- 1School of Psychology and Computer Science, University of Central Lancashire, Preston, Lancashire, United Kingdom
- 2Complex Trauma and Resilience Research Unit, Greater Manchester Mental Health NHS Foundation Trust, Manchester Academic Health Science Centre, Manchester, United Kingdom
- 3Division of Psychology and Mental Health, School of Health Sciences, Faculty of Biology, Medicine and Health, Manchester Academic Health Science Centre, The University of Manchester, Manchester, United Kingdom
- 4Greater Manchester Mental Health NHS Foundation Trust, Manchester Academic Health Science Centre, Manchester, United Kingdom
Trauma and trauma-specific mental health difficulties (e.g., post-traumatic stress disorder) are highly prevalent in people with psychosis. However, not everyone develops post-traumatic symptoms, and some people even experience post-traumatic growth (PTG) following trauma. It is important to identify which protective factors are associated with less severe trauma symptoms and/or positive outcomes to inform the development and implementation of interventions fostering these variables. Eighty-five patients with experiences of psychosis took part in a cross-sectional study. They were administered questionnaires measuring exposure to traumatic events, symptoms of PTSD and complex PTSD and potential protective factors assumed to be associated with lower vulnerability for post-traumatic symptoms and higher post-traumatic growth (trait resilience, secure attachment, social support, adaptive coping, optimism, general self-efficacy). Multiple hierarchical regression showed that some of these protective factors, in particular optimism, were associated with lower post-traumatic symptoms, explaining 21% of the variance in complex PTSD symptoms and 16% of the variance in PTSD symptoms. However, the hypothesized protective factors, in particular resilience and adaptive coping, explained a considerably larger proportion of variance in PTG (44%). Our results suggest that whilst these variables provide only moderate protection from the vulnerability to experience post-traumatic stress, they may play an important role in allowing people to find meaning despite multiple traumas and subsequently lead more fulfilling lives. Therapies targeting the emotional and psychological consequences of trauma in people with psychosis might benefit from the integration of intervention strategies to enhance these additional psychological protective factors, which in turn may lead to positive treatment outcomes beyond the mere reduction of post-traumatic stress symptoms.
Introduction
Trauma and trauma-related conditions such as post-traumatic stress disorder (PTSD) are highly prevalent among people with psychosis (1–3). Different relationships have been suggested to exist between trauma, PTSD, and psychosis. Trauma exposure, especially during childhood, can increase vulnerability to psychotic disorders or psychotic-like experiences such as delusions, hallucinations, disorganized thinking, and abnormal behavior (4–6). Furthermore, due to the phenomenological similarity between post-traumatic stress symptoms and specific symptoms of psychosis (e.g., flashbacks and hallucinatory experiences), it has been suggested that psychosis and PTSD could be part of the same spectrum of responses to traumatic events. The way these intrusive experiences are labeled determines the diagnostic interpretation of these symptoms as either a function of psychosis or PTSD (7, 8). Finally, psychotic symptoms or related experiences can be so distressing that they cause symptoms of PTSD—an idea captured with the term psychosis-related PTSD (9, 10).
PTSD is not the only adverse outcome that could follow exposure to traumatic events. In addition to PTSD, the International Classification of Diseases 11th edition manual (ICD-11) proposed the distinct diagnosis of complex PTSD (CPTSD), which is supported by an increasing number of studies (11, 12). CPTSD comprises both the core PTSD symptoms (re-experiencing, avoidance, and sense of threat), plus three additional symptom clusters collectively referred to as “Disturbances in Self Organization” (DSO) (13). These comprise affective dysregulation (i.e., difficulties in regulating emotions, which can manifest in heightened emotional arousal or feeling of numbness and dissociation), negative self-concept (i.e., persistent negative views of the self and extremely negative self-evaluations) and disturbed relationships (i.e., difficulties with developing and maintaining interpersonal relationships, which can result in feeling distant from others) (11). Despite the recognition of the co-occurrence of psychotic symptoms and CPTSD (14), the increasing evidence in support of the ICD-11 CPTSD diagnosis, and research suggesting that psychological constructs consistent with the DSO may be important mediators of the association between trauma and psychosis (15), research specifically focusing on CPTSD in psychosis is still lacking (3, 16).
While PTSD and CPTSD are two recognized negative outcomes that can follow a traumatic experience, research has shown the existence of protective factors that might instead lead to more positive outcomes. These outcomes refer to circumstances when individuals can use their social and personal characteristics to remain immune to the effects of trauma, to “bounce back” to previous levels of adjustment or to prosper and experience post-traumatic growth (PTG) (17). PTG is described as a positive change that people experience after a traumatic event, to the point of developing beyond their previous level of psychological functioning in certain areas of their lives (18). Furthermore, numerous meta-analyses and systematic reviews have been carried out to understand which factors seem to favor different positive outcomes following trauma in non-clinical populations. Social support (19–21), adaptive coping (21, 22), optimism (23, 24), trait resilience (25), self-efficacy (26, 27) and secure attachment (28, 29) are among the factors that seem to be more consistently associated to these positive post-traumatic outcomes.
Some research has been conducted on protective factors from trauma in people with psychosis, and PTG and its underpinnings are being increasingly investigated among service users (30). However, this has not been done as extensively as in other populations and never looking at numerous protective factors within the context of one study. When protective factors such as secure attachment were investigated, they were usually studied in association with their influence on psychotic symptoms [e.g., (31)]. In the rare instances where studies looked specifically at trauma and trauma-related responses in psychosis, research found that trait resilience (32) and adaptive coping (33) mediated the relationship between trauma and psychotic-like experiences, and that social support protected against the effects of trauma (34). To address the paucity of research on the topic, this present study investigated commonly recognized protective factors (social support, adaptive coping, optimism, trait resilience, self-efficacy and secure attachment) for three different post-traumatic outcomes in a sample of people with experiences of psychosis. First, we examined what protective factors were associated to different posttraumatic outcomes (PTSD, DSO and PTG), and then if these factors moderated the relationship between potentially traumatic life events and post-traumatic outcomes. It was hypothesized that: (1) participants with higher scores on the protective factors scales will report less severe symptoms of PTSD and DSO; (2) participants with higher scores on the protective factors scales will report higher scores on the PTG scale; (3) the protective factors will moderate the relationship between the amount of adverse event and PTSD and DSO symptoms severity.
Materials and Methods
Participants
Eighty-five participants were recruited from inpatient and outpatient services and from a list of eligible participants who had previously given consent to be contacted for research purposes by researchers at the authors' institution. Recruitment took place across five NHS Trusts in the North-West of England. Participants were considered eligible if they were: (1) aged 16 or above; (2) able to provide informed consent; (3) experiencing psychosis (e.g., having a diagnosis of schizophrenia) as confirmed with their mental health professional.
Measures
A brief self-report demographic questionnaire was used to collect data on participants' gender, age, nationality, ethnicity, legal status, level of education, employment status, present mental health illnesses and treatment history.
The Trauma And Life Events Checklist [TALE; (35)] is a 22-item self-report measure specifically designed for routine trauma screening in psychosis services. It includes a list of common traumatic or stressful life events commonly reported by people with psychosis. For each event that is endorsed, participants are asked if the event occurred more than once and at which age(s). A total trauma exposure score can be derived by summing the number of items endorsed. Three additional items ask participants to identify which events are still affecting the person, as well as the extent of such impact using a scale from “not at all (0)” to “extremely (10).” Currently, the TALE is the only trauma checklist that includes psychosis-specific potentially traumatic events (e.g., traumatic reactions to psychotic symptoms, unusual behaviors or hospitalizations), and has shown moderate psychometric acceptability overall, with excellent reliability and convergent validity for sexual abuse (35).
