- 1College of Health Science, Oda Bultum University, Chiro, Ethiopia
- 2Department of Midwifery, College of Health Science, Oda Bultum University, Chiro, Ethiopia
- 3Department of Public Health, College of Medicine and Health Science, Debre Markos University, Debre Markos, Ethiopia
- 4Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 5Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
Introduction: Anxiety and depression are among the common comorbidities of people diagnosed with cancer. However, despite the progress in therapeutic options and outcomes, mental health care and support have lagged behind for cancer patients. Estimating the extent and determinants of mental health disorders among cancer patients is crucial to alert concerned bodies for action. In view of this, we aimed to determine the pooled prevalence and determinants of anxiety and depression among cancer patients in Ethiopia.
Methods: Relevant literatures were searched on PubMed, African Journals Online, Hinari, Epistemonikos, Scopus, EMBASE, CINAHL, Cochrane Library, and Gray literature sources. Data were extracted into an Excel spreadsheet and analyzed using STATA 17 statistical software. The random effect model was used to summarize the pooled effect sizes with their respective 95% confidence intervals. The I2 statistics and Egger’s regression test in conjunction with the funnel plot were utilized to evaluate heterogeneity and publication bias among included studies respectively.
Results: A total of 17 studies with 5,592 participants were considered in this review. The pooled prevalence of anxiety and depression among cancer patients in Ethiopia were 45.10% (95% CI: 36.74, 53.45) and 42.96% (95% CI: 34.98, 50.93), respectively. Primary and above education (OR= 0.76, 95% CI: 0.60, 0.97), poor social support (OR= 2.27, 95% CI: 1.29, 3.98), occupational status (OR= 0.59; 95% CI: 0.43, 0.82), advanced cancer stage (OR= 2.19, 95% CI: 1.38, 3.47), comorbid illness (OR= 1.67; 95% CI: 1.09, 2.58) and poor sleep quality (OR= 11.34, 95% CI: 6.47, 19.89) were significantly associated with depression. Whereas, advanced cancer stage (OR= 1.59, 95% CI: 1.15, 2.20) and poor sleep quality (OR= 12.56, 95% CI: 6.4 1, 24.62) were the factors associated with anxiety.
Conclusion: This meta-analysis indicated that a substantial proportion of cancer patients suffer from anxiety and depression in Ethiopia. Educational status, occupational status, social support, cancer stage, comorbid illness and sleep quality were significantly associated with depression. Whereas, anxiety was predicted by cancer stage and sleep quality. Thus, the provision of comprehensive mental health support as a constituent of chronic cancer care is crucial to mitigate the impact and occurrence of anxiety and depression among cancer patients. Besides, families and the community should strengthen social support for cancer patients.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42023468621.
Introduction
In the recent world, non-communicable diseases have become common and cancer is among the leading causes of death worldwide accounting for 1 every 6 deaths (1). In 2018, World Health Organization (WHO) estimated that cancer caused about 18 million new cases and 9.6 million deaths worldwide (2). Cancer is known to cause immature death mainly if it reaches an advanced stage without diagnosis and treatment. In addition, cancer is related to disturbing the victim’s psychological health by causing common mental health disorders like depression and anxiety (3). The burden of cancer is far higher in developing countries due to different factors mainly socio-demographic and weak prevention and control methods. In Ethiopia, cancer accounts for about 5.8% of total national mortality, and the incidence of cancer is estimated to be at least 60960 cases, and a death rate of more than 44000 each year (4).
Being diagnosed with cancer may cause many complex feelings and lifestyle changes in people who are diagnosed with it, and many people feel to blame for getting cancer and suffer from psychological disorders like depression and anxiety (5, 6). Depression and anxiety are known to complicate the lives of patients with cancer than the general population. More than 300 million people are now living with depression, an increase of more than 18% between 2005 and 2015 in the general population (7), whereas approximately half of all patients with cancer have common psychological disorders such as anxiety and depression (8). Both depression and anxiety among patients with cancer are associated with complicating the outcome of the cancer treatment since they have to take medications for both cancer and depression or anxiety, lower adherence, extend hospitalization, reduce the quality of life, increase the risk of suicide and predict cancer advancement and mortality (9–13).
Anxiety and depression co-morbidity among cancer patients is common in underdeveloped settings (14). In Ethiopia, few studies reported the magnitude of anxiety and depression among cancer patients. However, they present inconsistent findings and failed to summarize the national figure. For instance, depression was found to affect 15.3% to 70.9% of respondents (15, 16), whereas anxiety was figured from 27.8% to 64.9% (17, 18). This demonstrates substantial variation among previous studies.
These common mental disorders are related to various factors that make them more common, as per different literature. Factors like age, education level, poor patient-provider interaction, social support, financial support, sleep quality, and stage of cancer were documented as significant predictors of anxiety and depression among cancer patients (6, 16, 19, 20). Nevertheless, their importance varies between studies.
Although it needs global attention, most of the studies regarding common mental disorders among cancer patients came from the developed world (21), while very limited studies addressed the subject in low-income countries like Ethiopia (6, 18, 22). Even those studies showed no stated national level of depression and anxiety among patients with cancer. In addition, there is no consistent finding regarding associated factors of depression and anxiety among those studies. Therefore, this study aimed to assess the pooled prevalence and determinants of depression and anxiety among cancer patients in Ethiopia.
Materials and methods
Protocol registration and reporting
The protocol of this systematic review is available in the international database of the Prospective Register of Systematic Reviews (PROSPERO) with registration number CRD42023468621. This review closely followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement (23).
Search strategy
We did a comprehensive literature search on PubMed, African Journals Online (AJOL), Hinari, Epistemonikos, Scopus, EMBASE, CINAHL, and Cochrane Library to retrieve relevant articles. In addition, other gray literature like Google Scholar and online repositories of Ethiopian universities were audited. The reference list of pertinent articles was also scrutinized to identify additional studies. Two independent reviewers (HG and MBS) searched the databases from September 5 to October 5, 2023. The following keywords were used for the search: Prevalence OR “Period Prevalence” OR “Point Prevalence” OR Magnitude OR Epidemiology) AND (“Associated factor*” OR Determinant* OR Factor* OR “Risk factor*”) AND (Depression OR “Depressive Symptoms” OR “Emotional Depression” OR Anxiety OR Angst OR Anxiousness OR “Social Anxiety” OR “Anxiety Disorders”) AND (Neoplasm* OR “Benign Neoplasm*” OR Cancer OR Malignancy OR “Malignant Neoplasm” OR “Malignant Neoplasms” OR Neoplasia OR Benign OR Tumor*) AND (Ethiopia).
