- 1Department of Laboratory Medicine, West China Second University Hospital, Sichuan University, Chengdu, China
- 2Key Laboratory of Birth Defects and Related Diseases of Women and Children, Sichuan University, Ministry of Education, Chengdu, China
Neurosyphilis is a chronic infectious disease caused by the invasion of Treponema pallidum into the central nervous system. In recent years, with the increase in the latent syphilis infection rate, the incidence of neurosyphilis has gradually increased, the typical symptoms of neurosyphilis have decreased, atypical manifestations have increased, and the clinical manifestations have become increasingly diverse. Cerebrospinal fluid testing plays an important role in the diagnosis of neurosyphilis. In recent years, there have been many advances in cerebrospinal fluid testing. This review focuses on the current and potential laboratory indicators of neurosyphilis in cerebrospinal fluid, aiming to provide a reference for clinical application and ideas for future experimental research of neurosyphilis.
Introduction
Syphilis is a chronic infectious disease caused by Treponema pallidum (T. pallidum), and humans are the only host. T. pallidum is highly neuroinvasive and can invade the central nervous system and result in neurosyphilis at any time after the initial infection. Studies have shown that T. pallidum can disseminate to the central nervous system of rabbits within hours to days after inoculation (1). In recent years, with the increasing prevalence of syphilis around the world, the incidence of neurosyphilis has also increased markedly each year (2).
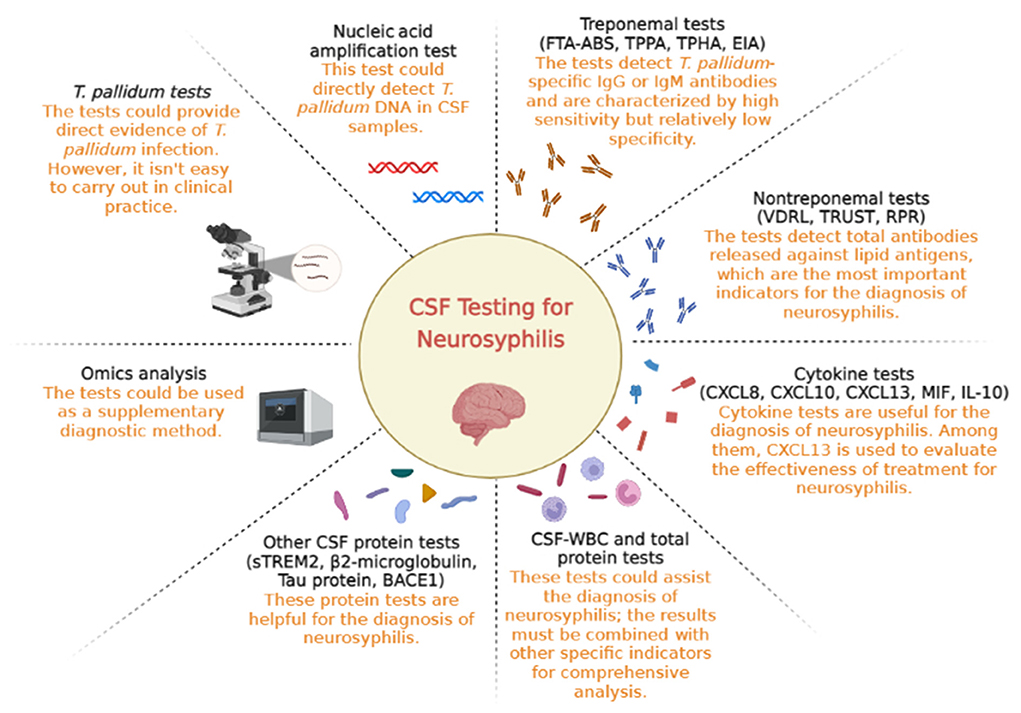
Neurosyphilis varies according to the infection period and central site of infection. In the early stage of infection, T. pallidum mainly invades meningeal nerves and meningeal blood vessels, which could cause meningitis, cranial nerve damage, multiple nerve root disease and meningeal damage. Meningeal vascular damage mainly manifests as occlusive cerebrovascular syndrome, which can occur as hemiplegia, aphasia, or epileptic seizures. In the late stage of infection, T. pallidum further invades the brain parenchyma, resulting in clinical manifestations such as paralytic dementia and spinal tuberculosis. T. pallidum can also cause symptoms of optic nerve and auditory nerve damage, which are known as ocular syphilis and ear syphilis (3). There is no clear time point that marks the division between early and late neurosyphilis. Different types of neurosyphilis are manifestations of different time periods of the disease, and there is often partial overlap. The diagnostic model for neurosyphilis has limitations. To date, there is no commonly accepted gold standard test for neurosyphilis diagnosis, and the algorithms used for the diagnosis of neurosyphilis vary between countries. Cerebrospinal fluid (CSF) testing plays a very important role in the diagnosis of neurosyphilis. In recent years, there has been progress in developing new biomarkers for CSF testing, and these biomarkers are helpful for neurosyphilis diagnosis (see Figure 1). This review summarizes the current and potential laboratory indicators in CSF testing to provide a reference for the diagnosis of neurosyphilis.
Pathological testing for T. pallidum in CSF
Dark-field examination, direct immunofluorescence and silver staining
The three methods of dark-field examination, direct immunofluorescence and silver staining are often used to detect T. pallidum in chancroid lesions or regional lymph nodes that are enlarged in syphilis. Because the lesions contain large numbers of treponemes, the positivity rate and specificity are high. However, the volume of CSF that can be used for testing is low, and the number of T. pallidum in CSF is low, resulting in the low sensitivity of the methods mentioned above. Therefore, these methods are difficult to use for the clinical diagnosis of neurosyphilis (4).
Rabbit infection test
Traditionally, the reference method for the direct detection of T. pallidum was the rabbit infection test (RIT). First, the CSF of an individual suspected of having neurosyphilis was injected into the testes of normal New Zealand rabbits. One week after inoculation, the testicular size of rabbits was examined, and blood was used for serological testing (Treponema pallidum particle agglutination (TPPA) test and rapid plasma response (RPR) test). If the results of the rabbit serological tests were positive, the animal was considered positive. CSF-RIT could provide direct evidence of T. pallidum invasion of the nervous system (4). However, due to the time-consuming, expensive and cumbersome nature of CSF-RIT, it is difficult to carry out in clinical practice. With the abuse of antibiotics, CSF-RIT sensitivity has been further reduced, and this method is used only for laboratory research. Tong et al. found that RIT was no longer highly sensitive for the detection of T. pallidum in clinical samples and was not considered adequate as a reference method for measuring the sensitivity of other methods in the current era (5). In addition, recent research has revealed the viability of the long-term continuous propagation of T. pallidum in vitro. However, this methodology is also cumbersome and time-consuming (6). Therefore, it is undeniable that RIT is useful for recovering T. pallidum from infected tissues and maintaining its survival for scientific studies.
