Cost-Effectiveness Analysis of Group vs. Weblog Telecommunication (Web Tel) Nutrition Education Program on Glycemic Indices in Patients With Non-Insulin Dependent Diabetes Mellitus Type 2: A Randomized Controlled Trial
- 1Department of Community Nutrition, School of Nutrition and Food Sciences, Shiraz University of Medical Sciences, Shiraz, Iran
- 2Health Human Resources Research Center, Department of Health Economics, School of Management and Information Sciences, Shiraz University of Medical Sciences, Shiraz, Iran
- 3Department of Nutrition Research, National Nutrition and Food Technology Research Institute, Faculty of Nutrition Sciences and Food Technology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 4Department of Internal Medicine, Endocrinology and Metabolism Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
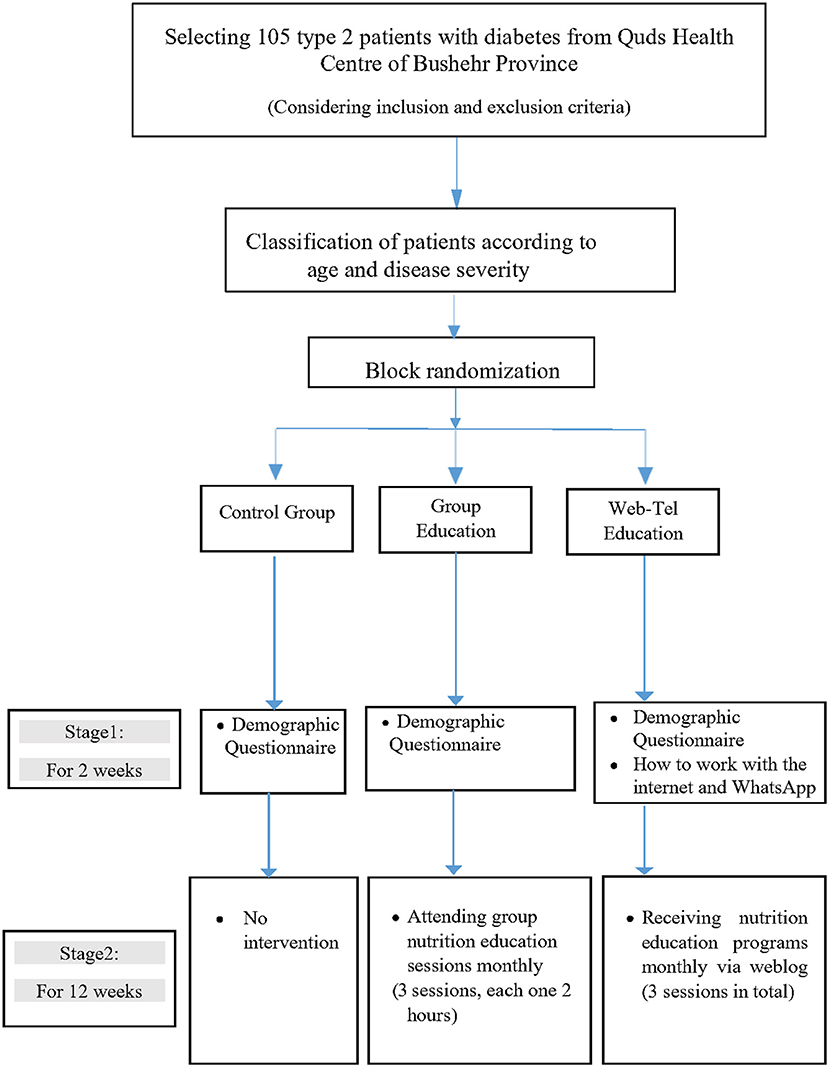
This a randomized controlled trial study with a cost-effectiveness analysis that aimed to compare the cost-effectiveness of group nutrition education with that of Web-Tel nutrition education in the glycemic control of patients with non-insulin-dependent type 2 diabetes mellitus (T2DM). The study was conducted on 105 patients with T2DM for 3 months in Quds health centre of Bushehr province, Iran. The participants were classified based on age and disease severity (hemoglobin A1c level); then, they were randomly assigned to one of the three groups: group education, Web-Tel education, and the control group using block randomization method. The clinical (intermediate) outcome was changes in hemoglobin A1c (HbA1c). Patients' perspective was adopted, and a deterministic one-way sensitivity analysis was conducted to identify the effects of uncertainties. The results indicated that the expected effectiveness was 0.46, 0.63, and 0.4; the mean costs was 27,188, 5,335, and 634 purchasing power parity (PPP) dollars for group education, Web-Tel education, and the control group, respectively. The incremental cost-effectiveness ratio (ICER) of Web-Tel education vs. the control group was positive and equal to $21, 613.04 PPP; since it was less than three times of the threshold, the Web-Tel education method was considered as a more cost-effective method than the control group. On the other hand, the ICER of group education vs. control group was $447,067 PPP and above the threshold, so group education was considered as a dominated method compared with the control group. In conclusion, considering the ICER, Web-Tel education is a more cost-effective method than the other two and can be used as the first priority in educating patients with T2DM. The present study was registered in Thailand Clinical Trials Registry (TCTR20210331001).
