Minimally invasive management of pediatric osteoarticular infections
- 1Pediatric Rheumatology Unit, Hospital Universitario La Paz, Madrid, Spain
- 2Pediatrics Department, Hospital Materno-Infantil, Málaga, Spain
- 3Pediatric Infectious Diseases Department, Hospital Universitario La Paz, Fundación IdiPaz, Madrid, Spain
- 4Translational Research Network in Pediatric Infectious Diseases (RITIP), Madrid, Spain
- 5CIBER Enfermedades Infecciosas (CIBERINFEC), Madrid, Spain
Introduction
Osteoarticular infections (OAI) is an umbrella term for inflammation usually due to bacterial infection of bone and/or joints. The term OAI includes osteomyelitis (OM), septic arthritis (SA), septic osteoarthritis, spondylodiscitis (SD), pyogenic sacroiliitis (PSI), septic tenosynovitis, and chondritis. Acute OAI are defined as the diagnosis within 2 weeks after the onset of clinical manifestations in a previously uninfected location (1, 2).
Historically, Staphylococcus aureus has been described as the most prevalent microorganism involved in OAI in any age group (3). However, in recent years Kingella kingae has been described as the main causative agent of OAI in children aged 6–48 months (4). K. kingae OAI are usually characterized by a mild clinical presentation, minor increase in biological markers, and a better outcome than those caused by other bacteria, especially S. aureus (5). Children with S. aureus OAI tend to be older, have an associated fever, and a marked rise in acute phase reactants levels and white blood cell counts (5, 6). Likewise, methicillin-resistant S. aureus (MRSA) OAI has been related to severe purulent complications, increased probability of secondary-procedure, and a significantly higher admission rate to the intensive care unit (7, 8).
These different degrees of clinical presentation call into question whether it is time to rethink traditional recommendations and start treating the patient on an individualized basis. In fact, there is growing evidence of good outcomes in patients with primary hematogenous OAI treated with a minimally invasive approach consisting of stricter surgical indications and short courses or no intravenous therapy.
Route of antibiotic therapy
Traditionally, children with acute OAI receive intravenous antibiotic therapy for several weeks, then switch to oral therapy. However, classical practice of a long duration of parenteral therapy is currently a source of controversy since this practice has been associated with prolonged hospitalization, high cost, and sometimes the need for central venous access (3). For this reason, some authors have suggested the possibility of reducing the duration of intravenous antibiotic therapy to only a few days, and then switching to oral therapy (9–11).
Recently, Peltola et al. conducted a prospective, randomized, and controlled study assessing 131 children aged 3 months to 15 years with culture positive OAI (11). The patients were randomly assigned to receive clindamycin or a first-generation cephalosporin for 20 or 30 days, including an intravenous phase for the first 2 to 4 days. Their conclusions were that most cases of pediatric OAI could be treated for only 20 days with a short initial period intravenously with large doses of a well-absorbed antimicrobial, including in infections caused by S. aureus.
Furthermore, in a systematic review and meta-analysis about short- vs. long-course antibiotics in pediatric and adult patients with osteomyelitis, no significant difference in the rate of treatment failure was found. This study showed that short-course antibiotics might be as effective as long-course antibiotics for patients with osteomyelitis, although inconsistent results were found in studies on vertebral osteomyelitis (12).
In addition, antibiotics with longer half-lives such as dalbavancin are also under study, predominantly in adult patients, to avoid or reduce admission time. Dalbavancin is a lipoglycopeptide with activity against a wide spectrum of gram-positive bacteria, including MRSA. Its pharmacokinetic profile includes a prolonged elimination half-life of 14.4 days and good penetration into bone and synovial fluid (13), offering potential for outpatient parenteral antibiotic therapy (14, 15). A two-dose regimen of weekly dalbavancin has proven to be effective for the treatment of osteomyelitis in adults in a randomized clinical trial (16). Also, a low rate of adverse events has been notified in a recent retrospective multicenter study, including two pediatric patients (17). So dalbavancin is currently considered an alternative for the treatment of osteomyelitis in adults. Its use must be based on risk-benefit considerations (18). However, data on its clinical efficacy in children are still limited.
Beyond reducing intravenous treatment time, in early 2022 Wald-Dickler et al. published the results of a revision of 20 randomized controlled trials comparing oral to intravenous therapy for blood and bone infection, with seven of them regarding osteomyelitis in 1,321 adult patients. Staphylococcus aureus and Pseudomonas aeruginosa were the most common monomicrobial organisms (19). They concluded that oral antibiotic therapy was at least as effective as IV, showing higher adverse event rates and decreased patient satisfaction in the IV groups. They suggest considering oral therapy in patients who meet certain criteria, including clinical and hemodynamical stability, good oral tolerance, availability of oral therapy, and no psychosocial or logistical reasons to prefer IV therapy.
