- 1Non-Communicable Diseases Research Center, Ilam University of Medical Sciences, Ilam, Iran
- 2Department of Occupational Health Engineering and Safety at Work, School of Public Health, Kerman University of Medical Sciences, Kerman, Iran
- 3Department of Nursing, School of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran
- 4Department of Neurology, Shohadaye Tajrish Hospital, Shahid Beheshti University of Medical Science, Tehran, Iran
- 5Health in Disasters and Emergencies Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
- 6Department of Health in Disasters and Emergencies, School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Introduction: Health Care Workers (HCWs) use Personal Protective Equipment (PPE) during the COVID-19 pandemic to protect themselves and prevent the transmission of the disease. The use of PPE, especially respiratory masks, has adverse consequences, including headaches, which have been secondary and unusual. The aim of the present systematic review and meta-analysis study was to investigate the prevalence of PPE-associated headaches in HCWs during COVID-19 pandemic.
Methods: The present review study was performed based on the PRISMA guideline. The protocol of the present study was registered in PROSPERO with the code CRD42022304437. Valid data resources such as Scopus, PubMed, Web of Science, Science Direct, Google Scholar, Embase were used to identify and extract relevant studies. The searches were conducted between the beginning of 2020 and the end of January 2022. A random effects model was used for meta-analysis and I2 index was used to investigate between-study heterogeneity. Data were analyzed using STATA ver. 14.
Results: A total of 539 articles were first identified through initial search and finally 26 final studies were selected to undergo the meta-analysis phase. According to the results of meta-analysis, the prevalence of headache after and before the use of PPE was 48.27% (95% CI: 40.20–56.34, I2 = 99.3%, p = 0 < 001) and 30.47% (95% CI: 20.47–40.47, I2 = 97.3%, p = 0 < 001), respectively.
Conclusion: The results of the present study showed that the prevalence of PPE-associated headache in HCWs was relatively high, so, the use of PPE during COVID-19 pandemic can be considered as one of the causes of headache. Therefore, management strategies such as regular screening of HCWs for headaches and regular rest periods without the use of PPE can be effective in reducing the prevalence of headaches.
Introduction
COVID-19 pandemic has affected the care activities of health care workers (HCWs) (1). Based on the available evidence, the Covid-19 virus is transmitted through close contact between individuals. Those who are in close contact with a Covid-19 patient or care for COVID-19 patients are at higher risk for the disease. HCWs are therefore required to use Personal Protective Equipment (PPE) to prevent the virus transmission while performing their duties to protect themselves (2–4).
According to the World Health Organization (WHO), PPE included guns, non-sterile gloves, goggles and respiratory masks (2). Although each country has its own certification standard for each mask type (3), in fact, the use of PPE by HCWs has unpleasant and annoying effects that will be exacerbated in the long run (4). However, long-term use of PPE is essential due to the prevalence of infectious diseases such as COVID-19 (4, 5).
The use of PPE, especially respiratory masks, can have a number of consequences, including headaches for HCWs. PPE-associated headaches are an unusual secondary headache, that mainly occur among HCWs due to the use of protective masks, Face masks and/or googles and have recently been studied in various studies (6, 7). PPE-associated headaches are considered as a subtype of external compression headaches (8). Although these headaches are often short-lived and without long-term side effects, they can affect occupational health, professional performance of HCWs, and their behavior in the proper use of PPEs (9).
Changes in staff conditions during the COVID-19 pandemic are more likely to cause PPE-associated headaches (6). Extended hours of work shifts (more than 8 h), combined use of PPE for long periods of time, or a higher physical and cognitive workload of HCWs when using PPE can increase the prevalence of PPE-associated headaches (7, 10–12). Studies have shown that using PPE every hour increases the risk of new symptoms (including headaches) by 1.38 times (18). Considering that the COVID-19 pandemic has provided an opportunity to study PPE-associated headaches among HCWs, the prevalence of PPE- associated headaches among HCWs has been assessed and reported in many studies since the onset of the COVID-19 pandemic (6, 13, 14). However, the results showed that there has been no comprehensive study on the prevalence of PPE- associated headaches HCWs during COVID-19 pandemic.
Therefore, this study was conducted with the aim of investigating the prevalence of headache associated with PPE in HCWs during COVID-19, and the prevalence of headache after using PPE and before using PPE was investigated among the studies conducted in this field. The results of this study can show whether HCWs are more prone to headaches after using PPE. Considering the importance of the subject matter, the results of the present systematic review and meta-analysis may provide an important source of information for health planning in addition to adding information about PPE-related headaches.
Methods
Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) guideline was used to conduct the present systematic review and meta-analysis (15). The protocol of the present review study was registered in International Prospective Register of Systematic Review (PROSPERO) with the code CRD42022304437.