Introduction
Uncontrolled diabetes mellitus (DM) could lead to micro-/macrovascular complications, decreasing the quality of life, increasing the risk of premature death, and imposing a substantial economic burden of work absenteeism and healthcare on societies (1–5). The total annual cost of diabetes in Iran is estimated to 3.64 billion US dollars (including $1.71 billion direct and $1.93 billion indirect costs) in 2009, and is estimated to reach to 9 billion US dollars by 2030 (including $4.2 billion in direct and $4.8 billion in indirect costs) (1).
Education is considered as a basic principle in diabetes care (6). Accordingly, one of the most important methods in diabetes self-management education (DSME) is “group education.” This method enables patients to discuss nutritional issues and increase their quality of life (6–8). On the other hand, Web-Tel nutrition education includes the use of weblog and mobile apps, and is considered as a new way for educational purposes (9).
There are numerous studies worldwide that focused on the economic burden of DM, but limited studies have been conducted on the cost-effectiveness of nutrition education in patients with diabetes. A 6-month randomized controlled trial examined the cost-effectiveness of nutrition education in 179 patients with diabetes but free of complications of diabetes and co-morbidities in the United States. The results showed that the cost-effectiveness was $4.2 in the intervention group and $5.32 in the control group (10). Also, three studies were conducted in 2014, 2015, and 2018; all showed that DSME had better cost-effectiveness than usual care in the quality of life (11–13).
Although a group or virtual nutrition education program has been tried on a worldwide scale, the results have been inconclusive. To the best of our knowledge, there is no consensus on the most cost-effective approach of nutrition education for patients with diabetes. Therefore, the present study aimed to compare the cost-effectiveness of two nutrition education methods, Web-Tel and group education, with a control group in the HbA1c level of patients with non-insulin-dependent T2DM.
Materials and Methods
Study Design and Participants' Recruitment
The present study was a cost-effectiveness analysis and a parallel randomized controlled clinical trial. The study population consisted of adult patients with T2DM who were recruited from Quds health centre of Bushehr province, Iran in 2021. The inclusion criteria included: patients with T2DM with poor glycemic control (HbA1c ≥ 7), diagnosis of the disease under 1 year, patients with non-insulin-dependent type 2 diabetes (either on medication or not), adults above 20 years old, reading and writing literacy; having access and ability to use the internet and mobile phones, and tendency to participate in the study. However, the following individuals were not included in the study: individuals with any mental or physical disabilities, individuals under treatment for AIDS, cancers, chronic heart failure, cerebrovascular, renal, and hepatic diseases, pregnant or lactating women, individuals who have participated in professional nutrition education classes during the last year, and individuals who attended in other clinical studies in the past 6 months. The exclusion criteria included being diagnosed with any chronic diseases during the trial, failure to attend more than one educational session, and lack of motivation to continue at any time of the study. Before the study commenced, the main researcher explained all the possible benefits and harms of it to the participants, and then written consent forms were signed by them.
