The Effective Management of Fever in Pediatrics and Insights on Remote Management: Experts' Consensus Using a Delphi Approach
- 1Pediatric Infectious Disease Unit, Anna Meyer Children's University Hospital, Florence, Italy
- 2Department of Pediatrics, Azienda Ospedaliera San Giuseppe Moscati, Avellino, Italy
- 3Department of Clinical and Experimental Sciences, Pediatrics Clinic, University of Brescia and ASST-Spedali Civili, Brescia, Italy
- 4Pediatric Primary Care, National Pediatric Health Care System, Lastra a Signa, Italy
- 5Pediatric Primary Care, National Pediatric Health Care System, Novara, Italy
- 6Pediatric Primary Care, National Pediatric Health Care System, Margherita di Savoia, Barletta-Andria-Trani, Italy
- 7Pediatric Primary Care, National Pediatric Health Care System, Chioggia, Italy
- 8Department of Translational Medical Science, Section of Pediatrics, University of Naples Federico II, Naples, Italy
Background: Even after the publication of the 2017 update of Italian guidelines on treatment of fever in pediatrics, some fundamental questions are still open and new ones emerged during the COVID-19 pandemic.
Objective: To assess the level of consensus among Italian pediatricians on different topics related to treatment of fever in children by using the Delphi technique.
Methods: A Delphi study was undertaken between June and September 2021, when two questionnaires were consecutively sent to a panel of experts to be answered anonymously. An invitation to participate was sent to 500 pediatricians distributed over the whole national territory and 80 (16%) of them accepted to participate on a voluntary basis. The questionnaires were structured into three specific topics: “therapeutic appropriateness and management of the febrile child,” “management of the febrile child in the presence of other diseases,” and “future perspectives in remote management.” Each topic had six statements.
Results: A first-round questionnaire was sent to 80 accepting pediatricians from different Italian regions. Of the 72 respondents (23% working in hospitals and 72% outside), 33% were from northern, 12% central, and 55% southern Italy or islands. A second-round questionnaire was sent to the same 80 pediatricians and 69 of them responded, without significant differences for workplaces or geographical distribution as compared with the first questionnaire. Overall, 75 participants answered at least one of the two questionnaires. All the statements on the topics of “therapeutic appropriateness and management of the febrile child” and “future perspectives in remote management” reached the predefined cut off for consensus (75% or more). Only one statement on “management of the febrile child in the presence of other diseases” did not achieve the consensus even after the second round.
Conclusions: Italian pediatricians agree on several aspects of treatment of febrile children and their expert opinions could support everyday decision process complementary to recommendations by regulatory agencies and guidelines.
Introduction
In 2017, the Italian Society of Pediatrics published an update of the guidelines on the management of fever in children (1). However, differences may have persisted among regions and between settings, namely, hospital vs. community, and may have further increased with the outbreak of SARS-CoV-2 virus pandemic (COVID-19), due to limited resource availability and social containment measures. Moreover, the pandemic has stressed the difficulties for local services in securing the continuity of care to patients suffering from rare or common diseases, difficulties that a remote approach could have reduced. Therefore, the COVID-19 outbreak has raised questions that weaken the applicability of the available guidelines to everyday clinical practice.
In making clinical decisions where no gold standard exists or when new situations, like COVID-19, emerge, formal consensus techniques among peers represent a recognized method of scientific advancement based on clinical experience and an authoritative opinion to support therapeutic decisions in clinical practice (2). One of the most validated formal methods for consensus processes in various fields is the Delphi method (3). It consists of an iterative process in which experts are consulted individually with a series of questionnaires and receive anonymous group feedback from authoritative experts between iterations.
In this study, we used a modified Delphi process to assess the level of consensus among pediatricians from different Italian regions and workplaces on the management of pediatric fever, in terms of both therapeutic appropriateness and management in the presence of other diseases, including COVID-19 infection. The possible role of remote management of the patient was also evaluated, with reference to both the current situation and other similar possible future situations. The ultimate output was to propose statements made by a board of pediatric experts about a standard treatment to be applied in daily practice for the febrile child, which could also be feasible with a remote approach. The study does not aim to provide guidelines.
