- 1School of Public Health, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Shanghai Municipal Center for Disease Control and Prevention, Shanghai, China
- 3Renji Hospital, Affiliated With the School of Medicine Shanghai Jiao Tong University, Shanghai, China
Introduction: Internal migrant Men who have sex with men (IMMSM), which has the dual identity of MSM and floating population, should be more concerned among the vulnerable groups for HIV in society. Establishing appropriate prediction models to assess the risk of HIV infection among IMMSM is of great significance to against HIV infection and transmission.
Methods: HIV and syphilis infection were detected using rapid test kits, and other 30 variables were collected among IMMSM through questionnaire. Taking HIV infection status as the dependent variable, three methods were used to screen predictors and three prediction models were developed respectively. The Hosmer-Lemeshow test was performed to verify the fit of the models, and the net classification improvement and integrated discrimination improvement were used to compare these models to determine the optimal model. Based on the optimal model, a prediction nomogram was developed as an instrument to assess the risk of HIV infection among IMMSM. To quantify the predictive ability of the nomogram, the C-index measurement was performed, and internal validation was performed using bootstrap method. The receiver operating characteristic (ROC) curve, calibration plot and dynamic component analysis (DCA) were respectively performed to assess the efficacy, accuracy and clinical utility of the prediction nomogram.
Results: In this study, 12.52% IMMSMs were tested HIV-positive and 8.0% IMMSMs were tested syphilis-positive. Model A, model B, and model C fitted well, and model B was the optimal model. A nomogram was developed based on the model B. The C-index of the nomogram was 0.757 (95% CI: 0.701–0.812), and the C-index of internal verification was 0.705.
Conclusions: The model established by stepwise selection methods incorporating 11 risk factors (age, education, marriage, monthly income, verbal violence, syphilis, score of CUSS, score of RSES, score of ULS, score of ES and score of DS) was the optimal model that achieved the best predictive power. The risk nomogram based on the optimal model had relatively good efficacy, accuracy and clinical utility in identifying internal migrant MSM at high-risk for HIV infection, which is helpful for developing targeted intervention for them.
Introduction
In recent years, men who have sex with men (MSM) have emerged as a high-risk group for HIV infection in China, with the rate of HIV infection rising year by year (1). A large-scale systematic analysis reported that the national HIV prevalence among MSM from 2001 to 2018 was 5.7%, and the study prevalence ranged from 0 to 22.91% (2). Previous studies have shown that the internal migrant MSM (IMMSM) constituted most of the MSM populations, ranging from 71.2 to 91.3% (3–5). IMMSM is defined as changes of usual residence within countries and have had sex with a male in the last 6 months (6). Migration within China has been identified as a major factor influencing the transmission of HIV in China, and the high migration rate among MSM populations poses a huge challenge to HIV prevention and control (1, 7).
Because of the better employment opportunities, less social discrimination, and more comfortable living environment, a large number of MSM moved to the metropolis and developed regions, but due to the imperfection of China's household registration system and urban social security system, the migrant populations had lower access to social benefits such as education and health services than the local populations (1, 8). According to prior studies, migrant MSM had lower levels of HIV knowledge and fewer opportunities for HIV testing compared with the local MSM populations, but they were at higher risk of engaging in high-risk sexual behaviors, such as unprotected anal intercourse (UAI), multiple sexual partners (MSP), and transactional sex (9–11). It has been documented that the HIV infection rates in migrant MSM were higher than those in local MSM (1, 12). Migrant MSM, which has the dual identity of MSM and floating population, should be more concerned among the vulnerable groups in society.
Joint United Nations Programme on HIV/AIDS (UNAIDS) has set the 95-95-95 strategy to achieve the goal of ending the global HIV epidemic by 2030, with the goal of making 95% of people living with HIV aware of their HIV serostatus by 2030 (13). Nevertheless, HIV testing rate among MSM has been low in China. A study including 988 participants found that only 57.1% of MSM have been tested for HIV in the past year (14). Thus, other methods are required to distinguish those at high-risk for HIV infection. Establishing appropriate prediction models to assess the risk of HIV infection in migrant MSM populations is beneficial for an individual to aware risk of infection and proactively avoid adverse factors, and is also in favor of the government to identify high-risk groups and integrate limited resources for targeted interventions specific to this population. While several HIV risk assessment tools have been targeted at MSM domestic and overseas (15–18), none has yet been developed for internal migrant MSM.
A variety of risk factors associated with HIV infection among MSM have been identified within the existing literatures. Among these factors, sociodemographic characteristics like age and education, behaviors such as UAI, sex trade and alcohol use before sex, sexually transmitted diseases have been widely studied (19–23). However, most studies to date have overlooked the important role that psychological factors play on HIV infection. As a sexual minority, MSM lives in surroundings full of stressors, such as stigma, prejudice and discrimination, which may compound negative mental health. Accordingly, compared with the heterosexual communities, MSM have suffered from serious mental health problems, including depression, distress, and trauma (24). Unfortunately, psychological problems and the relationship between these problems and HIV infection among migrant MSM is an underexplored area. Therefore, prediction models that incorporating psychological factors may assess the vulnerabilities for HIV infection more effectively.
Given these multiple gaps in knowledge of risk assessments of HIV infection among migrant MSM, in the present study, we explored numerous risk factors including sociodemographic characteristics, behaviors and experiences, condom use related factors, STDs infection status and psychological variables for HIV infection. After that, three different methods (Boruta, stepwise selection and univariable selection) were used to establish and validate prediction models. Then, an optimal model was selected to develop nomogram as an instrument to assess the risk of HIV infection among IMMSM, which may help to develop targeted interventions for them in the future.
Method
Study design and sampling
A cross-sectional study was performed simultaneously in four cities in China: east China (Shanghai), southern China (Shenzhen), northeastern China (Shenyang) and Southwest China (Kunming). It is difficult to target MSM by using probability sampling because they tend to hide their sexual orientation. The “snowball” sampling technique, which is advantageous in addressing population covertness was chosen for the present study. In each city, with the help of non-government organizations or local center for disease control and prevention, 5–10 socially adept MSM were recruited as “seeds” for the “snowball sampling”. Subsequently, with the introduction of the initial “seeds”, more and more MSM were recruited and acted as new “seeds”. Each participant took part in a face-to-face interview with a trained staff in which they were informed of the details of the study. Written informed consent was obtained from participants before the survey. The recruitment procedure and the design of this study were approved by the Ethics Committee of School of Public Health, Shanghai Jiao Tong University.
Inclusion and exclusion criteria
Inclusion criteria: physiologically male, at least 18 years of age, and self-reported to have had sex with a male in the past 6 months. Exclusion criteria: those whose current place of residence and registered place are the same; cannot complete the questionnaire independently. 229, 195, 92, and 187 IMMSMs were recruited in Shanghai, Shenyang, Kunming and Shenzhen, respectively. All of them completed the test and questionnaire and were included in this study. All participants were given one free HIV test as well as a $17.84 subsidy.
Measurements
HIV and syphilis infections were tested by using rapid test kits (Beijing Aipu Medical Equipment Co.). The information collected through the questionnaire included basic demographic information (age, marriage, monthly income, etc.), homosexual sexuality (condom use, commercial sex, etc.), substance use (alcohol, cigarettes, drugs).
Rosenberg self-esteem scale (RSES)
The level of self-esteem was assessed by the 10 items, 4-point Likert-type RSES. Answers ranging from 1 (strongly disagree) to 4 (strongly agree), the higher the scores, the higher the level of self-esteem.
University of California at Los Angels loneliness scale (ULS)
Loneliness was assessed by ULS, which included 8 items, answers ranging from 1 (never) to 4 (often). The higher total scores indicated the stronger feeling of loneliness.
Patient health questionnaire-9 (PHQ-9)
Depression was assessed by the PHQ-9, with the total scores from 0 to 27. Answers range from 0 (never) to 3 (almost everyday). The higher scores indicated the higher level of depression.
Entrapment scale (ES)
Entrapment was assessed by the 16-item ES with answers ranging from 0 (never) to 4 (always), the higher the scores, the higher the level of entrapment.
Defeat scale (DS)
Defeat was assessed by the 16-item DS, with answers ranging from 0 (never) to 4 (always), the higher the scores, the higher the level of defeat.
Interpersonal needs questionnaire (INQ-15)
Interpersonal need was measured using the 15-item, 7-point Likert-type INQ-15. Answers were rated ranging from 1 (strongly not comply) to 7 (strongly comply) where a higher total score indicates a higher level of unmet interpersonal needs.
Suicidal ability scale (SAS)
The 9-item Likert-type SAS was applied to measure individual's suicidal ability. Answers were rated ranging from 0 (strongly disagree) to 8 (strongly agree), with a higher total score indicating higher suicidal ability.
Social support scale (SSS)
We employed the SSS to assess subjectively recognized social support from family, friends, and significant others. The scale is a 7-point Likert scale with 12 items, ranging from 1 (very strongly disagree) to 7 (very strongly agree). A higher total score indicated higher social support.
Sexual compulsivity scale (SCS)
The 10-item Likert-type SCS was applied to measure individual's out-of-control sexual thoughts and behaviors. Answers were rated ranging from 1 (strongly disagree) to 4 (strongly agree), with a higher total score indicating higher sexual compulsivity.
All of the above scales are widely used in the MSM population (25–40), and total of 31 independent variables were collected.
