- Department of Clinical Pharmacy and Pharmacy Administration, School of Pharmacy, Fudan University, Shanghai, China
Objectives: To assess the contemporary prevalence and decadal trends of depression and antidepressant use among adults with cardiovascular disease (CVD) in the United States, as well as their risk factors from 2009 to 2020.
Materials and methods: We used the National Health and Nutrition Examination Survey data to calculate the weighted prevalence of depression and antidepressant use. Adults aged 20 years or older with CVD were included. Depression and CVD were assessed by the Patient Health Questionnaire (PHQ-9) and self-report, respectively.
Results: A total of 3,073 eligible participants with CVD aged >20 years were included. The overall prevalence of depression defined by PHQ-9 score ≥10 was 15.7% (95% CI 13.8–17.5), with a steady trend during 2009–March 2020 (p = 0.777). Female gender (aOR 1.78, 95% CI 1.20–2.64) and sleep disorder (aOR 2.62, 95% CI 1.78–3.86) were independent risk factors for depression in CVD patients, while high education level, high income, longer sleep duration, and non-current smokers were considered protective factors. The weighted prevalence of antidepressant use among depressed patients with CVD was 38.6%, which also remained unchanged during the survey period (p = 0.699). Participants with normal sleep pattern and duration were significantly less likely to take antidepressants (p = 0.003).
Conclusion: The longitudinal trends in the prevalence of depression among CVD patients in the United States have been stable over the past decade, despite being significantly higher in women, and those with sleep disorders. Overall, antidepressant use was fairly low. Aggressive screening and tailored treatment are recommended for specific vulnerable subpopulations to improve their clinical outcomes.
Introduction
Depression, also known as major depressive disorder (MDD), is one of the most common mental disorders, associated with a decline in health-related quality of life and one of the leading causes of disability (1, 2). In 2008, depression was ranked as the third leading cause of global disease burden by the World Health Organization, and is expected to rise to second place by 2030 (3). An estimated 5.0% of adults worldwide, or 280 million people, suffer from depression (4). In the United States, the prevalence of depression has risen significantly from 6.62% in 2005 to 7.28% in 2015 (2), and appears to be continuing to increase. The increase in depression has been more pronounced in recent years, from 8.7% in 2017–2018 to more than 10% in 2020 during the COVID-19 pandemic (5).
Depression is often comorbid with chronic diseases such as diabetes, hypertension, and coronary heart disease, which may further worsen health outcomes when they interact synergistically (1, 6–10). Studies have shown that 50% of people with chronic diseases suffer from depression (10). Depression can cause severe damage to personal wellbeing, occupational performance, family and social roles (11, 12). Worst of all, it can lead to suicidal behavior (13, 14). Despite the potential negative impact on individuals and society, a significant proportion of people with depression remains undertreated, especially in developing countries (4, 15–17). As the prevalence of chronic diseases rises, so does the need for effective depression management.
Previous studies have clearly suggested that patients with cardiovascular disease (CVD) experience increased risk for depression compared to the general population (15–20 vs. 5%), which makes them more vulnerable to physical limitations, low quality of life, recurrence, high mortality and high healthcare costs (18, 19). There are multiple pathophysiological mechanisms that explain the association between depression and CVD that does not occur by chance, such as increased levels of inflammatory markers, impaired heart rate variability, and hypothalamic-pituitary-adrenal (HPA) axis dysfunction (10, 20). On the other hand, depression can also affect the prognosis of existing CVD and increase its burden (21–23). CVD accompanied by depression may result in more serious health hazards than either disease alone (10, 22). As two leading causes of morbidity and mortality, a better understanding of depression prevalence and improved management in CVD patients is highly valuable from both personal and public health perspectives.
Currently, there is little evidence regarding the prevalence and treatment rates of depression in CVD patients. Although several epidemiological studies have reported relevant data, the prevalence varied widely from 11 to 65% depending on screening tools, survey samples, and disease diversity (18, 24–26). In addition, conclusions about whether characteristics such as gender and race influence the development of depression were very conflicting. Strategies such as cardiac rehabilitation, exercise, general support, cognitive behavioral therapy, and antidepressants have all been shown to be effective in depressed patients with CVD (27). Despite this, depression remains undertreated and details of antidepressant treatment were rarely reported. Therefore, this article aims to estimate the national prevalence of depression in the United States over the past decade, to investigate the relationship between CVD and depression and risk factors for depression in patients with different characteristics, and to clarify the usage patterns of antidepressants, using longitudinal data from the National Health and Nutrition Examination Survey (NHANES).
Methods and materials
Data sources and study populations
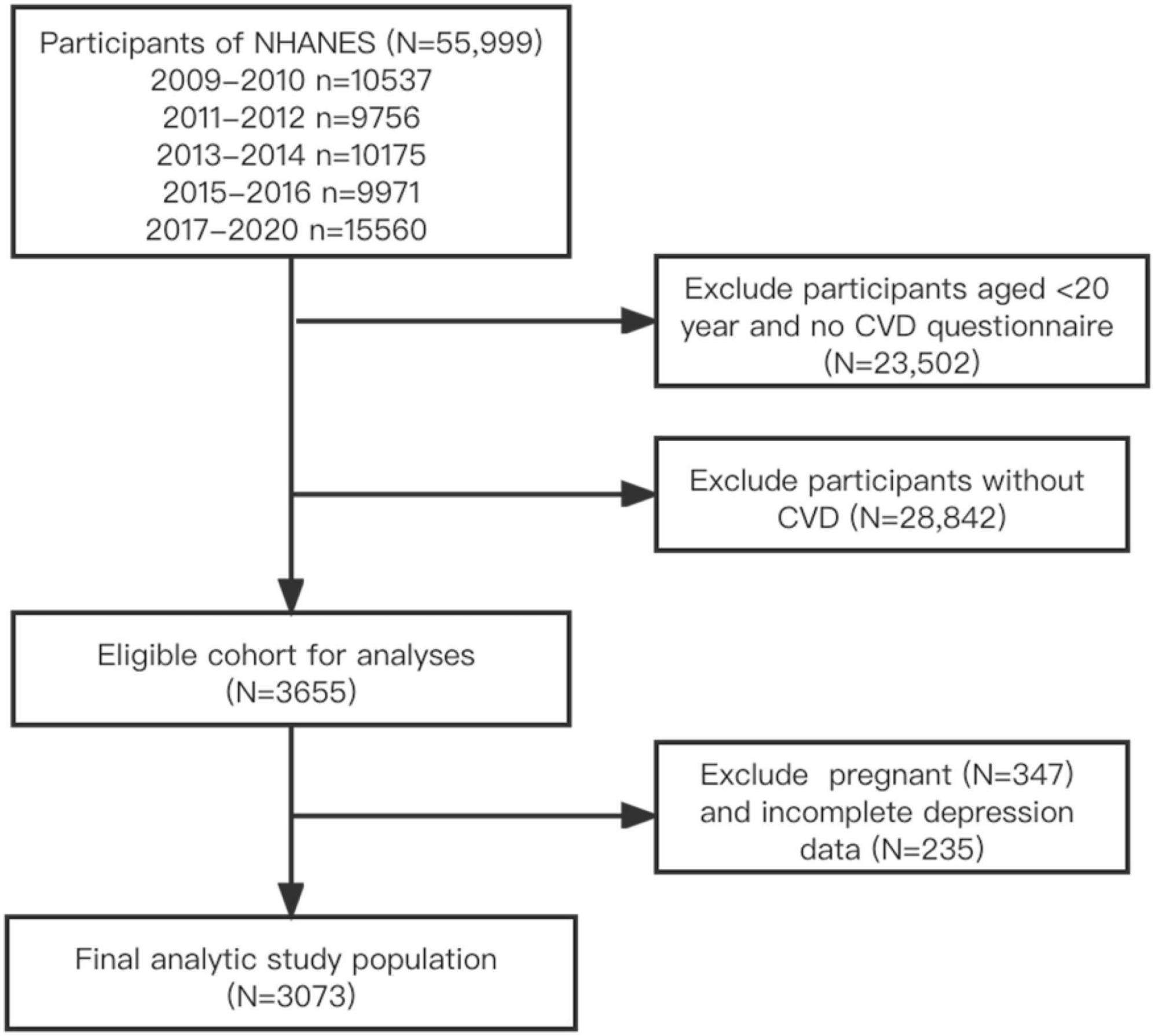
The NHANES is a cross-sectional survey of a nationally representative sample of the civilian, non-institutionalized United States population. Since 1999, NHANES has collected data through in-home personal interviews, as well as physical examinations and laboratory tests in mobile examination centers (MECs), and has released it publicly on a 2-year cycles (28). Accurate forecasts can often be made by combining data from different periods. The time frame of this study covered 11.2 years from 2009 to March 2020 to examine trends in the prevalence of depression among adults with CVD. Participants with CVD over 20 years of age were included, while pregnant women and those without self-reported CVD or depression were excluded. This study was exempt from Institutional Review Board review as it used de-identified, publicly available data. The inclusion and exclusion process for all eligible participants was shown in Figure 1.
