New insights into metabolic dysfunction-associated steatotic liver disease and oxidative balance score
- 1Department of Gastroenterology, First Affiliated Hospital of Nanjing Medical University, Nanjing, China
- 2Department of Endocrinology, Children's Hospital of Nanjing Medical University, Nanjing, China
Background: The relationship between oxidative stress and metabolic dysfunction-associated steatotic liver disease (MASLD) has not been studied, which remains inadequately recognized. This is a cross-sectional study in a US adult population to explore the relationship between MASLD and oxidative balance scores (OBS), which containing integrating dietary nutrition and lifestyle factors.
Methods: We analyzed data from National Health and Nutrition Examination Survey during 2017–2018. Multivariate logistic regression, restricted cubic spline curve (RCS) and subgroup analysis were used to investigate the association between OBS and MASLD. Cox regression analysis was utilized to assess the association between OBS and all-cause mortality among individuals.
Results: The multivariable-adjusted odds ratio (OR) and 95% confidence interval (CI) for the highest quartile of OBS (Q4) was 0.30 (0.12, 0.77) (p = 0.012) compared to the lowest quartile of OBS (Q1). The RCS regression and subgroup analysis indicated an inverted relationship between OBS and the development of MASLD. The OBS Q4 group (HR: 0.15, 95% CI: 0.03–0.87; p = 0.035) exhibited a lower risk of all-cause death than the Q1 group.
Conclusion: OBS is statistically significantly and negatively correlated with the risk of MASLD and all-cause mortality in US adults. More prospective investigations are required to substantiate our findings.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a clinically common chronic liver disease that pathologically manifests as excessive lipid deposition in liver parenchymal cells (1). With changing lifestyles, NAFLD is becoming prevalent worldwide, and approximately 25% of adults are affected by this disease (2, 3). NAFLD can progress to the development of severe hepatic disease or even liver cell carcinoma, with a lack of effective treatment and a poor prognosis at late stages (4). NAFLD has an indisputable onset and is often asymptomatic in its early stages and is often not appreciated; therefore, early prevention, diagnosis and intervention of NAFLD are needed to slow its progression (5). Following the Delphi Consensus process, the term “metabolic dysfunction-associated steatohepatitis” (MASLD) became the successor to the term “NAFLD” (6) to enhance the precision of nomenclature.
MASLD is a highly heterogeneous disease in which multiple factors, such as genetics, environment, aging, and poor dietary practice, especially the over-intake of high-calorie diets abundant in saturated fatty acids or simple carbohydrates, may be involved in its pathophysiological mechanisms (7). Thus, changing dietary behavior and diet structure is a feasible strategy for the prevention and treatment of MASLD (8). It has been shown that changes in oxidative stress indicators occur in patients with NAFLD, including elevated oxidative stress marker 8-oxo-dG (9) and decreased coenzyme Q10 (10), suggesting that oxidative stress may exert an essential part in the pathophysiological process of MASLD. Therefore, antioxidants in food, including certain antioxidant vitamins and micronutrients, exhibit some antioxidant stress activity and may be effective in preventing and treating MASLD (11, 12). Although studies have shown a relationship between oxidative stress-related nutrients/foods and MASLD, it is possible that dietary interfactions may interfere with the effectiveness of integrated nutrients (13). Therefore, a new strategy based on dietary models related to oxidative and antioxidant modification is needed.
The oxidative balance score (OBS) evaluates an individual’s level of oxidative stress by integrating dietary nutrition and lifestyle (14). The OBS was first proposed in 2002 in an epidemiologic study of a Belgian male smoking population, which used vitamin C and β-carotene as the antioxidant constituents and iron as the pro-oxidant constituent and showed that the lower the OBS score was, the higher the level of oxidative homeostasis in an individual, indicating that the lower the oxidative homeostasis score was, the higher the mortality rate in the population (15). Thereafter, numerous studies were conducted to investigate the relationship between OBS and a wide range of chronic disorders, such as type 2 diabetes mellitus (16), cardiovascular disease (17), and colorectal cancer (18). Recently, a study conducted in Iran showed that the greater the adherence to an OBS, the lower the odds of developing NAFLD (19).
Therefore, cross-sectional research based on the 2017–2018 National Health and Nutrition Examination Survey (NHANES) was carried out to evaluate the association between OBS and the degree of hepatosteatosis as measured by quantification of vibration-controlled transient elastography (VCTE) in US adults.
Materials and methods
Study design and data source
The current study is a retrospective, cross-sectional, population-based analysis of data extracted from the 2017–2018 US National Health and Nutrition Examination Survey (NHANES) database, which is intended to provide an assessment of the dietary state of health and nutrition using a sophisticated, multiphasic design to collect and analyze data that are representative of the nation as a whole. An extensive assessment process was required for participants, including a household interview and a mobile examination center (MEC) visit, which consisted of a medical physical examination, specialized measurements, and laboratory tests (20). In this study, liver ultrasound transient elastography (TE) examinations were first used, and participants supplied two 24-h periods of detailed dietary intake information, subsequently used to estimate energy, nutrient and other food component intake. Initial dietary memories were collected over the course of the NHANES visit, and the subsequent ones were gathered over the phone 3–10 days afterwards.
Study population
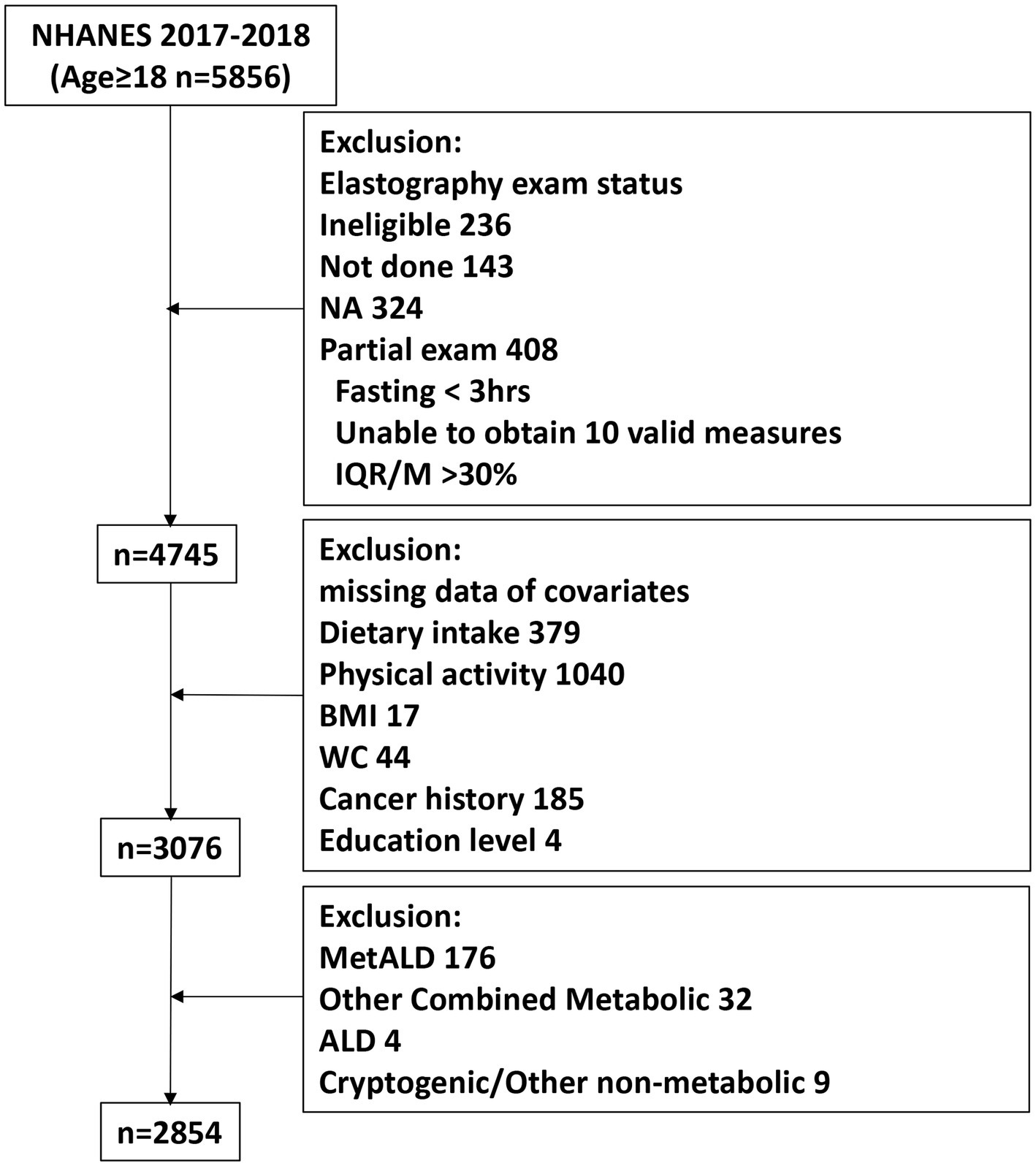
The present study was originally comprised of 5,856 participants aged ≥18 years. Of these, 4,745 underwent complete elastography. In addition, participants with the following conditions were excluded: (1) missing data (dietary intake information, exercise data, body mass index, waist circumference, cancer history, and education level);(2) MASLD with increased alcohol intake (MetALD), defined as a daily intake of 20–50 g of alcohol for females and 30–60 g daily for males; (3) alcoholic liver disease (ALD), defined as a daily intake of more than 50 g of alcohol for females and more than 60 g daily for males; (4) other underlying etiologies of hepatic disease. Finally, we recruited 2,854 participants in this study (Figure 1).
