- Beijing HuiLongGuan Hospital, Peking University, Beijing, China
Background: The prevalence of adolescent depression in China during the COVID-19 pandemic is increasing. Self-disclosing depressive emotions could help release stress. Self-disclosure, which is a prerequisite for self-efficacy, can directly contribute to people’s psychological health, and depression and the choice of coping strategy are determined by the level of self-efficacy perceived.
Purpose: We aimed to discuss the relationship between self-efficacy, self-disclosure, and medical coping strategy. Further, we explore the mediation effect of self-efficacy on the influence of self-disclosure on medical coping strategies in adolescents with depression.
Methods: A total of 585 patients aged 11–24 years with moderate and major depression were recruited. All the assessments were completed on the second day after admission, including the General Self-Efficacy Scale (GSE), Distress Disclosure Index (DDI), and Medical Coping Modes Questionnaire (MCMQ). Pearson correlation was performed to explore the relationships of these variables. The bootstrap analysis was used to conduct to assess the mediation effects.
Results: Both direct and indirect effects of self-disclosure on medical coping strategy were found. As predicted, self-efficacy partially mediated the relationship between self-disclosure and medical coping strategy (b = 0.0385, 95% CI: 0.0244–0.0538 for Confrontation; b = –0.0466, 95%CI: –0.0651 to –0.0296 for Resignation), respectively. The effect size for Confrontation and Resignation was 0.2659 and 0.2485, respectively.
Conclusion: Self-efficacy played a partial mediating role in the effect of self-disclosure on medical coping strategies for adolescent depression during the COVID-19 pandemic, and the use of a positive self-disclosure mechanism may be anticipated to promote improved self-efficacy and the use of active coping strategies.
Introduction
Depression has been more prevalent among adolescents during the worldwide COVID-19 pandemic compared to before (1), when it was as high as 52.4% in China (2), 32% in Peru, and 9% in Vietnam (3), which will cause an increased risk of negative health outcomes (4). The previous study has found that self-disclosure can directly contribute to people’s psychological health (5), and disclosing depressive emotions could help reduce stress and depression (6).
The onset of depression is important in relationships with coping strategies (7). Coping strategy refers to intrapsychic activities, as well as to the communications and behaviors of patients, designed to the decrease of distress caused by illness. As techniques used by patients to deal with disease, coping strategies are generally categorized into two broad types: active strategies and evasive strategies. Active strategies aim at making an active stress response. Evasive strategies mean evading stressful situations (8), and usually entail maladaptive consequences among adolescents (9–11). Compared with healthy people, depressive patients more often utilize strategies based on avoidance and denial, and experience more difficulty in finding positive characteristics in stressful events (12). However, the influence and pathway of self-disclosure among depressive adolescents in terms of adopting coping strategies has been unclear.
The choice of one coping strategy over another is determined by the level of perceived self-efficacy (13). Self-efficacy is a belief in one’s own capacity to face challenges (14), which is a key factor for adolescents’ emotional wellbeing. Low subjective wellbeing may significantly predict increased depressive symptoms (15). Based on Bandura’s social cognitive theory (16), self-efficacy is the faith in one’s ability to perform the behaviors that are necessary to attain a desired goal. Self-efficacy beliefs guide action both directly and indirectly through self-expectations regarding the result of a certain behavior (14). High self-efficacy for dealing with stress can prevent or reduce stress along with its health influences (17). However, the previous study showed that authentic self-disclosure to at least one person is a prerequisite for self-efficacy of psychological adjustment (18). In this situation, the use of a positive self-disclosure behavior may promote improved self-efficacy, the use of active coping strategies, and reduce depression. However, the increase in depression during the COVID-19 pandemic means that many of them need to choose the proper coping strategy to solve their depressive disorders.
However, much of the existing literature focuses on the relationship among self-disclosure, self-efficacy, coping strategies, and depression. Therefore, the present study was designed to discuss the relationship between self-disclosure, self-efficacy, and medical coping strategies and to explore the mediation effect of self-efficacy on the influence of self-disclosure on medical coping strategies in adolescents with depression (Figure 1). The outcomes of the present study may ultimately help adolescents to deal with their situations more positively. Moreover, we provide foundational data for developing nursing interventions to improve depression in adolescents before antidepressant therapy.
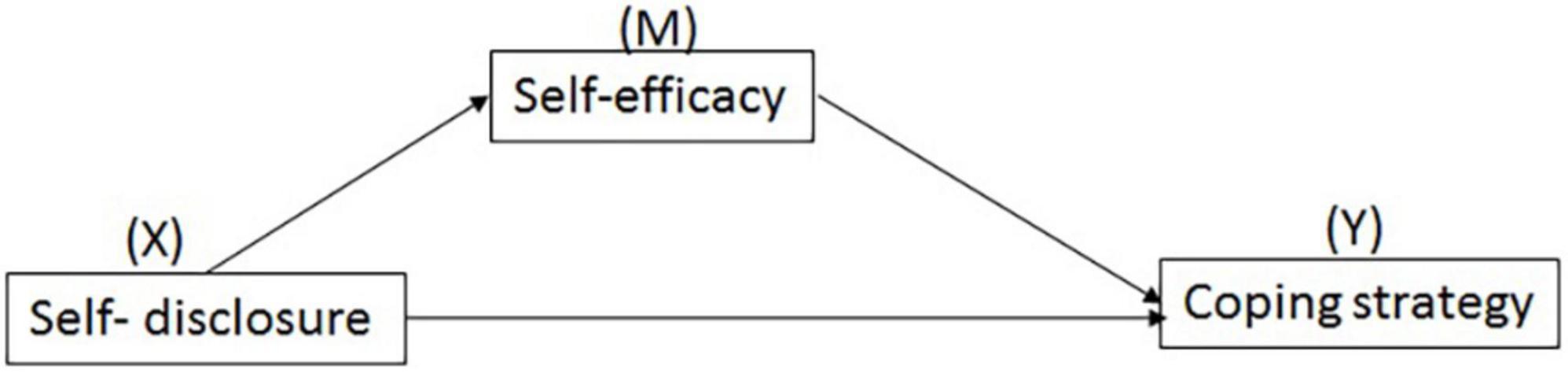
Figure 1. Path model for the mediation effect of self-efficacy on the influence of self-disclosure on medical coping strategy of adolescents with depression.
