- National Research Centre for the Working Environment, Copenhagen, Denmark
Objective: This study aimed to investigate the association between perceived stress and odds of low-back pain (LBP) in a population of Danish healthcare workers.
Methods: Utilizing a prospective cohort design with 1-year follow-up, a total of 1,944 healthcare workers from 389 departments at 19 hospitals responded to questionnaires containing items related to lifestyle, health, and working environment. Using Cohen's Perceived Stress Scale, associations between baseline stress levels and LBP intensity (0–10 scale) at follow-up were modeled using cumulative logistic regression, accounting for clustering at the department level and adjusting for age, sex, baseline intensity of LBP, education, seniority, number of daily patient transfers, psychosocial work environment, and lifestyle factors.
Results: For the entire population, moderate and high stress (reference: low stress) at baseline increased the odds of LBP at 1-year follow-up with odds ratios (ORs) of 1.39 (95% CI 1.13–1.71) and 1.99 (95% CI 1.49–2.66), respectively. Sensitivity analyses among female nurses showed similar results [i.e., OR 1.40 (95% CI 1.08–1.80) and OR 2.08 (95% CI 1.44–3.00) for moderate and high stress, respectively], while only high stress significantly increased the odds among those without LBP at baseline.
Conclusions: Psychological stress increases the odds of LBP among healthcare workers. Identifying and diminishing work-related psychosocial stressors should be included in strategies that aim to prevent musculoskeletal disorders in this population.
Introduction
The physiological phenomenon known as “stress” is—in animals and humans alike—most often characterized as the result of real or perceived threat to the organism, typically as a reaction to various external exposures (1). However, while the bi-directional stress processes between the brain and the cardiovascular, autonomic, and immune systems are essential in promoting short-term allosteric adaptations to stressors with the noble, primary goal of maintaining homeostasis, exposure to long-term stressful conditions leads to a wide array of negative health consequences (1, 2).
Indeed, persistent stress has been associated with numerous indicators of poor health, including abnormal cortisol patterns (3), depression and anxiety (4), type II diabetes (5), obesity (6), poor sleep (7, 8), persistent pain (9, 10) as well as cardiovascular- and all-cause mortality (11). Generally, greater lifetime stress severity predicts poor mental and physical health (2, 12, 13), and cumulative exposure to work-related stressors has been linked to absenteeism from work, increased healthcare costs, and decreased job performance (14–17). Following this, several work-related situational- and environmental stressors have been identified in the literature, including high job demands, poor support from colleagues, reward imbalance, job insecurity, and over-commitment (16, 18–21).
Specifically among healthcare workers, work-related stress has been associated with job (dis)satisfaction, burnout as well as poor mental- and physical health outcomes (22). Additionally, it is likely that certain job groups within the realm of healthcare are exposed to more work-related stressors than others: For example, a recent study among healthcare workers showed that nurses in primary care experience higher levels of perceived stress and lower levels of subjective well-being compared with their colleagues (23), indicating that this subgroup of the working population may exhibit an increased risk of negative health outcomes due to work-related stress. This notion needs to be considered in relation to the myriad of work-related factors known to influence pain among healthcare workers (24, 25), among which indicators of stress (e.g., emotional exhaustion, high emotional demands, and poor psychosocial safety climate) are known to significantly amplify the risk of musculoskeletal pain (24, 26).
However, while increases in cortisol levels have been shown to precede increases in pain levels hours later (27), it is currently unclear to what extent stress exacerbates future pain levels in healthcare workers. Therefore, the primary aim of this study was to investigate associations between baseline stress levels and odds of low-back pain (LBP) at 1-year follow-up in a population of Danish healthcare workers. Additionally, sensitivity analyses were performed, including individuals with and without LBP at baseline.
Methods
Utilizing a prospective cohort design with baseline- and 1-year follow-up questionnaires, this study presents associations between stress levels and LBP intensity. Specifically, using Cohen's Perceived Stress Scale (28), we investigated associations between subjectively measured stress levels at baseline and odds of a one-point increase on the Visual Analog Scale at follow-up.