Statistical analysis
Scale reliability test
Scale reliability is broadly defined in the population as the ratio of the variance of true scores to the variance of observed scores, while Cronbach's coefficient alpha is a statistic for assessing scale reliability based on internal consistency (41). Cronbach's coefficient alpha ≥0.7 represents a good correlation and alpha < 0.5 represents an unacceptable correlation (42, 43).
Feature description
Categorical variables were expressed as frequencies and percentages, and continuous variables were described as medians and quartiles (non-normal distributions). Chi-square test, corrected Chi-square test and Fisher exact test were used to assess the differences in categorical variables between HIV-positive MSM and HIV-negative MSM. Differences in continuous variables between HIV-positive MSM and HIV-negative MSM were evaluated using Mann–Whitney U test. All tests were two-sided and P ≤ 0.05 was set as the level of significant difference.
Variable selection methods
Boruta
Boruta is based on the same idea which forms the foundation of the random forest classifier, namely, that by adding randomness to the system and collecting results from the ensemble of randomized samples one can reduce the misleading impact of random fluctuations and correlations. The Boruta algorithm consists of following steps (44):
1. Extend the Information System by Adding Copies of all the 31 Variables.
2. The Added Attributes Are Processed to Remove Their Association With the Response.
3. Run a Random Forest Classifier on the Extended Information System and Gather the Z Scores Computed.
4. Find the Maximum Z Score Among Shadow Attributes (MZSA), and Then Assign a hit to Each Attribute That Scored Better Than MZSA.
5. For Each Attribute With Undetermined Importance Perform a two-Sided Test of Equality With the MZSA.
6. Deem the Attributes Which Have Importance Significantly Lower Than MZSA as ‘Unimportant' and Permanently Remove Them From the Information System.
7. Deem the Attributes Which Have Importance Significantly Higher Than MZSA as ‘Important'.
8. Remove all Shadow Attributes.
9. Repeat the Procedure Until the Importance Is Assigned for all the Attributes, or the Algorithm Has Reached the Previously set Limit of the Random Forest Runs.
Stepwise selection
Stepwise selection is a variation of forward selection. At each step of the variable selection process, after a variable has been added to the model, variables are allowed to be removed from the model (45). For example, if the significance of a given predictor is higher than a specific threshold, it is removed from the model. The iterative process is ended when the pre-defined stopping rule is satisfied.
Univariate selection
The steps for univariate selection were: variables with P ≤ 0.1 in the comparison of differences between HIV-positive and HIV-negative groups were included in the univariate logistic regression, and the variables with P ≤ 0.05 in the univariate logistic regression would be used to develop the prediction model.
Hosmer-Lemeshow test
Assessing the goodness of fit of a model is an important and essential part of any modeling exercise. The Hosmer-Lemeshow (H-L) test for the goodness of fit of logistic regression is very popular because it is easy to implement, simple to interpret, and widely adopted by popular statistical packages (46). It is widely used for the evaluation of risk-scoring models in medicine (47, 48). The null hypothesis of H-L test is that there is no significant difference between the predicted and observed values, which implies a perfect fit of the model (49).
Determination of the optimal model
Three prediction models were developed by using multivariate logistic regression and we compared the models by determining the net reclassification improvement (NRI) and integrated discrimination improvement (IDI) to select the optimal model.
Development and validation of nomogram
The nomogram is a visualization of the prediction model. In this study, a nomogram will be developed based on the best prediction model to assess the risk of HIV infection among IMMSM. The receiver operating characteristic (ROC) curve, calibration plot and dynamic component analysis (DCA) were respectively performed to assess the efficacy, accuracy and clinical utility of the prediction nomogram. Discrimination was calculated using the C-index, ranging from 0.5 to 1.0 (1.0 means perfect discrimination) (50), and internal validation was performed using bootstrap method. Bootstrap samples are random samples drawn with replacement from the original sample, and 1,000 bootstrap samples were fitted in this study to calculate a relatively corrected C-index.
Results
Statistical description
Cronbach's alpha of mental health scales: RSES was 0.842, ULS was 0.824, PHQ-9 was 0.905, ES was 0.969, DS was 0.938, INQ-15 was 0.854, SAS was 0.787, SSS was 0.949, SCS was 0.934. The results showed good reliability for all mental health scales.
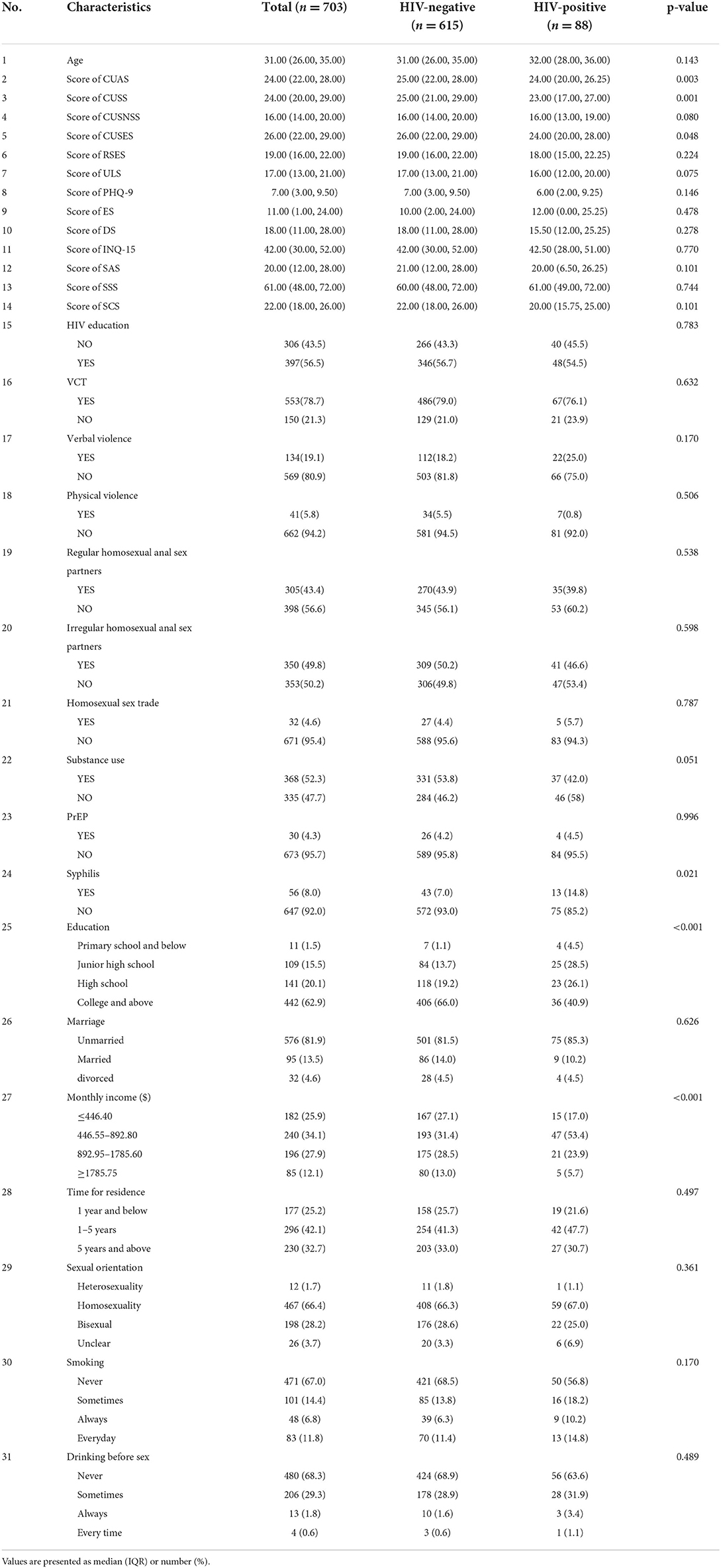
703 IMMSM were included in this study. The median age of the IMMSMs was 31.00 (26.00, 35.00) years old, 576 (81.9) IMMSMs were unmarried, 442 (62.9%) IMMSMs had received a college education, 88 (12.52%) IMMSMs were tested HIV-positive, 56 (8.0%) IMMSMs were tested syphilis-positive, 134 (19.1%) IMMSMs had experienced verbal violence due to their sexual orientations, 350 (49.8%) IMMSMs had irregular homosexual anal sex partners, 368 (52.3%) IMMSMs had substance use experience. Specific demographic and scale scores are shown in Table 1.