Nucleic acid amplification test
Due to the biological characteristics of T. pallidum and the performance restrictions of RIT and dark-field observation, it is difficult to culture T. pallidum in vitro. Therefore, microbiological examination of T. pallidum is not possible to use for diagnosing neurosyphilis. With the development of science and technology, the detection of pathogen nucleic acids by nucleic acid amplification tests (NAATs) is becoming increasingly important in the detection of infectious disease pathogens. Molecular assays with NAATs of T. pallidum DNA are used for direct detection to improve diagnostic sensitivities. There are various NAATs, such as PCR, nested PCR, quantitative PCR, and reverse transcriptase PCR (4). Villanueva et al. found that different storage temperatures and length of time after CSF specimen collection had little effect on the stability of PCR products used to detect T. pallidum in CSF. This result indicates that CSF-PCR may have important clinical value in the diagnosis of neurosyphilis (7). Various T. pallidum genes have been used for NAATs, including those encoding treponemal surface or subsurface lipoproteins (such as the DNA polymerase I gene [i.e., polA], T. pallidum 47 kDa lipoprotein [Tp47], subsurface lipoprotein 4D [4D], treponemal membrane protein A [tmpA] and basic membrane protein [bmp]) (8–10). Among these targets, the most frequently described and evaluated target genes are Tp47 and polA.
Direct detection of T. pallidum DNA in CSF by NAATs has been assessed as a potential additional tool for the diagnosis of neurosyphilis. A total of 124 patients with positive T. pallidum serological results were recruited and classified according to the 2008 European syphilis management guidelines. Among these patients, Tp47 and polA NAATs were positive in 25 (76%) and 23 (70%) of 33 neurosyphilis patients and 12 (13%) and 7 (8%) of 91 patients without neurosyphilis, respectively (11). Another prospective study evaluated the diagnostic value of nested PCR for the detection of T. pallidum in CSF specimens. The nested PCR assay had an overall sensitivity of 42.5%, a specificity of 97%, a positive predictive value of 77%, and a negative predictive value of 86%. These results suggest that PCR is highly specific and has potential value when used together with other neurosyphilis indicators (12).
However, in a recent study, the CSF-PCR results of 8 patients with clinically diagnosed neurosyphilis were negative, suggesting that the clinical application of these methods is still far in the future (13). Another meta-analysis related to CSF-PCR showed that the sensitivity of PCR for the definitive diagnosis of neurosyphilis varied from 40 to 70%, and the specificity ranged from 60 to 100%. Tp47 is the most commonly used target gene in PCR assays, with an overall sensitivity of 68% and a specificity of 91.9%, which were lower than those of the treponemal test (14). Currently, the use of a CSF-PCR assay to detect T. pallidum DNA requires further study. The low detection rate might be because T. pallidum is less abundant in the CSF of neurosyphilis patients. On the one hand, the time and clinical features of T. pallidum invasion into the nervous system should be explored. On the other hand, methods to improve the DNA detection rate in specimens with low T. pallidum loads should be studied. Recent studies have shown that digital PCR, detecting trace genes, can detect T. pallidum DNA in saliva, and there is no significant difference in the detection rate between saliva and plasma. Whether this technique could be used for the detection of T. pallidum DNA in CSF remains to be further studied (15).
Non-treponemal tests
Non-treponemal tests detect total antibodies (IgM and IgG) released against lipid antigens (e.g., cardiolipin and lecithin) and non-specific antibodies produced by T. pallidum surface lipids after T. pallidum infection of host cells. The non-treponemal tests mainly include the venereal disease research laboratory (VDRL) test, toluidine red unheated serum test (TRUST) and RPR test (16). The measuring principles and processes of these tests, which involve quantitative detection through continuous dilution of serum, are similar, and the results are reported by titer. These three tests could be used for CSF detection in neurosyphilis patients.
The CSF-VDRL test has been considered the gold standard for neurosyphilis diagnosis for a long time and is the main diagnostic test for neurosyphilis in domestic and foreign guidelines (17–21). It is generally believed that the CSF-VDRL test has high specificity but low sensitivity for the diagnosis of neurosyphilis. A meta-analysis showed that the sensitivity of the CSF-VDRL test was 49–87%, and the specificity was 74–100% for diagnosis (22). The proportion of positive CSF-VDRL tests was higher in neurosyphilis patients who were infected by human immunodeficiency virus (HIV) (23). Performing the VDRL test is complicated; the reagent must be prepared before testing, the specimen must be tested within 2 h after collection, and the results are observable only by optical microscopy. Furthermore, other diseases might influence VDRL results. A case report described a false-positive CSF-VDRL test result in a patient with central nervous system malignancies (24). CSF contamination by blood (which may occur in situations such as craniocerebral trauma) may lead to false-positive CSF-VDRL test results in patients with syphilis (25).
The RPR test uses the same antigen as the VDRL test except it is bound to carbon particles and uses charcoal particles as the visualizing agent. Studies have reported that the CSF-RPR test sensitivity ranged from 51.5 to 81.8%, and the specificity ranged from 81.8 to 100% (26, 27). The TRUST is similar to the RPR test but uses toluidine red as the visualizing agent rather than charcoal. It has been reported that CSF-TRUST sensitivity ranges from 58.9 to 82.5%, and specificity ranges from 82.1 to 93.1% (27). The operation of the RPR test and TRUST is simple, and the results are stable and can be observed by the naked eye without a microscope.
One study focused on the performance of a non-treponemal test in CSF neurosyphilis specimens and found that the sensitivity and specificity of the CSF-VDRL test, CSF-RPR test and CSF-TRUST were similar. Therefore, the CSF-RPR test and CSF-TRUST could be considered alternative tests for neurosyphilis in HIV-negative patients, especially when the CSF-VDRL test is unavailable (27). However, another study showed that CSF-RPR test sensitivity and specificity are lower than those of the CSF-VDRL test (26).