The International Trauma Questionnaire [ITQ; (12)] is a self-report assessment tool to assess whether someone meets the criteria for ICD-11 PTSD and CPTSD. It consists of 12 items, 6 items measuring PTSD symptoms (re-experiencing, avoidance, and sense of current threat) and 6 items measuring DSO symptoms (negative self-concept, affective dysregulation, and disturbances in relationship). Impairment caused by PTSD and DSO symptoms is measured with three items each. Each item is rated on a 5-point Likert scale ranging from “Not at all” (0) to “Extremely” (4). In this study, ITQ responses were anchored on the traumatic event described as having the most significant impact on the person's life on the TALE. Possible scores for the PTSD and DSO symptoms subscales range from 0 to 24 and do not include the scores from the impairment items. The criteria for PTSD are met when each relevant symptom scores at least 2 (moderately), and when functional impairment is also observed (at least one of the three items scores ≥2). The criteria for possible CPTSD are met, when, in addition to PTSD, the participant also presents at least moderate scores across each DSO symptom, in conjunction with functional impairment. The ITQ has good psychometric and diagnostic properties and has shown to effectively capture the distinction between PTSD and CPTSD (12). Cronbach's α in this study was excellent for both PTSD 0.81 and DSO 0.89 scales.
The Post-Traumatic Growth Inventory [PTGI; (36)] is a 21-item scale that assesses positive changes occurring in response to major adversities. The items capture valued, positive changes resulting from the experience of trauma and adversity across several areas' of the person's life, including relating to others (e.g., “I have more compassion for others”), developing new possibilities (e.g., “I established a new path for my life”), personal strengths (e.g., “I know better that I can handle difficulties”), spiritual changes (e.g., “I have a stronger religious faith”), and appreciation for life (e.g., “I changed my priorities about what is important in life”). Items are scored on a 6-point Likert-type scale, from “I did not experience this change as a result of my crisis (0)” to “I experienced this change to a very great extent as a result of my crisis (5).” The total score, ranging from 0 to 105, is calculated by adding all the responses. The PTGI has satisfactory internal consistency in previous research (36). The reliability of the total PTGI scores was Cronbach's α = 0.88.
The Connor-Davidson Resilience Scale [CD-RISC; (37)] is a well-established measure of trait resilience that consists of 25 items. Each item is rated on a 5-point Likert scale ranging from “Not at all true” (0) to “True nearly all the time” (4). The total score ranges from 0–100, with higher scores reflecting greater trait resilience. Rating is based on how the respondent has felt during the past month. The CD-RISC demonstrates high construct validity, as well as high internal consistency (38). In this study, the Cronbach's α was 0.92.
The Relationship Questionnaire [RQ; (39)] is a self-report questionnaire that identifies four types of adult attachment styles (secure, dismissing, preoccupied, and fearful). In this study, the RQ was used to measure secure attachment, which is described by a paragraph depicting a confident attitude toward relationships in general. Participants are asked to rate their degree of correspondence with this paragraph on a 7-point scale, ranging from “Disagree strongly (1)” to “Agree strongly (7).” The RQ has shown to have good psychometric properties (39).
The Multidimensional Scale of Perceived Social Support [MSPSS; (40)] is a 12-item, self-report measure that evaluates support from family, friends and significant others, where “significant other” could be any person the participant feels particularly close to. The items are rated on a 7-point Likert-type scale with scores ranging from “very strongly disagree (1)” to “very strongly agree (7).” The MSPSS has demonstrated high internal consistency and convergent validity in a psychiatric sample (41). The scale has shown high internal reliability in this study with Cronbach's α = 0.93.
The Brief Coping Orientation to Problems Experienced inventory [Brief-COPE; (42)] is a 28-item self-report multidimensional inventory assessing 14 different forms of copying, each comprised of 2 items. Participants indicate whether they employed certain coping strategies based on a 4-point Likert scale ranging from “I haven't been doing this at all (1)” to “I've been doing this a lot (4).” Studies have grouped the original 14 coping scales into various overarching subscales. For this study, we used the adaptive coping subscale, which has been previously used in the psychosis literature (33, 43). Adaptive coping included active coping, planning, use of emotional support, use of instrumental support, positive reframing, religion, and humor items. The internal consistency in the present sample was good, with Cronbach's α = 0.78.
The Life Orientation Test-Revised [LOT-R; (44)] assesses individual trait differences in optimism. It contains 10 self-report items which ask respondents to indicate the degree to which they agree or disagree with six general statements, such as “In uncertain times, I usually expect the best,” “Overall, I expect more good things to happen to me than bad,” and “If something can go wrong for me it will (reverse-coded).” The LOT-R also comprises three positive, three negative and four filler items whose scores are not computed. Each item is rated on a 5-point Likert scale ranging from “strongly disagree (0)” to “strongly agree (4).” Higher scores indicate more life optimism. The psychometric properties of the LOT-R have been found to be satisfactory in non-clinical populations (45). The internal consistency in this study was high, with Cronbach's α = 0.90.
The General Self-Efficacy Scale [GSE; (46)] is a self-report measure of self-efficacy beliefs, with a focus on coping with hassles and stressful events. Respondents indicate their agreement with each of the ten items (e.g., “I can always manage to solve difficult problems if I try hard enough”) on a four-point Likert scale ranging from “Not at all true (1)” to “Exactly true (4),” and higher summated score represents better general self-efficacy among the participants. The GSE has shown high internal consistency coefficients for a variety of samples and countries (47). The Cronbach's α in the present study was 0.94.
The Positive And Negative Syndrome Scale [PANSS; (48)] was used to investigate if the severity of psychotic symptoms was a possible covariate in our analysis. Each item is rated on a seven-point severity scale ranging from “Absent (1)” to “Extreme (7)”. The PANSS assesses positive symptoms (e.g., delusions hallucinations) negative symptoms (e.g., blunted affect, emotional withdrawal) and general psychopathology (e.g., anxiety, depression) experienced by the person in the previous week. The PANSS is well established and validated measure of symptom severity in severe mental health problems and has shown to have adequate psychometric properties (49). The interviewer was trained to administer the PANSS and achieved an excellent overall reliability score against gold standard scores (ICC = 0.901). Queries concerning scoring were regularly discussed with the wider research team.
Procedure
After receiving NHS and Health Research Authority ethics approval (reference number: 18/NW/0469), participants were recruited between May 2019 and December 2019. Testing took place in locations convenient to participants, including the participants' homes, hospitals, community mental health centers, and university premises. After providing informed written consent, participants were asked to complete the demographic form, the PANSS clinical interview and the battery of research questionnaires. Participants were then fully debriefed and received £10 as a thank you for participating.