Eligibility criteria
All observational studies published in the English language and reported the prevalence and/or determinants of anxiety and/or depression among cancer patients in Ethiopia were included in this review. Nonetheless, clinical trials, duplicate studies, editorial letters, qualitative studies, and abstracts without full text were excluded from this analysis.
Population: Cancer patients
Setting: Studies conducted only in Ethiopia
Exposure: predictors of anxiety and depression. These are attributes of cancer patients that may increase or decrease their likelihood of developing anxiety and depression, such as educational status, social support, cancer stage, sleep quality, and so forth.
Outcome: anxiety and depression
Outcome of interest
Our primary outcome of interest was the magnitude of anxiety and depression among cancer patients in Ethiopia. In this analysis, the hospital anxiety and depression scale (HADS) with a cut-off point ≥ 8, and the patient health questionnaire (PHQ) with a cut-off point ≥ 10, were used to diagnose anxiety and depression among cancer patients (15, 22). Secondly, we also sought to identify determinants of anxiety and depression among cancer patients in Ethiopia.
Study selection, quality assessment, and data extraction
Studies were assessed according to their titles and abstracts after duplicates were eliminated. For studies found to be suitable by title and abstract, a full-text review against pre-defined inclusion/exclusion criteria was done to determine potential articles to be included in this analysis. Reference management software (Endnote version X7.2) was used to combine database search results, manage the citation process, and remove duplicate entries.
Quality of included studies was assessed using the Joanna Brigg’s Institute (JBI) quality assessment checklist (24), (Supplementary File 1). Two authors of the review (HG and MBS) independently evaluated the quality of each study and inconsistencies were resolved by involving a third author (SA).
The data were extracted into to Excel spreadsheet using a standard data extraction form that was developed considering the JBI guide for data extraction and synthesis (25). Two independent authors extracted records of primary studies and then cross-checked one another. Extracted data include last name of the first author and year of publication, study area, study participants (all cancer patients or specific cancer type), methods employed (hospital anxiety and depression scale or patient health questionnaire), outcome reported (anxiety and/or depression), sample size and prevalence of anxiety and/or depression. Besides, data about determinants of anxiety and/or depression were also abstracted in a two-by-two table format.
Data processing and analysis
Data were extracted using the Excel spreadsheet and then imported to STATA version 17 software for further statistical analysis. The prevalence and its standard error of each primary study were considered to calculate the pooled prevalence estimates. The random effects model was used to pool the prevalence of anxiety and depression, and estimates were presented by forest plots. Heterogeneity between included studies was assessed using the I2 statistics and it was regarded as high, moderate, or low when I2 test statistics results were 75%, 50%, and 25% respectively (26). Eggers regression test in conjunction with funnel plot was used to evaluate publication bias and a p-value of less than 0.05 was considered to declare the presence of publication bias (27). In light of the high heterogeneity among included studies, subgroup analysis was conducted by study area and method of diagnosis to further explore it. Besides, a leave-one-out sensitivity analysis was done to evaluate the impact of each study on the overall estimate.
Results
Study selection
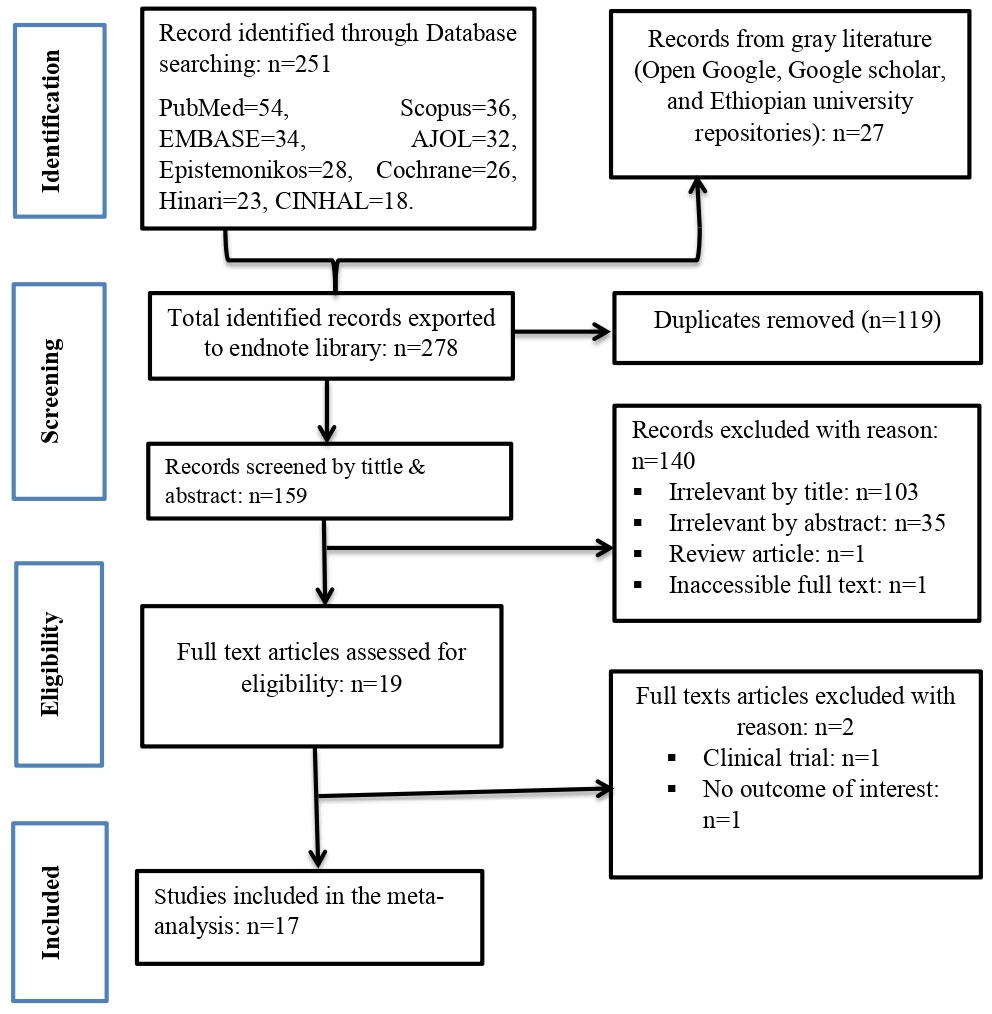
The combined literature search gave us a total of 278 studies. After the removal of 119 duplicate studies, 159 studies were screened by reviewing their title and abstract of which 140 articles were irrelevant. The full texts of 19 studies were assessed and 17 studies were deemed suitable for inclusion in this meta-analysis (Figure 1).
