- 1Faculty of Psychology, Second Military Medical University, Shanghai, China
- 2The Affiliated Suzhou Science and Technology Town Hospital of Nanjing Medical University, Suzhou, China
- 3Changshu Hospital Affiliated to Nanjing University of Traditional Chinese Medicine, Changshu, China
- 4Department of Psychology, Fudan University, Shanghai, China
Introduction: One year after the Coronavirus disease 2019 (COVID-19) outbreak, China has made substantial progress in the prevention and control of the pandemic, while the epidemic situation remains grim in China since virus may easily survive with the falling temperature in winter. The present study aimed to compare the prevalence and associated factors of anxiety between high-risk and low-risk nurses 1 year after the COVID-19 outbreak, and examine the association between resilience and anxiety and its underlying mechanisms.
Method: Connor-Davidson Resilience scale, Perceived Social Support Scale and Generalized Anxiety Disorder Scale were administrated to 701 nurses from Jiangsu Province, China, 1 year after the COVID-19 outbreak. The mediating effect was examined by Mackinnon's four-step procedure, while the moderated mediation model was tested by Hayes PROCESS macro.
Results: The findings presented the prevalence of anxiety among nurses was 21.4% 1 year after the COVID-19 pandemic. High-risk nurses presented a higher prevalence of anxiety (24.5 vs. 19.3%) than low-risk nurses. Age and professional title were significantly associated with anxiety only in high-risk nurses (all P < 0.05). Perceived social support mediated the association between resilience and anxiety and the indirect effect was stronger for high-risk nurses than low-risk nurses.
Conclusion: Anxiety remains prevalent among nurses 1 year after the COVID-19 outbreak, and resilience plays a protective role against anxiety. Programs that enhance resilience and social support should be designed and special attention should be paid to nurses from high-risk units.
Introduction
On December 30, 2019, the Coronavirus Disease 2019 (COVID-19) was first identified in Wuhan, China with unknown etiology (1). The outbreak spread rapidly throughout China and to almost every country (2). In March 2020, World Health Organization (WHO) declared COVID-19 as a global pandemic (3). Currently, the epidemic still rages in many parts of the world. As of January 29, 2021, the number of confirmed COVID-19 cases worldwide has reached 100 million, with more than 2 million confirmed deaths reported (4). Many countries are facing the “second wave” of the COVID-19 outbreak since it is easier for the novel coronavirus to survive with the falling temperature in winter. The epidemic situation is still grim in China and scattered COVID-19 outbreaks are unavoidable (5). A slightly increasing trend in infections has been reported in China during the past month. As of the end of January 2021, a total of 1614 patients were diagnosed with COVID-19 in China (6). To curb the pandemic in this winter, provincial government of Jiangsu has issued notifications to expand nucleic acid testing to a larger scale and enhance the frequency of regular testing (7). There is no doubt that these measures have placed a great burden on the healthcare system. The availability of health care workers is vital in controlling the pandemic.
In the face of the continuing crisis, nurses, as the largest part of health care workers (8), are crucial to the pandemic response and care. Nurses are inevitably confronted with a broad range of stressors such as overwhelming workload caused by the high demand on the strained system, shift duties, work-family conflict and so on (9), which makes them, especially high-risk nurses, more susceptible to poor mental health (10). According to the previous literature, health care workers from high-risk working departments had a higher rate of mental problems than those from low-risk working departments during the COVID-19 outbreak (11). McAlonan et al. (12) pointed out that although no significant differences in the stress level were found between high-risk and low-risk health care workers at the initial stage of Severe Acute Respiratory Syndrome (SARS) outbreak, high-risk nurses exhibited higher levels of stress than low-risk nurses 1 year after the SARS outbreak. Psychological problems negatively affect cognitive functioning, including attention, memory, risk perception and so on, which would further impair work performance (13). Under the current circumstance, it is of great importance to pay special attention to the mental health of nurses as a way of avoiding unnecessary attrition of hospital workforce. Previous literature regarding the psychological impact of COVID-19 on health professionals suggested the heavy mental toll of COVID-19 outbreak in nurses, with anxiety being frequently observed (14, 15). To date, existing literature has rarely investigated the prevalence of anxiety under the current epidemic situation and the differences in the associated factors of anxiety between high-risk and low-risk nurses. Thus, there is an urgent need to explore the impact of COVID-19 on nurses' mental health and potential influential factors of anxiety 1 year after the pandemic.
Resilience is defined as the capacity to successfully thrive and adapt despite encountering adversity (16). Resilience could decrease the negative impact of stressful events on mental health (17). Resilient individuals presented less severe psychological problems and recovered more quickly from the adversity (18). Previous studies have consistently proved the negative association between resilience and anxiety both cross-sectionally and longitudinally (18–20). Thus, we expected that resilience exerted a protective effect on the anxiety of nurses 1 year after the COVID-19 outbreak. Social support is another common protective factor against psychological difficulties. According to the stress-buffering hypothesis proposed by Cohen and Wills (21), social support could act as a buffer against negative outcomes of stress through enhancing the experience of self-esteem and self-efficacy. Perceived social support is the individuals' subjective perception of the amount and quality of supportive resources received from their social networks. Perceived social support is positively correlated with mental well-being and helps individuals cope with stressful events (22, 23). Several recent studies have investigated the role of perceived social support pertaining to anxiety amid the COVID-19 pandemic. Young adults with lower levels of social support had a higher risk of experiencing anxiety symptoms than those with higher levels of social support during the first several weeks of COVID-19 pandemic (24). In a study performed on frontline nurses during the COVID-19 pandemic, nurses with high social support were less likely to suffer from anxiety (25). Furthermore, it is well-documented that resilience as an internal factor and perceived social support as an external factor are highly correlated (26, 27). Resilient people tend to have strong social networks, which are the great sources of support when they are facing the difficulties. Additionally, resilient individuals had more positive perceptions toward current situation, which indicates resilient people would report higher levels of perceived social support than non-resilient people who have the same actual social support (28). Thus, we hypothesized that social support might be the possible pathway through which resilience influences anxiety of nurses 1 year after the COVID-19 pandemic.