Data Analysis
Established procedures to identify multivariate outliers (combination of unusual scores on at least two variables) (50) found no evidence of influential cases in this dataset. As our variables were not normally distributed, non-parametric correlational analyses (Spearman's ρ) were carried out to examine the bivariate associations between the number of adverse life events, protective factors (adaptive coping, trait resilience, social support, secure attachment, optimism and general self-efficacy) and the outcome variables (PTSD, DSO and PTG). Following bivariate analyses, three multiple hierarchical regression models were conducted to examine whether protective factors predicted each of the post-traumatic outcomes (PTSD, DSO and PTG), and to investigate any increment in variation accounted for the addition of potential confounders (PANSS total, age, gender, and ethnicity). As PTSD and DSO were not normally distributed, the regression models including these dependent variables were bootstrapped. All regression analyses met the assumption of absence of multicollinearity (as confirmed by inspection of collinearity diagnostics, including variance inflation factor and tolerance statistics) and the assumption of normality of residuals. PROCESS (Model 1), a macro for SPSS, was then used to carry out an analysis to investigate if any of the protective factors moderated the relationship between the number of adverse events and outcome variables. All statistical analyses were carried out using SPSS version 25.
Results
Sample Characteristics
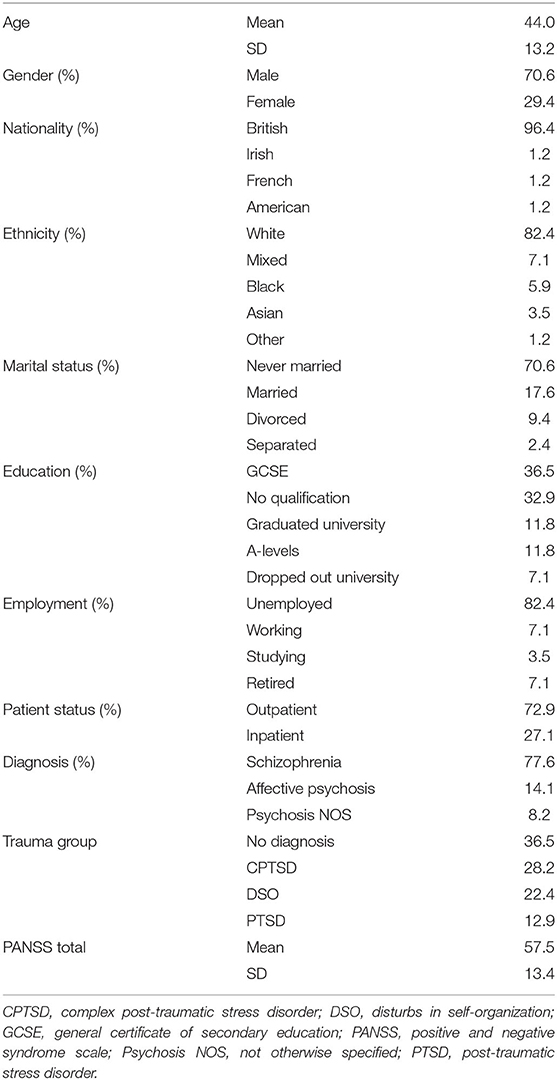
Demographic and descriptive measures for the current sample are displayed in Table 1. In summary, 60 participants were males and 25 were females, with a mean age of 44. Most of our participants had a diagnosis of schizophrenia (78%), followed by affective psychosis (14%) and psychosis NOS (8%). More than half of the participants reported clinically relevant post-traumatic symptoms on the ITQ (64%), with 13% meeting criteria for a diagnosis of PTSD, 29% meeting criteria for a diagnosis of CPTSD, and 22% meeting criteria for DSO symptoms (but not CPTSD).
All participants reported at least two different traumas and three participants reported up to seventeen different traumas out of the twenty included in the TALE. During childhood, 46% reported to have felt unsafe, unloved or unimportant, 31% reported to have experienced sexual abuse, and 20% reported to have gone thirsty, hungry or not have had a safe place to stay. Participants also reported to have often experienced potentially traumatic and highly distressing psychosis-related life events, with 85% reporting to have felt in danger or distress because of psychosis-related experiences, 62% reporting to have experienced a threatening or upsetting contact with mental health services, and 44% reporting acting in a way that put them or someone else in danger or that was strange or embarrassing.
Correlational Analyses
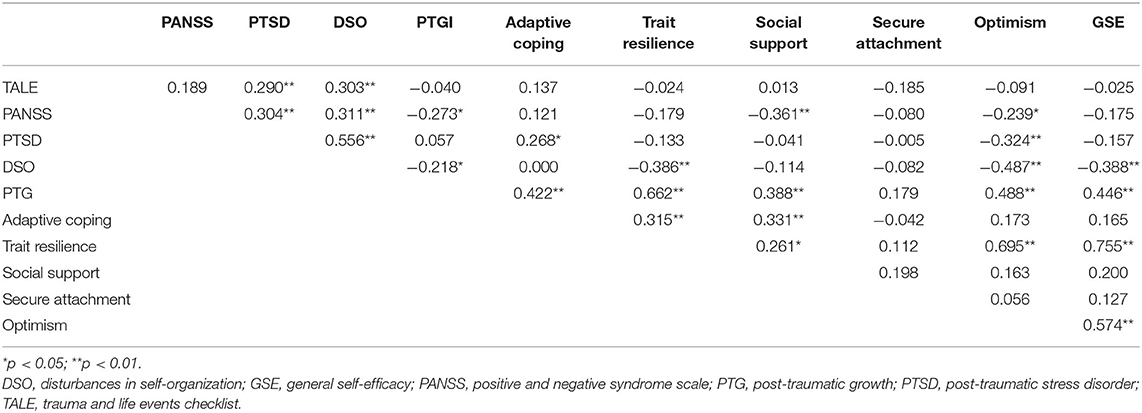
Non-parametric correlational analyses are reported in Table 2. In partial support of our hypothesis, some but not all the protective factors were associated with less severe symptoms of PTSD and DSO. Optimism was associated with lower PTSD scores, whereas resilience, optimism and self-efficacy were associated with lower DSO scores. Contrary to predictions, adaptive coping was associated with higher PTSD symptoms. To better understand this unexpected association, we carried out additional correlation analyses considering the specific subscales of the adaptive coping measure and PTSD, and we found that planning (r = 0.409, p < 0.001), positive reframing (r = 0.220, p = 0.043) and religion (r = 0.254, p = 0.019) were the only subscales positively related to PTSD scores. In partial support of our hypothesis, participants with higher scores on some of the protective factor scales reported higher scores on the PTGI scale. PTG had a significant positive association with adaptive coping, resilience, optimism, and general self-efficacy. Contrary to predictions, secure attachment was not correlated with any post-traumatic outcome. The correlational analysis also showed a relationship between the number of potentially traumatic events as reported in the TALE, and PTSD and DSO. However, no association was found between number of traumatic events and PTG.
