- 1University of Leuven, University Psychiatric Center, Leuven, Belgium
- 2Faculty of Medicine, University of Leuven, Leuven, Belgium
- 3Department for Welfare, Public Health and Family, Flemish Government, Brussels, Belgium
- 4Health Psychology Research Group, University of Leuven, Leuven, Belgium
Excessive crying and sleep problems affect up to 30% of infants and often coexist. Although usually benign and self-limiting, persistent crying, and sleep problems exceeding 6 months of age need attention as they may impair the mental health of the infant and its family. The source and the impact of these persistent regulatory problems is often not restricted to the infant, but extends to the parents and the parent–infant relationship. Clinical practice needs interdisciplinary and multi-method interventions focusing beyond regulatory problems of the infant but also on parental self-regulation and parent's co-regulatory responses toward the infant. Treating clinicians may encounter limitations of home-visits, outpatient, and pediatric residential settings when working with families in distress. We describe an infant mental health day-clinic treatment, drawing attention to this viable future direction. It offers a therapeutic climate based on forming a triangle of co-regulation between clinician, parent and infant to first help the parent and the infant settle down. This stress reduction restores parent–infant connectedness and parental learning and reflecting capacity. Clinicians then use established therapeutic modalities to support parental self- and co-regulatory skills which is important for the development of self-regulation in the infant. Experience with this treatment program suggests that a day-clinic setting facilitates interdisciplinary and integrative multi-method intervention, infant and parental stress reduction and integration of parental self- and co-regulatory skills in daily family life, improving overall outcomes. This perspective warrants further investigation.
Introduction
An Illustrative Case Report
Laura's mother sought help desperately stating: “Nobody listens, but there is something wrong with Laura and I cannot take it anymore!”. Laura, 9 months old, had had severe sleep problems since birth. She didn't sleep during the day or more than 90 min at night. When waking at night, she repeatedly needed parental support for more than 30 min before falling asleep again. Since birth, Laura had been restless, often crying, and inconsolable unless she was carried around by her mother while being comforted.
Laura's parents previously consulted many pediatricians—none of them found an organic cause. The midwife advised Laura's parents to swaddle her and the nurses' education on normal sleep and crying patterns was perceived as invalidating to the parents' concerns. Cow milk free feeding formula, a hypoallergenic diet, omeprazole, and osteopathy were also unsuccessful solutions. A behavioral approach of installing positive bedtime routines and letting Laura cry with only brief parental reassurance was ineffective.
Over time, both parents were exhausted from the 24/7 care which Laura needed and Laura's well-being and functioning became significantly impaired. Laura did not laugh, smile, or play anymore, but whined all day. The parental stress and exhaustion over time triggered maternal postnatal depression and parent-relational problems. The non-understanding attitude of the parents' social network (e.g., “You spoil her”) caused a decline in their amount of social contact and support. Both parents had little-to-no pleasant experiences with Laura since birth. Laura was perceived as a burden to the whole family, leaving little room for love and warmth.
Persistent Sleep and Crying Problems
In the first 6 months of life, between 15 and 35% of parents report a problem with their infant's sleep and 14–29% with infant crying (1–6). These regulatory problems (RP) may occur separately, but often coexist. They are usually benign and self-limiting as transient features of normal development. However, in about 8% of infants RP persist after the age of 3 months (1, 4, 7) and have been associated with developmental and mental health problems across childhood, parental distress and poor general health, parental postnatal depression, and parent–child relationship problems with increased risk of abusive caregiver responses (1–4, 7–13). If no underlying organic cause or other infant mental health disorders are found, persistent RP exceeding the age of 6 months that impair the functioning of the infant, the family or both, are considered to be disorders which require treatment (3, 4, 7).
Current Treatment Approaches
Persistent RP are often managed in primary care with reassurance and education of the parents about normal sleep, eating and crying patterns and/or behavioral strategies (14, 15), and/or offered the same treatment as infant colic (a self-limited phenomenon of excessive crying during the first 2–3 months of life discussed in pediatric handbooks), including dietary alterations, probiotics prescriptions and pharmacological treatment (5, 6, 16).
When primary care doesn't resolve RP, parents often turn to complementary approaches such as swaddling, herbal remedies, acupuncture, manipulative therapies, and reflexology. All of these treatment methods have poor evidence (5, 6, 16).