Prior to this analysis, we have previously published associations between lifestyle factors and the outcome of poor sleep and pain (8, 29), as well as data on the prospective association between patient transfers and back injury (30).
Study Design and Participants
The baseline questionnaire was sent to 7,025 hospital workers from 389 departments at 19 hospitals in Denmark, of which 4,151 (59%) responded to the full questionnaire. Comparatively, Millar and Dillman (31) found an average of 42% response rate for web-based questionnaires, while Baruch (32)—based on 175 studies and more than 200,000 respondents—report a mean (SD) response rate of 55.6% (19.7).
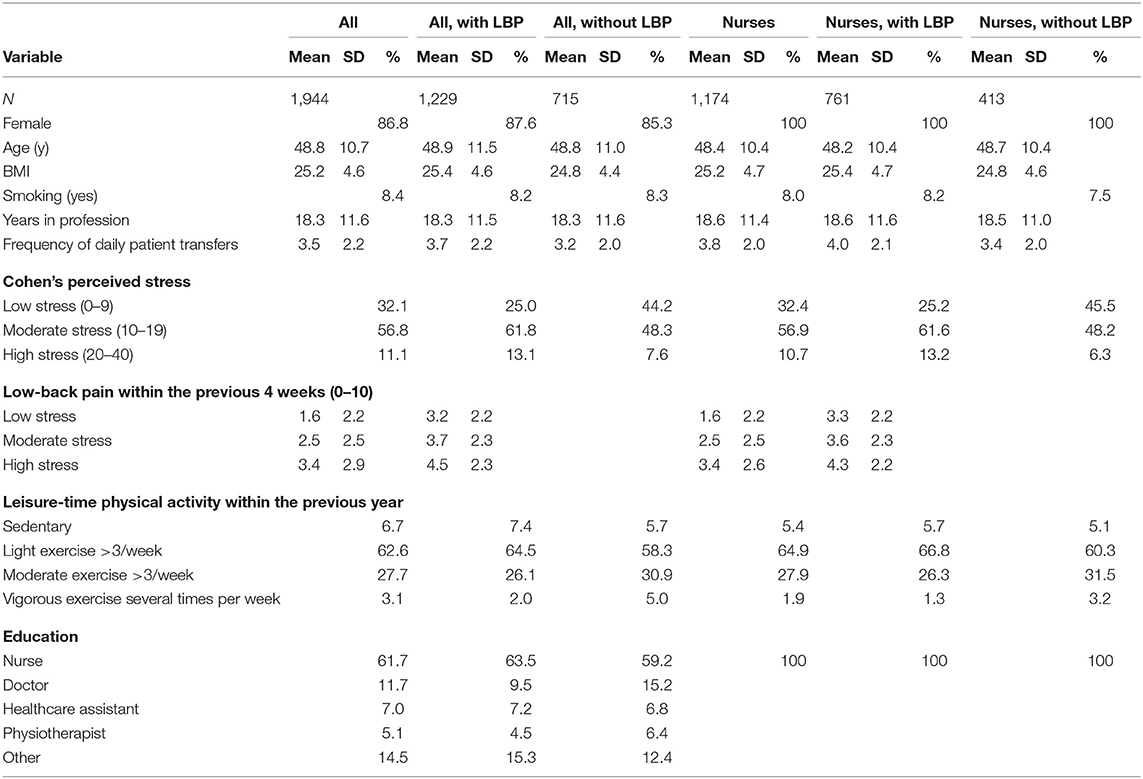
In this analysis, we included healthcare workers who frequently engage with patients (i.e., nurses, healthcare assistants, nurses' aides, physical and occupational therapists, medical doctors, midwives, porters, and radiologists) and who responded to both baseline and follow-up questionnaires, yielding a final sample size of 1,944 healthcare workers. Furthermore, in subsequent sensitivity analyses, this study also includes associations specific to workers with and without LBP at baseline (n = 1,229 and n = 715, respectively), as well as to the subpopulation of nurses (n = 1,174), nurses without LBP (n = 413), and nurses with LBP at baseline (n = 761). Table 1 shows the baseline characteristics of the included participants.