Depression assessment
Participants’ depression status was evaluated through trained interviews using the Patient Health Questionnaire (PHQ-9) in MECs. The PHQ-9 is a nine-item questionnaire that has been validated as a reliable assessment tool with good internal consistency and is recommended for screening for depression of varying severity (29, 30). The scale has a total score of 0–27, with a score ≥10 considered clinically relevant depression (CRD). This definition showed good sensitivity and specificity compared with semi and fully structured diagnostic interviews (29).
Cardiovascular disease assessment
Cardiovascular disease was defined as any self-reported congestive heart failure, coronary heart disease, angina, heart attack or stroke. Specifically, if a participant answered “yes” to any of the questions “Has a doctor or other health professional ever told you that you have congestive heart failure/coronary heart disease/angina/heart attack/stroke?” (five separate questions), then he or she would be considered a self-reported CVD patient (31).
Antidepressant treatment
The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM)1 was used to refer to the reasons for receiving the treatment. On this basis, the definition of “receiving antidepressant treatment” in this study was restricted to participants’ self-reported use of antidepressant medications due to a primary diagnosis of “major depressive disorder, single episode, unspecified” (F32.9) or “major depressive disorder, recurrent, unspecified” (F33.9) (32).
Other variables
Other variables included age, gender, race, education level, marital status, poverty income ratio (PIR), body mass index (BMI), smoking, sleep disorders, physical activity, and medical history. Marital status was categorized as cohabitated (including married and living with a partner), solitary (including widowed, divorced, or separated) and never married. Smoking status was categorized as current smoker (who has smoked 100 cigarettes in lifetime and currently smokes cigarettes), former smoker (who has smoked at least 100 cigarettes in lifetime but had quit smoking at the time of interview), and never smoker (who has never smoked or has smoked less than 100 cigarettes in lifetime) (33). Participants were also divided into three income statuses, low (PIR < 1.3), moderate (1.3 ≤ PIR < 3.5), and high (PIR ≥ 3.5), by dividing family income by a poverty threshold specific to household size and survey year, where lower PIR indicates greater poverty (34, 35). The total amount of physical activity was calculated by multiplying the number of minutes of activity per week (min/wk) by the metabolic equivalent of task (MET) of each activity, and was graded as high (MET⋅min/wk ≥ 600) and low (MET⋅min/wk < 600) (36). Regarding the criteria for the presence of comorbidities, diabetes was defined as self-reported physician-diagnosed diabetes, current use of hypoglycemic medications, fasting plasma glucose level ≥126 mg/dL, HbA1c ≥6.5% (37), or 2-h blood glucose (OGTT) ≥200 mg/dL. Hypertension was defined as systolic blood pressure ≥130 mmHg, diastolic blood pressure ≥80 mmHg, self-reported hypertension, or taking antihypertensive medications, where SBP and DBP were obtained by calculating the average of all available blood pressure measurements (37). Hypercholesterolemia was defined as self-reported total cholesterol level ≥240 mg/dL, or taking lipid-lowering drugs. Chronic kidney disease (CKD) was defined as a self-reported diagnosis of CKD.
Study goals and objectives
The primary objectives of this study were to investigate the current prevalence and decadal trends of depression, and to identify predictors of depression among adults with CVD; a secondary objective was to determine the proportion of adults with depression and CVD who are treated with antidepressants.
Statistical analysis
In accordance with the National Center for Health Statistics analysis guidelines, data were weighted to ensure that appropriate estimates were representative of the total civilian non-institutionalized United States population (37–39). Continuous variables were expressed as weighted mean [standard error (SE)], and categorical variables were expressed as number (weighted percentage). The Rao-Scott χ2 test was used to assess whether there were significant differences in sociodemographic characteristics between the depression and non-depression groups. The Taylor linearization method was used to estimate SEs and 95% confidence intervals (CI). Survey-weighted multiple logistic regression analysis was used to identify predictors of depression among CVD patients by calculating odds ratios and 95% CIs, with all categorical variables described above as covariates. To examine trends from 2009 to 2020, we reported p-values for logistic regression with the year of NHANES as a continuous variable (ordered categorical) predicting the prevalence of depression. A 2-sided p < 0.05 was considered statistically significant. Data analyses were performed using R Studio (version 1.4.1717, PBC, United States).
