A web app-based music intervention reduces experimental thermal pain: A randomized trial on preferred versus least-liked music style
- 1International Laboratory for Brain, Music and Sound Research (BRAMS), University of Montreal, McGill University, Montreal, QC, Canada
- 2Department of Psychology, University of Montreal, Montreal, QC, Canada
- 3Research Centre, Sherbrooke's University Hospital, Sherbrooke, QC, Canada
- 4Faculty of Medicine and Health Sciences, University of Sherbrooke, Sherbrooke, QC, Canada
Digital technologies are increasingly being used to strengthen national health systems. Music is used as a management technique for pain. The objective of this study is to demonstrate the effects of a web app-based music intervention on pain. The participants were healthy adults and underwent three conditions: Conditioned Pain Modulation (CPM), Most-Liked Music (MLM) and Least-Liked Music (LLM). The music used is MUSIC CARE©, a web app-based personalized musical intervention (“U” Sequence based on a musical composition algorithm). Thermal pain was measured before starting the 20-min music intervention and after three time points for each music condition: 2.20, 11.30, and 20 min. Mean pain perceptions were significantly reduced under both LLM and MLM conditions. Pain decrease was more important under MLM condition than LLM condition at 2.20 min with a mean difference between both conditions of 9.7 (±3.9) (p = 0.0195) and at 11.30 min [9.2 (±3.3), p = 0.0099]. LLM is correlated with CPM but not MLM, suggesting different mechanisms between LLM and MLM. Musical intervention, a simple method of application, fits perfectly into a multidisciplinary global approach and helps to treat the pain and anxiety disorders of participants.
Clinical trial registration: [https://clinicaltrials.gov/ct2/show/NCT04862832], ClinicalTrials.gov [NCT04862832].
Introduction
Music has been reported as a management technique of acute and chronic pain since 1960 (1) and is nowadays widely used as an alternative or complementary treatment to reduce patient pain (2). Music is easy to implement in clinical contexts as it is safe, non-invasive, and inexpensive (3, 4). Multiple clinical environments can be found using music today (5, 6) for conditions such as childbirth (7–10), resuscitation (11), cardiac surgery (12, 13), cancer (14, 15), in cardiology, during a catheter installation (16), or cataract surgery (17).
Converging evidence suggests that music is indeed beneficial for different types of pain (13, 14, 18, 19), in addition to psychological distress, ranging from smaller-scale mood improvements to anxiety disorders (20). Music can also improve the management of chronic pain conditions, such as cancer by reducing pain and its associated components of anxiety, depression, and quality of life (21).
There are different music procedures used to reduce pain (22), especially one based on music in a medical context (23). In the treatment of pain, the most widely used music is relaxing (5), even if no consensus was reached to indicate a difference between relaxing and stimulating music's ability to reduce pain.
A multitude of endogenous mechanisms can modulate pain perception. Music involves different inputs such as sensory, cognitive, or emotional (24), which, according to the Neuromatrix theory of pain (25) can modulate the final pain perception. Music-induced analgesia could be explained by a change of perception such as distraction (26). Another potential mechanism is the recruitment of Conditioned Pain Modulation (CPM). CPM is based on the recruitment of diffuse noxious inhibitory control (DNIC) from different structures in the brainstem (e.g., periaqueductal gray, nucleus raphe Magnus) following a localized nociceptive stimulation (27). However, CPM is also influenced by descending higher center activities (28). Music is suggested to increase the efficacy of descending mechanisms like conditioned pain modulation (CPM) (29). Brain imaging studies reported that listening to music activate spinal and supraspinal regions known to be involved in endogenous descending pain modulation (30).
Perceived pleasantness has also been suggested to play a role in the analgesic potential of music. Pleasant music according to the participant is superior to unpleasant music or silence in decreasing experimental pain (31). Allowing the patient to choose the style of music adds to pain relief and adds a sense of control over pain (5, 6, 32–34). Paying attention to personal musical preferences and cultural background are among the main characteristics of a successful musical intervention (35, 36). However, in many studies evaluating the effect of music on pain, there is a lack of details of the musical choice (33). It was also reported that pain was even more reduced when participants were selecting preferred music from a list given by the researcher (5). Recent technological developments now enable patients or caregivers to control the use of music-based interventions using hand-held devices. Silence condition is frequently used as a control condition for music, as sensory, cognitive or emotional inputs are limited during this condition.
Studying the effect of music-based interventions in medical contexts is complex and requests strong methodology. Discussion with researchers in this field suggested that the main methodological research challenges relate to treatment, outcomes, research designs, and implementation (37). According to a systemic review, music sessions should last between 20 and 60 min and consist principally of harmonic variations (38). There is a growing interest to design and implement new and cost-effective online treatments using technological advances. The Ministries of Health of the WHO European Region are increasingly investing in Digital Therapeutics (DTx). They are helping overcome barriers to the adoption of DTx to strengthen health systems and to explore ways to accelerate DTx for public health. Digital health technologies can improve access to health services, lower costs, improve the quality of care and increase the efficiency of health systems. They offer ways to manage personal health, with a focus on disease prevention rather than just treatment (39).
Based on these recent scientific recommendations, MUSIC CARE©, a web app-based personalized music intervention, has developed a “U” Sequence based on a musical composition algorithm. The music sequence can last from 20 to 60 min and is divided into several phases that gradually enable the patient to lower their pain and anxiety levels in line with the “U” Sequence technique (11, 40, 41). Previous studies had confirmed the effectiveness of this web app-based music intervention in reducing pain and/or anxiety in patients with a variety of conditions (2, 42, 43).
The principal objective of this study was therefore to describe the effects of a web app-based music intervention on the modulation of pain and the difference between the most-liked music (MLM) and least-liked music (LLM) conditions. A secondary objective was to compare the effect of CPM with MLM and LLM on pain perception. Our hypothesis was that most-liked music will be superior to least-liked music in reducing pain perception. Our second hypothesis was that the pain relief during the music interventions would be correlated with CPM, suggesting comparable mechanisms.
Materials and methods
Study design
A randomized, multi-center, open-label, controlled, crossover clinical trial was conducted in four centers: Sherbrooke University Hospital Centre, Sherbrooke University, the campus of Bishop's University and Cégep Champlain. Participants were recruited in these 4 centers, but the procedures were conducted at Sherbrooke University Hospital Centre by two research assistants. This study was composed of 3 experimental sessions on 3 consecutive days: on day 1 CPM was tested in all participants for a baseline endogenous pain inhibition measurement. All subjects then entered a randomized crossover part of the study with MLM or LLM on day 2 and day 3.