Materials and methods
Participants
Data of the present study were collected through a cross-sectional research in Beijing, China between June 2020 and July 2021 during the COVID-19 pandemic. Based on the literature recently published (19), the age range of description of adolescence was 10–24 years. A total of 585 patients aged 11–24 years old with moderate and major depression were recruited. All participants were students without married, and they lived with parents and schoolmates.
All participants met the eligibility criteria, i.e., meeting the diagnostic criteria for depression according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition. The exclusion criteria for the patients were rigorous, such as neurological disorders, head trauma, intellectual disability, bipolar disorder, and other psychiatric disorders.
Sociodemographic data, including age and years of education, were collected. Clinical data, including disease course, was obtained according to medical records, and self-report and confirmed by the next of kin and family members.
Approval for the present study was obtained from the Ethics Committee of Beijing HuiLongGuan Hospital which was in accordance with the principles in the Declaration of Helsinki. Written informed consent was obtained from all patients or their guardians before study enrollment.
Measures
In the present study, all the assessments were completed for all patients on the second day after admission, including the General Self-Efficacy Scale (GSE), Distress Disclosure Index (DDI), and Medical Coping Modes Questionnaire (MCMQ).
General self-efficacy scale
The GSE is a 10-item self-report scale which assesses general self-efficacy as a prospective and operative construct. Each item is scored from 1 (not at all true) to 4 (totally true). The total score ranges from 10 to 40, with higher scores showing higher self-efficacy (20). The GSE assesses optimistic self-belief in dealing with the demands, tasks, and challenges of life in general (21). Cronbach’s α coefficient was 0.84 (22).
Distress disclosure index
The DDI is a 12-item self-report assessment of one’s tendency to disclose personally distressing thought, a construct termed distress disclosure. DDI measures individual typical disclosure of distressing thoughts, personal difficulties, and distasteful emotions across time and circumstances. Participants assessed their agreement with each item from 1 (strongly disagree) to 5 (strongly agree). As a result, the DDI is useful to measure individual differences in emotional self-disclosure which is relevant to the counseling or seeking support process. Cronbach’s α coefficient was 0.93 (23).
Medical coping modes questionnaire
The Chinese version of the MCMQ which is aimed to measure three coping strategies that participants may utilize when facing life-threatening diseases, namely, Confrontation, Avoidance, and Resignation, contains 20 items (1 item was added to keep the original meaning of the scale when it was translated into Mandarin Chinese). For each item, individuals choose the response from the 4 choices that best reflects his or her experience (1 = none, 2 = a few, 3 = quite a few, 4 = a lot). Eight of the 20 items are reverse-scored. Subscale scores are attained by summing each item scores (range = 8–32 for Confrontation, 7–28 for Avoidance, 5–20 for Resignation). Higher scores show that an individual has more behaviors described by that specific coping scale when handle medical incidents. The MCMQ-C was used in the current study, and a good internal consistency was shown in the subscales, with Cronbach’s α coefficients as follows: Confrontation, 0.74; Avoidance, 0.73; and Resignation, 0.83 (24).
Statistical analyses
Descriptive statistics were used to calculate the frequency of characteristics of the samples. Continuous variables were described by mean and standard deviation (SD), and categorical variables by frequency and percentage (%). Correlation analysis was performed using partial correlation.
Mediation analysis was computed for self-disclosure as an independent variable, medical coping mode as a dependent variable (Y), and self-efficacy as a possible mediator (M). The PROCESS v3.5 for SPSS (25) was used with bootstrapping with coefficients estimated from 5,000 bootstraps. A simple mediational approach was conducted using Model 4 with 5,000 bootstraps with education and disease course as covariates. The output mediation models were explained as follows: b (YX) is the total effect of the independent variable X on the dependent variable Y; b (MX) is the effect of the independent variable on the assumed mediator M; b (YM.X) is the effect of the mediator on the dependent variable, excluding the independent variable; and b (YX.M) is the direct effect of the independent variable on the dependent variable except for the mediator. The indirect effect of X on Y through M was estimated. The ratio of the indirect effect to the total effect was treated as the effect size for mediation (26). The statistical analyses were conducted using IBM SPSS Statistics for Windows (version 23.0; IBM Corp., Armonk, NY). P-value < 0.05 was considered significant.
Results
Descriptive statistics
A total of 585 participants were included in the analysis, with an average of 17.04 ± 3.23 years old. As shown in Table 1, male participants were 135 (23.08%) and the rest of participants were female (n = 450, 76.92%). There were 346 participants of age ≤ 18 years (14.75 ± 1.55), while 239 participants were aged >18 years (20.36 ± 1.88). The average years of education is 11.04 ± 3.23. The average disease course is 2.18 ± 1.67 years. The distributions of DDI, GSES, Confrontation, Avoidance, and Resignation of MCMQ were 31.73 ± 9.64, 20.07 ± 6.44, 17.53 ± 4.07, 16.40 ± 3.10, 12.43 ± 3.98 (Table 1).