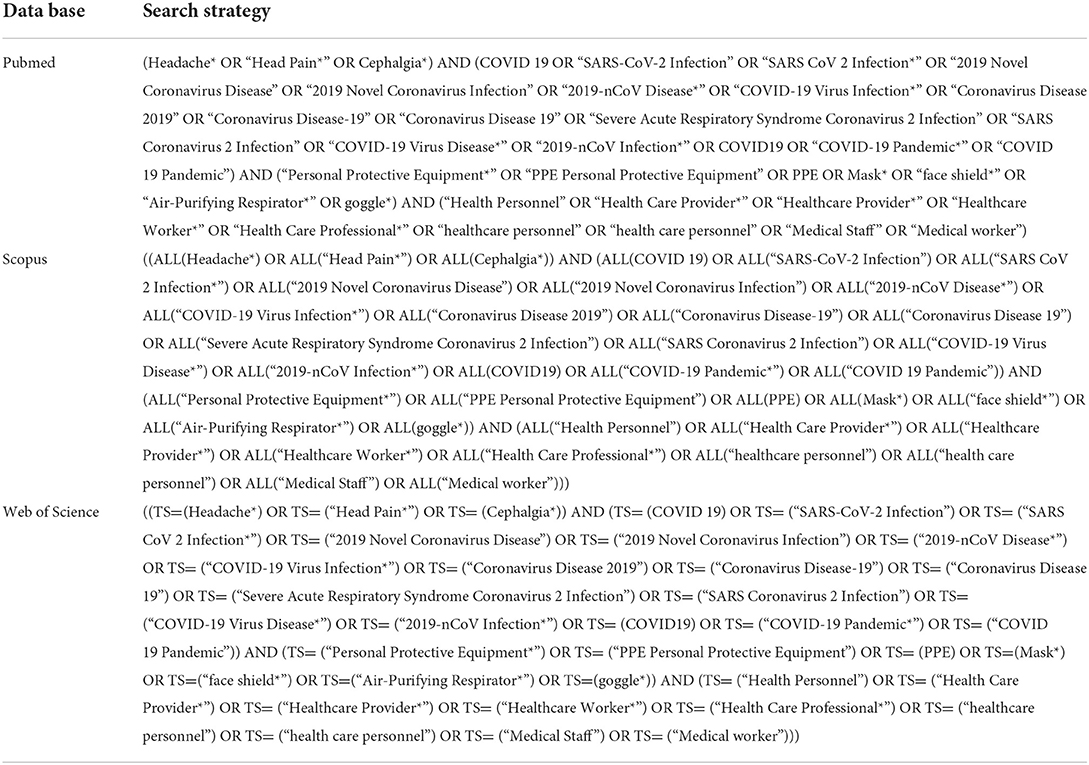
Data resources and search strategy
In this research, Data resources including PubMed, Scopus, Web of Science, Science Direct, Google Scholar, Embase, were used to search and extract studies. Also, valid keywords such as Headache*, “Head Pain*,” Cephalgia*, COVID 19, “SARS-CoV-2 Infection”, “SARS CoV 2 Infection,*” “2019 Novel Coronavirus Disease,” “2019 Novel Coronavirus Infection,” “2019-nCoV Disease,*” “COVID-19 Virus Infection,*” “Coronavirus Disease 2019,” “Coronavirus Disease-19,” “Coronavirus Disease 19,” “Severe Acute Respiratory Syndrome Coronavirus 2 Infection,” “SARS Coronavirus 2 Infection,” “COVID-19 Virus Disease,*” “2019-nCoV Infection,*” COVID19 OR “COVID-19 Pandemic,*” “COVID 19 Pandemic,” “Personal Protective Equipment,*” “PPE Personal Protective Equipment,” PPE OR Mask,* “face shield,*” “Air-Purifying Respirator,*” goggle*, “Health Personnel,” “Health Care Provider,*” “Healthcare Provider,*” “Healthcare Worker,*” “Health Care Professional,*” “healthcare personnel,” “health care personnel,” “Medical Staff,” “Medical worker,” Search fields and operators were used to formulate the search strategy. The searches were conducted in English from the beginning of 2020 to the end of January 2022. The search strategy for types of databases is listed in Table 1.
Inclusion criteria
The inclusion criteria included English articles that investigated PPE-associated headaches in HCWs during COVID-19 pandemic.
Exclusion criteria
Case report studies, review studies, intervention studies, letter-to-the editor and headache report in non-HCWs as well as report of PPE-associated headache in HCWs in non-COVID 19 situation and also during other pandemics.
Selection of studies
Endnote 7 software was used to collect the primary identified studies. After removing the duplicates, the titles and abstracts of the remaining studies were screened. In the studies selection phase, two researchers independently read the full text of potentially relevant studies and finally selected studies for qualitative assessment. Any disagreement between reviewers was resolved by a third reviewer.