Study variables
Measurement of MASLD, MASH and liver fibrosis
The severity of liver steatosis was evaluated by the controlled attenuation parameter (CAP) derived from FibroScan®, which is available at the Mobile Examination Center (MEC) using vibration-controlled transient elastography (VCTE) technology (21). According to a previous study, the definition of SLD is a median CAP ≥263 dB/m (22). The SLD participants meet one of the 5 cardiometabolic risk factors as suggested on the recent Delphi consensus statement (23) and excluded MetALD, ALD, underlying etiologies of hepatic disease were defined as MASLD. The definition we used to classify metabolic dysfunction-associated steatohepatitis (MASH) is ALT >25 U/L or AST > 25 U/L on the basis of MASLD (24). Liver stiffness measurements (LSM) determined clinically significant and advanced fibrosis with cut-offs of 8.6 kPa and 13.1 kPa based on Youden’s study, respectively (25).
Oxidative balance score
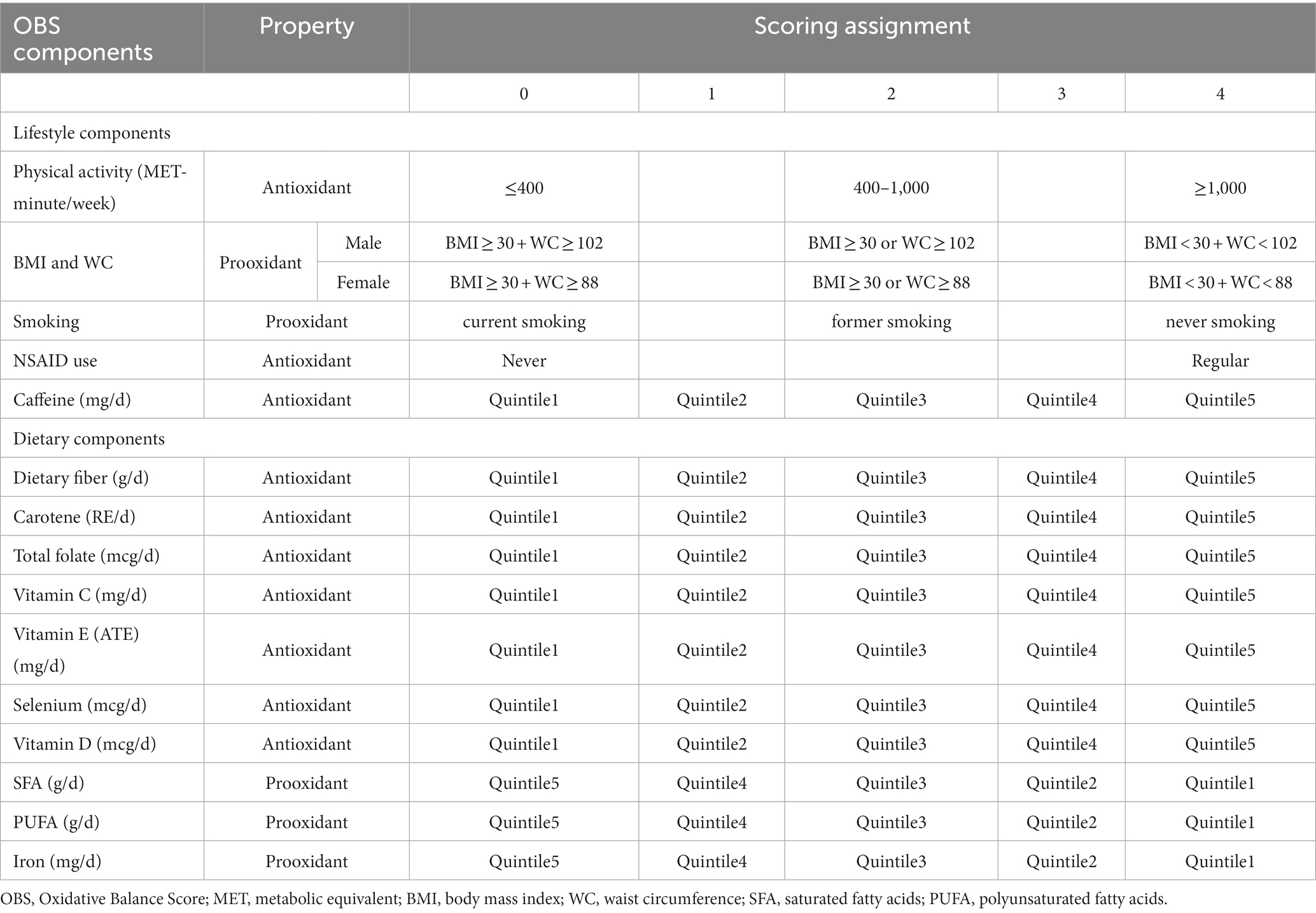
In the present study, we obtain the OBS for each individual participant. According to Azita’s study (19), we selected 10 dietary components (selenium, fiber, β-carotene, folic acid, iron, vitamin D, vitamin C, vitamin E, saturated fatty acids, and polyunsaturated fatty acids) and lifestyle components (physical activity, smoking and obesity) for their association with oxidative stress (Table 1). Besides, the coffee/tea consumption and non-steroidal anti-inflammatory drug (NSAID) using participant as important modulator of oxidant balance (26, 27), we added them to the lifestyle components. The dietary components were categorized into quintiles. In the case of dietary antioxidants, the first through fifth quintiles were scored as 0–4. A reversed scoring method was used for dietary pro-oxidants. For NSAID using, we assigned 0: never, 4: regular user. For physical activity, we assigned 0: MET-minute/week≤400, 2: 400 < MET-minute/week ≤1000, and 4: MET-minute/week>1,000. For BMI and WC, we gave the following scores: 0 for BMI ≥ 30 kg/m2 and male WC ≥ 102 cm/female WC ≥ 88 cm; 2 for BMI ≥ 30 kg/m2 or male WC ≥ 102 cm/female WC ≥ 88 cm; and 4 for BMI < 30 kg/m2 and male WC < 102/female WC < 88 cm. With regard to smoking, the scale was as follows: 0 for current smoker (smoked >100 cigarettes in a lifetime and smoked on several days or every day), 2 for ex-smoker (smoked >100 cigarettes in a lifetime and currently do not smoke), and 4 for never smoker (smoked <100 cigarettes in a lifetime). The scores were then added together to calculate the OBS for each subject.
