- 1Institute of Education, Xiamen University, Xiamen, China
- 2School of Psychology, Centre for Studies of Psychological Applications, Guangdong Key Laboratory of Mental Health and Cognitive Science, Ministry of Education Key Laboratory of Brain Cognition and Educational Science, South China Normal University, Guangzhou, China
Aims: This study aimed to examine the subtype classification characteristics of sleep disturbance (SD) in college students and their associations with sample characteristic factors and mental health outcomes.
Methods: The sample comprised 4,302 college students (Mean age = 19.92 ± 1.42 years, 58.6% females). The Youth Self-Rating Insomnia Scale, Beck Depression Inventory, 8-item Positive Subscale of the Community Assessment of Psychic Experiences, and 10-item Connor-Davidson Resilience Scale were used to assess adolescents’ sleep disturbance, depressive symptoms, psychotic-like experiences (PLEs), and resilience. Latent profile analysis, logistic regression, and liner regression analysis were used to analyze the data.
Results: Three subtypes of SD in college students were identified: the high SD profile (10.6%), the mild SD profile (37.5%), and the no SD profile (51.9%). Compared with college students in the “no SD” profile, risk factors for “high SD” include being male and poor parental marital status. Sophomores were found to predict the “high SD” profile or “mild SD” profile relative to the “no SD” profile. College students in the “mild SD” profile or “high SD” profile were more likely to have a higher level of depressive symptoms and PLEs, while a lower level of resilience.
Conclusion: The findings highlighted that target intervention is urgently needed for male college students, sophomores, and those with poor parental marital status in the “mild SD” profile or “high SD” profile.
Introduction
Sleep disturbance (SD) is prevalent among adolescents and young adults, with main symptoms of insomnia, poor sleep quality, and other sleep complaints. College students, one of the most sleep deprived student groups, are particularly vulnerable to disturbed sleep. One epidemiological survey showed that more than 60% of college students were suffering from SD [on the Pittsburgh Sleep Quality Index (PSQI)] (1). Gaultney, in a sample of 1845 college students, found that 27% have clinically significant symptoms of SD (on the SLEEP-50 questionnaire) (2). Recent systematic review, involving 250 studies, estimated that global prevalence of SD among college students was 41.16% during the COVID-19 pandemic (3). Adolescents entering college is a major life transition, which means leaving home and living independently, completing demanding course and trying to earn academic degrees, facing a new social environment, and adopting new social roles (4–6). This transition contributes to increased stress levels, which, in turn, can have a profound and lasting effect on sleep (7). Moreover, studies have also shown that excessive media use by college students contributes to poor sleep hygiene and a series of sleep disturbances (8).
A growing number of research have focused on SD of college students and its symptoms, such as insomnia (difficulty initiating sleep, difficulty maintaining sleep, or early morning awakening) (9), poor subjective sleep quality (10, 11), daytime sleepiness (12), salient nightmares (13), and other general sleep problems (14). The majority of extant research on SD has relied on variable-centered analyses, which provides insight into the average relations among symptoms or diagnoses of SD within a specific group. However, the methodological approaches fail to reveal different patterns between individuals and may therefore draw over-generalized conclusions based on overall samples (15). On the contrary, the use of person-centered approaches such as latent class analysis (LCA) and latent profile analysis (LPA), to evaluate the structure of psychopathology, enables a more refined understanding of symptom presentations and is ideal for psychopathology research (16, 17).
Till now, the heterogeneity of SD for college students has only been scarcely explored. Based on the available literature, only three studies have been conducted using a person-centered methodological approach to explore the heterogeneous patterns of sleep-related impairment among college students. For instance, Carpi et al. (18) identified a five-class solution among a small sample of college students (N = 490) by using LPA, which were termed as the “severe insomnia” subtype, “moderate insomnia with medication use” subtype, “subthreshold insomnia” subtype, “subthreshold insomnia with sleep latency complaints” subtype, and “moderate insomnia with sleep duration complaints” subtype (18). Zhou et al. (19) applied LCA to discern heterogeneous patterns of sleep behaviors among 1,288 Chinese college students, and summarized four subtypes: good sleep, prolonged sleep latency, sleep disturbances–daytime dysfunction, and multiple poor sleep behavior (19). Another study in 312 at-risk college drinkers also indicted that the four profiles can clearly explain sleep and sleep-related consequences (20). Therefore, further studies with a large sample are needed to confirm heterogeneous patterns of SD among general college students.
This study intended to explore the heterogeneity of SD among the college students group with a large sample web-based survey for college students. As suggested by prior research, the risks of occurrence and persistence of SD are associated with numerous sample characteristic factors, including age (21, 22), sex (23, 24), parental marital status (25), and family economic status (26). Additionally, solid evidence showed that SD is also associated with a wide variety of adverse mental health outcomes, such as depression (27) and psychotic-like experiences (PLEs) (28), as well as inhibits the development of positive mental qualities, such as resilience (29). Collectively, there are three main aims of this study. First, the study aims to identify the heterogeneity differences in SD among college students, employing LPA. Second, it explores what sample characteristic factors (e.g., sex, age) are significant predictors of distinct profiles of SD in college students. Finally, it examines the associations among these different subtypes of SD and mental health outcomes. Based on previous research, we speculated that the college students’ SD feature obvious latent profiles, and several sample characteristic factors, such as sex, parental marital status, were significant predictors of distinct profiles for SD. We also anticipated that there are robust associations between SD subtypes and depression, PLEs and resilience.
Materials and methods
Participants and procedure
A convenience sample of college students was recruited from Taiyuan city in Shanxi Province, China. The online survey was conducted during January 2021, using the “Questionnaire Star” software platform. All participants scanned the Quick Response (QR) code of the questionnaire through their mobile phones to complete the web-based survey. If respondents agree to participate in this study, they shall select the “I agree to participate” option and upload their electronic signature of informed consent on the first page of the questionnaire platform. The investigation used the principle of voluntary participation, and participants could withdraw from the survey at any time if they felt discomfort. To improve data quality, inclusion criteria for participation included: (a) upload the electronic signed version of the informed consent form; (b) response time for web-based survey was above 5 min; and (c) have no current significant physical disease or history of psychiatric illness. Finally, 4,302 responses were qualified and included in the subsequent analyses.
The current study was carried out in accordance with the Helsinki Declaration as revised in 1989 and was approved by the Ethics Committees of South China Normal University.
Measures
SD
The Chinese version of Youth Self-Rating Insomnia Scale (YSIS) was used to measure the SD in the past month (30). It consists of 8 items, clustering into two dimensions, namely daytime distress/impairment and insomnia symptoms. Each item scored from 1 to 5, and a higher total score indicate a greater level of SD. The cut-off point of 26 represents identified cases of clinically SD (30). In this study, Cronbach’s α was 0.89.
Depressive symptoms
The Beck Depression Inventory (BDI) was used to assess depressive symptoms in the past week (31). It consists of 21 items, and each item was rated on a four-point Likert scale, from 0 to 3, and a higher total score suggested a greater level of depressive symptoms. A cut-off score of 14 was suggested to identify the clinically significant depression (32).The Chinese version of BDI-21 has demonstrated good internal reliability and the concurrent validity (33), and Cronbach’s α was 0.91 in this sample.