Results
Characteristics of the analytic sample
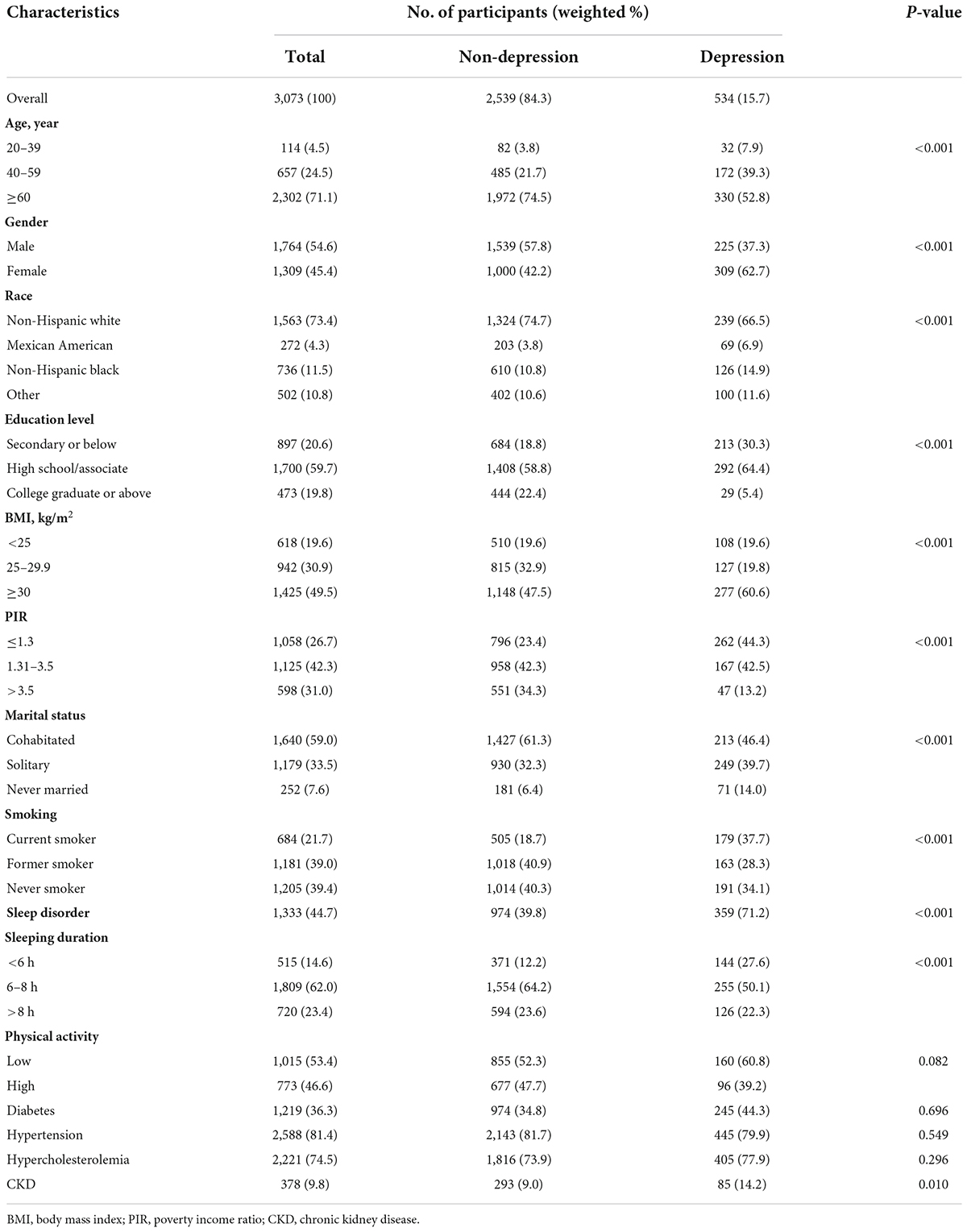
A total of 3,073 participants were analyzed for this study, representing a weighted total population of 18,925,324. Of the 534 participants with depression, the majority (62.7%) were female, 52.8% were older than 60, and 66.5% were non-Hispanic whites (Table 1). Significant differences were found between the depression and non-depression group in age, gender, race, education level, BMI, PIR, marital status, smoking, sleeping duration, and presence of sleep disorder and CKD (p < 0.05).
Prevalence and risk factors of depression
From 2009 to March 2020, the estimated prevalence of depression (defined by PHQ-9 score ≥ 10) among adults with CVD in the United States was 15.7% (95% CI 13.8–17.5%), equivalent to 2.96 million adults. As shown in Table 2, female gender (aOR 1.78, 95% CI 1.20–2.64), and sleep disorder (aOR 2.62, 95% CI 1.78–3.86) remained significant as an independent predictor of depression in adults with CVD after controlling for covariates. In contrast, patients aged ≥60 years, those with college graduates or above, PIR ≥3.5, non-current smoker, and sleeping duration ≥6 h per night were shown to decrease risk of depression.
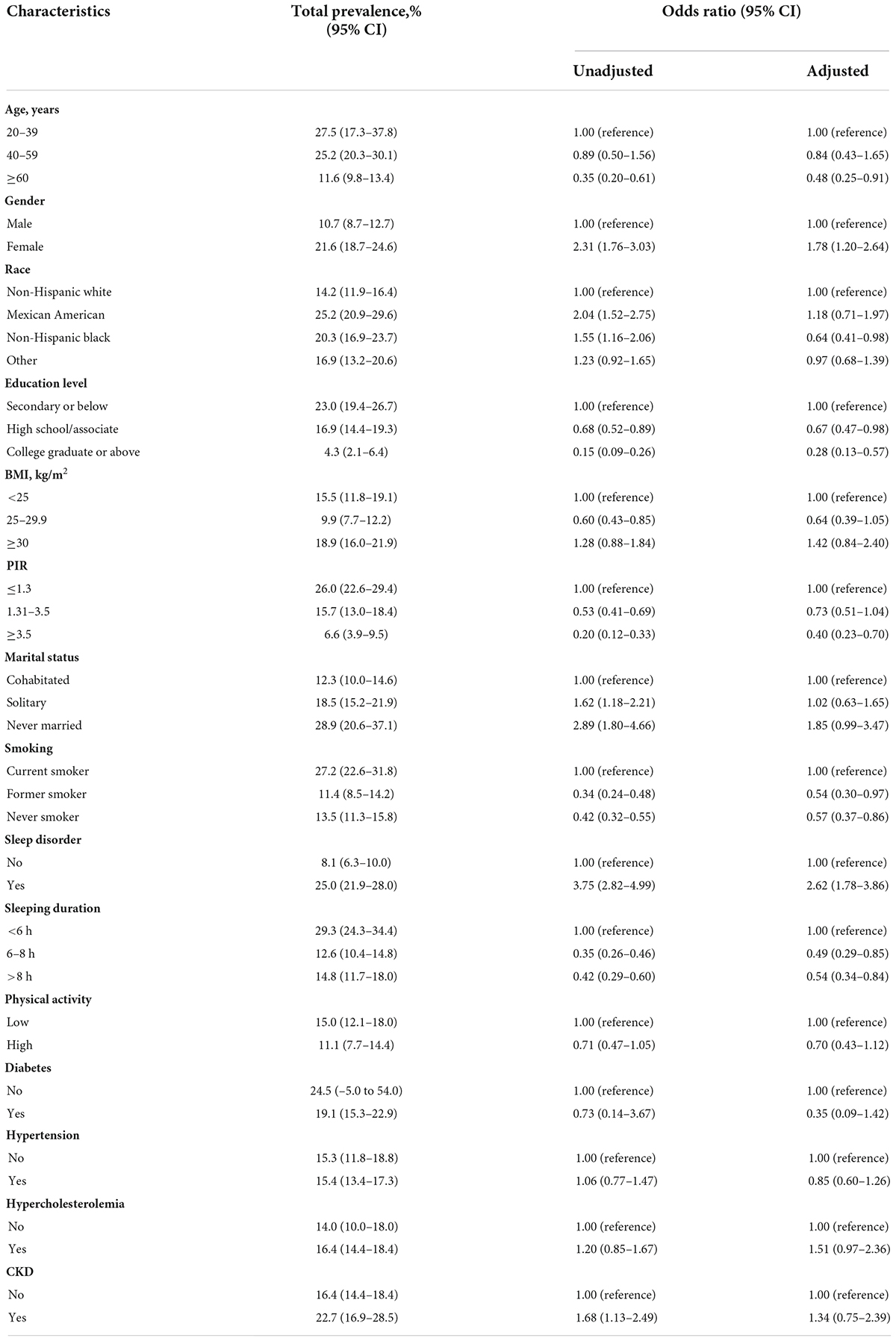
Table 2. Prevalence and odds ratios for depression by characteristics among adults with cardiovascular disease in the United States, 2009–March 2020.