Covariables
Drawing on existing publications and clinical considerations, a selection of covariates that may serve as potential confounders in the relationship between OBS and MASLD was made. Through standardized household interviews, we obtained demographic features, including age, gender, ethnicity, educational level, and financial condition. Educational level was classified into several categories: below high school, high school graduate/GED or equivalent, and college or above. Financial condition was categorized as low (PIR ≤ 1.0), medium (1 < PIR ≤ 4), and high (PIR > 4). To be evaluated for diabetes, subjects were required to fulfill one of the following criteria: (1) history of insulin use, (2) clinically previous diagnosis of diabetes, (3) taking glucose-lowering medication, and (4) laboratory data HbA1c ≥ 6.5% and fasting blood glucose ≥126 mg/dL (28). Inclusion criteria for hypertensive patients were as follows: (1) Subjects were required to answer at least one of the following questions by answering “(1) Be ever told on two or more occasions that they have hypertension or (2) Whether they have ever been told about their hypertension and taken prescribed medication” and obtaining at least one affirmative answer. (2) Subjects were identified as having hypertension by a clinical measurement of blood pressure with a mean of three consecutive systolic blood pressure measurements ≥140 mmHg or a mean of three consecutive diastolic blood pressure measurements ≥90 mmHg. Multiple imputation was performed by R for missing covariables measured at the baseline visit according to a previous study (29).
Statistical analysis
We used weighted samples, strata, and subgroups from the NHANES database and calculated weighted populations for this research using the SURVEY program in SAS. Continuous variables were presented in the form of weighted means and standard errors, with categorical variables presented in the form of unweighted numbers and weighted proportions. We performed logistic regression analysis using SURVEYLOGISTIC statements to examine the relationship between OBS and MASLD. We performed multivariate regression analyses to adjust for potential confounders identified in single-variable regressions, consisting of age in years, sex, race, education level, and comorbidities (history of diabetes, hypertension, and cancer). Statistical analyses of categorical variables were performed using weighted χ2 tests, and analyses of continuous variables were performed using weighted linear regression models to identify between-group differences. Stratified multivariate regression analysis was used for subgroup analysis. It is also recommended to use the RCS function when adjusting for continuous exposure to minimize residual confounding (30). In this study, a RCS model with four nodes was used to investigate the relationship between OBS and MASLD prior to and after adjustment for confounders. All analyses were performed using the R program and EmpowerStats. p values less than 0.05 were considered statistically significant.
Results
Participant characteristics
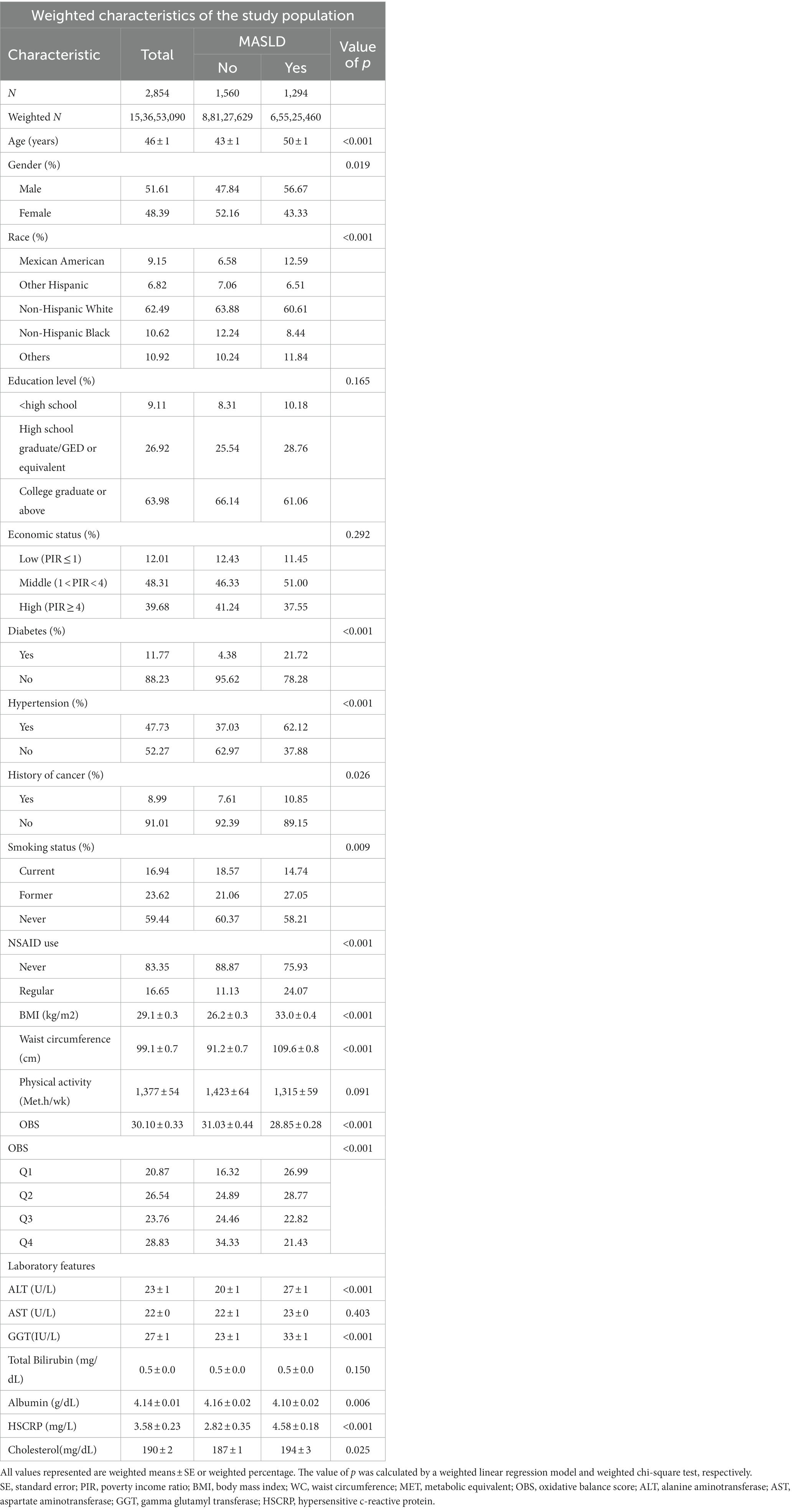
A total of 2,854 participants from NHANES (2017–2018) were included in this study, of whom 1,294 (45.34%) were diagnosed with MASLD based on a previous study. Among all participants with MASLD, the prevalence was higher in males (56.67%) than in females (43.33%) (p = 0.019). Patients who had MASLD were much older and were more likely to be non-Hispanic white, with no differences in educational attainment or income between these two groups (Table 2). Baseline comparison of characteristics indicated that patients with MASLD had a greater prevalence of diabetes mellitus (21.72% vs. 4.38%, p < 0.001), hypertension (62.12% vs. 37.03%, p < 0.001), and smoking (41.79% vs. 39.63%, p = 0.009). The MASLD patients also had higher BMIs and waist circumferences. Participants without MASLD had significantly greater OBS (p < 0.001) in comparison to participants suffering from MASLD. Comparing laboratory characteristics, we found that ALT, GGT, HSCRP, and cholesterol were significantly higher in the MASLD group, while serum albumin was significantly lower (Table 2). When we separate the MASLD into MASH and MASLD1(MASLD without MASH)(27.44%) based on ALT and AST, the incidence of MASH was 17.90%. The OBS was decreased in MASH group (Supplementary Table S1). However, when compared participants with clinically significant fibrosis (12.75%) and advanced fibrosis (3.63%) to non-fibrosis, OBS showed no difference in the population (p = 0.237) (Supplementary Table S2).