Interestingly, very similar conclusions and selection criteria for exclusive oral therapy were described by our group in 2018 based on the results of the prospective study performed in an only pediatric population. The authors compared 25 outpatients who received just oral antibiotics with 228 hospitalized children who received initial IV treatment. The patients who received oral antibiotic since the diagnosis had good general condition, adequate oral intake, close control, and acceptance by legal guardians. All the OAI outpatients had a favorable outcome without sequelae (6).
In fact, most recently, the results of a nationwide multicenter registry from the Spanish Network of Osteoarticular Infections were published. In this study, 893 children who initially received intravenous antibiotics were compared (group 1) with 64 children who received exclusively oral therapy (group 2). Patients from group 2 were characterized as being younger, having a lower percentage of Staphylococcus aureus, and a higher proportion of Kingella kingae than in group 1, without showing any complications or clinical sequelae in this group. They concluded that an exclusively oral administration could be a safe option in selected patients with OAI clinically suggestive of K. kingae etiology and without risk factors for developing sequelae and complications. They propose low-risk criteria that should be met to be selected for this option of treatment (Table 1) (20).
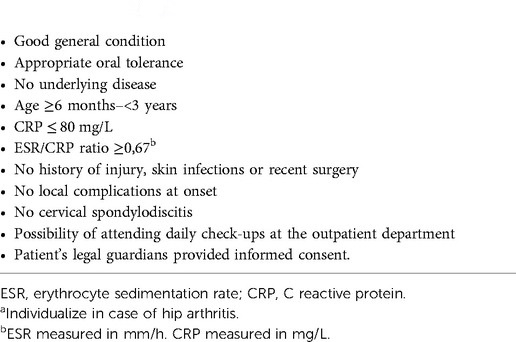
Table 1. Proposed criteria for minimally invasive approach (all must be fulfilled)a (20).
Oral treatment is usually well tolerated, and most compliance failures are related to intercurrent processes (poor oral tolerance or vomiting). In addition, it provides increased patient comfort and decreases the risk of nosocomial infection associated with prolonged intravenous therapy (21), so further studies are needed. In fact, a multi-center clinical trial called BEST (BonE and Joint Infections—Simplifying Treatment in Children Trial) is currently being carried out. The results of this trial will possibly shed light on this issue.
Surgery
Together with antibiotics, surgery plays a key role in the treatment of acute osteomyelitis and septic arthritis in children (22). Surgery makes it possible to obtain biological samples that are useful for identifying the etiologic agent and then guiding the selection and duration of antimicrobial therapy (23).
Acute osteomyelitis
Surgery in patients with OM has been described as able to alter the process of bone necrosis, to remove the demineralized bone, and to clean the surrounding soft tissue, thereby reducing the bacterial load (24).
Historically, early biopsy and debridement were recommended. However, there is little current high-quality evidence on which to base current surgical practice, and some retrospective case series have shown that up to 90% of patients with an early OM can be cured with conservative treatment, especially when antibiotics are initiated during the first days of the onset of symptoms (25, 26).
Although most cases of hematogenous osteomyelitis resolve with antimicrobial therapy alone, surgical intervention may be required in patients who do not respond to antibiotic treatment for the suspicion of an underlying complication, to control the focus of infection and preserve joint function.
Despite the fact that no clear indications have been established, general guidelines recommend surgical drainage for patients who present multifocal disease, who do not respond to antibiotics after 48–72 h, where ther is radiological evidence of a substantial pus collection, and sequestration as well as in patients with septic aspect at onset (1, 23, 27–30). Data regarding abscess size that mandates surgical drainage are very limited, although drainage of abscesses 2 cm or more in diameter has been suggested (23).
In current practice, the relative roles of bacterial virulence, host age, and immunity are unclear. More invasive surgery appears more common when bacteria have specific virulence genes, such as PVL. Acute osteoarticular infections caused by MRSA or S. aureus producing PVL often require more surgical sessions as these bacteria are associated with a more aggressive clinical course (3, 31, 32). However, most children with K. kingae OAI respond rapidly to conservative treatment with appropriate antibiotics and do not usually require invasive surgical procedures to achieve clinical improvement (33).