PLEs
The Chinese version of 8-item positive subscale of the community assessment of psychic experiences (CAPE-P8) was used to evaluate frequency of PLEs in the past month (34, 35). CAPE-P8 originated from 42-item community assessment of psychic experiences (36, 37), which addresses the following domains, namely delusional experiences and hallucinatory experiences. Responses to items range from 1—never, 2—sometimes, 3—often, to 4—nearly always, with a higher score reflecting more frequent PLEs. Frequent PLEs were defined as having “often” or “nearly always” on one or more items (38, 39), and Cronbach’s α was 0.84 in the current sample.
Resilience
The 10-item Connor-Davidson Resilience Scale (CD-RISC-10) was used to assess the level of resilience (40). Five response options are available on a scale of 0 (not true at all) to 4 (true nearly all the time). Higher score means higher level of resilience. Psychometric properties of the CD-RISC-10 have been described in the Chinese population (41, 42). In our study, Cronbach’s α was rather high (α = 0.97).
Sample characteristic variables
Sample characteristic variables were collected in a self-report fashion, including sex [1 = male; 2 = female], age, grade [1 = freshman; 2 = sophomore; 3 = junior; 4 = senior], ethnicity [1 = Han (the major ethnic group in China); 2 = others], parental married status [1 = good; 2 = poor (separated, divorced, and widowed)], family income [1 = <3,000 RMB; 2 = 3,000 ~ 5,000 RMB; 3= >5,000 RMB], parents’ education level [1 = junior high school or less; 2 = senior high school; 3 = college or more], and single child status [1 = yes; 2 = no].
Statistical analysis
Data analysis was performed using SPSS 24.0 and Mplus 8.30. First, the Harman’s one-factor test through exploratory factor analysis (EFA) was performed to examine common method bias (43). The EFA found out that there were 5 factors with eigenvalues >1 and the first factor accounted for 11.17% of the total variance, indicating common method bias was not a serious issue in the study (44). Second, the LPA was conducted to determine whether there were heterogeneous latent classification differences in SD among college students. LPA is a form of LCA that is used when working with continuous variables. The fit of a one-class model is initially evaluated, and models with increasing number of latent profiles were estimated. To identify the optimal number of latent profiles to fit the data, we compared several fit indicates of each model, including Akaike’s information criterion (AIC), the Bayesian information criterion (BIC), sample-size-adjusted Bayesian information criterion (aBIC), Entropy, Vuong-Lo–Mendell–Rubin Likelihood Ratio Test (VLMR-LRT), and bootstrapped likelihood ratio test (BLRT). Lower AIC, BIC, and aBIC values (45), higher entropy values (46), and significant VLMR-LRT and BLRT p-values (47) were considered as signs of a better fit. In addition, we took interpretability of the profiles into great consideration, and ensured that each profile consisted of no less than 5% of samples (48). Third, multivariate logistic regression analyses were implemented to test whether sample characteristic variables differentially predicted SD profile membership. Finally, YSIS, BDI-21, CAPE-P8, and CD-RISC-10 total scores were compared through the ANOVA test. We also treated the subtypes of SD as dummy variables and further examined the relationship between SD subtypes and depression, PLEs and resilience using linear regression. A two-tailed p < 0.05 was considered statistically significant.
Results
Description of the sample
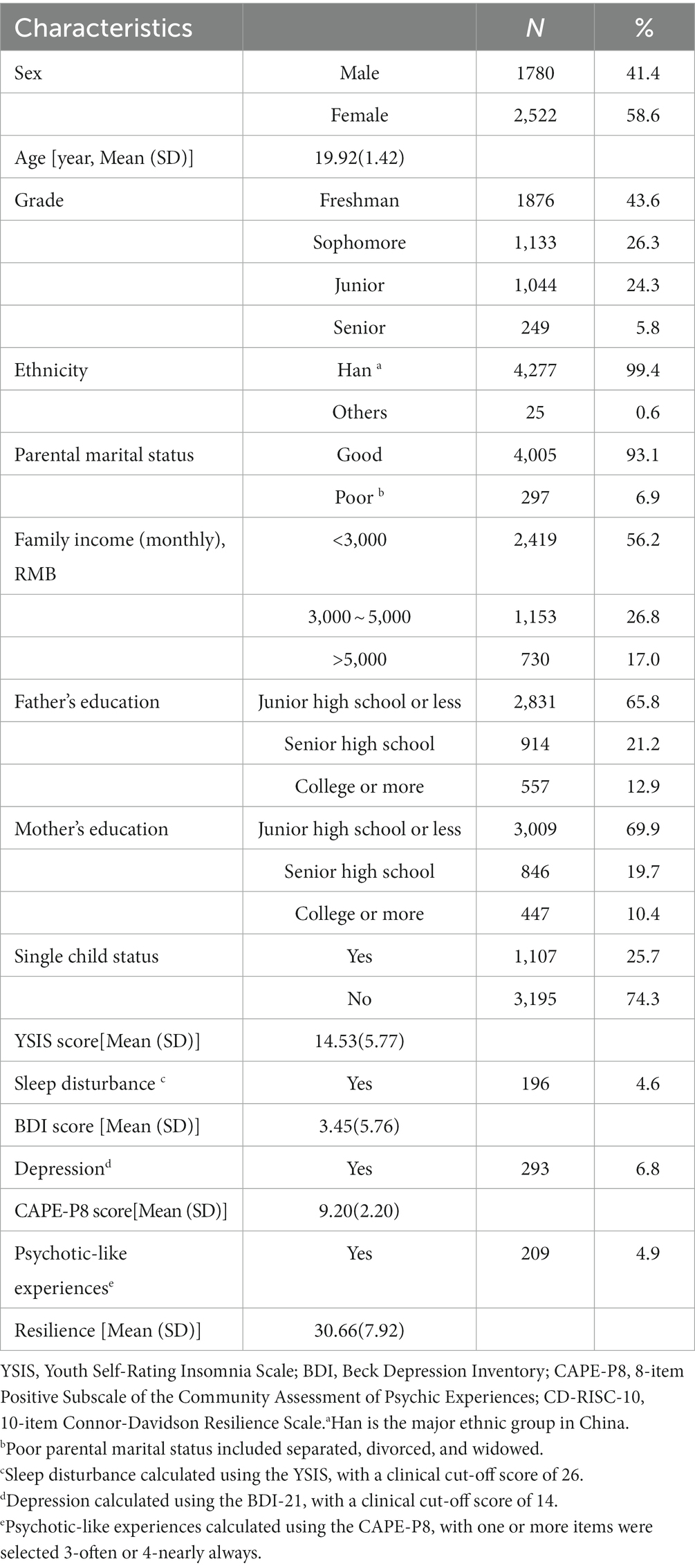
In total, 4,302 participants completed questionnaires, among which 2,522 were female. The mean age of the sample was 19.92 ± 1.42 years. A majority of college students was ethnicity Han (99.4%), and reported with a good parental marital status (93.1%). Other sample characteristic variables are presented in Table 1.
Table 1 also displays 4.6% of participants (N = 196) reported the presence of clinically SD. 6.8% (N = 293) had depression, and 4.9% (N = 209) respondents were identified as frequents PLEs.