Variable Description: No. 1, Age, Age of the participant at the time of the survey; No. 2, CUAS, the Condom Use Attitude Scale, with higher scores indicating more positive attitudes; No. 3, CUSS, the Condom Use Skills Scale, assessed subjects' negotiation skills with condom use and refusal of unprotected sex, the higher the scores, the better the condom use skills; No. 4, CUSNSS, the Condom Use Subjective Normative Scale, assessed others' (family, friends, peers at the same job, significant others) perceptions of participants' adherence to condom use during anal sex, with higher scores indicating more positive attitudes; No. 5, CUSES, the Condom Use Self-Efficacy Scale, assessed their ability to participate effectively in condom use, and the higher the scores, the higher the condom use self-efficacy; No. 6, RSES, the Rosenberg Self-Esteem Scale, assessed their level of self-esteem, and the higher the scores, the higher the level of self-esteem; No. 7, ULS, the UCLA (University of California at Los Angels) Loneliness Scale, assessed their level of loneliness, the higher the scores, the stronger the loneliness; No. 8, PHQ-9, the Patient Health Questionnaire, assessed their level of depression, and the higher the scores, the higher the level of depression; No. 9, ES, the Entrapment Scale, assessed their level of entrapment, and the higher the scores, the higher the level of entrapment; No. 10, DS, the Defeat Scale, assessed their level of defeat, and the higher the scores, the higher the level of defeat; No. 11, INQ-15, the Interpersonal Needs Questionnaire, assessed their level of interpersonal needs, the higher the scores, the more unmet interpersonal needs; No. 12, SAS, the Suicidal Ability Scale, assessed their level of suicidal ability, and the higher the scores, the higher the level of suicidal ability; No. 13, SSS, the Social Support Scale, assessed their level of social support, the higher the scores, the higher the support; No. 14, SCS, the Sexual Compulsivity Scale, assessed their level of sexual compulsivity, the higher the scores, the stronger the compulsivity; No. 15, experienced of receiving HIV education, Yes or No; No. 16, had HIV Voluntary Counseling and Test, Yes or No; No. 17, experienced of verbal violence such as harassment, insults, threats, Yes or No; No. 18, experienced of physical violence such as pushing, Yes or No; No. 19, had regular homosexual anal sex partners, Yes or No; No. 20, had irregular homosexual anal sex partners, Yes or No; No. 21, supplied sexual services for male sexual partners, Yes or No; No. 22, used substances, Yes or No; No. 23, had taken pre-exposure prophylaxis in the past, Yes or No; No. 24, had infected with syphilis, Yes or No; No. 25, education level; No. 26, marriage status; No. 27, Monthly income; No. 28, residence time; No. 29, sexual orientation; No. 30, frequency of smoking, never means not even once, sometimes means 3 to 5 times a month, always means more than 3 times a week, and Everyday means at least once a day; No. 31, frequencies of drinking behavior before sex.
Screening of predictive factors by three methods
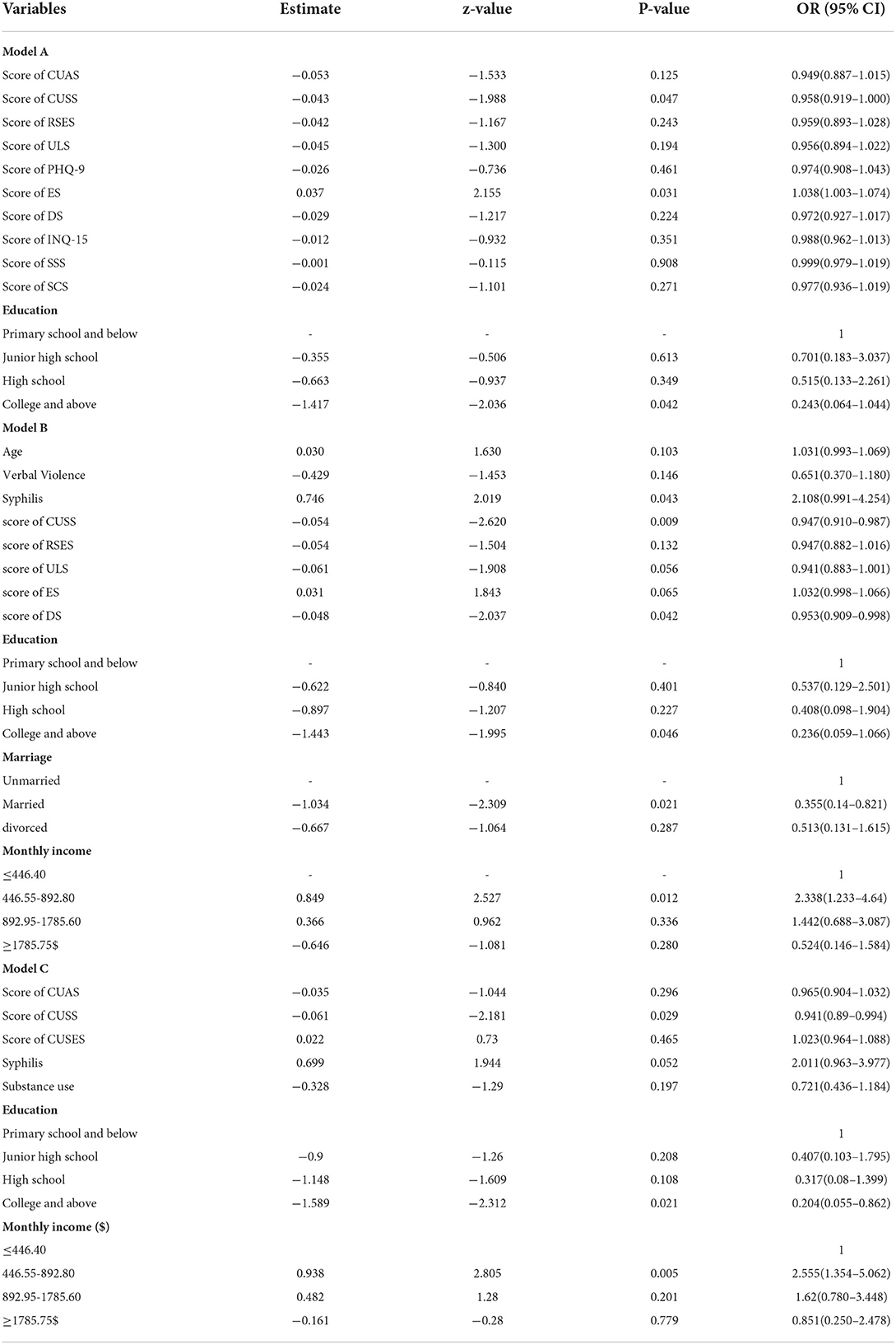
Three HIV infection prediction models were developed based on three different variable screening methods. The Boruta algorithm screened 11 factors (Education, score of CUAS, score of CUSS, score of RSES, score of ULS, score of PHQ-9, score of ES, score of DS, score of INQ-15, score of SAS and score of SCS) and developed model A (Supplementary Table 1). Stepwise selection method (both forward and backward) was used to screen 11 factors (Age, Education, Marriage, Monthly income, Verbal Violence, Syphilis, score of CUSS, score of RSES, score of ULS, score of ES and score of DS) and built model B (Supplementary Table 2). There were 9 variables with P-values ≤ 0.1 in the exploration of differences between HIV-positive IMMSM and HIV-negative IMMSM (Table 1). Subsequently, univariate logistic regression was created for each of these variables with HIV infection status, and the results showed that 7 variables (score of CUAS, score of CUSS, score of ULS, Education, Monthly income, Syphilis and Substance use) had P-values ≤ 0.05 (Supplementary Table 3). So, the univariate selection screened 7 factors and built model C. The coefficients and P-values of the variables for each model were shown in Table 2. The results of Hosmer-Lemeshow test showed that the corresponding P-values of the 3 models were 0.7124, 0.1066, and 0.153, respectively. The P-values of the three models were greater than 0.05, indicating that these models had good fits and were valid.
Hosmer-Lemeshow test for model fit
Model A, model B and model C were performed H-L test respectively, and the P-values of the results were 0.683, 0.663, and 0.579 respectively. All results were insignificant, which indicated that all three models were fitted well.
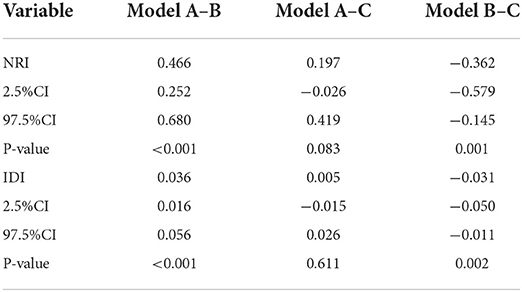
Comparison of models and determination of the best prediction model
Table 3 shows the NRI and IDI between these three models. Taking model A as the reference, we compared model A with model B. The values of NRI and IDI were greater than zero and both were significant (P < 0.05), which indicates that model B was superior to model A. The values of NRI and IDI for model C compared to model A were not statistically significant, which indicates model C did not exhibit superiority for predicting HIV infection among IMMSM. Taking model B as the reference, model C compared with model B, the values of NRI and IDI were less than zero and both were significant (P < 0.05), which indicates that model B was superior to model C. There was a significant improvement in model B compared to model A and model C. Therefore, model B was the optimal prediction model to predict the risk of HIV infection among IMMSM in this study.