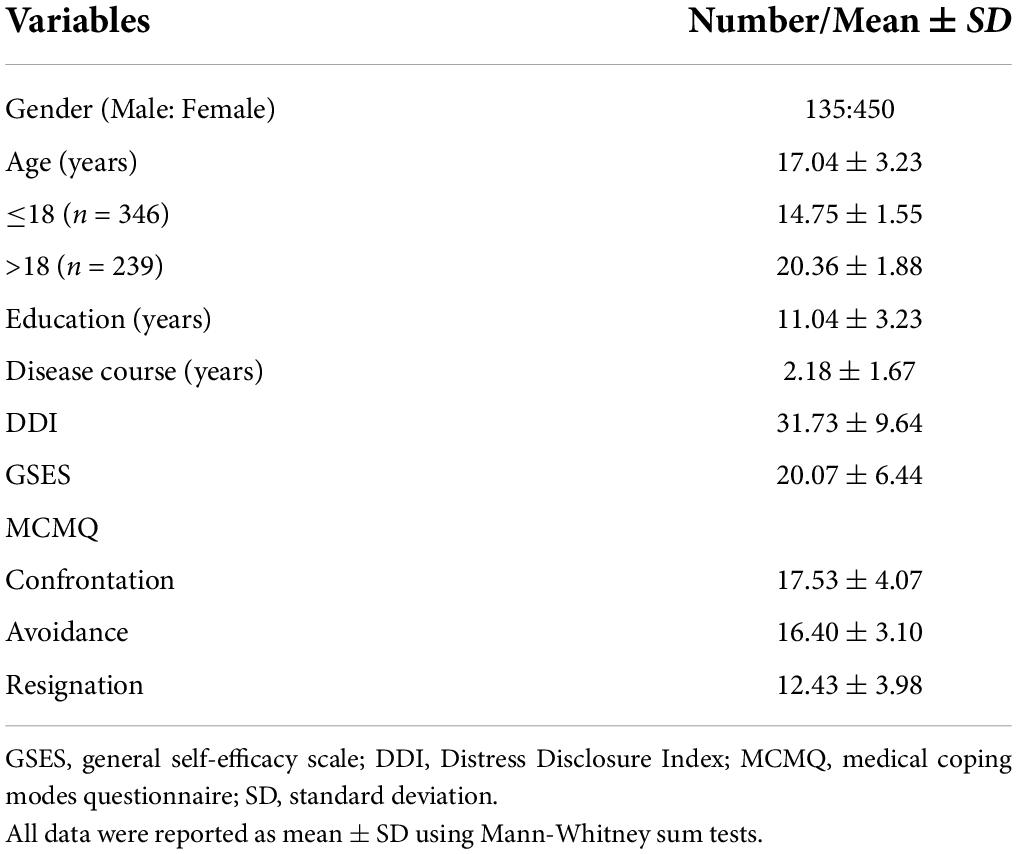
Table 1. The demographic and psychotypical characteristics of adolescents with depression on admission (n = 585).
Correlation analysis
Table 2 shows the correlation between the variables from the multivariate analysis with education and disease course as covariates. The scores of DDI and GSES were both correlated with the scores of confront and resignation coping strategies, respectively (r = 0.341/-0.441 and r = 0.347/-0.430, all p < 0.001). The scores of DDI were correlated with the scores of GSES (r = 0.349, p < 0.001). However, neither DDI nor GSES was correlated with avoidance coping strategy (both p > 0.05).
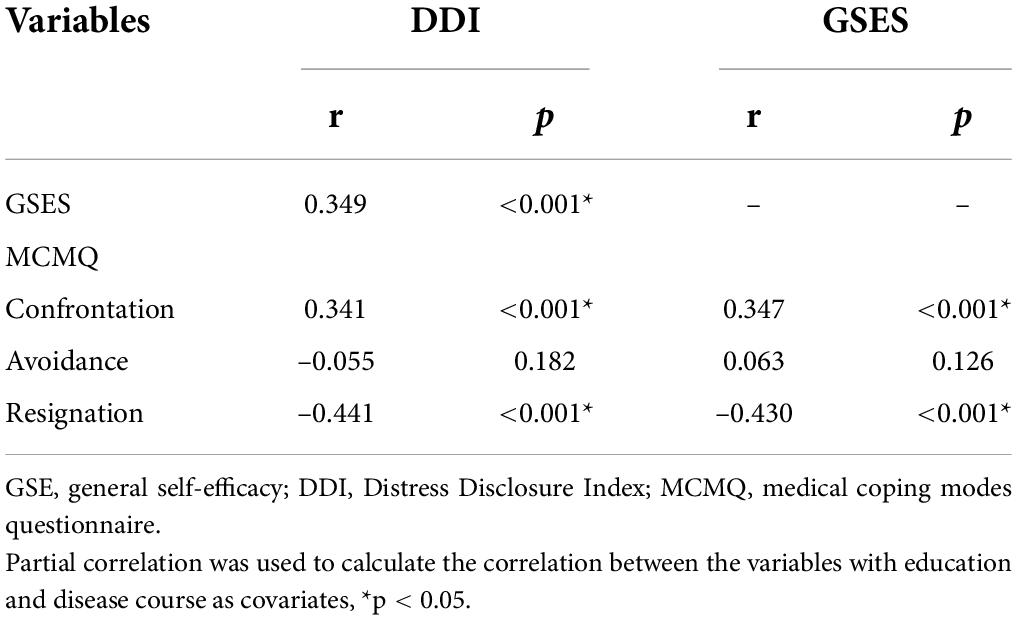
Table 2. Correlation among psychotypical characteristics of adolescents with depression before (n = 585).
