Editorial: Vein of galen malformation: a scientific and clinical journey targeting the best outcome
- 1Neonatal and Pediatric Intensive Care Unit, Acceptance and Emergency Department, IRCCS Istituto Giannina Gaslini, Genoa, Italy
- 2Neurointerventional Radiology, Boston Children’s Hospital, Boston, MA, United States
- 3Interventional Radiology, University of Toronto and the Hospital for Sick Children, Toronto, ON, Canada
- 4Department of Radiology, Great Ormond Street Hospital, London, United Kingdom
Editorial on the Research Topic
Vein of galen malformation: a scientific and clinical journey targeting the best outcome
Vein of Galen aneurysmal malformation (VGAM) represents nearly 30% of all pediatric cerebrovascular malformations, yet, as a rare condition, presents several knowledge gaps that should be addressed. Over the past three decades, advances in diagnostic and therapeutic strategies have resulted in markedly improved survival and prognosis, but mortality and adverse neurological outcomes are unfortunately still not rare.
When we initially proposed the specific topics for this editorial assignment, we included all aspects of research that could structure a scientific and clinical journey focusing on the best outcome (Table 1). The contributions to this project highlight the extraordinary interest that this condition arouses in the multidisciplinary group of specialists involved in the care of children with VGAM, and through the submitted manuscripts several aspects have been studied and discussed from diverse perspectives.
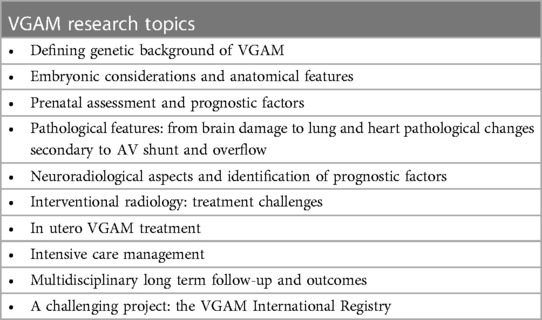
Table 1. Vein of galen malformation: a scientific and clinical journey targeting the best outcome. Research topics.
The genetic background and the molecular pathophysiology of cerebrovascular malformations represent a key topic in research and several genes encoding proteins involved in vascular development have been identified in association with VGAM (1). Tas et al. in the retrospective review “Arteriovenous Cerebral High Flow Shunts in Children: From Genotype to Phenotype” observed that Ephrin type-B receptor 4 (EPHB4) variants seemed to be specific to VGAM, RASp21 Protein Activator 1 (RASA1) variants were associated with either pial arteriovenous fistulas or with VGAM, and Hereditary Hemorrhagic Telangiectasia (HHT) gene variants seemed specific to pial arteriovenous fistulas not draining into the vein of Galen. As stated by the authors, misclassifications of AV fistulas or malformations that drain into a dilated vein of Galen as true VGAMs are frequent and may lead to catastrophic consequences if deep venous drainage is not well defined. This is a key point in treatment strategies and in the prevention of severe hemorrhagic or ischemic procedural complications, especially at the earliest ages, when it is difficult to definitively establish a clear diagnosis and classification.
Since the late 1980s, endovascular embolization has become the standard of care in the management of VGAM. Modern techniques and materials allow staged occlusion of the arterial feeders using advanced microcatheters and liquid embolic systems and/or coils with the goal of complete treatment of the malformation. Yet, the high and turbulent flow characterizing the AV shunts in VGAM makes the procedure very challenging for the risk of glue migration and severe embolic complications (2). To increase the safety and efficacy of endovascular treatment, several adjunctive flow-control techniques have been developed to improve the accuracy of the treatment and prevent complications. Baranoski et al. in “Rapid ventricular overdrive pacing and other advanced flow-control techniques for the endovascular embolization of vein of Galen malformations” presented detailed flow-control techniques, including regionally targeted strategies (transvenous embolization and balloon-assisted transarterial embolization) and global flow-control methods (pharmacologic cardiac arrest and rapid ventricular overdrive pacing). The technical challenges and significant advancements in this field are presented in this review, highlighting the key role of the neurointerventional radiologist in the multidisciplinary management of this complex condition.