These linear approaches have significant limits because only in a minority of the infants an underlying organic cause is found and evidence from diverse fields of investigation of RP demonstrates that it is a complex problem. There are multiple dynamically interacting and co-evolving factors with the compromised parent–infant relationship being a main moderator of infant problem behavior and outcome: prenatal and perinatal stress factors; infant temperament and neurodevelopmental problems with self-regulatory, dietary, and gastrointestinal factors; parent's perception and tolerance to their infant's RP; and parental psychosocial risks such as parental anxiety and depression, (transgenerational) trauma, family dysfunction, and socioeconomic risks (3–7, 16–20).
Infant mental health care addresses RP by focusing on parental co-regulation within the parent–infant relationship which is necessary for the development of self-regulation in the infant. Co-regulation is a parent–infant interaction in which parents are sensitive for the signals of their infant experiencing stress and/or overwhelming emotional arousal and respond by calming their infant with soothing voice tone, warm physical contact and meeting the infant's physical and emotional needs. Repeated cycles of emotional upset, followed by relaxation after the caretakers calming intervention, provide basis for a secure attachment relationship while setting a foundation for the infant's developing self-regulation. Over time, the infant internalizes the expectation of a soothing response through which they increasingly meet their own needs and manage their own behavioral and emotional responses. Thus, according to this Mutual Regulation Model by Tronick, infants learn self-regulation skills by experiencing co-regulation in caregiving (7, 20–41).
Clinical practice needs to focus beyond RP of the infant but also on parental self-regulation and parent's co-regulatory responses toward the infant. Many effective therapeutic modalities have been developed and researched such as parent infant psychotherapy, mentalization based therapy and video feedback on parent–infant interaction. They promote parental sensitivity, meaning-making and responding to the signals of the infant; parent–infant attunement; parents' self-reflection, and awareness of how their distress, traumatic memories, and/or their own upbringing may influence their parenting (7, 20, 23, 28, 29, 37, 39–42). Treatments focused on mother–infant dyads affected by postnatal depression show promising effects on infant regulation (39, 42).
The established interventions are implemented by clinicians trained in the specific treatment modality and offered in outpatient settings, including home visiting, dyadic and group based intervention. However, the treating clinician may be challenged in how to effectively and immediately help exhausted parents who may have difficulties to engage and to transfer insights and skills from therapy sessions to daily life, compromising overall outcomes. Meanwhile, exhausted parents resort to hospital emergency departments demanding a pediatric admission.
Approaching a Family in Distress
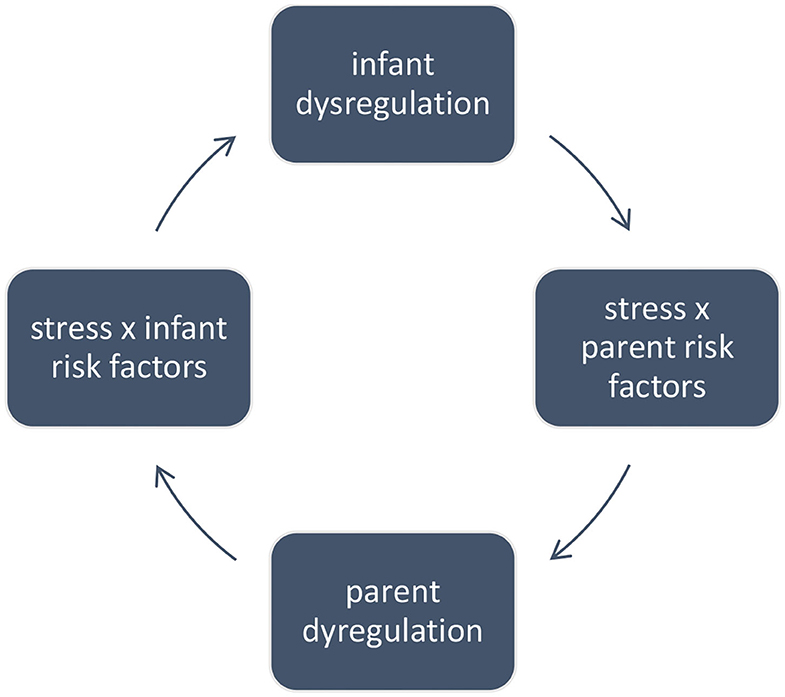
Infants with RP have both temperamental and physiological regulation difficulties and may be in a physical state that makes it difficult to be soothed by techniques which are usually effective (3, 7, 13, 17, 18, 20, 33, 36). This lack of responsiveness to usual care elicits acute stress reaction causing cumulative infant and parental fatigue. Parents with own vulnerabilities and lack of resources and social support are at risk to lose their own self-regulated state (7). Highly stressed and exhausted themselves, parents have no access to their own intuitive and co-regulatory skills in dealing with their infant's dysregulated behavior. As a result, a mutual parent–infant dysregulation spiraling mechanism (Figure 1) may start creating high levels of stress for both parties.
