine, generally available technologies, and drug therapy at PHC, and not implemented a national list of essential medicines and technology (20), and adhering to the WHO Package of Essential NCDs (PEN) interventions (21). Acccording to the WHO NCD monitor (22), there is poor implementation of NCD reduction measures, including unhealthy diet, tobacco demand and harmful use of alcohol, and public education and awareness campaigns on physical activity.
Study approval was provide by the Ministry of Health Ethical Committee, Sao Tome and Principe, and participants gave written informed consent (15). The data collection followed the WHO’s three STEPS methodology: the first step included the administration of questionnaires (social epidemiology, medical history, use of medicines and health risk behaviour); the second step involved body weight, height and blood pressure measurements; and the third step included biochemical tests (glucose and blood lipids) (23).
Assessments
Risk factors for NCDs were included on the basis of previous research (8, 10, 11, 24), as follows: Behavioural risk factors of NCD included current tobacco use, frequent alcohol use (≥5 days/week) (15), low physical activity defined by the “Global Physical Activity Questionnaire” (25), and IFVI (<5 servings/day); Biological risk factors for NCD: Diabetes: fasting plasma glucose ≥7.0 mmol/L, and/or presently medication for diabetes (26); Hypertension: measured blood pressure (BP) (average of two of last three measurements) defined as “systolic BP ≥140 mm Hg and/or diastolic BP ≥90 mm Hg” or presently on medication for hypertension (27); measured body mass index (overweight: 25.0–29.9 kg/m2 and obesity: ≥30.0 kg/m2) (26).
Social and demographic information consisted of sex, age, education, adult members in household and interview language (15).