At present, there is no unified view on the sensitivity and specificity of the CSF-VDRL test, CSF-RPR test and CSF-TRUST, and it is unlikely that the role of the CSF-VDRL test could be completely replaced by the CSF-RPR test and CSF-TRUST in the diagnosis of neurosyphilis. There are also some different opinions about the role of CSF non-treponemal tests in the diagnosis of neurosyphilis among different country guidelines. The guidelines for the Treatment of Sexually Transmitted Diseases of the United States Centers for Disease Control and Prevention (CDC) emphasize that CSF-VDRL test positivity could be used as an important diagnostic criterion for symptomatic neurosyphilis patients, but CSF-VDRL test negativity does not exclude a neurosyphilis diagnosis (28). The European Syphilis Management Guidelines suggest that CSF-VDRL/RPR test positivity could diagnose neurosyphilis (20). CSF-VDRL test abnormalities have been included in the diagnostic criteria of neurosyphilis in the Chinese Guidelines for Diagnosis and Treatment of Syphilis. The Chinese and European Guidelines pointed out that the CSF-TRUST or CSF-RPR test could be used to replace the CSF-VDRL test in the absence of these conditions (17, 20).
CSF non-treponemal test results are the most important indicators for the diagnosis of neurosyphilis at present. However, this test is difficult to automate, the results observed by the naked eye are relatively subjective, and the sensitivity is not high. Biological false positives due to cross reactivity may be related to various infectious and non-infectious diseases, and the anterior band phenomenon may cause false-negative results. Therefore, it is necessary to determine more sensitive laboratory indicators as supplementary tests for CSF non-treponemal tests.
Treponemal tests
Treponemal tests use T. pallidum extract or recombinant T. pallidum protein as a specific antigen to detect serum anti-T. pallidum IgG or IgM antibodies. At present, treponemal tests mainly include the fluorescent treponemal antibody absorption (FTA-ABS) test, Treponema pallidum haemagglutination assay (TPHA), TPPA test and enzyme immunoassay (EIA). The FTA-ABS, TPHA and TPPA tests are used to detect total antibodies against T. pallidum antigen. EIA mainly detects IgG and IgM antibodies against recombinant T. pallidum proteins (such as TpN15, TpN17 and TpN47). The tests mentioned above can be used to detect anti-T. pallidum IgG or IgM antibodies in CSF. Studies have reported that the sensitivity of the CSF-FTA-ABS test is 90.9–100%, and the specificity is 100% (29–31). It has been reported that the CSF-TPPA test sensitivity is 75.6–95%, and the specificity ranges from 85.5 to 100% (31–33). One study showed that the diagnostic specificity of a CSF-TPPA titer ≥1:640 was significantly higher than that of lower dilutions and was not significantly different from that of the CSF-VDRL test (31). There was no significant difference in CSF-TPPA test results between HIV-infected and non-infected neurosyphilis patients (31). The TPHA test is similar to the TPPA test, and a study has shown that a CSF-TPHA titer ≥1:640 is specific for the diagnosis of neurosyphilis (34). The CSF-FTA-ABS test requires fluorescence microscope observation, while the TPHA and TPPA tests are simpler flocculation tests, and the results can be observed by the naked eye.
One study revealed the performance of EIA tests in detecting CSF specimens. The Trep-Sure and Maxi-Syph tests measure both IgG and IgM anti-treponemal antibodies. The sensitivity of Trep-Sure was 92.9%, the sensitivity of Maxi-Syph was 100%, and the specificity of both tests was 100% (32). Although the results showed high sensitivity and specificity of the CSF-EIA test in the diagnosis of neurosyphilis, it is worth noting that there were few samples, and the data in this study were limited. In addition, a systematic review of CSF treponemal tests for neurosyphilis indicated that there were significant differences in the sensitivity and specificity of treponemal tests in different studies (35).
Because the anti-treponemal IgG antibody can cross the blood–brain barrier and enter the CSF, which causes false positives in treponemal tests, it is considered to be a controversial indicator in the diagnosis of neurosyphilis (33). Therefore, the diagnosis of neurosyphilis could be excluded in syphilis patients with negative treponemal tests according to the guidelines for the diagnosis and treatment of syphilis in the United States and Europe. The Chinese guideline takes CSF-FTA-ABS test results as a diagnostic indicator of neurosyphilis and points out that the CSF-TPPA test could be used to replace the CSF-FTA-ABS test in the absence of these conditions. The CSF treponemal test plays an important role in the diagnosis of neurosyphilis, and it is characterized by high sensitivity but relatively low specificity. The positive results need to be evaluated along with clinical manifestations, such as the CSF-VDRL test results and the CSF white blood cell count and protein quantity, to better diagnose neurosyphilis.
Cytokine tests
Chemotactic factor tests
Chemokines are small cytokines or signaling proteins secreted by cells. Chemokines and their receptors are expressed in the neurons and glial cells of the central nervous system. Increased levels of chemokines in CSF were found to be associated with the severity or progression of inflammatory diseases of the central nervous system. Chemokines are the most studied cytokines as potential CSF indicators in neurosyphilis patients, among which CXCL13 has been studied extensively and intensively. The concentrations of CXCL13, CXCL10, and CXCL8 were increased in the CSF of neurosyphilis patients, which was related to the CSF protein concentration and the CSF-VDRL titer. The sensitivity/specificity of CXCL13, CXCL10, and CXCL8 in the diagnosis of neurosyphilis were 85.4/89.1%, 79/90.1%, and 79.6/91.1%, respectively (36). Furthermore, there was no correlation between serum and CSF concentrations of CXCL13, which means that the increased CSF CXCL13 level is the result of enhanced synthesis of nervous system cells (37). Some studies have defined asymptomatic neurosyphilis as CSF-VDRL positivity or CSF WBC count > 20 × 106/L and defined symptomatic neurosyphilis as visual or hearing loss. It was found that CSF CXCL13 ≥250 pg/mL had a sensitivity of 41% for both asymptomatic and symptomatic neurosyphilis and a specificity of 93 and 79%, respectively (38). Another study defined neurosyphilis as CSF-VDRL or CSF-TRUST positive results and CSF WBC count >10 × 106/L and/or protein level higher than 500 mg/L. The results showed that the diagnostic sensitivity of CSF CXCL13 concentration ≥13.37 pg/mL in neurosyphilis patients was 84.9%, and the specificity was 78.87% (39). HIV infection can slightly increase CSF CXCL13 concentration, which is negligible in the case of a large increase in CSF CXCL13 concentration in neurosyphilis patients (40). Another study indicated that CSF CXCL13 is more suitable for the diagnosis of neurosyphilis patients with HIV infection (41). At present, CSF CXCL13 is considered to be a potential indicator of the antibiotic treatment response and is used to evaluate the effectiveness of treatment for neurosyphilis (39). However, it is noteworthy that the sensitivity and specificity of CSF CXCL13 are different in neurosyphilis due to the different diagnostic criteria, population characteristics and cut-off values of CSF CXCL13. Further studies are needed to support the diagnostic value of CSF CXCL13.