Although resilience and social support might influence anxiety of nurses, not all nurses with lower levels of resilience or social support experience more anxiety symptoms. Hence, it is vital to investigate the influential factor that might moderate the associations of resilience and social support with anxiety among nurses 1 year after the COVID-19. As mentioned above (12), high-risk nurses might be more susceptible to develop anxiety 1 year after the outbreak. Thus, we speculated that high-risk nurses might experience higher levels of anxiety than low-risk nurses 1 year after the COVID-19 outbreak and the pathway through which anxiety could be mitigated would be strengthened among high-risk nurses. Specifically, the associations of resilience and social support with anxiety would be stronger for nurses from high-risk units than those from low-risk units 1 year after the COVID-19 pandemic.
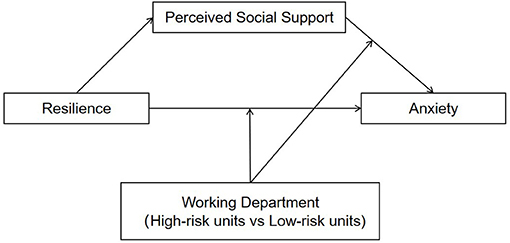
To date, no study has investigated the sustained psychological impact of COVID-19 on nurses and the potential mechanisms underlying the association between resilience and anxiety 1 year after the COVID-19 pandemic, especially differentiating high-risk and low-risk nurses. Therefore, the present study was initiated to investigate the prevalence of anxiety among nurses and compare the associated factors of anxiety between high-risk and low-risk nurses 1 year after the COVID-19 outbreak. Moreover, this study examined the mediating role of social support between resilience and anxiety, and whether the association between resilience and anxiety through perceived social support differed between high-risk and low-risk nurses. A moderated mediation model is proposed to address the hypotheses perceived social support might mediate the effect of resilience on anxiety and the direct and/or indirect (perceived social support—anxiety path) effect of resilience on anxiety might be stronger for high-risk nurses than low-risk nurses 1 year after the COVID-19 pandemic (see Figure 1).
Method
Participants and Procedures
This cross-sectional study was conducted in early January, 2021, 1 year after the outbreak of COVID-19 pandemic. Random cluster sampling was utilized to enroll nurses from 5 local hospitals in Jiangsu Province China. A total of 707 nurses voluntarily completed the questionnaires. The inclusion criteria were as follows: (a) working in the hospital from the height of the COVID-19 outbreak to 1 year after, (b) no dyslexia, and (c) age > 18 years. The exclusion criterion was that respondents reported a history of mental illnesses. Finally, 701 participants were included in the analysis.
Ethical approval was obtained from the Second Military Medical University before the initiation of the research project. Prior to the online survey, informed written consent was given by all participants. Participants were assured their responses were anonymous and confidential. Participants were free to withdraw at any time without penalty.
Measures
Demographics
In the present study, demographic information included age, gender, marital status, educational level, years of working, professional title, and working department. Age was divided into two intervals (younger group and middle-aged group). Marital status was categorized into married and unmarried (single, divorced, and widowed). Educational level was classified into two levels (high school or under and college or above). Years of working was set as a binary variable (5 years or less and more than 5 years). Professional title was divided into three levels: junior, intermediate and senior. Working departments were grouped into high-risk and low-risk units. Nurses from fever clinics, COVID-19 medical unit and emergence department were considered high-risk, while the others were identified as low-risk nurses (29). Fever clinics are specialist clinics that are responsible for the identification of COVID-19 infections. COVID-19 medical units are designated to treat COVID-19 patients. Nurses from emergency department work as the initial hospital caregivers for the badly ill patients with confirmed or suspected COVID-19. Thus, compared with other departments, nurses from fever clinics, COVID-19 medical unit and emergence department have a higher chance of contacting COVID-19 patients.
Resilience
The 25-item Connor-Davidson Resilience scale (CD-RISC) was employed to measure resilience (30). The items used a 5-point Likert scale ranging from 0 (never) to 4 (very often). The Chinese version of CD-RISC supports a three-factor structure including tenacity (i.e., “when things look hopeless, I don't give up”), strength (i.e., “able to adapt to change”), and optimism (i.e., “can deal with whatever comes”). The total scores were the sum of the 25 items and ranged from 0 to 100, with higher scores denoting greater resilience. The scale has demonstrated strong reliability and validity (31, 32). In the current study, the Cronbach's alpha was 0.984 for the total scale, 0.976 for tenacity subscale, 0.960 for strength subscale and 0.854 for optimism subscale.
Perceived Social Support
The Chinese version of Perceived Social Support Scale (PSSS) was utilized to measure the perception of social support quality (33). The scale consists of three subscales indexing the sources of social support from friends (i.e., “I can talk about my problems with my friends”), family (e.g., “I get the emotional help and support I need from my family”) and significant others (e.g., “I have a special person who is a real source of comfort to me”), respectively. Participants were required to rate their agreement with each item using a 7-point Likert scale from 1 (very strongly disagree) to 7 (very strongly agree). Items were summed to yield total scores ranging from 12 to 84. The scale has been widely used with excellent psychometric properties (34, 35). In the present study, the Cronbach's alpha was 0.968 for the overall scale, 0.949 for the friend subscale, 0.938 for the family subscale and 0.908 for the significant others subscale.