Temporal trends in the prevalence of depression during the study period (2009–March 2020)
As demonstrated in Figure 2 and Table 3, the prevalence of depression (defined by PHQ-9 score ≥ 10) did not change significantly from 2009 to March 2020, neither by sociodemographic characteristics nor by comorbidities (p > 0.05), except in the high-level physical activity group (p = 0.025). Nevertheless, the year 2013–2014 witnessed the highest prevalence at 19.7% (95% CI 15.1–24.4), and regardless of the survey period, women were more likely to suffer from depression than men.
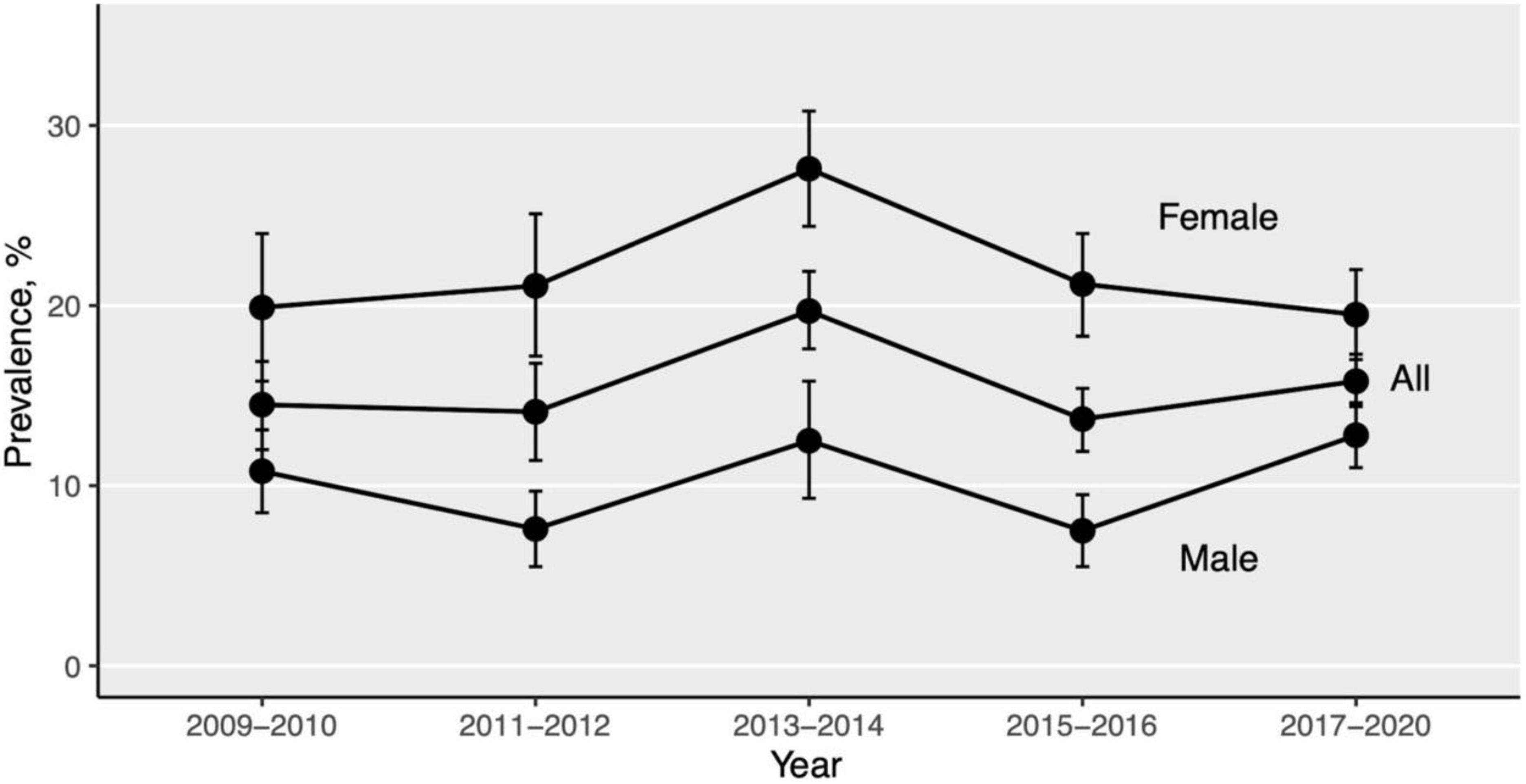
Figure 2. Trends in prevalence of depression by gender, 2009–March 2020. Error bars indicate standard errors. Specific estimates are shown in Table 3.