Spondylodiscitis
In most of the children with SD, conservative treatment without surgery is usually sufficient. Currently, surgical management is indicated in case of vertebral instability, neurological signs, or failure of conservative treatment (34–36).
Drainage technique in SA
Acute septic arthritis in children is considered an orthopedic emergency. Its treatment includes drainage of the joint to reduce the risk of complications such as avascular necrosis of the bone and permanent cartilage damage due to increased intra-articular pressure (37). However, the literature is scarce with respect to the optimal drainage technique in children with SA.
According to the guideline of the European Society for Paediatric Infectious Diseases (ESPID), SA in children should be treated with joint drainage by aspiration (arthrocentesis), arthroscopy, or arthrotomy followed by intravenous antibiotics (1).
Recently, Spaans and Donders have published three systematic reviews of the literature (including retrospective and prospective studies) on drainage techniques for septic hip, knee, and shoulder arthritis in children (38–40). These joints are important in the pediatric population since the hip and knee are the most commonly affected locations in children with SA and hip and shoulder have been described as the joints with greater prognosis interest due to the potential risk of avascular necrosis. Although it is inappropriate to draw firm conclusions from these reviews, they could help to better understand the possible role of each technique in children with SA. Globally, these systematic reviews show that both aspiration and arthrotomy can achieve good clinical results in the treatment of SA. However, there are some points of interest.
First, hip SA patients treated by arthrotomy required fewer additional drainage procedures in comparison with arthroscopy and arthrocentesis. Arthrocentesis of hip joint followed by a drain seemed to be associated with less likelihood of an additional arthrotomy than only with arthrocentesis without a drain (40).
Nevertheless, inferior clinical outcomes and more radiological sequelae were seen in hip SA patients treated with an arthrotomy as the first approach. Furthermore, most of the patients with hip SA treated initially with arthrocentesis who showed radiological changes had needed an additional arthrotomy as a second step (40).
Similarly, Smith et al. also found a higher percentage of damage to the glenohumeral joint in the arthrotomy group in shoulder SA patients, but the difference was not statistically significant (41). However, most of the radiological sequelae described in knee SA patients were seen in those who were treated with arthrocentesis but without irrigation (42).
Second, the time between onset of symptoms and treatment has been also described as a possible predictor of clinical and radiological outcomes in different studies, being poor in those with higher delay (43–46).
Thirdly, age and acute phase reactants have also been assessed. Failure of joint aspiration was evaluated by Tornero et al. who conducted a retrospective study that included 74 children with septic knee arthritis initially treated with needle joint aspiration. They found that arthrocentesis did not require additional drainage in any patient younger than one year old and in all patients between 1 and 3 years with a CRP < 20 mg/l (47), possibly related to K. kingae.
Finally, small or difficult-to-access joints such as sacroiliac, sternoclavicular, or interphalangeal are notoriously more difficult to aspirate, especially in children. For this reason, in these cases, a trial of medical management with antibiotics could be attempted (20, 48, 49). In patients in whom a sample from the site of infection cannot be obtained, detection of K. kingae DNA in oropharynx could point to etiology by this bacterium (50).
Conclusion
This paper presents an up-to-date look at the approach and treatment of pediatric patients with primary hematogenous OAI. In the light of recent research, it appears that, in selected patients, minimally invasive treatment could be a safe and effective option, although further studies are needed.