Statistical analysis
The proportion of NCD risk factors was grouped on the basis of previous studies (13, 24), 3–7 NCD risk factors (compared to 0–2 risk factors). Chi-square tests were used to estimate differences in proportions. Logistic regressions were used to assess predictors of each of the seven NCD risk factors, adjusted by study year, proportion of adult members, education, sex, age, and interview language. Missing values (IFVI = 5.3%, low physical activity = 1.5%, current tobacco use = 0.1%, frequent alcohol use = 0%, overweight/obesity = 2.1%, hypertension = 2.0%, and diabetes = 7.1%) were discarded and p < 0.05 indicated significance. Statistical analyses were done with STATA software version 15.0 accounting for sample weighting and complex study design. The analysis weight was calculated by taking the reverse probability of each participant’s selection. These weights were adjusted to accommodate differences in the age-sex composition of the sample population compared to the target population. Different weight variables were calculated for (1) for interview data, (2) for physical measures, and (3) for biochemical measures (15).
Results
Sample characteristics
The sample included 2,457 adults, with a median age 37 years (IQR = 29–47) in 2008 and 1893 adults median age 38 years (IQR 32–48) in 2019. The proportion of younger adults increased, and higher education and number of adult household members decreased from 2008 to 2019 (see Table 1).
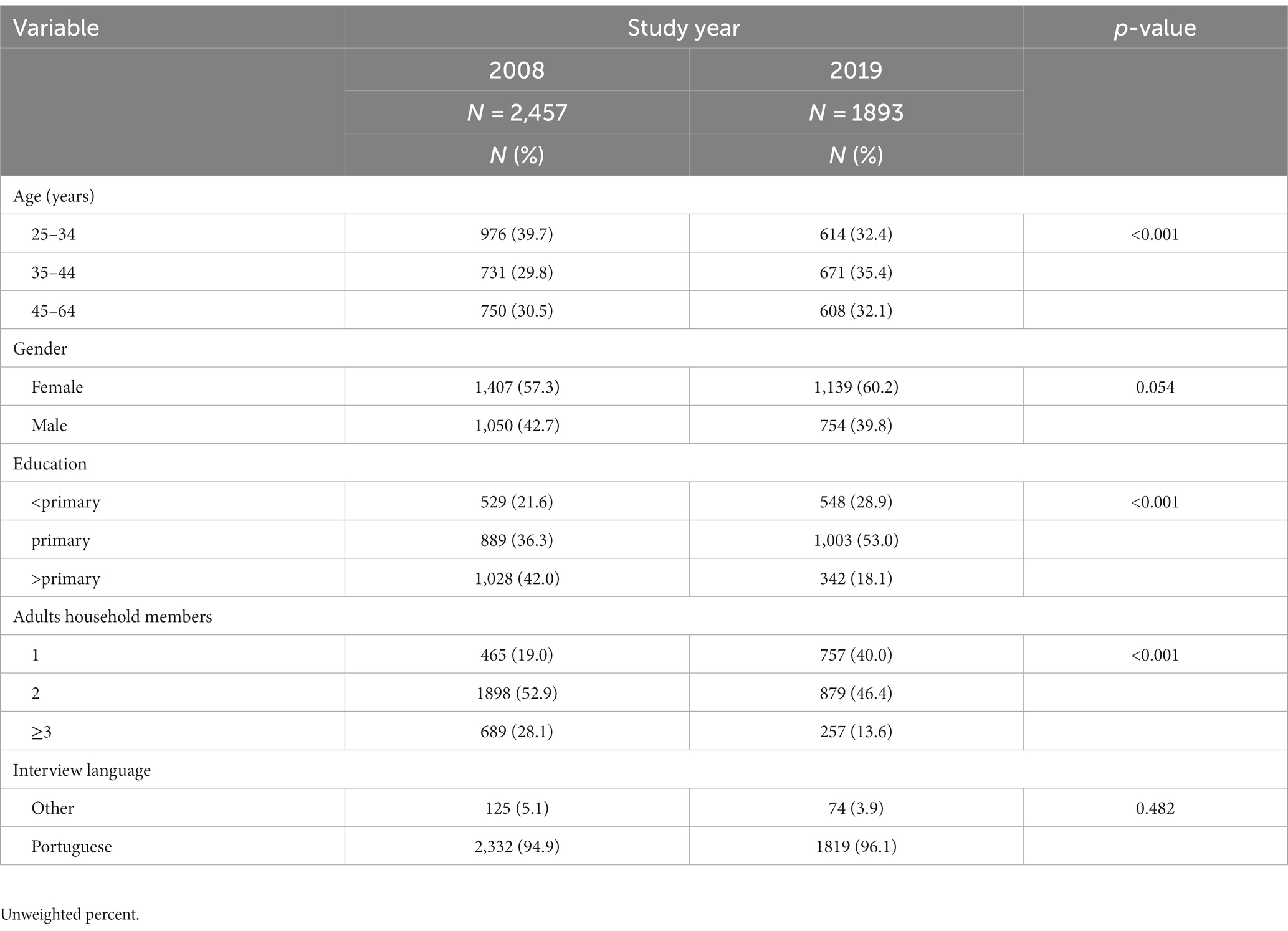
Table 1. Sociodemographic characteristics of individuals 25 to 64 years and older in Sao Tome and Principe 2008 and 2019.
Distribution of NCD risk factors from 2008 to 2019