Regression Analyses
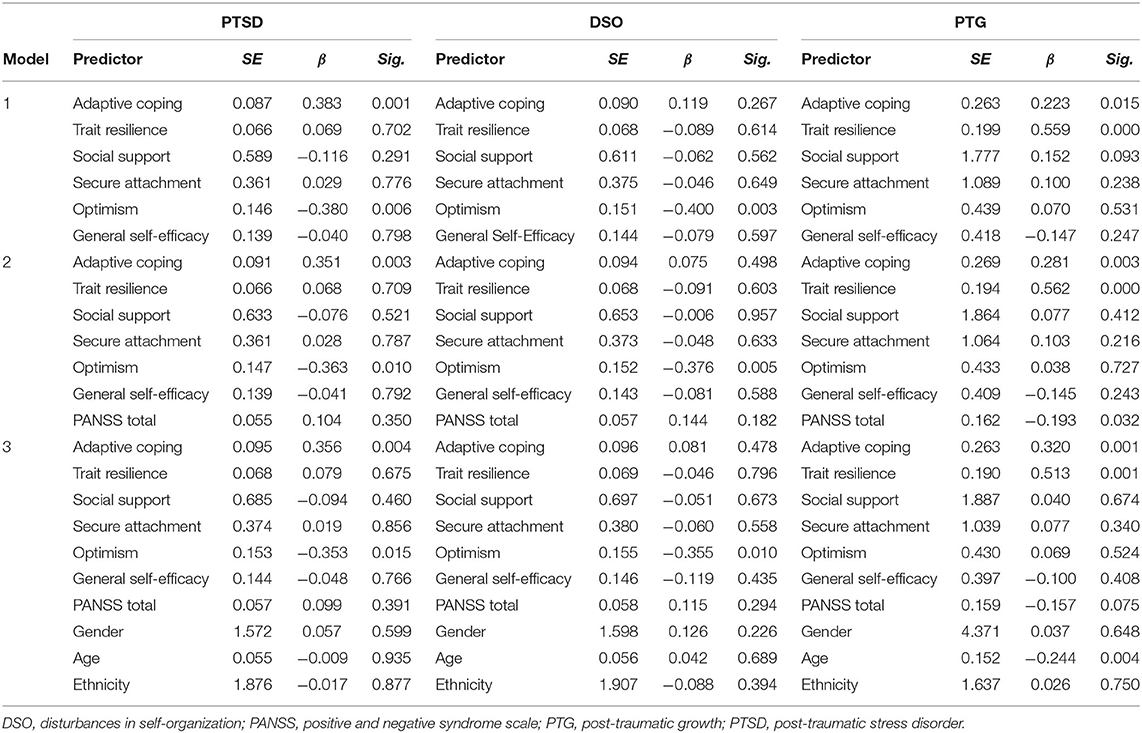
Three separate hierarchical regressions were carried out with post-traumatic outcomes (PTSD, DSO and PTG) as the dependent variables while controlling for psychotic symptoms (PANSS Total) and demographic variables (age, gender, and ethnicity) (Table 3). The first hierarchical regression was carried out with PTSD as the dependent variable. After entering all the protective factors (adaptive coping, resilience, social support, secure attachment, optimism and GSE) in the first step of the analysis, the model explained 16% of the variance in the PTSD outcome [F(6, 78) = 3.74, p = 0.003, R2 = 0.22, = 0.16]. The inclusion of psychotic symptoms in the second step did not significantly improve the prediction of PTSD (R2 = 0.23, significance of R2 change p = 0.35). In step three, the demographic variables did not contribute to the prediction of PTSD (respectively R2 = 0.24, significance of R2 change p = 0.96). Throughout the three steps of the regression, adaptive coping and optimism remained significant. Adaptive coping was positively associated with PTSD symptoms (I: β = 0.383, p = 0.001; II: β = 0.351, p = 0.003; III: β = 0.356, p = 0.004), while optimism was negatively associated with PTSD symptoms (I: β = −0.380, p = 0.006; II: β = −0.363, p = 0.010; III: β = −0.353, p = 0.015).
A second regression model was estimated with DSO as the dependent variable. When entering the protective factors in step one, this model explained 21% of variance [F(6, 78) = 4.79, p < 0.001, R2 = 0.27, = 0.21]. The inclusion of PANSS total in step two (R2 = 0.29, significance of R2 change p = 0.18) and of gender, age and ethnicity in step three (R2 = 0.31, significance of R2 change p = 0.48) did not significantly improve the prediction of DSO. Optimism was the only variable significantly associated with lower DSO symptoms across the three steps of the analysis (I: β = −0.400, p = 0.003; II: β = −0.376, p = 0.005; III: β = −0.355, p = 0.010).
The last hierarchical regression was conducted with PTG as the dependent variable, and in step one the model explained 44% of the variance [F(6, 78) = 12.00, p < 0.001, R2 = 0.48, = 0.44]. In step one, resilience (β = 0.559, p < 0.001) and adaptive coping (β = 0.223, p = 0.015) predicted higher PTG scores. Adding PANSS total in step two significantly improved the prediction of PTG (R2 = 0.51, significance of R2 change p = 0.03). In step two adaptive coping (β = 0.281, p = 0.003) and resilience (β = 0.562, p < 0.001) were still significant predictors; furthermore, it was found that PANSS total was negatively associated with growth (β = −0.193, p = 0.032). Step three also showed a small significant improvement in the prediction of PTG (R2 = 0.57, significance of R2 change p = 0.03). Adaptive coping (β = 0.320, p = 0.001) and resilience (β = 0.513, p = 0.001) remained significant in step three, whereas PANSS was no longer a significant predictor. Age predicted lower PTG scores (β = −0.244, p = 0.004).
Moderation Analysis
A series of moderation analyses were carried out using PROCESS (Model 1) to investigate if any of the protective factors moderated the relationship between the number of adverse life events and post-traumatic outcomes. The results of the analyses (shown in Appendix A) revealed that none of the interaction terms were significant.
Discussion
This study investigated potential protective factors (social support, adaptive coping, optimism, trait resilience, self-efficacy, and secure attachment) and their relationship with post-traumatic outcomes (PTSD, DSO and PTG) in a sample of people experiencing psychosis. We hypothesized that the potential protective factors would be associated with less severe trauma symptoms and higher levels of PTG. We also hypothesized that the protective factors would moderate the relationship between number of adverse life events and post-traumatic outcomes. Correlational analyses showed that PTSD was negatively associated with optimism, DSO was negatively associated with resilience, optimism and general self-efficacy and PTG had a significant positive association with adaptive coping, resilience, optimism and general self-efficacy. Regression analyses carried out for each post-traumatic outcome while controlling for psychotic symptoms and demographic variables showed that adaptive coping predicted higher PTSD symptoms, that optimism negatively predicted both PTSD and DSO symptoms and that resilience and adaptive coping predicted higher PTG. The series of moderation analyses found that none of the protective factors moderated the relationship between adverse life events and PTSD and DSO symptoms.
Our results, in line with previous studies, indicated that participants had experienced multiple traumas and reported high rates of post-traumatic symptoms, with 13% of the sample meeting possible criteria for PTSD and 28% meeting criteria for CPTSD. Twenty-two percent of the sample presented potentially clinically significant DSO scores, despite not meeting criteria for CPTSD. Considering the high levels of DSO symptoms in this sample (across people meeting CPTSD criteria and not), our results suggest that people with psychosis might be more likely to experience complex trauma and particularly prone to develop DSO symptoms, thus supporting the need for more research on complex trauma and psychosis (3). It is also worth noting that most participants reported “psychosis-related traumas” (85% reported being scared by symptoms, 44% reported behaving in dangerous or embarrassing ways and 62% reported being upset from a contact with a mental health service). These results are consistent with previous studies highlighting high rates of psychosis-related trauma and associated post-traumatic stress in psychosis (9, 10). Despite the high rates of psychosis-related trauma, none of these events could be used as index traumas in this study (i.e., the event participants selected when reporting levels of traumatic stress on the ITQ scale). This was because in all cases these traumas were still ongoing and, as the authors of the TALE suggest, it would have been difficult to use ongoing events as a clear anchor for a post-traumatic symptoms assessment (35). Not being able to use psychosis-related traumas highlights the difficulty of assessing PR-PTSD using current PTSD diagnostic tools and suggesting that rates of PTSD and DSO symptoms may be even higher in people experiencing psychosis. It is worth noting that the TALE was developed for clinical purposes, and although it is a highly acceptable measure for people with psychosis, it does not instruct on how to consider the impact of recurrent or ongoing traumatic experiences. The measure, however, has great potential and might be a more sensible way to approach future research about trauma in psychosis, compared to trauma measures that do not capture elements that are specific for this population (i.e., PR-PTSD) (35).