Model fitting
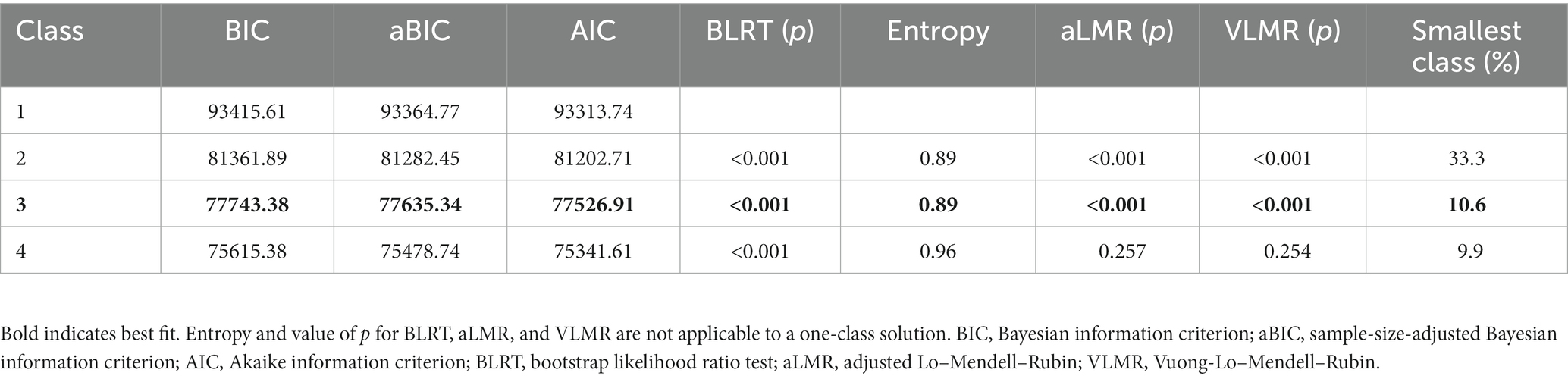
Based on the 8 items of the YSIS, a potential profile analysis was conducted, which, in turn, established four latent profile models. The results of the LPA are reported in Table 2. The VLMR-LRT and BLRT values were statistically significant for two and three-category model. Moreover, the fit of the three-category model was better than a two-category model, as indicated by the lower AIC and BIC values. Also, Entropy value for three-category model was 0.89, indicating a high accuracy of these classifications. Therefore, the three-category model was selected as the optimal model. The average probability of samples belonging to each potential category was between 92.2 and 96.8%.
Sleep disturbance profiles characterization
A latent class profile plot of the sample is shown in Figure 1. Profile 1 labeled as the “high SD” profile (N = 456, accounting for 10.6% of the total sample) was characterized by the highest level of SD, and its YSIS total score (26.12 ± 3.53) > 26 (the cut-off point). Profile 3 defined as the “no SD” profile (N = 2,234, 51.9%) was characterized by the lowest level of SD, and its YSIS total score (10.05 ± 1.95) much lower than the sample mean value (14.53 ± 5.77). Additionally, profile 2 comprised approximately 37.5% of the sample (N = 1,612) and included college students with a higher level of SD compared to the sample reported in profile 3, while lower than those belonging to profile 1. The YSIS total score of this profile (17.45 ± 2.37) slightly above the sample mean value (14.53 ± 5.77). This profile was named as “mild SD” profile.
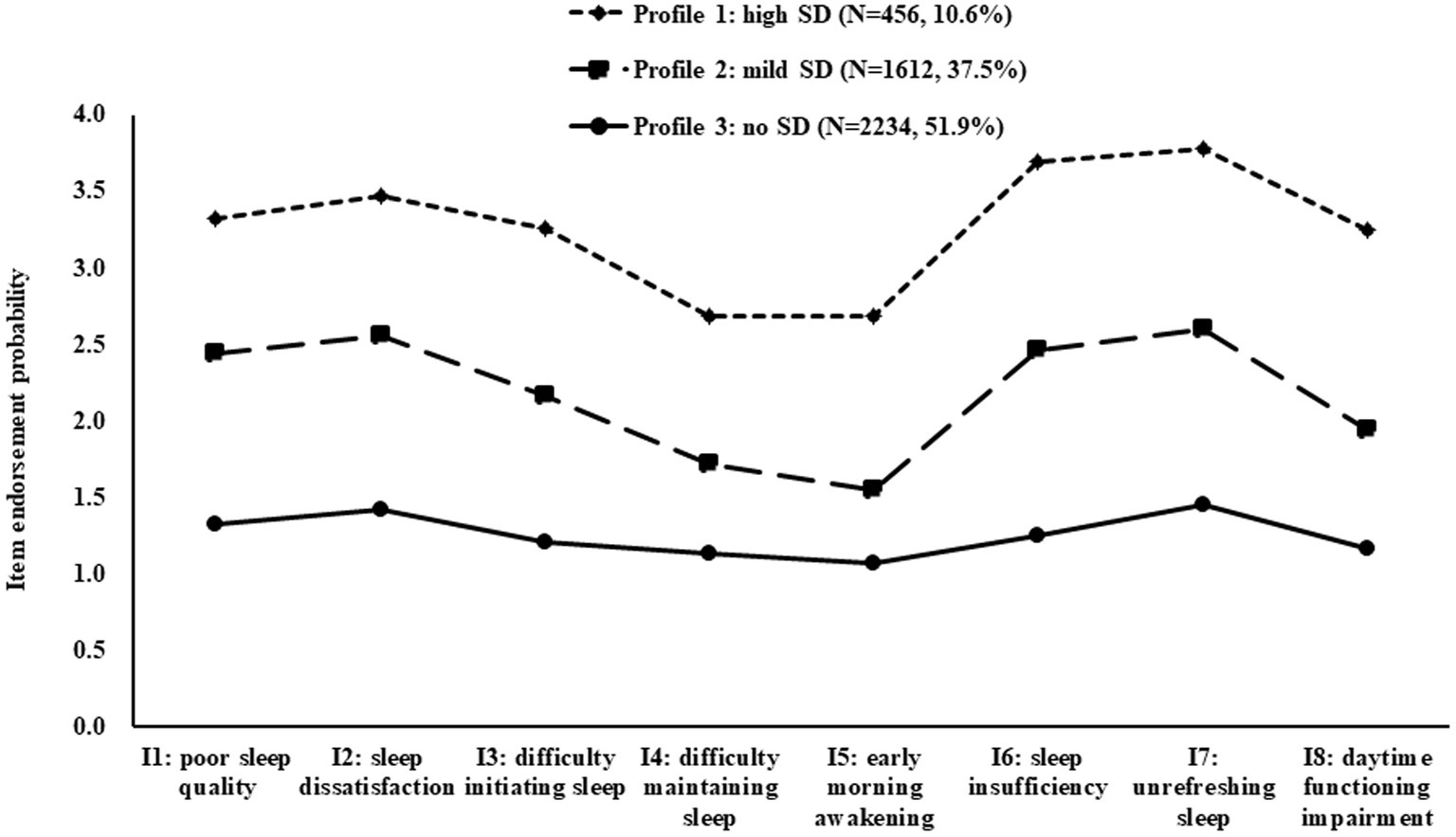
Figure 1. Mean sleep disturbance symptom cluster scores in the three latent profiles. SD, sleep disturbance.