The “window of tolerance,” a term coined by Dan Siegel, is useful in motivating why stress reduction takes precedence in treatment. The window of tolerance describes the zone of arousal in which the autonomic nervous system is performing well and the brain can effectively process stimuli. In this zone, a person is likely to be able to reflect, think rationally, make decisions calmly and be socially engaged without feeling either overwhelmed or withdrawn. Extreme stress stimulates the autonomic nervous system, resulting in sympathetic hyper-arousal and parasympathetic hypo-arousal states accompanying animal defense survival responses such as fight, flight, and freeze. In either of these states, the prefrontal cortex region of the brain shuts down, and a person is said to be outside of the window of tolerance, functioning in survival mode (43). This explains why exhausted and dysregulated parents may not benefit from therapy, since the latter requires higher cognitive skills, and why parent–infant connectedness is more difficult to restore when families are in distress.
Parents need support in returning to their window of tolerance to increase their sense of calmness and connectedness as well as their learning and reflecting capacity. Then they will have the ability to deal with stress in more adaptive ways, think rationally and calmly connect with their infant and help regulate its behavioral and physiological state. An inpatient setting might facilitate providing a co-regulating space which fosters infant and parental regulated state. This might widen their window of tolerance, prevent dysregulation and at the same time amplify the existing arsenal of therapeutic approaches, making the clinician's efforts more effective.
Very little is documented or investigated on offering inpatient treatment. Wittberger describes a positive effect of an inpatient treatment with an overnight stay during 2–6 days on stress experienced by parents with excessively crying infant (44). While parents gain confidence and develop coping strategies, stress on the parents increases again upon hospital discharge.
Treatment in a Semi-residential Infant Mental Health Setting
We describe a day-clinic treatment at the University Psychiatric Center of KU Leuven-Department Child-Psychiatry embedded in the University Hospital. It was developed between 2016 and 2020 based on literature, clinical experience, and feedback of participating families and clinical experts.
This day-clinic serves weekly 12 families of infants 3–30 months of age (demograhic data Table 1) and employs 10 clinicians for 6 full-time equivalent. It offers a multi-disciplinary and integrative multi-method approach aiming to target parental distress and ability for co-regulation of infant distress (manifested as RP).
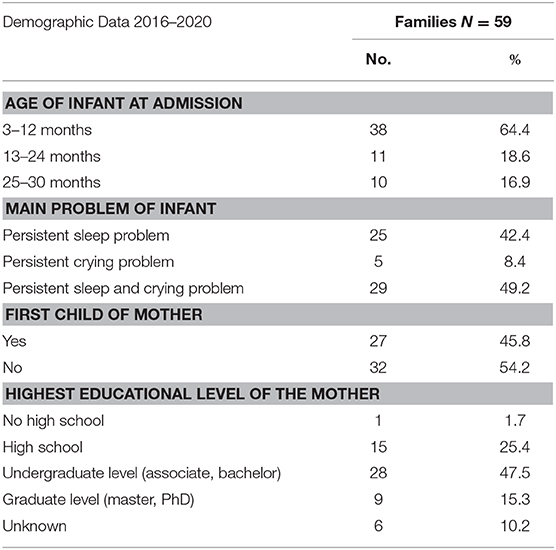
Table 1. Demographics of admitted families of infants with persistent sleep and/or crying problems between 2016 and 2020.