Participants
Thirty-three healthy adults [20 women and 13 men mean age of 23.5 years (±4,9)] participated in this study. Participants were excluded if they were musicians with knowledge of music theory, diagnosed and taking medication for chronic pain, skin problems, psychological or neurological pathologies. The protocol was approved by the ethics committee of Centre Hospitalier Universitaire de Sherbrooke and informed consent was obtained from all participants. The verbal and written instructions including the questionnaires were presented in French or English at the choice of the participant. The patient flow chart is presented in Figure 1.
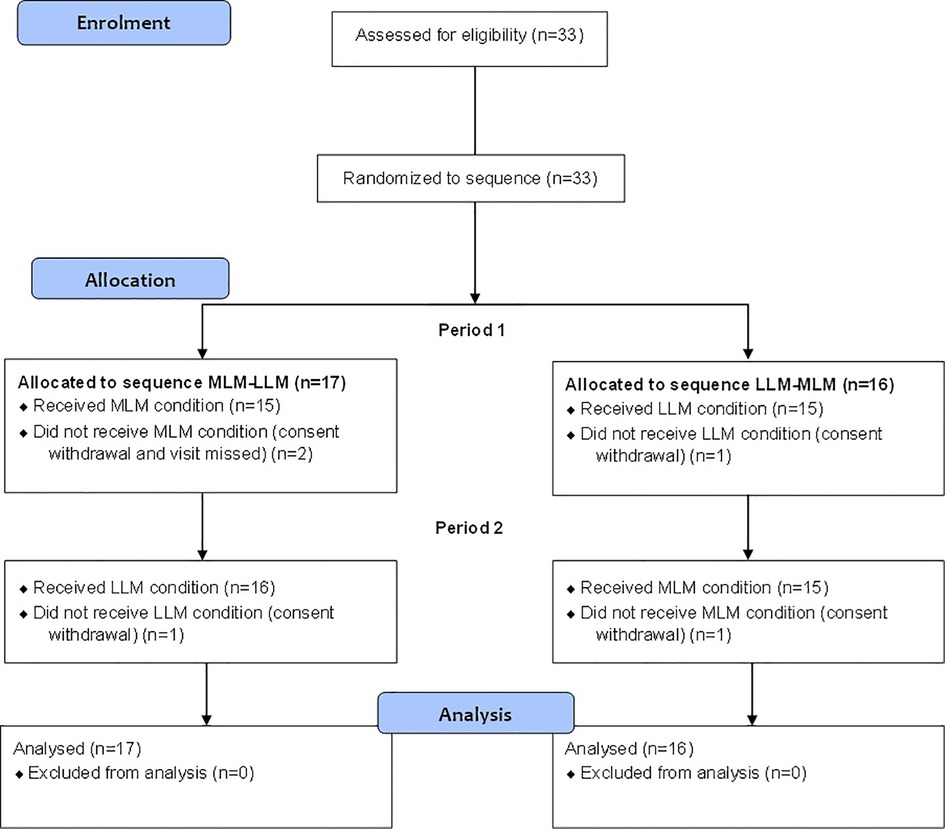
Figure 1. Participant flow chart following consolidated standards of reporting trials guidelines for MLM-LLM and LLM-MLM randomized arms.
Web app-based music intervention
The web app-based music intervention was administered using headphones via a tablet-based application called MUSIC CARE©. The MUSIC CARE© app is a receptive music intervention and utilizes the “U” sequence (Figure 2) designed to gradually relax the listener (41–43).
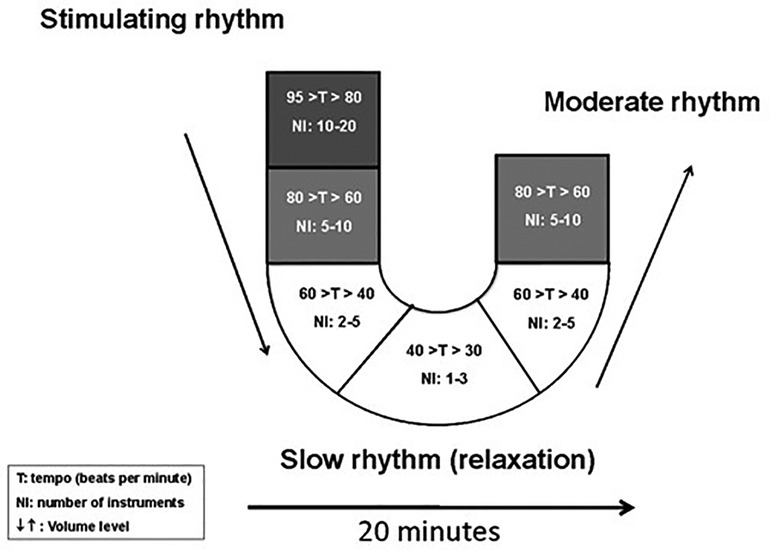
Figure 2. The “U” sequence. The musical sequence of 20 min is divided into 6 different musical pieces at 3–4 min each.
It is implemented using a musical sequence of 20 min that was divided into 6 different musical pieces at 3–4 min each. The first five sections are in minor mode where the first one starts with stimulating musical rhythm 80–95 beats per minute (bpm). Then, the remaining four sub-pieces are presented in a blended fashion in an attempt for the patient to gradually fall into a relaxed state via a gradual reduction in musical tempo (40–80 bpm), orchestral size, frequencies, and volume (descending arms of the “U”) followed by a phase of maximum relaxation (downward phase of the “U”). The last section is in major mode which corresponds to a phase that gradually returns to baseline dynamics (ascending arms of the “U”). This is thought to induce a catharsis. This construction is hypothesized to allow a mirror effect with the patient's emotions throughout the sequence. This is similar to the iso principle of music therapy (44) that describes the process of alteration of the patient's state by music. The minor mode validates the patient's suffering (negative emotions) and then the relaxation phase calms the patients, and finally the major mode incites positive emotions. In 1936 it was shown that the minor mode is known to be related to negative emotions while the major mode is related to positive emotions (45).
Thirty musical sequences were available (classical, folk, jazz, reggae and traditional music from South America, Caledonia, Asia, India or the Middle East) (Table 1), allowing for a personalized choice for the subjects. The music sequences are all 20 min, instrumental, professionally recorded in the studio and composed specifically for the MUSIC CARE© application and are thus unfamiliar to participants. The participants of this group listened, with headphones (QuietComfort® 25 Acoustic Noise Cancelling® headphones, Framingham, Massachusetts, Bose Corporation) plugged to a tablet (Samsung Galaxy Tab, 2013, 3 Lite 7.0, Suwon, South Korea, Samsung Electronics Co., Ltd.) to 30 s samples of the available sequences and rated them on a 0–10 scale in which 0 is “I do not want to listen to this one” and 10: “I really want to listen to this one.” The order of the 30 samples was randomized for each participant. The highest rating was selected for the MLM condition and the lowest was for the LLM condition.