Profile predictors and outcomes
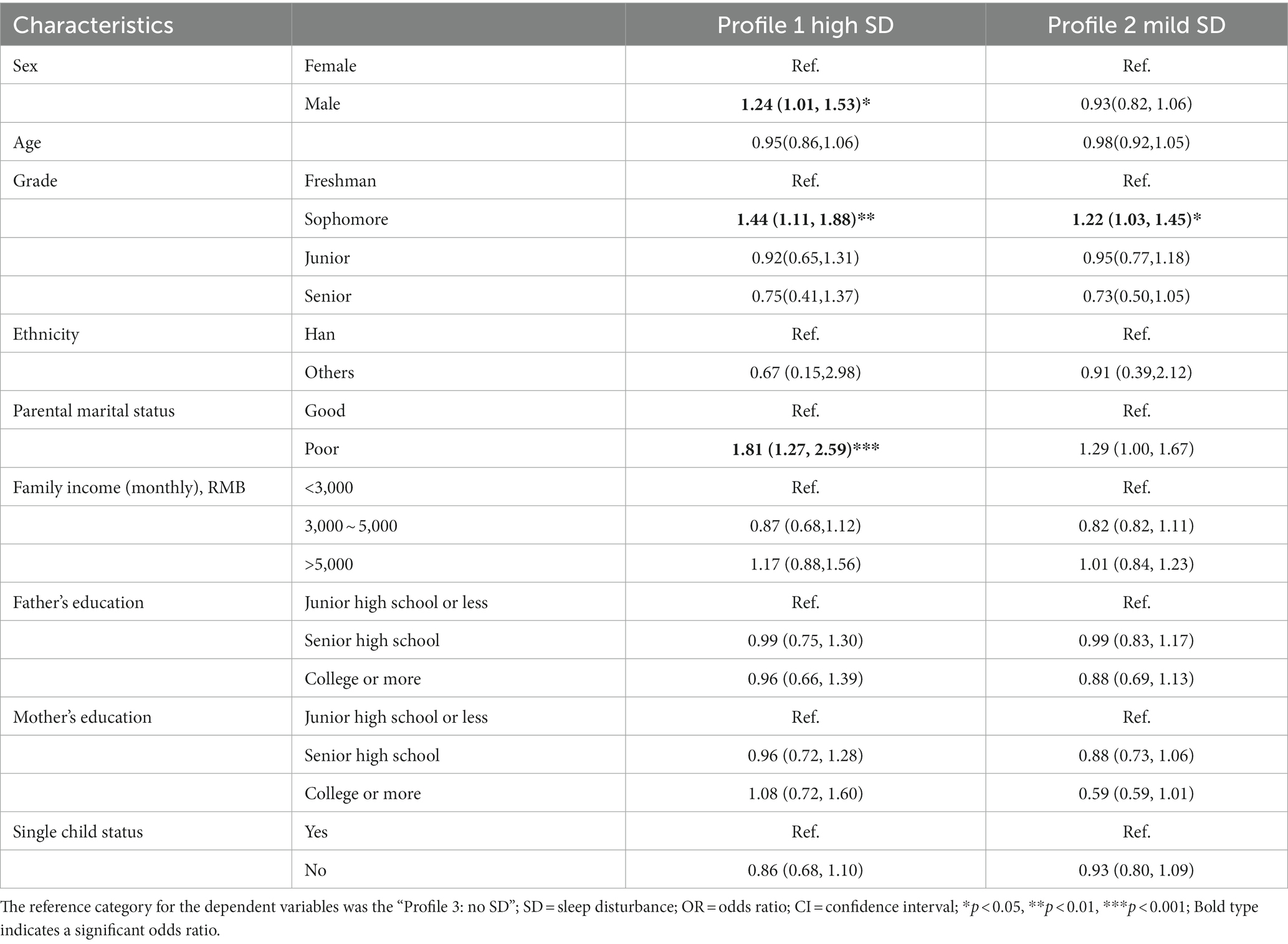
Taking the profile of SD as the dependent variable, the “no SD” profile was used as the reference category. Sex, age, grade, ethnicity, parental married status, family income, parents’ education level, and single child status were used as independent variables to carry out a multivariate logistic regression. The results (Table 3) showed that, compared with college students in the “no SD” profile, risk factors for “high SD” include being male (OR = 1.24, 95% CI = 1.01–1.53) and poor parental marital status (OR = 1.81, 95% CI = 1.27–2.59). Meanwhile, sophomores tended to predict the “high SD” profile (OR = 1.44, 95% CI = 1.11–1.88) or “mild SD” profile (OR = 1.22, 95% CI = 1.03–1.45) relative to the “no SD” profile.
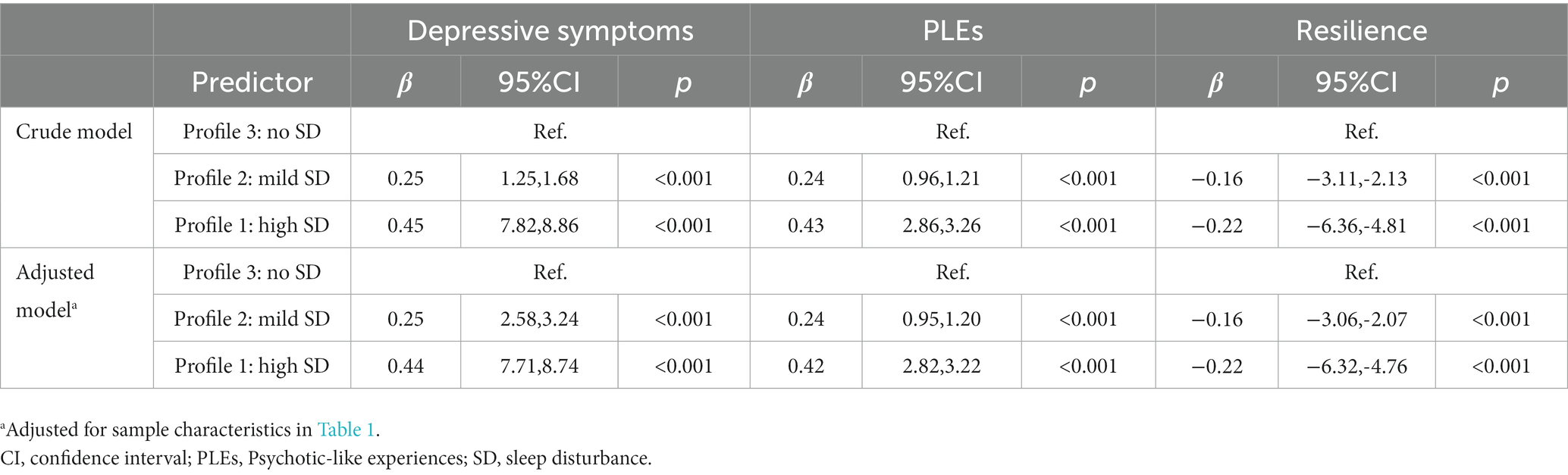
Figure 2 compares YSIS, BDI-21, CAPE-P8, and CD-RISC-10 total scores among the three profile of SD. The “high SD” profile had higher YSIS (F = 11119.46, p < 0.001, Figure 2A), BDI-21 (F = 541.26, p < 0.001, Figure 2B), and CAPE-P8 scores (F = 491.81, p < 0.001, Figure 2C) while lower CD-RISC-10 score (F = 123.34, p < 0.001, Figure 2D) than the other two profiles. The relations among profiles and mental health outcomes are described in Table 4. In the crude model, college students in the “mild SD” profile or “high SD” profile were more likely to have a higher level of depressive symptoms and PLEs, while a lower level of resilience compared with those in the “no SD” profile. This significant effect between the mild/high SD and college students’ mental health persisted after adjusting for sample characteristics variable.