Parents apply for admission; no specific pre-assessment is needed. An interview of the parents with a simultaneous observation of the infant by a child-psychiatrist then follows to evaluate the indication for admission. Families who are caught in the mutual dysregulation spiral mechanism and for whom high levels of stress interfere with outpatient care, are admitted to the program. Families come 2 days every week, e.g. during day program for parent–infant dyads and evening program for parents. Full diagnostics and treatment is offered in collaboration with adult-psychiatry, pediatrics and Center for Infant Developmental Disorders, all located at the same hospital. Between 2016 and 2019 the admission duration varied from 3 to 37 weeks with an average of 19 weeks. The nationally funded leave system allows working parents to participate. Most of the costs are subsidized by the nationally funded mental health care system; the remaining cost for the families is 12 euros a week, if they don't have additional personal health insurance.
Phases in Treatment: Diagnostics, Treatment, Discharge, and Aftercare
The first 6 weeks are mainly focused on diagnostics to determine a treatment plan tailored to the family's needs; nevertheless families benefit from the beginning of the therapeutic approach of diagnostics and offered group treatment. A basic diagnostic consists of interviews of parents about complaints history, developmental history, and somatic health of the infant, family history (including the childhood experiences of the parents, couple relationship, parenting development, well-being of parents and siblings, social support and financial status of the family, genetic predisposition of diseases); interview of the concerning day care; multi-disciplinary observation of the infant, parent–infant relationship and parents and scoring of DC: 0–5 observation questionnaires (3). When necessary an additional (neuro)pediatric and developmental assessment (of cognitive, verbal, and non-verbal communication and motoric skills) of the infant and mental health assessment of the parent possibly suffering from psychopathology are carried out.
Child-psychiatrist discusses the diagnosis and treatment plan with the parents for mutuality and collaboration. Progress is evaluated and treatment is refined every 6–8 weeks together with the parents. Once the mutual parent–infant regulation is established (manifested as diminishing RP in the infant, ameliorated parent–child relationship and improved well-being of the family) a discharge is prepared. If necessary, aftercare in outpatient care is started during the admission; this ensures that parents engage. Six to eight weeks after discharge families are offered follow-up with the child-psychiatrist.
Day Treatment Program for Parent–Infant Dyad
We run two groups with infants 3–18 months of age and one group with infants 18–30 months of age, as the developmental needs are different in these age groups.
From 9 to 16 h a group of four parent–infant dyads and three clinicians meet weekly in a homey, apartment space with four bedrooms. The group moves through a fixed structure of therapeutic interventions embedded in daily life routines and with room for individual attuned support: music and dance therapy, Greenspan floortime, mindful parenting, baby massage, Sherborne developmental movement, mentalization based therapy, parent–infant psychotherapy, pre- and perinatal baby therapy alternate with eating, nursing, playing, resting, putting infants to sleep, having short conversations with peers or clinicians and going for a walk in nature (40, 45–54).
The core element is providing a co-regulating and “holding” therapeutic climate which fosters infant and parental regulated state by the installment of the “chain and triangle of co-regulation”.
Clinicians, who are themselves adequately self-regulated, form a triangle with the parent–infant dyad to first downregulate their stress and negative affect. They use their own (social) connectedness and create a safe supporting surrounding emphasizing their own physical and emotional availability and the person-to-person attunement to help the parent and the infant settle down. Releasing stress enables the parent and the infant to be more emotionally available to connect, communicate, and interact with each other.
Clinicians then form a chain with the downregulated parent–infant dyad to support parents co-regulate their infant. Clinicians model self- and co-regulatory skills and practice them together with parents. When their infant shows dysregulated behavior clinicians help parents to remain calm, be sensitive to their infant's cue and respond with new soothing behavior.
In this way, the chain and triangle of co-regulation open the door for infants and their families to shift and settle from the mutual dysregulation to mutual regulation. Concurrently, the parents benefit from peer-support during the process.
Evening Treatment Program for Parents
From 16 to 20.30 h one evening every week, the parents join (alone or as couple) a therapeutic program embedded in an informal meeting space, where they may have a peaceful meal and some leisure time with their spouse and peers. The therapeutic program offers three sessions: a semi-structured group intervention offering parental education and enhancing peer support, a downregulating group sessions to experience several ways of self-regulation (such as mindfulness, yoga, walking in nature, breathing exercises, etc.), and an individual therapeutic session tailored to the family's needs (offering parenting advice, parent–infant psychotherapy, video feedback, mentalization based therapy, trauma therapy, couple therapy, session promoting parental self-care and social support to enhance parental resilience, etc.). Parents appreciate the combination of these evenings with the day treatment program and being at home in between: discussing problems encountered during day treatment or at home with each other, peers and clinicians, and practicing new insights together with clinicians during day treatment and subsequently at home themselves, helps parents to come to sustainable changes.