Methods
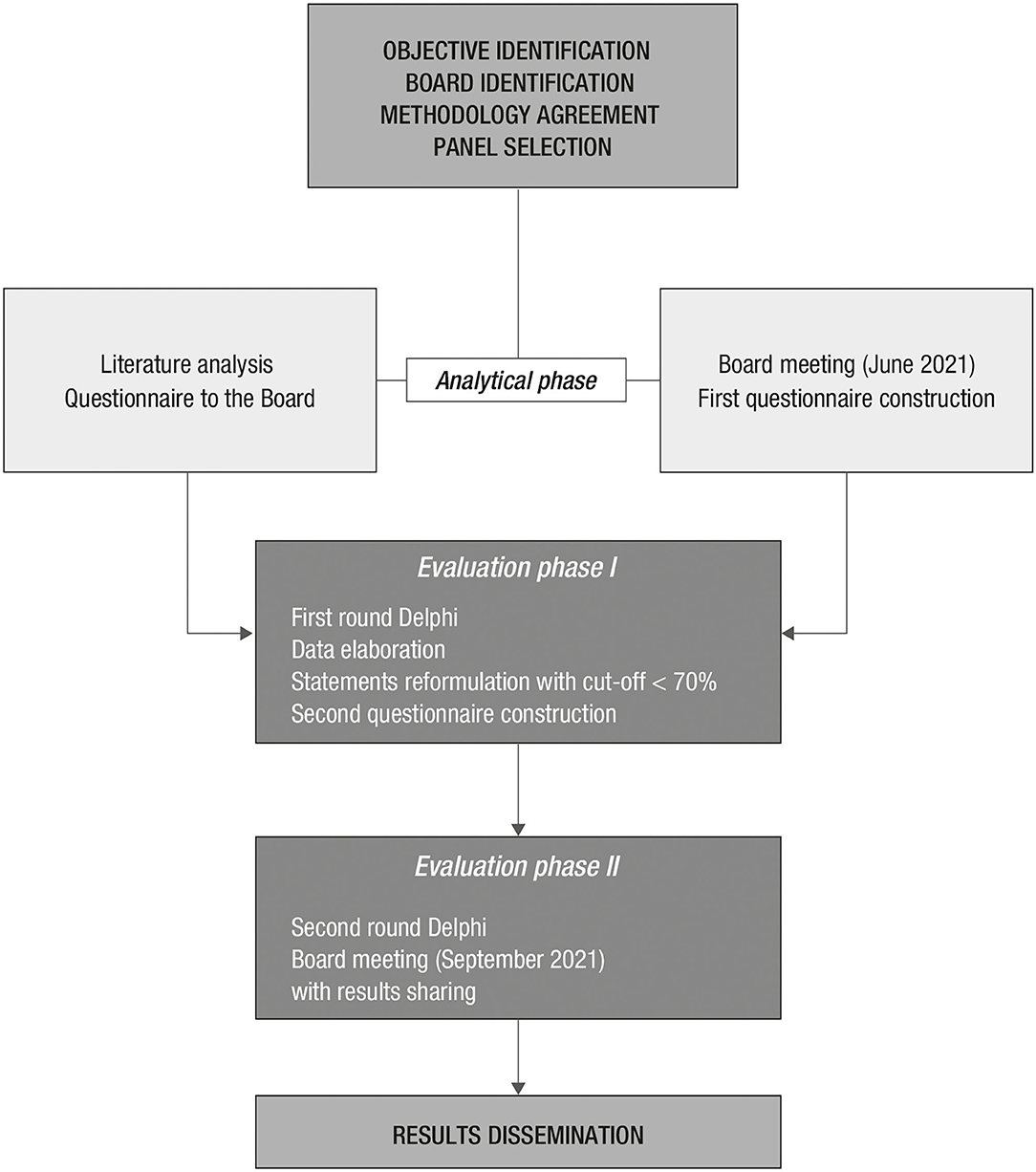
The study was conducted between June and September 2021 (Figure 1) among Italian pediatricians with relevant clinical experience in the treatment of the febrile patient, operating in either hospital or community settings (see Appendix).
Exploratory Phase
A board of pediatricians working in academic institutions or hospitals or community settings with ≥10 years of clinical experience, active participation in boards and committees of the Italian Society of Pediatrics and other scientific societies, and at least 10 international publications on the topic of fever management was identified (the authors of the current study).
A panel of board-certified pediatricians was selected from a database of Menthalia S.r.l., a provider for scientific and medical communication. They were required to have the following qualifications: clinical experience in the pediatric field for 5 years at least, working in hospitals or primary care settings over the Italian territory, at least 5 scientific publications on fever treatment in the last 5 years, and participation in national or international meetings and in the activities of scientific societies. A total of 500 pediatricians distributed over the country were invited by Menthalia and 80 (16%) accepted to participate on a voluntary basis, which was considered as acceptable.
Analytical Phase
Guidelines and consensus documents on pediatric fever management were initially collected to assess the state of the art at the national level. A literature search was performed in May 2021 on PubMed by using the PICO criteria:
• Population: children (age: 0–18 years).
• Intervention: medical management.
• Comparators: paracetamol vs. ibuprofen.
• Outcomes: subjective and objective.
• Areas: outpatient and inpatient.
The search included randomized clinical trials, observational studies (prospective or retrospective cohorts, case-control or cross-sectional studies), systematic reviews and meta-analyses, and guidelines published between 2015 and 2021. Publications in languages other than English or Italian, case reports, letters, editorials, and gray literature were not included.