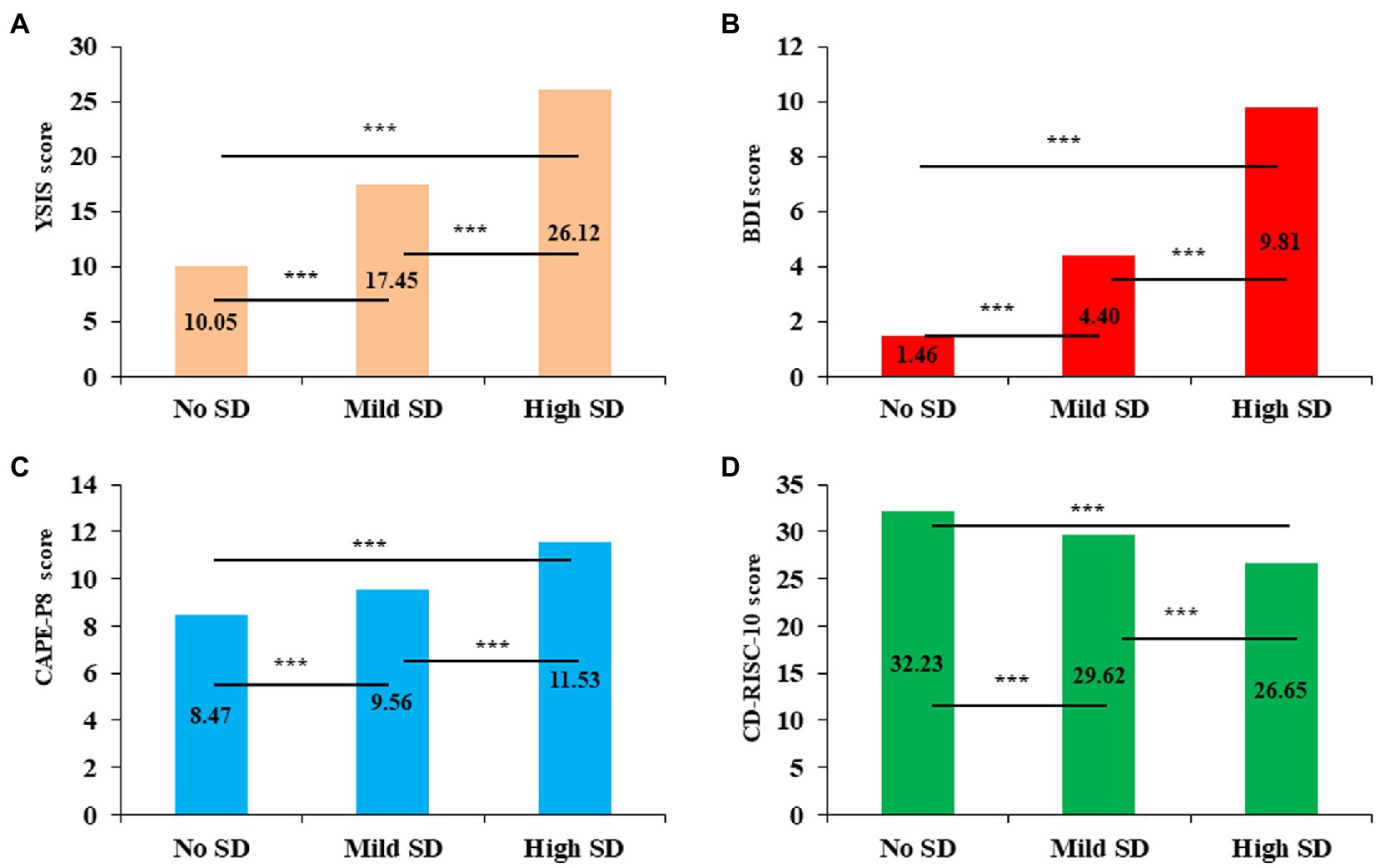
Figure 2. Comparison of mental health variables across different SD profiles. SD, sleep disturbance; YSIS, Youth Self-Rating Insomnia Scale; BDI, Beck Depression Inventory; CAPE-P8, 8-item Positive Subscale of the Community Assessment of Psychic Experiences; CD-RISC-10, 10-item Connor-Davidson Resilience Scale. ***p < 0.001.
Discussion
The present study adopted LPA to explore subtypes of SD and their related factors in college students. The findings are beneficial to education administrators and clinicians better understand the heterogeneous cluster classification characteristics of SD in college students to formulate more specific and targeted intervention measures.
First, three latent profiles of SD among college students were identified in this study: “high SD,” “mild SD,” and “no SD.” The finding of the presence of three potential SD profiles is similar to previous studies in other groups (49, 50). For example, Tejada and colleagues explored the heterogeneity of SD in 1,331 chemotherapy patients using LPA, pointing out three SD profiles: “low,” “high,” and “very high” (50). Our data showed that approximately half of the samples (51.9%) were categorized as “no SD” profile, and only 10.6% have high SD. We compared the results with previous studies of similar university students. Zhou and colleagues used LCA to analyze the distinct classes of sleep behavior (on the Dysfunction Beliefs and Attitudes about Sleep [DBAS] and PSQI), and concluded that 6.8% of college students was in the “sleep disturbances and daytime dysfunction” subtype, while 31.8% was in the “good sleep” subtype (19). Another study (on the Insomnia Severity Index [ISI] and PSQI) adapted LPA and pointed out that 8.8% college students have severe insomnia, 66.9% reported subthreshold insomnia or subthreshold insomnia with sleep latency complaints (composed by students with relatively low insomnia severity) (18). Due to instruments and sampling, the findings differ to some extent. However, these studies have reached consistent conclusions, that is, most individuals could cope well to stressor of life events and maintain good sleep function, while only a small percentage exhibit clinical levels of SD. In addition, 37.5% of the samples were categorized as “mild SD” profile. Although the YSIS scores of these college students did not meet the criteria for clinically SD (cut-off value = 26), they had higher than average levels of SD. College students in “mild SD” profile still exhibited low frequency (the average score of the 8 YSIS item was 2.18) of SD related symptoms. Therefore, it is necessary to employ targeted interventions for those in this subtype to prevent them from sliding into sleep-related impairment and SD.
Second, multivariate logistic regression identified several risk factors associated with increased likelihood of experiencing moderate and high SD. Our data showed that male students were more likely to be found in the “high SD” profile than the female. Although previous studies have examined SD in the college students group, findings concerning the effects of sex on SD have been inconsistent. Several studies found that male students exhibiting greater SD (51–53). However, some studies suggested that SD among female students was even more severe than that of the male (23, 54, 55), while others reported no sex differences in SD (56–58). We speculated that male college students have more sleep-adverse lifestyles, such as Internet addiction, alcohol and energy drinks consumption, and cigarette smoking (59, 60). Poor parental marital status was also one of the risk factors for SD, in line with previous research (25, 61). Stressful changes in the parents’ relationship lead to disruptions in family processes, which, in turn, negatively impact the individual’s physiologic functioning (62, 63), and physiologic changes may interfere with sleep (64, 65). The results also indicate the possible impacts of the sophomores on the development of SD among college students. The finding is similar with previous study (66), in which sophomores had more professional course loads compared with freshmen, and these stress may have affected their sleep quality to some extent.