Discussion
Our clinical experience suggests that a day-clinic setting facilitates an interdisciplinary and integrative multi-method intervention, infant and parental stress reduction and integration of parental self- and co-regulatory skills in daily family life, making the clinician's efforts more effective when treating distressed families of infants with severe and persistent RP. Compared to home visiting or outpatient care parents find it helpful shutting out the daily stress factors for one day, just to experience what it means to them and their baby. This contrast reveals the changes to be made at home and motivates parents. Parents appreciate having a full day, week after week, with many opportunities to observe and learn together with clinicians in many different ways. Due to collaboration with adult-psychiatry and pediatrics, organizing after-care during admission at the day clinic and follow-up after discharge, parents seem to experience less fragmentation and discontinuity in care. Peer support helps parents to normalize their experiences, counter feelings of guilt/failure, destigmatize and break through the social isolation. Observing and listening to other parents' experiences may shed light more spontaneously on issues parents had not thought of themselves or are not willing to confront. Parents learn from each other: “seniors” reassure “juniors” in their doubts and struggles and “juniors” show “seniors” how far they have progressed; live testimonials from discharged families offer hope.
This day-clinic treatment intends to be complimentary and collaborative with existing perinatal and infant mental health care.
Mother-baby units primarily focus on mothers' psychiatric disorders, while this treatment program primarily focuses on the infant RP and needs the parent to mediate the treatment for the infant and therefore also supports the parents. In case of severe parental psychopathology the parent is referred to adult psychiatric care, such as mother-baby units. If necessary, the infant may be treated parallel or subsequently at the day-clinic.
Compared to residential care, a part-time admission at day-clinic allows families to integrate what they have learned in their home environment and continue their normal life, e.g., work, social contacts, care for siblings, etc. This might facilitate transfer, lower the risk of relapse upon discharge and make the admission practically and financially feasible. But for infants living in unsafe home environment, other care is needed, such as facilities ensuring safety of the infant, mother-baby units, and family units.
The treatment we described is an intensive and costly approach, challenging parents work-life balance, challenging health services to form a bridge between services for adults' and infants' well-being and mental health, and challenging focus of subsidy by public health policy and modalities of payment by health insurance companies. The duration of the treatment is long, but it targets severe and persistent infant RP requiring intensive treatment, if only to manage the secondary impact. However, it is a challenge and important to investigate the difference between spontaneous recovery and the effect of the treatment.
Clearly, more research is needed to study the short and long-term effectiveness of the intervention we described.
Laura's Illustrative Case Report: Day-clinic Treatment With Co-regulation At the Core
Taking the first step toward co-regulating the distress in Laura's family, her mothers' concerns were validated and her father was involved from the beginning. In treatment, Laura's parents slowed down and together with peers and clinicians observed and experienced the distinct ways in which self-regulation affected themselves and their infant. They reduced their daily stress due to parental leave of Laura's father, household help, support of grandparents, and Laura's successful start at day care. These changes created more quality time for the parents to spend with Laura and alone as marital partners, fostering the family's resilience. Simultaneously, this improved their ability to benefit from the psychiatric treatment for the mother's depression, parenting advice with video feedback and couple therapy. Laura's parents were more calm and emotionally available, learned to interpret Laura's cues more quickly and were able to successfully soothe her. They shared more pleasurable interaction with their daughter. Gradually, Laura's crying and whining diminished and she appeared to be happier and more relaxed. Laura began sleeping during the day as the parents improved their perception of self-efficacy in caring for Laura. Now under these circumstances previously failed behavioral strategies such as gradual extinction and positive bedtime routines effectively helped Laura to sleep for longer periods at night.
During these 5 months of treatment Laura became a gift for the wellbeing of her whole family instead of a burden, when her parents realized that helping Laura started by helping themselves.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author Contributions
BS, drafting the manuscript. BV and MD, critical revision of the article. BS, BV, and MD, final approval of the version to be published. All authors contributed to the article and approved the submitted version.