The Boolean terms used for the search were:
- children AND fever management NOT cancer (344 results)
- children AND fever management AND therapeutic appropriateness (27 results)
- children AND fever management AND paracetamol (22 results)
- fever management AND pediatric patients AND paracetamol NOT cancer (2 results)
- children AND fever management AND AOM (acute otitis media) (6 results)
- children AND fever management AND asthma (7 results)
- children AND fever management AND kidney disease (5 results)
- children AND fever management AND sinusitis (2 results)
- children AND fever management AND COVID-19 (29 results)
- children AND fever management AND telemedicine (3 results).
After a preliminary analysis of the titles and abstracts from all search results, the appropriateness of the contents with respect to the objective of the study, the geographical area of reference, and the treated diseases were evaluated. Duplicates, papers on critically ill children, or fever management in developing countries were discarded.
Finally, 29 papers relevant to the objective of the study were retained, to which three relevant documents related to telemedicine were added, and divided into the following four areas of interest:
1. Therapeutic appropriateness and management of the febrile child.
2. Management of the febrile child in the presence of other diseases.
3. Management of fever and COVID-19.
4. Future perspectives: remote management.
Delphi Process
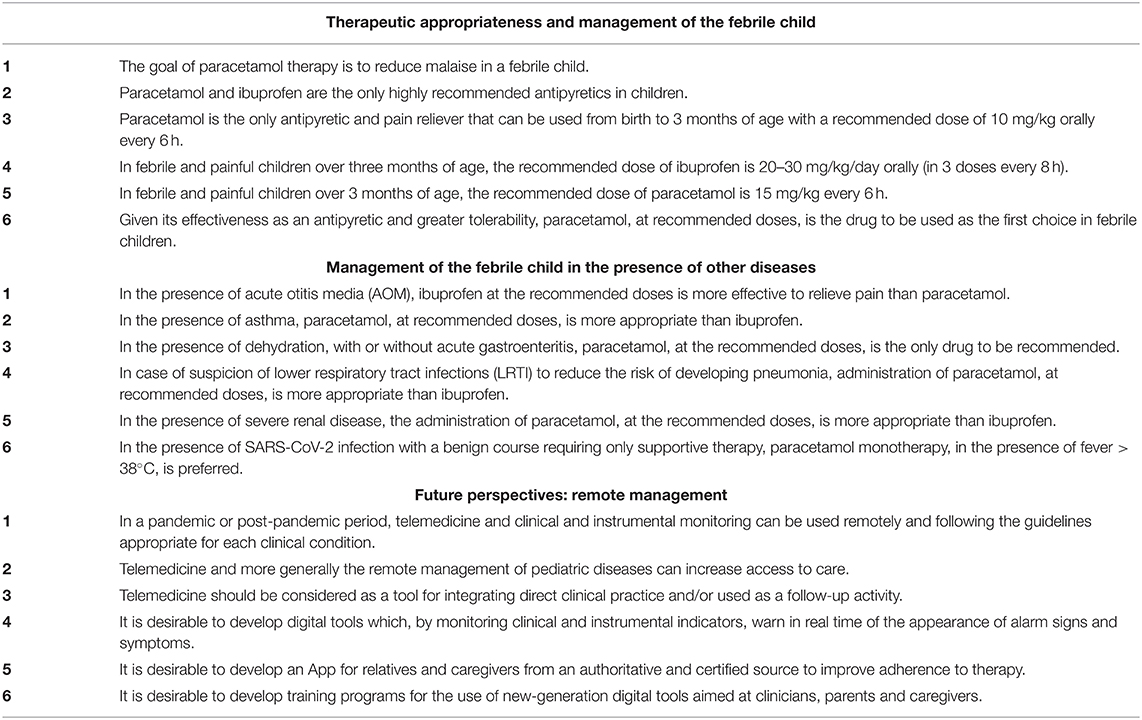
Based on the literature search (1, 4–18), a questionnaire (Table 1) was prepared by one of the board members (Antonio Vitale) and submitted to the board, in a non-anonymous manner, in order to identify areas of agreement and acquire further information to improve the survey through open questions. The responses of the board members to each statement were analyzed by a descriptive statistic performed by Menthalia and discussed during two web meeting brainstorms, moderated by a facilitator from Menthalia. The discussion led to reformulating some statements and deleting others. The section on COVID-19 was omitted, and only one statement on it was included in the section on febrile child with other diseases.