Outcome and Predictor Variables
The intensity of LBP was quantified by the following question:
Rate your pain for the low-back within the previous 4 weeks (0–10, where 0 is no pain and 10 is worst imaginable pain).
Stress levels of the participants were quantified using Cohen's Perceived Stress Scale, the Danish version of which exhibits satisfactory validity, reliability, and internal consistency (33). It is a widely used instrument designed to measure “the degree to which individuals appraise situations in their lives as stressful” (28), and the scale shows well-established psychometric properties across populations (34, 35). Furthermore, it is often used as an outcome measure in intervention research (36, 37), allowing for the measurement of psychological stress among large cohorts. Presently, the 10-item questionnaire was used, with each item rated on a five-point Likert scale (ranging from “never” to “almost always”). The scores were subsequently summed, with higher scores indicative of higher levels of perceived stress. The normative values (mean ± SD) in the general population are 12.1 (5.9) and 13.7 (6.6) for men and women, respectively, with scores >20 considered as high (28). Therefore, a summed score between 0 and 9 was considered as “low,” 10–19 as “moderate,” and >20 as “high” in the present analysis.
Covariates
In the “Results” section below, we report fully adjusted associations between baseline stress level and prospective odds of a one-point increase in LBP intensity. The analysis accounts for the following possible confounders relating to the individual, psychosocial, and working environment: Age, sex, LBP at baseline, education, body mass index, smoking, seniority, physical activity during leisure time, and frequency of patient transfer—as well as for factors related to the psychosocial work environment, i.e., recognition and influence at work.
Ethics
By agreement with the Danish Data Protection Agency, the National Research Centre for the Working Environment is allowed to register all questionnaire studies in-house. According to Danish law, questionnaire- and register-based studies need neither informed consent nor approval from ethical and scientific committees. All data were de-identified and analyzed anonymously.
Statistics
Associations between stress at baseline and LBP at follow-up were modeled using cumulative logistic regression (Proc Genmod, SAS), i.e., odds ratios (ORs) express the odds of LBP increasing one point on the 0–10 scale. Analyses were adjusted for the aforementioned covariates. To account for clustering, hospital department was entered in the “repeated subject” statement. Estimates are provided as ORs and 95% confidence intervals.
Results
Among healthcare workers who were pain-free at baseline, we report LBP intensities of 0.65 (SD 1.57), 0.74 (SD 1.42), and 1.52 (SD 2.06) at 1-year follow-up for the low-, moderate-, and high-stress groups, respectively. For the sub-population of nurses who were pain-free at baseline, LBP intensities of 0.75 (SD 1.69), 0.74 (SD 1.44), and 1.5 (SD 1.9) for the three groups were reported at follow-up.
Furthermore, using “low stress” as reference, this study reports fully adjusted associations between stress levels and odds of an increase in LBP at follow-up among the full population of Danish healthcare workers (moderate stress: OR 1.44, 95% CI 1.12–1.86; high stress: OR 2.30, 95% CI 1.61–3.29). In the subgroup population who were pain-free at baseline, high stress—but not moderate stress—was significantly associated with increased odds (moderate stress: OR 1.25, 95% CI 0.89–1.76; high stress: OR 2.67, 95% CI 1.51–4.75). Likewise, in the sensitivity analysis including female nurses, high stress—but not moderate stress—was associated with increased odds at follow-up (moderate stress: OR 1.34, 95% CI 0.97–1.86; high stress: OR 3.17, 95% CI 1.88–5.37). Finally, in the subgroup of female nurses who were pain-free at baseline, high stress—but not moderate stress—was associated with increased odds of developing LBP (moderate stress: OR 1.09, 95% CI 0.71–1.69; high stress: OR 3.13, 95% CI 1.28–7.70) (Table 2).