Funding
We would like to thank Giselle Garnett for editing the English manuscript and formatting the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all parents and their children who followed the day-clinic treatment for sharing their experiences and all clinicians for their valuable expertise and involvement.
References
1. Schmid G, Schreier A, Meyer R, Wolke D. A prospective study on the persistence of infant crying, sleeping and feeding problems and preschool behaviour. Acta Paediatrica. (2010) 99:286–90. doi: 10.1111/j.1651-2227.2009.01572.x
2. Cook F, Bayer J, Le H, Mensah F, Cann W, Hiscock H. Baby Business: a randomised controlled trial of a universal parenting program that aims to prevent early infant sleep and cry problems and associated parental depression. BMC Pediatrics. (2012) 12:13. doi: 10.1186/1471-2431-12-13
3. Zero to Three. DC:0-5TM: Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood. Washington, DC: Zero to Three Press (2016). p. 90–112.
4. Olsen AL, Ammitzbøll J, Olsen EM, Skovgaard AM. Problems of feeding, sleeping and excessive crying in infancy: a general population study. Arch Dis Childhood. (2019) 104:1034–41. doi: 10.1136/archdischild-2019-316851
5. Becerra-Granados LM, Bejarano-Roncancio JJ, Bages-Mesa MC. Interdisciplinary management of infantile colic. Rev Fac Med. (2017) 65:507–12. doi: 10.15446/revfacmed.v65n3.55920
6. Sarasu JM, Narang M, Shah D. Infantile colic: an update. Indian Pediatr. (2018) 55:979–87. doi: 10.1007/s13312-018-1423-0
7. Cierpka M. Regulatory Disorders in Infants: Assessment, Diagnosis, and Treatment. Springer Int Publishing (2016).
8. Hemmi MH, Wolke D, Schneider S. Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioral outcomes in childhood: a meta-analysis. Arch Dis Childhood. (2011) 96:622–9. doi: 10.1136/adc.2010.191312
9. Bayer JK, Hiscock H, Hampton A, Wake M. Sleep problems in young infants and maternal mental and physical health. J Paediatr Child Health. (2007) 43:66–73. doi: 10.1111/j.1440-1754.2007.01005.x
10. Wake M, Morton-Allen E, Poulakis Z, Hiscock H, Gallagher S, Oberklaid F. Prevalence, stability, and outcomes of cry-fuss and sleep problems in the first 2 years of life: prospective community-based study. Pediatrics. (2006) 117:836–42. doi: 10.1542/peds.2005-0775
11. Martin J, Hiscock H, Hardy P, Davey B, Wake M. Adverse associations of infant and child sleep problems and parent health: an Australian population study. Pediatrics. (2007) 119:947–55. doi: 10.1542/peds.2006-2569
12. Skovgaard AM. Mental health problems and psychopathology in infancy and early childhood. An epidemiological study. Danish Med Bull. (2010) 57:B4193.
13. Postert C, Averbeck-Holocher M, Achtergarde S, Müller J, Furniss T. Regulatory disorders in early childhood: correlates in child behavior, parent-child relationship, and parental mental health. Infant Ment Health J. (2012) 33:173–86. doi: 10.1002/imhj.20338
14. Ramchandani P, Webb V, Stores G. A systematic review of treatment of settling problems and night waking in young children. Western J Med. (2000) 173:33–8. doi: 10.1136/ewjm.173.1.33
15. Meltzer L, Mindell J. Systematic review and meta-analysis of behavioral interventions for pediatric insomnia. J Pediatr Psychol. (2014) 39:932–48. doi: 10.1093/jpepsy/jsu041
16. Zeevenhooven J, Browne PD, L'Hoir MP, de Weerth C, Benninga MA. Infant colic: mechanisms and management. Nat Rev Gastroenterol Hepatol. (2018) 15:479–95. doi: 10.1038/s41575-018-0008-7
17. Sidor A, Fischer C, Cierpka, M. The link between infant regulatory problems, temperament traits, maternal depressive symptoms and children's psychopathological symptoms at age three: a longitudinal study in a German at-risk sample. Child Adolesc Psychiatry mental Health. (2017) 11:10. doi: 10.1186/s13034-017-0148-5
18. Martini J, Petzoldt J, Knappe S, Garthus-Niegel S, Asselmann E, Wittchen, et al. Infant, maternal, and familial predictors and correlates of regulatory problems in early infancy: the differential role of infant temperament and maternal anxiety and depression. Early Hum Dev. (2017) 115:23–31. doi: 10.1016/j.earlhumdev.2017.08.005
19. Papousek M. Resilience, strengths, and regulatory capacities: hidden resources in developmental disorders of infant mental health. Infant Ment Health J. (2011) 32:29–46. doi: 10.1002/imhj.20282
20. Gold CM. The Developmental Science of Early Childhood: Clinical Applications of Infant Mental Health Concepts from Infancy Through Adolescence. New York, NY: W.W. Norton (2017).