Development and validation of the nomograms
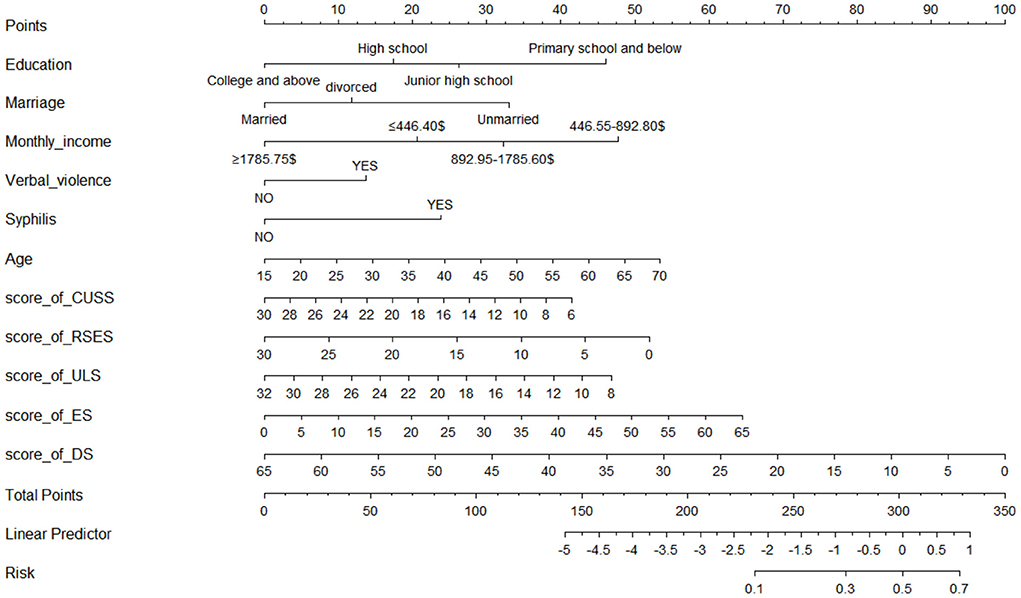
A nomogram with 11 variables (Age, Education, Marriage, Monthly income, Verbal Violence, Syphilis, score of CUSS, score of RSES, score of ULS, score of ES and score of DS) was constructed based on the model B (Figure 1), and a dynamic nomogram can be accessed and used via a URL: https://liubi.shinyapps.io/DynNomapp/. The AUC of the nomogram was 0.757(95% CI: 0.701–0.812), and the ROC showed in Figure 2. Calibration curves of the nomogram demonstrated good consistency between the predicted and observed results (Figure 3). The result of DCA revealed that using the nomograms to predict HIV infection among IMMSM added more net benefit than the treat-all or treat-none strategies (Figure 4), suggesting good clinical utility of the nomograms. The C-index for the prediction nomogram was 0.757 (95% CI: 0.701–0.812), which was confirmed to be 0.705 via bootstrapping validation.
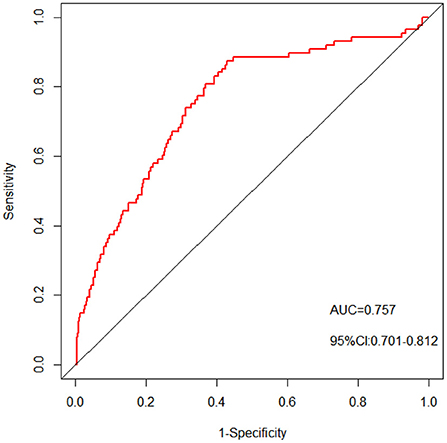
Figure 2. The pooled AUC of the ROC curve. The y-axis means the true positive rate of the risk prediction. The x-axis means the false positive rate of the risk prediction. The red line represents the performance of the nomogram.
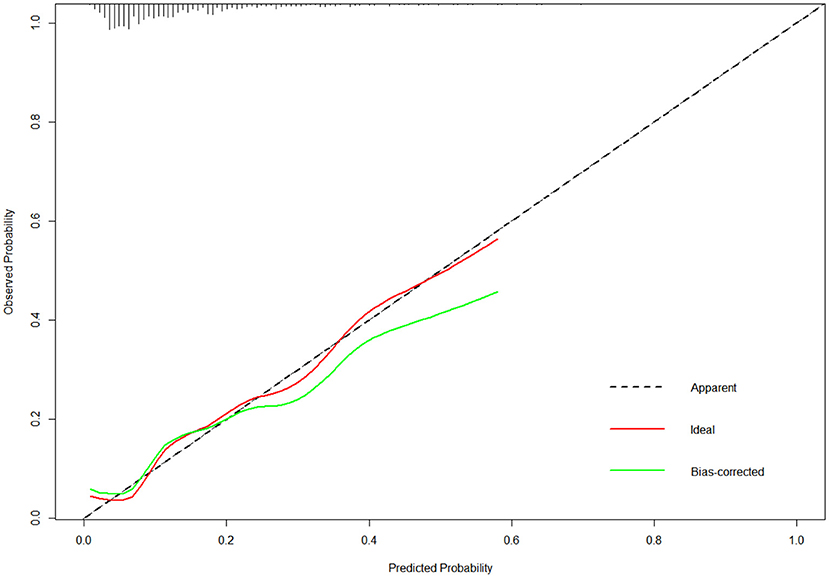
Figure 3. The calibration curves of the nomogram. The x-axis represents the predicted risk of HIV infection. The y-axis represents the actual diagnosed HIV incidence. The diagonal dotted line represents a perfect prediction by an ideal model. The green line represents the performance of the nomogram, of which a closer fit to the diagonal dotted line represents a better prediction.
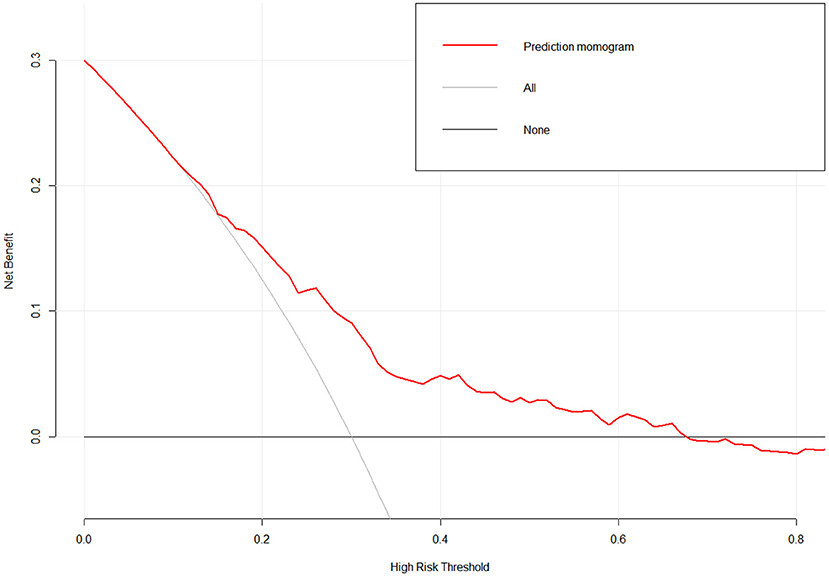
Figure 4. Decision curves of the nomogram. The y-axis measures the net benefit. The red line represents the HIV incidence risk nomogram. The light black solid line represents the assumption that all patients are diagnosed as DN. Deep black solid line represents the assumption that no patients are diagnosed as HIV.
Discussion
In this study, 30 variables were collected among IMMSM through questionnaire on four aspects—sociodemographic characteristics, homosexual behavior, substance use, and mental health. Another 2 variables-HIV and syphilis infection were detected using rapid test kits. Taking HIV infection status as the dependent variable, three methods (Boruta, stepwise selection and univariable selection) were used to screen predictors and three prediction models (model A, model B and model C) were developed by multivariate logistic regression respectively. By comparing NRI and IDI between these three models, model B was considered the optimal model. The nomogram passed the validation of ROC, calibration curve and DCA, indicating its good efficacy, accuracy and clinical utility in predicting HIV infection among IMMSM. The C-index of internal verification was 0.705, which indicated that the model had medium prediction accuracy. To summarize the above validation results, the nomogram of the model has moderate predictive power.
Sociodemographic characteristics in the prediction nomogram
Four sociodemographic characteristics (age, education level, monthly income and marital status) were incorporated in our prediction nomogram. Age was found to be a risk factor for HIV infection among IMMSM, as participants with higher age were more likely to report HIV infection. Several studies have reported similar results (2, 51, 52). One reason might be that older IMMSM have been exposed to HIV for a longer time. It has been argued that as IMMSM get older, they might have a greater chance of becoming infected over time, so prevalence within older age will be higher than that in the younger groups (52). Additionally, unprotected anal intercourse is more common in older MSM than in younger MSM (53). Another possible reason was that the older MSM may not be as prudent as the younger counterparts when engaging in sexual behavior due to their rich sexual experience.
In the prediction nomogram, lower levels of education contributed higher risk values for HIV infection among IMMSM. In the one hand, the less educated IMMSM usually have less chance to obtain health information and support (2), which may lead to their poorer abilities on protecting themselves from HIV infection. In the other hand, ADDIN EN.CITE (54, 55) some studies found that condom use frequencies as well as the number of consistent sexual partner were significantly higher among MSM with higher levels of education (e.g., college students or teachers) than among others (56–58), which suggested that low HIV infection risk in more educated IMMSM may benefits from their low participation in risky sexual behaviors.
In this study, the monthly income range with the highest contribution risk value was 446.55–892.80$, then 892.95–1785.60$, followed by ≤ 446.40$, and the lowest was ≥1,785.75$. Socioeconomic status (SES) is an important determinant of health. It seems complicated to explain the contribution of monthly income to the risk value of HIV infection among IMMSM. In terms of MSM with higher economic status, they were more willing to participate in HIV testing and counseling services, possibly because they were more capable of affording the cost of these services (20, 58, 59). What's more, individual with higher incomes tend to have better educational background and have better access to health information. As for MSM with low incomes (60, 61), it was reported by two studies conducted in China that they were more likely to take pre-exposure prophylaxis, which is an efficient way to prevent HIV infection. Additionally, MSM with lower incomes were less likely to report UAI (62). ADDIN EN.CITE (63) ADDIN EN.CITE (64, 65) our findings suggest that the mechanism how individual's economic status play a role on their HIV infection risk among IMMSM is warranted in the future studies.