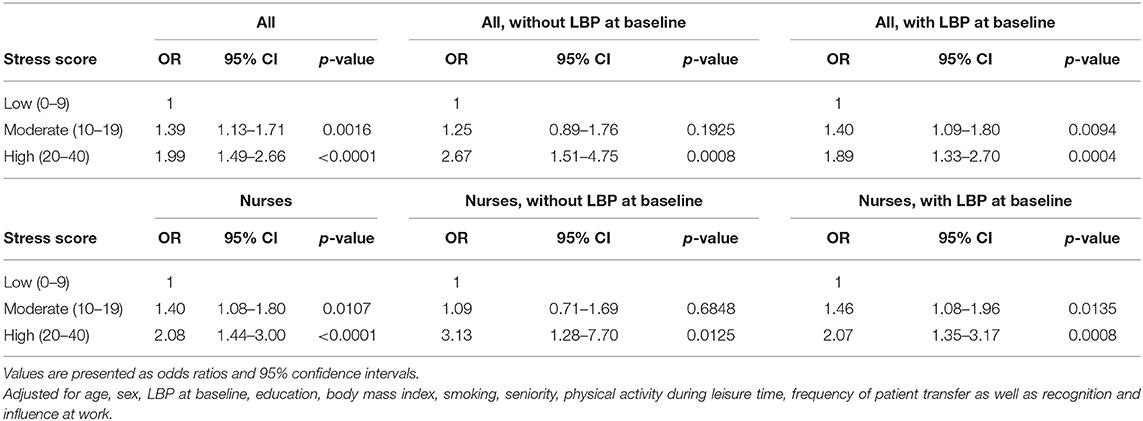
Table 2. Stress level and odds of 1-point increase in low-back pain intensity (0–10) at 1-year follow-up.
Discussion
This study shows robust associations between perceived stress and increased odds of LBP among healthcare workers, utilizing Cohen's Perceived Stress Scale and the Visual Analog Scale, respectively. Specifically, for the whole population, a clear relationship was identified between stress levels (moderate and high) and increased odds of LBP at follow-up, while only high stress was associated with increased odds in the population free from LBP at baseline as well as for the subgroup of female nurses. This is important new knowledge in this occupational group, in which traditional preventive strategies have focused almost solely on ergonomic factors.
The main finding of this study—i.e., high stress being consistently associated with greater odds of future LBP—is in congruence with the existing literature on the relationship between psychosocial stress and pain (9, 10, 27, 38–40). For example, the population-based prospective cohort study by McBeth et al. (39) found that increased levels of evening-cortisol predicts the onset of persistent widespread pain at 15-months follow-up. Likewise, a Danish cross-sectional study including 4,739 adults reported strong associations between perceived stress and the use of over-the-counter analgesics (41). In the present cohort of healthcare workers, we find that baseline stress levels are highly predictive of increases in LBP intensity 1 year later, indicating that—among this and similar populations of the workforce—perceived stress constitutes a potent risk factor for developing future musculoskeletal disorders. Considering the biopsychosocial model of health by Engel (42), it is clear that individual perception of stress can be related to (and initiated by) an array of biomedical, psychological, and social stressors, presenting themselves in all shapes and sizes. For example, job demands, job control, over-commitment at the workplace, and social support from colleagues have been shown to predict stress outcomes (43), whereas emotional exhaustion was recently identified as a strong predictor of work-related injuries among healthcare workers (26). In relation to pain, the biopsychosocial model acknowledges potent influences such as catastrophizing, fear avoidance, expectation, meaning, context, etc.; all indicative of the substantial contribution arising from various psychosocial stressors (44). Following this, psychosocial stress in the workplace is traditionally gauged within the framework of the job demand–control model introduced by Karasek (45), describing work-related stress as an ongoing balancing act between strain/demands and control/support (45). However, in order to fully understand the dynamic bi-directional processes taking place during work-related stress (i.e., interactions between individual capacity and environmental stressors) as well as to shed light on the inconsistent relationships between various work-related stressors and performance, the conservation of resources theory (46) and the challenge–hindrance model (47) have since emerged. In combination, these frameworks emphasize the role of individual psychosocial factors (e.g., fluctuating psychological resources such as self-efficacy and the resulting difference as to whether a stressor is viewed as a challenge or hindrance), hereby further acknowledging the complexity of maneuvering a hierarchical, socially constructed workplace.