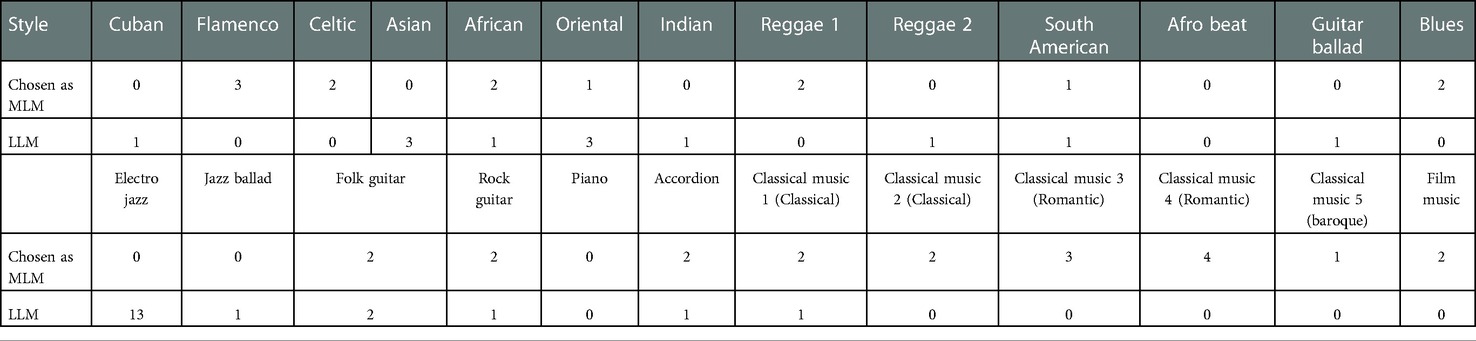
Table 1. Number of participants by musical style choices for most-liked music (MLM) and least-liked music (MLM).
Thermal stimulation and conditioned pain modulation (CPM)
CPM was measured the first day in all subjects to have a baseline of the efficacy of endogenous pain modulation as previously describe (46). Since CPM is variable amongst healthy subjects and patients (47, 48), this baseline permitted to test for a correlation in pain changes between CPM and music sessions that could suggest comparable mechanisms.
The CPM paradigm to study the efficacy of inhibitory mechanisms is obtained by calculating the difference in pain levels elicited by the test stimulus (TS) before and after the conditioning stimulus (CS) (46, 48). The TS was generated by a 3 cm2 thermode (TSA II, NeuroSensory Analyzer, Medoc Instruments, North Carolina, USA) applied on the non-dominant forearm of each participant at a predetermined, individually tailored temperature (pain levels of 50/100 based on pretests). The temperature remains constant over the next 120 s. Participants were asked to continuously record their pain level using a 10 cm Computerized Visual Analog Scale (CoVAS). Participants were asked to move the slider to reflect their pain from the left boundary (identified as “no pain”—score = 0) to the right boundary (identified as “worst pain imaginable”—score = 100). The CoVAS sampling rate was set at 10 Hz (10 pain measurements per second). The CS consists of a cold pressor test (CPT), wherein subjects immerse the opposite forearm in a cold-water bath (10°) for 120 s. The thermal stimulation intensities used before and after the music conditions are the same as the one used for the CPM paradigm.
Measures
Sociodemographic data collected were sex, age and years of schooling.
For anxiety, the State Trait Anxiety Inventory (STAI) was used. There are two subscales: one for trait anxiety (STAI-Trait Y2) and one for state anxiety (STAI-State Y1). Each subscale contains 20 items and each statement is rated on a 4-point scale from: 1 “not at all” to 4 “very much so.” The overall score for each subscale ranges from 20 to 80. Participants with a score of 20–45 have low anxiety, 46–55 moderate anxiety and 56–80 severe anxiety.
For depression, the Beck Depression Inventory (BDI) was used. There are 21 items on a 4-point scale, so the overall score is from 0 to 63. Participants with a score from 0 to 10 do not have depression, between 11 and 16, they have mild mood disturbance, 17–20 borderline clinical depression, 21–30 moderate depression, 31–40 severe depression and more than 40 extreme depression.
For pain catastrophizing, the Pain Catastrophizing Scale (PCS) was used. There are 13 items from 0: “not at all” to 4: “all the time”. The overall score ranges from 0 to 52 in which participants with a score between 0 and 16 are non-catastrophizers, 17–29 are low catastrophizers and 30–52 severe catastrophizers.
At the end of the music intervention (i.e., after 20 min of listening), the perception of time was evaluated. The duration of the session was not communicated to the participants and they were asked how long they thought the session had lasted.
Procedure
There was three testing days for each participant. The participant was seated in a comfortable chair in a quiet room. The first day, before the pain tests started, consent form was read and signed by the participants. Then, the MLM and LLM were determined according to the process described above. Sociodemographic data, STAI, BDI and PCS questionnaires were administered. Then, a first 2-min thermal pain test was performed followed by the CPT and a second thermal pain test. The second and third days consisted of a first two-minute thermal pain test followed by one of the music conditions (MLM or LLM). The order of music condition was randomized per a generated randomized sequence of integers based on a pseudo-random number algorithm. Under the music conditions, three thermal pain tests were performed: the first one at 2.20 min after the music started; the second one was after the relaxation phase at 11.30 min and the third one after the whole 20-min cycle. STAI questionnaire was also completed during these testing days.
Statistical analyses
Based on data from previous studies managed in the Pain Research Laboratory (MUSEC: music, emotion and cognition), an effect size (d of Cohen) of 0.69 was used for sample size calculation (49). With a power of 80% and a type I risk of 5% (50), thirty-three participants needed to be included.
Evolution of overall pain perception was performed using a mixed effect model for repeated measures with an unstructured covariance matrix. Comparisons of continuous endpoints between pre-and post-condition, and between conditions were performed using paired student t-tests or Wilcoxon Sign Rank tests (non-parametric form of paired student t-tests, if distributions for variables were not normal). Bonferroni method was used for the correction of multiple comparisons.
All statistical tests were conducted using SAS® Studio (version 3.8, Edition enterprise, SAS Institute Inc, Cary, NC, USA). Comparisons of continuous endpoints between pre-and post-condition, and between conditions were performed using Wilcoxon Sign Rank tests (non-parametric form of paired student t-tests, as distributions for all dependent variables were not normal) (51). Normality of the distributions was tested using Shapiro-Wilk test. Comparisons between both music conditions were performed using Grizzle's model for crossover design with condition, period and sequence as fixed effects and participants within sequence as a random effect. Carryover effect was tested using Student t-tests. Statistics reported include means ± standard deviation and associated two-tailed p values as significance levels (cut-off of 0.05 for statistical significance). The research was submitted and approved by the Human Health Research Ethics Board from the CHUS. The analysis was conducted under the Intent-to-Treat (ITT) principle maintaining balance generated from the original random treatment allocation and avoiding statistical bias. As suggested for ITT, we ignored noncompliance, protocol deviations, withdrawal, and anything that happens after randomization (52). All subjects were then included in the analysis.