Qualitative assessment and data extraction
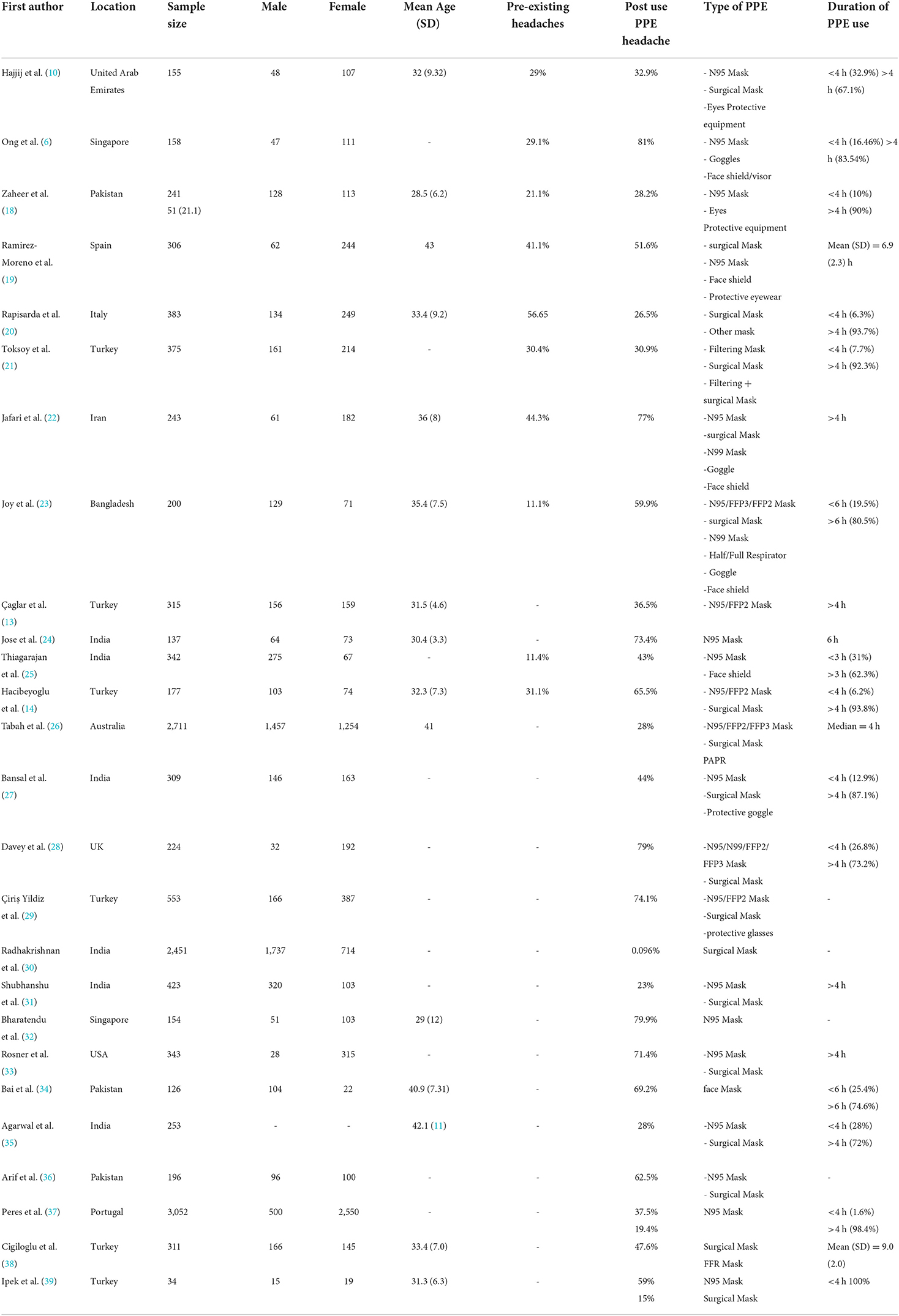
After selecting the studies, two researchers independently used the Tool Appraisal tool for Cross-Sectional Studies (AXIS) (16) to assess the quality of the selected studies. The possible score range is 0 to 20 and studies with a score above 12 entered the meta-analysis phase. Any disagreement between the reviewers was resolved by the third reviewer. Also, in the data extraction stage, two researchers independently extracted the type of PPE used as well as the prevalence of subsequent headache before and after the use of PPE and using a pre-prepared checklist that includes information on first author, place of study, average age, number of men and women, sample size, duration of PPE use. A third person was used to resolve any disagreement between the two researchers.
Statistical analysis
I2 index was used to evaluate the between-study heterogeneity. I2 index <25%, 25–50%, 50–75% and more than 75% showed no heterogeneity, moderate, high and very high heterogeneity, respectively (17). In order to reduce the between-study heterogeneity, a random effects model was used for meta-analysis. Begg test was used to evaluate the publication bias. Data analysis was carried out using STATA software ver. 14.
Results
In this review, 539 initial articles were identified by searching the aforementioned databases. After eliminating duplicates, 451 studies were screened. Afterwards, 94 studies were selected, and finally, 26 studies were selected to undergo quality assessment and then all of them entered the meta-analysis phase (Figure 1). Also, 14,172 HCWs were examined for headaches, of whom 7,986 were male and 6,186 were female. All studies were cross-sectional studies (Table 2). Among the selected studies, face shields were used in 5 studies and protective glasses were used along with masks in 4 studies. In most of the studied studies, surgical masks were used, and in some studies, N95 masks were also used along with surgical masks (Table 2). It should be noted that in the selected studies, most of the study participants used PPE more than 4 h a day. More detailed information about the time of use of the participants in the reviewed studies is presented in Table 2.
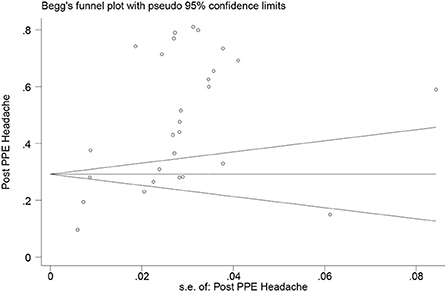
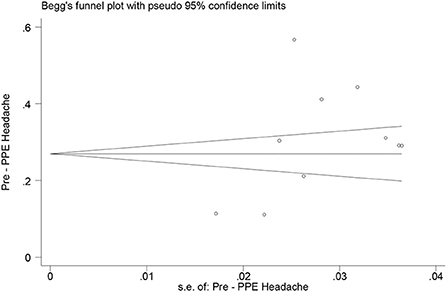
According to the results of meta-analysis, the prevalence of headache after and before the use of PPE was 48.27% (95% CI: 40.20–56.34, I2 = 99.3%, p = 0 < 001) (Figure 2) and 30.47% (95% CI: 20.47–40.47, I2 = 97.3%, p = 0 < 001), respectively (Figure 3). The I2 index showed that the between-study heterogeneity is very high. Results of Begg test showed that publication bias in headache after (P = 0.133) and before the use of PPE (P = 0.531) was negligible (Figures 4, 5).