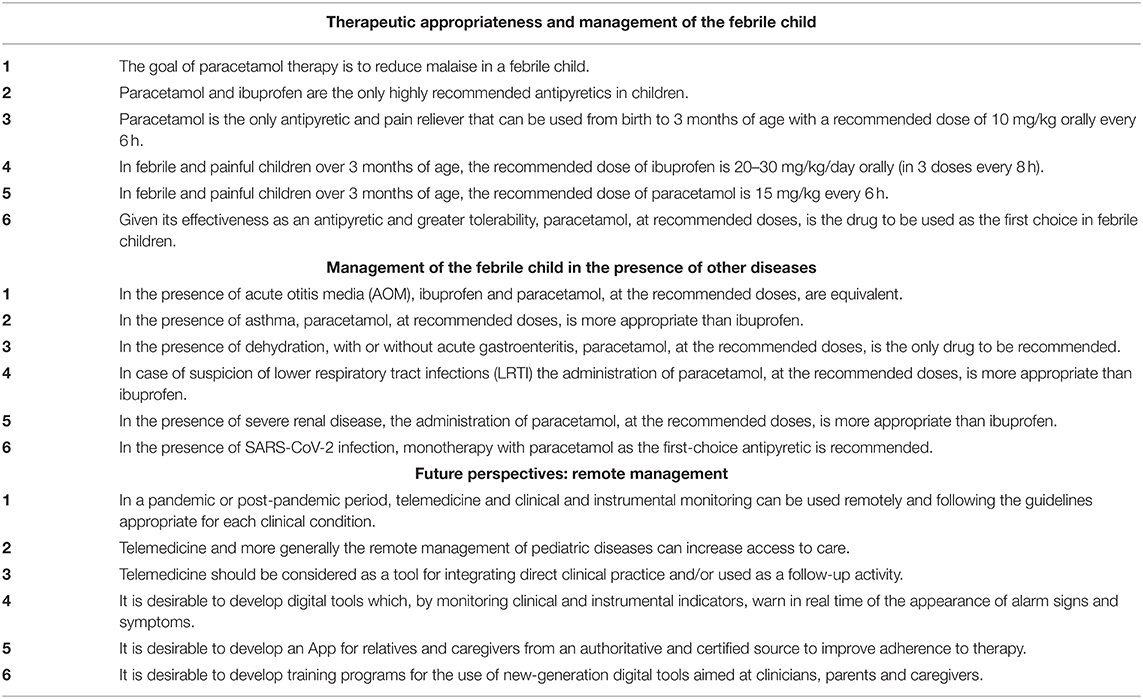
A first questionnaire for anonymous consultation with the panel was then formulated, consisting of 18 statements divided into three sections (Table 2). Two questions related to panelists' geographical areas (north, center, or south) and workplace (hospital or territorial) were added. After the first round of consultation, the board processed the answers given by the panelists and produced a second questionnaire, which was eventually submitted to the same panel of experts.
Evaluation Phase
The questionnaires shared by the board were administered to the panel of experts via a web platform that guaranteed anonymity and the impossibility for the manager to associate the single questionnaire with the compiler. Each panelist had previously received the literature references supporting the questionnaire. Panelists were asked to score each statement by the following scale: 1, strong disagreement; 2, fair disagreement; 3, no opinion; 4, fair agreement; 5, strong agreement. For the analysis of results, responses were categorized as negative (score 1–2) or neutral (score 3), and positive (score 4–5). For each statement, the average score and the percentage of voters who gave positive responses were considered, and the cut-off level for consensus was 75% agreement. After the first round, the board evaluated the responses in order to identify areas of agreement and acquire further information to improve the survey through a second questionnaire (Table 3).
Results
The first questionnaire administered to the panel (Table 2) was sent to 80 pediatricians, and 72 of them responded. Of them, 23% were working in hospitals and 72% outside, 33% were from northern, 12% central, and 55% southern Italy or islands. The second questionnaire administered to the panel (Table 3) was sent to the same 80 pediatricians and 69 of them responded, without significant differences for workplaces or geographical distribution as compared with the first questionnaire. Overall, 75 participants answered at least one of the two questionnaires.