Author contributions
RMAR, ENC, and CCR contributed to conception, content selection, and literature search. RMAR wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Saavedra-Lozano J, Falup-Pecurariu O, Faust SN, Girschick H, Hartwig N, Kaplan S, et al. Bone and joint infections. Pediatr Infect Dis J. (2017) 36:788–99. doi: 10.1097/INF.0000000000001635
2. Saavedra-Lozano J, Calvo C, Huguet Carol R, Rodrigo C, Núñez E, Pérez C, et al. SEIP-SERPE-SEOP consensus document on aetiopathogenesis and diagnosis of uncomplicated acute osteomyelitis and septic arthritis. An Pediatr (Barc). (2015) 83(3):216.e1–10. doi: 10.1016/j.anpedi.2014.08.006
3. Castellazzi L, Mantero M, Esposito S. Update onthe management of pediatric acute osteomyelitis and septic arthritis. Int J Mol Sci. (2016) 17(6):855. doi: 10.3390/ijms17060855
4. Yagupsky P. Kingella kingae reveals its secrets. Microorganisms. (2022) 10(7):1261. doi: 10.3390/microorganisms10071261
5. Gouveia C, Subtil A, Norte S, Arcangelo J, Santos MA, Corte-Real R, et al. Distinguishing Kingella kingae from pyogenic acute septic arthritis in young portuguese children. Microorganisms. (2022) 10(6):1233. doi: 10.3390/microorganisms10061233
6. Alcobendas R, Remesal A, Murias S, Nuñez E, Calvo C. Outpatients with acute osteoarticular infections had favourable outcomes when they received just oral antibiotics without intravenous antibiotics. Acta Paediatr. (2018) 107(10):1792–7. doi: 10.1111/apa.14373
7. Jain MJ, Bradko V, Zhu H, Inneh I, Shinava VR. Pediatric osteoarticular infection: trend in surgically treated patients and association of methicillin-resistant Staphylococcus aureus with requirement of secondary procedures. J Pediatr Orthop B. (2021) 30(6):579–84. doi: 10.1097/BPB.0000000000000819
8. Kaushik A, Kest H. Pediatric methicillin-resistant Staphylococcus aureus osteoarticular infections. Microorganisms. (2018) 6(2):40. doi: 10.3390/microorganisms6020040
9. Jagodzinski NA, Kanwar R, Graham K, Bache CE. Prospective evaluation of a shortened regimen of treatment for acute osteomyelitis and septic arthritis in children. Pediatr Orthop. (2009) 29(5):518–25. doi: 10.1097/BPO.0b013e3181ab472d
10. Jaberi FM, Shahcheraghi GH, Ahadzadeh M. Short-term intravenous antibiotic treatment of acute hematogenous bone and joint infection in children: a prospective randomized trial. J Pediatr Orthop. (2002) 22(3):317–20.11961446
11. Peltola H, Pääkkönen M, Kallio P, Kallio MJ. Osteomyelitis-septic arthritis study group. Short- versus long-term antimicrobial treatment for acute hematogenous osteomyelitis of childhood: prospective, randomized trial on 131 culture-positive cases. Pediatr Infect Dis J. (2010) 29(12):1123–8. doi: 10.1097/INF.0b013e3181f55a89
12. Huang CY, Hsieh RW, Yen HT, Hsu TC, Chen CY, Chen YC, et al. Short- versus long-course antibiotics in osteomyelitis: a systematic review and meta-analysis. Int J Antimicrob Agents. (2019) 53(3):246–60. doi: 10.1016/j.ijantimicag.2019.01.007
13. Dunne MW, Puttagunta S, Sprenger CR, Rubino C, Van Wart S, Baldassarre J. Extended-duration dosing and distribution of dalbavancin into bone and articular tissue. Antimicrob Agents Chemother. (2015) 59(4):1849–55. doi: 10.1128/AAC.04550-14
14. Bassetti M, Peghin M, Carnelutti A, Righi E. The role of dalbavancin in skin and soft tissue infections. Curr Opin Infect Dis. (2018) 31(2):141–7. doi: 10.1097/QCO.0000000000000430
15. Almangour TA, Alhifany AA. Dalbavancin for the management of osteomyelitis: a major step forward? J Antimicrob Chemother. (2020) 75(10):2717–22. doi: 10.1093/jac/dkaa188
16. Rappo U, Puttagunta S, Shevchenko V, Shevchenko A, Jandourek A, Gonzalez P L, et al. Dalbavancin for the treatment of osteomyelitis in adult patients:a randomized clinical trial of efficacy and safety. Open Forum Infect Dis. (2018) 6(1):ofy331. doi: 10.1093/ofid/ofy331
17. Wunsch S, Krause R, Valentin T, Prattes J, Jonata O, Lenger A, et al. Multicenter clinical experience of real life Dalbavancin use in gram-positive infections. Int J Infect Dis. (2019) 81:210–4. doi: 10.1016/j.ijid.2019.02.013