Anxiety
The 7-item Generalized Anxiety Disorder Scale (GAD-7) was used to measure anxiety over the past 2 weeks (36). Participants were asked to rate each item on a 4-point Likert scale ranging from 1 (never) to 3 (nearly every day). Item ratings were summed to obtain total scores ranging from 0 to 21, with higher scores representing more severe symptoms of anxiety. The cut-off point for identifying the symptoms of anxiety was 7 (37). The scale has been widely used and adequate psychometric properties have been reported for the Chinese version of GAD-7 (10, 37). The Cronbach's alpha for GAD-7 was 0.952 in the present study.
Statistical Analysis
Firstly, Harman single factor test was employed to test common method bias and descriptive analyses were conducted to describe demographic characteristics stratified by working department. Secondly, linear regressions were used to calculate univariate associations between demographic characteristics and anxiety stratified by working department. Thirdly, Pearson's correlation analyses were calculated to explore the bivariate correlations between the variables of interest. Fourthly, Mackinnon's four-step procedure was employed to examine the mediation effect (38). Four conditions should be met to establish the mediating effect: (1) a significant association of resilience with anxiety; (2) a significant association between resilience and perceived social support; (3) a significant association between perceived social support and anxiety after controlling for resilience; (4) a significant coefficient for the indirect path between resilience and anxiety via perceived social support. The last condition was determined by the bias-corrected percentile bootstrap method, which has been widely employed to construct the sampling distribution of a statistic. Bootstrap sampling is a statistical process that could resample a single dataset to create a distribution of datasets and bootstrap sampling distributions are created by sampling repeatedly with replacement from the original dataset (39). In the present study, bootstrap method produced 95% bias- corrected confidence intervals (CIs) based on 5000 resamples of the data. If the 95% CI does not include zero, the mediating effect would be established. Compared with the traditional causal steps approach, bootstrapping method is better in statistical power and type I error (40). The parameters for the mediation effect were estimated by Hayes (41) PROCESS macro (Model 4).
Finally, we utilized Hayes (41) PROCESS macro (Model 15) to examine the moderated mediation effect. SPSS macro PROCESS, a computational tool, has been widely used to examine complex models with both mediating and moderating variables (42, 43). A set of models have been defined by a model number and preprogrammed into PROCESS. Researchers could choose a model corresponding to the diagram they estimate (44). The 95% CI that excluded zero indicated the establishment of the moderated mediation model. Simple slope test was performed for further analysis.
Age, gender, marital status, educational level, years of working and professional title were included in all models as covariates and all variables were standardized. All statistical analyses were performed using SPSS 25.0 and two-tailed P-values < 0.05 were considered statistically significant.
Results
Common Method Bias Test
The research data were collected using a self-report survey, which indicated a possibility of a common method bias problem (45). The Harman single factor test was conducted to test common method bias (46, 47). The KMO value was 0.963 (p < 0.001), suggesting the research data were suitable for factor analysis. Exploratory factor analysis presented that there were 20 factors with eigenvalues more than 1 and the interpretation rate of the first factor was 25.335%, which did not reach the reference value of 40%. Hence, the results revealed that there was no serious common method bias problem in this research.
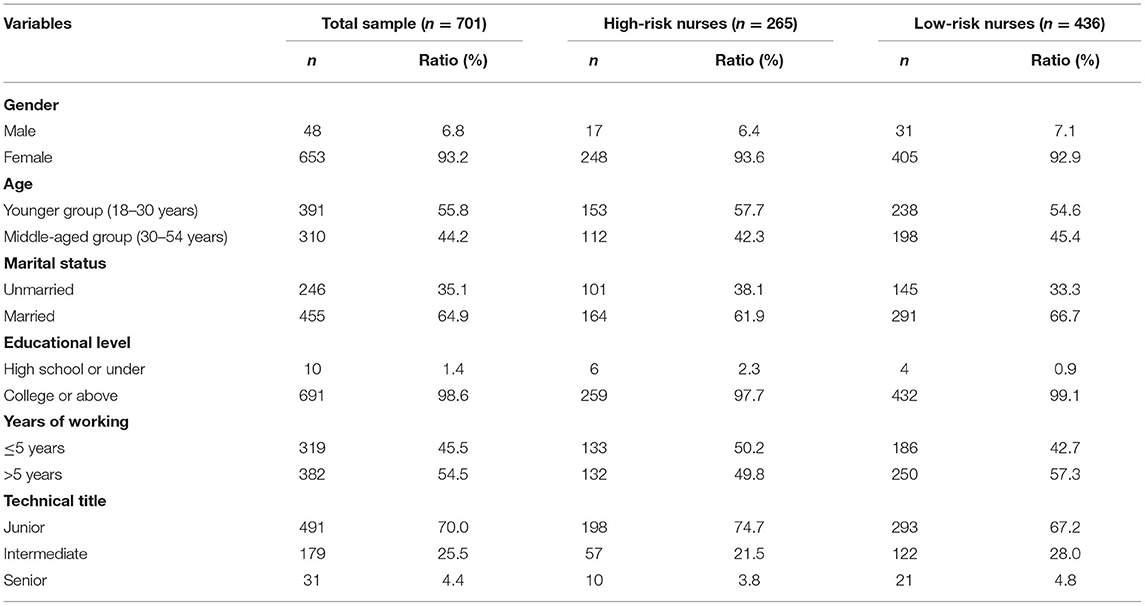
Demographic Characteristics Stratified by Working Department
The demographic characteristics stratified by working department are presented in Table 1. Of the 701 respondents, 265 (37.8%) worked in the high-risk unit. Most of the participants were female [653 (93.2%)], aged below 30 years [391 (55.8%)] and married [455 (64.9%)], had an educational level of college or above [691 (98.6%)], worked more than 5 years [382 (54.5%)] and obtained a junior technical title [491 (70.0%)].