Results
Thirty-three participants were included in the study. Three participants failed to complete the protocol (3 conditions), two completed only the CPT condition and one did not complete MLM condition. Among these 33 participants, all were randomized in the crossover part (17 to sequence 1 and 16 to sequence 2, Figure 1). The results of this controlled, randomized study are presented in compliance with the guidelines from the Consortium on the Assessment of Non-pharmacological Treatments (53).
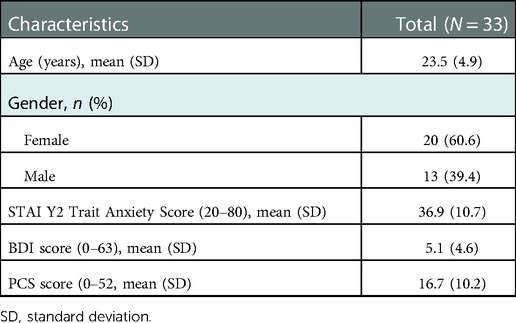
The sociodemographic and baseline characteristics of the participants are described in Table 2. The mean age of the participants was 23.5 ± 4.9 years. There were 20 females (60.6%). In our sample, 28 participants had low trait anxiety, four moderate and one severe. For depression, 28 had no depression, four had mild mood disturbance and one had borderline clinical depression non-diagnosed. As for pain catastrophizing, we had 17 non-catastrophists, 14 mild catastrophizers and two severe ones.
Primary endpoint
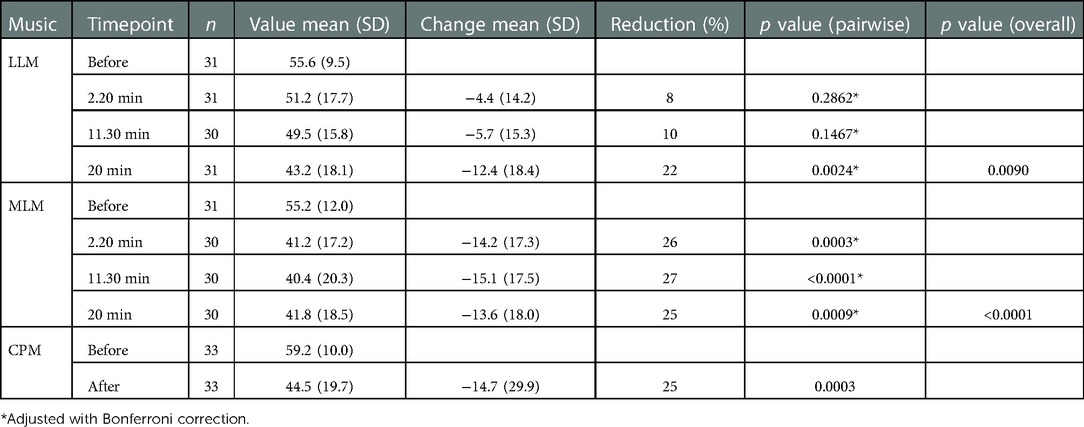
Before the music intervention, mean pain perceptions were similar in both conditions: 55.2 (SD ± 12.0) in MLM and 55.6 (SD ± 9.5) in LLM. Overall, mean pain perceptions were significantly reduced under LLM and MLM conditions (p = 0.0090 and p < 0.0001, respectively), earlier under MLM condition (2.20 min) compared to LLM (20 min) (Table 3 and Figure 3).
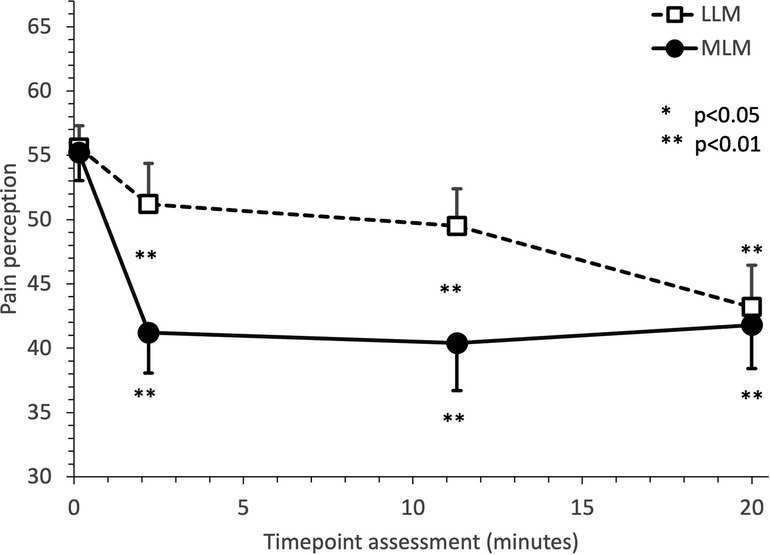
Figure 3. Evolution of mean pain perception under music intervention. Pain perception was collected using a Computerized Visual Analog Scale (CoVAS), which consists of a slider running along a 100 mm horizontal slider connected to the computer. Participants were asked to move the slider to reflect their pain from the left boundary (identified as “no pain”—score = 0) to the right boundary (identified as “worst pain imaginable”—score = 100). Timepoints of assessments were before music intervention, 2.20 min after the music started, 11.30 min after the music started (after the relaxation phase) at and after the whole 20-min cycle. Both conditions (LLM and MLM) are represented. Whiskers indicate SEMs.
Under LLM condition, the reduction in pain levels was 4.4 (SD ± 14.2) after 2.20 min (p = 0.2862), 5.7 (SD ± 15.3) after 11.30 min (p = 0.1467) and 12.4 (SD ± 18.4) after 20 min (p = 0.0024). Under MLM condition, the reduction in pain levels was 14.2 (SD ± 17.3) after 2.20 min (p = 0.0003), 15.1 (SD ± 17.5) after 11.30 min (p < 0.0001) and 13.6 (SD ± 18.0) after 20 min (p = 0.0009).
Secondary endpoints
Reduction in pain observed at 2.20 min under MLM condition is comparable to the one observed under the CPM condition. Under CPM condition, the reduction in pain levels was 14.7 (SD ± 29.9) after the immersion of the participants’ arm in 10 degrees circulating water for 2 min.