Third, college students in the “mild SD” and “high SD” profile report greater depressive symptoms and PLEs in comparison to those in the no SD profile. A great volume of literature has consistently asserted that SD as a risk factor for depressive symptoms and PLEs (28, 67, 68). Recent evidence has also suggested that college students with SD are prone to maladaptive emotion regulation (69) and impaired social functioning (70), resulting in the development of depressive symptoms and PLEs. Additionally, our study also found SD negatively associated with resilience. Studies in children have reported that greater SD reduced resilience (71). Another longitudinal study also found that higher sleep rhythmicity and fewer SD in early age predicted higher behavioral control in adolescence, which, in turn, predicted resilience in young adulthood (72).
Accordingly, therapeutic interventions targeting SD may benefit from a tailored approach that takes individual symptom patterns of SD into great consideration. For example, college students in profile 1 (high SD) have poor sleep quality and more adverse psychological outcomes, therefore require prompt clinical treatment to help alleviate their sleep disorders. Meanwhile, although college students in profile 1 (mild SD), who did not have particularly severe SD related symptoms, were still at higher risk for mental health problems relative to those in the no SD profile. Therefore, it is necessary to optimize the sleep habits of these students and improve their sleep quality. Several interventions can be carried out (e.g., cognitive behavioral therapy, mindfulness and hypnotherapy (73)) to improve sleep quality for college students in the mild SD and high SD profile. Also, influential factors should also be taken into consideration for effective psychosocial intervention for college students. Some students, especially those with male gender, sophomores and poor parental marital status, exhibit moderate or high SD. Thus, the need for individualized intervention with these students is indicated.
Limitations
Despite all the relevant findings, several limitations of the current study should be noted. First, measures of SD, depressive symptom, PLEs, and other psychological factors relied on self-report questionnaires, which might be influenced by reporting bias caused by recollection inaccuracy and individuals’ own psychiatric states. Second, the data were collected in the Shanxi Province of China, which is uncertain whether the findings could be generalized to all college students to other regions of China. Thus, future studies would benefit from increasing the sampling range and sample size. Finally, this was a cross-sectional study, which limits the ability to make causal inference. In clinical practice, SD and mental health may do form a bidirectional relationships (74–76). Therefore, future research is necessary to design longitudinal studies to further explore the effects of different SD subtypes on mental health outcomes.
Conclusion
These findings indicate that SD in Chinese college students has obvious classification characteristics. We identified three profiles of SD in college students. Furthermore, we suggest that education or clinical workers should pay particular attention to college students classified into the mild SD and high SD profile and especially male college students, sophomores and those with poor parental marital status.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committees of South China Normal University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
DW: conceptualization. CC and DW: methodology, formal analysis, and writing—original draft. ZH, BX, and JS: data curation. BX and DW: writing–review and editing. All authors contributed to the article and approved the submitted version.
Funding
The present study was funded by Graduate Research and Innovation Project of School of Psychology, South China Normal University (PSY-SCNU202017).
Acknowledgments
The authors would like to thank all the students who took part in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lund, HG, Reider, BD, Whiting, AB, and Prichard, JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. (2010) 46:124–2. doi: 10.1016/j.jadohealth.2009.06.016
2. Gaultney, JF. The prevalence of sleep disorders in college students: impact on academic performance. J Am Coll Heal. (2010) 59:91–7. doi: 10.1080/07448481.2010.483708
3. Jahrami, HA, Alhaj, OA, Humood, AM, Alenezi, AF, Fekih-Romdhane, F, AlRasheed, MM, et al. Sleep disturbances during the COVID-19 pandemic: a systematic review, meta-analysis, and meta-regression. Sleep Med Rev. (2022) 62:101591. doi: 10.1016/j.smrv.2022.101591
4. Arnett, JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. (2000) 55:469–09, 480. doi: 10.1037//0003-066X.55.5.469
5. Brougham, RR, Zail, CM, Mendoza, CM, and Miller, JR. Stress, sex differences, and coping strategies among college students. Curr Psychol. (2009) 28:85–97. doi: 10.1007/s12144-009-9047-0
6. Pierceall, EA, and Keim, MC. Stress and coping strategies among community college students. Commun Coll J Res Pract. (2007) 31:703–2. doi: 10.1080/10668920600866579
7. Akerstedt, T. Psychosocial stress and impaired sleep. Scand J Work Environ Health. (2006) 32:493–1. doi: 10.1080/10668920600866579
8. Tavernier, R, and Willoughby, T. Sleep problems: predictor or outcome of media use among emerging adults at university? J Sleep Res. (2014) 23:389–6. doi: 10.1111/jsr.12132
9. Sivertsen, B, Vedaa, O, Harvey, AG, Glozier, N, Pallesen, S, Aarø, LE, et al. Sleep patterns and insomnia in young adults: a national survey of Norwegian university students. J Sleep Res. (2019) 28:e12790. doi: 10.1111/jsr.12790
10. Schlarb, AA, Kulessa, D, and Gulewitsch, MD. Sleep characteristics, sleep problems, and associations of self-efficacy among German university students. Nat Sci Sleep. (2012) 4:1–7. doi: 10.2147/NSS.S27971
11. Becker, SP, Jarrett, MA, Luebbe, AM, Garner, AA, Burns, GL, and Kofler, MJ. Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health. (2018) 4:174–1. doi: 10.1016/j.sleh.2018.01.001
12. Moo-Estrella, J, Perez-Benitez, H, Solis-Rodriguez, F, and Arankowsky-Sandoval, G. Evaluation of depressive symptoms and sleep alterations in college students. Arch Med Res. (2005) 36:393–8. doi: 10.1016/j.arcmed.2005.03.018
13. Nadorff, MR, Nazem, S, and Fiske, A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep. (2011) 34:93–8. doi: 10.1093/sleep/34.1.93
14. Buboltz, WJ, Brown, F, and Soper, B. Sleep habits and patterns of college students: a preliminary study. J Am Coll Heal. (2001) 50:131–5. doi: 10.1080/07448480109596017
15. von Eye, A, and Bergman, LR. Research strategies in developmental psychopathology: dimensional identity and the person-oriented approach. Dev Psychopathol. (2003) 15:553–09. doi: 10.1017/s0954579403000294
16. Laursen, BP, and Hoff, E. Person-centered and variablecentered approaches to longitudinal data. Merrill-Palmer Q. (2006) 52:377–9. doi: 10.1353/mpq.2006.0029
17. Hybels, CF, Blazer, DG, Pieper, CF, Landerman, LR, and Steffens, DC. Profiles of depressive symptoms in older adults diagnosed with major depression: latent cluster analysis. Am J Geriatr Psychiatry. (2009) 17:387–6. doi: 10.1097/JGP.0b013e31819431ff