18. Spellberg B, Aggrey G, Brennan MB, Footer B, Forrest G, Hamilton F, et al. Use of novel strategies to develop guidelines for management of pyogenic osteomyelitis in adults: a WikiGuidelines group consensus statement. JAMA Netw Open. (2022) 5(5):e2211321. doi: 10.1001/jamanetworkopen.2022.11321
19. Wald-Dickler N, Holtom P, Phillips MC, Centor RM, Lee RA, Baden R, et al. Oral is the new IV-challenging decades of blood and bone infection dogma: a systematic review. Am J Med. (2022) 135(3):369–79.e1. doi: 10.1016/j.amjmed.2021.10.007
20. Alcobendas Rueda RM, Núñez E, Martín L, Hernández MB, Saavedra-Lozano J, Udaondo C, et al. Oral versus intravenous antibiotics for pediatric osteoarticular infection: when and to whom? Pediatr Infect Dis J. (2022) 41(9):e351–57. doi: 10.1097/INF.0000000000003619
21. Tetzlaff TR, Mc Cracken GH, Nelson JD. Oral antibiotic therapy for skeletal infections of children. J Pediatr. (1978) 92:485–90, 21. doi: 10.1016/S0022-3476(78)80455-7
22. Pääkkönen M, Peltola H. Simplifying the treatment of acute bacterial bone and joint infections in children. Expert Rev Anti Infect Ther. (2011) 9:1125–231. doi: 10.1586/eri.11.140
23. Woods CR, Bradley JS, Chatterje A, Coppley LA, Robinson J, Kronman MP, et al. Clinical practice guideline by the pediatric infectious diseases society and the infectious diseases society of America: guideline on diagnosis and management of acute hematogenous osteomyelitis in pediatrics. J Pediatric Infect Dis Soc. (2021) 10(8):801–44. doi: 10.1093/jpids/piab027
24. Ceroni D, Kampouroglou G, Valaikaite R, Anderson della Llana R, Salvo D. Osteoarticular infectionsin young children: what has changed over the last years? Swiss Med Wkly. (2014) 144:w13971. doi: 10.4414/smw.2014.13971
25. Vaughan PA, Newman NM, Rosman MA. Acute hematogenous osteomyelitis in children. J Pediatr Orthop. (1987) 7:652–5. doi: 10.1097/01241398-198707060-00004
26. Cole WG, Dalziel RE, Leitl S. Treatment of acute osteomyelitis in childhood. J Bone Joint Surg Br. (1982) 64:218–23. doi: 10.1302/0301-620X.64B2.6802854
27. Dartnell J, Ramachandran M, Katchburian M. Haematogenous acute and subacute paediatric osteomyelitis: a systematic review of the literature. J Bone Joint Surg Br. (2012) 94:584–95. doi: 10.1302/0301-620X.94B5.28523
28. Gornitzky AL, Kim AE, O’Donnell JM, Swarup I. Diagnosis and management of osteomyelitis in children: a critical analysis review. JBJS Rev. (2020.) 8(6):e1900202. doi: 10.2106/JBJS.RVW.19.00202
29. Upasani VV, Burns JD, Bastrom TP, Baldwin KD, Schoenecker JG, Shore BJ, et al. Practice variation in the surgical management of children with acute hematogenous osteomyelitis. J Pediatr Orthop. (2022) 42(5):e520–5. doi: 10.1097/BPO.0000000000002123
30. Palmer B, Wang ME. Clinical guideline highlights for the hospitalist: Diagnosis and management of acute hematogenous osteomyelitis in children. J Hosp Med. (2022) 17(2):114–6. doi: 10.1002/jhm.2742
31. Albiński MK, Lutz N, Ceroni D, N´Dele D, Zambelli PY, Bregou A. Paediatric musculoskeletal infections with Panton-Valentine leucocidin. Swiss Med Wkly. (2018) 148:w14669. doi: 10.4414/smw.2018.14669
32. Tuason DA, Gheen T, Sun D, Huang R, Copley L. Clinical and laboratory parameters associated with multiple surgeries in children with acute hematogenous osteomyelitis. J Pediatr Orthop. (2014) 34:565–70. doi: 10.1097/BPO.0000000000000136
33. Yagupsky P. Kingella kingae: from medical rarity to an emerging paediatric pathogen. Lancet Infect Dis. (2004) 4:358–67. doi: 10.1016/S1473-3099(04)01046-1
34. Roversi M, Mirra G, Musolino A, Barbuti D, Lancella L, Deriu D, et al. Spondylodiscitis in children: a retrospective study and comparison with non-vertebral osteomyelitis. Front Pediatr. (2021) 9:727031. doi: 10.3389/fped.2021.727031