Collectively and despite historical disagreement on how to quantify stress, work-related stress is defined as “the general process in which individuals respond to and manage demands to meet multiple goals over time” (48). The results from the present study indicates that, regardless of the origin and nature of work-related stressors, high levels of perceived stress are strongly associated with increased odds of LBP, which—paradoxically—may very well turn into an additional stressor. This, in turn, initiates a rapacious circle in which the stressors and the stress response often become equally entangled and indistinguishable. This notion is echoed in the “Results” section, illustrating that participants experiencing pain at baseline are more like to suffer an increase in LBP due to moderate stress levels compared to their pain-free counterparts. Therefore, to counteract this, it appears critical that the ill-famed working environment in healthcare—known to cultivate high ratings of perceived exertion (49, 50), high prevalence of musculoskeletal disorders (25) as well as high levels of fatigue and stress (51)—undergo a substantial overhauling and reevaluation of core principles. The overarching aim of identifying and improving potent psychosocial influencers/stressors inherent to the local working environment should take precedence, as these issues arguably constitute the low-hanging fruits of this conundrum.
Strengths and Limitations
Limitations of this study include the risk of underreporting of musculoskeletal disorders, recall- and non-response bias as well as ambiguity related to questions and questionnaire design; all inherent to questionnaire surveys (52–54). Additionally, although the vast majority of LBP cases are classified as “non-specific” (55, 56), the quantitative method used does not allow for the identification of possible contributors to pain in this population.
Strengths of this study include the adjustment for various confounders and inclusion of sensitivity analyses specific to nurses and pain-free participants as well as using Cohen's Perceived Stress Scale as a widely used and validated indicator of perceived stress. Finally, this analysis combines the advantages of a relatively large sample size, a prospective design as well as statistical adjustments for known physical- and psychosocial confounders. Future studies aiming to elaborate on these results should, if possible, include longer follow-up periods to confirm the robustness as well as to determine the generalizability of the presented results outside the hospital environment.
Conclusion
In this cohort of Danish healthcare workers, perceived psychosocial stress was strongly associated with increased risk of LBP at 1-year follow-up, whereas being pain-free at baseline attenuated this relationship. Identifying and diminishing potent psychosocial stressors inherent to the local working environment are paramount in combating the high prevalence of musculoskeletal disorders seen in this population.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JV drafted the manuscript. MJ and LA revised it critically. All authors contributed substantially to the conception of the project as well as to the analysis and the interpretation of data, and provided approval for publication.
Funding
LA obtained a grant from the Danish Working Environment Research Fund for this study (Grant Number AMFF 26-2015-09).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wholeheartedly thank the healthcare workers for participating in the study.
References
1. McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease: central links between stress and SES. Ann N Y Acad Sci. (2010) 1186:190–222. doi: 10.1111/j.1749-6632.2009.05331.x
2. Toussaint L, Shields GS, Dorn G, Slavich GM. Effects of lifetime stress exposure on mental and physical health in young adulthood: how stress degrades and forgiveness protects health. J Health Psychol. (2016) 21:1004–14. doi: 10.1177/1359105314544132
3. Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol Bull. (2007) 133:25–45. doi: 10.1037/0033-2909.133.1.25
4. Doane LD, Mineka S, Zinbarg RE, Craske M, Griffith JW, Adam EK. Are flatter diurnal cortisol rhythms associated with major depression and anxiety disorders in late adolescence? The role of life stress and daily negative emotion. Dev Psychopathol. (2013) 25:629–42. doi: 10.1017/S0954579413000060
5. Harris ML, Oldmeadow C, Hure A, Luu J, Loxton D, Attia J. Stress increases the risk of type 2 diabetes onset in women: a 12-year longitudinal study using causal modelling. PLoS ONE. (2017) 12:e0172126. doi: 10.1371/journal.pone.0172126
6. Tomiyama AJ. Stress and obesity. Annu Rev Psychol. (2019) 70:703–18. doi: 10.1146/annurev-psych-010418-102936
7. Lo Martire V, Caruso D, Palagini L, Zoccoli G, Bastianini S. Stress & sleep: a relationship lasting a lifetime. Neurosci Biobehav Rev. (2019). doi: 10.1016/j.neubiorev.2019.08.024. [Epub ahead of print].