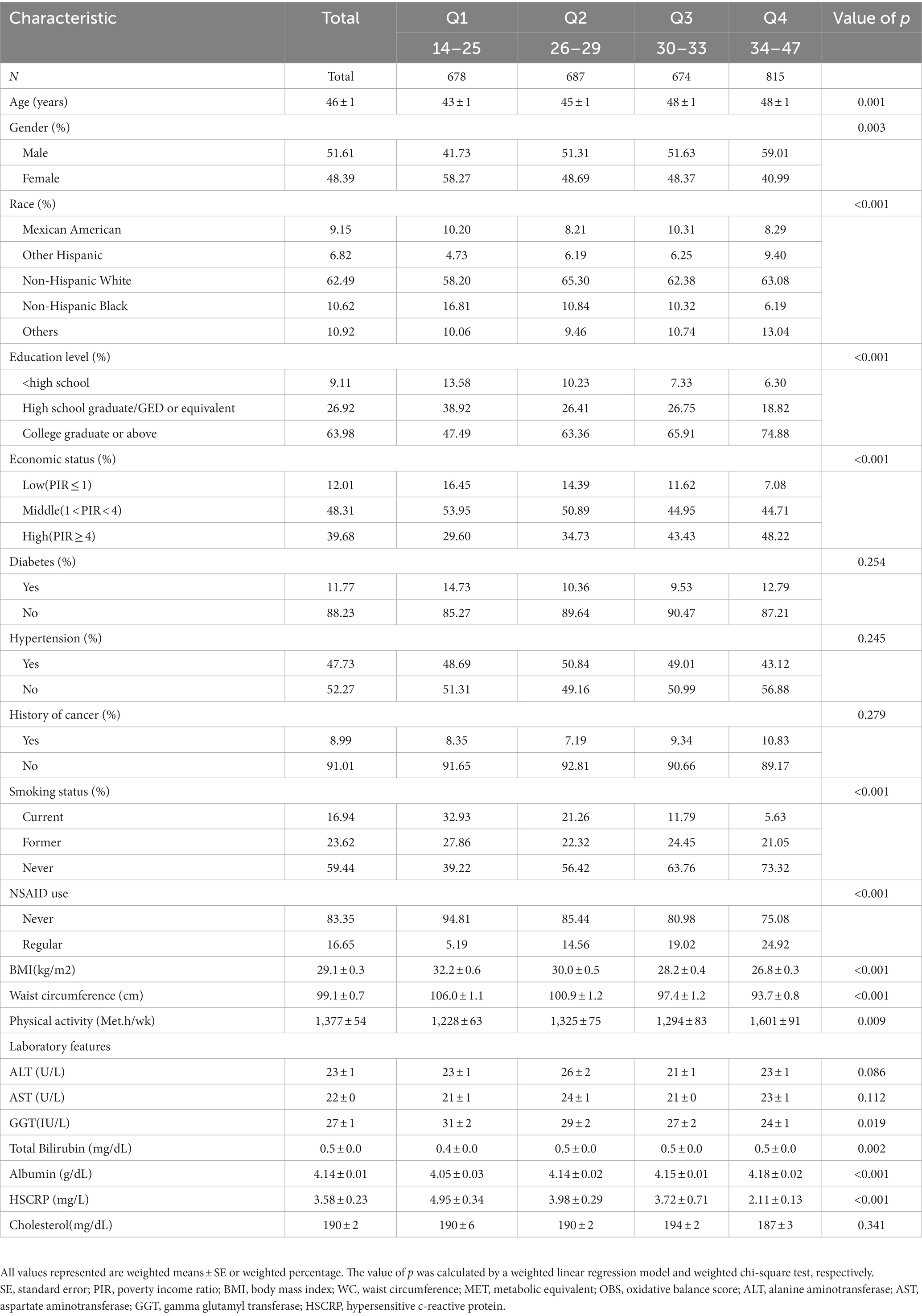
Then, all 2,854 individuals were divided into four groups based on OBS quartiles: group 1 (OBS Q1, OBS: 14 to 25), group 2 (OBS Q2, OBS: 26 to 29), group 3 (OBS Q3, OBS: 30 to 33), and group 4 (OBS Q4, OBS: 34 to 47). Individuals in the 1st quartile (Q1) with lower OBS (as a reference group) were more likely to be younger, women, white, less educated, and with less income. Furthermore, participants in Q1 were more likely to smoke and be less physically active. As OBS quartiles progressively increase, BMI progressively decreases. Compared with those in the lowest quartile of OBS, subjects in the highest quartile had lower levels of GGT, HSCRP and higher level of albumin (Table 3). Serum GGT (31) and albumin (32) are considered prooxidant and antioxidant indicators in previous studies, respectively. From OBS Q1 to Q4, GGT gradually decreased (p = 0.019) and albumin gradually increased (p < 0.001).
Relationship between OBS and MASLD/liver fibrosis
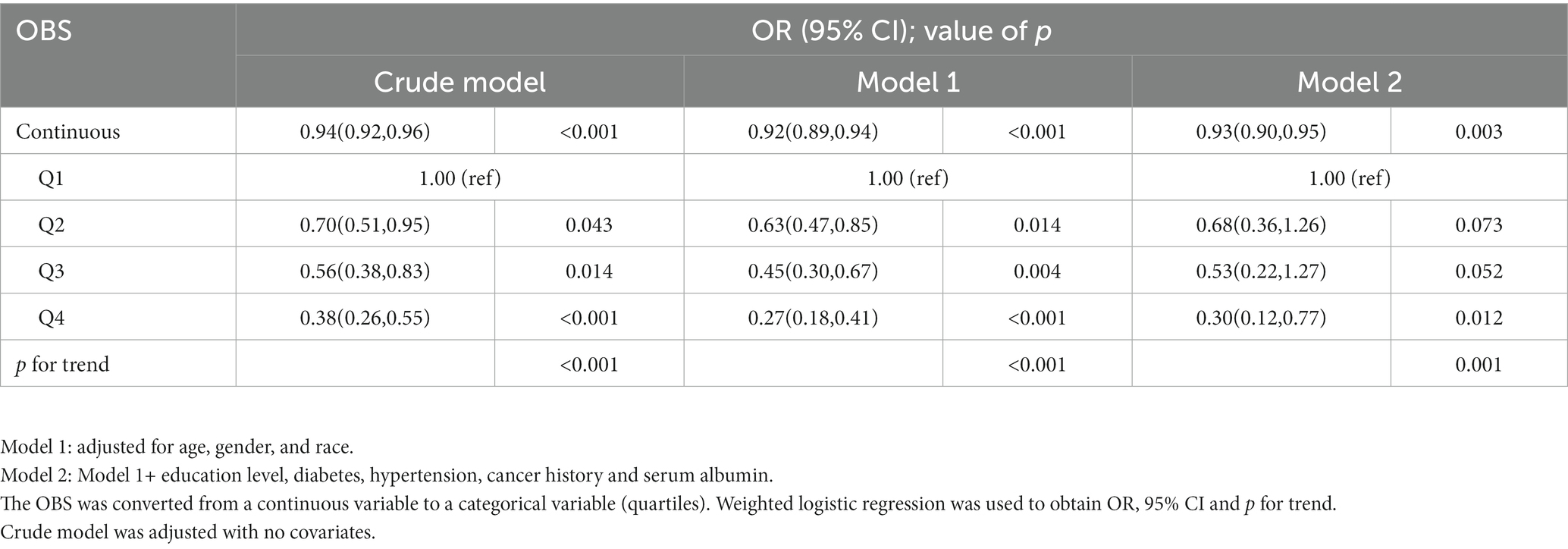
Multivariate logistic regression indicated that OBS was statistically correlated with MASLD (Table 4). In model 2, we found that each 1-unit increase in OBS resulted in a 7% reduction in the risk of MASLD (OR = 0.93, 95% confidence interval (CI) 0.90–0.95), suggesting that OBS was negatively associated with the risk of MASLD. In the crude model and model 1, the highest quartile was significantly associated with MASLD compared with the lowest quartile (p for trend<0.001, <0.001). In addition, adherence to the 4th quartile of OBS was also found to be correlated with MASLD after adjusting for confounders in model 2 (OR = 0.30, 95% CI 0.12–0.77; p = 0.012, p for trend = 0.001). However, OBS (continuous and categorical) was not associated with the risk of clinically significant fibrosis and advanced fibrosis in the all models (Supplementary Table S3).