Characteristics of included studies
Among the 17 studies included in this analysis, one study reported anxiety alone (28), five studies reported depression alone (15, 16, 29–31), while the remaining 11 studies reported both depression and anxiety (6, 17, 18, 20, 22, 32–37). Correspondingly, the magnitudes of anxiety and depression were determined by pooling findings of 12 (6, 17, 18, 20, 22, 28, 32–37) and 16 (6, 15–18, 20, 22, 29–37) studies respectively. All included studies utilized institutional based cross-sectional study design with a sample size ranging from 77 (34), to 428 (31). Two studies included breast cancer patients only (31, 33), while others included all malignancies (6, 15–18, 20, 22, 28–30, 32, 34–37). All included primary studies involved cancer patients who were receiving care. Regarding the methods of diagnosis, 12 studies utilized the hospital anxiety and depression scale (6, 17, 18, 20, 22, 28, 32–37), while five studies used the patient health questionnaire (15, 16, 29–31). Nine of the studies were conducted in the national capital, Addis Ababa (15, 18, 22, 28–33), whereas eight of the included studies were conducted in different regions of the country (6, 16, 17, 20, 34–37) (Table 1).
Prevalence of anxiety and depression
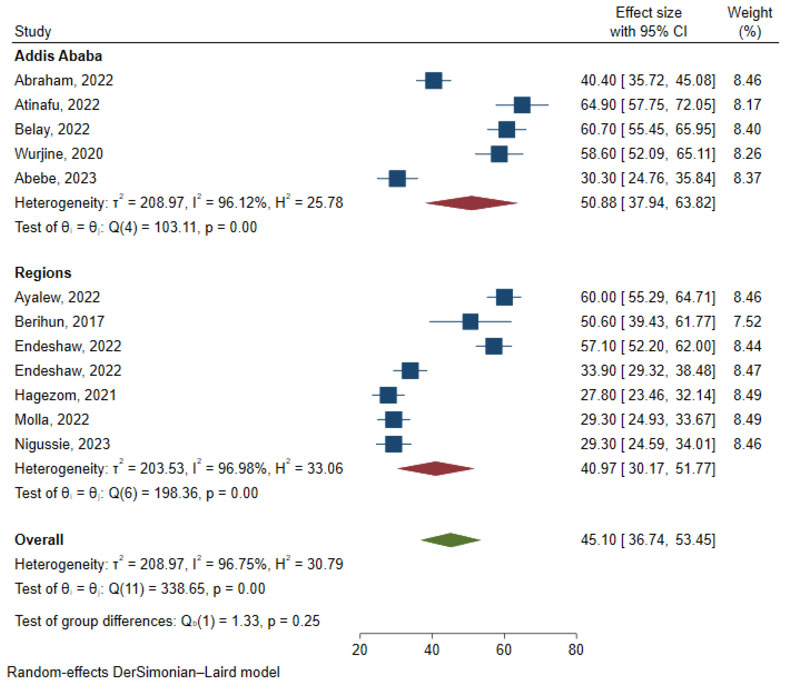
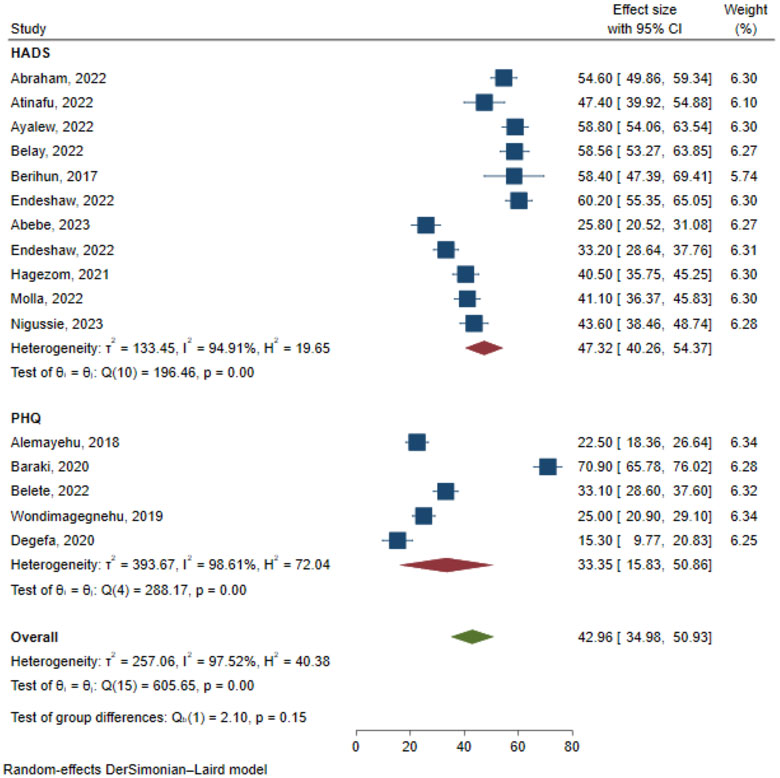
The results of 12 studies involving 3,889 respondents indicated that the overall pooled prevalence of anxiety among cancer patients in Ethiopia was 45.10% (95% CI: 36.74, 53.45) (Figure 2). Egger’s regression test indicated that there was no evidence of publication bias (p = 0.173). The symmetrical funnel plot further strengthens this finding (Figure 3).
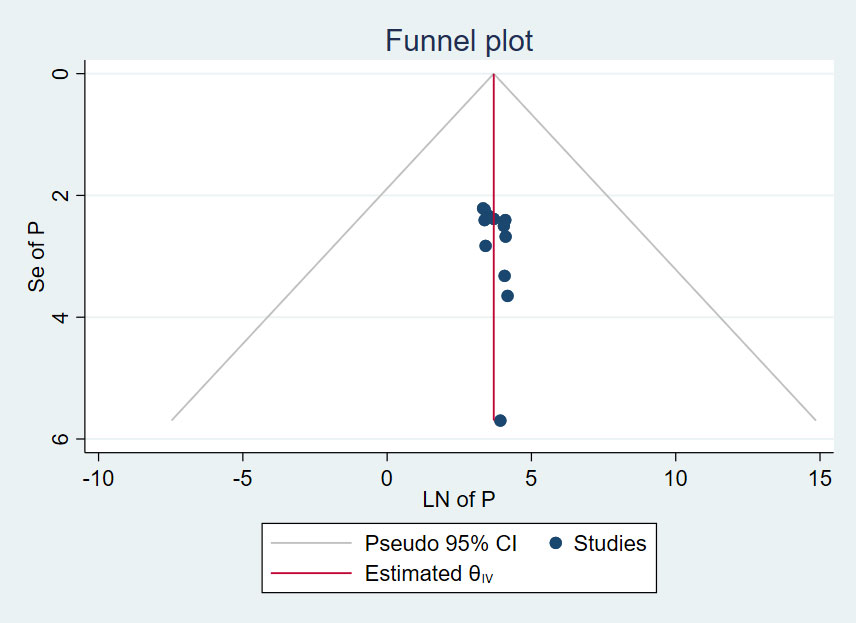
Figure 3 Funnel plot, evaluating existence of publication bias for prevalence of anxiety among cancer patients in Ethiopia.