35. Skaf GS, Domloj NT, Fehlings MG, Bouclaous CH, Sabbagh AS, Kanafani ZA, et al. Pyogenic spondylodiscitis: an overview. J Infect Public Health. (2010) 3(1):5–16. doi: 10.1016/j.jiph.2010.01.001
36. de Moraes Barros Fucs PM, Robert M, Yamada HH. Spinal infections in children: a review. Int Orthop. (2012) 36(2):387–95. doi: 10.1007/s00264-011-1388-2
37. Pääkkönen M, Peltola H. Management of a child with suspected acute septic arthritis. Arch Dis Child. (2012) 97:287–92. doi: 10.1136/archdischild-2011-300462
38. Spaans AJ, Donders CM, Bessems JHJM, van Bergen CJA. Aspiration or arthrotomy for paediatric septic arthritis of the shoulder and elbow: a systematic review. EFORT Open Rev. (2021) 6(8):651–7. doi: 10.1302/2058-5241.6.200122
39. Donders CM, Spaans AJ, Bessems JHJM, van Bergen CJA. Arthrocentesis, arthroscopy or arthrotomy for septic knee arthritis in children: a systematic review. J Child Orthop. (2021) 15(1):48–54. doi: 10.1302/1863-2548.15.200129
40. Donders CM, Spaans AJ, Bessems JHJM. A systematic review of the optimal drainage technique for septic hip arthritis in children. Hip Int. (2022) 32(5):685–93. doi: 10.1177/1120700021989666
41. Smith SP, Thyoka M, Lavy CB, Pitani A. Septic arthritis of the shoulder in children in Malawi: a randomised, prospective study of aspiration versus arthrotomy and washout. J Bone Joint Surg Br. (2002) 84:1167–72. doi: 10.1302/0301-620X.84B8.0841167
42. Strong M, Lejman T, Michno P, Hayman M. Sequelae from septic arthritis of the knee during the first two years of life. J Pediatr Orthop. (1994) 14:745–51. doi: 10.1097/01241398-199414060-00010
43. Umer M, Hashmi P, Ahmad T, Ahmed M, Umer M. Septic arthritis of the hip in children–aga khan university hospital experience in Pakistan. J Pak Med Assoc. (2003) 53:472–8.14696888
44. Rutz E, Spoerri M. Septic arthritis of the paediatric hip—a review of current diagnostic approaches and therapeutic concepts. Acta Orthop Belg. (2013) 79:123–34. doi: 10.1302/0301-620X.93B11
45. Bos CF, Mol LJ, Obermann WR, Tjin a Ton ER. Late sequelae of neonatal septic arthritis of the shoulder. J Bone Joint Surg Br. (1998) 80:645–50. doi: 10.1302/0301-620X.80B4.0800645
46. Ernat J, Riccio AI, Fitzpatrick K, Jo C, Wimberly RL. Osteomyelitis is commonly associated with septic arthritis of the shoulder in children. J Pediatr Orthop. (2017) 37:547–52. doi: 10.1097/BPO.0000000000000709
47. Tornero E. Knee arthritis in children: when can it be safely treated with needle joint aspiration? A large children’s tertiary hospital study. J Pediatr Orthop. (2019) 39(3):130–5. doi: 10.1097/BPO.0000000000000883
48. Alhariri S, Kalas MA, Hassan M, Carter JT, Ghafouri SR, Dihown F. Medical management of septic arthritis of the sternoclavicular joint with extended-spectrum beta-lactamase-producing Escherichia coli: a case report. Cureus. (2022) 14(4):e23969. doi: 10.7759/cureus.23969
49. Kwon HY, Cha B, Im JH, Baek JH, Lee JS. Medical management of septic arthritis of sternoclavicular joint: a case report. Medicine (Baltimore). (2020) 99(44):e22938. doi: 10.1097/MD.0000000000022938
Keywords: osteomyelitis, oral, arthrocentesis, children, osteoarticular infections, treatment, septic arthritis (SA)
Citation: Alcobendas RM, Núñez E and Calvo C (2022) Minimally invasive management of pediatric osteoarticular infections. Front. Pediatr. 10:1017035. doi: 10.3389/fped.2022.1017035
Received: 11 August 2022; Accepted: 21 September 2022;
Published: 11 November 2022.
Edited by:
Pablo Yagupsky, Soroka Medical Center, IsraelReviewed by:
Eleftheria Samara, Centre Hospitalier Universitaire Vaudois (CHUV), Switzerland© 2022 Alcobendas, Nuñez and Calvo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rosa María Alcobendas rosaalcobendasrueda@gmail.com
†ORCID Rosa María Alcobendas orcid.org/0000-0002-0749-1506
Specialty Section: This article was submitted to Pediatric Infectious Diseases, a section of the journal Frontiers in Pediatrics
 Rosa María Alcobendas
Rosa María Alcobendas Esmeralda Núñez2
Esmeralda Núñez2  Cristina Calvo
Cristina Calvo