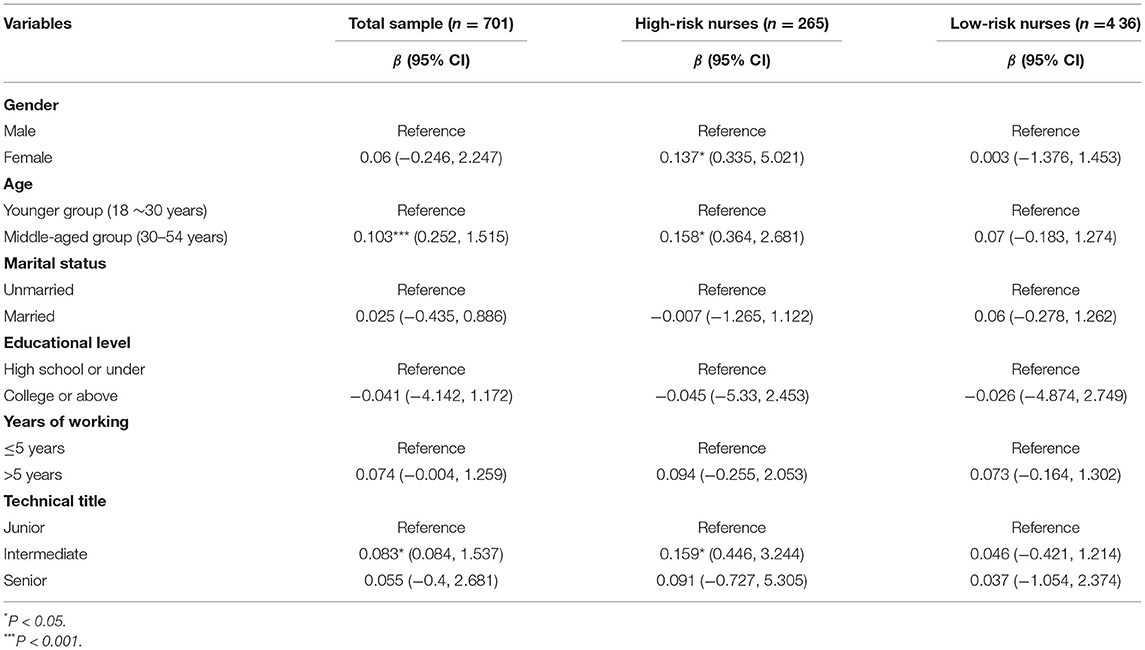
Associations of Demographic Characteristics With Anxiety
The prevalence of anxiety among nurses 1 year after the COVID-19 pandemic was 21.4%. The prevalence of anxiety in high-risk nurses was 24.9%, whereas the rate of anxiety in low-risk nurses was 19.3%. In the univariate linear regression model, high-risk nurses presented a significantly higher level of anxiety than low-risk nurses [β = −0.102, 95% CI = (−1.544, −0.250)]. Female nurses reported more anxiety than males only in high-risk group [β = 0.137, 95% CI = (0.335, 5.021)]. Across the overall sample, middle-aged nurses experienced more symptoms of anxiety [β = 0.103, 95% CI = (0.252, 1.515)]. However, the difference was not significant in low-risk group. In the overall sample, nurses with intermediate professional titles had more anxiety than those with junior professional titles [β = 0.083, 95% CI = (0.084, 1.537)]. Nonetheless, the disparity disappeared in low-risk nurses (see Table 2).
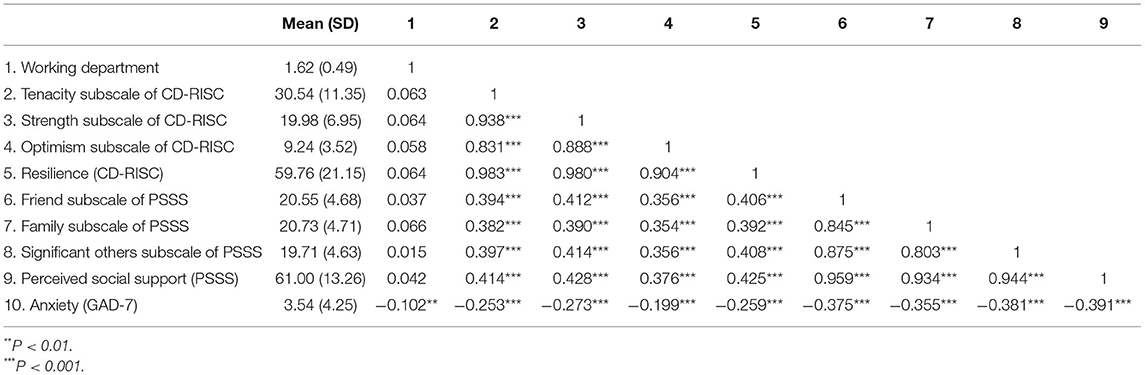
Bivariate Analysis
Table 3 shows the descriptive statistics and correlations among the variables of interest. The results revealed that resilience and its three subscales were all significantly and positively correlated with perceived social support and its three subscales (all P < 0.001). Anxiety was significantly and negatively related to resilience, perceived social support and their subscales (all P < 0.001).