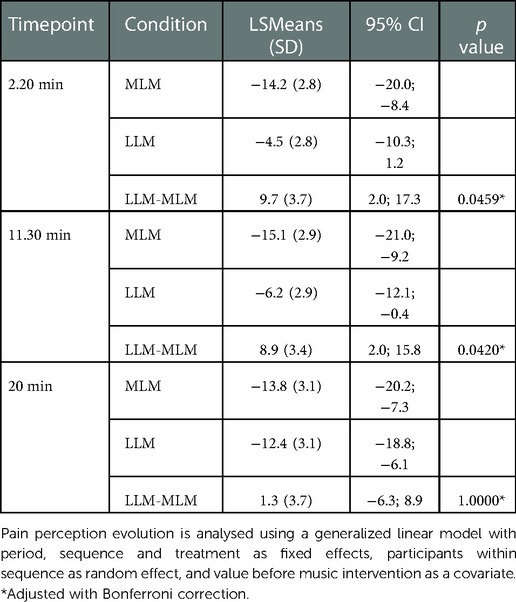
Mean pain perceptions were significantly more reduced under MLM condition than under LLM condition at 2.20 min with an adjusted mean difference between both conditions of 9.7 (±3.7) (p = 0.0459) and at 11.30 min with an adjusted mean difference between both conditions of 8.9 (±3.4) (p = 0.0420) (Table 4). The differences between MLM and LLM are no longer significantly different after 20 min (p = 1.0000).
Regarding the perception of time, the musical intervention session appeared to be significantly shorter under MLM condition with a mean duration of 14.8 min (SD ± 5.5) than under the LLM condition with a mean perceived duration of 18.9 min (SD ± 7.1) (p = 0.0239).
No significant differences have been found between the conditions and the mood scores (BDI) or the pain catastrophizing scores (PCS). There was a small but significant level of anxiety difference between the 3 conditions (p = 0.0335), with an average value of 31.5 (±7.7) under the CPT condition, 30.7 (±9.4) under the LLM condition and 27.7 (±6.9) under the MLM condition.
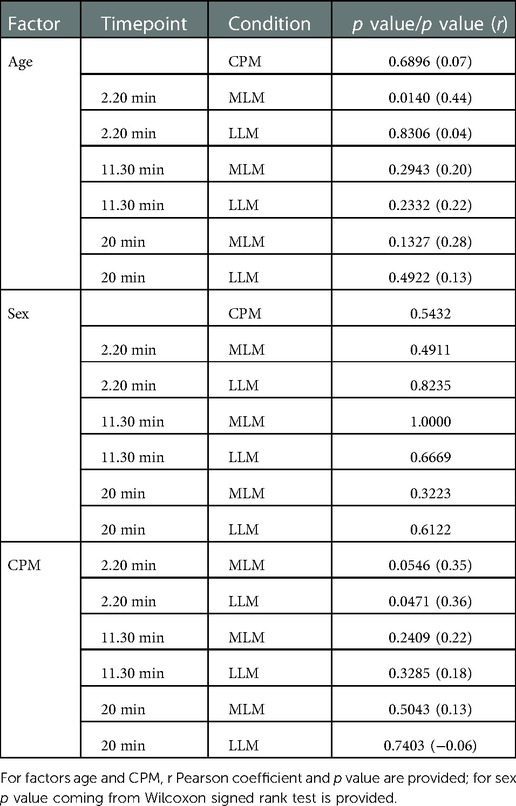
Finally, to verify for similarities in the amplitude of the pain reduction between CPM and music sessions, correlation analysis were done between pain changes for CPM, MLM and LLM and different parameters like age and sex. A correlation on pain perception evolution at 2.20 min between CPM and LLM conditions was shown (Pearson coefficient of 0.36, p = 0.0471) as well as a correlation on pain perception evolution at 2.20 min between age and MLM condition (Pearson coefficient of 0.44, p = 0.0140) (Table 5).
Discussion
For the past few years, digital therapeutics (DTx), a subset of digital health, is changing the healthcare delivery system with evidence-based technologies driven by high quality software to prevent, manage, or treat a medical disorder or disease and that improve patient outcomes (54). The consensus among researchers in the field of DTx is that it requires more clinical data and investigation to be fully evaluated. Music is one of these approaches that was demonstrated to have significant pain reduction effects for different clinical conditions (3–6).
Several mechanisms have been suggested to understand music-induced pain reduction. A significant correlation between music pleasantness and pain reduction in healthy subjects was reported, suggesting the importance of the emotional valence for music-induced pain reduction (31). However, in another study also using experimental pain, the authors found that emotional responses were not correlated to the analgesic effects, but that perception of control in the selected music during the experiment and the engagement with music in the subject's everyday life were the most important parameters (55). Interestingly, antagonists drugs of endogenous dopamine and opioids did not reduce the effect of music analgesia (56). The authors found that the main source of the effect was related to the expectation of analgesia from music, suggesting mechanisms comparable to placebo analgesia. Based on these results, we could conclude that distraction and expectation are probably the main effect, but other mechanisms including endogenous pain modulation such as CPM was suggested (29). In support of this hypothesis, a study measured pain-related activity in the brain, brainstem, and spinal cord using magnetic resonance imaging (MRI) during sessions of favorite music versus no music (30). They found significant activation during the music session in regions related to descending pain inhibition mechanisms implicated in CPM such as the periaqueductal gray, rostral ventromedial medulla, and the spinal cord.
The goal of the present study was to compare the effect of most-liked music to least-liked music on pain perception at different times during the 20-min music sessions. We also compared the effects of CPM with the two music sessions on pain perception in the same subjects. A positive correlation between CPM and the music conditions will not determine if the mechanisms are the same but will give a hint in that direction and confirm the interest of future tests on music-induced analgesia mechanisms.
For the effect of music on pain, we found that the pain level decreased is significantly higher under MLM condition than under LLM condition from 2.20 min of listening to 11.30 min. At the end of the 20-min session, the decrease in pain level is comparable under LLM and MLM. Pain alleviation is thus faster and stable for MLM from the beginning up to 20 min, while the LLM's pain alleviation is by increments needing more than half of the session to perceive a decrease in pain with end results statistically comparable for both conditions.
The cold pressor pain significantly reduced pain perception, supporting a CPM effect. The only significant correlation between music and CPM is for pain perception at 2.20 min for LLM. We can theorize that the “unpleasant” effect of the least preferred music might have activated inhibitory mechanisms such as the unpleasant aspect of the cold pressor pain during the immersion of the arm in cold water. We did not systematically ask for feedback regarding the music at the end of the session, but several subjects spontaneously reported that they finally learned to enjoy the music that they rated as their LLM at the beginning later during the listening. As the music ends up being enjoyed, this “counter-irritation-like” effect of “unpleasant music” seems to disappear with time. This could be due to the mere-exposure effect (57). This cognitive principle states that the more you are exposed to something, the more you like it. This could also suggest that the mechanism of action of music could be comparable to CPM over the first 2 min, but that beyond that, music would allow pain control according to other neurophysiological mechanisms.