Sample Size Calculation
According to the previous study by Kim et al. (14), and considering HbA1c as a primary outcome, with the power and confidence level of 99%, sample size was calculated as 26 participants in each group using the NCSS (PASS) 2007 software (NCSS, Kaysville, UT, United States). After applying attrition rate of 35% in sample size calculation, a total of 105 participants were obtained (n = 35 in each group). The following formula was used for sample size calculation:
In the above formula: d = 100 z, α = 0.01, β = 0.01, δ1 = 0.81, and δ1 = 0.61.
Random Allocation and Allocation Concealment
After checking the participants' compatibility with the inclusion and exclusion criteria, eligible ones received a unique code. In order to control for prognostic factors, the participants were classified based on their age and disease severity (hemoglobin A1c); then, they were randomly assigned to one of the three groups using block randomization method by the main researcher. For this purpose, random allocation software version 2.0 was used.
Data Collection and Measurement Intervals
At the beginning of the study, a demographic questionnaire (including sex, age, education, and occupation) was completed by each participant. Glycemic indices were measured in months 0 and 3 of the study. The intermediate (clinical) outcome was changes in HbA1c.
Biochemical Measurements
Participants' blood samples were collected early in the morning after at least 10 h of fasting. Also, they were asked to stop taking glucose-lowering drugs for 8–10 h before the test. HbA1c was measured using a complete blood sample by high-performance liquid chromatography (HPLC) (Bio-Rad Variant II, Sydney, Australia). Fasting blood sugar (FBS) was measured by hexokinase (Roche Modular Analyzer; Tokyo, Japan). Fasting insulin levels was measured quantitatively by enzyme-linked immunosorbent assay (ELISA).
Intervention
The current study was divided into two stages (2 phases).
Phase 1 (Pre-intervention) for 2 Weeks
In this phase, “demographic” questionnaires were completed. In addition, participants in the Web-Tel group were taught how to work on the internet in the form of weblog and WhatsApp by the main researcher at the Quds health centre of Bushehr province.
Phase 2 (Intervention) for 3 Months
In this phase, the participants received nutrition education. The educational contents were the same in both groups (Web-Tel and group method). The Web-Tel group received one lesson each month. They used their special password to enter the weblog and read the educational contents. In group education, educational sessions were held monthly (3 sessions in total and each session lasted for 2 h). The control group received none of the nutrition educational contents that were delivered to the intervention groups. Due to the COVID 19 pandemic, none of the participants received any usual care. The study design and educational contents are summarized in Figure 1 and Supplementary Table 1, respectively.
Statistical Analysis
The collected data were analyzed with SPSS software version 22, within an intent-to-treat (ITT) framework in which missing data were simply imputed and the last measurement of every participant was used. Baseline values were shown as mean ± standard deviation (SD) for quantitative variables, and frequency (percentage) for qualitative variables. The chi-square method was used to compare qualitative variables among the three groups. For quantitative variables, first, the normality of the data was assessed by Kolmogorov-Smirnov and Shapiro-Wilk tests. Then, for between-group comparisons of normally distributed variables, one-way ANOVA, and for abnormal distributed ones, Kruskal Wallis test were conducted. P < 0.05 was considered as significant.
Data Collection of Costs
The cost-effectiveness was determined with patient perspective. In general, the costs were divided into two categories: (1) direct medical costs (DMCs) including cost of education, educational tools, and execution, and (2) direct nonmedical costs (DNMCs), which were the costs of infrastructural materials. DMCs and DNMCs were collected using cost collection forms, self-reporting of the patients, and experts' opinions. Details of costs have been summarized in the footnotes of Table 2.
Cost-Effectiveness Analysis
In the present study, effectiveness was defined as a reduction in HbA1c level. Then, costs, effectiveness, and incremental cost-effectiveness ratio (ICER) were calculated with TreeAge Software version 2020. ICER was calculated using the following formula: (cost intervention – cost control)/(Effectiveness intervention- Effectiveness control).