Subgroup analysis
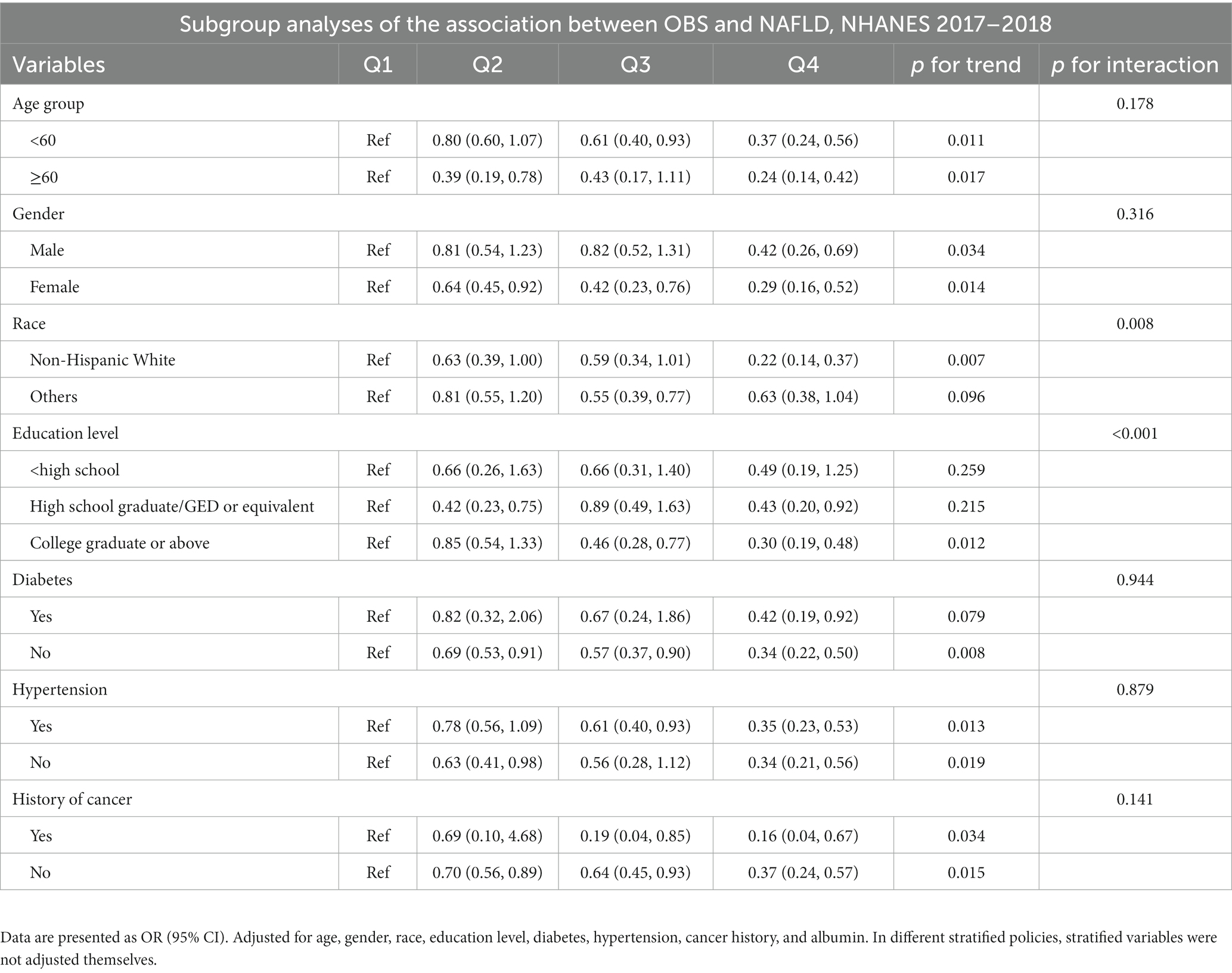
Group analyses were performed based on age, gender, race, education level, and history of diabetes, hypertension and cancer (Table 5). Regarding the race and education subgroup, statistical significance was found (interaction p = 0.008 and < 0.001). When stratified by race, among non-Hispanic whites, we found that OBS was associated with a lower prevalence of MASLD, whereas in other races, this trend was less pronounced than that in non-Hispanic whites. When considering education level, the negative association between OBS and MASLD was more pronounced among those with college or higher education. However, age stratification, gender subgroup, history of diabetes, HBP, and cancer had no significant effect on the results of the analysis (Table 5).
RCS analysis
We further assessed the relationship between OBS and MASLD with the use of RCS curves and multivariate logistic regression. We identified a nonlinear association between OBS and MASLD (nonlinear p = 0.315, 0.256, 0.077) in crude models, model 1 and model 2, respectively (Figure 2). We detected that the risk of MASLD gradually decreased as OBS increased.
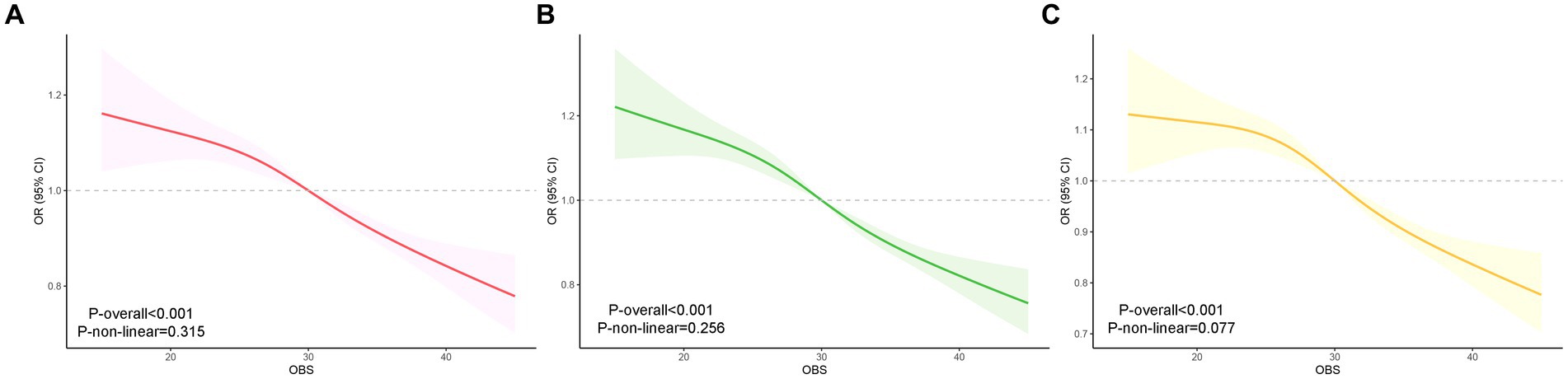
Figure 2. RCS analysis of the association between OBS and MASLD. Crude model was adjusted with no covariates. Model 1: adjusted for age, gender and race. Model 2: in addition to the variables in Model 1, education level, diabetes, hypertension, cancer history, and albumin were added. RCS curve of the association between OBS and MASLD of crude model (A), Model 1 (B) and Model 2 (C). RCS, restricted cubic spline.