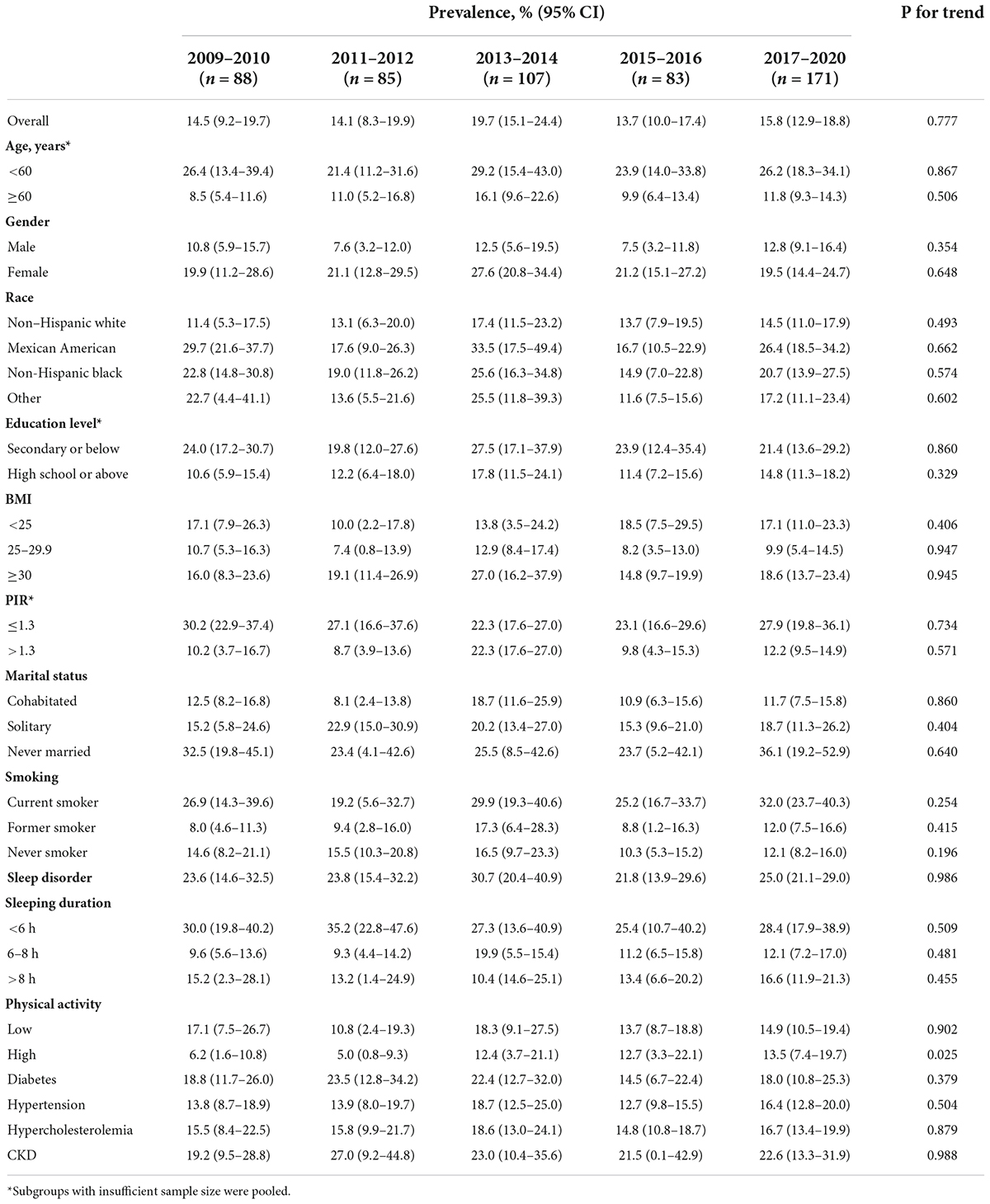
Table 3. Trends in the prevalence of depression among adults with cardiovascular disease in the United States, 2009–March 2020.
Antidepressant treatment in cardiovascular disease patients with depression
The weighted prevalence of antidepressant use among CVD patients with depression was 38.6% (95% CI 30.8–46.5%) from 2013 to March 2020, and remained essentially unchanged during the survey period (p for trend = 0.699). Of the patients who reported taking antidepressants, 42.4% were using selective serotonin reuptake inhibitors (SSRIs). We observed that people without sleep disorders and those who slept 6–8 h a day were less likely to use antidepressants than their counterparts (p = 0.003). There were no statistically significant differences between other subgroups (Table 4).
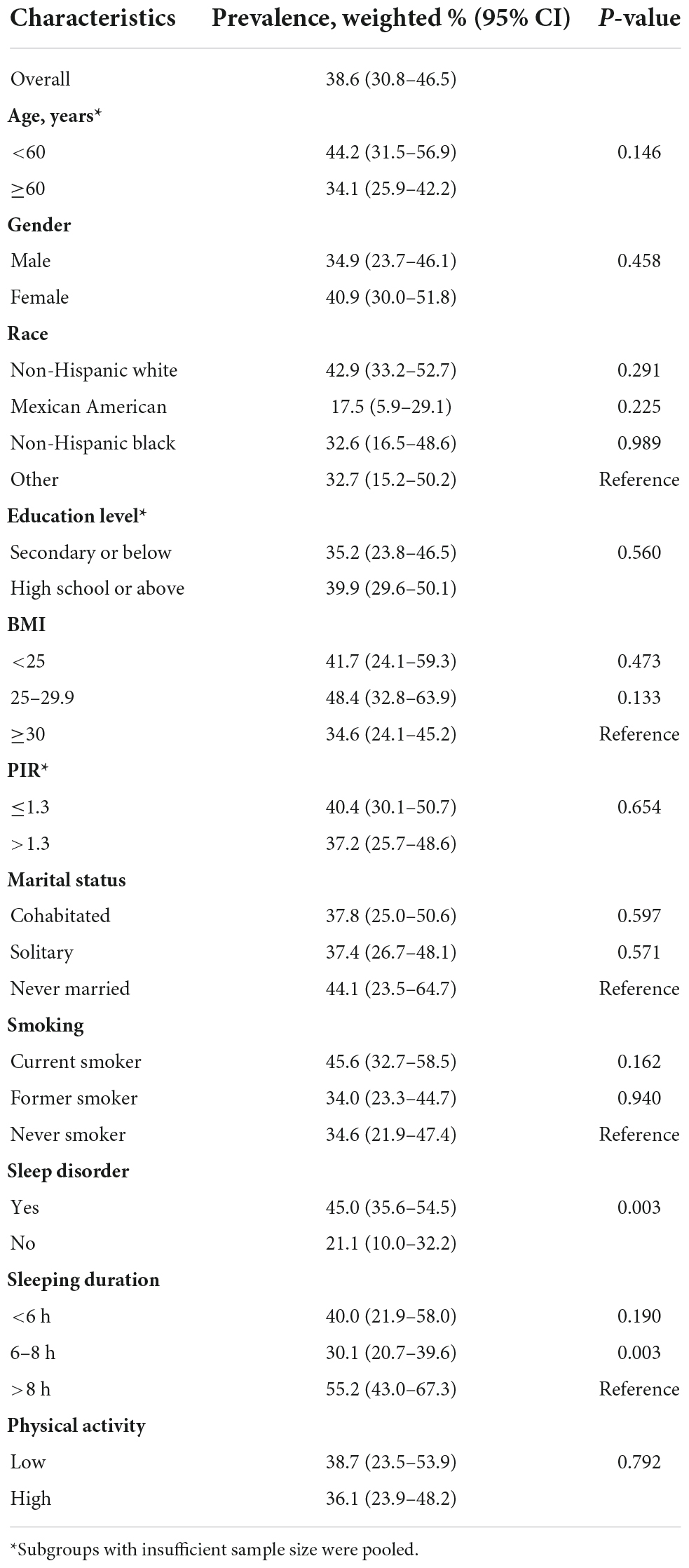
Table 4. Antidepressant use among depressed cardiovascular patients in the United States, 2013–March 2020.
Discussion
In this nationally representative sample of United States adults aged 20 years and older, we observed that the prevalence of depression (defined by PHQ-9 score ≥ 10) among self-reported CVD patients remained fairly high, despite the trend plateauing over the past decade (p for trend = 0.777). Specifically, the estimated prevalence was 15.7% (95% CI 13.8–17.5%) during 2009–March 2020, which was consistent with the prevalence of 15–20% reported in previous studies (21, 40).