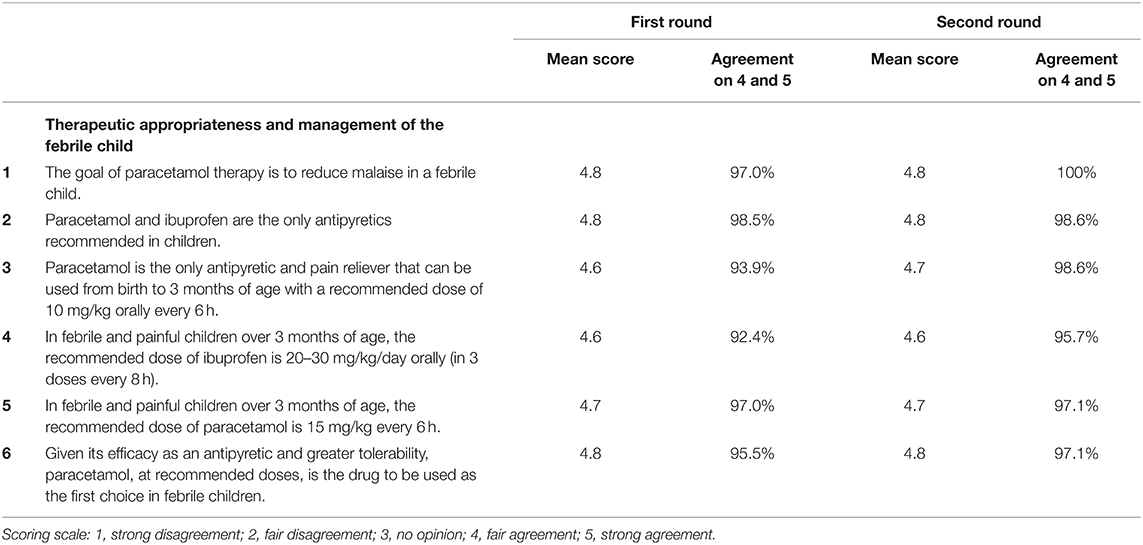
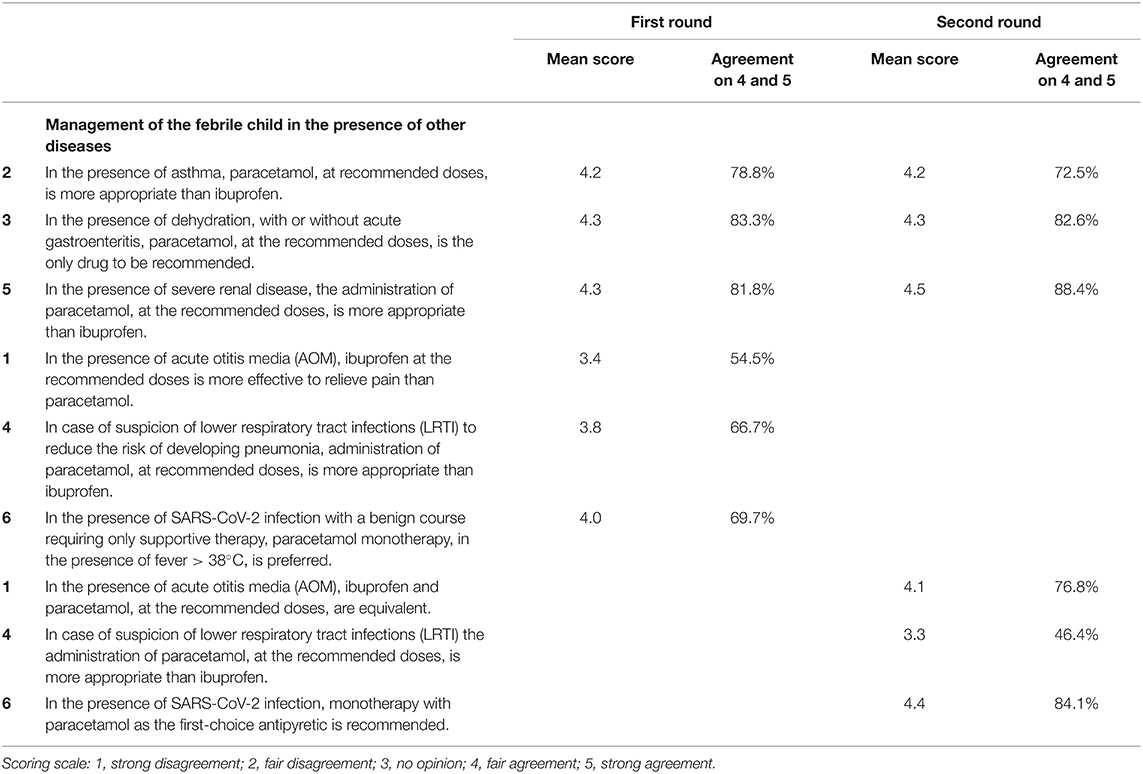
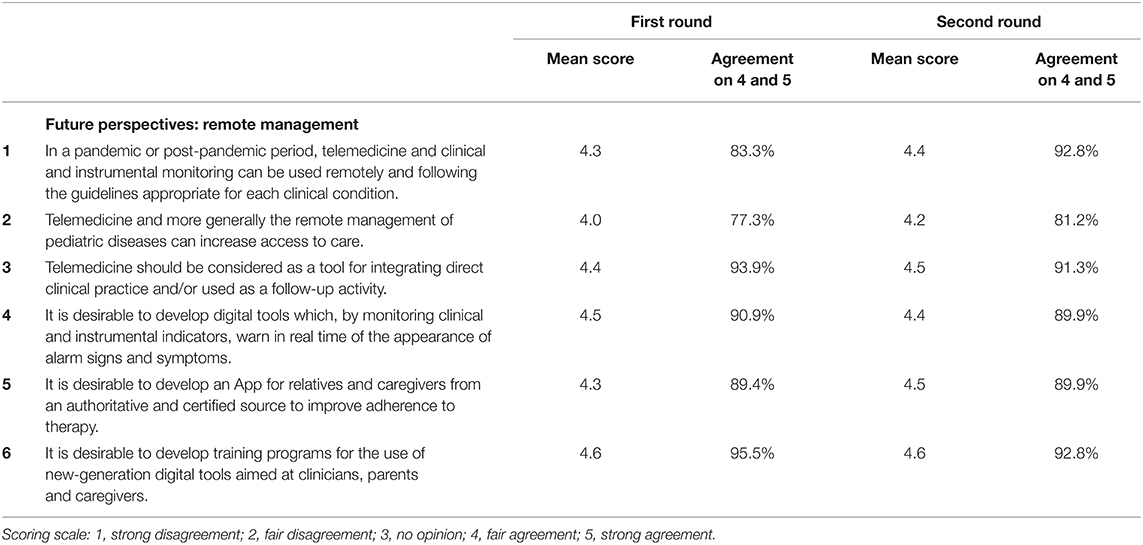
The results of both rounds are presented in Tables 4a–c. After the first round, there was a high level of consensus for all the statements of the first section, which is “Therapeutic appropriateness and management of the febrile child,” with average scores from 4.6 to 4.8 and over 90% of positive responses. For the second section, “Management of the febrile child in the presence of other diseases,” there was consensus level on three statements only, namely, on asthma, dehydration, and severe renal disease, with average scores from 4.2 to 4.3 and agreement from 79% to 84%. Three statements, namely, on AOM, lower respiratory tract infections, and COVID-19, obtained average scores from 3.4 to 4.0 and agreement from 55% to 70%, thus below the level of consensus. For the third section, “Future perspectives: remote management,” there was good consensus on all statements, with average scores from 4.0 to 4.6 and agreement from 77% to 96%.
Therefore, based on the results of the first round, the board modified statements for the second round. Statement no. 1, “In the presence of acute otitis media (AOM), ibuprofen at the recommended doses is more effective to relieve pain than paracetamol,” became “In the presence of acute otitis media (AOM), ibuprofen and paracetamol, at recommended doses are equivalent.” Statement no. 4, “In case of suspicion of lower respiratory tract infections (LRTI) to reduce the risk of developing pneumonia, the administration of paracetamol, at the recommended doses, is more appropriate than ibuprofen,” became “In case of suspicion of lower respiratory tract infections (LRTI), the administration of paracetamol, at the recommended doses, is more appropriate than ibuprofen.” Statement no. 6, “In the presence of SARS-CoV-2 infection with a benign course requiring only supportive therapy, monotherapy with paracetamol, in the presence of fever> 38°C, is preferred,” became “In the presence of SARS-CoV-2 infection, monotherapy with paracetamol as the first-choice antipyretic is recommended.”
The results of the second round confirmed the consensus on all previous statements and achieved the consensus on statements no. 1 and 6 as modified. Despite the modification, statement no. 4 did not achieve the required level of consensus.
Discussion