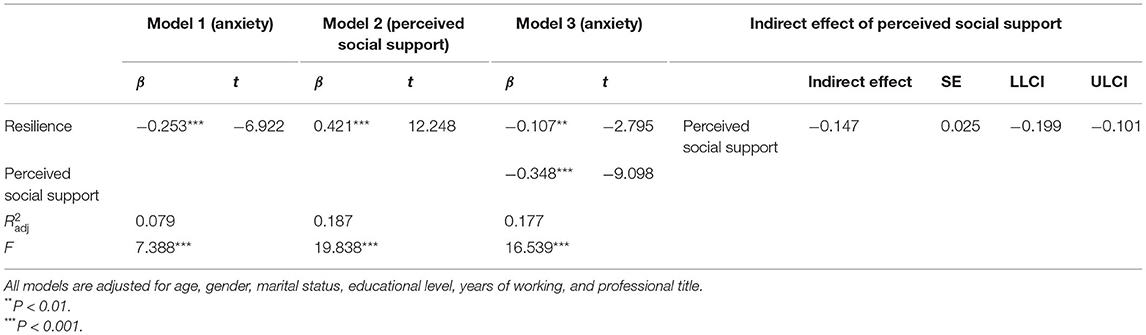
Testing the Mediating Role of Perceived Social Support
As noted, we predicted perceived social support would mediate the association between resilience and anxiety among nurses. MacKinnon's (38) four-step procedure was performed to examine the mediating effect (see Table 4). Firstly, resilience was significantly related to anxiety (β = −0.253, P < 0.001) (see Model 1 in Table 4). Secondly, resilience was significantly associated with perceived social support (β = 0.421, P < 0.001) (see Model 2 in Table 4). Thirdly, perceived social support was significantly associated with anxiety when resilience was controlled (β = −0.348, P < 0.001) (see Model 3 in Table 4). Finally, the biased-corrected percentile bootstrap method indicated the indirect effect of resilience on anxiety via perceived social support was significant [ab = −0.147, SE = 0.025, 95% CI = (−0.199, −0.101)]. The ratio of the indirect effect of the total effect was 57.9%. Thus, all four conditions for the mediation effect have been satisfied and perceived social support mediated the relation between resilience and anxiety among nurses 1 year after the outbreak of COVID-19.
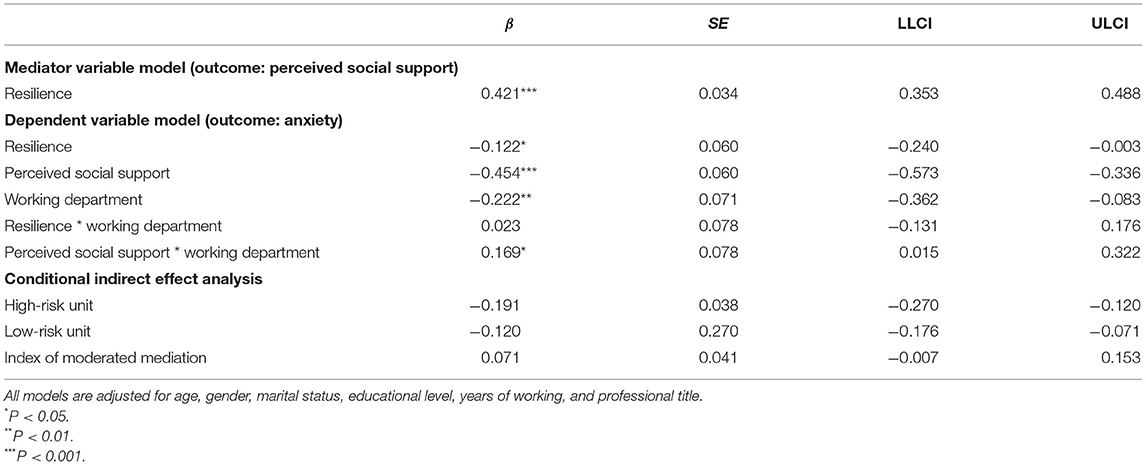
Testing for Moderated Mediation Effect
The study expected the working department would moderate the direct and indirect (the second stage of the mediating path: perceived social support—anxiety) effects of resilience on anxiety. The results showed the interaction of perceived social support and working department had a significant effect on anxiety (β = 0.169, P < 0.05), suggesting the association between perceived social support and anxiety was moderated by working department (see Table 5). Thus, the moderated mediation was established in our study since the second stage of the mediation effect was moderated by working department (41).
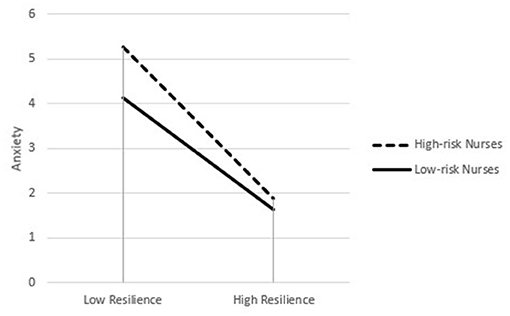
Simple slope analysis revealed perceived social support was significantly and negatively related to anxiety for high-risk nurses (βsimple = −0.285, P < 0.001), while for low-risk nurses, the association between perceived social support and anxiety became insignificant (βsimple = −0.117, P = 0.315). For descriptive purpose, the current study plotted the association between perceived social support and anxiety, separately for high-risk and low-risk nurses (see Figure 2).
Table 5 also presented the indirect effect was moderated by working department. Specifically, the indirect effect of resilience on anxiety through perceived social support was stronger for high-risk nurses [β= −0.191, 95% CI = (−0.270, −0.120)] than low-risk nurses [β = −0.120, 95% CI = (−0.176, −0.071)].
Discussion
Our results revealed that the overall prevalence of anxiety among nurses was 21.4% 1 year after the COVID-19 pandemic, which suggests that more than one-fifth of the nurses suffer from anxiety. This is lower than the one reported by a meta-analysis (15) during the peak period of the COVID-19 pandemic (27%). However, our result is 3 times higher when compared with the reported prevalence of anxiety across the globe (7.3%) in non-epidemic period (48). This indicated, despite the prevalence of anxiety diminished from the peak of the COVID-19 outbreak in 2020 to 1 year after, nurses still experience higher levels of anxiety. The findings also showed the prevalence found in high-risk nurses (24.5%) was higher than that in low-risk nurses (19.3%) 1 year after the outbreak of COVID-19. This is consistent with previous literature, suggesting the ongoing adverse mental health impact is stronger in high-risk nurses 1 year after the SARS outbreak (12). More attentions should still be paid to the anxiety of nurses even 1 year after the pandemic, which might exert the detrimental effect on the safety of patients and prevention and control of COVID-19 (49).