Mediation analysis for self-efficacy
Confrontation and Resignation coping strategies were, respectively used as Y, and mediation analysis results showed that Model b (YX) (total effect, b = 0.1448, t = 8.7446, 95%CI: 0.1123–0.1774 for Confrontation and b = –0.1875, t = –11.8580, 95%CI: –0.2185 to –0.1565 for Resignation; both p < 0.001), Model b (MX) (X – > M, for both Confrontation and Resignation, b = 0.2370, t = 8.9899, 95%CI: 0.1852–0.2887 and both p < 0.001), Model b (YM.X) (M – > Y, b = 0.1448, t = 8.7446, 95%CI: 0.1123–0.1774 for Confrontation and b = –0.1875, t = –11.8580, 95%CI: –0.2185 to –0.1565 for Resignation; both p < 0.001), and Model b (YX.M) (X – > Y, b = 0.1063, t = 6.2206, 95%CI: 0.0727–0.1399 for Confrontation and b = –0.1409, t = –8.8305, 95%CI: –0.1726 to –0.1096; both p < 0.001 for Resignation). The coefficient of indirect of Confrontation and Resignation was 0.0385 and –0.0466 (X – > M – > Y, 95%CI: 0.0244–0.0538 for Confrontation and 95%CI: –0.0651 to –0.0296 for Resignation). The ratio of indirect effect/total effect for Confrontation and Resignation was 0.2659 and 0.2485, respectively. These outputs identified the partial mediation effect of self-efficacy (M) on Confrontation and Resignation (Y) (Figure 2). However, there was no mediation effect of self-efficacy (M) on Avoidance (p > 0.05).
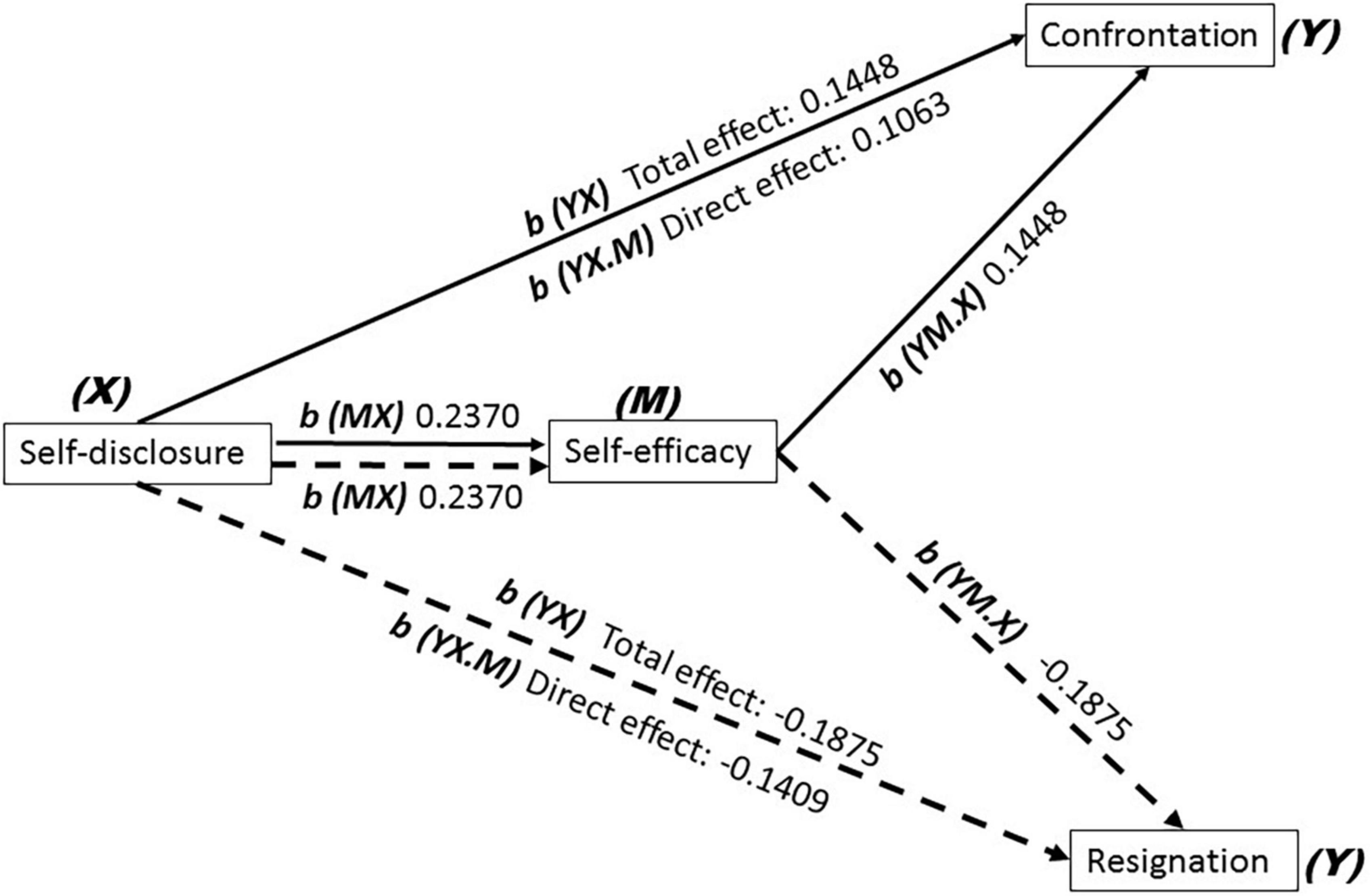
Figure 2. On admission, Confrontation and Resignation coping strategies of adolescents with depression were, respectively used as Y, and mediation analysis results showed that Model b (YX) (total effect, b = 0.1448 for Confrontation, and b = –0.1875 for Resignation; both p < 0.001), Model b (MX) (X – > M, for both Confrontation and Resignation, b = 0.2370, p < 0.001), Model b (YM.X) (M – > Y, b = 0.1448 for Confrontation, and b = –0.1875 for Resignation; both p < 0.001), Model b (YX.M) (X – > Y, b = 0.1063 for Confrontation and b = –0.1409 for Resignation; both p < 0.001). The coefficient of indirect of Confrontation and Resignation was 0.0385 and –0.0466 (X – > M – > Y, for Confrontation and for Resignation).