It was reported that pleasant music decreased pain more than unpleasant music and silence (31). This is congruent in part with our results as after 2.20 min of LLM, pain perception was higher than after MLM. Participants reported enjoying the MLM more than the LLM when choosing the music at the beginning. Some subjects also spontaneously reported learning to enjoy fairly more the LLM over time. All the conditions may act from different endogenous descending modulatory systems, according to the time frames. More direct evaluation of the implicated mechanisms would be of interest in future studies.
Another interesting aspect is the perception of time during the music conditions. The musical intervention session appeared to be perceived as significantly shorter under MLM condition than the LLM condition. This effect could be related to the “immersive” effect of most-liked music compared to least-liked music. Using subjects’ selected music in video games is enhancing time underestimation (58). Other important psychological factors are anxiety, depression and pain catastrophizing that can affect pain perception (59–61). In this study the only significant effect was a lower anxiety score during MLM compared to CPT, suggesting a relaxation effect of MLM. Altogether these results suggest that MLM is rapidly active in reducing pain, reduce anxiety and give the impression that the time was shorter than it was. All positive characteristics for intervention pain control during painful procedures.
MUSIC CARE©, the web app-based music intervention evaluated has good ecological validity, which is hard to find in experimental music studies. It is already used in clinical contexts to alleviate pain and allows for reduced consumption of analgesics. The analgesia provided by medication usually starts 20–30 min after intake. However, the MLM chosen shows here a music-induced analgesia already present after 2.20 min and maintained for 20 min. As a result, using the participants’ favorite MUSIC CARE©'s style could be a convenient and valuable adjuvant to acute pain treatments. Moreover, with its selection of 30 different styles of music, it has more potential of personalized care. Patients in clinics could also bring their own music and increase even more the valence of the music and its associated analgesia. Nevertheless, in an experimental setting, MUSIC CARE© allowed for a higher comparability between the music sequences compared to many music interventions studies as they are all constructed in the same way.
This study has some limitations. We compared music-induced analgesia to the cold bath to induce CPM to look for similarities or differences in responses. Other control conditions could have been used. The silence gives a setting with no distraction of attention or emotions (62). White noise, pink noise (white noise using the same frequency range as music) or audio books could be used. These approaches distract attention and have very limited emotional potential (63). They are painless auditory inputs and already used in some research as control conditions to music (11). Future studies comparing different distraction modalities could be of interest.
These results are comparable to previous studies (64–66). Future studies with patients experiencing chronic pain to see the effect on clinical pain and related endogenous pain modulation mechanisms would be important. Brain activation could be assessed as well when listening to MUSIC CARE© to better understand the related brain regions implicated. To further explore musical appreciation, it would also have been interesting to include any measures that extend beyond participants’ mentions of their own experiences with the conditions. The literature supports enormous diversity in antecedents and causes of music appreciation across contexts, individuals, cultures, and historical periods. But the processes implicated in that are still unexplored (67).
In conclusion, MLM significantly reduce pain perception and more rapidly than LLM, but both types are analgesics after 20 min. Interestingly, the LLM pain reduction was correlated with CPM after 2.20 min. We hypothesized that the unpleasantness of the LLM music is triggering a “counterirritation effect” possibly comparable to CPM that fades over time when the unpleasantness seems to fade over time. LLM is correlated with CPM but not MML, suggesting different mechanisms between LLM and MLM.
In France, general practitioners can now prescribe music as part of the overall pain management of patients suffering from chronic diseases. This means that apps like MUSIC CARE© can be prescribed by general practitioners and used outside the hospital environment. The MUSIC CARE© application is currently used in 500 hospital departments around the world. The music intervention is administered via a smartphone- (or tablet- and computer-) based application called MUSIC CARE© which is low-cost, highly available to the public, and usable in a home environment. The MUSIC CARE© app is a receptive music intervention, allowing the patient to freely adjust the length of and choose the preferred style between varying sequences of instrumental music.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Human Health Research Ethics Board from the CHUS. The patients/participants provided their written informed consent to participate in this study.
Author contributions
Both OS and SM have substantially contributed to data collection, analysis and the manuscript preparation. All authors contributed to the article and approved the submitted version.
Funding
We are indebted to SM grants from CIHR# 130619 and NSERC #2018-2422 and Catherine Theriault, our research assistant, for her commitment to the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gardner WJ, Licklider JC, Weisz AZ. Suppression of pain by sound. Science. (1960) 132(3418):32–3. doi: 10.1126/science.132.3418.32
2. Hoareau SG, De Diego E, Guetin S. Pain management and music therapy. Rev Infirm. (2016) 217:31–3. doi: 10.1016/j.revinf.2015.10.025
3. Lunde SJ, Vuust P, Garza-Villarreal EA, Vase L. Music-induced analgesia: how does music relieve pain? Pain. (2019) 160(5):989–93. doi: 10.1097/j.pain.0000000000001452
4. Li CH, Liu CK, Yang YH, Chou MC, Chen CH, Lai CL. Adjunct effect of music therapy on cognition in Alzheimer's disease in Taiwan: a pilot study. Neuropsychiatr Dis Treat. (2015) 11:291–6. doi: 10.2147/NDT.S73928
5. Kuhlmann AYR, de Rooij A, Kroese LF, van Dijk M, Hunink MGM, Jeekel J. Meta-analysis evaluating music interventions for anxiety and pain in surgery. Br J Surg. (2018) 105(7):773–83. doi: 10.1002/bjs.10853
6. Bradt J, Dileo C, Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database Syst Rev. (2013) 2013(12):CD006577. doi: 10.1002/14651858.CD006577.pub3