The proportion of specific risk factors of NCD risk factors increased significantly for low physical activity from 17.4% in 2008 to 30.9% in 2019, and overweight/obesity from 37.3% in 2008 to 51.0% in 2019. There was a significant decrease in IFVI from 83.1% in 2008 to 53.3% in 2019, frequent alcohol use from 32.6% in 2008 to 24.8% in 2019, and diabetes from 3.1% in 2008 to 1.2% in 2019, while the prevalence of current tobacco use and hypertension remained unchanged from 2008 to 2019. Among men but not among women, current tobacco use and frequent alcohol use significantly decreased from 2008 to 2019, while among women but not among men diabetes significantly decreased. The overweight/obesity prevalence only increased significantly among women (from 43.3 to 58.1%) but not among men. Having 3–7 NCD risk factors decreased from 36.6% in 2008 to 31.7% in 2019, but this was only significant for men and not for women and overall (see Table 2).
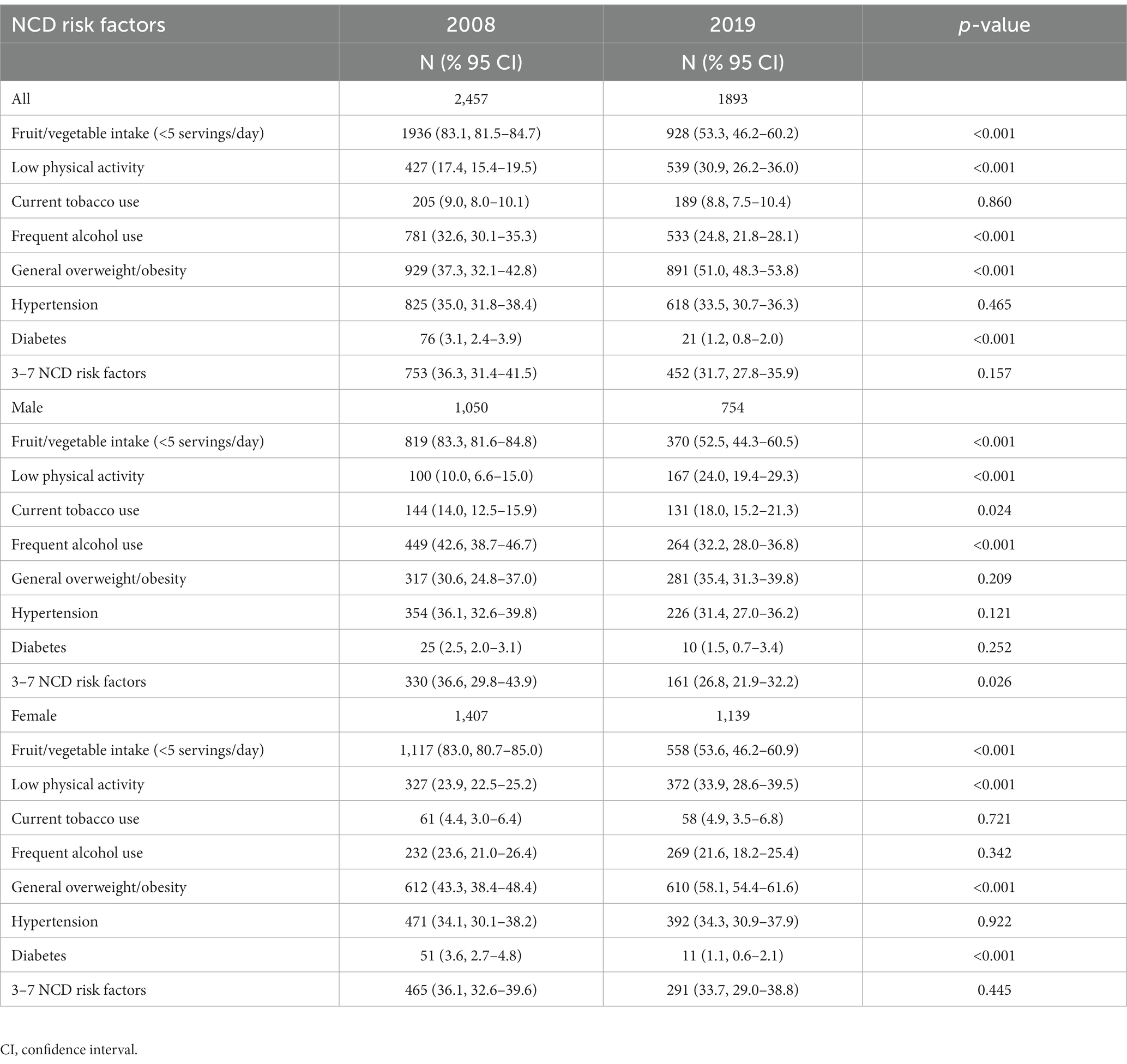
Table 2. Prevalence of risk factors for non-communicable diseases (NCDs) among adults in Sao Tome and Principe 2008 and 2019.
Social and demographic associations with individual behavioural risk factors for NCDs
Compared to participants in the 2008 study, participants in the 2019 study had a significantly higher prevalence of low physical activity, significantly lower IFVI and fewer frequent alcohol consumption. Older groups were more likely to use tobacco at present, and middle-aged participants were more likely to consume alcohol frequently. Men engaged more often than women in current tobacco use and frequent alcohol use, and women had higher rates of low physical activity and than men. Higher educational levels were negatively associated with IFVI, and frequent alcohol use. Having two or three or more adult household members (lower economic status) was negatively associated with low physical activity and IFVI. Portuguese interview language increased the odds of frequent alcohol use, low physical activity and IFVI (see Table 3).