These results above partially support the hypothesis that self-efficacy which mediated medical coping strategies with self-disclosure remains a predictor.
Discussion
To the best of our knowledge, much of the existing literature focuses on the relationship among self-disclosure, self-efficacy, coping strategies, and depression, but there are few studies of the mediation of self-efficacy between self-disclosure and medical coping strategy in adolescents with depression. The present study is the first to examine the relationship between self-disclosure and medical coping strategy during the COVID-19 pandemic. Further, we explored the possible pathways underlying this association concerning depressive adolescents’ self-efficacy by constructing a mediation model, and offering a more comprehensive picture of self-disclosure-coping strategy pathways. Understanding the coping strategies of depressive adolescents during the COVID-19 pandemic and its underlying psychological mechanisms are crucial for the effective intervention of adolescents with depression before medication and are beneficial for establishing a team of high-quality nurses’ and consultants’ to fight future public health emergencies.
The primary finding in the present study revealed that self-disclosure has a direct effect on medical coping strategies, mainly the choice of Confrontation and Resignation. Adolescents would need direct contact with the outside world, and long-term staying at home would have a great influence on emotion. The prolonged home confinement decreased social interactions with peers for children and adolescents (27, 28). They are compelled to lock themselves down comprehensively, and find it harder to articulate their feelings during the COVID-19 pandemic, which has caused a persistent influence on the mental health of children and adolescents and ultimately contribute to the occurrence of depressive symptoms (29). It was found in a domestic study that the occurrence of emotional difficulties in children and adolescents is much higher than that before the pandemic (30).
Previous studies have shown that disclosing depressive emotions could help release depression (6). Self-disclosure refers to the course by which persons open themselves up to others (31), and has long been identified as a key coping behavior in therapeutic situation (32). Several studies have demonstrated self-disclosure as a prerequisite for healthy adjustment (33). An individual with positive self-disclosure can have effective communication with the outside world (30). On the other hand, non-disclosure is often used to refer to non-expression, inhibition, or topic avoidance. A growing body of research documents that non-disclosure is associated with poor psychological adjustment and increased distress (34). The social-cognitive processing model of adjustment to stressors illustrates the impact of non-disclosure on emotional distress (34), which may undermine an individual’s ability to confront others. A previous study has demonstrated the negative impact of non-disclosure of stress-related thoughts and feelings on depressive symptoms (35, 36). Disclosing stressful events and discussing related thoughts and feelings with others may present the opportunity to integrate the cognitive discrepancy by receiving new information and/or attaining appropriate support (37) which, in turn, may promote emotional adjustment.
Based on the definition of the coping strategies of stress and the coping theory, self-disclosure can be considered as a coping strategy when people disclose their problems and need to attain social support (38). Coping refers to how people try to deal with traumatic events or everyday stressful situations. It plays a crucial role in adolescence, which is a period during which individuals manage new challenges that can stand for Mayordomo-Rodríguez et al. (39). The previous study has reported that positive coping strategies were connected to a greater feeling of control over occurrences and the search for useful information to cope with difficulties (40). According to the stress-buffering model (41), a positive coping style offers buffering effects in the path of disease and psychological distress (42). Some researchers have confirmed that adopting a positive and effective coping strategy can reduce the psychological pressure on them (43), thus improving depression.
Generally, Confrontation is a positive coping strategy, while Avoidance and Resignation are negative coping strategies (44). The use of active coping is supportive of mental health (45), which helps prevent depression (46). Avoidance coping strategy is oriented toward denying, minimizing, or else avoiding dealing directly with stressful requests and is closely linked to distress, and the use of Avoidance-coping strategy has been related to relapse among patients treated for depression (47). However, the course of depression among the participants was 2.18 ± 1.67 years, and there were fewer patients with recurrent depression. Therefore, the effect of self-disclosure on Avoidance was not found in the present study. The literature suggests that Resignation is related to depression (48, 49). Resignation as a negative orientation has a negative influence on stress and has been associated with an increase in depressive symptoms and poorer wellbeing, and reflects factors related to hopelessness and giving up (49). Consequently, self-disclosure was positively and negatively correlated with Confrontation and Resignation, respectively, in our study, which will help us understand the direct effect of self-disclosure on medical coping strategy.