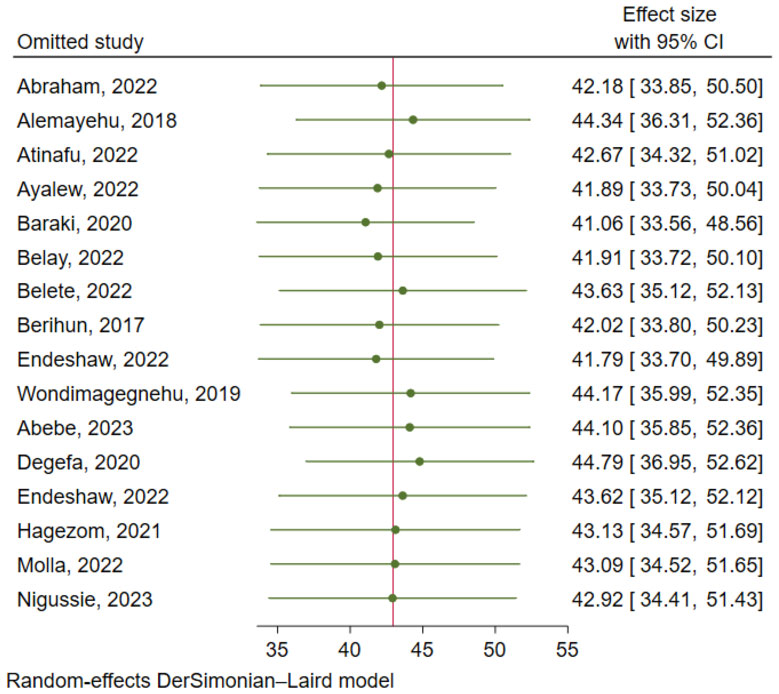
After pooling the results of 16 studies with 5,372 participants, the estimated overall prevalence of depression among cancer patients in Ethiopia was 42.96% (95% CI: 34.98, 50.93) (Figure 4). Findings of Egger’s regression test (p = 0.237) and funnel plot (Figure 5) indicated no evidence of publication bias.
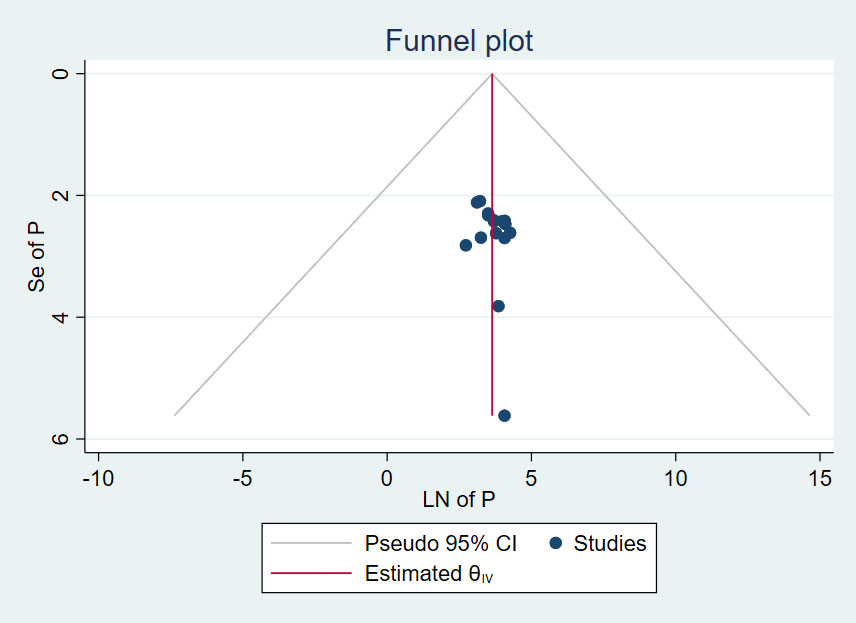
Figure 5 Funnel plot, evaluating the existence of publication bias for prevalence of depression among cancer patients in Ethiopia.
Heterogeneity and publication bias
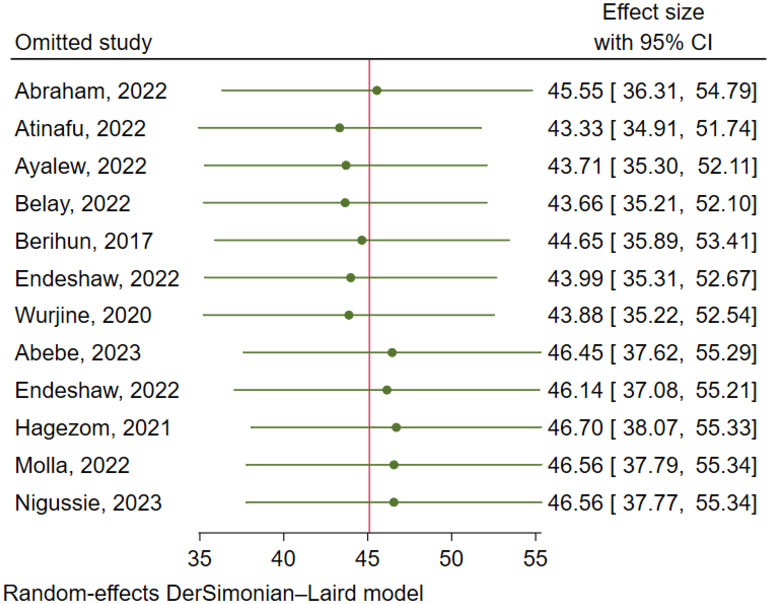
There was a significant level of heterogeneity among included studies for both the anxiety and depression analysis with the Cochrane I2 values of 96.75% and 97.52% respectively. To account for this substantial heterogeneity, the random effect model (DerSimonian-Laird method) was used to determine the pooled estimates. In both cases, there was no evidence of publication bias as depicted by a symmetrical funnel plot and insignificant Egger’s regression test. In addition, a leave-one-out sensitivity analysis was employed to investigate the influence of each study on the overall estimate. As a result, the pooled estimates of anxiety (Figure 6) and depression (Figure 7) among cancer patients in Ethiopia were steady and reliable when analyzed by omitting one study at a time.