Macrophage migration inhibitory factor test
Macrophage migration inhibitory factor (MIF) is a multieffect immunoregulatory cytokine with a unique structure. MIF plays an important role in innate immunity, immune cell recruitment and inflammation. Therefore, it has become a relevant indicator of the inflammatory response in various diseases. MIF is a key indicator of central nervous system infection. Studies have shown that the sensitivity of CSF MIF concentration for neurosyphilis diagnosis was 74.42%, and the specificity was 67.74% (42). The MIF level was higher in the CSF of neurosyphilis patients than in syphilis/non-neurosyphilis patients. MIF has been considered a new potential CSF indicator to establish or exclude the diagnosis of neurosyphilis, but further study is needed.
Interleukins
Interleukins are cytokines produced by multiple cells that act on multiple cells. Interleukins play an important role in immune function modulation. Studies have shown that the level of IL-17A in the CSF of patients with asymptomatic neurosyphilis is significantly higher than that in patients without neurosyphilis (43). In another study, researchers detected changes in IL-1β, IL-4, IL-6, IL-10, IL-17A and IL-21 levels in the CSF of neurosyphilis patients before penicillin treatment. The results showed that only IL-10 was significantly increased. The sensitivity/specificity of CSF IL-10 in neurosyphilis and asymptomatic neurosyphilis were 86.7/91.7% and 83.3/91.7%, respectively. It is suggested that the CSF IL-10 concentration is useful for the diagnosis of neurosyphilis, especially for asymptomatic neurosyphilis patients. Furthermore, it was found that the CSF IL-10 level was positively correlated with the level of neuronal damage markers, the CSF protein concentration, the CSF white blood cell count and the CSF-RPR titer in neurosyphilis patients. These results suggested that excessive CSF IL-10 might promote the further development of neurosyphilis (44). However, the number of patients included in the above two studies was small. The diagnosis of neurosyphilis with interleukins as a single indicator lacks specificity, and the various interleukins can be elevated in intracranial infection. Therefore, it is necessary to combine CSF indicators for neurosyphilis diagnosis.
CSF white blood cells and total protein tests
The CSF white blood cell (WBC) count and total protein test, as traditional laboratory indicators for the diagnosis of central nervous system infection, also play an important role in the diagnosis of neurosyphilis. Abnormalities in the routine biochemical examination of CSF are considered important laboratory evidence for the diagnosis of neurosyphilis in many national guidelines. The European guidelines for the diagnosis and treatment of neurosyphilis specifically suggest that CSF examination must include total protein, monocyte count, and treponemal and non-treponemal tests. If there is an abnormal CSF examination result (high protein levels and/or increased number of cells), CSF analysis must be repeated after treatment (6 weeks-6 months) (45). The American guidelines suggest that neurosyphilis should also be considered if the CSF-VDRL result is negative but the patient has neurological symptoms and/or signs, positive serological tests for syphilis, and abnormal CSF white blood cell count and/or protein levels. If neurosyphilis patients are coinfected with HIV, CSF WBC counts are usually elevated (>5 × 106/L), with >20 × 106/L used as the cut-off value to improve the specificity of neurosyphilis diagnosis (19). In the Chinese guidelines, neurosyphilis can be diagnosed in syphilis patients who meet the following two criteria: (1) CSF white blood cell count ≥5 × 106/L (combined with HIV infection, white blood cell count is often >20 × 106/L) and protein > 500 mg/L, with no other evident causes of these abnormalities. (2) Positive CSF-VDRL test (or RPR test/TRUST) or FTA-ABS test (or TPPA/TPHA test) (17). Another study has shown that the more WBCs there are in the CSF of neurosyphilis patients, the higher the total protein level and the worse the prognosis, suggesting that CSF WBCs and total protein are of great significance in judging the progress of neurosyphilis (46). However, CSF WBC count and total protein level lack specificity. The protein levels and the number of monocytes in the CSF of neurosyphilis patients may be normal, and a large number of monocytes in the CSF could be observed in many cases, including HIV infection without syphilis. Therefore, CSF WBC count and total protein level can only assist the diagnosis of neurosyphilis, and the results must be combined with other specific indicators for a comprehensive analysis.
Other CSF protein tests
Tau protein
Tau protein is the main microtubule-associated protein in neurons and is located mostly in the axons of neurons. A study found that there was a significant difference in CSF Tau protein content between neurosyphilis and Alzheimer's disease patients. The Tau protein level in the CSF of neurosyphilis patients was significantly higher than that of non-neurosyphilis patients, suggesting that Tau protein is helpful for the diagnosis of neurosyphilis with a history of syphilis and cognitive decline (47, 48). However, Tau protein is an acute-phase reactive protein that is increased to different degrees in a variety of neurological diseases, especially neurodegenerative diseases, with low specificity (49). Whether Tau protein can be an indicator of neurosyphilis needs further study.
β-amyloid precursor protein lyase
β-Amyloid precursor protein lyase (BACE1) is a key enzyme responsible for the cleavage of pathological amyloid β-protein precursors (50). The study found that plasma BACE1 levels were significantly correlated with CSF BACE1 levels in the neurosyphilis group. Therefore, plasma BACE1 may be a promising biomarker for early diagnosis (48).
Triggering receptor expressed on bone marrow cells 2
Triggering receptor expressed on bone marrow cells 2 (TREM2) is a cell surface receptor protein. For the brain, the focus is on the expression of TREM2 in microglia, which promotes phagocytosis, inhibits toll-like receptor-induced inflammatory cytokine production, and enhances anti-inflammatory cytokine transcription in vitro (51, 52). Its soluble variant (sTREM2) can be detected in CSF. Studies have found that the level of CSF sTREM2 was significantly higher in neurosyphilis patients than in syphilis/non-neurosyphilis patients, and sTREM2 levels were higher in late neurosyphilis than in early neurosyphilis, suggesting that sTREM2 can provide a basis for the clinical prognosis of neurosyphilis (53).