21. Tronick E, Beeghly M. Infants' meaning-making and the development of mental health problems. Am Psychol. (2011) 66:107–19. doi: 10.1037/a0021631
22. Gianino A, Tronick E. The mutual regulation model: the infant's self and interactive regulation and coping and defensive capacities. In: Field TM, McCabe PM, Schneiderman N, editors. Stress and Coping Across Development. Lawrence Erlbaum Associates, Inc. (1998). p. 47–68.
23. Fonagy P. Mutual regulation, mentalization, and therapeutic action: a reflection on the contributions of Ed Tronick to developmental and psychotherapeutic thinking. Psychoanal Inquiry. (2015) 35:355–69. doi: 10.1080/07351690.2015.1022481
24. Morris AS, Williamson AC. Building Early Social and Emotional Relationships With Infants and Toddlers: Integrating Research and Practice. Springer Int Publishing (2018).
25. Gordon M, Gohil J, Banks SSC. Parent training programs for managing infantile colic (review). Cochrane Database Syst Rev. (2019) 12:CD012459. doi: 10.1002/14651858.CD012459.pub2
26. Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of Attachment: Assessed in the Strange Situation and at Home. Hillsdale, NJ: Erlbaum (1978).
27. Berger A, Kofman O, Livneh U, Henik A. Multidisciplinary perspective on attention and the development of self-regulation. Prog Neurobiol. (2007) 82:256–86. doi: 10.1016/j.pneurobio.2007.06.004
28. Calkins SD, Hill A. Caregiver influences on emerging emotion regulation. In: Gross JJ, editor. Handbook of Emotion Regulation. New York, NY: Guilford Press (2007). p. 229–48.
29. Cole PM, Teti LO, Zahn-Waxler C. Mutual emotion regulation and the stability of conduct problems between preschool and early school age. Dev Psychopathol. (2003) 15:1–18. doi: 10.1017/S0954579403000014
30. Sroufe LA, Egeland B, Carlson EA, Collins WA. The Development of the Person: The Minnesota Study of Risk and Adaptation from Birth to Adulthood. New York, NY: Guilford Press (2005).
32. Shipman KL, Zeman J. Socialization of children's emotion regulation in mother-child dyads: A developmental psychopathology perspective. Development and Psychopathology. (2001) 13:317–36. doi: 10.1017/S0954579401002073
33. Dale LP, O'Hara EA, Keen J, Porges SW. Infant regulatory disorders: temperamental, physiological, and behavioral features. J Dev Behav Pediatr. (2011) 32:216–24. doi: 10.1097/DBP.0b013e3181e32c4f
34. Kopp CB. Regulation of distress and negative emotions: a developmental view. Dev Psychol. (1989) 25:343–54. doi: 10.1037/0012-1649.25.3.343
35. Field T. The effects of mother's physical and emotional unavailability on emotion regulation. Monogr Soc Res Child Dev. (1994) 59:208–27. doi: 10.2307/1166147
36. Feldman R, Greenbaum CW, Yirmiya, N. Mother-infant affect synchrony as an antecedent to the emergence of self-control. Dev Psychol. (1999) 35, 223–231. doi: 10.1037/0012-1649.35.1.223
37. Keefe MR, Kajrlsen KA, Lobo ML, Kotzer AM, Dudley WN. Reducing parenting stress in families with irritable infants. Nurs Res. (2006) 55:198–205. doi: 10.1097/00006199-200605000-00006