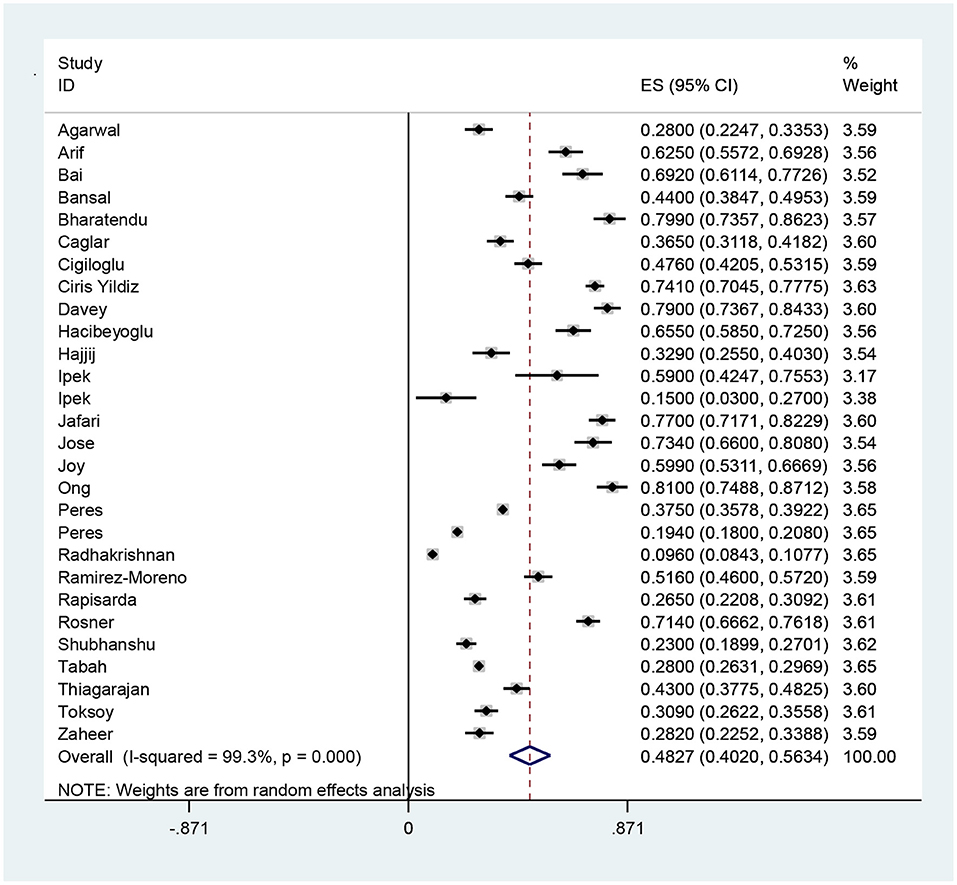
Figure 2. The prevalence of headache after the use of PPE and 95% confidence interval for each of the reviewed studies and the total studies. The midpoint of each segment shows the headache estimate and the length of the segment shows a 95% confidence interval. The diamond symbol indicates the total headache.
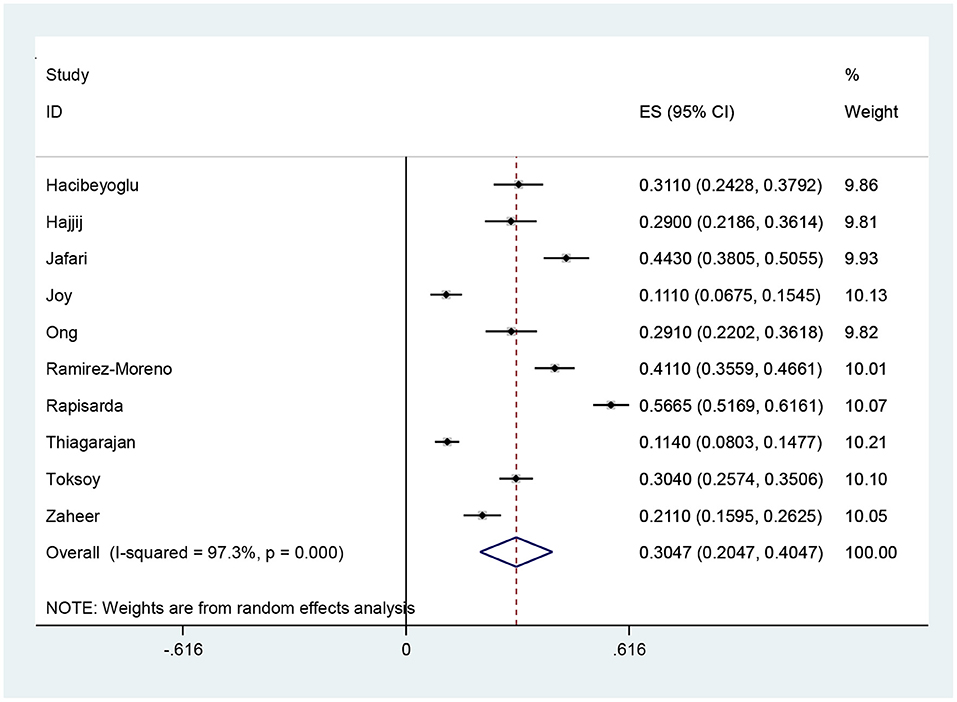
Figure 3. Headache rate before the use of PPE and 95% confidence interval for each of the reviewed studies and the total studies. The midpoint of each segment shows the headache estimate and the length of the segment shows a 95% confidence interval. The diamond symbol indicates the total headache.