β2-microglobulin
β2-microglobulin is a protein composed of 11 polypeptide chains that is one of the light chain components of major histocompatibility complex class I molecules and is associated with aging-related cognitive impairment and Alzheimer's disease (54). The level of β2-microglobulin in normal CSF is very low. If the concentration of β2-microglobulin in CSF increases, it indicates that there is pathological damage in the central nervous system. Studies have found that the expression of β2-microglobulin in the CSF of children with congenital syphilis increases significantly, and the level of β2-microglobulin gradually decreases to normal after corresponding treatment. These results suggest that β2-microglobulin is very useful in the diagnosis of congenital syphilis central nervous system injury and in monitoring the response to treatment (55).
Omics analysis
CSF metagenome sequencing analysis
Increasing data have shown that metagenomic sequencing can play a role in neurological infectious diseases (such as unexplained encephalitis and meningitis), and metagenomic next-generation sequencing (mNGS) analysis of CSF can quickly detect pathogens. A recent study showed that T. pallidum in CSF was detectable by metagenomic sequencing. However, it is difficult to use metagenomic sequencing as a conventional screening tool due to its high cost. For neurosyphilis patients with atypical symptoms or negative results as detected by conventional methods, mNGS could be used as a supplementary diagnostic method.
CSF metabolomics analysis
Metabolomics is a quantitative analysis of all metabolites in organisms and a search for the relative relationship between metabolites and physiological and pathological changes. Metabolomics provides a large amount of information on energy metabolism, physiology and possible pathogen diagnostic biomarkers and intervention strategies. A metabolic analysis of CSF in patients with neurosyphilis showed that bilirubin, L-histidine, prostaglandin E2, α-mannuronic acid, butyryl L-carnitine and palmitoyl L-carnitine were significantly increased in the CSF of neurosyphilis patients. The metabolism of CSF may provide a new way to explore the pathogenesis of neurosyphilis (56). In another study, several metabolites in the CSF of neurosyphilis patients were found to be significantly altered, including d-mannitol, N-acetyl-tyrosine, hypoxanthine and s-methyl-5'-adenosine, and N-acetyl-tyrosine was 87.4 and 7.5 times higher in the CSF of neurosyphilis patients than in that of non-secondary syphilis patients and non-syphilis patients, respectively. However, the metabolites in the CSF of neurosyphilis patients lack specificity, and the types of metabolites reported in different studies are not consistent. Whether these metabolites can be new potential markers of neurosyphilis needs further evaluation and study (57).
Conclusions
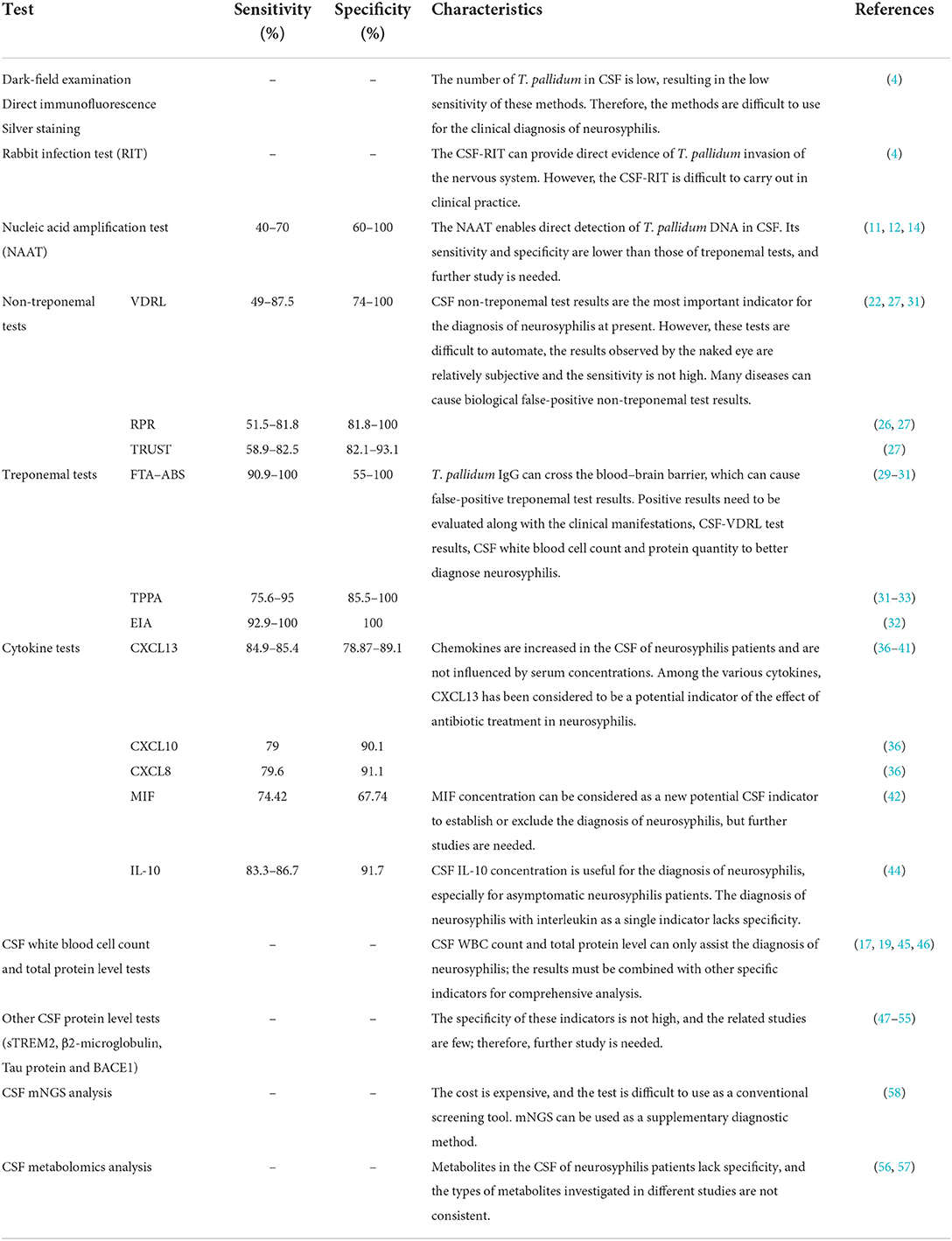
At present, the diagnosis of neurosyphilis is mainly based on the patient's epidemiological history, clinical manifestations and laboratory tests. Elevated CSF WBC count and total protein level are an important basis for suspected neurosyphilis, but the existing diagnosis cannot meet clinical needs. The sensitivity and specificity of non-treponemal and treponemal tests are different. Because the existing laboratory tests cannot meet clinical needs, the diagnosis of neurosyphilis still faces challenges. With the development of related technologies, new methods and biomarkers have emerged for CSF detection in neurosyphilis. Detecting T. pallidum DNA in CSF by NAATs has gradually become possible, and CSF cytokines as indicators for neurosyphilis diagnosis continue to be defined. CSF CXCL13, which shows good diagnostic efficacy, is most likely to be applied in clinical practice. Interleukin, MIF, Tau protein, BACE1, sTREM2, and β2-microglobulin and metagenomic and metabolomic factors are considered to be potential markers in the CSF detection of neurosyphilis. However, the specificity of these indicators is not high, and the related studies are few; therefore, further study is needed (see Table 1). In conclusion, no single test can diagnose all cases of neurosyphilis. Generally, the diagnosis of neurosyphilis is based on clinical manifestations and CSF tests. The CSF tests should include non-treponemal and treponemal tests and CSF white blood cell count and total protein level tests. If necessary, NAATs, cytokine tests and other CSF protein tests should be performed to assist the diagnosis of neurosyphilis. Furthermore, new diagnostic markers with high sensitivity and specificity are needed. Carrying out high-quality multicentre clinical research is very important for future neurosyphilis laboratory diagnostic Studies.