8. Vinstrup J, Jakobsen MD, Calatayud J, Jay K, Andersen LL. Association of stress and musculoskeletal pain with poor sleep: cross-sectional study among 3,600 hospital workers. Front Neurol. (2018) 9:968. doi: 10.3389/fneur.2018.00968
9. Arguelles LM, Afari N, Buchwald DS, Clauw DJ, Furner S, Goldberg J. A twin study of posttraumatic stress disorder symptoms and chronic widespread pain. Pain. (2006) 124:150–7. doi: 10.1016/j.pain.2006.04.008
10. Corcoran L, Roche M, Finn DP. Chapter six - the role of the Brain's endocannabinoid system in pain and its modulation by stress. In: Parsons L, Hill M, editors. International Review of Neurobiology. Endocannabinoids. Galway: Academic Press (2015). p. 203–55. doi: 10.1016/bs.irn.2015.10.003
11. Kumari M, Shipley M, Stafford M, Kivimaki M. Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: findings from the Whitehall II study. J Clin Endocrinol Metab. (2011) 96:1478–85. doi: 10.1210/jc.2010-2137
12. Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. (2007) 298:1685–7. doi: 10.1001/jama.298.14.1685
13. Ganster DC, Rosen CC. Work stress and employee health: a multidisciplinary review. J Manag. (2013) 39:1085–122. doi: 10.1177/0149206313475815
14. Ganster DC, Fox ML, Dwyer DJ. Explaining employees' health care costs: a prospective examination of stressful job demands, personal control, and physiological reactivity. J Appl Psychol. (2001) 86:954–64. doi: 10.1037/0021-9010.86.5.954
15. Heo YS, Leem JH, Park SG, Jung DY, Kim HC. Job stress as a risk factor for absences among manual workers: a 12-month follow-up study. Ind Health. (2015) 53:542–52. doi: 10.2486/indhealth.2015-0021
16. Jackson AT, Frame MC. Stress, health, and job performance: what do we know? J Appl Biobehav Res. (2018) 23:e12147. doi: 10.1111/jabr.12147
17. Nisar SK, Rasheed MI. Stress and performance: investigating relationship between occupational stress, career satisfaction, and job performance of police employees. J Public Aff. (2019) 20:e1986. doi: 10.1002/pa.1986
18. D'Souza RM, Strazdins L, Broom DH, Rodgers B, Berry HL. Work demands, job insecurity and sickness absence from work. how productive is the new, flexible labour force? Aust N Z J Public Health. (2006) 30:205–12. doi: 10.1111/j.1467-842X.2006.tb00859.x
19. Eddy P, Wertheim EH, Hale MW, Wright BJ. A systematic review and meta-analysis of the effort-reward imbalance model of workplace stress and hypothalamic-pituitary-adrenal axis measures of stress. Psychosom Med. (2018) 80:103–13. doi: 10.1097/PSY.0000000000000505
20. Head J, Kivimäki M, Siegrist J, Ferrie JE, Vahtera J, Shipley MJ, et al. Effort-reward imbalance and relational injustice at work predict sickness absence: the Whitehall II study. J Psychosom Res. (2007) 63:433–40. doi: 10.1016/j.jpsychores.2007.06.021
21. Julià M, Catalina-Romero C, Calvo-Bonacho E, Benavides FG. The impact of job stress due to the lack of organisational support on occupational injury. Occup Environ Med. (2013) 70:623–9. doi: 10.1136/oemed-2012-101184
22. Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. IJERPH. (2015) 12:652–66. doi: 10.3390/ijerph120100652
23. Atanes ACM, Andreoni S, Hirayama MS, Montero-Marin J, Barros VV, Ronzani TM, et al. Mindfulness, perceived stress, and subjective well-being: a correlational study in primary care health professionals. BMC Complement Altern Med. (2015) 15:303. doi: 10.1186/s12906-015-0823-0
24. Boocock MG, Trevelyan F, Ashby L, Ang A, Diep N, Teo S, et al. The influence of psychosocial and patient handling factors on the musculoskeletal health of nurses. In: Bagnara S, Tartaglia R, Albolino S, Alexander T, Fujita Y, editors. Proceedings of the 20th Congress of the International Ergonomics Association (IEA 2018). Cham: Springer International Publishing (2018). p. 596–603. doi: 10.1007/978-3-319-96083-8_78