18. Carpi, M, Marques, DR, Milanese, A, and Vestri, A. Sleep quality and insomnia severity among Italian university students: a latent profile analysis. J Clin Med. (2022) 11:4069. doi: 10.3390/jcm11144069
19. Zhou, J, Jin, LR, Tao, MJ, Peng, H, Ding, SS, and Yuan, H. The underlying characteristics of sleep behavior and its relationship to sleep-related cognitions: a latent class analysis of college students in Wuhu city. China Psychol Health Med. (2020) 25:887–7. doi: 10.1080/13548506.2019.1687915
20. DeMartini, KS, and Fucito, LM. Variations in sleep characteristics and sleep-related impairment in at-risk college drinkers: a latent profile analysis. Health Psychol. (2014) 33:1164–73. doi: 10.1037/hea0000115
21. Chung, KF, and Cheung, MM. Sleep-wake patterns and sleep disturbance among Hong Kong Chinese adolescents. Sleep. (2008) 31:185–4. doi: 10.1093/sleep/31.2.185
22. Zhou, HQ, Shi, WB, Wang, XF, Yao, M, Cheng, GY, Chen, PY, et al. An epidemiological study of sleep quality in adolescents in South China: a school-based study. Child Care Health Dev. (2012) 38:581–7. doi: 10.1111/j.1365-2214.2011.01300.x
23. Cheng, SH, Shih, CC, Lee, IH, Hou, YW, Chen, KC, Chen, KT, et al. A study on the sleep quality of incoming university students. Psychiatry Res. (2012) 197:270–4. doi: 10.1016/j.psychres.2011.08.011
24. Guo, L, Deng, J, He, Y, Deng, X, Huang, J, Huang, G, et al. Prevalence and correlates of sleep disturbance and depressive symptoms among Chinese adolescents: a cross-sectional survey study. BMJ Open. (2014) 4:e5517. doi: 10.1136/bmjopen-2014-005517
25. Troxel, WM, Lee, L, Hall, M, and Matthews, KA. Single-parent family structure and sleep problems in black and white adolescents. Sleep Med. (2014) 15:255–1. doi: 10.1016/j.sleep.2013.10.012
26. Philbrook, LE, Saini, EK, Fuller-Rowell, TE, Buckhalt, JA, and El-Sheikh, M. Socioeconomic status and sleep in adolescence: the role of family chaos. J Fam Psychol. (2020) 34:577–6. doi: 10.1037/fam0000636
27. Ivanenko, A, Crabtree, VM, and Gozal, D. Sleep and depression in children and adolescents. Sleep Med Rev. (2005) 9:115–9. doi: 10.1016/j.smrv.2004.09.006
28. Wang, D, Chen, H, Chen, Z, Yang, Z, Zhou, X, Tu, N, et al. Resilience buffers the association between sleep disturbance and psychotic-like experiences in adolescents. Schizophr Res. (2022) 244:118–5. doi: 10.1016/j.schres.2022.05.018
29. Arbinaga, F. Self-reported perceptions of sleep quality and resilience among dance students. Percept Mot Skills. (2018) 125:351–8. doi: 10.1177/0031512518757352
30. Liu, X, Yang, Y, Liu, ZZ, Luo, Y, Fan, F, and Jia, CX. Psychometric properties of youth self-rating insomnia scale (YSIS) in Chinese adolescents. Sleep Biol Rhyth. (2019) 17:339–8. doi: 10.1007/s41105-019-00222-3
31. Beck, AT, Ward, CH, Mendelson, M, Mock, J, and Erbaugh, J. An inventory for measuring depression. Arch Gen Psychiatry. (1961) 4:561–1. doi: 10.1001/archpsyc.1961.01710120031004
32. Bennett, DS, Ambrosini, PJ, Bianchi, M, Barnett, D, Metz, C, and Rabinovich, H. Relationship of Beck depression inventory factors to depression among adolescents. J Affect Disord. (1997) 45:127–4. doi: 10.1016/s0165-0327(97)00045-1
33. Zheng, YP, Wei, LA, Goa, LG, Zhang, GC, and Wong, CG. Applicability of the Chinese Beck depression inventory. Compr Psychiatry. (1988) 29:484–9. doi: 10.1016/0010-440x(88)90063-6
34. Wang, D, Sun, M, Xi, C, Yang, X, Mwansisya, T, Ouyang, X, et al. Gender and longitudinal measurement invariance of the community assessment of psychic experiences-positive subscale. Chin J Clin Psychol. (2020) 28:41–5. [In Chinese]
35. Wang, D, Sun, M, Ouyang, X, and Fang, F. Validity and reliability of the simplfied version of community assessment of psychic Exeriences in college students. Chin Ment Health J. (2022) 36:172–8. [In Chinese]
36. Mark, W, and Toulopoulou, T. Validation of the Chinese version of community assessment of psychic experiences (CAPE) in an adolescent general population. Asian J Psychiatr. (2017) 26:58–65. doi: 10.1016/j.ajp.2017.01.012
37. Konings, M, Bak, M, Hanssen, M, van Os, J, and Krabbendam, L. Validity and reliability of the CAPE: a self-report instrument for the measurement of psychotic experiences in the general population. Acta Psychiatr Scand. (2006) 114:55–61. doi: 10.1111/j.1600-0447.2005.00741.x
38. Wang, D, Chen, H, Chen, Z, Liu, W, Wu, L, et al. Current psychotic-like experiences among adolescents in China: identifying risk and protective factors. Schizophr Res. (2022) 244:111–7. doi: 10.1016/j.schres.2022.05.024
39. Sun, M, Xue, Z, Zhang, W, Guo, R, Hu, A, Li, Y, et al. Psychotic-like experiences, trauma and related risk factors among "left-behind" children in China. Schizophr Res. (2017) 181:43–8. doi: 10.1016/j.schres.2016.09.030
40. Campbell-Sills, L, and Stein, MB. Psychometric analysis and refinement of the Connor-davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. (2007) 20:1019–28. doi: 10.1002/jts.20271
41. Cheng, C, Dong, D, He, J, Zhong, X, and Yao, S. Psychometric properties of the 10-item Connor-Davidson resilience scale (CD-RISC-10) in Chinese undergraduates and depressive patients. J Affect Disord. (2020) 261:211–09. doi: 10.1016/j.jad.2019.10.018
42. Wang, L, Shi, Z, Zhang, Y, and Zhang, Z. Psychometric properties of the 10-item Connor-Davidson resilience scale in Chinese earthquake victims. Psychiatry Clin Neurosci. (2010) 64:499–4. doi: 10.1111/j.1440-1819.2010.02130.x
43. Johnson, RE, Rosen, CC, and Djurdjevic, E. Assessing the impact of common method variance on higher order multidimensional constructs. J Appl Psychol. (2011) 96:744–1. doi: 10.1037/a0021504
44. Podsakoff, PM, and Organ, DW. Self-reports in organizational research: problems and prospects. J Manage. (1986) 12:531–4. doi: 10.1177/014920638601200408
45. Burnham, K, and Anderson, D. Multimodel inference: Understad ing AIC and BIC in model selection. Sociol Method Res. (2004) 3:261–4.
46. Ramaswamy, V, Desarbo, WS, and Robinson, RWT. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Market Sci. (1993) 12:103–24. doi: 10.1287/mksc.12.1.103
47. Lo, YT, Mendell, NR, and Rubin, DB. Testing the number of components in a normal mixture. Biometrika. (2001) 88:767–8. doi: 10.1093/biomet/88.3.767
48. Nylund, KL, Asparouhov, T, and Muthén, BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model Multidiscip J. (2007) 14:535–9. doi: 10.1080/10705510701575396
49. Lin, Y, Bailey, DJ, Docherty, SL, Porter, LS, Cooper, BA, Paul, SM, et al. Distinct sleep disturbance profiles in patients with gastrointestinal cancers receiving chemotherapy. Cancer Nurs. (2022) 45:E417–27. doi: 10.1097/NCC.0000000000000975
50. Tejada, M, Viele, C, Kober, KM, Cooper, BA, Paul, SM, Dunn, LB, et al. Identification of subgroups of chemotherapy patients with distinct sleep disturbance profiles and associated co-occurring symptoms. Sleep. (2019) 42:zsz151. doi: 10.1093/sleep/zsz151
51. Xiao, R, Zhang, X, Xie, Y, Liu, H, and Feng, X. Sleep quality of the students of military medical school. Chin Ment Health J. (2005) 19:61–3. [In Chinese].