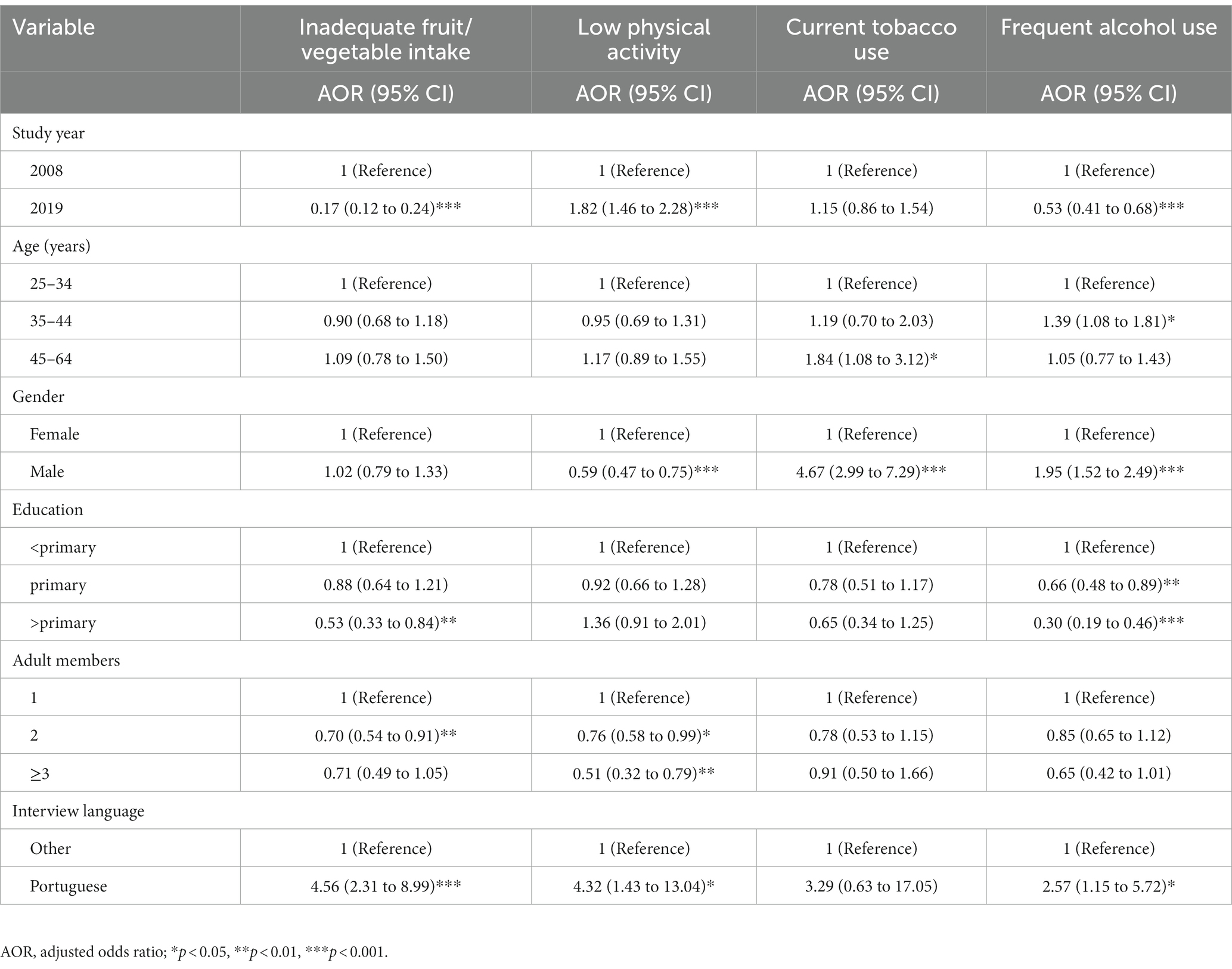
Table 3. Determinants of behavioural non-communicable disease risk factors in Sao Tome and Principe 2008 and 2019.
Sociodemographic determinants of individual biological NCD risk factors
Compared to 2008 participants, 2019 participants had a significantly higher prevalence of overweight/obesity and a lower prevalence of diabetes. Age was positively associated with obesity/obesity, hypertension and diabetes. Women had a higher rate of overweight/obesity than men. Higher educational levels and Portuguese interview language were associated with overweight/obesity. The number of adult households did not affect the prevalence of three biological risk factors for NCDs (see Table 4).
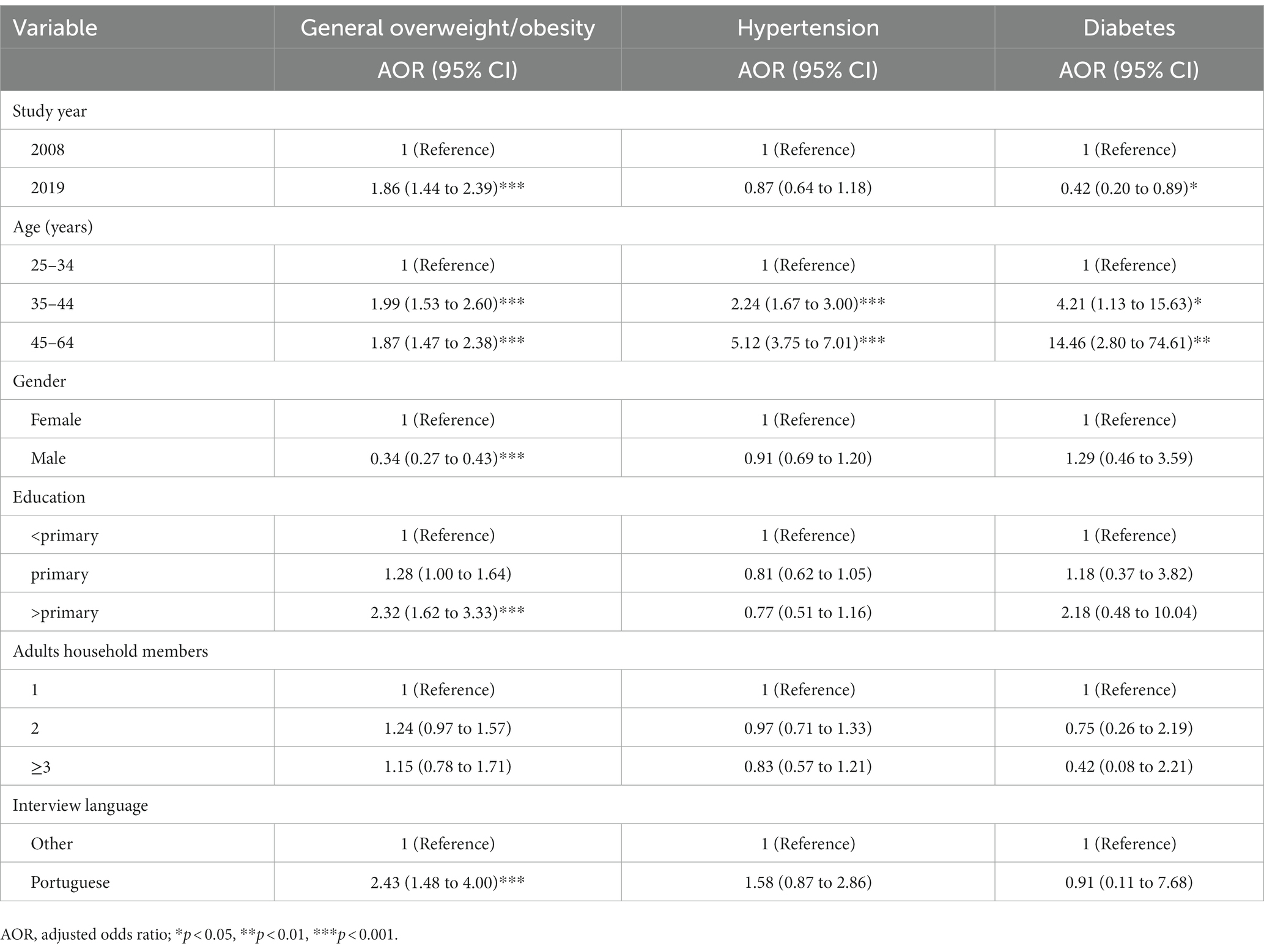
Table 4. Asociations with biological non-communicable disease risk factors in Sao Tome and Principe 2008 and 2019.
Discussion
The study showed that having 3–7 NCD risk factors among male but not female adults significantly decreased from 36.6% in 2008 to 26.8% in 2019 in Sao Tome and Principe. Some of this reduction may be attributed to strengthened implementation of NCD programme in Sao Tome and Principe (19). Having overweight/obesity and low physical activity significantly increased, and IFVI, frequent alcohol use, and diabetes significantly decreased from 2008 to 2019, while the prevalence of current tobacco use and hypertension remained unchanged from 2008 to 2019. According to the Global Nutrition Report (28), Sao Tome and Principe did not achieve their diet NCD targets, with still having high rates of obesity (19.7% in women and 8.9% in men). Similar to previous trend studies in India (29), Mongolia (30, 31) and Iran (32) having high body mass index and/or low physical activity increased over time. Although Sao Tome has implemented some national food and NCD policies, such as sugar-sweetened beverage tax and operational policy, strategy, or action plan to reduce unhealthy diet related to NCDs, additional implementation of some of the following are indicated food-based dietary guidelines, policy to eliminate industrially produced trans fatty acids, policy to reduce the impact of marketing of foods and beverages high in saturated fats, trans fatty acids, free sugars, or salt on children, and policy to limit saturated fatty acid intake (28). Regarding physical inactivity, the implementation of some of the following may help in increasing physical activity, including national physical activity communications campaigns, national mass participation events on physical activity, promotion of physical activity in different settings, brief intervention on physical activity in primary health care, quality physical education and national guidelines on physical activity in different age groups (16).
In this survey the prevalence of diabetes reduced over time, whereas in India (29), South Kivu, Democratic Republic of Congo (33), and Mozambique (34), the prevalence of diabetes increased over time. The unchanged current tobacco use in Sao Tome and Principe may be attributed to reduced compliance with the MPOWER tobacco control strategy, e.g., cigarettes have not become less affordable, no smokefree laws in public places, no tollfree telephone quit line, no smoking cessation support available in the community and health care setting, and no anti-tobacco mass media campaigns (35).