25. Ribeiro T, Serranheira F, Loureiro H. Work related musculoskeletal disorders in primary health care nurses. Appl Nurs Res. (2017) 33:72–7. doi: 10.1016/j.apnr.2016.09.003
26. Zadow AJ, Dollard MF, Mclinton SS, Lawrence P, Tuckey MR. Psychosocial safety climate, emotional exhaustion, and work injuries in healthcare workplaces. Stress Health. (2017) 33:558–69. doi: 10.1002/smi.2740
27. Fischer S, Doerr JM, Strahler J, Mewes R, Thieme K, Nater UM. Stress exacerbates pain in the everyday lives of women with fibromyalgia syndrome—The role of cortisol and alpha-amylase. Psychoneuroendocrinology. (2016) 63:68–77. doi: 10.1016/j.psyneuen.2015.09.018
28. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
29. Vinstrup J, Jakobsen MD, Andersen LL. Poor sleep is a risk factor for low-back pain among healthcare workers: prospective cohort study. Int J Environ Res Public Health. (2020) 17:996. doi: 10.3390/ijerph17030996
30. Andersen LL, Vinstrup J, Villadsen E, Jay K, Jakobsen MD. Physical and psychosocial work environmental risk factors for back injury among healthcare workers: prospective cohort study. Int J Environ Res Public Health. (2019) 16:4528. doi: 10.3390/ijerph16224528
31. Millar MM, Dillman DA. Improving response to web and mixed-mode surveys. Public Opin Q. (2011) 75:249–69. doi: 10.1093/poq/nfr003
32. Baruch Y. Response rate in academic studies-a comparative analysis. Hum Relat. (1999) 52:421–38. doi: 10.1177/001872679905200401
33. Eskildsen A, Dalgaard VL, Nielsen KJ, Andersen JH, Zachariae R, Olsen LR, et al. Cross-cultural adaptation and validation of the Danish consensus version of the 10-item perceived stress scale. Scand J Work Environ Health. (2015) 41:486–90. doi: 10.5271/sjweh.3510
34. Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res. (2012) 6:121–7. doi: 10.1016/j.anr.2012.08.004
35. Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the perceived stress scale. J Coll Couns. (2006) 9:135–47. doi: 10.1002/j.2161-1882.2006.tb00100.x
36. Sood A, Prasad K, Schroeder D, Varkey P. Stress management and resilience training among department of medicine faculty: a pilot randomized clinical trial. J Gen Intern Med. (2011) 26:858–61. doi: 10.1007/s11606-011-1640-x
37. Willert MV, Thulstrup AM, Hertz J, Bonde JP. Changes in stress and coping from a randomized controlled trial of a three-month stress management intervention. Scand J Work Environ Health. (2009) 35:145–52. doi: 10.5271/sjweh.1313
38. Booker S, Cardoso J, Cruz-Almeida Y, Sibille KT, Terry EL, Powell-Roach KL, et al. Movement-evoked pain, physical function, and perceived stress: an observational study of ethnic/racial differences in aging non-Hispanic Blacks and non-Hispanic whites with knee osteoarthritis. Exp Gerontol. (2019) 124:110622. doi: 10.1016/j.exger.2019.05.011
39. McBeth J, Silman AJ, Gupta A, Chiu YH, Ray D, Morriss R, et al. Moderation of psychosocial risk factors through dysfunction of the hypothalamic–pituitary–adrenal stress axis in the onset of chronic widespread musculoskeletal pain : findings of a population-based prospective cohort study. Arthritis Rheum. (2007) 56:360–71. doi: 10.1002/art.22336
40. Tsuboi Y, Ueda Y, Naruse F, Ono R. The association between perceived stress and low back pain among eldercare workers in Japan. J Occup Environ Med. (2017) 59:765–7. doi: 10.1097/JOM.0000000000001062