38. Paousek M, Schieche M, Wurmser H. Regulationsstorungen der Fruhen Kindheid. Bern: Verlag Hans Huber (2004).
39. Gleason MM, Goldson E, Yogman MW. Addressing early childhood emotional and behavioral problems. Pediatrics. (2016) 138:e20163025. doi: 10.1542/peds.2016-3025
40. Barlow J, Bennett C, Midgley N, Larkin SK, Wei Y. Parent-infant psychotherapy: a systematic review of the evidence for improving parental and infant mental health. J Reprod Infant Psychol. (2016) 34:464–82. doi: 10.1080/02646838.2016.1222357
41. Provenzi L, Scotto di Minico G, Giusti L, Guida E, Müller M. Disentangling the dyadic dance: theoretical, methodological and outcomes systematic review of mother-infant dyadic processes. Front Psychol. (2018) 9:348. doi: 10.3389/fpsyg.2018.00348
42. Clark R, Tluczek A, Brown R. A mother-infant therapy group model for postpartum depression. Infant Ment Health J. (2008) 29:514–36. doi: 10.1002/imhj.20189
44. Wittberger L, Albermann K, Pehlke-Milde J, Koppitz, A. The effect of inpatient treatment on the stress experienced by parents with an excessively crying infant / Die Auswirkungen eines Spitalaufenthaltes auf die Belastung von Eltern mit einem exzessiv schreienden Kind. Int J Health Professions. (2017) 4:14–24. doi: 10.1515/ijhp-2017-0003
46. Doonan F, Bräuninger I. Making space for the both of us: how dance movement therapy enhances mother-infant attachment and experience. Body Mov Dance Psychotherapy. (2015) 10:227–42. doi: 10.1080/17432979.2015.1063547
47. Boshoff K, Bowen H, Paton H, Cameron-Smith S, Graetz S, Young A, et al. Child development outcomes of DIR/Floortime TM-based programs: a systematic review. Can J Occup Therapy. (2020) 87:153–64. doi: 10.1177/0008417419899224
48. Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH. Pairing attachment theory and social learning theory in video-feedback intervention to promote positive parenting. Curr Opin Psychol. (2015) 15:189–94. doi: 10.1016/j.copsyc.2017.03.012
49. Potharst ES, Aktar E, Rexwinkel M, Rigterink M, Bögels SM. Mindful with your baby: feasibility, acceptability, and effects of a mindful parenting group training for mothers and their babies in a mental health context. Mindfulness. (2017) 8:1236–50. doi: 10.1007/s12671-017-0699-9
50. Diane Reynolds Infant Mental Health Services Coordinator. Mindful Parenting: a group approach to enhancing reflective capacity in parents and infants. J Child Psychotherapy. (2003) 29:357–74. doi: 10.1080/00754170310001625413
51. Laurent HK, Duncan LG, Lightcap A, Khan F. Mindful parenting predicts mothers' and infants' hypothalamic-pituitary-adrenal activity during a dyadic stressor. Dev Psychol. (2017) 53:417–24. doi: 10.1037/dev0000258
52. Weston C. Becoming bonded through Developmental Movement Play: review of a parent and child movement group incorporating the theory, practice and philosophy of Sherborne Developmental Movement. Body Mov Dance Psychotherapy. (2012) 7:245–62. doi: 10.1080/17432979.2012.669795
53. Byrne G, Murphy S, Connon G. Mentalization-based treatments with children and families: a systematic review of the literature. Clin Child Psychol Psychiatry. (2020) 25:1022–48. doi: 10.1177/1359104520920689
Keywords: co-regulation, excessive crying, sleep problems, parent–child relation, infant, day-clinic treatment, window of tolerance, infant regulatory problems
Citation: Singh BSK, Danckaerts M and Van den Bergh BRH (2021) Helping Families of Infants With Persistent Crying and Sleep Problems in a Day-Clinic. Front. Psychiatry 12:591389. doi: 10.3389/fpsyt.2021.591389
Received: 04 August 2020; Accepted: 28 January 2021;
Published: 26 February 2021.
Edited by:
Susan Garthus-Niegel, Medical School Hamburg, GermanyReviewed by:
Ayten Bilgin, University of Kent, United KingdomMaria Muzik, University of Michigan, United States
Copyright © 2021 Singh, Danckaerts and Van den Bergh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Binu S. K. Singh, binu.singh@upckuleuven.be; orcid.org/0000-0002-1560-6545
 Binu S. K. Singh
Binu S. K. Singh Marina Danckaerts1,2
Marina Danckaerts1,2 Bea R. H. Van den Bergh
Bea R. H. Van den Bergh