Our study presented that gender was significantly associated with anxiety only in high-risk nurses. However, it is important to note that the sample in the present study is very skewed with regard to the gender variable. The gender-driven finding could be totally biased since 93.2% of the participants were female. Our study also found that age and professional title were significantly associated with anxiety only in high-risk nurses. Compared with younger high-risk nurses, anxiety appeared to reach a higher level among middle-aged nurses. This might be due to the fact that middle-aged nurses were more likely to take responsibilities to raise both elderly parents and young children. Thus, apart from the occupational stress, middle-aged high-risk nurses also faced the greater pressure to raise families (50), which might account for the age difference in anxiety. It is noteworthy to mention high-risk nurses with intermediate professional titles presented the higher level of anxiety than those with junior professional titles. Compared with the inexperienced and inadequately-trained junior nurses, nurses with intermediate professional titles not only need to implement the decisions made by senior nurses with physical and mental labor, but also need to take more responsibilities to guide and help junior nurses to complete the work.
As expected, perceived social support partially mediated the relationship between resilience and anxiety among nurses 1 year after the outbreak, which is consistent with the existing literature regarding the mediating role of social support in the resilience—psychological problems path (51–53). Moreover, the moderated mediation analysis found that working department moderated the indirect effect of resilience on anxiety via perceived social support among nurses, which partially supported our hypothesis. Specifically, nurses from high-risk working units showed stronger association between perceived social support and anxiety 1 year after the COVID-19 pandemic. This study adds to the existing literature by combining internal (resilience) and external (social support) resources and the environmental characteristic (working department) to explore anxiety among nurses 1 year after the outbreak. These findings have profound theoretical and practical implications. This study provided a theoretically grounded framework for a more in-depth understanding of the underlying mechanisms behind the association between resilience and anxiety among nurses. Practically, the present study informed public health policies of the potential preventive measures of anxiety for nurses 1 year after the outbreak. To help prevent anxiety 1 year after the COVID-19 outbreak, programs that enhance resilience and social support should be designed and special attention should be paid to nurses from high-risk units. Additionally, policies on hospital infection-control measures should be designed and implemented to reduce the risk of being infected in the hospital. Before each shift, hospital staff should be screened to check out the signs of COVID-19 infection, such as fever and cough. All staff should be required to wear personal protective equipment and practice social distancing. Emergency infection protocols should be instituted by hospital to contain COVID-19. Clinical inpatient and outpatient services should be adjusted and all non-essential visits should be suspended (54).
Limitation
Some limitations should be addressed when interpreting the results. Firstly, the current study utilized a cross-sectional design, which is insufficient to infer the temporal sequence among variables. We are unable to tease apart the causal relationship. Longitudinal or experimental research should be conducted in the future to verify the findings. Second, the present study utilized self-reported scales, which might bias the association among variables. In the future studies, multi-informant approaches are suggested to collect data. Thirdly, nurses analyzed in our study were only from Jiangsu Province, limiting the generalization of the findings. Further studies are needed to recruit participants from a broad range of geographic regions. Fourthly, we observed a very skewed gender distribution in our sample, with 93.2% of the participants being females. The gender-related findings might be totally biased. Further study should be conducted to replicate our findings in a gender-balanced sample. Fifthly, anxiety could be affected by a variety of factors. The model in our study could just account for a part of the variance. Therefore, a more integrated model of anxiety of nurses is recommended for future research. Finally, apart from anxiety, depression is another common mental disorder that needs to be addressed. Further study should investigate the prevalence of and factors associated with depression 1 year after the COVID-19 pandemic.
To the best of our knowledge, this is the first study to report the prevalence of anxiety among nurses 1 year after the COVID-19 pandemic, and examine the relationship between resilience and anxiety through a moderated mediation model. Anxiety remains prevalent (21.4%) in the nursing workforce 1 year after the COVID-19 outbreak. Special attentions should be paid to nurses from high-risk units, especially those who were middle-aged and had intermediate professional titles. The resilience-based psychological program such as self-enabled distraction and relieving stress from exercise should be designed to prevent and reduce anxiety of nurses (55). Our findings also suggested non-resilient nurses, especially those working in the high-risk unit, could benefit from interventions aiming at the enhancement of perceived social support, including expanding social networks, increasing the quality of social support and so on, 1 year after the COVID-19 pandemic (56).
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Second Military Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
TH, QY, YX, and JG contributed to the writing of this article and the statistical analysis. CN, GD, and WD leaded the whole study, including carrying out this study, and putting forward the study. LB, HL, WC, and YL contributed to the data collection and statistical analysis. All authors contributed to editing the manuscript and have approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to acknowledge all nurses who participated in the research and the research assistants from Naval Medical University.
References
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
2. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. doi: 10.1016/S0140-6736(20)30185-9
3. Mahase E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. (2020) 368:m1036. doi: 10.1136/bmj.m1036
4. World Health Organization. Coronavirus Disease (COVID-19) Pandemic (2021). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed 31 January, 2021).
5. China Daily. Can I Go home for the Spring Festival? Many Places Clearly Need to Meet This Condition (2020). Available online at: http://enapp.chinadaily.com.cn/a/202101/11/AP5ffbd0c4a310f03332f9326d.html
6. National Health Commission of the People's Republic of China. Up to 24 January 31st, the Latest Situation of a COVID-19 Epidemic (2021). Available online at: http://www.nhc.gov.cn/xcs/yqtb/202102/c23e5fc6ffb642a286e3a3fd60afd066.shtml (accessed 25 March, 2021).