8. Phumdoung S, Good M. Music reduces sensation and distress of labor pain. Pain Manag Nurs. (2003) 4(2):54–61. doi: 10.1016/S1524-9042(02)54202-8
9. Ebneshahidi A, Mohseni M. The effect of patient-selected music on early postoperative pain, anxiety, and hemodynamic profile in cesarean section surgery. J Altern Complement Med. (2008) 14(7):827–31. doi: 10.1089/acm.2007.0752
10. Hole J, Hirsch M, Ball E, Meads C. Music as an aid for postoperative recovery in adults: a systematic review and meta-analysis. Lancet. (2015) 386(10004):1659–71. doi: 10.1016/S0140-6736(15)60169-6
11. Jaber S, Bahloul H, Guetin S, Chanques G, Sebbane M, Eledjam JJ. Effects of music therapy in intensive care unit without sedation in weaning patients versus non-ventilated patients. Ann Fr Anesth Reanim. (2007) 26(1):30–8. doi: 10.1016/j.annfar.2006.09.002
12. Jafari H, Emami Zeydi A, Khani S, Esmaeili R, Soleimani A. The effects of listening to preferred music on pain intensity after open heart surgery. Iran J Nurs Midwifery Res. (2012) 17(1):1–6.23493927
13. Hamid MR A, Mansor MB, Zainal Abidin MF. Music therapy for reducing anxiety in patients undergoing total knee replacement surgery under subarachnoid anesthesia. J Orthop Surg. (2022) 30(2):10225536221122347. doi: 10.1177/10225536221122347
14. Rennie C, Irvine DS, Huang E, Huang J. Music therapy as a form of nonpharmacologic pain modulation in patients with cancer: a systematic review of the current literature. Cancers. (2022) 14(18):4416. doi: 10.3390/cancers14184416
15. Duzgun G, Karadakovan A. Effect of music on pain in cancer patients in palliative care service: a randomized controlled study. Omega. (2021) 10:302228211059891. doi: 10.1177/00302228211059891
16. Karakul A, Akgul EA, Yaliniz R, Mese T. Effectiveness of music during cardiac catheterization on children's pain, fear, anxiety and vital signs: a randomized, blind controlled trial. J Pediatr Nurs. (2022) 65:e56–62. doi: 10.1016/j.pedn.2022.02.009
17. Guerrier G, Abdoul H, Jilet L, Rothschild PR, Baillard C. Efficacy of a web app-based music intervention during cataract surgery: a randomized clinical trial. JAMA Ophthalmol. (2021) 139(9):1007–13. doi: 10.1001/jamaophthalmol.2021.2767
18. Evans D. The effectiveness of music as an intervention for hospital patients: a systematic review. J Adv Nurs. (2002) 37(1):8–18. doi: 10.1046/j.1365-2648.2002.02052.x
19. Monteiro J, da Silva Barbirato D, Moraes SLD, Pellizzer EP, do Egito Vasconcelos BC. Does listening to music reduce anxiety and pain in third molar surgery?-a systematic review. Clin Oral Investig. (2022) 26(10):6079–86. doi: 10.1007/s00784-022-04640-5
20. McFerran KS, Hense C, Koike A, Rickwood D. Intentional music use to reduce psychological distress in adolescents accessing primary mental health care. Clin Child Psychol Psychiatry. (2018) 23(4):567–81. doi: 10.1177/1359104518767231
21. Fernando G, Wanigabadu LU, Vidanagama B, Samaranayaka TSP, Jeewandara J. “Adjunctive effects of a short session of music on pain, low-mood and anxiety modulation among cancer patients” - a randomized crossover clinical trial. Indian J Palliat Care. (2019) 25(3):367–73. doi: 10.4103/IJPC.IJPC_22_19
22. Raglio A, Oasi O. Music and health: what interventions for what results? Front Psychol. (2015) 6:230. doi: 10.3389/fpsyg.2015.00230
23. Gochenour KS, Ellis RS, Meredith SL, Vesely KC, Kang P, Haefner S. Music and medicine come together over pain in the air medical transport environment. Air Med J. (2020) 39(6):484–8. doi: 10.1016/j.amj.2020.08.003
24. Sarkamo T, Tervaniemi M, Laitinen S, Forsblom A, Soinila S, Mikkonen M, et al. Music listening enhances cognitive recovery and mood after middle cerebral artery stroke. Brain. (2008) 131(Pt 3):866–76. doi: 10.1093/brain/awn013
25. Melzack R. Pain and the neuromatrix in the brain. J Dent Educ. (2001) 65(12):1378–82. doi: 10.1002/j.0022-0337.2001.65.12.tb03497.x
26. Fields HL, Basbaum A, Heinrich RL. Central nervous system mechanisms of pain modulation. In: McMahon SB, Koltzenburg M, editors. Wall and melzack's texbook of pain. 5. Philadelphia: Elsevier Limited (2006). p. 125–42.
27. Le Bars D, Dickenson AH, Besson JM. Diffuse noxious inhibitory controls (DNIC). II.lack of effect on non-convergent neurones, supraspinal involvement and theoretical implications. Pain. (1979) 6(3):305–27. doi: 10.1016/0304-3959(79)90050-2
28. Goffaux P, Redmond WJ, Rainville P, Marchand S. Descending analgesia–when the spine echoes what the brain expects. Pain. (2007) 130(1-2):137–43. doi: 10.1016/j.pain.2006.11.011
29. Chai PR, Gale JY, Patton ME, Schwartz E, Jambaulikar GD, Wade Taylor S, et al. The impact of music on nociceptive processing. Pain Med. (2020) 21(11):3047–54. doi: 10.1093/pm/pnaa070
30. Dobek CE, Beynon ME, Bosma RL, Stroman PW. Music modulation of pain perception and pain-related activity in the brain, brain stem, and spinal cord: a functional magnetic resonance imaging study. J Pain. (2014) 15(10):1057–68. doi: 10.1016/j.jpain.2014.07.006
31. Roy M, Peretz I, Rainville P. Emotional valence contributes to music-induced analgesia. Pain. (2008) 134(1-2):140–7. doi: 10.1016/j.pain.2007.04.003
32. Bradt J, Norris M, Shim M, Gracely EJ, Gerrity P. Vocal music therapy for chronic pain management in inner-city African Americans: a mixed methods feasibility study. J Music Ther. (2016) 53:178–206. doi: 10.1093/jmt/thw004
33. Bradt J, Teague A. Music interventions for dental anxiety. Oral Dis. (2018) 24(3):300–6. doi: 10.1111/odi.12615
34. Mitchell LA, MacDonald RA. An experimental investigation of the effects of preferred and relaxing music listening on pain perception. J Music Ther. (2006) 43(4):295–316. doi: 10.1093/jmt/43.4.295
35. Good M, Picot BL, Salem SG, Chin CC, Picot SF, Lane D. Cultural differences in music chosen for pain relief. J Holist Nurs. (2000) 18(3):245–60. doi: 10.1177/089801010001800306
36. Hamburg MA, Collins FS. The path to personalized medicine. N Engl J Med. (2010) 363(4):301–4. doi: 10.1056/NEJMp1006304
37. Grau-Sanchez J, Jamey K, Paraskevopoulos E, Dalla Bella S, Gold C, Schlaug G, et al. Putting music to trial: consensus on key methodological challenges investigating music-based rehabilitation. Ann N Y Acad Sci. (2022) 1518:12–24. doi: 10.1111/nyas.14892
38. Martin-Saavedra JS, Vergara-Mendez LD, Pradilla I, Velez-van-Meerbeke A, Talero-Gutierrez C. Standardizing music characteristics for the management of pain: a systematic review and meta-analysis of clinical trials. Complement Ther Med. (2018) 41:81–9. doi: 10.1016/j.ctim.2018.07.008
39. World Health Organization. Towards a digital health roadmap for the WHO European Region. World Health Organization (2019). Available at: https://www.euro.who.int.