Discussion
In the present review study, which was performed to investigate the prevalence of PPE-associated headaches in HCWs during the COVID-19 pandemic, 26 studies were selected for meta-analysis. According to the results of the present meta-analysis, the prevalence of headache after and before the use of PPE use was 48.27% and 30.47%, respectively, indicating that HCWs are more prone to PPE after using it.
In a study on psychological consequences and physical symptoms of HCWs during COVID-19, Chew et al. (40) showed that the prevalence of headache among HCWs was 31.9% and that there is a significant relationship between psychological disorders and physical symptoms (40). In a study on depression among neurosurgeons during COVID-19 pandemic, Sharif et al. (41) reported a headache rate of 20% (41). Yifan et al. (42) reported a headache rate of 19.3% when examining nurses' physical disorders during the Covid-19 pandemic (42). Since the results of the previous studies are consistent with the present study and emphasize the prevalence of headaches without the use of PPE in HCWs, so, it is suggested that health managers should assess these people for headaches due to several factors, including physical and psychological factors. On the other hand, in this study, the prevalence of headache associated with the PPE use was higher than studies in the study of headache without the PPE use, which shows the significant effect of the PPE use on headache among HCWs during the COVID-19 pandemic.
In study on HCWs who used the N95 mask during the SARS epidemic, Lim et al. (43) reported that the prevalence of face mask-associated headaches was 37.3% (43), which is lower than in the present study. Given that the COVID-19 disease is a pandemic and has affected HCWs for a long time, this difference in the prevalence of headache among HCWs can be justified.
A review study investigated the physiological and adverse effects of PPE use and results showed that headache was significant among other side effects (44). In a report sent as a letter-to-the editor, Swaminathan et al., reported that the prevalence of PPE-associated headache was 61.7% (45). The results of these studies are also consistent with the present study.
The face mask and eyewear can exert mechanical forces and stimulate superficial sensory neurons in the skull and neck (46, 47). Scarano et al. showed that long-term use of the FFP2 mask reduced hemoglobin oxygen saturation, increased heart rate, and facial temperature, which may lead to stress and headaches among HCWs (48). High blood carbon dioxide levels can also contribute to side effects such as dizziness, shortness of breath and headache (47). In these studies, factors have been identified as possible risk factors for headaches that are likely to occur to HCWs with the use of PPEs during the COVID-19 pandemic. Therefore, the results of the present study were not unexpected.
Various studies have concluded that headache is associated with prolonged PPE use (13, 24). Spontaneous headache relief has been reported within 60 min after PPE removal (6). Considering that duration of PPE use has increased during the Covid-19 outbreak, it is obvious that, as the results of the present study showed, the prevalence of headache will also increase during this period.
The effect of headache on personal health (both physical and mental health) and work performance has been confirmed in various studies (49–51). Although various factors, such as increased psychological and physical overload and occupational psychosocial stressors (52), may have caused headaches among HCWs during the outbreak of COVID-19 (40, 41), the PPE use has been cited in various studies as a major cause of headache. In their review study, Ong et al. discussed the clinical features and possible causes of PPE-associated headaches during the COVID-19 pandemic (7). In a narrative review, Romero et al. investigated the causes of headaches among HCWs during COVID-19 and stated that the physical and homeostatic effects of PPE use may also affect headache (47).
Proper PPE use is crucial for protecting HCWs from COVID-19 and airborne-transmitted infections (53). Therefore, since the results of the present study indicate a significant prevalence of PPE-associated headaches, it is worthwhile for planning committees to take steps to minimize the negative effects of PPE on their personnel and to increase their efforts to address this issue.
However, it is remarkable that PPE-associated headaches are also associated with psychological stress, depression, and sleep disorders, which increased during COVID-19 outbreak among HCWs, as headache is also the most common COVID-19-related neurological symptom (43). Because the aggravation of headaches can have a great impact on the wellbeing and occupational performance of HCWs.
Limitations
In this study, there was a high heterogeneity between studies, because in different studies that were conducted in this field, the sample size and tools used to assess the prevalence of PPE-Associated headaches were different.
We also failed to assess the prevalence of PPE- associated headaches by gender, Because most studies in this field have not done so. In addition, the timing of PPE use is likely to affect the prevalence of headache, but due to the fact that PPE timing varied in studies, we were unable to investigate this association.