7. News J. Jiangsu Issued Notifications on the Prevention and Control of COVID-19 During New Year's Day and Spring Festival in 2021 (2021). Available online at: http://baijiahao.baidu.com/s?id=1687603905718604077&wfr=spider&for=pc
8. Said NB, Chiang VCL. The knowledge, skill competencies, and psychological preparedness of nurses for disasters: a systematic review. Int Emerg Nurs. (2020) 48:100806. doi: 10.1016/j.ienj.2019.100806
9. Zheng R, Zhou Y, Fu Y, Xiang Q, Cheng F, Chen H, et al. Prevalence and associated factors of depression and anxiety among nurses during the outbreak of COVID-19 in China: a cross-sectional study. Int J Nurs Stud. (2021) 114:103809. doi: 10.1016/j.ijnurstu.2020.103809
10. Al Maqbali M, Al Sinani M, Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J Psychosom Res. (2021) 141:110343. doi: 10.1016/j.jpsychores.2020.110343
11. Cai Q, Feng H, Huang J, Wang M, Wang Q, Lu X, et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J Affect Disord. (2020) 275:210–5. doi: 10.1016/j.jad.2020.06.031
12. McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KW, Sham PC, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry Revue Can de Psychiatr. (2007) 52:241–7. doi: 10.1177/070674370705200406
13. Hong S, Ai M, Xu X, Wang W, Chen J, Zhang Q, et al. Immediate psychological impact on nurses working at 42 government-designated hospitals during COVID-19 outbreak in China: a cross-sectional study. Nurs Outlook. (2021) 69:6–12. doi: 10.1016/j.outlook.2020.07.007
14. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
15. Santabárbara J, Bueno-Notivol J, Lipnicki DM, Olaya B, Pérez-Moreno M, Gracia-García P, et al. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: a rapid systematic review (on published articles in Medline) with meta-analysis. Prog Neuro Psychopharm Biol Psychiatry. (2021) 107:110244. doi: 10.1016/j.pnpbp.2021.110244
17. Verdolini N, Amoretti S, Montejo L, García-Rizo C, Hogg B, Mezquida G, et al. Resilience and mental health during the COVID-19 pandemic. J Affect Disord. (2021) 283:156–64. doi: 10.1016/j.jad.2021.01.055
18. Paredes MR, Apaolaza V, Fernandez-Robin C, Hartmann P, Yañez-Martinez D. The impact of the COVID-19 pandemic on subjective mental well-being: the interplay of perceived threat, future anxiety and resilience. Pers Indiv Diff . (2021) 170:110455. doi: 10.1016/j.paid.2020.110455
19. Chen S, Bagrodia R, Pfeffer CC, Meli L, Bonanno GA. Anxiety and resilience in the face of natural disasters associated with climate change: a review and methodological critique. J Anxiety Disord. (2020) 76:102297. doi: 10.1016/j.janxdis.2020.102297
20. Sheerin CM, Lind MJ, Brown EA, Gardner CO, Kendler KS, Amstadter AB. The impact of resilience and subsequent stressful life events on MDD and GAD. Depress Anxiety. (2018) 35:140–7. doi: 10.1002/da.22700
21. Cohen S, Wills T. Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
22. Huang Y, Wu R, Wu J, Yang Q, Zheng S, Wu K. Psychological resilience, self-acceptance, perceived social support and their associations with mental health of incarcerated offenders in China. Asian J Psychiatry. (2020) 52:102166. doi: 10.1016/j.ajp.2020.102166
23. Xu Q, Li S, Yang L. Perceived social support and mental health for college students in mainland China: the mediating effects of self-concept. Psychol Health Med. (2019) 24:595–604. doi: 10.1080/13548506.2018.1549744
24. Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. (2020) 290:113172. doi: 10.1016/j.psychres.2020.113172
25. Labrague LJ, De los Santos JAA. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. (2020) 28:1653–61. doi: 10.1111/jonm.13121
26. Ratajová K, Blatný J, Poláčková Šolcová I, Meier Z, Hornáková T, Brnka R, et al. Social support and resilience in persons with severe haemophilia: an interpretative phenomenological analysis. Haemophilia. (2020) 26:e74–80. doi: 10.1111/hae.13999
27. Yu Y, Peng L, Chen L, Long L, He W, Li M, et al. Resilience and social support promote posttraumatic growth of women with infertility: the mediating role of positive coping. Psychiatry Res. (2014) 215:401–5. doi: 10.1016/j.psychres.2013.10.032
28. Padrón YN, Waxman HC, Lee Y-H. Classroom learning environment differences between resilient, average, and nonresilient middle school students in reading. Educ Urban Soc. (2012) 46:264–83. doi: 10.1177/0013124512446217
29. Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. (2020) 131:132–7. doi: 10.1016/j.jpsychires.2020.09.007
30. Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
31. Xie Y, Peng L, Zuo X, Li M. The psychometric evaluation of the Connor-Davidson resilience scale using a Chinese military sample. PLoS ONE. (2016) 11:e0148843. doi: 10.1371/journal.pone.0148843
32. Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson resilience scale (CD-RISC) with Chinese people. Soc Behav Pers Int J. (2007) 35:19–30. doi: 10.2224/sbp.2007.35.1.19
33. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. (1988) 52:30–41. doi: 10.1207/s15327752jpa5201_2
34. Xiang G, Teng Z, Li Q, Chen H, Guo C. The influence of perceived social support on hope: a longitudinal study of older-aged adolescents in China. Child Youth Serv Rev. (2020) 119:105616. doi: 10.1016/j.childyouth.2020.105616
35. Zhao X, Zhang D, Wu M, Yang Y, Xie H, Li Y, et al. Loneliness and depression symptoms among the elderly in nursing homes: a moderated mediation model of resilience and social support. Psychiatry Res. (2018) 268:143–51. doi: 10.1016/j.psychres.2018.07.011
36. He XY, Li CB, Qian J, Cui HS, Wu WY. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatient. Shanghai Arch Psychiatry. (2010) 22:200–3.