In China, some MSM would marry women due to widespread social rejection and pressure from their parents (66). Being married to a woman does not completely preclude them from having sex with men (37, 67), but they might reduce the frequency of homosexual sex to avoid disclosure of sexual orientation. In addition, the responsibilities of maintaining a family consumed so much time and energy that they were unable to engage in homosexual behavior as they once did. The vast majority of IMMSM in this study were unmarried, which is consistent with most studies (68–70). Unmarried IMMSM might be more assertive about their sexual orientation and take advantage of their migrant status to escape the discrimination and pressure from society and family. They also changed their homosexual partners and engaged in risky sexual behaviors more frequently (71, 72).
Psychometric measurements in the prediction nomogram
The lower score of RSES contributed to the higher risk value. Self-esteem serves as a protective buffer against negative emotions that arise from disruptive or threatening experiences. For MSM, self-esteem acted as a sexual risk buffer for MSM (73). But the widespread stigmatization and marginalization of MSM could continue destroying their self-esteem. On the one hand, MSM with low self-esteem tended to engage in less self-care behaviors and was more likely to be involved in high-risk sexual behaviors (74, 75). On the other hand, the desire for self-esteem drove them to seek validation and stronger social relationships among homosexual partners, which might lead to more sexual partners and more frequent high-risk sexual behavior (76, 77).
In the prediction nomogram, lower ULS scores contributed to higher risk values for HIV infection. Higher scores of ULS indicated stronger feelings of loneliness. Loneliness has been defined as the distress that exists between actual and desired relationships (78, 79). For internal migrant MSM, what they expect was to build a good social relationship with other MSM (80). Higher scores of ULS indicated higher levels of loneliness and a greater likelihood of being in poor social relationships, which may lead to fewer homosexual partners and less risky sexual behaviors, thus reducing the risk of HIV infection.
Gilbert and Allen defined entrapment as a personal feeling that an individual was in an unfavorable state or situation and had a strong motivation to escape or get rid of the stressor, but was not capable to escape (81). Compulsive sexual behavior, sexual abuse, promiscuity and commercial sexuality are common among MSM and can increase the risk of HIV infection (82–85). Internal migrant MSM with higher ES scores might be trapped by these behaviors and unable to escape. ADDIN EN.CITE (86–89).
Defeat can arise from a loss or reduction in one's perceived ability to compete for social status (81, 90). For internal migrant MSM, defeat might stem from being rejected due to sexual orientation, feeling inferior to others, or feeling incompetent in various roles. Defeat involved a loss of emotional autonomy and a sense of being broken, expressed through statements such as “I feel like a loser” (91). To cope with the defeat, they might reduce their exploration and involvement in homosexual relationships, and thus indirectly reduce the risk of HIV infection (86, 92).
Behavior, experiences and STDs in the prediction nomogram
MSM were often subjected to verbal violence because their sexual orientation was not accepted by mainstream society (93–95). Prolonged exposure to verbal violence might have a negative impact on their behavior and mental health. Experiences of verbal violence were reported to be associated with high-risk sexual behaviors and substance use which were also risk factors for HIV infection (96–98). In addition, verbal violence might indirectly increase the risk of HIV infection by promoting the occurrence of anxiety and depression (99–101).
It is well known that condoms are one of the most effective HIV prevention methods, and condom use skills can directly affect MSM's consistent use of condoms (102–104). Higher scores of CUSS represent stronger condom use negotiation skills and unprotected sex refusal skills (39, 105). These skills can help MSM protect themselves from HIV infection by promoting them to use condoms consistently when they engage in high-risk sexual behaviors.
Syphilis is another highly prevalent sexually transmitted disease among MSM and it shares common risk factors with HIV (106–108). If an IMMSM was infected with syphilis, it means that he might also has some risk factors for HIV infection. More importantly, syphilis infection can directly increase the risk of HIV infection. Strong epidemiologic studies have provided substantial evidence that syphilis infection, one of the causes of genital ulcer disease, facilitates HIV transmission (109). Syphilitic ulcers disrupt epithelium and mucosa, which provides a portal of entry for HIV virus (110).
Conclusion
Our study screened the risk factors related to HIV infection among IMMSM through three variable-selection methods (Boruta, stepwise selection and univariable selection). The model established by stepwise selection methods incorporating 11 risk factors (age, education, marriage, monthly income, verbal violence, syphilis, score of CUSS, score of RSES, score of ULS, score of ES and score of DS) was the optimal model that achieved the best predictive power by comparing the NRI and IDI between three models. The risk nomogram based on the optimal model had relatively good efficacy, accuracy and clinical utility in identifying IMMSM at high-risk for HIV infection, which is helpful for developing targeted intervention for them.
Limitations
Some limitations of the study should be noted. First, snowball sampling was used to recruit participants, and those who participated in the study might share some similar characteristics. Second, many of the scales and questions were made into questionnaires that were filled out subjectively by the participants, which made the objectivity of the study insufficient. Finally, the entire study was cross-sectional based, and results need to be further confirmed by cohort studies.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of School of Public Health, Shanghai Jiao Tong University School of Medicine. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YC and YiW: designed the study. SL, DY, and LX: designed and completed the questionnaire production. RC and RW: created the research database and entered research data. AL: assisted in data collection. SL, YL, and HC: completed the statistical analysis of the data. SL and DX: wrote the first draft of the article. FH, YC, and YiW: have revised the first draft into the final draft. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Shanghai Jiao Tong University School of Public Health Local High-level University Achievement-oriented Top-notch Cultivation Programme for Undergraduate Students (Grant No. 18ZYGW20), the National Natural Science Foundation of China (Grant No. 71603166), and the fifth round of Shanghai public health three-year action plan key disciplines construction (Grant No. GWV-10.1-XK18).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1015699/full#supplementary-material
References
1. Chen Y, Tang W, Chen L, Shi L, Liu X, Xu J, et al. Changing epidemic of HIV and syphilis among resident and migrant men who have sex with men in Jiangsu, China. Sci Rep. (2017) 7:9478. doi: 10.1038/s41598-017-08671-x
2. Dong M-J, Peng B, Liu Z-F, Ye Q-N, Liu H, Lu X-L, et al. The prevalence of HIV among MSM in China: a large-scale systematic analysis. BMC Infect Dis. (2019) 19:1000. doi: 10.1186/s12879-019-4559-1
3. Mi G-D, Zhang B-B, Yu F, Ren X-L, Ong JJ, Fan Y-Q, et al. HIV incidence among men who have sex with men using geosocial networking smartphone application in Beijing, China: an open cohort study. Infect Dis Poverty. (2021) 10:27. doi: 10.1186/s40249-021-00814-7
4. Lau JTF Li D, Wang Z, Lai CHY. Repeated HIV voluntary counseling and testing increased risk behaviors among men who have sex with men in China: a prospective cohort study. AIDS Behav. (2015) 19:1966–77. doi: 10.1007/s10461-015-1034-x
5. Huang W, Wang Y, Lu H, Wu D, Pan SW, Tucker JD, et al. High HIV incidence among men who have sex with men in 8 Chinese cities: results from a trial. Open Forum Infect Dis. (2020) 7:ofaa147. doi: 10.1093/ofid/ofaa147
6. Kuhn R. Internal migration: developing countries. In:Wright JD, , editor. International Encyclopedia of the Social & Behavioral Sciences (Second Edition). Oxford: Elsevier (2015). p. 433–42. doi: 10.1016/B978-0-08-097086-8.31120-5
7. Hu J, Gu X, Tao X, Qian Y, Babu GR, Wang G, et al. Prevalence and trends of HIV, syphilis, and HCV in migrant and resident men who have sex with men in Shandong, China: results from a serial cross-sectional study. PLoS ONE. (2017) 12:e0170443. doi: 10.1371/journal.pone.0170443
8. Qin Q, Tang W, Ge L, Li D, Mahapatra T, Wang L, et al. Changing trend of HIV, syphilis and hepatitis C among men who have sex with men in China. Sci Rep. (2016) 6:31081. doi: 10.1038/srep31081
9. Shi T-X, Zhang B-C, Li X-F, Xu J-X, Wang N, Yu Z-Z, et al. Study on the high risk behaviors related to aids among men who having sex with men in the floating population. Zhonghua Liu Xing Bing Xue Za Zhi. (2009) 30:668–71. doi: 10.3760/cma.j.issn.0254-6450.2009.07.004
10. Wu J, Wu H, Li P, Lu C. HIV/STIS risks between migrant MSM and local MSM: a cross-sectional comparison study in China. PeerJ. (2016) 4:e2169. doi: 10.7717/peerj.2169
11. Ruan S, Yang H, Zhu Y, Ma Y, Li J, Zhao J, et al. Hiv prevalence and correlates of unprotected anal intercourse among men who have sex with men, Jinan, China. AIDS Behav. (2008) 12:469–75. doi: 10.1007/s10461-008-9361-9
12. Liu Y, Vermund SH, Ruan Y, Liu H, Zhang C, Yin L, et al. HIV testing and sexual risks among migrant men who have sex with men: findings from a large cross-sectional study in Beijing, China. AIDS Care. (2018) 30:86–94. doi: 10.1080/09540121.2017.1381331
13. UNAIDS. Understanding Fast Track: Accelerating Action to End the Aids Epidemic by 2030. Available online at: https://www.unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_FastTrack_en.pdf (accessed July 15, 2022).