Factors associated with anxiety
Data about five different variables (marital status, educational status, cancer stage, sleep quality, and social support) were extracted in a two-by-two table and analyzed separately. As a result, the pooled effect size of two variables (cancer stage and sleep quality) showed a significant association with anxiety. Accordingly, the likelihood of experiencing anxiety symptoms was 59% higher among individuals with advanced-stage cancer than individuals with non-advanced cancer (OR= 1.59; 95% CI: 1.15, 2.20). Similarly, cancer patients who had poor sleep quality were 12.56 (95% CI: 6.41, 24.62) times more likely to experience anxiety than their counterparts (Table 2). On the other hand, pooling the effect size of some variables deemed meaningless because of the marked variation in categories between the primary studies. For instance, six studies investigated the association between age and occurrence of anxiety; five of them found no significant association between age and anxiety, even if some of the studies treated age as continuous variable while others categorized it (6, 20, 28, 33, 34). In contrast, one study showed a statistically significant association between age and anxiety, where older patients had higher risk of anxiety (18). But, combining the effect size of those studies is misleading because of the heterogeneous categories between studies. Besides, some reports treated age as continuous variable while others categorized it.
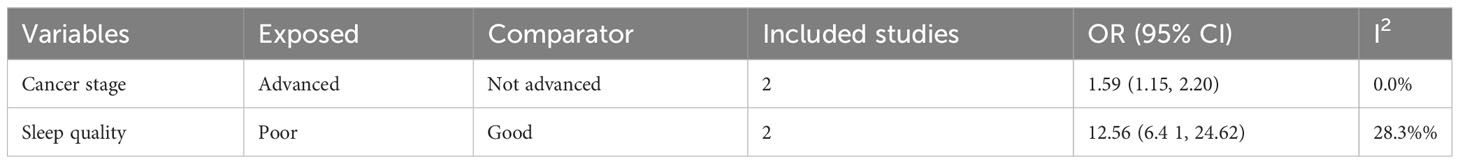
Table 2 Summary estimate of OR for factors associated with anxiety among cancer patients in Ethiopia.
Factors associated with depression
For predictors of depression, data about all variables that were reported to have a significant association in one of the included studies and also recorded in at least one other study (with or without significant association) were extracted in a two-by-two table and analyzed separately. Subsequently, data about the association between depression and nine independent variables (sex, educational status, occupational status, stage of cancer, anatomical site of cancer, sleep quality, social support, nutritional status and presence of other comorbid illness) were extracted into excel spreadsheet and analyzed separately. The pooled effects of six variables (educational status, occupational status, stage of cancer, sleep quality, social support and comorbid illness) indicated a significant association with depression among cancer patients in Ethiopia. Correspondingly, the risk of depression was 24% lower among cancer patients who had attended formal education (primary or above) as compared to those who had not attended formal education (OR= 0.76; 95% CI: 0.60, 0.97). Unemployed cancer patients had 41% higher risk of depression than employed ones (OR= 0.59; 95% CI: 0.43, 0.82). Patients who had advanced-stage cancer were more than two times more likely to suffer from depression than their counterparts (OR= 2.19; 95% CI: 1.38, 3.47). Similarly, the odds of depression were about 11 times higher among cancer patients who had poor sleep quality than those who had good sleep quality (OR= 11.34; 95% CI: 6.47, 19.89). Cancer patients who had other comorbid illness were 1.67 times more likely to suffer from depression than cancer patients who did not had comorbid illness (OR= 1.67; 95% CI: 1.09, 2.58). Lastly, we found that cancer patients who received poor social support had a higher risk of depression as compared to those who received strong social support (OR= 2.27; 95% CI: 1.29, 3.98) (Table 3).
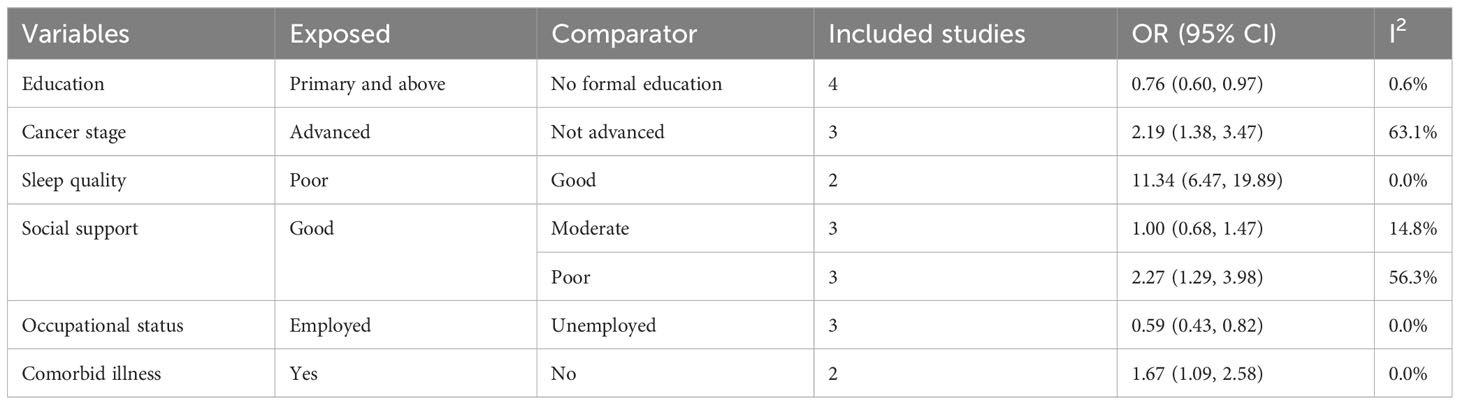
Table 3 Summary estimate of OR for factors associated with depression among cancer patients in Ethiopia.
However, some variables like age were differently categorized across studies, thus making effect size combination inappropriate. Generally, nine studies assessed the association between age and depression. Of these, five studies indicated that age was not significantly associated with depression (16, 18, 20, 29, 34), whereas four studies reported a statistically significant association between age and depression, out of which three of them showed higher risk of depression among younger patients (22, 31, 33), while one study showed higher risk of depression among older cancer patients (6). This variation between studies might be due to the difference in age categorization and/or sample size across the primary studies.
Discussion
In spite of the development in therapeutic options and outcomes, mental health care and support have lagged behind for cancer patients (38). The problem is more prominent in underdeveloped settings where there are prevalent cases, adding to the poor resources needed to implement comprehensive care for people with cancer (39). Estimating the extent and determinants of mental health disorders among cancer patients is crucial to alert concerned bodies for action. In view of this, this study was conducted to estimate the magnitude of anxiety and depression among cancer patients in Ethiopia.