In this study, we found that women were almost twice as likely to be depressed as men (21.6 vs. 10.7%) and had a significantly higher risk (aOR 1.78, 95% CI 1.20–2.64), even after controlling for other variables. Similar findings have been documented in other studies conducted in patients with myocardial infarction (MI) (41). The lifetime prevalence of depression and the occurrence of depressive symptoms at the onset of acute MI were also markedly higher in women than in men (48 vs. 24%, 39 vs. 22%, respectively; p < 0.0001) (42, 43). This phenomenon could be partly explained by the fact that women were indeed more prone to depression than men, and not just because they were more likely to remember or report criterion symptoms (44).
Besides this, we noticed that the prevalence of depression was lowest among people aged ≥60 years (11.6%) and non-Hispanic whites (14.2%). Our findings were consistent with previous literature on age (45), but not on racial differences (46, 47), probably due to the use of different screening tools and diagnostic criteria. In our final regression model, blacks are associated lower risk of depression than in whites. Consistently, previous research has found that whites have higher rates of depression than most other racial groups (2). Johnson et al. (46) and Pugh et al. (47) even explicitly claimed that white race was a risk factor for post-stroke depression. Further research is warranted to verify the effect of race on depression among patients with CVD.
In terms of marital status, the unmarried were more likely to suffer from depression than those who were or used to be married despite the association was not significant in the final model. Previous research has repeatedly shown that marital status was associated with depression, and that being married had a protective effect (48–51). These findings prompt clinicians to pay special attention when screening for depression in such subpopulations and further studies are needed to clarify these relations.
Moreover, sleep disorder, another risk factor, nearly tripled the risk of depression in patients with CVD (aOR 2.62, 95% CI 1.78–3.86). Evidence suggested sleep disorders put people at risk for CVD and depression (52). We found an inverse relationship between sleep duration and depression, with those who slept 6–8 h and >8 h per night having a significantly lower risk of depression compared to those who slept <6 h (aOR 0.49, 95% CI 0.29–0.85; 0.54, 95% CI 0.34–0.84, respectively), which was consistent with the literature (53, 54). Although the association between sleep deprivation and depression has been largely established, the impact of prolonged sleep on depression remained controversial (53, 55). In line with a study that included general adults in the NHANES from 2009 to 2016 (55), our findings suggested that those with 6–8 h of sleep had the lowest prevalence (12.6%), not only sleep deprivation but also excessive sleep was associated with depression. Further studies are warranted to clarify the possible causal relationship and underlying mechanisms between sleep and depression.
Early and timely identification through aggressive screening and tailored treatment are recommended when dealing with those vulnerable populations in clinical practice. Correspondingly, high-educated, overweight, high-income, and non-smoking patients with CVD had a lower risk of depression, but still cannot be ignored.
Despite the potential for adverse outcomes, some people with depression, such as women, were undertreated (56). In this study, antidepressant use among United States CVD patients remained steady during 2013–2020 (p for trend = 0.699), with only 38.6% of depressed patients reporting receiving antidepressant therapy. Those with normal sleep patterns and sleep duration were significantly less likely to take the medication (p = 0.003). Among all antidepressants, SSRIs were the most popular choice (42.4%). SSRIs were also considered a relatively safe treatment option which did not increase the rate of cardiovascular side effects or cardiac events in patients with coronary heart disease compared with placebo, and showed modest positive treatment effects (57–60). In contrast, the 2021 European Society of Cardiology (ESC) guidelines have raised specific concerns about increased risk of sudden cardiac death with psychopharmacological treatment (61). Traditional antidepressants, such as tricyclic antidepressants, may increase the risk of cardiac events, all-cause mortality, and adverse drug interactions (62). Rational use of antidepressants in the setting of CVD remains challenging given the current state of the evidence. Further studies are needed to evaluate the safety of other classes of antidepressants. Moreover, cognitive behavioral therapy (CBT), psychotherapy (or “talk therapy”) and nurse-led support can also facilitate patients at risk for CVD (63, 64). Given that depression is strongly related to CVD development and poorer prognosis (10, 61), prompt diagnosis and effective management strategies for depression are critical.
This study has several limitations. First, while we have quantified the disease burden in terms of prevalence and determined risk factors for depression, it should be emphasized that cross-sectional data cannot confirm causality. In addition, quality of life, disease-related costs and potential complications associated with depression were not analyzed. Second, although our study covered a large population sample, it may be subject to response bias and sampling bias due to the use of self-reported PHQ-9, CVD diagnoses, and antidepressant treatment, underestimating target participants, and nor is it absolutely equivalent to a clinical diagnosis of the disease. Therefore, the accuracy of the estimated prevalence derived in this study may need to be reassessed. Future research with more rigorous assessments of depression, such as structured interviews by health professionals, could help address the limitations of current findings. Third, the NHANES data did not record the start and end times of antidepressant treatment, nor the use of non-pharmacological treatments, thus partially limiting our study power. Finally, the timeframe of this study did not include the COVID-19 pandemic, which negatively affected people’s mental health and increased the global prevalence of depression by a massive 25% (65). However, despite these shortcomings, to our knowledge, this is the first study to estimate the prevalence of depression and antidepressant treatment in CVD patients using a well-validated dataset representative of the national United States population.
Conclusion
We elucidated that longitudinal trends in the prevalence of depression among CVD patients in the United States have been stable over the past decade, but was significantly higher in women and those with sleep disorders. Despite the availability of safe and effective treatments, treatment of patients with comorbid depression and CVD remained inadequate. Our findings will provide a reference for future promotion of individualized clinical and pharmacological interventions for high-risk patients.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
ZF: research idea and study design, statistical analysis, and manuscript drafting. ZF and WT: data acquisition and data analysis and interpretation. ZT: writing–review and editing, supervision, and funding acquisition. All authors contributed important intellectual content during manuscript drafting or revision and read and agreed to the published version of the manuscript.
Funding
This work was supported by the start-up grant for Zhijia Tang by Fudan University (No. JIF301001Y).
Acknowledgments
We acknowledge all the participants in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. (2007) 370:851–8. doi: 10.1016/S0140-6736(07)61415-9
2. Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, Goodwin RD. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. (2018) 48:1308–15. doi: 10.1017/S0033291717002781
3. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. (2006) 3:e442. doi: 10.1371/journal.pmed.0030442
4. Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx). Seattle, WA: Institute of Health Metrics and Evaluation (2019).