The main finding of this study was that a panel of Italian pediatricians agreed on most of the statements on the management of febrile children.
Therapeutic Appropriateness and Management of the Febrile Child
The first section of the questionnaire included statements mostly regarding the indications and dosage of paracetamol and ibuprofen in febrile children, as per regulatory and guidelines recommendations. The excellent levels of consensus achieved after both rounds suggest that the panelists of the present study consider, based on their clinical experience, the recommended use and dosage of these antipyretic drugs (paracetamol and ibuprofen) adequate even for very young children (10), which was not always the case in the past. The statement no. 6 on paracetamol as first-choice antipyretic in children achieved a high level of consensus. In the absence of an explicit recommendation by the current guidelines, this may reflect homogeneity of opinions derived from individual clinical practice.
Management of the Febrile Child in the Presence of Other Diseases
The second section of the questionnaire included statements on issues less disciplined by guidelines or supported by a limited number of studies (11–17). As expected, the agreement was variable, with only three statements, which focused on potential contraindications rather than efficacy, achieving the consensus level already after first round. Of the three statements not achieving consensus after the first round, no. 1 was focused on pain rather than fever, no. 2 on a clinically not well-defined condition as a preventive treatment to reduce complications, and no. 3 on COVID-19 domiciliary treatment slightly differing from the current recommendations by the Italian government. The disagreement on statement no. 1 likely reflects that the panelists did not consider ibuprofen as having superior analgesic properties, which was confirmed by the consensus achieved at the end of the second round on the modified statement, where pain was omitted with paracetamol and ibuprofen being considered equivalent. Similarly, the consensus on statement no. 6 was achieved at the second round after the limitation to fever > 38°C had been removed. This is partially in line with the protocol of the Italian government for general COVID-19 population, which recommends the use of paracetamol or non-steroidal anti-inflammatory drugs without fever threshold.