In this review, the pooled prevalence of anxiety among cancer patients in Ethiopia was 45.10% (95% CI: 36.74, 53.45). The estimate is in line with a recent meta-analysis by Hashemi et.al, 41.9% (40). This finding is also congruent with recent meta-analysis conducted in Iran 40.9% (41), and China 38% (42). However, our estimate was quite high when compared to a meta-analysis of studies from developed settings, 15.09% (43). This variation could be explained in part by the large difference in socioeconomic status and healthcare quality between high-income and low-income countries (39).
The pooled estimate of depression among cancer patients in Ethiopia was 42.96% (95% CI: 34.98, 50.93). Our depression estimate was also in line with other meta-analyses from China 38% (42), and Iran 50.1% (41). Nevertheless, the depression prevalence estimate in this study was higher than in a previous meta-analysis conducted in Low- and Lower-Middle–Income Countries 21% (39). The possible explanation for this variation might be due to the difference in methods employed to assess depression (44). The differences in study design, study settings, and sample size could also be another elucidation for the observed discrepancy.
The present study also identified factors associated with depression and anxiety. Educational status, social support, stage of cancer, and sleep quality were found to have a significant association with depression. Whereas, stage of cancer and sleep quality were significant determinants of anxiety. Accordingly, stage of cancer and sleep quality were significantly associated with both anxiety and depression. The odds of depression were more than two times higher among patients with advanced-stage cancer than their counterparts. Similarly, the risk of anxiety symptoms was 59% higher among individuals with advanced stage of cancer than individuals with non-advanced cancer. These findings are supported by earlier reports (45, 46). This might be due to the physical impediment and disability to perform activities of daily living with the advancement of cancer (47). The odds of anxiety and depression were also higher among cancer patients who had poor sleep quality as compared to their counterparts. This might be due to the cognitive deterioration and other sleep-induced physiological changes associated with poor sleep (48). Hence, implies the importance of including regular and good sleep pattern counseling in chronic cancer care (49).
This study showed that cancer patients who had attended formal (primary or above) education had a 24% lower risk of depression as compared to those who had not attended formal education. This association was also demonstrated by previous studies conducted in Germany (19), and India (50). This might be due to the lack of knowledge and understanding about the disease they are diagnosed with among patients without formal education (51). Unemployed cancer patients had a 41% higher risk of depression than employed ones. This association was also documented in a previous meta-analysis (52). The possible explanation for this association might be that unemployed individuals frequently have unhealthy lifestyle and habits, which in turn raise their risk of depression (53).
In the present study, cancer patients with poor social support had more than twofold risk of depression than those with good social support. This association was also documented by previous studies (46, 54), and underlines the key role of social support in mitigating the negative impact of cancer diagnosis and treatment through the belonging and care they receive from others (55). Similarly, cancer patients who had other comorbid illness were more likely to suffer from depression than their counterparts. This might be due to the increased therapeutic burden and physical deterioration associated with other comorbid illness (56).
This analysis is not without limitations. Firstly, some important variables were not considered in this analysis due to differences in categorization across included primary studies. Secondly, studies published only in the English language were included in this review. Finally, all studies included in this analysis employed cross-sectional design, hence temporal associations are difficult to infer. In addition, all participants included in primary studies were cancer patients who were receiving care, hence the rate of anxiety and depression cannot be depicted by treatment status of cancer patients.
Conclusion
This meta-analysis found that a substantial proportion of cancer patients suffer from anxiety and depression in Ethiopia. Educational status, occupational status, social support, cancer stage, comorbid illness and sleep quality were significantly associated with depression. Whereas, anxiety was predicted by cancer stage and sleep quality. Thus, the provision of comprehensive mental health support as a constituent of chronic cancer care is crucial to mitigate the impact and occurrence of anxiety and depression among cancer patients. Besides, families and the community should strengthen social support for cancer patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
HG: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SA: Data curation, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. EM: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. WT: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. AH: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. TT: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. AM: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. MM: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. BE: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. MB: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. LA: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – review & editing. MS: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We thank the authors of included studies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1341448/full#supplementary-material
Abbreviations
AOR, Adjusted odds ratio; CI, Confidence interval; HADS, Hospital anxiety and depression scale; PHQ, Patient health questionnaire.
References
1. WHO. WHO Report on Cancer: Setting Priorities, Investing Wisely and Providing Care for all (2020). Available at: https://www.who.int/publications/i/item/9789240001299.
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin (2018) 68:394–424. doi: 10.3322/caac.21492
3. Naser AY, Hameed AN, Mustafa N, Alwafi H, Dahmash EZ, Alyami HS, et al. Depression and anxiety in patients with cancer: a cross-sectional study. Front Psychol (2021) 12:1067. doi: 10.3389/fpsyg.2021.585534
4. Fedral Ministry of Health of Ethiopia: National cancer control plan 2016–2020. In: Addis Ababa Disease Prevention and Control Directorate, Editor Directorate Dpac. Available at: https://www.iccp-portal.org/sites/default/files/plans/NCCP%20Ethiopia%20Final%20261015.pdf.
5. Gregurek R, Braš M, Đorđević V, Ratković A-S, Brajković L. Psychological problems of patients with cancer. Psychiatria Danubina (2010) 22:227–30. Available at: https://hrcak.srce.hr/55684.
6. Ayalew M, Deribe B, Duko B, Geleta D, Bogale N, Gemechu L, et al. Prevalence of depression and anxiety symptoms and their determinant factors among patients with cancer in southern Ethiopia: a cross-sectional study. BMJ Open (2022) 12:e051317. doi: 10.1136/bmjopen-2021-051317