The secondary findings demonstrated that self-efficacy partially mediated the relationship between self-disclosure and medical coping strategies. The previous study showed that the prerequisite for self-efficacy is authentic self-disclosure (18). A high self-disclosure may mean a high level of self-efficacy (50, 51). Self-efficacy refers to a person’s faith about their ability to mobilize courses of action needed to achieve desired personal goals (52). Further, it is considered an influential motivational, cognitive, and affective determinant of student action, with a significant impact on their involvement, effort, persistence, self-regulation, and achievement (8). These features make self-efficacy a vital variable in controlling stress (8), and it is a protective factor against the influence of day-to-day stressors at school (53, 54). Moreover, a high level of self-efficacy is conducive for patients to take a positive coping strategy (55). Confrontation has been shown to be supportive of mental health (45) to protect against depression (46), and Resignation has been associated with an increase in depressive symptoms (49), respectively. In the present study, we also found that GSES was positively and negatively correlated with Confrontation and Resignation, respectively. All the literature above can explain fully the partial mediation of self-efficacy between self-disclosure and medical coping strategy.
Other findings of our current study included that the effect size for Confrontation and Resignation was 0.2659 and 0.2485, respectively. The previous study has reported that females had more frequent use of support-seeking and active coping strategies than males (56). However, the number of females in our study was more than that of males, therefore, it was reasonable that the effect size for Confrontation was higher than that for Resignation in our study.
There are some limitations to the present study. First, although the number of the recurrent and the first-episode depression, and the assessment of depressive symptoms were not provided, all participants who were diagnosed with moderate and major depression needed antidepressant medication, which means that their psychological state was assessed without knowing depressive symptoms to decrease the dependence on symptom scores and treatment or not, and there is no need to excessively increase the workload of nurses. Secondly, the effect of age range and gender differences on the pathway of the mediation was not discussed here, because what the whole children and adolescents were analyzed together will help us to take measurements of the effective intervention of the population. Thirdly, although the mediating effect size was very small in the present study, the previous study has reported that the ratio of the indirect effect to the total effect has been a popular measure in mediation analysis (57), and the ratio of indirect effect/total effect for Confrontation and Resignation was 0.2659 and 0.2485, respectively. Therefore, the mediation effect had been still reported. Finally, although our cross-sectional study did not determine the causality, and a longitudinal study design is better suited for confirming the relationship, the present study did provide evidence for medical coping strategies chosen in adolescents with depression.
Conclusion
In the present study, self-efficacy indeed played a partial mediating role in the effect of self-disclosure on medical coping strategies for adolescent depression during the COVID-19 pandemic. The use of a positive self-disclosure mechanisms may be necessary to promote improved self-efficacy and the use of active coping strategies.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by the Institutional Review Board of the Beijing HuiLongGuan Hospital. Written informed consent to participate in this study was provided by the participants or their legal guardian/next of kin.
Author contributions
YaW designed the study, led the statistical analyses, and drafted the manuscript. JS provided clinical coordination. DZ and YoW finished the assessments. SW collected the clinical data. YQ and JG provided the input data. YaW and ZW secured funding for the present study. All authors approved the final manuscript for submission.
Funding
This work was supported by the “Qingmiao” program of Beijing Municipal Hospital Management Center (QML20212003), the Youth Scientific Research Foundation of Beijing HuiLongGuan Hospital (LY202106), Capital’s Funds for Health Improvement and Research (2022-2-2133), and Beijing Municipal Science and Technology Project (Z17110000107022).
Conflict of interest
The handling editor declared a shared affiliation, though no other collaboration, with several of the authors, YaW, JS, DZ, YoW, SW, ZW, YQ, and JG at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rothe J, Buse J, Uhlmann A, Bluschke A, Roessner V. Changes in emotions and worries during the Covid-19 pandemic: an online-survey with children and adults with and without mental health conditions. Child Adolesc Psychiatry Ment Health. (2021) 15:11.
2. Zhang Z, Zhai A, Yang M, Zhang J, Zhou H, Yang C, et al. Prevalence of depression and anxiety symptoms of high school students in shandong province during the COVID-19 epidemic. Front Psychiatry. (2020) 11:570096. doi: 10.3389/fpsyt.2020.570096
3. Porter C, Favara M, Hittmeyer A, Scott D, Sanchez Jimenez A, Ellanki R, et al. Impact of the COVID-19 pandemic on anxiety and depression symptoms of young people in the global south: evidence from a four-country cohort study. BMJ Open. (2021) 11:e049653. doi: 10.1136/bmjopen-2021-049653
4. Mullen S. Major depressive disorder in children and adolescents. Ment Health Clin. (2018) 8:275–83.
5. Trepte S, Masur PK, Scharkow M. Mutual friends’ social support and self-disclosure in face-to-face and instant messenger communication. J Soc Psychol. (2018) 158:430–45. doi: 10.1080/00224545.2017.1398707
6. Zou ML, Li MX, Cho V. Depression and disclosure behavior via social media: a study of university students in China. Heliyon. (2020) 6:e03368. doi: 10.1016/j.heliyon.2020.e03368
7. Sariusz-Skapska M, Czabala JC, Dudek D, Zieba A. [Assessment of stressful life events and sense of coherence in patients with unipolar and bipolar disorder]. Psychiatr Pol. (2003) 37:863–75.