Uncertainty Analysis
A one-way sensitivity analysis was conducted to assess the effect of the parameter's uncertainty on the results of the study. The parameters included the effectiveness of group education, Web-Tel education, or the control group, and the costs of group education, Web-Tel education, and the control group. The values of each parameter changed by 20%, and tornado diagrams were drawn. Since there is no specific cost-effectiveness threshold in Iran, based on WHO recommendation, the threshold in developing countries was considered at one time to three times of gross domestic product per capita. According to the World Bank report, the threshold was about $13116 PPP for Iran in 2021 (15, 16).1,2
Results
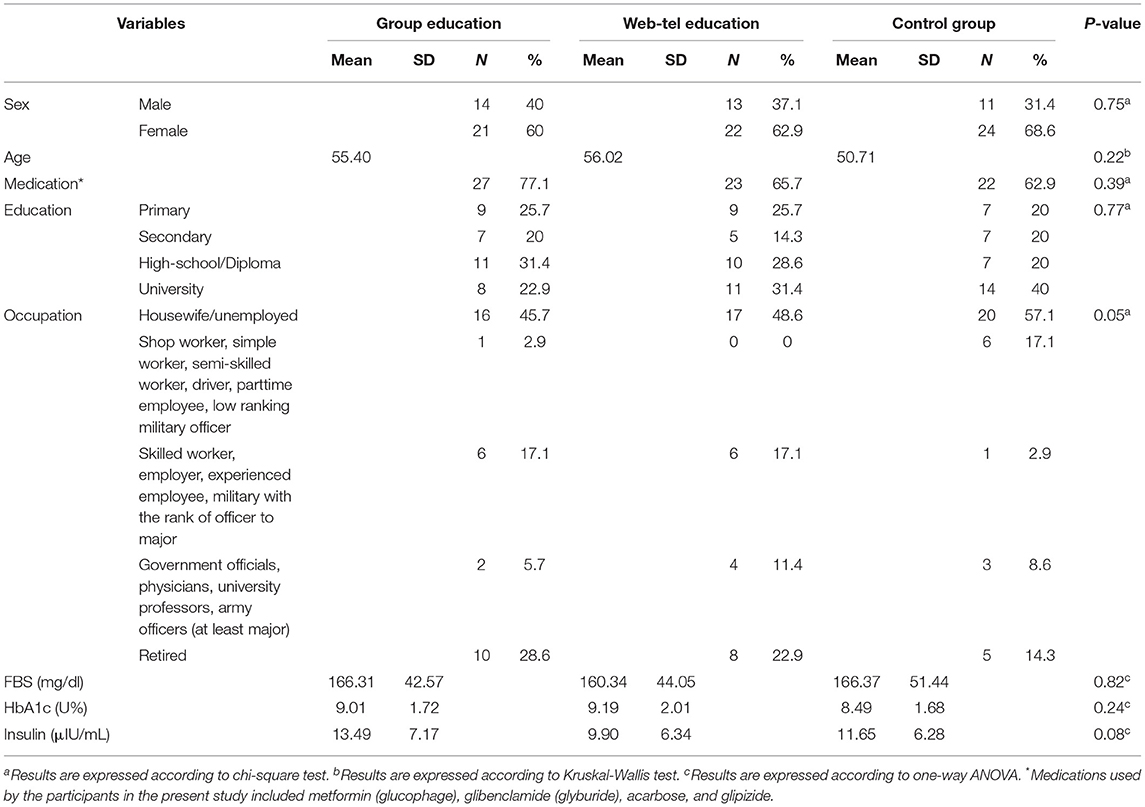
In the present study, twenty-three patients discontinued their participation (overall attrition rate = 21.9%). The attrition rate in group education was 22.85%, in Web-Tel education 20%, and in the control group 22.85% (Supplementary Figure 1). Also, the between-group comparisons of baseline variables indicated no significant differences (Table 1). According to Table 2, the mean DMCs per participant in group education, Web-Tel education, and the control group were 194.79, 335.98, and 30.91 dollars, respectively. Moreover, the mean DNMCs per participant in group education, Web-Tel education, and the control group were 26,993.7, 4,998.82, and 333.25 dollars, respectively. Based on the Kruskal-Wallis test, there was a significant difference among the three groups in each category of DMCs, DNMCs, and total costs (p < 0.001).