14. Jiang H, Hong H, Dong H, Jiang J, He L. HIV testing and risks of sexual behavior among HIV-negative men who have sex with men in Ningbo, China. Int J Environ Res Public Health. (2020) 17:1322. doi: 10.3390/ijerph17041322
15. Haukoos JS, Lyons MS, Lindsell CJ, Hopkins E, Bender B, Rothman RE, et al. Derivation and validation of the denver human immunodeficiency virus (HIV) risk score for targeted hiv screening. Am J Epidemiol. (2012) 175:838–46. doi: 10.1093/aje/kwr389
16. Wahome E, Fegan G, Okuku HS, Mugo P, Price MA, Mwashigadi G, et al. Evaluation of an empiric risk screening score to identify acute and early HIV-1 infection among MSM in Coastal Kenya. AIDS. (2013) 27:2163–6. doi: 10.1097/QAD.0b013e3283629095
17. Hoenigl M, Weibel N, Mehta SR, Anderson CM, Jenks J, Green N, et al. Development and validation of the San Diego early test score to predict acute and early HIV infection risk in men who have sex with men. Clin Infect Dis. (2015) 61:468–75. doi: 10.1093/cid/civ335
18. Dong Y, Liu S, Xia D, Xu C, Yu X, Chen H, et al. Prediction model for the risk of HIV infection among MSM in China: validation and stability. Int J Environ Res Public Health. (2022) 19:1010. doi: 10.3390/ijerph19021010
19. Balaji AB, Bowles KE, Le BC, Paz-Bailey G, Oster AM. High HIV incidence and prevalence and associated factors among young MSM, 2008. AIDS. (2013) 27:269–78. doi: 10.1097/QAD.0b013e32835ad489
20. Torres TS, Coelho LE, Konda KA, Vega-Ramirez EH, Elorreaga OA, Diaz-Sosa D, et al. Low socioeconomic status is associated with self-reported HIV positive status among young MSM in Brazil and Peru. BMC Infect Dis. (2021) 21:726. doi: 10.1186/s12879-021-06455-3
21. Vergara-Ortega DN, López-Gatell H, Bautista-Arredondo S, Colchero A, Sosa-Rubí SG, Morales-Vazquez M, et al. Regional disparity of HIV incidence and prevalence among men who have sex with men. BMC Infect Dis. (2021) 21:917. doi: 10.1186/s12879-021-06582-x
22. Hu HY, Chen YH, Zhou Y, Zhang Z, Lu J, Liu XY, et al. Recent hiv infection and associated factors among men who have sex with men in Jiangsu Province. Zhonghua Liu Xing Bing Xue Za Zhi. (2021) 42:1989–93. doi: 10.3760/cma.j.cn112338-20210601-00441
23. Oldenburg CE, Perez-Brumer AG, Reisner SL, Mimiaga MJ. Transactional sex and the HIV epidemic among men who have sex with men (MSM): results from a systematic review and meta-analysis. AIDS Behav. (2015) 19:2177–83. doi: 10.1007/s10461-015-1010-5
24. Mimiaga MJ, O'Cleirigh C, Biello KB, Robertson AM, Safren SA, Coates TJ, et al. The effect of psychosocial syndemic production on 4-year HIV incidence and risk behavior in a large cohort of sexually active men who have sex with men. J Acquir Immune Defic Syndr. (2015) 68:329–36. doi: 10.1097/QAI.0000000000000475
25. Xu C, Shi Y, Yu X, Chang R, Wang H, Chen H, et al. The syndemic condition of psychosocial problems related to depression among sexually transmitted infections patients. PeerJ. (2021) 9:e12022. doi: 10.7717/peerj.12022
26. Semple SJ, Zians J, Strathdee SA, Patterson TL. Sexual marathons and methamphetamine use among HIV-positive men who have sex with men. Arch Sex Behav. (2009) 38:583–90. doi: 10.1007/s10508-007-9292-y
27. Luo M, Zhu L, Dong Y, Wang Z, Shen Q, Mo D, et al. Sexual compulsivity and its relationship with condomless sex among unmarried female migrant workers in Shanghai, China: A Cross-Sectional Study. BMC Womens Health. (2018) 18:181. doi: 10.1186/s12905-018-0670-5
28. Liao W, Lau JT, Tsui HY, Gu J, Wang Z. Relationship between sexual compulsivity and sexual risk behaviors among Chinese sexually active males. Arch Sex Behav. (2015) 44:791–8. doi: 10.1007/s10508-014-0317-z
29. Ye Z, Chen L, Lin D. The relationship between posttraumatic stress disorder symptoms and posttraumatic growth among HIV-infected men who have sex with men in Beijing, China: The Mediating Roles of Coping Strategies. Front Psychol. (2018) 9:1787. doi: 10.3389/fpsyg.2018.01787
30. Wang S, Ni Y, Gong R, Shi Y, Cai Y, Ma J. Psychosocial syndemic of suicidal ideation: a cross-sectional study among sexually transmitted infection patients in Shanghai, China. BMC Public Health. (2020) 20:1314. doi: 10.1186/s12889-020-09404-y
31. Wei D, Hou F, Hao C, Gu J, Dev R, Cao W, et al. Prevalence of intimate partner violence and associated factors among men who have sex with men in China. J Interpers Violence. (2021) 36:NP11968–NP93. doi: 10.1177/0886260519889935
32. Jiang D, Hou Y, Chen X, Wang R, Fu C, Li B, et al. Interpersonal sensitivity and loneliness among Chinese gay men: a cross-sectional survey. Int J Environ Res Public Health. (2019) 16:2039. doi: 10.3390/ijerph16112039
33. Xu C, Yu X, Tsamlag L, Zhang S, Chang R, Wang H, et al. Evaluating the validity and reliability of the Chinese entrapment scale and the relationship to depression among men who have sex with men in Shanghai, China. BMC Psychiatry. (2021) 21:328. doi: 10.1186/s12888-021-03333-9
34. Arends RM, Grintjes KJT, van den Heuvel TJ, Foeken-Verwoert EGJ, Schene AH, van der Ven A, et al. Effectiveness of a group intervention to reduce sexual transmission risk behavior among MSM Living with HIV: a non-randomized controlled pilot study. AIDS Care. (2022) 34:515–26. doi: 10.1080/09540121.2021.2002252
35. Luo R, Silenzio VMB, Huang Y, Chen X, Luo D. The disparities in mental health between gay and bisexual men following positive HIV diagnosis in China: a one-year follow-up study. Int J Environ Res Public Health. (2020) 17:3414. doi: 10.3390/ijerph17103414
36. Aunon FM, Simoni JM, Yang JP, Shiu C, Chen WT, Edmunds SR, et al. Depression and anxiety among HIV-positive men who have sex with men and men who have sex with women in China. AIDS Care. (2020) 32:362–9. doi: 10.1080/09540121.2019.1683803
37. Yang Z, Li S, Zhang R, Na J, Li Y, Mu H, et al. Current heterosexual marriage is associated with significantly decreased levels of anxiety symptoms among Chinese men who have sex with men. BMC Psychiatry. (2020) 20:151. doi: 10.1186/s12888-020-02563-7
38. Grov C, Rendina HJ. Parsons JT. Comparing three cohorts of msm sampled via sex parties, bars/clubs, and craigslistorg: implications for researchers and providers. AIDS Educ Prev. (2014) 26:362–82. doi: 10.1521/aeap.2014.26.4.362
39. Wang Y, Jia M, Yuan D, Liang A, Zhang Z, Jiang X, et al. assessing consistent condom use among migrant men who have sex with men in Shanghai, China: validation of an information-motivation-behavioural skills model. BMC Infect Dis. (2019) 19:462. doi: 10.1186/s12879-019-4090-4
40. Vu NTT, Holt M, Phan HTT, La LT, Tran GM, Doan TT, et al. Amphetamine-type-stimulants (ATS) use and homosexuality-related enacted stigma are associated with depression among men who have sex with men (MSM) in two major cities in Vietnam in 2014. Subst Use Misuse. (2017) 52:1411–9. doi: 10.1080/10826084.2017.1284233
41. Yang Y, Green SB. Coefficient alpha: a reliability coefficient for the 21st century? J Psychoeduc Assess. (2011) 29:377–92. doi: 10.1177/0734282911406668
42. Moret L, Mesbah M, Chwalow J, Lellouch J. Internal validation of a measurement scale: relation between principal component analysis, cronbach's alpha coefficient and intra-class correlation coefficient. Rev Epidemiol Sante Publique. (1993) 41:179–86.
43. Shrestha N. Factor analysis as a tool for survey analysis. Am J Appl Mathem Statistics. (2021) 9:4–11. doi: 10.12691/ajams-9-1-2
44. Kursa MB, Rudnicki WR. Feature selection with boruta package. J Stat Softw. (2010) 36:1–13. doi: 10.18637/jss.v036.i11
45. Austin PC, Tu JV. Automated variable selection methods for logistic regression produced unstable models for predicting acute myocardial infarction mortality. J Clin Epidemiol. (2004) 57:1138–46.