Conclusion
The present study shows that a significant increase in the prevalence of headache among HCWs during the COVID-19 pandemic. In addition, the PPE use could be one of the causes of headache among HCWs during the COVID-19 pandemic, because the prevalence of headache after the use of PPE was higher than the prevalence of headache before the use of PPE in the present study. Therefore, further studies are needed to investigate the effects of PPE use on the onset of different categories of headache and other neurological conditions. Also, considering the effect of headache on HCWs performance (especially cognitive performance), which can lead to medical errors, in order to achieve a better PPE-user fit, further studies should be performed to provide intervention strategies in order to improve ergonomic features of PPEs that are used for a long time. In addition, management strategies such as regular screenings of HCWs for headaches and devoting rest periods so that HCWs can avoid using PPE for a period of time may also be effective in reducing the incidence of headaches. Therefore, it is recommended to conduct further studies in this field and investigate different solutions.
Author contributions
AS and ST managed the project. AS, ST, NH, and MS developed the inclusion criteria, screened titles, and abstracts. AY, AS, AT, and ST read and screened articles for inclusion. NH, AY, MS, and ST performed the qualitative assessment and data extraction. AS as a statistician and re-checked statistical analysis. ST, MS, and AT was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Acknowledgments
The systematic review design of the current study with research number 401000028 and ethical code IR.KMU.REC.1401.168 was approved and financially supported by Kerman University of Medical Sciences in 2022.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ahmad IA, Osei E. Occupational health and safety measures in healthcare settings during COVID-19: Strategies for protecting staff, patients and visitors. Disaster Med Public Health Preparedness. (2021) 2021:1–27. doi: 10.1017/dmp.2021.294
2. Organization WH. Rational Use of Personal Protective Equipment (PPE) for Coronavirus Disease (COVID-19): Interim Guidance, 19 March 2020. World Health Organization.(2020).
3. Jones RM, Rempel D. Standards for surgical respirators and masks: relevance for protecting healthcare workers and the public during pandemics. Ann Work Exposures Health. (2021) 65:495–504. doi: 10.1093/annweh/wxab008
4. Unoki T, Sakuramoto H, Sato R, Ouchi A, Kuribara T, Furumaya T, et al. Adverse effects of personal protective equipment among intensive care unit healthcare professionals during the COVID-19 pandemic: a scoping review. SAGE Open Nurs. (2021) 7:23779608211026164. doi: 10.1177/23779608211026164
5. Powell JB, Kim J-H, Roberge RJ. Powered air-purifying respirator use in healthcare: Effects on thermal sensations and comfort. J Occupat Environ Hyg. (2017) 14:947–54. doi: 10.1080/15459624.2017.1358817
6. Jy Ong J, Bharatendu C, Goh Y, Zy Tang J, Wx Sooi K, Lin Tan Y, et al. Headaches associated with personal protective equipment-a cross-sectional study amongst frontline healthcare workers during COVID-19 (HAPPE Study). Headache. (2020) 60:864–77. doi: 10.1111/head.13811
7. Ong JJ, Chan AC, Bharatendu C, Teoh HL, Chan YC, Sharma VK. Headache Related to PPE Use during the COVID-19 Pandemic. Curr Pain Headache Rep. (2021) 25:1–11. doi: 10.1007/s11916-021-00968-x
8. Arnold M. Headache classification committee of the international headache society (IHS) the international classification of headache disorders. Cephalalgia. (2018) 38:1–211. doi: 10.1177/0333102417738202
9. De Maio M, Onate J, Swain D, Morrison S, Ringleb S, Naiak D. Physical Performance Decrements in Military Personnel Wearing Personal Protective Equipment (PPE). Naval Medical Center Portsmouth VA (2009)
10. Hajjij A, Aasfara J, Khalis M, Ouhabi H, Benariba Jr F, El Kettani C. Personal protective equipment and headaches: cross-sectional study among Moroccan healthcare workers during COVID-19 pandemic. Cureus. (2020) 12:e12047. doi: 10.7759/cureus.12047
11. Carbajal AB, Boluarte AS, Boluarte AR, Soto CM. Working conditions and emotional impact in healthcare workers during COVID-19 pandemic. J Healthcare Q Res. (2020) 35:401. doi: 10.1016/j.jhqr.2020.08.002
12. Shoja E, Aghamohammadi V, Bazyar H, Moghaddam HR, Nasiri K, Dashti M, et al. Covid-19 effects on the workload of Iranian healthcare workers. BMC Public Health. (2020) 20:1–7. doi: 10.1186/s12889-020-09743-w
13. Çaǧlar A, Kaçer I, Hacimustafaoǧlu M, Öztürk B, Öztürk K. Symptoms associated with personal protective equipment among frontline health care professionals during the COVID-19 pandemic. Disaster Med Public Health Preparedness. (2022) 16:987–90. doi: 10.1017/dmp.2020.455