Author contributions
L-WP designed and edited the manuscript. Z-XG wrote the paper. YG and X-QL collected and analyzed the data. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Foundation (grant number: 21H1219). The funders played no role in the study design, data collection and analyses, decision to publish, or manuscript preparation.
Acknowledgments
We thank Professor Tian-ci Yang and Li-Rong Lin for their guidance of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Collart P, Franceschini P, Durel P. Experimental rabbit syphilis. Br J Venereal Dis. (1971) 47:389–400. doi: 10.1136/sti.47.6.389
2. Tan X, Zhang J, Li J, Yue X, Gong X. The prevalence of asymptomatic neurosyphilis among HIV-negative serofast patients in China: a meta-analysis. PLoS ONE. (2020) 15: e0241572. doi: 10.1371/journal.pone.0241572
4. Theel ES, Katz SS, Pillay AJCID. Molecular and direct detection tests for Treponema pallidum subspecies pallidum: a review of the literature 1964–2017. Clin Infect Dis. (2020) 71: S4–S12. doi: 10.1093/cid/ciaa176
5. Tong ML, Zhang HL, Zhu XZ, Fan JY, Gao K, Lin LR. et al. Re-evaluating the sensitivity of the rabbit infectivity test for Treponema pallidum in modern era. Clinica Chimica Acta. (2016) 464:136–41. doi: 10.1016/j.cca.2016.11.031
6. Edmondson DG, Hu B, Norris SJ. Long-term in vitro culture of the syphilis spirochete Treponema pallidum subsp. Pallidum MBio. (2018) 9:e01153–18. doi: 10.1128/mBio.01153-18
7. Villanueva AV, Podzorski RP, Reyes MP. Effects of various handling and storage conditions on stability of Treponema pallidum DNA in cerebrospinal fluid. J Clin Microbiol. (1998) 36:2117–9. doi: 10.1128/JCM.36.7.2117-2119.1998
8. Rodes B, Liu H, Johnson S, George R, Steiner B. Molecular cloning of a gene (polA) coding for an unusual DNA polymerase I from Treponema pallidum. J Med Microbiol. (2000) 49:657–67. doi: 10.1099/0022-1317-49-7-657
9. Noordhoek GT, Wolters EC, De Jonge ME, Van Embden JD. Detection by polymerase chain reaction of Treponema pallidum DNA in cerebrospinal fluid from neurosyphilis patients before and after antibiotic treatment. J Clin Microbiol. (1991) 29:1976–84. doi: 10.1128/jcm.29.9.1976-1984.1991
10. Radolf JD, Fehniger TE, Silverblatt FJ, Miller JN, Lovett MA. The surface of virulent Treponema pallidum: resistance to antibody binding in the absence of complement and surface association of recombinant antigen 4D. Infect Immun. (1986) 52:579–85. doi: 10.1128/iai.52.2.579-585.1986
11. Castro R, Águas MJ, Batista T, Araújo C, Mansinho K, Pereira FD. Detection of Treponema pallidum Sp. Pallidum DNA in cerebrospinal fluid (CSF) by two PCR techniques. J Clin Lab Anal. (2016) 30:628–32. doi: 10.1002/jcla.21913
12. Vanhaecke C, Grange P, Benhaddou N, Blanche P, Salmon D, Parize P, et al. Clinical and biological characteristics of 40 patients with neurosyphilis and evaluation of Treponema pallidum nested polymerase chain reaction in cerebrospinal fluid samples. Clin Infect Dis. (2016) 63:1180–6. doi: 10.1093/cid/ciw499
13. Smit D, De Graaf M, Meyer D, de Groot-Mijnes JD. Immunoblot and polymerase chain reaction to diagnose ocular syphilis and neurosyphilis in HIV-positive and HIV-negative patients. Ocul Immunol Inflamm. (2020) 28:1049–55. doi: 10.1080/09273948.2019.1698753
14. Marks M, Lawrence D, Kositz C, Mabey D. Diagnostic performance of PCR assays for the diagnosis of neurosyphilis: a systematic review. Sexually Trans infect. (2018) 94:053666. doi: 10.1136/sextrans-2018-053666
15. Wang C, Hu Z, Zheng X, Ye M, Liao C, Shang M, et al. A new specimen for syphilis diagnosis: evidence by high loads of Treponema pallidum DNA in saliva. Clin Infect Dis. (2021) 73:e3250–e3258. doi: 10.1093/cid/ciaa1613
16. Peeling RW, Mabey D, Kamb ML, Chen XS. Justin D. Radolf4 and Adele S. Benzaken5 Abstract| Treponema pallidum subspecies pallidum (T. pallidum) causes syphilis via sexual exposure or via vertical transmission during pregnancy. T. pallidum is renowned for its invasiveness and immune-evasiveness; its clinical manifestations result from local inflammatory responses to replicating. Syphilis. (2017) 2:448–9. doi: 10.1038/nrdp.2017.73
17. Wang QQ. Guidelines for diagnosis and treatment of syphilis, gonorrhea and genital Chlamydia trachomatis infection (2020). Chin J Dermatol. (2020) 53:168–79. doi: 10.35541/cjd.20190808
18. Klein M, Angstwurm K, Esser S, Hahn K, Maschke M, Scheithauer S, et al. German guidelines on the diagnosis and treatment of neurosyphilis. Neurol Res Pract. (2020) 2020:33. doi: 10.1186/s42466-020-00081-1
19. Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. (2021) 70:1–187. doi: 10.15585/mmwr.rr7004a1