7. WHO. Depression and Other Common Mental Disorders: Global Health Estimates Geneva: World Health Organization (2017).
8. Barrera I, Spiegel D. Review of psychotherapeutic interventions on depression in cancer patients and their impact on disease progression. Int Rev Psychiatry (2014) 26:31–43. doi: 10.3109/09540261.2013.864259
9. Wang Y-H, Li J-Q, Shi J-F, Que J-Y, Liu J-J, Lappin JM, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry (2020) 25:1487–99. doi: 10.1038/s41380-019-0595-x
10. Pitman A, Suleman S, Hyde N, Hodgkiss A. Depression and anxiety in patients with cancer. Bmj (2018) 361. doi: 10.1136/bmj.k1415
11. Prieto JM, Blanch J, Atala J, Carreras E, Rovira M, Cirera E, et al. Psychiatric morbidity and impact on hospital length of stay among hematologic cancer patients receiving stem-cell transplantation. J Clin Oncol (2002) 20:1907–17. doi: 10.1200/JCO.2002.07.101
12. Wang X, Wang N, Zhong L, Wang S, Zheng Y, Yang B, et al. Prognostic value of depression and anxiety on breast cancer recurrence and mortality: a systematic review and meta-analysis of 282,203 patients. Mol Psychiatry (2020) 25:3186–97. doi: 10.1038/s41380-020-00865-6
13. Shim E-J, Lee JW, Cho J, Jung HK, Kim NH, Lee JE, et al. Association of depression and anxiety disorder with the risk of mortality in breast cancer: a National Health Insurance Service study in Korea. Breast Cancer Res Treat (2020) 179:491–8. doi: 10.1007/s10549-019-05479-3
14. Mejareh ZN, Abdollahi B, Hoseinipalangi Z, Jeze MS, Hosseinifard H, Rafiei S, et al. Global, regional, and national prevalence of depression among cancer patients: A systematic review and meta-analysis. Indian J Psychiatry (2021) 63:527. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_77_21
15. Degefa M, Dubale B, Bayouh F, Ayele B, Zewde Y. Validation of the PHQ-9 depression scale in Ethiopian cancer patients attending the oncology clinic at Tikur Anbessa specialized hospital. BMC Psychiatry (2020) 20:446. doi: 10.1186/s12888-020-02850-3
16. Baraki AG, Tessema GM, Demeke EA. High burden of depression among cancer patients on chemotherapy in University of Gondar comprehensive hospital and Felege Hiwot referral hospital, Northwest Ethiopia. PloS One (2020) 15:e0237837. doi: 10.1371/journal.pone.0237837
17. Hagezom HM, Amare T, Hibdye G, Demeke W. Magnitude and associated factors of suicidal ideation among cancer patients at ayder comprehensive specialized hospital, Mekelle, Ethiopia, 2019: Cross-sectional study. Cancer Manage Res (2021) 13:4341–50. doi: 10.2147/CMAR.S268669
18. Atinafu BT, Demlew TM, Tarekegn FN. Magnitude of Anxiety and Depression and Associated Factors among Palliative Care Patients with Cancer at Tikur Anbessa Specialized Hospital, Ethiopia. Ethiopian J Health Sci (2022) 32:331–42.
19. Breidenbach C, Heidkamp P, Hiltrop K, Pfaff H, Enders A, Ernstmann N, et al. Prevalence and determinants of anxiety and depression in long-term breast cancer survivors. BMC Psychiatry (2022) 22:101. doi: 10.1186/s12888-022-03735-3
20. Endeshaw D, Walle TA, Yohannes S. Depression, anxiety and their associated factors among patients with cancer receiving treatment at oncology units in Amhara Region, Ethiopia: a cross-sectional study. BMJ Open (2022) 12:e063965. doi: 10.1136/bmjopen-2022-063965
21. Brandenbarg D, Maass SW, Geerse OP, Stegmann ME, Handberg C, Schroevers MJ, et al. A systematic review on the prevalence of symptoms of depression, anxiety and distress in long-term cancer survivors: Implications for primary care. Eur J Cancer Care (2019) 28:e13086. doi: 10.1111/ecc.13086
22. Abraham Y, Gebeyehu A, Fanta T, Ashegu T. Depression and anxiety prevalence and correlations among cancer patients at Tikur Anbesa Hospital in Addis Ababa, Ethiopia, 2018: Cross-sectional study. Front Psychiatry (2022) 13:939043. doi: 10.3389/fpsyt.2022.939043
23. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Internal Med (2009) 151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
24. JBI. The Joanna Briggs Institute critical appraisal tool for use in JBI systematic reviews checklist for prevalence studies. North Adelaide: The Joanna Briggs Institute (2017).
25. Munn Z, Tufanaru C, Aromataris E. JBI's systematic reviews: data extraction and synthesis. Am J Nurs (2014) 114:49–54. doi: 10.1097/01.NAJ.0000451683.66447.89
26. Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? psychol Methods (2006) 11:193–206. doi: 10.1037/1082-989X.11.2.193
27. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
28. Wurjine TH, Goyteom MH. Prevalence of cancer pain, anxiety and associated factors among patients admitted to oncology ward, Tikur Anbessa Specialized Hospital, Ethiopia, 2019. Open J Pain Med (2020) 4:009–17. doi: 10.17352/ojpm.000018
29. Alemayehu M, Deyessa N, Medihin G, Fekadu A. A descriptive analysis of depression and pain complaints among patients with cancer in a low income country. PloS One (2018) 13:e0193713. doi: 10.1371/journal.pone.0193713
30. Belete AM, Alemagegn A, Mulu AT, Yazie TS, Bewket B, Asefa A, et al. Prevalence of depression and associated factors among adult cancer patients receiving chemotherapy during the era of COVID-19 in Ethiopia. Hospital-based cross-sectional study. PloS One (2022) 17:e0270293. doi: 10.1371/journal.pone.0270293
31. Wondimagegnehu A, Abebe W, Abraha A, Teferra S. Depression and social support among breast cancer patients in Addis Ababa, Ethiopia. BMC Cancer (2019) 19:1–8. doi: 10.1186/s12885-019-6007-4
32. Abebe E, Giru BW, Boka A. Sleep quality and associated factors among adult cancer patients on treatments at tikur anbessa specialized hospital oncology unit, Addis Ababa, Ethiopia, 2021. Cancer control J Moffitt Cancer Center (2023) 30:10732748231160129. doi: 10.1177/10732748231160129
33. Belay W, Labisso WL, Tigeneh W, Kaba M, Haileselassie W. Magnitude and factors associated with anxiety and depression among patients with breast cancer in central Ethiopia: A cross-sectional study. Front Psychiatry (2022) 13:957592. doi: 10.3389/fpsyt.2022.957592