Future Perspectives: Remote Management
The third section of the questionnaire was focused on remote medical management, not specifically limited to febrile children (18). Although this is a topic not widely considered in the pediatric literature, all statements achieved high levels of consensus already after the first round and were confirmed after the second. This may reflect the awareness of unmet needs generated by COVID-19 lockdown periods. Indeed, some telemedicine programs that were already existing for chronic diseases, such as diabetes, hypothyroidism, inflammatory bowel diseases, celiac disease, cystic fibrosis, and epilepsy, have been further implemented during the pandemic. The issue of telemedicine was discussed in depth during the board meetings, and there was unanimous consensus that telemedicine might be useful for the management of chronic clinical diseases, monitoring of therapies, and giving advice to parents of children living in remote areas, therefore experiencing access difficulties to reach the hospital or their primary care pediatricians. However, it should be used carefully for acute diseases, such as infectious diseases, and for emergencies. In the case of febrile children, the board agreed that remote visits may help in collecting history before ambulatory visits, making a first diagnosis, and monitoring certain parameters. However, it must be kept in mind that the management cannot be disconnected from the ultimate diagnosis of the underlying disease, and one must be sufficiently skilled to quickly realize whether patient's conditions are deteriorating, thus requiring an urgent ambulatory or hospital visit with physical examination.
Limitations
This study has some limitations. First, the questionnaire included only statements considering paracetamol and ibuprofen without multiple-choice questions giving panelists the opportunity of giving opinions on other antipyretic drugs, which may have induced bias. Second, the panel included a small number of pediatricians, all working in Italy. This may limit the generalizability of the results to all specialists within Italy or abroad. However, it should be noted that all the panel members had high clinical experience and their responses were most likely based on the most recent knowledge in the field.
Currently, there is no gold standard for sample size for Delphi panels. In published studies, the size can range from 10 to 1,000 participants (19), and many Delphi panels have been conducted on fewer than 15 participants (20).
Furthermore, according to experts, the success of a survey using the Delphi approach stems more from the qualification of the participating experts rather than the sample size (21).
Conclusions
This consensus initiative using the Delphi process revealed a high level of consensus among Italian pediatricians on several aspects of the management of febrile children. In particular, there was consensus on the adequacy of all statements reflecting the recommendations given by regulatory agencies and guidelines, and on the position of paracetamol as first-line choice symptomatic treatment of fever in children. Moreover, there was consensus on the need of nationwide standardized implementation of telemedicine for management of selected conditions. Because of the limited number of participating pediatricians, the consensus statements of the present study should represent only expert opinions to support everyday decision process complementary to recommendations by regulatory agencies and existing guidelines.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This study received an unconditioned grant from Angelini Pharma S.p.A., Rome, Italy. The funder was not involved in the study design, collection, analysis, interpretation of data, and the writing of this article or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Medical writing support was provided by Ilaria Scaricabarozzi, Ph.D., on behalf Menthalia S.r.l., Naples, Italy.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.834673/full#supplementary-material
References
1. Chiappini E, Venturini E, Remaschi G, Principi N, Longhi R, Tovo PA, et al. 2016 Update of the italian pediatric society guidelines for management of fever in children. J Pediatr. (2017) 180:177–83. doi: 10.1016/j.jpeds.2016.09.043
2. Murphy M, Sanderson C, Black N. Consensus development methods and their use in clinical guideline development. Health Technol Assess. (1998) 2:1–100. doi: 10.3310/hta2030
3. Hasson F, Keeney S, McKenna H. Research guidelines for the delphi survey technique. J Adv Nurs. (2000) 32:1008–15. doi: 10.1046/j.1365-2648.2000.t01-1-01567.x
4. Chiappini E, Bortone B, Galli L, de Martino M. Guidelines for the symptomatic management of fever in children: systematic review of the literature and quality appraisal with AGREE II. BMJ Open. (2017) 7:e015404. doi: 10.1136/bmjopen-2016-015404
5. Cioffredi LA, Jhaveri R. Evaluation and management of febrile children: a review. JAMA Pediatr. (2016) 170: 794–800. doi: 10.1001/jamapediatrics.2016.0596