41. Koushede V, Holstein BE, Andersen A, Ekholm O, Hansen EH. Use of over-the-counter analgesics and perceived stress among 25–44-year olds. Pharmacoepidemiol Drug Saf. (2010) 19:351–7. doi: 10.1002/pds.1897
42. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. (1977) 196:129–36. doi: 10.1126/science.847460
43. Adriaenssens J, Hamelink A, Bogaert PV. Predictors of occupational stress and well-being in first-line nurse managers: a cross-sectional survey study. Int J Nurs Stud. (2017) 73:85–92. doi: 10.1016/j.ijnurstu.2017.05.007
44. Moseley GL. Reconceptualising pain according to modern pain science. Phys Ther Rev. (2007) 12:169–78. doi: 10.1179/108331907X223010
45. Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. (1979) 24:285–308. doi: 10.2307/2392498
46. Hobfoll SE. Conservation of resources. A new attempt at conceptualizing stress. Am Psychol. (1989) 44:513–24. doi: 10.1037/0003-066X.44.3.513
47. Lepine JA, Podsakoff NP, Lepine MA. A meta-analytic test of the challenge stressor–hindrance stressor framework: an explanation for inconsistent relationships among stressors and performance. AMJ. (2005) 48:764–75. doi: 10.5465/amj.2005.18803921
48. Griffin MA, Clarke S. Stress and well-being at work. In: Zedeck S, editor. APA Handbook of Industrial and Organizational Psychology, Vol 3: Maintaining, Expanding, and Contracting the Organization. Bentley, KS: American Psychological Association (2011). p. 359–97. doi: 10.1037/12171-010
49. Jakobsen MD, Sundstrup E, Brandt M, Jay K, Aagaard P, Andersen LL. Physical exercise at the workplace reduces perceived physical exertion during healthcare work: cluster randomized controlled trial. Scand J Public Health. (2015) 43:713–20. doi: 10.1177/1403494815590936
50. Vieira ER, Kumar S, Coury HJCG, Narayan Y. Low back problems and possible improvements in nursing jobs. J Adv Nurs. (2006) 55:79–89. doi: 10.1111/j.1365-2648.2006.03877.x
51. Zboril-Benson LR. Why nurses are calling in sick: the impact of health-care restructuring. Can J Nurs Res. (2002) 33:89–107. Available online at: https://cjnr.archive.mcgill.ca/article/download/1660/1660
52. Menzel NN. Underreporting of musculoskeletal disorders among health care workers: research needs. AAOHN J. (2008) 56:487–94. doi: 10.3928/08910162-20081201-06
53. Cheung KL, ten Klooster PM, Smit C, de Vries H, Pieterse ME. The impact of non-response bias due to sampling in public health studies: a comparison of voluntary versus mandatory recruitment in a Dutch national survey on adolescent health. BMC Public Health. (2017) 17:276. doi: 10.1186/s12889-017-4189-8
54. Choi BCK, Pak AWP. A catalog of biases in questionnaires. Prev Chronic Dis. (2004) 2:A13. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1323316/pdf/PCD21A13.pdf
55. O'Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther. (2005) 10:242–55. doi: 10.1016/j.math.2005.07.001
Keywords: Cohen, psychological stress, pain, workplace, nurses, healthcare
Citation: Vinstrup J, Jakobsen MD and Andersen LL (2020) Perceived Stress and Low-Back Pain Among Healthcare Workers: A Multi-Center Prospective Cohort Study. Front. Public Health 8:297. doi: 10.3389/fpubh.2020.00297
Received: 22 January 2020; Accepted: 04 June 2020;
Published: 11 August 2020.
Edited by:
Marissa G. Baker, University of Washington, United StatesReviewed by:
Yuke Tien Fong, Singapore General Hospital, SingaporeEvangelia Nena, Democritus University of Thrace, Greece
Copyright © 2020 Vinstrup, Jakobsen and Andersen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jonas Vinstrup, jov@nfa.dk
†ORCID: Jonas Vinstrup orcid.org/0000-0001-8430-0139
 Jonas Vinstrup
Jonas Vinstrup Markus D. Jakobsen
Markus D. Jakobsen Lars L. Andersen
Lars L. Andersen