46. Paul P, Pennell ML, Lemeshow S. Standardizing the power of the hosmer-lemeshow goodness of fit test in large data sets. Stat Med. (2013) 32:67–80. doi: 10.1002/sim.5525
47. Newman TB, Escobar GJ. Frequency of neonatal bilirubin testing and hyperbilirubinemia in a large health maintenance organization. Ambul Pediatr. (2001) 1:126. doi: 10.1367/1539-4409
48. Cole TJ, Hey E, Richmond S. The PREM score: a graphical tool for predicting survival in very preterm births. Archf Dis Childhood Fetal Neonatal Ed. (2010) 95:F14–9. doi: 10.1136/adc.2009.164533
49. Lai X, Liu L, A. Simple test procedure in standardizing the power of hosmer–lemeshow test in large data sets. J Stat Comput Simul. (2018) 88:2463–72. doi: 10.1080/00949655.2018.1467912
50. Fan C, Ding X, Song Y, A. New prediction model for acute kidney injury in patients with sepsis. Ann Palliat Med. (2021) 10:1772–8. doi: 10.21037/apm-20-1117
51. Cao Z, Xu J, Zhang H, Song D, She M, Wang J, et al. Risk factors for syphilis among married men who have sex with men in China. Sex Transm Dis. (2014) 41:98–102. doi: 10.1097/OLQ.0000000000000074
52. Le TM, Lee PC, Stewart DE, Long TN. Quoc CN. What are the risk factors for HIV in men who have sex with men in Ho Chi Minh City, Vietnam?. Cross-Sec Study BMC Public Health. (2016) 16:406. doi: 10.1186/s12889-016-3088-8
53. Li Y-Z, Xu J-J, Qian H-Z, You B-X, Zhang J, Zhang J-M, et al. High prevalence of HIV infection and unprotected anal intercourse among older men who have sex with men in China: a systematic review and meta-analysis. BMC Infect Dis. (2014) 14:531. doi: 10.1186/1471-2334-14-531
54. Jiao K, Wei R, Li H, Chow EPF, Piqueiras E, Lewis T, et al. HIV testing frequency and associated factors among five key populations in ten cities of China: a cross-sectional study. BMC Infect Dis. (2022) 22:195.
55. Li R, Pan X, Ma Q, Hui W, Xia S. Prevalence of prior hiv testing and associated factors among MSM in Zhejiang Province, China: a cross-sectional study. BMC Public Health. (2016) 16:1152. doi: 10.1186/s12889-016-3806-2
56. Yang Z, Huang Z, Dong Z, Zhang S, Han J, Jin M. Prevalence of high-risky behaviors in transmission of HIV among high school and college student MSM in China: a meta-analysis. BMC Public Health. (2015) 15:1272. doi: 10.1186/s12889-015-2614-4
57. Ye M, Giri M. Prevalence and correlates of HIV infection among men who have sex with men: a multi-provincial cross-sectional study in the southwest of China. HIV AIDS (Auckl). (2018) 10:167–75. doi: 10.2147/HIV.S176826
58. Yang J, Xu H, Li S, Cheng W, Gu Y, Xu P, et al. The characteristics of mixing patterns of sexual dyads and factors correlated with condomless anal intercourse among men who have sex with men in Guangzhou, China. BMC Public Health. (2019) 19:722. doi: 10.1186/s12889-019-7082-9
59. Sun Y, Li G, Lu H. Awareness and use of nonoccupational HIV post-exposure prophylaxis and factors associated with awareness among MSM in Beijing, China. PLoS ONE. (2021) 16:e0255108. doi: 10.1371/journal.pone.0255108
60. Zhang Y, Peng B, She Y, Liang H, Peng HB, Qian HZ, et al. Attitudes toward HIV pre-exposure prophylaxis among men who have sex with men in western China. AIDS Patient Care STDS. (2013) 27:137–41. doi: 10.1089/apc.2012.0412
61. Jackson T, Huang A, Chen H, Gao X, Zhong X, Zhang Y. Cognitive, psychosocial, and sociodemographic predictors of willingness to use HIV pre-exposure prophylaxis among Chinese men who have sex with men. AIDS Behav. (2012) 16:1853–61. doi: 10.1007/s10461-012-0188-z
62. Wang X, Wang Z, Jiang X, Li R, Wang Y, Xu G, et al. A cross-sectional study of the relationship between sexual compulsivity and unprotected anal intercourse among men who have sex with men in Shanghai, China. BMC Infect Dis. (2018) 18:465. doi: 10.1186/s12879-018-3360-x
63. He L, Pan X, Yang J, Ma Q, Jiang J, Wang W, et al. HIV risk behavior and HIV testing among rural and urban men who have sex with men in Zhejiang Province, China: a respondent-driven sampling study. PLoS ONE. (2020) 15:e0231026.
64. Long JE, Montao M, Cabello R, Sanchez H, Lama JR, Duerr A. Brief report: comparing sexual risk behavior in a high-risk group of men who have sex with men and transgender women in Lima, Peru. JAIDS J Acquired Immune Deficiency Syndr. (2019) 80:522. doi: 10.1097/QAI.0000000000001966
65. Whittle HJ, Palar K, Napoles T, Hufstedler LL, Ching I, Hecht FM, et al. Experiences with food insecurity and risky sex among low-income people living with HIV/AIDS in a resource-rich setting. J Int AIDS Soc. (2015) 18:20293. doi: 10.7448/IAS.18.1.20293
66. Liu Z, Chen Y, Yao T, Zhang T, Song D, Liu Y, et al. Factors related to HIV testing frequency in MSM based on the 2011–2018 survey in Tianjin, China: a hint for risk reduction strategy. BMC Public Health. (2021) 21:1900. doi: 10.1186/s12889-021-11948-6
67. Wu W, Yan X, Zhang X, Goldsamt L, Chi Y, Huang D, et al. Potential HIV transmission risk among spouses: marriage intention and expected extramarital male-to-male sex among single men who have sex with men in Hunan, China. Sex Transm Infect. (2020) 96:151–6. doi: 10.1136/sextrans-2018-053906
68. Mao H, Ma W, Lu H, Wang L, Zheng H, Zhu Y, et al. High incidence of HIV and syphilis among migrant men who have sex with men in Beijing, China: a prospective cohort study. BMJ Open. (2014) 4:e005351. doi: 10.1136/bmjopen-2014-005351
69. Mi G, Ma B, Kleinman N, Li Z, Fuller S, Bulterys M, et al. Hidden and mobile: a web-based study of migration patterns of men who have sex with men in China. Clin Infect Dis. (2016) 62:1443–7. doi: 10.1093/cid/ciw167
70. He X, Ren Y, Ma Z, Guo W, Jin C, Xing W. (2021). Evaluatiing the Effects of HIV Self-testing used Professional Rapid Test Kits among MSM in Some Areas of China. doi: 10.21203/rs.3.rs-1019127/v1
71. Dai W, Luo Z, Xu R, Zhao G, Tu D, Yang L, et al. Prevalence of HIV and syphilis co-infection and associated factors among non-commercial men who have sex with men attending a sexually transmitted disease clinic in Shenzhen, China. BMC Infect Dis. (2017) 17:86. doi: 10.1186/s12879-017-2187-1
72. Wei L, Chen L, Zhang H, Yang Z, Zou H, Yuan T, et al. Use of gay app and the associated HIV/syphilis risk among non-commercial men who have sex with men in shenzhen, china: a serial cross-sectional study. Sex Transm Infect. (2019) 95:496–504. doi: 10.1136/sextrans-2018-053902
73. De Santis JP, Colin JM, Provencio Vasquez E, McCain GC. The relationship of depressive symptoms, self-esteem, and sexual behaviors in a predominantly hispanic sample of men who have sex with men. Am J Men's Health. (2008) 2:314–21. doi: 10.1177/1557988307312883
74. Pharr JR, Lough NL, Ezeanolue EE. Barriers to HIV testing among young men who have sex with men (MSM): experiences from clark county, Nevada. Glob J Health Sci. (2015) 8:9–17. doi: 10.5539/gjhs.v8n7p9
75. Maatouk I, Jaspal R. Increasing PREP uptake in MSM at risk of HIV in lebanon: some social psychological insights. Acad Lett. (2021). doi: 10.20935/AL2529
76. Jayawardena M, Pepping CA, Lyons A, Hill AO. Geosocial networking application use in men who have sex with men: the role of adult attachment. Sex Res Social Policy. (2021) 19:85–90. doi: 10.1007/s13178-020-00526-x
77. Zervoulis K, Smith DS, Reed R, Dinos S. Use of ‘Gay Dating Apps' and its relationship with individual well-being and sense of community in men who have sex with men. Psychol Sex. (2019) 11:88–102. doi: 10.1080/19419899.2019.1684354
78. Greene M, Hessol NA, Perissinotto C, Zepf R, Hutton Parrott A, Foreman C, et al. Loneliness in older adults living with HIV. AIDS Behav. (2018) 22:1475–84. doi: 10.1007/s10461-017-1985-1
79. West DA, Kellner R, Moore-West M. The effects of loneliness: a review of the literature. Compr Psychiatry. (1986) 27:351–63. doi: 10.1016/0010-440X(86)90011-8