The identification of factors influencing neurological outcome is one of the main topics in VGAM research, with the aim of preventing acute and chronic neurological damage. Several aspects have been studied in cohort studies and meta-analyses (3–8), but it is very difficult to define clear-cut modifiable risk factors due to the rarity and extreme complexity of the disease. This problem is well demonstrated in the manuscript “Outcomes of endovascular embolization for Vein of Galen malformations: An individual participant data meta-analysis”. The goal of this study by Savage et al. was to identify risk factors associated with all-cause mortality and clinical outcome after endovascular embolization. Overall all-cause mortality was 16%, and overall good clinical outcome was achieved in 68% of participants. First embolization as a neonate, incomplete embolization, and heart failure at presentation were associated with the study outcomes. Despite the methodology (meta-analysis), and inclusion of older studies, this manuscript provides important data regarding risk factors and burden of disease in terms of mortality and morbidity.
Risk stratification, patient selection and time of intervention have a paramount role in the therapeutic planning. The case report by Saliou et al. “Pseudo-feeders as a red flag for impending or ongoing severe brain damage in vein of Galen aneurysmal malformation” is very illustrative. The authors highlight relevant arguments: the rapid onset and progression of cerebral damage in an infant with previously normal neuroimaging, the role of a specific factor in identifying at risk patients, and the importance of the appropriate time window for treatment. In particular, Saliou et al. focused on the role of arterial pseudofeeders as red flag of severe vascular steal phenomena through the shunt, and poor cerebral haemodynamic status.
A model of patient evaluation and therapeutic approach is presented in “Vein of Galen aneurysmal malformation in newborns: a retrospective study to describe a paradigm of treatment and identify risk factors of adverse outcome in a referral center,” by Buratti et al. In this single-center retrospective cohort study, the association of fetal and neonatal cardiologic and neuroradiologic parameters with severe high output heart failure (HOHF), endovascular complications and death in 40 consecutive newborns was assessed. Despite a high percentage of newborns developed severe haemodynamic compromise, none of the patients died due to HOHF and multiorgan failure. Specialized intensive care management focused on the complexity of VGAM pathophysiology and early endovascular treatment allowed reduction in mortality and optimization of clinical outcomes. Another relevant argument highlighted in this study is that severe congenital brain damage was the only indication for palliation, excluding critical hemodynamic compromise as a ground for palliation.
Campi et al., in “Neurodevelopmental and genetic findings in neonates with intracranial arteriovenous shunts: A case series” observed the importance of multimodal neurophysiological studies during the neonatal period. This retrospective observational study highlighted, despite inhomogeneities in the neurophysiological data, the value of early neurophysiological monitoring with aEEG and video EEG in the assessment of neurological status and in the early detection of complications secondary to the disease or to the endovascular treatment. Moreover, specific neurophysiological tests, in particular somatosensory evoked potentials, have been identified as promising potential markers of early and long term neurological impairment.
Conclusions
It is well known that research on rare diseases is well-grounded and accurate if based on large scale data, international collaboration, and multidisciplinary debate. This editorial project launched by Frontiers two years ago created the opportunity for the international community to join in a shared research effort that went far beyond the initial aims. The VGAM network, developed thanks to the Frontiers Research Topic contributors, realized two relevant objectives: the first international meeting on VGAM in newborns and children held in Genoa, in May 2023, and the ongoing development of an international clinical research registry. We expect that these achievements, and new diagnostic and therapeutic options, such as endovascular liquid biopsy to study somatic mutations (9), ultrasound-guided fetal embolization (10), and gamma knife treatment in children (11) may define new perspectives and frame further promises for patients and families.