5. Daly M, Sutin AR, Robinson E. Depression reported by US adults in 2017-2018 and March and April 2020. J Affect Disord. (2021) 278:131–5. doi: 10.1016/j.jad.2020.09.065
6. Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiat. (2003) 54:216–26. doi: 10.1016/S0006-3223(03)00273-7
7. Noel PH, Williams JW Jr, Unutzer J, Worchel J, Lee S, Cornell J, et al. Depression and comorbid illness in elderly primary care patients: impact on multiple domains of health status and well-being. Ann Fam Med. (2004) 2:555–62. doi: 10.1370/afm.143
8. Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiat. (1992) 14:237–47. doi: 10.1016/0163-8343(92)90094-Q
9. Harpole LH, Williams JW Jr, Olsen MK, Stechuchak KM, Oddone E, Callahan CM, et al. Improving depression outcomes in older adults with comorbid medical illness. Gen Hosp Psychiat. (2005) 27:4–12. doi: 10.1016/j.genhosppsych.2004.09.004
10. Zhang Y, Chen Y, Ma L. Depression and cardiovascular disease in elderly: current understanding. J Clin Neurosci. (2018) 47:1–5. doi: 10.1016/j.jocn.2017.09.022
11. Lopez AD, Mathers CD. Measuring the global burden of disease and epidemiological transitions: 2002-2030. Ann Trop Med Parasitol. (2006) 100:481–99. doi: 10.1179/136485906X97417
12. Saint Onge JM, Krueger PM, Rogers RG. The relationship between major depression and nonsuicide mortality for U.S. adults: the importance of health behaviors. J Gerontol B Psychol Sci Soc Sci. (2014) 69:622–32. doi: 10.1093/geronb/gbu009
13. Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiat. (2005) 62:1097–106. doi: 10.1001/archpsyc.62.10.1097
14. Chang SS, Stuckler D, Yip P, Gunnell D. Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ. (2013) 347:f5239. doi: 10.1136/bmj.f5239
15. Riolo SA, Nguyen TA, Greden JF, King CA. Prevalence of depression by race/ethnicity: findings from the National Health and Nutrition Examination Survey III. Am J Public Health. (2005) 95:998–1000. doi: 10.2105/AJPH.2004.047225
16. Shim RS, Baltrus P, Ye J, Rust G. Prevalence, treatment, and control of depressive symptoms in the United States: results from the National Health and Nutrition Examination Survey (NHANES), 2005-2008. J Am Board Fam Med. (2011) 24:33–8. doi: 10.3122/jabfm.2011.01.100121
17. Whiteford HA, Harris MG, McKeon G, Baxter A, Pennell C, Barendregt JJ, et al. Estimating remission from untreated major depression: a systematic review and meta-analysis. Psychol Med. (2013) 43:1569–85. doi: 10.1017/S0033291712001717
18. Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiat. (2017) 16:163–80. doi: 10.1002/wps.20420
19. Henao Perez M, Lopez Medina DC, Lemos Hoyos M, Rios Zapata P. Depression and the risk of adverse outcomes at 5 years in patients with coronary heart disease. Heliyon. (2020) 6:e05425. doi: 10.1016/j.heliyon.2020.e05425
20. Empana JP, Sykes DH, Luc G, Juhan-Vague I, Arveiler D, Ferrieres J, et al. Contributions of depressive mood and circulating inflammatory markers to coronary heart disease in healthy European men: the Prospective Epidemiological Study of Myocardial Infarction (PRIME). Circulation. (2005) 111:2299–305. doi: 10.1161/01.CIR.0000164203.54111.AE
21. Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American heart association. Circulation. (2014) 129:1350–69. doi: 10.1161/CIR.0000000000000019
22. Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. (2006) 27:2763–74. doi: 10.1093/eurheartj/ehl338
23. Wu Q, Kling JM. Depression and the risk of myocardial infarction and coronary death: a meta-analysis of prospective cohort studies. Medicine. (2016) 95:e2815. doi: 10.1097/MD.0000000000002815
24. Cay EL, Vetter N, Philip AE, Dugard P. Psychological status during recovery from an acute heart attack. J Psychosom Res. (1972) 16:425–35. doi: 10.1016/0022-3999(72)90068-2
25. Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. (2006) 48:1527–37. doi: 10.1016/j.jacc.2006.06.055
26. Harshfield EL, Pennells L, Schwartz JE, Willeit P, Kaptoge S, Bell S, et al. Association between depressive symptoms and incident cardiovascular diseases. JAMA. (2020) 324:2396–405. doi: 10.1001/jama.2020.23068
27. Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. (2014) 35:1365–72. doi: 10.1093/eurheartj/eht462
28. Saint-Maurice PF, Troiano RP, Bassett DR Jr, Graubard BI, Carlson SA, Shiroma EJ, et al. Association of Daily Step Count and Step Intensity With Mortality Among US Adults. JAMA. (2020) 323:1151–60. doi: 10.1001/jama.2020.1382
29. Levis B, Benedetti A, Thombs BD, Collaboration DESD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476. doi: 10.1136/bmj.l1476
30. Levis B, Benedetti A, Ioannidis JPA, Sun Y, Negeri Z, He C, et al. Patient health questionnaire-9 scores do not accurately estimate depression prevalence: individual participant data meta-analysis. J Clin Epidemiol. (2020) 122:115–28.e1.
31. Xu C, Liang J, Xu S, Liu Q, Xu J, Gu A. Increased serum levels of aldehydes are associated with cardiovascular disease and cardiovascular risk factors in adults. J Hazard Mater. (2020) 400:123134. doi: 10.1016/j.jhazmat.2020.123134
32. Mojtabai R, Amin-Esmaeili M, Spivak S, Olfson M. Remission and treatment augmentation of depression in the United States. J Clin Psychiat. (2021) 82:21m13988. doi: 10.4088/JCP.21m13988
33. Kahende JW, Adhikari B, Maurice E, Rock V, Malarcher A. Disparities in health care utilization by smoking status–NHANES 1999-2004. Int J Environ Res Public Health. (2009) 6:1095–106. doi: 10.3390/ijerph6031095
34. Xu Y, Wu Q. Prevalence trend and disparities in rheumatoid arthritis among US adults, 2005-2018. J Clin Med. (2021) 10:3289. doi: 10.3390/jcm10153289
35. Lehmler HJ, Simonsen D, Liu B, Bao W. Environmental exposure to pyrethroid pesticides in a nationally representative sample of U.S. adults and children: the National Health And Nutrition Examination Survey 2007-2012. Environ Pollut. (2020) 267:115489. doi: 10.1016/j.envpol.2020.115489
36. Chu NM, Hong J, Harasemiw O, Chen X, Fowler KJ, Dasgupta I, et al. Chronic kidney disease, physical activity, and cognitive function in older adults- results from the National Health And Nutrition Examination Survey (2011-2014). Nephrol Dial Transplant. (2021): [Epub ahead of print]. doi: 10.1093/ndt/gfab338
37. Wang L, Li X, Wang Z, Bancks MP, Carnethon MR, Greenland P, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018. JAMA. (2021) 326:1–13. doi: 10.1001/jama.2021.9883
38. Chen TC, Clark J, Riddles MK, Mohadjer LK, Fakhouri THI. National Health and Nutrition Examination Survey, 2015-2018: sample design and estimation procedures. Vital Health Stat 2. (2020) 184:1–35.