14. Hacibeyoglu G, Eren AS, Arican S, Yilmaz R, Reisli R, Uzun ST. Research for the factors effecting the headache experienced by the health-care personnel in COVID-19 pandemic: A monocentric survey study. Agri: Agri (Algoloji) Dernegi'nin Yayin Organidir. (2022) 34:7–15. doi: 10.14744/agri.2021.47108
15. Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Internal Med. (2009) 151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
16. Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. (2016) 6:e011458. doi: 10.1136/bmjopen-2016-011458
17. Sahebi A, Abdi K, Moayedi S, Torres M, Golitaleb M. The prevalence of insomnia among health care workers amid the COVID-19 pandemic: An umbrella review of meta-analyses. J Psychosomatic Res. (2021) 149:110597. doi: 10.1016/j.jpsychores.2021.110597
18. Zaheer R, Khan M, Tanveer A, Farooq A, Khurshid Z. Association of personal protective equipment with de novo headaches in frontline healthcare workers during COVID-19 pandemic: a cross-sectional study. Eur J Dentistry. (2020) 14(S 01):S79–85. doi: 10.1055/s-0040-1721904
19. Ramirez-Moreno JM, Ceberino D, Gonzalez Plata A, Rebollo B, Macias Sedas P, Hariramani R, et al. Mask-associated ‘de novo' headache in healthcare workers during the COVID-19 pandemic. Occupat Environ Med. (2021) 78:541–7. doi: 10.1101/2020.08.07.20167957
20. Rapisarda L, Trimboli M, Fortunato F, De Martino A, Marsico O, Demonte G, et al. Facemask headache: a new nosographic entity among healthcare providers in COVID-19 era. Neurol Sci. (2021) 42:1267–76. doi: 10.1007/s10072-021-05075-8
21. Toksoy CK, Demirbaş H, Bozkurt E, Acar H, Börü ÜT. Headache related to mask use of healthcare workers in COVID-19 pandemic. Korean J Pain. (2021) 34:241–5. doi: 10.3344/kjp.2021.34.2.241
22. Jafari E, Togha M, Kazemizadeh H, Haghighi S, Nasergivehchi S, Saatchi M, et al. Evaluation of headache associated with personal protective equipment during COVID-19. Brain Behav. (2021). doi: 10.1002/brb3.2435
23. Joy K, Mahmud R, Rabbani G, Islam M, Khalil M, Kundu N. Mask and Personal Protective Equipment (PPE) Associated Headache Among the COVID-Time Physicians of Bangladesh. J Headache Pain. (2021) 2021:2. doi: 10.52828/hmc.v1i2.8
24. Jose S, Cyriac MC, Dhandapani M. Health problems and skin damages caused by personal protective equipment: Experience of frontline nurses caring for critical COVID-19 patients in intensive care units. Ind J Crit Care Med. (2021) 25:134–9. doi: 10.5005/jp-journals-10071-23713
25. Thiagarajan S, Shetty P, Gulia A, Prakash G, Pramesh CS, Puri A. A survey of personnel protective equipment's (PPE) use and comfort levels among surgeons during routine cancer surgery in the COVID-19 pandemic. Ind J Surg Oncol. (2021) 12:365–73. doi: 10.1007/s13193-021-01316-6
26. Tabah A, Ramanan M, Laupland KB, Buetti N, Cortegiani A, Mellinghoff J, et al. Personal protective equipment and intensive care unit healthcare worker safety in the COVID-19 era (PPE-SAFE): an international survey. J Crit Care. (2020) 59:70–5. doi: 10.1016/j.jcrc.2020.06.005
27. Bansal K, Saji S, Mathur VP, Rahul M, Tewari N. A survey of self-perceived physical discomforts and health behaviors related to personal protective equipment of indian dental professionals during COVID-19 pandemic. Int J Clin Pediatric Dentistry. (2021) 14:784–9. doi: 10.5005/jp-journals-10005-2061
28. Davey SL, Lee BJ, Robbins T, Randeva H, Thake CD. Heat stress and PPE during COVID-19: impact on healthcare workers' performance, safety and well-being in NHS settings. J Hospital Infect. (2021) 108:185–8. doi: 10.1016/j.jhin.2020.11.027
29. Çiriş Yildiz C, Ulaşli Kaban H, Tanriverdi FS. COVID-19 pandemic and personal protective equipment: Evaluation of equipment comfort and user attitude. Arch Environ Occupat Health. (2020) 2020:1–8. doi: 10.1080/19338244.2020.1828247
30. Radhakrishnan N, Sudarsan SS, Deepak Raj K, Krishnamoorthy S. Clinical audit on symptomatology of Covid-19 healthcare workers and impact on quality-of-life (QOL) due to continuous facemask usage: a prospective study. Ind J Otolaryngol Head Neck Surgery. (2021) 73:486–93. doi: 10.1007/s12070-021-02530-y
31. Shubhanshu K, Singh A. Prolonged use of N95 mask a boon or bane to healthcare workers during Covid−19 pandemic. Ind J Otolaryngol Head Neck Surg. (2014) 2021:1–4.
32. Bharatendu C, Ong JJ, Goh Y, Tan BY, Chan AC, Tang JZ, et al. Powered Air Purifying Respirator (PAPR) restores the N95 face mask induced cerebral hemodynamic alterations among Healthcare Workers during COVID-19 Outbreak. J Neurol Sci. (2020) 417:117078. doi: 10.1016/j.jns.2020.117078
33. Rosner E. Adverse effects of prolonged mask use among healthcare professionals during COVID-19. J Infect Dis Epidemiol. (2020) 6:130. doi: 10.23937/2474-3658/1510130
34. Bai K, Kumar R, Bhatti U, Rani K, Memon MA. Association of headache and other attributes to duration of wearing face mask during pandemic COVID-19. Pakistan J Physiol. (2021) 17:26–9.