52. Lu, J, Fang, GE, Shen, SJ, Wang, Y, and Sun, Q. A questionnaire survey on sleeping in class phenomenon among Chinese medical undergraduates. Med Teach. (2011) 33:508.
53. Fan, Q, Zhang, X, Wen, J, Lin, Z, and Cai, Q. Sleep quality and its influencing factors among medical students in Putian City. Chin J Health Educ. (2014) 33:624–7. [In Chinese]
54. Jin, Y, Ding, Z, Fei, Y, Jin, W, Liu, H, Chen, Z, et al. Social relationships play a role in sleep status in Chinese undergraduate students. Psychiatry Res. (2014) 220:631–8. doi: 10.1016/j.psychres.2014.08.029
55. Lemma, S, Gelaye, B, Berhane, Y, Worku, A, and Williams, MA. Sleep quality and its psychological correlates among university students in Ethiopia: a cross-sectional study. BMC Psychiatry. (2012) 12:237. doi: 10.1186/1471-244X-12-237
56. Adams, SK, and Kisler, TS. Sleep quality as a mediator between technology-related sleep quality, depression, and anxiety. Cyberpsychol Behav Soc Netw. (2013) 16:25–30. doi: 10.1089/cyber.2012.0157
57. Kang, JH, and Chen, SC. Effects of an irregular bedtime schedule on sleep quality, daytime sleepiness, and fatigue among university students in Taiwan. BMC Public Health. (2009) 9:248. doi: 10.1186/1471-2458-9-248
58. Choueiry, N, Salamoun, T, Jabbour, H, El, ON, Hajj, A, and Rabbaa, KL. Insomnia and relationship with anxiety in university students: a cross-sectional designed study. PLoS One. (2016) 11:e149643:e0149643. doi: 10.1371/journal.pone.0149643
59. Gupta, R, Taneja, N, Anand, T, Gupta, A, Gupta, R, Jha, D, et al. Internet addiction, sleep quality and depressive symptoms amongst medical students in Delhi. India Commun Ment Health J. (2021) 57:771–6. doi: 10.1007/s10597-020-00697-2
60. Lohsoonthorn, V, Khidir, H, Casillas, G, Lertmaharit, S, Tadesse, MG, Pensuksan, WC, et al. Sleep quality and sleep patterns in relation to consumption of energy drinks, caffeinated beverages, and other stimulants among Thai college students. Sleep Breath. (2013) 17:1017–28. doi: 10.1007/s11325-012-0792-1
61. Gregory, AM, Caspi, A, Moffitt, TE, and Poulton, R. Family conflict in childhood: a predictor of later insomnia. Sleep. (2006) 29:1063–7. doi: 10.1093/sleep/29.8.1063
62. Dopp, JM, Miller, GE, Myers, HF, and Fahey, JL. Increased natural killer-cell mobilization and cytotoxicity during marital conflict. Brain Behav Immun. (2000) 14:10–26. doi: 10.1006/brbi.1999.0567
63. Smith, TW, and Gallo, LC. Hostility and cardiovascular reactivity during marital interaction. Psychosom Med. (1999) 61:436–5. doi: 10.1097/00006842-199907000-00005
64. El-Sheikh, M, and Buckhalt, JA. Vagal regulation and emotional intensity predict children's sleep problems. Dev Psychobiol. (2005) 46:307–7. doi: 10.1002/dev.20066
65. Phillips, B, and Mannino, DM. Does insomnia kill? Sleep. (2005) 28:965–1. doi: 10.1093/sleep/28.8.965
66. Wang, D, Chen, H, Zhai, S, Zhu, Z, Huang, S, Zhou, X, et al. Is returning to school during the COVID-19 pandemic stressful? A study on immediate mental health status of Chinese college students. J Affect Disord. (2021) 287:261–7. doi: 10.1016/j.jad.2021.03.035
67. Pandi-Perumal, SR, Monti, JM, Burman, D, Karthikeyan, R, BaHammam, AS, Spence, DW, et al. Clarifying the role of sleep in depression: a narrative review. Psychiatry Res. (2020) 291:113239. doi: 10.1016/j.psychres.2020.113239
68. Simor, P, Bathori, N, Nagy, T, and Polner, B. Poor sleep quality predicts psychotic-like symptoms: an experience sampling study in young adults with schizotypal traits. Acta Psychiatr Scand. (2019) 140:135–6. doi: 10.1111/acps.13064
69. Niu, X, and Snyder, HR. The role of maladaptive emotion regulation in the bidirectional relation between sleep and depression in college students during the COVID-19 pandemic. Anxiety Stress Coping. (2022) 36:83–96. doi: 10.1080/10615806.2022.2073441
70. Korenic, SA, Ered, A, Pierce, KM, Calvo, EM, Olino, TM, Murty, VP, et al. Examining self-reported social functioning, sleep quality, and psychotic-like experiences in college students. J Psychiatr Res. (2021) 143:54–9. doi: 10.1111/j.1600-0447.2005.00741.x
71. Doi, S, Fujiwara, T, Ochi, M, Isumi, A, and Kato, T. Association of sleep habits with behavior problems and resilience of 6- to 7-year-old children: results from the A-CHILD study. Sleep Med. (2018) 45:62–8. doi: 10.1016/j.sleep.2017.12.015
72. Wong, MM, Puttler, LI, Nigg, JT, and Zucker, RA. Sleep and behavioral control in earlier life predicted resilience in young adulthood: a prospective study of children of alcoholics and controls. Addict Behav. (2018) 82:65–71. doi: 10.1016/j.addbeh.2018.02.006
73. Friedrich, A, and Schlarb, AA. Let's talk about sleep: a systematic review of psychological interventions to improve sleep in college students. J Sleep Res. (2018) 27:4–22. doi: 10.1111/jsr.12568
74. Wang, D, Zhou, L, Wang, J, and Sun, M. The bidirectional associations between insomnia and psychotic-like experiences before and during the COVID-19 pandemic. Nat Sci Sleep. (2021) 13:2029–37. doi: 10.2147/NSS.S335508
75. Wang, J, Zhang, X, Simons, SR, Sun, J, Shao, D, and Cao, F. Exploring the bi-directional relationship between sleep and resilience in adolescence. Sleep Med. (2020) 73:63–9. doi: 10.1016/j.sleep.2020.04.018
Keywords: sleep disturbance, depressive symptoms, psychotic-like experience, resilience, college students
Citation: Chen C, He Z, Xu B, Shao J and Wang D (2023) A latent profile analysis of sleep disturbance in relation to mental health among college students in China. Front. Public Health. 11:1107692. doi: 10.3389/fpubh.2023.1107692
Edited by:
Karen Spruyt, Institut National de la Santé et de la Recherche Médicale (INSERM), FranceReviewed by:
Katerina M. Marcoulides, University of Minnesota, United StatesHenning Johannes Drews, University of Copenhagen, Denmark
Copyright © 2023 Chen, He, Xu, Shao and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongfang Wang, wdfpsyc@126.com
 Chunping Chen1
Chunping Chen1 Dongfang Wang
Dongfang Wang