20. Janier M, Unemo M, Dupin N, Tiplica GS, Potočnik M, Patel R. 2020 European guideline on the management of syphilis. J Eur Acad Dermatol Venereol. (2021) 35:574–88. doi: 10.1111/jdv.16946
21. Wong T, Fonseca K, Chernesky MA, Garceau R, Levett PN, Serhir B. Canadian public health laboratory network laboratory guidelines for the diagnosis of neurosyphilis in Canada. Can J Infect Dis Med Microbiol Immunol. (2015) 26:18A−22A. doi: 10.1155/2015/167484
22. Tuddenham S, Katz SS, Ghanem KG. Syphilis laboratory guidelines: performance characteristics of non-treponemal antibody tests. Clin Infect Dis. (2020) 71:S21–42. doi: 10.1093/cid/ciaa306
23. Martins RT, Castilhos RM, da Silva PS, Costa LS. Frequency of screening and prevalence of neurosyphilis in stroke population. Cerebrovas Dis. (2020) 49:301–6. doi: 10.1159/000508491
24. Madiedo G, Ho KC, Walsh P. False-positive VDRL and FTA in cerebrospinal fluid. J Am Med Assoc. (1980) 244:688–9. doi: 10.1001/jama.244.7.688
25. Izzat NN, Bartruff JK, Glicksman JM, Holder WR, Knox JM. Validity of the VDRL test on cerebrospinal fluid contaminated by blood. Br J Vener Dis. (1971) 47:162–4. doi: 10.1136/sti.47.3.162
26. Marra CM, Tantalo LC, Maxwell CL, Ho EL, Sahi SK, Jones T. The rapid plasma reagin test cannot replace the venereal disease research laboratory test for neurosyphilis diagnosis. Sex Transm Dis. (2012) 39:453–7. doi: 10.1097/OLQ.0b013e31824b1cde
27. Zhu L, Gu X, Peng RR, Wang C, Gao Z, Zhou P, et al. Comparison of the cerebrospinal fluid (CSF) toluidine red unheated serum test and the CSF rapid plasma reagin test with the CSF venereal disease research laboratory test for diagnosis of neurosyphilis among HIV-negative syphilis patients in China. J Clin Microbiol. (2014) 52:736–40. doi: 10.1128/JCM.02522-13
28. Workowski KA. Centers for disease control and prevention. Sexually transmitted diseases treatment guidelines. MMWR Recomm Rep. (2015) 64:1–137.
29. Marra CM, Tantalo LC, Maxwell CL, Dougherty K. Wood B. Alternative cerebrospinal fluid tests to diagnose neurosyphilis in HIV-infected individuals. Neurology. (2004) 138:702. doi: 10.1016/j.ajo.2004.08.016
30. Marra CM, Critchlow CW, Hook EW, Collier AC, Lukehart SA. Cerebrospinal-fluid treponemal antibodies in untreated early syphilis. Arch Neurol. (1995) 52:68–72. doi: 10.1001/archneur.1995.00540250072015
31. Marra CM, Maxwell CL, Dunaway SB, Sahi SK, Tantalo LC. Cerebrospinal fluid Treponema pallidum particle agglutination assay for neurosyphilis diagnosis. J Clin Microbiol. (2017) 55:1865–70. doi: 10.1128/JCM.00310-17
32. Guarner J, Jost H, Pillay A, Sun Y, Cox D, Notenboom R, et al. Evaluation of treponemal serum tests performed on cerebrospinal fluid for diagnosis of neurosyphilis. Am J Clin Pathol. (2015) 143:479–84. doi: 10.1309/AJCPWSL3G8RXMCQR
33. Park IU, Tran A, Pereira L, Fakile Y. Sensitivity and specificity of treponemal-specific tests for the diagnosis of syphilis. Clin Infect Dis. (2020) 71: S13–20. doi: 10.1093/cid/ciaa349
34. LLevchik N, Ponomareva M, Surganova V, Zilberberg N. Kungurov NL. Criteria for the diagnosis of neurosyphilis in cerebrospinal fluid: relationships with intrathecal immunoglobulin synthesis and blood-cerebrospinal fluid barrier dysfunction. Sex Transm Dis. (2013) 40:917–92222. doi: 10.1097/OLQ.0000000000000049
35. Harding AS, Ghanem KG. The performance of cerebrospinal fluid treponemal-specific antibody tests in neurosyphilis: a systematic review. Sex Transm Dis. (2012) 39:291–7. doi: 10.1097/OLQ.0b013e31824c0e62
36. Wang C, Wu K, Yu Q, Zhang S, Gao Z, Liu Y, et al. CXCL13, CXCL10 and CXCL8 as potential biomarkers for the diagnosis of neurosyphilis patients. Sci Rep. (2016) 6:33569. doi: 10.1038/srep33569
37. Gudowska-Sawczuk M, Mroczko B. Chemokine ligand 13 (CXCL13) in neuroborreliosis and neurosyphilis as selected spirochetal neurological diseases: a review of its diagnostic significance. Int J Mol Sci. (2020) 21:2927. doi: 10.3390/ijms21082927
38. Marra CM, Tantalo LC, Sahi SK, Maxwell CL, Lukehart SA. CXCL13 as a cerebrospinal fluid marker for neurosyphilis in HIV-infected patients with syphilis. Sex Transm Dis. (2010) 37:283–7. doi: 10.1097/OLQ.0b013e3181d877a1
39. Li D, Huang X, Shi M, Luo L, Tao C. Diagnostic role of CXCL13 and CSF serology in patients with neurosyphilis. Sex Transm Infect. (2021) 97:485–9. doi: 10.1136/sextrans-2020-054778
40. Masouris I, Klein M, Ködel U. The potential for CXCL13 in CSF as a differential diagnostic tool in central nervous system infection. Exp Rev Anti Infect Ther. (2020) 18:875–85. doi: 10.1080/14787210.2020.1770596