35. Agarwal A, Agarwal S, Motiani P. Difficulties encountered while using PPE kits and how to overcome them: An Indian perspective. Cureus. (2020) 12:e11652. doi: 10.7759/cureus.11652
36. Arif A, Bhatti AM, Iram M, Masud M, Hadi O, Inam SHA. Compliance and difficulties faced by health care providers with variants of face masks, eye protection and face shield. Pakistan J Med Health Sci. (2021) 15:94–7. doi: 10.53350/pjmhs211592215
37. Peres DRV, Monteiro J, Boléo-Tomé JP. Medical masks' and respirators' pattern of use, adverse effects and errors among Portuguese health care professionals during the COVID-19 pandemic: A cross-sectional study. Am J Infect Control. (2022) 50:618–23. doi: 10.1016/j.ajic.2021.10.002
38. Cigiloglu A, Ozturk E, Ganidagli S, Ozturk ZA. Different reflections of the face mask: sleepiness, headache and psychological symptoms. Int J Occupat Safety Ergonomics. (2021) 22:1–6. doi: 10.1080/10803548.2021.1984712
39. Ipek S, Yurttutan S, Güllü UU, Dalkiran T, Acipayam C, Doganer A. Is N95 face mask linked to dizziness and headache? Int Arch Occupat Environ Health. (2021) 94:1627–36. doi: 10.1007/s00420-021-01665-3
40. Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immunity. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
41. Sharif S, Amin F, Hafiz M, Benzel E, Peev N, Dahlan RH, et al. COVID 19–depression and neurosurgeons. World Neurosurg. (2020) 140:e401–10. doi: 10.1016/j.wneu.2020.06.007
42. Yifan T, Ying L, Chunhong G, Jing S, Rong W, Zhenyu L, et al. Symptom cluster of ICU nurses treating COVID-19 pneumonia patients in Wuhan, China. J Pain Sympt Manage. (2020) 60:e48–53. doi: 10.1016/j.jpainsymman.2020.03.039
43. Lim E, Seet R, Lee KH, Wilder-Smith E, Chuah B, Ong B. Headaches and the N95 face-mask amongst healthcare providers. Acta Neurol Scand. (2006) 113:199–202. doi: 10.1111/j.1600-0404.2005.00560.x
44. Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Impact of personal protective equipment use on health care workers' physical health during the COVID-19 pandemic: a systematic review and meta-analysis. Am J Infect Control. (2021) 49:1305–15. doi: 10.1016/j.ajic.2021.04.084
45. Swaminathan R, Mukundadura BP, Prasad S. Impact of enhanced personal protective equipment on the physical and mental well-being of healthcare workers during COVID-19. Postgraduate Med J. (2022) 98:231–3. doi: 10.1136/postgradmedj-2020-139150
46. Krymchantowski AV. Headaches due to external compression. Curr Pain Headache Rep. (2010) 14:321–4. doi: 10.1007/s11916-010-0122-x
47. Romero JGdAJ, de Salles-Neto FT, Stuginski-Barbosa J, Conti PCR, Almeida-Leite CM. COVID-19 pandemic impact on headache in healthcare workers: a narrative review. Headache Med. (2021) 2021:75–82. doi: 10.48208/HeadacheMed.2021.17
48. Scarano A, Inchingolo F, Rapone B, Festa F, Rexhep Tari S, Lorusso F. Protective face masks: Effect on the oxygenation and heart rate status of oral surgeons during surgery. Int J Environ Res Public Health. (2021) 18:2363. doi: 10.3390/ijerph18052363
49. Blumenfeld A, Ashkenazi A, Napchan U, Bender SD, Klein BC, Berliner R, et al. Expert consensus recommendations for the performance of peripheral nerve blocks for headaches–a narrative review. Headache. (2013) 53:437–46. doi: 10.1111/head.12053
50. Waldie KE, Welch D. Cognitive function in tension-type headache. Curr Pain Headache Rep. (2007) 11:454–60. doi: 10.1007/s11916-007-0233-1
51. Moore DJ, Keogh E, Eccleston C. Headache impairs attentional performance. PAIN®. (2013) 154:1840–5. doi: 10.1016/j.pain.2013.06.006
52. Chirico F, Nucera G, Sacco A, Magnavita N. Proper respirators use is crucial for protecting both emergency first aid responder and casualty from COVID-19 and airborne-transmitted infections. Adv Respirat Med. (2021) 89:99–100. doi: 10.5603/ARM.a2021.0028
Keywords: headache, personal protective equipment, health care workers, respiratory mask, COVID-19
Citation: Sahebi A, Hasheminejad N, Shohani M, Yousefi A, Tahernejad S and Tahernejad A (2022) Personal protective equipment-associated headaches in health care workers during COVID-19: A systematic review and meta-analysis. Front. Public Health 10:942046. doi: 10.3389/fpubh.2022.942046
Received: 12 May 2022; Accepted: 20 September 2022;
Published: 12 October 2022.
Edited by:
Susana Viegas, New University of Lisbon, PortugalReviewed by:
Francesco Chirico, Catholic University of the Sacred Heart Rome, ItalyMahdi Malakoutikhah, Kashan University of Medical Sciences, Iran
Copyright © 2022 Sahebi, Hasheminejad, Shohani, Yousefi, Tahernejad and Tahernejad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Somayeh Tahernejad, tahernezhad.somaye@gmail.com
 Ali Sahebi
Ali Sahebi Naser Hasheminejad2
Naser Hasheminejad2 Somayeh Tahernejad
Somayeh Tahernejad