80. Giano Z, Hubach RD, Deboy K, Meyers H, Currin JM, Wheeler DL, et al. Comparative analysis of rural and urban MSM depressive symptomology: the mediating effects of loneliness. Psychol Sex. (2019) 10:200–11. doi: 10.1080/19419899.2019.1593885
81. Gilbert P, Allan S. The role of defeat and entrapment (arrested flight) in depression: an exploration of an evolutionary view. Psychol Med. (1998) 28:585–98. doi: 10.1017/S0033291798006710
82. Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. Am J Public Health. (2012) 102:156–62. doi: 10.2105/AJPH.2011.300284
83. Amaral ML, Abdo CH. Tavares H, Scanavino Mde T. Personality among sexually compulsive men who practice intentional unsafe sex in São Paulo, Brazil. J Sex Med. (2015) 12:557–66. doi: 10.1111/jsm.12761
84. Esser S, Krotzek J, Dirks H, Scherbaum N, Schadendorf D. Sexual risk behavior, sexually transmitted infections, and HIV transmission risks in HIV-positive men who have sex with men (MSM)—approaches for medical prevention. J Dtsch Dermatol Ges. (2017) 15:421–8. doi: 10.1111/ddg.13217
85. Coleman CL. Physical and psychological abuse among seropositive African American MSM 50 aged years and older. Issues Ment Health Nurs. (2018) 39:46–52. doi: 10.1080/01612840.2017.1397828
86. Griffiths AW, Wood AM, Maltby J, Taylor PJ, Tai S. The prospective role of defeat and entrapment in depression and anxiety: a 12-month longitudinal study. Psychiatry Res. (2014) 216:52–9. doi: 10.1016/j.psychres.2014.01.037
87. Siddaway AP, Taylor PJ, Wood AM, Schulz J, A. Meta-analysis of perceptions of defeat and entrapment in depression, anxiety problems, posttraumatic stress disorder, and suicidality. J Affect Disord. (2015) 184:149–59. doi: 10.1016/j.jad.2015.05.046
88. Sun S, Pachankis JE Li X, Operario D. Addressing minority stress and mental health among men who have sex with men (MSM) in China. Curr HIV/AIDS Rep. (2020) 17:35–62. doi: 10.1007/s11904-019-00479-w
89. Tao J, Qian HZ, Kipp AM, Ruan Y, Shepherd BE, Amico KR, et al. Effects of depression and anxiety on antiretroviral therapy adherence among newly diagnosed HIV-infected Chinese MSM. AIDS. (2017) 31:401–6. doi: 10.1097/QAD.0000000000001287
90. Lincoln SH, Johnson T, Laquidara JR, Wilt J, Obeid R. Increased rates of social defeat and schizotypy in racial minorities. Person Ind Diff. (2022) 186:111324. doi: 10.1016/j.paid.2021.111324
91. Nagata S, Seki Y, Shibuya T, Yokoo M, Murata T, Hiramatsu Y, et al. Does cognitive behavioral therapy alter mental defeat and cognitive flexibility in patients with panic disorder? BMC Res Notes. (2018) 11:23. doi: 10.1186/s13104-018-3130-2
92. Gilbert P, Allan S, Brough S, Melley S, Miles J. Relationship of anhedonia and anxiety to social rank, defeat and entrapment. J Affect Disord. (2002) 71:141–51. doi: 10.1016/S0165-0327(01)00392-5
93. Gyamerah AO, Taylor KD, Atuahene K, Anarfi JK, Fletcher M, Raymond HF, et al. Stigma, discrimination, violence, and HIV testing among men who have sex with men in four major cities in Ghana. AIDS Care. (2020) 32:1036–44. doi: 10.1080/09540121.2020.1757020
94. Sun S, Sun X, Wei C, Shi L, Zhang Y, Operario D, et al. Domestic violence victimization among men who have sex with men in china during the COVID-19 lockdown. J Interpers Violence. (2022):8862605211072149. doi: 10.1177/08862605211072149
95. Micheni M, Rogers S, Wahome E, Darwinkel M, van der Elst E, Gichuru E, et al. Risk of sexual, physical and verbal assaults on men who have sex with men and female sex workers in coastal Kenya. AIDS. (2015) 29 Suppl 3:S231–6. doi: 10.1097/QAD.0000000000000912
96. Brown MJ, Serovich JM, Kimberly JA. Depressive symptoms, substance use and partner violence victimization associated with hiv disclosure among men who have sex with men. AIDS Behav. (2016) 20:184–92. Msm N. 2011. AIDS Behav. (2017) 21:227–37. doi: 10.1007/s10461-015-1122-y
97. Balaji AB, Bowles KE, Hess KL, Smith JC, Paz-Bailey G, Group NS. Association between enacted stigma and HIV-related risk behavior among MSM, national HIV behavioral surveillance system, 2011. AIDS Behav. (2017) 21:227–37. doi: 10.1007/s10461-016-1599-z
98. Murphy EC, Segura ER, Lake JE, Huerta L, Perez-Brumer AG, Mayer KH, et al. Intimate partner violence against transgender women: prevalence and correlates in Lima, Peru (2016–2018). AIDS Behav. (2020) 24:1743–51.
99. Ali NS, Azam IS, Ali BS, Tabbusum G, Moin SS. Frequency and associated factors for anxiety and depression in pregnant women: a hospital-based cross-sectional study. SciWorldJ. (2012) 2012:653098. doi: 10.1007/s10461-019-02728-w
100. Keiley MK, Keller PS, El-Sheikh M. Effects of physical and verbal aggression, depression, and anxiety on drinking behavior of married partners: a prospective and retrospective longitudinal examination. Aggress Behav. (2009) 35:296–312. doi: 10.1100/2012/653098
101. Teicher MH, Samson JA, Sheu YS, Polcari A, Mcgreenery CE. Hurtful words: association of exposure to peer verbal abuse with elevated psychiatric symptom scores and corpus callosum abnormalities. Am J Psychiatry. (2010) 167:1464–71. doi: 10.1176/appi.ajp.2010.10010030
102. Morell-Mengual V, Gil-Llario MD, Fernadez-Garcia O, Ballester-Arnal R. Factors associated with condom use in anal intercourse among spanish men who have sex with men: proposal for an explanatory model. AIDS Behav. (2021) 25:3836–45. doi: 10.1007/s10461-021-03282-0
103. Nydegger LA, Walsh JL. Strength of implementation intentions to use condoms among men who have sex with men. AIDS Behav. (2018) 22:3491–9.
104. Nwaosu U, Raymond-Williams R, Meyrick J. Are psychosocial interventions effective at increasing condom use among black men? A Syst Rev Int J STD AIDS. (2021) 32:1088–105.
105. Hu L, Luo Y, Zhong X, Lu R, Wang Y, Sharma M, et al. Condom use and related factors among rural and urban men who have sex with men in western china: based on information-motivation-behavioral skills model. Am J Mens Health. (2020) 14:1557988319899799.
106. Wu MY, Gong HZ, Hu KR, Zheng HY, Wan X, Li J. Effect of syphilis infection on hiv acquisition: a systematic review and meta-analysis. Sex Transm Infect. (2021) 97:525–33. doi: 10.1177/1557988319899799
107. Branger J, van der Meer JT, van Ketel RJ, Jurriaans S, Prins JM. High incidence of asymptomatic syphilis in hiv-infected msm justifies routine screening. Sex Transm Dis. (2009) 36:84–5. doi: 10.1136/sextrans-2020-054706
108. Chen L, Yang J, Ma Q, Pan X. Prevalence of active syphilis infection and risk factors among HIV-positive MSM in Zhejiang, China in 2015: a cross-sectional study. Int J Environ Res Public Health. (2019) 16:1507. doi: 10.3390/ijerph16091507
109. Karp G, Schlaeffer F, Jotkowitz A, Riesenberg K. Syphilis and HIV co-infection. Eur J Intern Med. (2009) 20:9–13.
Keywords: prediction model, nomogram, internal migrant MSM, HIV, random forests, stepwise selection, univariable selection
Citation: Liu S, Xia D, Wang Y, Xu H, Xu L, Yuan D, Liang A, Chang R, Wang R, Liu Y, Chen H, Hu F, Cai Y and Wang Y (2022) Predicting the risk of HIV infection among internal migrant MSM in China: An optimal model based on three variable selection methods. Front. Public Health 10:1015699. doi: 10.3389/fpubh.2022.1015699
Received: 10 August 2022; Accepted: 04 October 2022;
Published: 25 October 2022.
Edited by:
Shanquan Chen, University of Cambridge, United KingdomReviewed by:
C MA, University of Cambridge, United KingdomHarry H. X. Wang, Sun Yat-sen University, China
Yunfei Li, National Center for Global Health and Medicine, Japan
Yanning Li, Guangxi Medical University, China
Fan Zhang, Hainan Medical University, China
Copyright © 2022 Liu, Xia, Wang, Xu, Xu, Yuan, Liang, Chang, Wang, Liu, Chen, Hu, Cai and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fan Hu, joyking2003@163.com; Yong Cai, caiyong202028@hotmail.com; Ying Wang, yingwangxun@outlook.com
†These authors have contributed equally to this work
 Shangbin Liu1†
Shangbin Liu1† Lulu Xu
Lulu Xu Fan Hu
Fan Hu Yong Cai
Yong Cai Ying Wang
Ying Wang