41. Mothapo KM, Verbeek MM, van der Velden LB, Ang CW, Koopmans PP, van der Ven A, et al. Has CXCL13 an added value in diagnosis of neurosyphilis? J Clin Microbiol. (2015) 53:1693–6. doi: 10.1128/JCM.02917-14
42. Lin LR, Lin DH, Tong ML, Liu LL, Fan JY, Zhu XZ. et al. Macrophage migration inhibitory factor as a novel cerebrospinal fluid marker for neurosyphilis among HIV-negative patients. Clinica Chimica Acta. (2016) 463:103–8. doi: 10.1016/j.cca.2016.10.018
43. Wang C, Zhu L, Gao Z, Guan Z, Lu H, Shi M, et al. Increased interleukin-17 in peripheral blood and cerebrospinal fluid of neurosyphilis patients. PLoS Negl Trop Dis. (2014) 8:e3004. doi: 10.1371/journal.pntd.0003004
44. Li W, Wu W, Chang H, Jiang M, Gao J, Xu Y, et al. Cerebrospinal fluid cytokines in patients with neurosyphilis: the significance of interleukin-10 for the disease. Biomed Res Int. (2020) 2020:3812671. doi: 10.1155/2020/3812671
45. Satyaputra F, Hendry S, Braddick M, Sivabalan P, Norton R. The laboratory diagnosis of syphilis. J Clin Microbiol. (2021) 59:e00100–00121. doi: 10.1128/JCM.00100-21
46. Dunaway SB, Maxwell CL, Tantalo LC, Sahi SK, Marra CM. Neurosyphilis treatment outcomes after intravenous penicillin g vs. intramuscular procaine penicillin plus oral probenecid. Clin Infect Dis. (2020) 71:267–73. doi: 10.1093/cid/ciz795
47. Paraskevas GP, Kapaki E, Kararizou E, Mitsonis C, Sfagos C, Vassilopoulos D. Cerebrospinal fluid tau protein is increased in neurosyphilis: a discrimination from syphilis without nervous system involvement? Sex Transm Dis. (2007) 34:220–3. doi: 10.1097/01.olq.0000233738.23278.4e
48. Zhang M, Zhong X, Shi H, Vanmechelen E, De Vos A, Liu S, et al. BACE1 and other alzheimer's-related biomarkers in cerebrospinal fluid and plasma distinguish alzheimer's disease patients from cognitively-impaired neurosyphilis patients. J Alzheimers Dis. (2020) 77:313–22. doi: 10.3233/JAD-200362
49. Didonna A. Tau at the interface between neurodegeneration and neuroinflammation. Genes Immun. (2020) 21:288–300. doi: 10.1038/s41435-020-00113-5
50. Vassar R, Kovacs DM, Yan R, Wong PC. The beta-secretase enzyme BACE in health and Alzheimer's disease: regulation, cell biology, function, and therapeutic potential. J Neurosci. (2009) 29:12787–94. doi: 10.1523/JNEUROSCI.3657-09.2009
51. Neumann H, Takahashi K. Essential role of the microglial triggering receptor expressed on myeloid cells-2 (TREM2) for central nervous tissue immune homeostasis. J Neuroimmunol. (2007) 184:92–9. doi: 10.1016/j.jneuroim.2006.11.032
52. Paradowska-Gorycka A, Jurkowska M. Structure, expression pattern and biological activity of molecular complex TREM-2/DAP12. Hum Immunol. (2013) 74:730–7. doi: 10.1016/j.humimm.2013.02.003
53. Li W, Chang H, Wu W, Xu D, Jiang M, Gao J, et al. Increased CSF soluble TREM2 concentration in patients with neurosyphilis. Front Neurol. (2020) 11:62. doi: 10.3389/fneur.2020.00062
54. Chen F, Liu J, Li FQ, Wang SS, Zhang YY, Lu YY, et al. β2-microglobulin exacerbates neuroinflammation, brain damage, and cognitive impairment after stroke in rats. Neural Regenerat Res. (2023) 18:603–8. doi: 10.4103/1673-5374.350204
55. Tagarro A, García-Alix A, Alarcón A, Hernanz A, Quero J. Congenital syphilis: beta2-microglobulin in cerebrospinal fluid and diagnosis of neurosyphilis in an affected newborn. J Perinat Med. (2005) 33:79–82. doi: 10.1515/JPM.2005.015
56. Qi S, Xu Y, Luo R, Li P, Huang Z, Huang S, et al. Novel biochemical insights in the cerebrospinal fluid of patients with neurosyphilis based on a metabonomics study. J Mol Neurosci. (2019) 69:39–48. doi: 10.1007/s12031-019-01320-0
57. Liu LL, Lin Y, Chen W, Tong ML, Luo X, Lin LR, et al. Metabolite profiles of the cerebrospinal fluid in neurosyphilis patients determined by untargeted metabolomics analysis. Front Neurosci. (2019) 13:150. doi: 10.3389/fnins.2019.00150
Keywords: Treponema pallidum, cerebrospinal fluid, neurosyphilis, testing, syphilis
Citation: Gao Z-X, Gou Y, Liu X-Q and Peng L-W (2022) Advances in laboratory diagnostic methods for cerebrospinal fluid testing for neurosyphilis. Front. Public Health 10:1030480. doi: 10.3389/fpubh.2022.1030480
Received: 29 August 2022; Accepted: 28 October 2022;
Published: 14 November 2022.
Edited by:
Yuan Quan, Xiamen University, ChinaReviewed by:
Arshi Munawwar, University of Maryland, United StatesQian-Qiu Wang, Chinese Academy of Medical Sciences and Peking Union Medical College, China
Albert Stezin, Indian Institute of Science, India
Copyright © 2022 Gao, Gou, Liu and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei-Wen Peng, lwpeng99@163.com
 Zheng-Xiang Gao
Zheng-Xiang Gao Yu Gou1,2
Yu Gou1,2