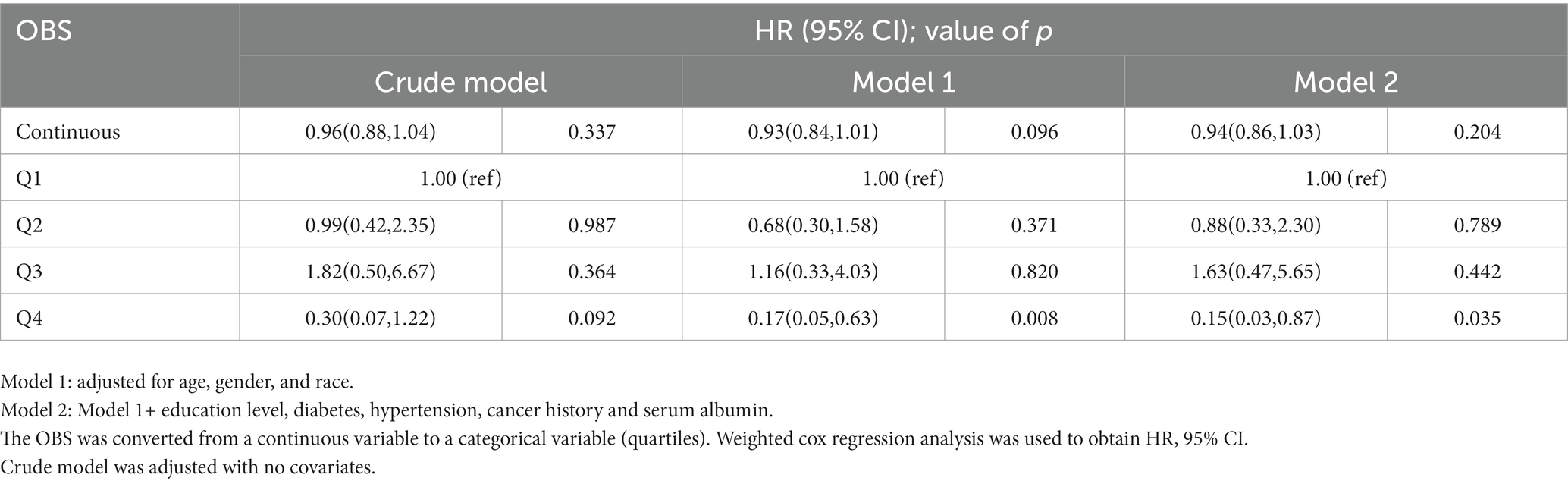
Correlation between OBS and all-cause mortality
The relationship between OBS and all-cause mortality was further assessed by Cox proportional hazards models. We found that continuous OBS resulted in an 6% reduction in the risk of all-cause mortality (OR = 0.94, 95% CI 0.86–1.03; p = 0.204). While OBS was assessed as a categorical variable, after adjusting for covariables, the OBS Q4 group (HR: 0.15, 95% CI: 0.02–0.87; p = 0.035) exhibited a lower risk of all-cause mortality than the OBS Q1 group in all participants (Table 6). When adjusting for liver fibrosis, the lower risk of all-cause mortality in OBS Q4 group still exist (Supplementary Table S4), which means mortality risk might be indirectly affected by OBS itself rather than the level of fibrosis.
Discussion
We assessed the association between OBS and MASLD in this large cross-sectional study on the basis of NHANES (ranging from 2017 to 2018). A 15-component-based OBS was used to extensively evaluate exposure through dietary and lifestyle-related exposure to antioxidant and pro-oxidant components, which allowed us to adequately evaluate the complexity of oxidative homeostasis in individuals. We demonstrated in this study that participants without MASLD had significantly higher OBS than those with MASLD. After adjusting for confounders, the effect of OBS on MASLD was shown to be significantly dependent on race and education level.
Extensive studies have suggested that impaired oxidative stress is associated with the occurrence and progression of MASLD/MASH through the overproduction of reactive oxygen species (ROS) to mediate lipid metabolism, insulin signaling, and innate immune signaling pathways (33–35). Either pro-oxidants or antioxidants may act antagonistically or synergistically, while antioxidants may be pro-oxidants at high doses (36). In addition, supplementation with a multitude of dietary antioxidants (vitamin E, vitamin C), as well as lifestyle changes (exercise) may improve clinical markers in part by reducing oxidative stress in NAFLD patients (37). Consequently, there is a need for a comprehensive assessment of index-OBS to evaluate oxidative balance in individuals and to investigate the impact of this balance on MASLD. Prior investigations have examined the potential benefit of this index on NAFLD through inflammation, oxidative stress, and glycolipid metabolism (38). By the way, OBS is not associated with progression of liver fibrosis. A randomized controlled clinical trial showed that vitamin E was associated with improvement in NAFLD but not liver fibrosis (39), while other studies have found that antioxidants are associated with improved fibrosis in NAFLD patients (40, 41). The reason for this consideration may be that OBS is a composite index that includes pro-oxidants and antioxidants, and therefore its combined effect cannot be explained by the alleviation of fibrosis by antioxidants alone.
The traditional OBS contains 20 items related to oxidative stress (16), but a recent study on OBS in NAFLD contained only 13 items (19). In our study, we calculated OBS contained 13 items and added caffeine intake and NSAID using to get a new OBS. In addition, there is evidence suggesting that micronutrients such as vitamins, selenium, carotenoids, and magnesium, which have antioxidant, immunomodulatory, and lipoprotective properties, may play protective roles in NAFLD (42). Polyunsaturated fatty acids (PUFA) are susceptible to lipid peroxidation implicated in NAFLD, while vitamin E has been shown to protect against non-enzymatic lipid peroxidation (43). The accumulation of excess saturated fatty acids (SFA) induces cellular lipotoxic damage and increases the risk of MASLD (44). In our study, the lower intake of antioxidant properties (carotene, vitamin C and vitamin E) and higher intake of prooxidant properties (SFA, PUFA) could be associated with the onset of MASLD. It is important that n-3 and n-6 PUFA have a differing role in oxidative stress. The n-3 PUFA have been shown to be antioxidative. However, higher intakes of n-6 PUFAS have been associated with an increased oxidative stress (45). It’s a limitation that we did not categorize PUFAs into n-3 PUFAs and n-6 PUFAs to calculate OBS.
According to our study, lifestyle may have a significant impact on the development of MASLD. In addition to dietary nutrients, there is an important role of a healthy lifestyle in avoiding MASLD. Physical activity, body mass index control and smoking cessation might be effective, which is consistent with previous studies showing the impact of obesity, sedentary lifestyle, smoking and other individual variables and situational factors on NAFLD (46). Studies showed that caffeine could improved fatty liver in ApoE KO mice with NAFLD in vivo (47) and NSAID-activated gene-1 (NAG-1), or growth differentiation factor-15 (GDF15), is associated with NAFLD (48). This is the first study to identify OBS included caffeine intake and NSAID as a MASLD protective factor in US adults and find a significant negative association between OBS and MASLD.
The study has both strengths and weaknesses. First, this is the first study evaluating the relationship between OBS and MASLD in US adults. Second, based on the stratified and multistage nature of the NHANES data, our findings have a high generalization among the mobile community. Third, we endeavored to account for various confounders through the use of a questionnaire and massive adjustment for variables. However, there are some limitations to this study. The present study could not effectively assess causality in the nature of the cross-sections. Although we controlled for potential confounders, we still cannot rule out the effect of unknown indexes. Another weakness of this study may be that no examination of alcohol intake was performed. However, since heavy drinkers were excluded, examination of this component was unlikely to influence the outcomes. Further validation of the predictive value of OBS for MASLD through prospective studies is needed to improve the utility of our findings.