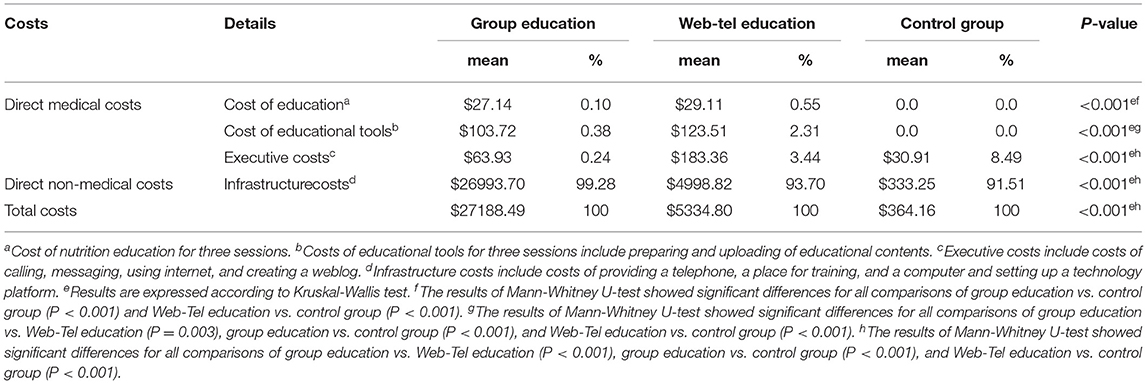
Table 2. Comparison of costs among the three groups of patients with type 2 diabetes mellitus (T2DM).
As shown in Table 3 and Figure 2, the expected effectiveness was 0.46, 0.63, and 0.4; the mean costs were 27,188, 5,335, and 634 PPP dollars for group education, Web-Tel education, and the control group, respectively. The comparison of Web-Tel education vs. control group showed that the ICER was $21,613.04, which indicated that for each additional percentage of success in decreasing HbA1c level by Web-Tel education, $21,613.04 should be spent. On the other side, the comparison of group education vs. control group showed that the ICER was $447,067, which indicated that for each additional percentage of success in decreasing HbA1c level by group education, $447,067 should be spent. To make a decision, we must compare the ICER with a threshold (15). Therefore, because the ICER was less than three times per capita GDP, the Web-Tel method was considered as a more cost-effective option than the control group, while the group education method was more than one to three times per capita GDP, so it was considered as a dominated method compared with the control group.
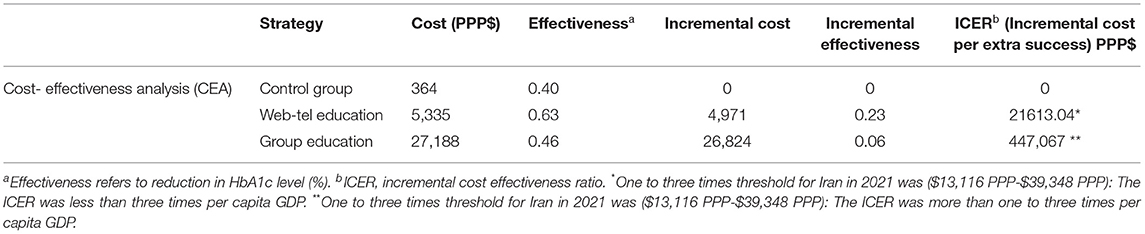
Table 3. Comparing the cost-effectiveness of three methods of nutrition education in patients with T2DM.