Furthermore, frequent alcohol use was significantly reduced from 2008 to 2019 in this study, while the recorded alcohol per capita (15+) consumption also reduced from 8.3 in litres of pure alcohol in both sexes in 2010 to 6.8 in 2016 (36). Compared to other African countries, having 3–7 risk factors for NCDs in this study (36.3% in 2008 and 31.7% in 2019) was higher than in Malawi (3–7 risk factors, 16.5%) (8) and Zambia (26.7%, 3–10 risk factors) (9). The prevalence of overweight/obesity in 2019 (51.0%) and the prevalence of diabetes (1.2%) in 2019 was similar or lower than in another island country in Africa in Comoros (50.8% overweight/obesity and 8.5% diabetes) (6, 7), but in terms of overweight/obesity higher than in Malawi (26.5%) (8) and Zambia (24.4%) (9). The prevalence of hypertension (33.5% in 2019) was similar to Malawi (32.9%) (8) but higher than in Zambia (18.9%) (9), the prevalence of current tobacco use (8.8% in 2019) was lower than in Malawi (14.1% current smokers) (8), and in Zambia (10.7% daily tobacco use) (9), and the rate of IFVI (53.3% in 2019) was lower than in Zambia (90.4%) (9).
There was a male preponderance of current tobacco use and frequent alcohol use and a female preponderance of general overweight/obesity and low physical activity, and there were no sex differences in hypertension, diabetes and IFVI. In previous studies (11, 24), the prevalence of substance use in men was higher than in women, and the rate of obesity/obesity in women was higher than in men. As expected (10–13), older age increased the odds of overweight/obesity, hypertension, diabetes, and current tobacco use and middle age was associated with frequent alcohol use. Lower education was associated with IFVI as well as with frequent use of alcohol and inversely associated with overweight/obesity. Portuguese interview language increased the odds of IFVI, low physical activity, frequent alcohol use and overweight/obesity. These findings show that the seven specific risk factors for NCDs can be targeted differently according to gender, age, level of education and interview language.
Comprehensive interventions can be directed to promote the control of body weight, the cessation of smoking, healthy diet, and the examination and control of high levels of sugar and blood pressure.
Study strength and limitations
The STEPS surveys in Sao Tome and Principe utilized nationally representative data and standardised assessment tools. The two surveys conducted were cross-sectional, thus hindering causative conclusions. Some variables, such as substance use, were assessed by self-report, which may have biased responses. The Sao Tome and Principe 2008 STEPS survey did not measure heavy drinking, other alcohol measures, household income and residence status, which could therefore not be included in the analysis. The total cholesterol variable was excluded from the analysis because of implausible values in 2019 (77.8% had elevated total cholesterol).
Conclusion
Based on two national household surveys in adults from 2008 to 2019 in Sao Tome and Principe, we found that the prevalence of seven risk factors of NCD decreased among men but not women from 2008 to 2019. Overweight/obesity, and low physical activity increased, and IFVI, frequent alcohol use, and diabetes decreased, and hypertension and current tobacco use stayed the same. Several factors associated with the risk factors of NCD have been identified, including age, gender, level of education and interview language that can guide interventions.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: World Health Organization NCD Microdata Repository at https://extranet.who.int/ncdsmicrodata/index.php/catalog/893.
Ethics statement
The studies involving humans were approved by Ministry of Health Ethical Committee, Sao Tome and Principe. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SP and KP fulfil the criteria for authorship, conceived and designed the research, performed statistical analysis, drafted the manuscript, and made critical revisions of the manuscript for key intellectual content. All authors contributed to the article and approved the submitted version.
Acknowledgments
This paper uses data from the Sao Tome and Principe 2008 and 2019 STEPS survey, implemented by the Ministry of Health with the support of the World Health Organization.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization (WHO). (2018). Noncommunicable diseases. Available at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (Accessed Aug 2, 2021).
2. World Health Organization (WHO). (2018). Sao Tome and Principe: Noncommunicable Diseases (NCD) Country Profiles. Available at: (Accessed April 2, 2023)https://cdn.who.int/media/docs/default-source/country-profiles/ncds/stp_en.pdf?sfvrsn=2316b45b_38&download=true.
3. Marquez, PV, and Farrington, JL. The challenge of non-communicable diseases and road traffic injuries in sub-Saharan Africa. An overview. Washington, DC.: The World Bank (2013).
4. Ministério da Saúde. Plano Nacional do Desenvolvimento da Saúde 2017–2021. (2017). Available at: (https://saotomeandprincipe.unfpa.org/sites/default/files/pub-pdf/pnds-2017-2021-actualizado.pdf).