8. Freire C, Ferradas MDM, Regueiro B, Rodriguez S, Valle A, Nunez JC. Coping strategies and self-efficacy in university students: a person-centered approach. Front Psychol. (2020) 11:841. doi: 10.3389/fpsyg.2020.00841
9. Tavolacci MP, Ladner J, Grigioni S, Richard L, Villet H, Dechelotte P. Prevalence and association of perceived stress, substance use and behavioral addictions: a cross-sectional study among university students in France, 2009-2011. BMC Public Health. (2013) 13:724. doi: 10.1186/1471-2458-13-724
10. Deasy C, Coughlan B, Pironom J, Jourdan D, Mannix-McNamara P. Psychological distress and coping amongst higher education students: a mixed method enquiry. PLoS One. (2014) 9:e115193. doi: 10.1371/journal.pone.0115193
11. Skinner EA, Pitzer JR, Steele JS. Can student engagement serve as a motivational resource for academic coping, persistence, and learning during late elementary and early middle school? Dev Psychol. (2016) 52:2099–117. doi: 10.1037/dev0000232
12. Orzechowska A, Zajaczkowska M, Talarowska M, Galecki P. Depression and ways of coping with stress: a preliminary study. Med Sci Monit. (2013) 19:1050–6. doi: 10.12659/MSM.889778
13. Vandercleyen F, Boudreau P, Carlier G, Delens C. Pre-service teachers in PE involved in an organizational critical incident: emotions, appraisal and coping strategies. Phys Educ Sport Pedagogy. (2014) 19:164–78.
14. Tak YR, Brunwasser SM, Lichtwarck-Aschoff A, Engels RC. The prospective associations between self-efficacy and depressive symptoms from early to middle adolescence: a cross-lagged model. J Youth Adolesc. (2017) 46:744–56. doi: 10.1007/s10964-016-0614-z
15. Grant F, Guille C, Sen S. Well-being and the risk of depression under stress. PLoS One. (2013) 8:e67395. doi: 10.1371/journal.pone.0067395
16. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. (1977) 84:191–215. doi: 10.1037//0033-295x.84.2.191
17. Tran T, La N, Nguyen H, Shochet I, Nguyen N, Wurfl A, et al. Validation of the coping self-efficacy scale: vietnamese version for adolescents. BMC Psychol. (2022) 10:59. doi: 10.1186/s40359-022-00770-3
18. Kreiner H, Levi-Belz Y. Self-disclosure here and now: combining retrospective perceived assessment with dynamic behavioral measures. Front Psychol. (2019) 10:558. doi: 10.3389/fpsyg.2019.00558
19. Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolescent Health. (2018) 2:223–8.
20. De Las Cuevas C, Penate W. Validation of the general self-efficacy scale in psychiatric outpatient care. Psicothema. (2015) 27:410–5.
21. Brunes A, Hansen MB, Heir T. General self-efficacy in individuals with visual impairment compared with the general population. PLoS One. (2021) 16:e0254043. doi: 10.1371/journal.pone.0254043
22. Dougherty CM, Johnston SK, Thompson EA. Reliability and validity of the self-efficacy expectations and outcome expectations after implantable cardioverter defibrillator implantation scales. Appl Nurs Res. (2007) 20:116–24.
23. Kahn JH, Hucke BE, Bradley AM, Glinski AJ, Malak BL. The distress disclosure index: a research review and multitrait-multimethod examination. J Couns Psychol. (2012) 59:134–49. doi: 10.1037/a0025716
24. Li L, Li S, Wang Y, Yi J, Yang Y, He J, et al. Coping profiles differentiate psychological adjustment in Chinese women newly diagnosed with breast cancer. Integr Cancer Ther. (2017) 16:196–204. doi: 10.1177/1534735416646854
25. Grasaas E, Helseth S, Fegran L, Stinson J, Smastuen M, Haraldstad K. Health-related quality of life in adolescents with persistent pain and the mediating role of self-efficacy: a cross-sectional study. Health Qual Life Outcomes. (2020) 18:19.
26. Walters GD. PM effect size estimation for mediation analysis: a cautionary note, alternate strategy, and real data illustration. Int J Soc Res Methodol. (2018) 21:25–33.
27. Tang S, Xiang M, Cheung T, Xiang YT. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J Affect Disord. (2021) 279:353–60. doi: 10.1016/j.jad.2020.10.016
28. Short MA, Louca M. Sleep deprivation leads to mood deficits in healthy adolescents. Sleep Med. (2015) 16:987–93. doi: 10.1016/j.sleep.2015.03.007
29. Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. (2020) 59:1218–1239.e3.
30. Chen L, Cheng R, Hu B. The effect of self-disclosure on loneliness in adolescents during COVID-19: the mediating role of peer relationships. Front Psychiatry. (2021) 12:710515. doi: 10.3389/fpsyt.2021.710515
31. Levi-Belz Y, Lev-Ari L. “Let’s talk about it”: the moderating role of self-disclosure on complicated grief over time among suicide survivors. Int J Environ Res Public Health. (2019) 16:3740. doi: 10.3390/ijerph16193740
32. Matthes J, Koban K, Neureiter A, Stevic A. Longitudinal relationships among fear of COVID-19, smartphone online self-disclosure, happiness, and psychological well-being: survey study. J Med Internet Res. (2021) 23:e28700. doi: 10.2196/28700
33. Levi-Belz Y, Gvion Y, Horesh N, Fischel T, Treves I, Or E, et al. Mental pain, communication difficulties, and medically serious suicide attempts: a case-control study. Arch Suicide Res. (2014) 18:74–87. doi: 10.1080/13811118.2013.809041
34. Lee M, Song Y, Zhu L, Ma GX. Coping strategies and benefit-finding in the relationship between non-disclosure and depressive symptoms among breast cancer survivors in China. Am J Health Behav. (2017) 41:368–77. doi: 10.5993/AJHB.41.4.1
35. Figueiredo MI, Fries E, Ingram KM. The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psychooncology. (2004) 13:96–105. doi: 10.1002/pon.717
36. Pennebaker JW, Kiecolt-Glaser JK, Glaser R. Disclosure of traumas and immune function: health implications for psychotherapy. J Consult Clin Psychol. (1988) 56:239–45. doi: 10.1037//0022-006x.56.2.239
37. Munro H, Scott SE, King A, Grunfeld EA. Patterns and predictors of disclosure of a diagnosis of cancer. Psychooncology. (2015) 24:508–14.