Conclusion
To summarize, it is suggested in this cross-sectional study that OBS is negatively associated with the incidence of MASLD and all-cause mortality in US adults. An negative association was observed between OBS and the prevalence of MASLD in a nationally representative sample of adults in the United States. Our findings confirm the role of healthy food and lifestyle choices in the prevention of MASLD. In addition, they can be used as a strategy to arrest the course of MASLD.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by National Health and Nutrition Examination Survey. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LP: Conceptualization, Formal analysis, Funding acquisition, Validation, Visualization, Writing – original draft, Writing – review & editing. LL: Formal analysis, Investigation, Methodology, Validation, Writing – original draft. JL: Investigation, Software, Validation, Writing – original draft. YL: Conceptualization, Data curation, Funding acquisition, Project administration, Resources, Supervision, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Nature Science Foundation of China (Nos. 82100595 and 82100712) and the Natural Science Foundation of Jiangsu Province (No. BK20210958).
Acknowledgments
The authors are grateful to NCHS for research design and data sharing and to all the researchers and participants in this cross-sectional study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1320238/full#supplementary-material
References
1. Gan, L, Feng, Y, Du, B, Fu, H, Tian, Z, Xue, G, et al. Bacteriophage targeting microbiota alleviates non-alcoholic fatty liver disease induced by high alcohol-producing Klebsiella pneumoniae. Nat Commun. (2023) 14:3215. doi: 10.1038/s41467-023-39028-w
2. Araujo, AR, Rosso, N, Bedogni, G, Tiribelli, C, and Bellentani, S. Global epidemiology of non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: what we need in the future. Liver Int. (2018) 38:47–51. doi: 10.1111/liv.13643
3. Younossi, Z, Anstee, QM, Marietti, M, Hardy, T, Henry, L, Eslam, M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. (2018) 15:11–20. doi: 10.1038/nrgastro.2017.109
4. Chen, K, Ma, J, Jia, X, Ai, W, Ma, Z, and Pan, Q. Advancing the understanding of NAFLD to hepatocellular carcinoma development: from experimental models to humans. Biochim Biophys Acta Rev Cancer. (2019) 1871:117–25. doi: 10.1016/j.bbcan.2018.11.005
5. Younossi, ZM, Blissett, D, Blissett, R, Henry, L, Stepanova, M, Younossi, Y, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. (2016) 64:1577–86. doi: 10.1002/hep.28785
6. Rinella, ME, Lazarus, JV, Ratziu, V, Francque, SM, Sanyal, AJ, Kanwal, F, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. (2023) 79:1542–56. doi: 10.1016/j.jhep.2023.06.003
7. Giraldi, L, Miele, L, Aleksovska, K, Manca, F, Leoncini, E, Biolato, M, et al. Mediterranean diet and the prevention of non-alcoholic fatty liver disease: results from a case-control study. Eur Rev Med Pharmacol Sci. (2020) 24:7391–8. doi: 10.26355/eurrev_202007_21907
8. De Nucci, S, Bonfiglio, C, Donvito, R, Di Chito, M, Cerabino, N, Rinaldi, R, et al. Effects of an eight week very low-calorie ketogenic diet (VLCKD) on white blood cell and platelet counts in relation to metabolic dysfunction-associated Steatotic liver disease (MASLD) in subjects with overweight and obesity. Nutrients. (2023) 15:4468. doi: 10.3390/nu15204468
9. Hamaguchi, K, Miyanishi, K, Osuga, T, Tanaka, S, Ito, R, Sakamoto, H, et al. Association between hepatic oxidative stress related factors and activation of Wnt/beta-catenin signaling in NAFLD-induced hepatocellular carcinoma. Cancers. (2022) 14:14. doi: 10.3390/cancers14092066
10. Ivan, L, Uyy, E, Suica, VI, Boteanu, RM, Cerveanu-Hogas, A, Hansen, R, et al. Hepatic Alarmins and mitochondrial dysfunction under residual Hyperlipidemic stress Lead to irreversible NAFLD. J Clin Transl Hepatol. (2023) 11:284–94. doi: 10.14218/JCTH.2022.00128
11. Oliveira, CP, Gayotto, LC, Tatai, C, Della, NB, Lima, ES, Abdalla, DS, et al. Vitamin C and vitamin E in prevention of nonalcoholic fatty liver disease (NAFLD) in choline deficient diet fed rats. Nutr J. (2003) 2:9. doi: 10.1186/1475-2891-2-9
12. Ipsen, DH, Tveden-Nyborg, P, and Lykkesfeldt, J. Does vitamin C deficiency promote fatty liver disease development? Nutrients. (2014) 6:5473–99. doi: 10.3390/nu6125473
13. Meydani, M . Dietary antioxidants modulation of aging and immune-endothelial cell interaction. Mech Ageing Dev. (1999) 111:123–32. doi: 10.1016/S0047-6374(99)00067-6
14. Liu, X, Liu, X, Wang, Y, Zeng, B, Zhu, B, and Dai, F. Association between depression and oxidative balance score: National Health and nutrition examination survey (NHANES) 2005–2018. J Affect Disord. (2023) 337:57–65. doi: 10.1016/j.jad.2023.05.071
15. Van Hoydonck, PG, Temme, EH, and Schouten, EG. A dietary oxidative balance score of vitamin C, beta-carotene and iron intakes and mortality risk in male smoking Belgians. J Nutr. (2002) 132:756–61. doi: 10.1093/jn/132.4.756
16. Wu, C, Ren, C, Song, Y, Gao, H, Pang, X, and Zhang, L. Gender-specific effects of oxidative balance score on the prevalence of diabetes in the US population from NHANES. Front Endocrinol. (2023) 14:1148417. doi: 10.3389/fendo.2023.1148417
17. Ilori, TO, Wang, X, Huang, M, Gutierrez, OM, Narayan, KM, Goodman, M, et al. Oxidative balance score and the risk of end-stage renal disease and cardiovascular disease. Am J Nephrol. (2017) 45:338–45. doi: 10.1159/000464257
18. Bentyaghoob, S, Dehghani, F, Alimohammadi, A, Shateri, Z, Kahrizsangi, MA, Nejad, ET, et al. Oxidative balance score and dietary phytochemical index can reduce the risk of colorectal cancer in Iranian population. BMC Gastroenterol. (2023) 23:183. doi: 10.1186/s12876-023-02826-z
19. Sohouli, MH, Rohani, P, Hosseinzadeh, M, and Hekmatdoost, A. Adherence to oxidative balance scores and lower odds of non-alcoholic fatty liver disease: a case-control study. Sci Rep. (2023) 13:6140. doi: 10.1038/s41598-023-33407-5
20. Zipf, G, Chiappa, M, Porter, KS, Ostchega, Y, Lewis, BG, and Dostal, J. National health and nutrition examination survey: plan and operations, 1999–2010. Vital Health Stat. (2013) 1:1–37.