5. Nyirenda, MJ. Non-communicable diseases in sub-Saharan Africa: understanding the drivers of the epidemic to inform intervention strategies. Int Health. (2016) 8:157–8. doi: 10.1093/inthealth/ihw021,
6. Ali, RAB, Hannoun, Z, Harraqui, K, Zeghari, L, Aboussaleh, Y, Mohamed, S, et al. Profile of diabetes and cardiovascular risk factors in adults Anjouan Island (Comoros). Pan Afr Med J. (2019) 33:140. doi: 10.11604/pamj.2019.33.140.19016
7. Ali, RAB, Harraqui, K, Hannoun, Z, Monir, M, Samir, M, Anssoufouddine, M, et al. Transition nutritionnelle, prévalence de la double charge de la malnutrition et facteurs de risque cardiovasculaires chez les adultes de l'île comorienne d'Anjouan [Nutrition transition, prevalence of double burden of malnutrition and cardiovascular risk factors in the adult population living in the island of Anjouan, Comoros]. Pan Afr Med J. (2020) 35:89. doi: 10.11604/pamj.2020.35.89.19043
8. Msyamboza, KP, Ngwira, B, Dzowela, T, Mvula, C, Kathyola, D, Harries, AD, et al. The burden of selected chronic non-communicable diseases and their risk factors in Malawi: nationwide STEPS survey. PLoS One. (2011) 6:e20316. doi: 10.1371/journal.pone.0020316
9. Pengpid, S, and Peltzer, K. Prevalence and correlates of multiple non-communicable disease risk factors among adults in Zambia: results of the first national STEPS survey in 2017. Pan Afr Med J. (2020) 37:265. doi: 10.11604/pamj.2020.37.265.25038
10. Aryal, KK, Mehata, S, Neupane, S, Vaidya, A, Dhimal, M, Dhakal, P, et al. The burden and determinants of non communicable diseases risk factors in Nepal: findings from a Nationwide STEPS survey. PLoS One. (2015) 10:e0134834. doi: 10.1371/journal.pone.0134834
11. Wekesah, FM, Nyanjau, L, Kibachio, J, Mutua, MK, Mohamed, SF, Grobbee, DE, et al. Individual and household level factors associated with presence of multiple non-communicable disease risk factors in Kenyan adults. BMC Public Health. (2018) 18:1220. doi: 10.1186/s12889-018-6055-8
12. Rafique, I, Saqib, MAN, Munir, MA, Qureshi, H, Rizwanullah, KS, Khan, SA, et al. Prevalence of risk factors for noncommunicable diseases in adults: key findings from the Pakistan STEPS survey. East Mediterr Health J. (2018) 24:33–41. doi: 10.26719/2018.24.1.33
13. Pelzom, D, Isaakidis, P, Oo, MM, Gurung, MS, and Yangchen, P. Alarming prevalence and clustering of modifiable noncommunicable disease risk factors among adults in Bhutan: a nationwide cross-sectional community survey. BMC Public Health. (2017) 17:975. doi: 10.1186/s12889-017-4989-x
14. Zaman, MM, Bhuiyan, MR, Karim, MN, Zaman, M, Rahman, MM, Akanda, AW, et al. Clustering of non-communicable diseases risk factors in Bangladeshi adults: an analysis of STEPS survey 2013. BMC Public Health. (2015) 15:659. doi: 10.1186/s12889-015-1938-4
15. World Health Organization. Sao Tome and Principe, 2008 and 2019. Available at: https://extranet.who.int/ncdsmicrodata/index.php/catalog/735; https://extranet.who.int/ncdsmicrodata/index.php/catalog/893 (Accessed May 3, 2023).
16. World Health Organization. Physical activity Sao Tome and Principe 2022 country profile. (2022). Available at: https://cdn.who.int/media/docs/default-source/country-profiles/physical-activity/physical-activity-stp-2022-country-profile.pdf?sfvrsn=5ad7829f_5&download=true República Democrática de São Tomé e Príncipe (Accessed July 2, 2023).
17. World Factbook. Sao Tome and Principe. (2023). Available at: (https://www.cia.gov/the-world-factbook/countries/sao-tome-and-principe/).
18. World Health Organization. (2023). Sao Tome and Principe, health data overview for the Democratic Republic of Sao Tome and Principe. Available at: https://data.who.int/countries/678 (Accessed July 2, 2023).
19. World Health Organization. (2015). Sao Tome and Principe, country corporation strategy. Available at: (Accessed April 2, 2023)https://apps.who.int/iris/bitstream/handle/10665/246244/ccsbrief_stp_en.pdf.
20. Tesema, AG, Ajisegiri, WS, Abimbola, S, Balane, C, Kengne, AP, Shiferaw, F, et al. How well are non-communicable disease services being integrated into primary health care in Africa: a review of progress against World Health Organization's African regional targets. PLoS One. (2020) 15:e0240984. doi: 10.1371/journal.pone.0240984
21. World Health Organization, Sao Tome and Principe. (2021). The World Health Organization supports São Tomé and Príncipe in validating the protocols for the prevention and management of cases of noncommunicable diseases (NCDs) in primary health care. Available at: https://www.afro.who.int/pt/news/organizacao-mundial-da-saude-apoia-sao-tome-e-principe-validar-os-protocolos-de-prevencao-e (Accessed July 2, 2023).
22. World Health Organization. Noncommunicable Diseases Progress Monitor 2022, Sao Tome and Principe. (2022). Available at: (https://www.who.int/publications/i/item/9789240047761).