In our analyses, optimism was consistently associated with lower levels of both PTSD and DSO symptoms, even after controlling for potential confounds. These findings support the results of a recent meta-analysis which found that optimism is associated with lower posttraumatic stress symptoms, possibly because it facilitates positive coping and adaptive response to obstacles (51). Longitudinal evidence has also suggested that individuals with high levels of optimism may be less prone to develop post-traumatic symptoms like avoidance and numbing because their optimist beliefs about their ability to cope with threats provide them with higher distress tolerance (52). Although the direction of influence between optimism and traumatic responses is still not clear, our results point at the potential importance of optimism as a protective factor from trauma in psychosis, and to the value of increasing it through targeted interventions (53). Counterintuitively, we found that adaptive coping predicted higher PTSD scores, despite being previously recognized as an important protective factor from post-traumatic outcomes (22), and being measured using a scale widely used with people with psychosis (43). Some items of the Brief-COPE (particularly those on the planning subscale i.e. “I've been trying to come up with a strategy about what to do” and “I've been thinking hard about what steps to take”) could substantially overlap with important processes involved in the maintenance of post-traumatic difficulties, such as avoidance and rumination, which have been shown to be key factors in the maintenance of PTSD symptoms (54). It is worth noting that the religion subscale (i.e., “I've been trying to find comfort in my religion or spiritual beliefs” and “I've been praying or meditating”) was also positively associated with PTSD symptom severity. However, the Brief-COPE only assesses to what extent a participant has adopted a specific coping strategy, and not if they benefited from it. It is possible that participants who tried to find comfort in their religion and failed might have felt hopeless, and might have experienced more traumatic symptoms as a consequence. The positive relationship between PTSD and hopelessness is well documented in the literature (55). This suggests that well-established measures of coping may not be always suitable in the context of assessing adapting coping in response to trauma. Also, prospective studies investigating the effects of religiosity on PTSD report mixed findings, ranging from no effect on symptoms to either improving or worsening (56), resulting in doubts on the effects of religiosity on PTSD.
When we investigated PTG, the results of the correlational and regression analysis showed that resilience and adaptive coping were positively associated with PTG even after controlling for confounds. It is important to note that while resilience and PTG both encompass the idea of thriving in adversity, they are generally regarded as distinct concepts, as resilience refers to positive adaptation despite significant adversity (57), while PTG suggests that people become stronger as a consequence of a trauma (18). Structural equation models have been used to illustrate that trait resilience is an important predictor of PTG (58) and it has been suggested that resilience plays a role in PTG as traumatic experiences may be less traumatic to resilient individuals (59). Supporting our findings, structural equation modeling has also shown that higher levels of adaptive coping predicts higher levels of PTG (60). As growth can coexist with the negative effects of trauma (61), adaptive coping might prove more useful in providing a framework to achieve a sense of control over adversity, which is necessary to experience PTG (62), rather than in protecting from traumatic symptoms. The regression analysis for PTG also suggested that the experience of growth might be negatively affected by the severity of psychotic symptoms, supporting the idea that psychotic symptoms are associated with a range of negative long-term functioning outcomes (63). Previous research on PTG in military personnel found some evidence that age can predict lower PTG scores (64) and suggests that the longer people live, the more likely they might be to experience growth.
Many hypothesized protective factors were not significantly related to any trauma outcomes, suggesting that they may be less important in understanding trauma responses in people with psychosis compared to other samples. Different factors might be more important in predicting trauma outcomes in people with experiences of psychosis, such as the content of voices and unusual beliefs. Furthermore, people with psychosis frequently present risk factors that could potentially interfere with these protective factors. For example, paranoid thoughts and consequent withdrawal from social contact could lead to isolation and prevent people from accessing social support (65). In this study, 15% of our participants could not identify anyone to whom they felt close to when completing the MSPSS, and 6% could only think of a member of their care team when asked who they felt they could rely on. Large social networks are important for improving global functioning in schizophrenia (66), and particularly having a partner helps lower levels of distress (67). In our sample, 22% indicated their romantic partner as their significant other, while 42% chose a family member, 13% chose a friend and 2% chose a religious guide. The relevance of having someone to whom we feel close to is further confirmed by the fact that 22% of our sample indicated “losing a close person” as the most traumatic event they experienced.
Certain protective factors, such as secure attachment, might not have emerged as protective for trauma because they are not very prevalent in people with psychosis. In our sample, 35% agreed to any extent (i.e., mildly, strongly, or very strongly) with the paragraph of the RQ which describes a secure attachment style. These results are not surprising considering that insecure attachment is pervasive in people with psychosis and directly links to psychotic vulnerability especially for paranoia (68, 69). Furthermore, secure attachment is associated with good social support (70) and a positive view of the self (71), both of which might have been lower in our sample, as highlighted by the high levels of DSO symptoms. Having a small sample, along with high levels of isolation, might have prevented social support and secure attachment from being recognized as significant protective factors in our analyses.
The fact that resilience was not found to be consistently protective from trauma is not entirely surprising. While the Connor-Davidson Resilience Scale (37) is recognized as a golden standard measure of resilience and is widely used in research, this tool specifically assesses trait resilience, and does not capture more recent conceptualizations that suggest that positive post-traumatic outcomes result from the combination of social and personal characteristics (17). Our results corroborate the idea that resilience might be better understood in terms of a collection of variables that allow individuals to successfully manage (i.e., cope with) the consequences of trauma, rather than simply as a trait. The results of the moderation analyses also showed that the hypothesized protective factors did not statistically moderate the association between the number of traumatic events and post-traumatic outcomes. However, we suggest that this might be due to our sample which was relatively small and highly traumatized.
This study has important implications as it suggests that interventions aiming to instill hope and optimism in service users, such as hearing stories of recovery or peer supporters who have recovered, might be used in dealing with post-traumatic symptoms. Such intervention might have the additional benefit of increasing hope in mental health staff, which would eventually benefit service users as positive professional expectancies have been recognized to affect patients' hopefulness (72). It is worth noting that most of the investigated protective factors, especially optimism, are already targeted in interventions such as the Cognitive Behavioral Therapy for Psychosis (CBTp), which examines how psychosocial dynamics can reduce the distress associated with the symptoms of psychosis and improve functioning (73, 74). There is strong evidence on the efficacy of CBTp (75), and our findings serve as a reminder of how this intervention could aim at enhancing some of these factors to ultimately facilitate recovery. Our results could also inform trauma therapies such as Trauma-focused Cognitive Behavior Therapy (TF-CBT) and Eye Movement Desensitization and Reprocessing (EMDR), which not only are safe and effective in improving traumatic symptoms in people with psychosis (76, 77), but can improve psychotic symptoms as well (78). According to TF-CBT after a patient processed their trauma and associated traumatic losses, they can start rebuilding life by restoring relationships and returning to pursuing one's aspirations (79), which relates to the proposed protective factor of social support and self-efficacy. Similarly, phase-based multimodal approaches for the treatment of CPTSD greatly focus on creating new meaning (80), which is at the base of the perception of gains necessary to experience growth (81). Our findings stress the importance of working on protective factors rather than on risk factors only and highlight the importance of recognizing post-traumatic growth as a viable post-traumatic outcome that clients could be helped to achieve with adequate support. Including the PTGI in routine clinical assessments, discussing growth with clients and focusing advice, resources and effort on supporting growth as well as recovery, would constitute important steps to support patients' wellbeing. Furthermore, clinicians should also explore the presence of DSO symptoms as these might be more relevant to this population in terms of post-traumatic reactions.