6. Peters MJ, Khan I, Woolfall K, Deja E, Mouncey PR, Wulff J, et al. Different temperature thresholds for antipyretic intervention in critically ill children with fever due to infection: the FEVER feasibility RCT. Health Technol Assess. (2019) 23:1–148. doi: 10.3310/hta23050
7. Peters MJ, Woolfall K, Khan I, Deja E, Mouncey PR, Wulff J, et al. FEVER investigators on behalf of the Pediatric Intensive Care Society Study Group (PICS-SG) permissive vs. restrictive temperature thresholds in critically ill children with fever and infection: a multicentre randomized clinical pilot trial. Crit Care. (2019) 23:69. doi: 10.1186/s13054-019-2354-4
8. Narayan K, Cooper S, Morphet J, Innes K. Effectiveness of paracetamol vs. ibuprofen administration in febrile children: a systematic literature review. J Pediatr Child Health. (2017) 53:800–7. doi: 10.1111/jpc.13507
9. Kanabar DJ. A clinical and safety review of paracetamol and ibuprofen in children. Inflammopharmacology. (2017) 25:1–9. doi: 10.1007/s10787-016-0302-3
10. Tan E, Braithwaite I, McKinlay CJD, Dalziel SR. Comparison of acetaminophen (Paracetamol) with ibuprofen for treatment of fever or pain in children younger than 2 years: a systematic review and meta-analysis. JAMA Netw Open. (2020) 1:3. doi: 10.1001/jamanetworkopen.2020.22398
11. Sjoukes A, Venekamp RP, van de Pol AC, Hay AD, Little P, Schilder AG, et al. Paracetamol (acetaminophen) or non-steroidal anti-inflammatory drugs, alone or combined, for pain relief in acute otitis media in children. Cochrane Database Syst Rev. (2016) 15:12. doi: 10.1002/14651858.CD011534.pub2
12. Marchisio P, Galli L, Bortone B, Ciarcià M, Motisi MA, Novelli A, et al. Italian panel for the management of acute otitis media in children updated guidelines for the management of acute otitis media in children by the italian society of pediatrics: treatment. Pediatr Infect Dis J. (2019) 38: S10–21. doi: 10.1097/INF.0000000000002452
13. Sherbash M, Furuya-Kanamori L, Nader JD, Thalib L. Risk of wheezing and asthma exacerbation in children treated with paracetamol versus ibuprofen: a systematic review and meta-analysis of randomised controlled trials. BMC Pulm Med. (2020) 20:72. doi: 10.1186/s12890-020-1102-5
14. Quaglietta L, Martinelli M, Staiano A. Serious infectious events and ibuprofen administration in pediatrics: a narrative review in the era of COVID-19 pandemic. Ital J Pediatr. (2021) 47:20. doi: 10.1186/s13052-021-00974-0
15. Henderson LA, Canna SW, Friedman KG, Gorelik M, Lapidus SK, Bassiri H, et al. American college of rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with SARS-CoV-2 and hyperinflammation in pediatric COVID-19: version 2. Arthritis Rheumatol. (2021) 73:e13–29. doi: 10.1002/art.41616
16. Venturini E, Montagnani C, Garazzino S, Donà D, Pierantoni L, Lo Vecchio A, et al. Italian SITIP-SIP SARS-CoV-2 pediatric infection study group. treatment of children with COVID-19: position paper of the Italian society of pediatric infectious disease. Ital J Pediatr. (2020) 46:139. doi: 10.1186/s13052-020-00900-w
17. Nunziata F, Bruzzese E, Poeta M, Pierri L, Cazzola A, Ciccarelli GP, et al. Health-care organization for the management and surveillance of SARS-CoV-2 infection in children during pandemic in Campania region, Italy. Ital J Pediatr. (2020) 46:170. doi: 10.1186/s13052-020-00928-y
18. Pappalardo M, Fanelli U, Chiné V, Neglia C, Gramegna A, Argentiero A, et al. Telemedicine in pediatric infectious diseases. Children (Basel). (2021) 8:260. doi: 10.3390/children8040260
19. Cascella M, Miceli L, Cutugno F, Di Lorenzo G, Morabito A, Oriente A, et al. On behalf of the Delphi Panel. A delphi consensus approach for the management of chronic pain during and after the COVID-19 Era. Int J Environ Res Public Health. (2021) 18:13372. doi: 10.3390/ijerph182413372
20. McPherson S, Reese C, Wendler MC. Methodology update: delphi studies. Nurs Res. (2018) 67:404–10. doi: 10.1097/NNR.0000000000000297
Keywords: fever, pediatrics, Delphi process, remote management, expert consensus
Citation: Chiappini E, Vitale A, Badolato R, Becherucci P, Careddu D, Di Mauro A, Doria M and Staiano A (2022) The Effective Management of Fever in Pediatrics and Insights on Remote Management: Experts' Consensus Using a Delphi Approach. Front. Pediatr. 10:834673. doi: 10.3389/fped.2022.834673
Received: 13 December 2021; Accepted: 21 March 2022;
Published: 26 April 2022.
Edited by:
Jérémie F. Cohen, Necker-Enfants Malades Hospital, FranceReviewed by:
Silvina C. Raiden, Hospital Pedro de Elizalde, ArgentinaSebastiano A.G. Lava, Centre Hospitalier Universitaire Vaudois (CHUV), Switzerland
Copyright © 2022 Chiappini, Vitale, Badolato, Becherucci, Careddu, Di Mauro, Doria and Staiano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elena Chiappini, elena.chiappini@unifi.it
 Elena Chiappini
Elena Chiappini Antonio Vitale2
Antonio Vitale2  Raffaele Badolato
Raffaele Badolato Domenico Careddu
Domenico Careddu Antonio Di Mauro
Antonio Di Mauro Annamaria Staiano
Annamaria Staiano