39. Akinbami LJ, Chen TC, Davy O, Ogden CL, Fink S, Clark J, et al. National health and nutrition examination survey, 2017-March 2020 prepandemic file: sample design, estimation, and analytic guidelines. Vital Health Stat 1. (2022) 190:1–36. doi: 10.15620/cdc:115434
40. Peters A, McEwen BS. Stress habituation, body shape and cardiovascular mortality. Neurosci Biobehav Rev. (2015) 56:139–50. doi: 10.1016/j.neubiorev.2015.07.001
41. Mallik S, Spertus JA, Reid KJ, Krumholz HM, Rumsfeld JS, Weintraub WS, et al. Depressive symptoms after acute myocardial infarction: evidence for highest rates in younger women. Arch Intern Med. (2006) 166:876–83. doi: 10.1001/archinte.166.8.876
42. Smolderen KG, Strait KM, Dreyer RP, D’Onofrio G, Zhou S, Lichtman JH, et al. Depressive symptoms in younger women and men with acute myocardial infarction: insights from the VIRGO study. J Am Heart Assoc. (2015) 4:e001424. doi: 10.1161/JAHA.114.001424
43. Parashar S, Rumsfeld JS, Reid KJ, Buchanan D, Dawood N, Khizer S, et al. Impact of depression on sex differences in outcome after myocardial infarction. Circ Cardiovasc Qual Outcomes. (2009) 2:33–40. doi: 10.1161/CIRCOUTCOMES.108.818500
44. Young MA, Fogg LF, Scheftner WA, Keller MB, Fawcett JA. Sex differences in the lifetime prevalence of depression: does varying the diagnostic criteria reduce the female/male ratio? J Affect Disord. (1990) 18:187–92. doi: 10.1016/0165-0327(90)90035-7
45. Goldstein BI, Carnethon MR, Matthews KA, McIntyre RS, Miller GE, Raghuveer G, et al. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease: a scientific statement from the American heart association. Circulation. (2015) 132:965–86. doi: 10.1161/CIR.0000000000000229
46. Johnson JL, Minarik PA, Nystrom KV, Bautista C, Gorman MJ. Poststroke depression incidence and risk factors: an integrative literature review. J Neurosci Nurs. (2006) 38(4 Suppl.):316–27. doi: 10.1097/01376517-200609000-00008
47. Pugh T, Hirsch MA, Nguyen VQC, Rhoads CF III, Harris GM, Yang Q, et al. Depression characterization and race among stroke survivors receiving inpatient rehabilitation. Am J Phys Med Rehabil. (2019) 98:325–30. doi: 10.1097/PHM.0000000000001037
48. Bulloch AGM, Williams JVA, Lavorato DH, Patten SB. The depression and marital status relationship is modified by both age and gender. J Affect Disord. (2017) 223:65–8. doi: 10.1016/j.jad.2017.06.007
49. Jang SN, Kawachi I, Chang J, Boo K, Shin HG, Lee H, et al. Marital status, gender, and depression: analysis of the baseline survey of the Korean longitudinal study of ageing (KLoSA). Soc Sci Med. (2009) 69:1608–15. doi: 10.1016/j.socscimed.2009.09.007
50. Bulloch AG, Williams JV, Lavorato DH, Patten SB. The relationship between major depression and marital disruption is bidirectional. Depress Anxiety. (2009) 26:1172–7. doi: 10.1002/da.20618
51. Inaba A, Thoits PA, Ueno K, Gove WR, Evenson RJ, Sloan M. Depression in the United States and Japan: gender, marital status, and SES patterns. Soc Sci Med. (2005) 61:2280–92. doi: 10.1016/j.socscimed.2005.07.014
52. Gulia KK, Kumar VM. Sleep disorders in the elderly: a growing challenge. Psychogeriatrics. (2018) 18:155–65. doi: 10.1111/psyg.12319
53. Matsui K, Kuriyama K, Yoshiike T, Nagao K, Ayabe N, Komada Y, et al. The effect of short or long sleep duration on quality of life and depression: an internet-based survey in Japan. Sleep Med. (2020) 76:80–5. doi: 10.1016/j.sleep.2020.10.012
54. Liu X, Uchiyama M, Kim K, Okawa M, Shibui K, Kudo Y, et al. Sleep loss and daytime sleepiness in the general adult population of Japan. Psychiat Res. (2000) 93:1–11. doi: 10.1016/S0165-1781(99)00119-5
55. Dong L, Xie Y, Zou X. Association between sleep duration and depression in US adults: a cross-sectional study. J Affect Disord. (2022) 296:183–8. doi: 10.1016/j.jad.2021.09.075
56. Huffman JC, Smith FA, Blais MA, Beiser ME, Januzzi JL, Fricchione GL. Recognition and treatment of depression and anxiety in patients with acute myocardial infarction. Am J Cardiol. (2006) 98:319–24. doi: 10.1016/j.amjcard.2006.02.033
57. Kim JM, Stewart R, Lee YS, Lee HJ, Kim MC, Kim JW, et al. Effect of escitalopram vs placebo treatment for depression on long-term cardiac outcomes in patients with acute coronary syndrome: a randomized clinical trial. JAMA. (2018) 320:350–8. doi: 10.1001/jama.2018.9422
58. Strik JJ, Honig A, Lousberg R, Lousberg AH, Cheriex EC, Tuynman-Qua HG, et al. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med. (2000) 62:783–9. doi: 10.1097/00006842-200011000-00007
59. Glassman AH, O’Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT Jr, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. (2002) 288:701–9. doi: 10.1001/jama.288.6.701
60. Pizzi C, Rutjes AW, Costa GM, Fontana F, Mezzetti A, Manzoli L. Meta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart disease. Am J Cardiol. (2011) 107:972–9. doi: 10.1016/j.amjcard.2010.11.017
61. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Back M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. (2021) 42:3227–337.
62. Prasitlumkum N, Cheungpasitporn W, Tokavanich N, Ding KR, Kewcharoen J, Thongprayoon C, et al. Antidepressants and risk of sudden cardiac death: a network meta-analysis and systematic review. Med Sci. (2021) 9:26. doi: 10.3390/medsci9020026
63. Strachowski D, Khaylis A, Conrad A, Neri E, Spiegel D, Taylor CB. The effects of cognitive behavior therapy on depression in older patients with cardiovascular risk. Depress Anxiety. (2008) 25:E1–10. doi: 10.1002/da.20302
64. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. (2022) 145:e895–1032. doi: 10.1161/CIR.0000000000001073
Keywords: depression, cardiovascular disease, prevalence, risk factor, NHANES
Citation: Feng Z, Tong WK and Tang Z (2022) Longitudinal trends in the prevalence and treatment of depression among adults with cardiovascular disease: An analysis of national health and nutrition examination survey 2009–2020. Front. Psychiatry 13:943165. doi: 10.3389/fpsyt.2022.943165
Received: 16 May 2022; Accepted: 22 August 2022;
Published: 08 September 2022.
Edited by:
Marcin Siwek, Jagiellonian University Medical College, PolandReviewed by:
Xin Li, Nanjing Medical University, ChinaCalvin Heal, The University of Manchester, United Kingdom
Alina Wilkowska, Medical University of Gdańsk, Poland
Copyright © 2022 Feng, Tong and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhijia Tang, zjtang@fudan.edu.cn
 Zhen Feng
Zhen Feng Wai Kei Tong
Wai Kei Tong Zhijia Tang
Zhijia Tang