23. World Health Organization (WHO). (2018). STEPwise approach to surveillance (STEPS). Available at: (https://www.who.int/ncds/surveillance/steps/en/).
24. Wesonga, R, Guwatudde, D, Bahendeka, SK, Mutungi, G, Nabugoomu, F, and Muwonge, J. Burden of cumulative risk factors associated with non-communicable diseases among adults in Uganda: evidence from a national baseline survey. Int J Equity Health. (2016) 15:195. doi: 10.1186/s12939-016-0486-6
25. Armstrong, T, and Bull, F. Development of the World Health Organization global physical activity questionnaire (GPAQ). J Public Health. (2006) 14:66–70. doi: 10.1007/s10389-006-0024-x
26. World Health Organization (WHO) WHO STEPS surveillance manual. (2027). Available at: https://www.who.int/docs/default-source/ncds/ncd-surveillance/steps/steps-manual.pdf?sfvrsn=c281673d_5 (Accessed April 22, 2022).
27. Chobanian, AV, Bakris, GL, Black, HR, Cushman, WC, Green, LA, Izzo, JL, et al. Seventh report of the joint National Committee of prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. (2003) 42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2
28. Global nutrition report. (2022). Country report: Sao Tome and Principe. The burden of malnutrition at a glance. Available at: https://globalnutritionreport.org/resources/nutrition-profiles/africa/middle-africa/sao-tome-and-principe/ (Accessed April 2, 2023).
29. Prabhakaran, D, Roy, A, Praveen, PA, Ramakrishnan, L, Gupta, R, Amarchand, R, et al. 20-year trend of CVD risk factors: urban and rural National Capital Region of India. Glob Heart. (2017) 12:209–17. doi: 10.1016/j.gheart.2016.11.004
30. Dashzeveg, D, Nakamura, K, Seino, K, Al-Sobaihi, S, and Palam, E. Changes in the configuration and patterns of physical activity among Mongolian adults, 2005–2013. J Rural Med. (2018) 13:151–9. doi: 10.2185/jrm.2977
31. Chimeddamba, O, Gearon, E, Brilleman, SL, Tumenjargal, E, and Peeters, A. Increases in waist circumference independent of weight in Mongolia over the last decade: the Mongolian STEPS surveys. BMC Obes. (2017) 4:19. doi: 10.1186/s40608-017-0155-3
32. Ghelichkhani, P, Baikpour, M, Mohammad, K, Rahim Fattah, FH, Rezaei, N, Ahmadi, N, et al. Age, Period and cohort analysis of smoking prevalence in Iranian population over a 25-year period. Arch Iran Med. (2021) 24:7–14. doi: 10.34172/aim.2021.02
33. Katchunga, PB, Mirindi, P, Baleke, A, Ntaburhe, T, Twagirumukiza, M, and M'buyamba-Kabangu, JR. The trend in blood pressure and hypertension prevalence in the general population of south Kivu between 2012 and 2016: results from two representative cross-sectional surveys-the Bukavu observational study. PLoS One. (2019) 14:e0219377. doi: 10.1371/journal.pone.0219377
34. Jessen, N, Damasceno, A, Silva-Matos, C, Tuzine, E, Madede, T, Mahoque, R, et al. Hypertension in Mozambique: trends between 2005 and 2015. J Hypertens. (2018) 36:779–84. doi: 10.1097/HJH.0000000000001618
35. World Health Organization. (2021). WHO report on the global tobacco epidemic, Country profile Sao Tome and Principe. Available at: (https://cdn.who.int/media/docs/default-source/country-profiles/tobacco/who_rgte_2021_sao_tome_and_principe.pdf?sfvrsn=37a7f1e9_5&download=true).
36. World Health Organization. Alcohol Sao Tome and Principe 2019 Country profile. (2019). Available at: (https://www.who.int/publications/m/item/alcohol-stp-2019).
Keywords: noncommunicable disease, risk factors, trends, Sao Tome and Principe, STEPS survey
Citation: Pengpid S and Peltzer K (2023) Trends in bio-behavioural risk factors of non-communicable diseases among adults in Sao Tome and Principe. Front. Public Health. 11:1238348. doi: 10.3389/fpubh.2023.1238348
Edited by:
Anand Krishnan, All India Institute of Medical Sciences, IndiaReviewed by:
Ahmed Mohammed Alwan, Mashhad University of Medical Sciences, IranDimple Kondal, Centre for Chronic Disease Control, India
Sitanshu Sekhar Kar, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), India
Copyright © 2023 Pengpid and Peltzer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karl Peltzer, kfpeltzer@gmail.com
 Supa Pengpid
Supa Pengpid Karl Peltzer
Karl Peltzer