38. Lei X, Wu H, Ye Q. Pregnant women’s coping strategies, participation roles and social support in the online community during the COVID-19. Inf Process Manag. (2022) 59:102932. doi: 10.1016/j.ipm.2022.102932
39. Mayordomo-Rodríguez T, Meléndez-Moral JC, Viguer-Segui P, Sales-Galán A. Coping strategies as predictors of well-being in youth adult. Soc Indic Res. (2015) 122:479–89.
40. Cattelino E, Testa S, Calandri E, Fedi A, Gattino S, Graziano F, et al. Self-efficacy, subjective well-being and positive coping in adolescents with regard to Covid-19 lockdown. Curr Psychol. (2021). 20:1–12. doi: 10.1007/s12144-021-01965-4
41. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98:310–57.
43. Lan CF, Nie CL, Lin YJ. Uncertainty in illness and the coping styles of severe patients with COVID-19: current status and correlation. Epidemiol Infect. (2021) 149:1–22. doi: 10.1017/S0950268821001448
44. Feifel H, Strack S, Nagy VT. Coping strategies and associated features of medically ill patients. Psychosom Med. (1987) 49:616–25.
45. Seguin M, Roberts B. Coping strategies among conflict-affected adults in low- and middle-income countries: a systematic literature review. Glob Public Health. (2017) 12:811–29.
46. Saxon L, Makhashvili N, Chikovani I, Seguin M, McKee M, Patel V, et al. Coping strategies and mental health outcomes of conflict-affected persons in the republic of Georgia. Epidemiol Psychiatr Sci. (2017) 26:276–86. doi: 10.1017/S2045796016000019
47. Holahan CJ, Moos RH, Holahan CK, Brennan PL, Schutte KK. Stress generation, avoidance coping, and depressive symptoms: a 10-year model. J Consult Clin Psychol. (2005) 73:658–66. doi: 10.1037/0022-006X.73.4.658
48. Wrosch C, Scheier MF, Miller GE, Schulz R, Carver CS. Adaptive self-regulation of unattainable goals: goal disengagement, goal reengagement, and subjective well-being. Pers Soc Psychol Bull. (2003) 29:1494–508. doi: 10.1177/0146167203256921
49. Wrosch C, Miller GE, Scheier MF, de Pontet SB. Giving up on unattainable goals: benefits for health? Pers Soc Psychol Bull. (2007) 33:251–65. doi: 10.1177/0146167206294905
50. McCarthy MH, Wood JV, Holmes JG. Dispositional pathways to trust: self-esteem and agreeableness interact to predict trust and negative emotional disclosure. J Pers Soc Psychol. (2017) 113:95–116. doi: 10.1037/pspi0000093
51. Molero MDM, Perez-Fuentes MDC, Gazquez JJ. Analysis of the mediating role of self-efficacy and self-esteem on the effect of workload on burnout’s influence on nurses’ plans to work longer. Front Psychol. (2018) 9:2605. doi: 10.3389/fpsyg.2018.02605
52. Wood R, Bandura A. Impact of conceptions of ability on self-regulatory mechanisms and complex decision making. J Pers Soc Psychol. (1989) 56:407–15. doi: 10.1037//0022-3514.56.3.407
53. Freire C, Ferradas MDM, Nunez JC, Valle A, Vallejo G. Eudaimonic well-being and coping with stress in university students: the mediating/moderating role of self-efficacy. Int J Environ Res Public Health. (2018) 16:48. doi: 10.3390/ijerph16010048
54. Schonfeld P, Brailovskaia J, Zhang XC, Margraf J. Self-efficacy as a mechanism linking daily stress to mental health in students: a three-wave cross-lagged study. Psychol Rep. (2019) 122:2074–95. doi: 10.1177/0033294118787496
55. Liu Q, Mo L, Huang X, Yu L, Liu Y. Path analysis of the effects of social support, self-efficacy, and coping style on psychological stress in children with malignant tumor during treatment. Medicine (Baltimore). (2020) 99:e22888. doi: 10.1097/MD.0000000000022888
56. Chandra A, Batada A. Exploring stress and coping among urban African American adolescents: the shifting the lens study. Prev Chronic Dis. (2006) 3:A40.
Keywords: adolescent depression, self-disclosure, self-efficacy, medical coping mode, mediation
Citation: Wu Y, Shao J, Zhang D, Wang Y, Wang S, Wang Z, Qu Y and Gu J (2022) Pathways from self-disclosure to medical coping strategy among adolescents with moderate and major depression during the COVID-19 pandemic: A mediation of self-efficacy. Front. Psychiatry 13:976386. doi: 10.3389/fpsyt.2022.976386
Received: 23 June 2022; Accepted: 15 August 2022;
Published: 02 September 2022.
Edited by:
Kai Yuan, Peking University Sixth Hospital, ChinaReviewed by:
Bikila Balis, Haramaya University, EthiopiaJianfei Xie, Central South University, China
Copyright © 2022 Wu, Shao, Zhang, Wang, Wang, Wang, Qu and Gu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Wu, wyan223@126.com; Zhiren Wang, Zhiren75@163.com
 Yan Wu
Yan Wu Jing Shao
Jing Shao Zhiren Wang
Zhiren Wang