Author contributions
SB: Conceptualization, Formal analysis, Validation, Writing – original draft. DO: Writing – review & editing. PM: Writing – review & editing. FR: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Duran D, Karschnia P, Gaillard JR, Karimy JK, Youngblood MW, DiLuna ML, et al. Human genetics and molecular mechanisms of vein of galen malformation. J Neurosurg Pediatr. (2018) 21(4):367–74. doi: 10.3171/2017.9.PEDS17365
2. Bhatia K, Mendes Pereira V, Krings T, Ter Brugge K, Kortman H, Dirks P, et al. Factors contributing to major neurological complications from vein of galen malformation embolization. JAMA Neurol. (2020) 77(8):992–9. doi: 10.1001/jamaneurol.2020.0825
3. Brinjikji W, Krings T, Murad MH, Rouchaud A, Meila D. Endovascular treatment of vein of galen malformations: a systematic review and meta- analysis. Am J Neuroradiol. (2017) 38(12):2308–14. doi: 10.3174/ajnr.A5403
4. Yan J, Wen J, Gopaul R, Zhang C-Y, Xiao S-W. Outcome and complications of endovascular embolization for vein of galen malformations: a systematic review and meta-analysis. J Neurosurg. (2015) 123(4):872–90. doi: 10.3171/2014.12.JNS141249
5. Giorgi L, Durand P, Morin L, Miatello J, Merchaoui Z, Lambert V, et al. Management and outcomes of neonatal arteriovenous brain malformations with cardiac failure: a 17 years’ experience in a tertiary referral center. J Pediatr. (2020) 218:85–91.e2. doi: 10.1016/j.jpeds.2019.10.090
6. Lecce F, Robertson F, Rennie A, Heuchan AM, Lister P, Bhate S, et al. Cross- sectional study of a United Kingdom cohort of neonatal vein of galen malformation. Ann Neurol. (2018) 84(4):547–55. doi: 10.1002/ana.25316
7. Jhaveri S, Berenstein A, Srivastava S, Shigematsu T, Geiger MK. High output cardiovascular physiology and outcomes in fetal diagnosis of vein of galen malformation. Pediatr Cardiol. (2021) 42:1416–24. doi: 10.1007/s00246-021-02627-9
8. Malarbi S, Gunn-Charlton JK, Burnett AC, Prentice TM, Williams A, Mitchell P, et al. Outcome of vein of galen malformation presenting in the neonatal period. Arch Dis Child. (2019) 104(11):1064–9. doi: 10.1136/archdischild-2018-316495
9. Bhatia K, Lord D, McCowage G, Sylvester D, Karpelowsky J, Olsson G, et al. LB-002 liquid biopsy identifies somatic KRAS mutations in paediatric cranio-spinal arterio-venous malformations: preliminary results. J Neurointerv Surg. (2023) 15:A243. doi: 10.1136/jnis-2023-SNIS.376
10. See AP, Wilkins-Haug LE, Benson CB, Tworetzky W, Orbach DB. Percutaneous transuterine fetal cerebral embolisation to treat vein of galen malformations at risk of urgent neonatal decompensation: study protocol for a clinical trial of safety and feasibility. BMJ Open. (2022) 12(5):e058147. doi: 10.1136/bmjopen-2021-058147
Keywords: VGAM, children, research, outcome, treatment
Citation: Buratti S, Orbach DB, Muthusami P and Robertson F (2023) Editorial: Vein of galen malformation: a scientific and clinical journey targeting the best outcome. Front. Pediatr. 11:1323889. doi: 10.3389/fped.2023.1323889
Received: 18 October 2023; Accepted: 23 October 2023;
Published: 3 November 2023.
Edited and Reviewed by: Eugene Dempsey, University College Cork, Ireland
© 2023 Buratti, Orbach, Muthusami and Robertson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Silvia Buratti buratti.silvia@gmail.com
 Silvia Buratti
Silvia Buratti Darren B. Orbach
Darren B. Orbach Prakash Muthusami
Prakash Muthusami Fergus Robertson
Fergus Robertson