34. Berihun F, Haile S, Abawa M, Mulatie M, Shimeka A. Prevalence and correlates of anxiety and depression among cancer patients in the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. Arch Depress Anxiety (2017) 3:042–8. doi: 10.17352/ada
35. Endeshaw D, Biresaw H, Asefa T, Yesuf NN, Yohannes S. Sleep quality and associated factors among adult cancer patients under treatment at oncology units in Amhara Region, Ethiopia. Nat Sci sleep (2022) 14:1049–62. doi: 10.2147/NSS.S356597
36. Molla A, Aderaw M, Mulat H, Fanta B, Nenko G, Adane A. Suicidal ideation, attempt and associated factors among people living with cancer in Ethiopia: a cross-sectional study. Ann Gen Psychiatry (2022) 21:28. doi: 10.1186/s12991-022-00407-0
37. Nigussie K, Tesfaye D, Abdisa L, Tolosa L, Bete T, Gemechu K, et al. Suicidal ideation, attempt and associated factors among people with cancer attending cancer center, eastern Ethiopia. Front Psychiatry (2023) 14. doi: 10.3389/fpsyt.2023.1184921
38. Elkefi S, Trapani D, Ryan S. The role of digital health in supporting cancer patients' mental health and psychological well-being for a better quality of life: A systematic literature review. Int J Med Inf (2023) 176:105065. doi: 10.1016/j.ijmedinf.2023.105065
39. Walker ZJ, Xue S, Jones MP, Ravindran AV. Depression, anxiety, and other mental disorders in patients with cancer in low-and lower-middle–income countries: a systematic review and meta-analysis. JCO Global Oncol (2021) 7:1233–50. doi: 10.1200/GO.21.00056
40. Hashemi SM, Rafiemanesh H, Aghamohammadi T, Badakhsh M, Amirshahi M, Sari M, et al. Prevalence of anxiety among breast cancer patients: a systematic review and meta-analysis. Breast Cancer (Tokyo Japan) (2020) 27:166–78. doi: 10.1007/s12282-019-01031-9
41. Darvishi N, Ghasemi H, Rahbaralam Z, Shahrjerdi P, Akbari H, Mohammadi M. The prevalence of depression and anxiety in patients with cancer in Iran: a systematic review and meta-analysis. Supportive Care Cancer Off J Multinational Assoc Supportive Care Cancer (2022) 30:10273–84. doi: 10.1007/s00520-022-07371-1
42. Tao F, Xu M, Zou Q, Tang L, Feng J, Li Z. Prevalence and severity of anxiety and depression in Chinese patients with breast cancer: a systematic review and meta-analysis. Front Psychiatry (2023) 14:1080413. doi: 10.3389/fpsyt.2023.1080413
43. Watts S, Leydon G, Birch B, Prescott P, Lai L, Eardley S, et al. Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open (2014) 4:e003901. doi: 10.1136/bmjopen-2013-003901
44. Yutrirak K, Ratta-apha W, Dankulchai P, Pukrittayakamee P. Psychometric properties of the PHQ-9, HADS, and CES-D questionnaires and the prevalence of depression in patients with cancer receiving radiotherapy. Siriraj Med J (2021) 73:793–800. doi: 10.33192/Smj.2021.103
45. Shankar A, Dracham C, Ghoshal S, Grover S. Prevalence of depression and anxiety disorder in cancer patients: An institutional experience. Indian J Cancer (2016) 53:432–4. doi: 10.4103/0019-509X.200651
46. Popoola AO, Adewuya AO. Prevalence and correlates of depressive disorders in outpatients with breast cancer in Lagos, Nigeria. Psycho-Oncology (2012) 21:675–9. doi: 10.1002/pon.1968
47. Wæhrens EE, Brandt ÅChecktae, Peoples H, la Cour K. Everyday activities when living at home with advanced cancer: A cross-sectional study. Eur J Cancer Care (2020) 29:e13258. doi: 10.1111/ecc.13258
48. O'Leary K, Bylsma LM, Rottenberg J. Why might poor sleep quality lead to depression? A role for emotion regulation. Cogn Emotion (2017) 31:1698–706. doi: 10.1080/02699931.2016.1247035
49. Pandi-Perumal SR, Monti JM, Burman D, Karthikeyan R, BaHammam AS, Spence DW, et al. Clarifying the role of sleep in depression: A narrative review. Psychiatry Res (2020) 291:113239. doi: 10.1016/j.psychres.2020.113239
50. Radhakrishnan R, Selvaraj H, Chidambaram K, Arshav K, James A, Thangavel S. Prevalence of depression and anxiety disorders among cancer patients: An insight from a single institute. Cureus (2023) 15. doi: 10.7759/cureus.42831
51. Chittem M, Norman P, Harris PR. Relationships between perceived diagnostic disclosure, patient characteristics, psychological distress and illness perceptions in Indian cancer patients. Psycho-oncology (2013) 22:1375–80. doi: 10.1002/pon.3149
52. Amiri S. Unemployment associated with major depression disorder and depressive symptoms: a systematic review and meta-analysis. Int J Occup Saf ergonomics (2022) 28:2080–92. doi: 10.1080/10803548.2021.1954793
53. Arcaya M, Glymour MM, Christakis NA, Kawachi I, Subramanian S. Individual and spousal unemployment as predictors of smoking and drinking behavior. Soc Sci Med (2014) 110:89–95. doi: 10.1016/j.socscimed.2014.03.034
54. Naseri N, Taleghani F. Social support and depression in Iranian cancer patients: The role of demographic variables. J caring Sci (2018) 7:143–7. doi: 10.15171/jcs.2018.023
55. Kadambi S, Soto-Perez-de-Celis E, Garg T, Loh KP, Krok-Schoen JL, Battisti NML, et al. Social support for older adults with cancer: Young International Society of Geriatric Oncology review paper. J geriatric Oncol (2020) 11:217–24. doi: 10.1016/j.jgo.2019.09.005
Keywords: anxiety, depression, prevalence, cancer patients, Ethiopia
Citation: Geremew H, Abdisa S, Mazengia EM, Tilahun WM, Haimanot AB, Tesfie TK, Mneneh AL, Mengie MG, Endalew B, Birhanu MY, Asmare L and Simegn MB (2024) Anxiety and depression among cancer patients in Ethiopia: a systematic review and meta-analysis. Front. Psychiatry 15:1341448. doi: 10.3389/fpsyt.2024.1341448
Received: 20 November 2023; Accepted: 05 February 2024;
Published: 22 February 2024.
Edited by:
Pedro Morgado, University of Minho, PortugalReviewed by:
Valeria Sebri, European Institute of Oncology (IEO), ItalySemra Bulbuloglu, Istanbul Aydın University, Türkiye
Copyright © 2024 Geremew, Abdisa, Mazengia, Tilahun, Haimanot, Tesfie, Mneneh, Mengie, Endalew, Birhanu, Asmare and Simegn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Habtamu Geremew, habteg29@gmail.com
 Habtamu Geremew
Habtamu Geremew Samuel Abdisa2
Samuel Abdisa2 Elyas Melaku Mazengia
Elyas Melaku Mazengia Werkneh Melkie Tilahun
Werkneh Melkie Tilahun Tigabu Kidie Tesfie
Tigabu Kidie Tesfie Bekalu Endalew
Bekalu Endalew