37. Tong X, An D, McGonigal A, Park S-P, Zhou D. Validation of the generalized anxiety disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. (2016) 120:31–6. doi: 10.1016/j.eplepsyres.2015.11.019
38. MacKinnon D. An Introduction to Statistical Mediation Analysis. New York, NY: Taylor & Francis Group (2008). p. 245.
39. Levy JA, Landerman LR, Davis LL. Advances in mediation analysis can facilitate nursing research. Nurs Res. (2011) 60:333–9. doi: 10.1097/NNR.0b013e318227efca
40. Eugene DR, Du X, Kim YK. School climate and peer victimization among adolescents: a moderated mediation model of school connectedness and parental involvement. Child Youth Serv Rev. (2021) 121:105854. doi: 10.1016/j.childyouth.2020.105854
41. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Press (2013).
42. Cero I, Sifers SK. Parenting behavior and the interpersonal-psychological theory of suicide: a mediated moderation analysis with adolescents. J Affect Disord. (2013) 150:987–92. doi: 10.1016/j.jad.2013.05.025
43. Fu X, Liu J, Liu R-D, Ding Y, Hong W, Jiang S. The impact of parental active mediation on adolescent mobile phone dependency: a moderated mediation model. Comput Hum Behav. (2020) 107:106280. doi: 10.1016/j.chb.2020.106280
44. Hayes AF, Montoya AK, Rockwood NJ. The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Aust Mark J. (2017) 25:76–81. doi: 10.1016/j.ausmj.2017.02.001
45. Campbell DT, Fiske DW. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol Bull. (1959) 56:81–105. doi: 10.1037/h0046016
46. Zhou H, You LR. Statistical remedies for common method biases. Adv Psychol Sci. (2004) 6:942–50.
47. Pan Y, Yang Z, Han X, Qi S. Family functioning and mental health among secondary vocational students during the COVID-19 epidemic: a moderated mediation model. Pers Individ Diff . (2021) 171:110490. doi: 10.1016/j.paid.2020.110490
48. Stein DJ, Scott KM, de Jonge P, Kessler RC. Epidemiology of anxiety disorders: from surveys to nosology and back. Dialogues Clin Neurosci. (2017) 19:127–36. doi: 10.31887/DCNS.2017.19.2/dstein
49. Thatrimontrichai A, Weber DJ, Apisarnthanarak A. Mental health among healthcare personnel during COVID-19 in Asia: a systematic review. J Formos Med Assoc. (2021). doi: 10.1016/j.jfma.2021.01.023. [Epub ahead of print].
50. Vlachantoni A, Evandrou M, Falkingham J, Gomez-Leon M. Caught in the middle in mid-life: provision of care across multiple generations. Ageing Soc. (2019) 40:1490–510. doi: 10.1017/S0144686X19000047
51. Ong HL, Vaingankar JA, Abdin E, Sambasivam R, Fauziana R, Tan M-E, et al. Resilience and burden in caregivers of older adults: moderating and mediating effects of perceived social support. BMC Psychiatry. (2018) 18:27. doi: 10.1186/s12888-018-1616-z
52. Ruisoto P, Contador I, Fernández-Calvo B, Serra L, Jenaro C, Flores N, et al. Mediating effect of social support on the relationship between resilience and burden in caregivers of people with dementia. Arch Gerontol Geriatr. (2020) 86:103952. doi: 10.1016/j.archger.2019.103952
53. Xu J, Ou L. Resilience and quality of life among Wenchuan earthquake survivors: the mediating role of social support. Public Health. (2014) 128:430–7. doi: 10.1016/j.puhe.2014.03.002
54. Derraz I. Stroke health care use and COVID-19. Am J Neuroradiol. (2020) 41:E36. doi: 10.3174/ajnr.A6563
55. Donohoe J, O'Rourke M, Hammond S, Stoyanov S, O'Tuathaigh C. Strategies for enhancing resilience in medical students: a group concept mapping analysis. Acad Psychiatry. (2020) 44:427–31. doi: 10.1007/s40596-020-01208-x
Keywords: coronavirus disease 2019, anxiety, high-risk nurses, low-risk nurses, resilience, perceived social support
Citation: Hou T, Yin Q, Xu Y, Gao J, Bin L, Li H, Cai W, Liu Y, Dong W, Deng G and Ni C (2021) The Mediating Role of Perceived Social Support Between Resilience and Anxiety 1 Year After the COVID-19 Pandemic: Disparity Between High-Risk and Low-Risk Nurses in China. Front. Psychiatry 12:666789. doi: 10.3389/fpsyt.2021.666789
Received: 11 February 2021; Accepted: 22 April 2021;
Published: 24 May 2021.
Edited by:
Christos Theleritis, National and Kapodistrian University of Athens, GreeceReviewed by:
Elena V. Libin, Independent Researcher, Chevy Chase, United StatesYinzi Jin, Peking University, China
Copyright © 2021 Hou, Yin, Xu, Gao, Bin, Li, Cai, Liu, Dong, Deng and Ni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunyan Ni, szkjcyy_ncy@126.com; Guanghui Deng, bfbedu@126.com; Wei Dong, sophiedongwei@163.com
†These authors have contributed equally to this work and share first authorship
 Tianya Hou1†
Tianya Hou1† Qianlan Yin
Qianlan Yin Wenpeng Cai
Wenpeng Cai Guanghui Deng
Guanghui Deng