40. Guetin S, Soua B, Voiriot G, Picot MC, Herisson C. The effect of music therapy on mood and anxiety-depression: an observational study in institutionalised patients with traumatic brain injury. Ann Phys Rehabil Med. (2009) 52(1):30–40. doi: 10.1016/j.annrmp.2008.08.009
41. Guetin S, Coudeyre E, Picot MC, Ginies P, Graber-Duvernay B, Ratsimba D, et al. Effect of music therapy among hospitalized patients with chronic low back pain: a controlled, randomized trial. Ann Readapt Med Phys. (2005) 48(5):217–24. doi: 10.1016/j.annrmp.2005.02.003
42. Guetin S, Ginies P, Siou DK, Picot MC, Pommie C, Guldner E, et al. The effects of music intervention in the management of chronic pain: a single-blind, randomized, controlled trial. Clin J Pain. (2012) 28(4):329–37. doi: 10.1097/AJP.0b013e31822be973
43. Mercadie L, Mick G, Guetin S, Bigand E. Effects of listening to music versus environmental sounds in passive and active situations on levels of pain and fatigue in fibromyalgia. Pain Manag Nurs. (2015) 16(5):664–71. doi: 10.1016/j.pmn.2015.01.005
45. Hevner K. Experimental studies of the elements of expression in music. Am J Psychol. (1936) 48(2):246. doi: 10.2307/1415746
46. Tousignant-Laflamme Y, Page S, Goffaux P, Marchand S. An experimental model to measure excitatory and inhibitory pain mechanisms in humans. Brain Res. (2008) 1230:73–9. doi: 10.1016/j.brainres.2008.06.120
47. Ocay DD, Ye DL, Larche CL, Potvin S, Marchand S, Ferland CE. Clusters of facilitatory and inhibitory conditioned pain modulation responses in a large sample of children, adolescents, and young adults with chronic pain. Pain Rep. (2022) 7(6):e1032. doi: 10.1097/PR9.0000000000001032
48. Potvin S, Marchand S. Pain facilitation and pain inhibition during conditioned pain modulation in fibromyalgia and in healthy controls. Pain. (2016) 157(8):1704–10. doi: 10.1097/j.pain.0000000000000573
49. Sutton KS, Pukall CF, Chamberlain S. Diffuse noxious inhibitory control function in women with provoked vestibulodynia. Clin J Pain. (2012) 28(8):667–74. doi: 10.1097/AJP.0b013e318243ede4
51. Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol Methods. (1996) 1:16–29. doi: 10.1037/1082-989X.1.1.16
52. Gupta SK. Intention-to-treat concept: A review. Perspect Clin Res. (2011) 2(3):109–12. doi: 10.4103/2229-3485.83221
53. Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P, Group CN. CONSORT statement for randomized trials of nonpharmacologic treatments: a 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med. (2017) 167(1):40–7. doi: 10.7326/M17-0046
54. Khirasaria R, Singh V, Batta A. Exploring digital therapeutics: The next paradigm of modern health-care industry. Perspect Clin Res. (2020) 11(2):54–8. doi: 10.4103/picr.PICR_89_19
55. Howlin C, Stapleton A, Rooney B. Tune out pain: agency and active engagement predict decreases in pain intensity after music listening. PLoS One. (2022) 17(8):e0271329. doi: 10.1371/journal.pone.0271329
56. Lunde SJ, Vuust P, Garza-Villarreal EA, Kirsch I, Moller A, Vase L. Music-induced analgesia in healthy participants is associated with expected pain levels but not opioid or dopamine-dependent mechanisms. Front Pain Res. (2022) 3:734999. doi: 10.3389/fpain.2022.734999
57. Zajonc RB. Attitudinal effects of mere exposure. J Pers Soc Psychol. (1968) 9:1–27. doi: 10.1037/h0025848
58. Cassidy GG, Macdonald RA. The effects of music on time perception and performance of a driving game. Scand J Psychol. (2010) 51(6):455–64. doi: 10.1111/j.1467-9450.2010.00830.x
59. Sullivan MJ, Rodgers WM, Kirsch I. Catastrophizing, depression and expectancies for pain and emotional distress. Pain. (2001) 91(1-2):147–54. doi: 10.1016/S0304-3959(00)00430-9
60. Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med. (2004) 66(1):17–22. doi: 10.1097/01.PSY.0000106883.94059.C5
61. Ploghaus A, Narain C, Beckmann CF, Clare S, Bantick S, Wise R, et al. Exacerbation of pain by anxiety is associated with activity in a hippocampal network. J Neurosci. (2001) 21(24):9896–903. doi: 10.1523/JNEUROSCI.21-24-09896.2001
62. McCaul KD, Malott JM. Distraction and coping with pain. Psychol Bull. (1984) 95(3):516–33. doi: 10.1037/0033-2909.95.3.516
63. Leventhal H. I know distraction works even though it doesn't!. Health Psychol. (1992) 11(4):208–9. doi: 10.1037/h0090350
64. Guetin S, De Diego E, Mohy F, Adolphe C, Hoareau SG, Touchon J, et al. A patient-controlled, smartphone-based music intervention to reduce pain—a multi-center observational study of patients with chronic pain. Eur J Integr Med. (2016) 8:182–7. doi: 10.1016/j.eujim.2016.01.002
65. Nilsson U. The anxiety- and pain-reducing effects of music interventions: a systematic review. AORN J. (2008) 87(4):780–807. doi: 10.1016/j.aorn.2007.09.013
66. Siedliecki SL, Good M. Effect of music on power, pain, depression and disability. J Adv Nurs. (2006) 54(5):553–62. doi: 10.1111/j.1365-2648.2006.03860.x
Keywords: music, pain, digital therapeutics, experimental pain in humans, adult, endogenous pain modulation, conditioned pain modulation
Citation: Soyeux O and Marchand S (2023) A web app-based music intervention reduces experimental thermal pain: A randomized trial on preferred versus least-liked music style. Front. Pain Res. 3:1055259. doi: 10.3389/fpain.2022.1055259
Received: 27 September 2022; Accepted: 5 December 2022;
Published: 16 January 2023.
Edited by:
Xuejing Lu, Chinese Academy of Sciences (CAS), ChinaReviewed by:
Cheng-Hao Tu, China Medical University, TaiwanAnna Woodbury, Emory University, United States
© 2023 Soyeux and Marchand. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Serge Marchand serge.marchand@usherbrooke.ca
Specialty Section: This article was submitted to Pain Mechanisms, a section of the journal Frontiers in Pain Research
 Orelle Soyeux
Orelle Soyeux Serge Marchand
Serge Marchand