This study has some limitations. As our research was cross-sectional in nature, the results cannot be used to define the direction of influence among the variables investigated. The relatively small and heterogeneous sample limits generalisability, and the fact that participants relied on retrospective recall of childhood and adult trauma might have introduced some recall bias. Future research needs to be conducted with larger samples and longitudinal analyses, which would provide a more robust test for the direction of influence between variables. Studies need to account for the possible moderating effect of risk factors, such as levels of isolation, loneliness and medications. Further studies should examine which factors protect from trauma and foster growth in psychosis, investigating variables more specific for this group, such as therapeutic alliance and positive relationship with voices, both related to more positive outcomes in psychosis (82, 83).
In conclusion, our results highlight the importance of optimism as a protective factor against negative post-traumatic outcomes such as PTSD and CPTSD. Our findings suggest that protective factors such as resilience and adaptive coping might be less important in terms of protecting against negative outcomes, and more important in terms of enabling people to live a meaningful life despite multiple traumas. By focusing on fostering these protective factors, rather than simply reducing factors involved in the maintenance of distressing symptoms, future interventions may lead to a broader range of positive outcomes for trauma survivors who struggle with psychosis.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by NHS and Health Research Authority Ethics Approval (Reference Number: 18/NW/0469). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CC was responsible for data collection, data analysis, and drafting the original manuscript. FV and KB supervised CC during all stages of the research. All authors contributed to the design of this study and approved the final manuscript.
Funding
This study was supported by a doctoral research grant from the University of Manchester. The sponsors had no role in the study design, collection, analysis, or interpretation of the data, or the preparation and approval of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank Dr. Amy Hardy for offering her support in the early design of this study and Dr. Isabelle Butcher for kindly providing feedback on the final manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.735870/full#supplementary-material
References
1. Achim AM, Maziade M, Raymond E, Olivier D, Merette C, Roy MA. How prevalent are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophr Bull. (2011) 37:811–21. doi: 10.1093/schbul/sbp148
2. Beards S, Gayer-Anderson C, Borges S, Dewey ME, Fisher HL, Morgan C. Life events and psychosis: a review and meta-analysis. Schizophr Bull. (2013) 39:740–7. doi: 10.1093/schbul/sbt065
3. Hardy KV, Mueser KT. Trauma, psychosis and posttraumatic stress disorder. Front Psychiatry. (2017) 8:220. doi: 10.3389/fpsyt.2017.00220
4. Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E, Bendall S. Childhood trauma is associated with severity of hallucinations and delusions in psychotic disorders: a systematic review and meta-analysis. Schizophr Bull. (2018) 44:1111–22. doi: 10.1093/schbul/sbx161
5. Gibson LE, Alloy LB, Ellman LM. Trauma and the psychosis spectrum: a review of symptom specificity and explanatory mechanisms. Clin Psychol Rev. (2016) 49:92–105. doi: 10.1016/j.cpr.2016.08.003
6. Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophr Bull. (2012) 38:661–71. doi: 10.1093/schbul/sbs050
7. Morrison AP, Frame L, Larkin W. Relationships between trauma and psychosis: a review and integration. Br J Clin Psychol. (2003) 42:331–53. doi: 10.1348/014466503322528892
8. Morrison AP, Read JE, Turkington DE. Trauma and Psychosis: Theoretical and Clinical Implications. (2005). Washington DC: APA.
9. Berry K, Ford S, Jellicoe-Jones L, Haddock G. PTSD symptoms associated with the experiences of psychosis and hospitalisation: a review of the literature. Clin Psychol Rev. (2013) 33:526–38. doi: 10.1016/j.cpr.2013.01.011
10. Rodrigues R, Anderson KK. The traumatic experience of first-episode psychosis: a systematic review and meta-analysis. Schizophr Res. (2017) 189:27–36. doi: 10.1016/j.schres.2017.01.045
11. Brewin CR, Cloitre M, Hyland P, Shevlin M, Maercker A, Bryant RA, et al. A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clin Psychol Rev. (2017) 58:1–15. doi: 10.1016/j.cpr.2017.09.001
12. Cloitre M, Shevlin M, Brewin CR, Bisson JI, Roberts NP, Maercker A, et al. The International Trauma Questionnaire: development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr Scand. (2018) 138:536–46. doi: 10.1111/acps.12956
13. Maercker A, Brewin CR, Bryant RA, Cloitre M, Reed GM, van Ommeren M, et al. Proposals for mental disorders specifically associated with stress in the International Classification of Diseases-11. Lancet. (2013) 381:1683–5. doi: 10.1016/S0140-6736(12)62191-6
14. Frost R, Louison Vang M, Karatzias T, Hyland P, Shevlin M. The distribution of psychosis, ICD-11 PTSD and complex PTSD symptoms among a trauma-exposed UK general population sample. Psychosis. (2019) 11:187–198. doi: 10.1080/17522439.2019.1626472
15. Williams J, Bucci S, Berry K, Varese F. Psychological mediators of the association between childhood adversities and psychosis: a systematic review. Clin Psychol Rev. (2018) 65:175–96. doi: 10.1016/j.cpr.2018.05.009
16. Grubaugh AL, Zinzow HM, Paul L, Egede LE, Frueh BC. Trauma exposure and posttraumatic stress disorder in adults with severe mental illness: a critical review. Clin Psychol Rev. (2011) 31:883–99. doi: 10.1016/j.cpr.2011.04.003
17. Ayed N, Toner S, Priebe S. Conceptualizing resilience in adult mental health literature: a systematic review and narrative synthesis. Psychol Psychotherapy Theory Res Pract. (2018). doi: 10.1111/papt.12185
18. Tedeschi RG, Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq. (2004) 15:1–18. doi: 10.1207/s15327965pli1501_01
19. Betancourt TS, Borisova I, Williams TP, Meyers-Ohki SE, Rubin-Smith JE, Annan J, et al. Psychosocial adjustment and mental health in former child soldiers—systematic review of the literature and recommendations for future research. J Child Psychol Psychiatry. (2013) 54:17–36. doi: 10.1111/j.1469-7610.2012.02620.x
20. Brooks SK, Dunn R, Amlot R, Greenberg N, Rubin G. Social and occupational factors associated with psychological distress and disorder among disaster responders: a systematic review. BMC Psychol. (2016) 4:18. doi: 10.1186/s40359-016-0120-9
21. Gordon-Hollingsworth AT, Yao N, Chen H, Qian M, Chen S. Understanding the impact of natural disasters on psychological outcomes in youth from mainland China: a meta-analysis of risk and protective factors for post-traumatic stress disorder symptoms. J Child Adolesc Trauma. (2018) 11:205–26. doi: 10.1007/s40653-015-0051-2
22. Sage CAM, Brooks SK, Greenberg N. Factors associated with Type II trauma in occupational groups working with traumatised children: a systematic review. Journal of Mental Health. (2018) 27:457–67. doi: 10.1080/09638237.2017.1370630
23. Greene T, Itzhaky L, Bronstein I, Solomon Z. Psychopathology, risk, and resilience under exposure to continuous traumatic stress: A systematic review of studies among adults living in southern Israel. Traumatology. (2018) 24:83–103. doi: 10.1037/trm0000136
24. Jakšić N, Brajković L, Ivezić E, Topić R, Jakovljević M. The role of personality traits in posttraumatic stress disorder (PTSD). Psychiatria Danub. (2012) 24:256–66.