21. Xie, R, and Zhang, Y. Is assessing the degree of hepatic steatosis and fibrosis based on index calculations the best choice for epidemiological studies? Environ Pollut. (2023) 317:120783. doi: 10.1016/j.envpol.2022.120783
22. Kalligeros, M, Vassilopoulos, A, Vassilopoulos, S, Victor, DW, Mylonakis, E, and Noureddin, M. Prevalence of Steatotic liver disease (MASLD, MetALD and ALD) in the United States: NHANES 2017–2020. Clin Gastroenterol Hepatol. (2023) 8:S1542–3565(23)00914-X. doi: 10.1016/j.cgh.2023.11.003
23. Lazarus, JV, Newsome, PN, Francque, SM, Kanwal, F, Terrault, NA, and Rinella, ME. Reply: a multi-society delphi consensus statement on new fatty liver disease nomenclature. Hepatology. (2023). doi: 10.1097/HEP.0000000000000696
24. Tseng, TS, Lin, WT, Ting, PS, Huang, CK, Chen, PH, Gonzalez, GV, et al. Sugar-sweetened beverages and artificially sweetened beverages consumption and the risk of nonalcoholic fatty liver (NAFLD) and nonalcoholic steatohepatitis (NASH). Nutrients. (2023) 15:3997. doi: 10.3390/nu15183997
25. Siddiqui, MS, Vuppalanchi, R, Van Natta, ML, Hallinan, E, Kowdley, KV, Abdelmalek, M, et al. Vibration-controlled transient Elastography to assess fibrosis and steatosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. (2019) 17:156–163.e2. doi: 10.1016/j.cgh.2018.04.043
26. Lin, G, Zhan, F, Zhu, J, Xue, L, and Wei, W. Relationship between oxidative balance score and kidney stone prevalence in US adults. Int Urol Nephrol. (2023). doi: 10.1007/s11255-023-03866-w
27. Tylavsky, FA, Han, L, Sims, TL, Mason, WA, Carroll, KN, Bush, NR, et al. Oxidative balance score during pregnancy is associated with oxidative stress in the CANDLE study. Nutrients. (2022) 14:2327:2327. doi: 10.3390/nu14112327
28. Rayburn, WF . Diagnosis and classification of diabetes mellitus: highlights from the American Diabetes Association. J Reprod Med. (1997) 42:585–6.
29. Cascino, TM, Colvin, MM, Lanfear, DE, Richards, B, Khalatbari, S, Mann, DL, et al. Racial inequities in access to ventricular assist device and transplant persist after consideration for preferences for care: a report from the REVIVAL study. Circ Heart Fail. (2023) 16:e009745. doi: 10.1161/CIRCHEARTFAILURE.122.009745
30. Yang, L, Chen, X, Cheng, H, and Zhang, L. Dietary copper intake and risk of stroke in adults: a case-control study based on National Health and nutrition examination survey 2013–2018. Nutrients. (2022) 14:409. doi: 10.3390/nu14030409
31. Jin, S, Cui, S, Mu, X, Liu, Z, Han, Y, Cui, T, et al. Exposure to phthalates and their alternatives in relation to biomarkers of inflammation and oxidative stress in adults: evidence from NHANES 2017–2018. Environ Sci Pollut Res Int. (2023). doi: 10.1007/s11356-023-30924-8
32. Ding, Y, and Xu, X. Dose-response relationship between leisure-time physical activity and biomarkers of inflammation and oxidative stress in overweight/obese populations. J Sci Med Sport. (2023) 26:616–21. doi: 10.1016/j.jsams.2023.09.010
33. Kourouma, A, Keita, H, Duan, P, Quan, C, Bilivogui, KK, Qi, S, et al. Effects of 4-nonylphenol on oxidant/antioxidant balance system inducing hepatic steatosis in male rat. Toxicol Rep. (2015) 2:1423–33. doi: 10.1016/j.toxrep.2015.10.006
34. Shimomura, Y, Takaki, A, Wada, N, Yasunaka, T, Ikeda, F, Maruyama, T, et al. The serum oxidative/anti-oxidative stress balance becomes dysregulated in patients with non-alcoholic steatohepatitis associated with hepatocellular carcinoma. Intern Med. (2017) 56:243–51. doi: 10.2169/internalmedicine.56.7002
35. Chen, Z, Tian, R, She, Z, Cai, J, and Li, H. Role of oxidative stress in the pathogenesis of nonalcoholic fatty liver disease. Free Radic Biol Med. (2020) 152:116–41. doi: 10.1016/j.freeradbiomed.2020.02.025
36. Nasri, H, Shirzad, H, Baradaran, A, and Rafieian-Kopaei, M. Antioxidant plants and diabetes mellitus. J Res Med Sci. (2015) 20:491–502. doi: 10.4103/1735-1995.163977
37. Rives, C, Fougerat, A, Ellero-Simatos, S, Loiseau, N, Guillou, H, Gamet-Payrastre, L, et al. Oxidative stress in NAFLD: role of nutrients and food contaminants. Biomol Ther. (2020) 10:1702. doi: 10.3390/biom10121702
38. Liu, Y, and Chen, M. Dietary and lifestyle oxidative balance scores are independently and jointly associated with nonalcoholic fatty liver disease: a 20 years nationally representative cross-sectional study. Front Nutr. (2023) 10:1276940. doi: 10.3389/fnut.2023.1276940
39. Sanyal, AJ, Chalasani, N, Kowdley, KV, Mccullough, A, Diehl, AM, Bass, NM, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. (2010) 362:1675–85. doi: 10.1056/NEJMoa0907929
40. Majzoub, AM, Nayfeh, T, Barnard, A, Munaganuru, N, Dave, S, Singh, S, et al. Systematic review with network meta-analysis: comparative efficacy of pharmacologic therapies for fibrosis improvement and resolution of NASH. Aliment Pharmacol Ther. (2021) 54:880–9. doi: 10.1111/apt.16583
41. Liu, X, Shen, H, Chen, M, and Shao, J. Clinical relevance of vitamins and carotenoids with liver steatosis and fibrosis detected by transient Elastography in adults. Front Nutr. (2021) 8:760985. doi: 10.3389/fnut.2021.760985
42. Berna, G, and Romero-Gomez, M. The role of nutrition in non-alcoholic fatty liver disease: pathophysiology and management. Liver Int. (2020) 40:102–8. doi: 10.1111/liv.14360
43. Graham, DS, Liu, G, Arasteh, A, Yin, XM, and Yan, S. Ability of high fat diet to induce liver pathology correlates with the level of linoleic acid and vitamin E in the diet. PLoS One. (2023) 18:e0286726. doi: 10.1371/journal.pone.0286726
44. Liu, W, Zhu, M, Gong, M, Zheng, W, Zeng, X, Zheng, Q, et al. Comparison of the effects of monounsaturated fatty acids and polyunsaturated fatty acids on liver lipid disorders in obese mice. Nutrients. (2023) 15:3200. doi: 10.3390/nu15143200
45. Wang, T, Goodman, M, Sun, YV, Thyagarajan, B, Gross, M, and Bostick, RM. DNA base excision repair genetic risk scores, oxidative balance, and incident, sporadic colorectal adenoma. Mol Carcinog. (2017) 56:1642–52. doi: 10.1002/mc.22620
46. Juanola, O, Martinez-Lopez, S, Frances, R, and Gomez-Hurtado, I. Non-alcoholic fatty liver disease: metabolic, genetic, epigenetic and environmental risk factors. Int J Environ Res Public Health. (2021) 18:5227. doi: 10.3390/ijerph18105227
47. Huang, YW, Wang, LT, Zhang, M, Nie, Y, Yang, JB, Meng, WL, et al. Caffeine can alleviate non-alcoholic fatty liver disease by augmenting LDLR expression via targeting EGFR. Food Funct. (2023) 14:3269–78. doi: 10.1039/D2FO02701A
Keywords: metabolic dysfunction-associated steatotic liver disease (MASLD), oxidative balance score (OBS), nutrition, NHANES, mortality
Citation: Peng L, Li L, Liu J and Li Y (2024) New insights into metabolic dysfunction-associated steatotic liver disease and oxidative balance score. Front. Nutr. 10:1320238. doi: 10.3389/fnut.2023.1320238
Edited by:
Md Wasim Khan, University of Illinois Chicago, United StatesReviewed by:
Johanna Arroyave, Universidad de Antioquia, ColombiaStefan Kabisch, Charité University Medicine Berlin, Germany
Copyright © 2024 Peng, Li, Liu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuanyuan Li, liyuanyuannjmu@163.com
†These authors have contributed equally to this work
 Lei Peng
Lei Peng Lurong Li1†
Lurong Li1†  Yuanyuan Li
Yuanyuan Li