25. Kornhaber R, Bridgman H, McLean L, Vandervord J. The role of resilience in the recovery of the burn-injured patient: an integrative review. Chron Wound Care Manag Res. (2016) 3:41–50. doi: 10.2147/CWCMR.S94618
26. Fritz J, de Graaff AM, Caisley H, van Harmelen AL, Wilkinson PO. A systematic review of amenable resilience factors that moderate and/or mediate the relationship between childhood adversity and mental health in young people. Front Psychiatry. (2018) 9:230. doi: 10.3389/fpsyt.2018.00230
27. Tol WA, Song S, Jordans MJ. Annual research review: resilience and mental health in children and adolescents living in areas of armed conflict—a systematic review of findings in low- and middle-income countries. J Child Psychol Psychiatry. (2013) 54:445–60. doi: 10.1111/jcpp.12053
28. Barazzone N, Santos I, McGowan J, Donaghay-Spire E. The links between adult attachment and post-traumatic stress: a systematic review. Psychol Psychother Theory, Res Pract. (2019) 92:131–47. doi: 10.1111/papt.12181
29. Woodhouse S, Ayers S, Field AP. The relationship between adult attachment style and post-traumatic stress symptoms: a meta-analysis. J Anxiety Disord. (2015) 35:103–17. doi: 10.1016/j.janxdis.2015.07.002
30. Mazor Y, Gelkopf M, Roe D. Posttraumatic growth among people with serious mental illness, psychosis and posttraumatic stress symptoms. Compr Psychiatry. (2018) 81:1–9. doi: 10.1016/j.comppsych.2017.10.009
31. Carr S, Hardy A, Fornells-Ambrojo M. Relationship between attachment style and symptom severity across the psychosis spectrum: a meta-analysis. Clin Psychol Rev. (2018) 59:145–58. doi: 10.1016/j.cpr.2017.12.001
32. Metel D, Arciszewska A, Daren A, Pionke R, Cechnicki A, Frydecka D, et al. Mediating role of cognitive biases, resilience and depressive symptoms in the relationship between childhood trauma and psychotic-like experiences in young adults. Early Interv Psychiatry. (2020) 14:87–96. doi: 10.1111/eip.12829
33. Ered A, Gibson LE, Maxwell SD, Cooper S, Ellman LM. Coping as a mediator of stress and psychotic-like experiences. European Psychiatry. (2017) 43:9–13. doi: 10.1016/j.eurpsy.2017.01.327
34. Morgan C, Gayer-Anderson C. Childhood adversities and psychosis: evidence, challenges, implications. World Psychiatry. (2016) 15:93–102. doi: 10.1002/wps.20330
35. Carr S, Hardy A, Fornells-Ambrojo M. The Trauma and Life Events (TALE) checklist: development of a tool for improving routine screening in people with psychosis. Eur J Psychotraumatol. (2018) 9:1512265. doi: 10.1080/20008198.2018.1512265
36. Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J Trauma Stress. (1996) 9:455–71. doi: 10.1002/jts.2490090305
37. Connor KM, Davidson JRT. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
38. Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health Qual Life Outcomes. (2011) 9:8. doi: 10.1186/1477-7525-9-8
39. Bartholomew K, Horowitz LM. Relationship questionnaire. Attachment styles among young adults: A test of a four-category model. J Personal Soc Psychol. (1991) 61:226–44. doi: 10.1037/0022-3514.61.2.226
40. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. (1988) 52:30–41. doi: 10.1207/s15327752jpa5201_2
41. Cecil H, Stanley MA, Carrion PG, Swann A. Psychometric properties of the MSPSS and NOS in psychiatric outpatients. J Clin Psychol. (1995) 51, 593–602. doi: 10.1002/1097-4679(199509)51:5<593::AID-JCLP2270510503>3.0.CO;2-W
42. Carver CS. You want to measure coping but your protocol'too long: Consider the brief cope. Int J Behav Med. (1997) 4:92. doi: 10.1207/s15327558ijbm0401_6
43. Misiak B, Kotowicz K, Loska O, Stramecki F, Beszłej JA, Samochowiec J, et al. Decreased use of active coping styles contributes to elevated allostatic load index in first-episode psychosis. Psychoneuroendocrinology. (2018) 96:166–72. doi: 10.1016/j.psyneuen.2018.06.021
44. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. (1994) 67:1063. doi: 10.1037/0022-3514.67.6.1063
45. Glaesmer H, Rief W, Martin A, Mewes R, Brähler E, Zenger M, et al. Psychometric properties and population-based norms of the Life Orientation Test Revised (LOT-R). Br J Health Psychol. (2012) 17:432–45. doi: 10.1111/j.2044-8287.2011.02046.x
46. Schwarzer R, Jerusalem M. General Self-Efficacy Scale Database Record. (1995). Available online at: PsycTESTS.
47. Scholz U, Doña BG, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur J Psychol Assess. (2002) 18:242. doi: 10.1027//1015-5759.18.3.242
48. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
49. Peralta V, Cuesta MJ. Psychometric properties of the positive and negative syndrome scale (PANSS) in schizophrenia. Psychiatry Res. (1994) 53:31–40. doi: 10.1016/0165-1781(94)90093-0
51. Gallagher MW, Long LJ, Phillips CA. Hope, optimism, self-efficacy, and posttraumatic stress disorder: a meta-analytic review of the protective effects of positive expectancies. J Clin Psychol. (2020) 76:329–55. doi: 10.1002/jclp.22882
52. Birkeland MS, Blix I, Solberg Ø, Heir T. Does optimism act as a buffer against posttraumatic stress over time? A longitudinal study of the protective role of optimism after the 2011 Oslo bombing. Psychol Trauma Theory Res Pract Policy. (2017) 9:207. doi: 10.1037/tra0000188
53. Malouff JM, Schutte NS. Can psychological interventions increase optimism? A meta-analysis. J Positive Psychol. (2017) 12:594–604. doi: 10.1080/17439760.2016.1221122
54. Szabo YZ, Warnecke AJ, Newton TL, Valentine JC. Rumination and posttraumatic stress symptoms in trauma-exposed adults: a systematic review and meta-analysis. Anxiety Stress Cop. (2017) 30:396–414. doi: 10.1080/10615806.2017.1313835
55. Florez IA, Allbaugh LJ, Harris CE, Schwartz AC, Kaslow NJ. Suicidal ideation and hopelessness in PTSD: spiritual well-being mediates outcomes over time. Anxiety Stress Coping. (2018) 31:46–58. doi: 10.1080/10615806.2017.1369260
56. Koenig HG, Al-Zaben F, VanderWeele TJ. Religion and psychiatry: recent developments in research. BJPsych Adv. (2020) 26, 262–272. doi: 10.1192/bja.2019.81
57. Luthar SS. Resilience in Development: A Synthesis of Research Across Five Decades. (2006). Amsterdam: Elseiver.
58. Bensimon M. Elaboration on the association between trauma, PTSD and posttraumatic growth: the role of trait resilience. Pers Individ Dif. (2012) 52:782–7. doi: 10.1016/j.paid.2012.01.011
59. Bonanno GA, Wortman CB, Nesse RM. Prospective patterns of resilience and maladjustment during widowhood. Psychol Aging. (2004) 19:260. doi: 10.1037/0882-7974.19.2.260
60. Cao W, Qi X, Cai DA, Han X. Modeling posttraumatic growth among cancer patients: the roles of social support, appraisals, and adaptive coping. Psycho-oncology. (2018) 27:208–15. doi: 10.1002/pon.4395
61. Zieba M, Wiecheć K, Biegańska-Banaś JM, Mieleszczenko-Kowszewicz W. Coexistence of post-traumatic growth and post-traumatic depreciation in the aftermath of trauma: qualitative and quantitative narrative analysis. Front Psychol. (2019) 10:687. doi: 10.3389/fpsyg.2019.00687
62. Schaefer LM, Howell KH, Schwartz LE, Bottomley JS, Crossnine CB. A concurrent examination of protective factors associated with resilience and posttraumatic growth following childhood victimization. Child Abuse Negl. (2018) 85:17–27. doi: 10.1016/j.chiabu.2018.08.019
63. Robertson BR, Prestia D, Twamley EW, Patterson TL, Bowie CR, Harvey PD. Social competence versus negative symptoms as predictors of real world social functioning in schizophrenia. Schizophr Res. (2014) 160:136–41. doi: 10.1016/j.schres.2014.10.037
64. Mark K. M., Stevelink S. A., Choi J., Fear N. T. (2018). Post-traumatic growth in the military: a systematic review. Occup Environ Med. 75:904–15.
65. Lim MH, Gleeson JFM, Alvarez-Jimenez M, Penn DL. Loneliness in psychosis: a systematic review. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:221–38. doi: 10.1007/s00127-018-1482-5
66. Degnan A, Berry K, Sweet D, Abel K, Crossley N, Edge D. Social networks and symptomatic and functional outcomes in schizophrenia: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:873–88. doi: 10.1007/s00127-018-1552-8
67. Kuranova A, Booij SH, de Jonge P, Jeronimus B, Lin A, Wardenaar KJ, et al. Don't worry, be happy: protective factors to buffer against distress associated with psychotic experiences. Schizophr Res. (2020) 223:79–86. doi: 10.1016/j.schres.2020.05.019
68. Bentall RP, Sitko K. The specific role of insecure attachment in paranoid delusions. Attach Theory Psychos Curr Perspect Fut Direct. (2019) 2:13–42. doi: 10.4324/9781315665573-2
69. Lavin R, Bucci S, Varese F, Berry K. The relationship between insecure attachment and paranoia in psychosis: a systematic literature review. Br J Clin Psychol. (2020) 59:39–65. doi: 10.1111/bjc.12231
70. Spence R, Jacobs C, Bifulco A. Attachment style, loneliness and depression in older age women. Aging Ment Health. (2020) 24:837–9. doi: 10.1080/13607863.2018.1553141
71. Mikulincer M, Shaver PR. An attachment perspective on psychopathology. World Psychiatry. (2012) 11:11–5. doi: 10.1016/j.wpsyc.2012.01.003
72. Berry C, Greenwood K. Hope-inspiring therapeutic relationships, professional expectations and social inclusion for young people with psychosis. Schizophr Res. (2015) 168:153–60. doi: 10.1016/j.schres.2015.07.032
73. Brabban A, Byrne R, Longden E, Morrison AP. The importance of human relationships, ethics and recovery-orientated values in the delivery of CBT for people with psychosis. Psychosis. (2017) 9:157–66. doi: 10.1080/17522439.2016.1259648
74. Tai S, Turkington D. The evolution of cognitive behavior therapy for schizophrenia: current practice and recent developments. Schizophr Bull. (2009) 35:865–73. doi: 10.1093/schbul/sbp080
75. Turner DT, Burger S, Smit F, Valmaggia LR, van der Gaag M. What constitutes sufficient evidence for case formulation–driven CBT for psychosis? Cumulative meta-analysis of the effect on hallucinations and delusions. Schizophr Bull. (2020) 46:1072–85. doi: 10.1093/schbul/sbaa045
76. Sin J, Spain D. Psychological interventions for trauma in individuals who have psychosis: a systematic review and meta-analysis. Psychosis. (2017) 9:67–81. doi: 10.1080/17522439.2016.1167946
77. Swan S, Keen N, Reynolds N, Onwumere J. Psychological interventions for post-traumatic stress symptoms in psychosis: a systematic review of outcomes. Front Psychol. (2017) 8:341. doi: 10.3389/fpsyg.2017.00341
78. Brand RM, McEnery C, Rossell S, Bendall S, Thomas N. Do trauma-focussed psychological interventions have an effect on psychotic symptoms? A systematic review and meta-analysis. Schizophr Res. (2018) 195:13–22. doi: 10.1016/j.schres.2017.08.037
79. Ennis N, Shorer S, Shoval-Zuckerman Y, Freedman S, Monson CM, Dekel R. Treating posttraumatic stress disorder across cultures: a systematic review of cultural adaptations of trauma-focused cognitive behavioral therapies. J Clin Psychol. (2020) 76:587–611. doi: 10.1002/jclp.22909
80. Cloitre M, Courtois CA, Charuvastra A, Carapezza R, Stolbach BC, Green BL. Treatment of complex PTSD: Results of the ISTSS expert clinician survey on best practices. J Trauma Stress. (2011) 24:615–27. doi: 10.1002/jts.20697
81. Tedeschi RG, Shakespeare-Finch J, Taku K, Calhoun LG. Posttraumatic Growth: Theory, Research, and Applications. (2018). OxfordShire: Routledge.
82. Browne J, Nagendra A, Kurtz M, Berry K, Penn DL. The relationship between the therapeutic alliance and client variables in individual treatment for schizophrenia spectrum disorders and early psychosis: narrative review. Clin Psychol Rev. (2019) 71:51–62. doi: 10.1016/j.cpr.2019.05.002
Keywords: post-traumatic growth, resilience, PTSD, post-traumatic stress disorder, psychosis, trauma, CPTSD, PTG
Citation: Campodonico C, Berry K, Haddock G and Varese F (2021) Protective Factors Associated With Post-traumatic Outcomes in Individuals With Experiences of Psychosis. Front. Psychiatry 12:735870. doi: 10.3389/fpsyt.2021.735870
Received: 03 July 2021; Accepted: 04 November 2021;
Published: 29 November 2021.
Edited by:
Kate Hardy, Stanford University, United StatesReviewed by:
Saeeda Paruk, University of KwaZulu-Natal, South AfricaKelly M. Standifer, University of Oklahoma Health Sciences Center, United States
Copyright © 2021 Campodonico, Berry, Haddock and Varese. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carolina Campodonico, ccampodonico@uclan.ac.uk
 Carolina Campodonico
Carolina Campodonico Katherine Berry2,3
Katherine Berry2,3 Filippo Varese
Filippo Varese