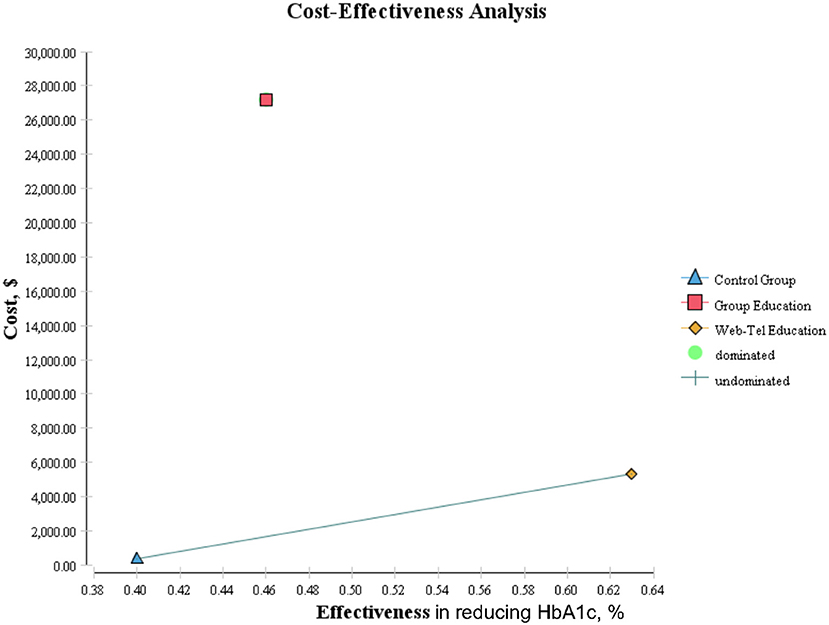
Figure 2. Comparison of cost-effectiveness analysis among three groups of patients with type 2 diabetes.
The results of the tornado diagram showed that in the comparison of group education vs. control group, ICER results had the most sensitivity to the effectiveness of group Education and the control group; and in the comparison of the Web-Tel education vs. control group, the model was most sensitive to the effectiveness of Web-Tel education. Also, in comparing Web-Tel education with group education, ICER results had the highest sensitivity to the effectiveness of Web-Tel education (Figure 3) (16).
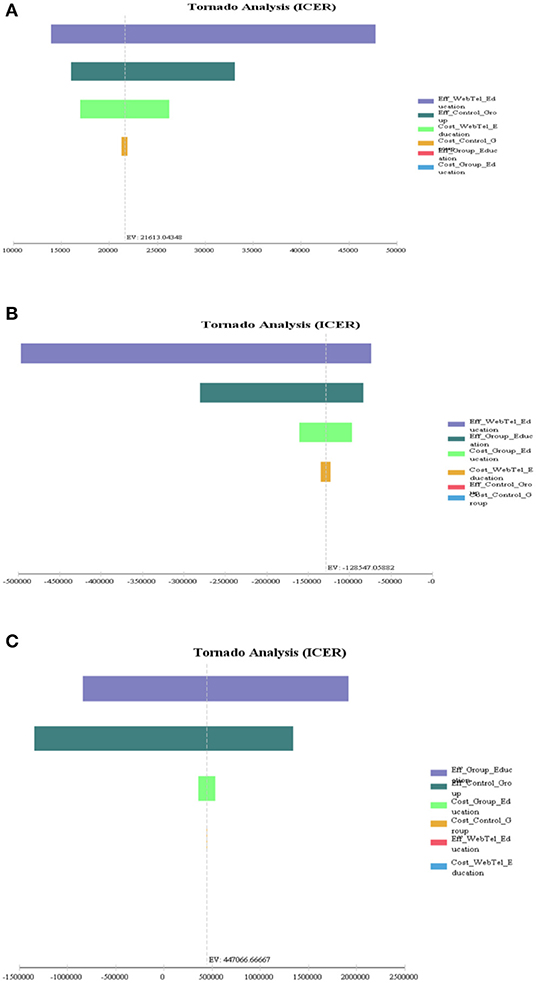
Figure 3. One-way sensitivity analysis and tornado diagram of incremental cost-effectiveness ratio (ICER) comparisons among the three groups of patients with type 2 diabetes. (A) Web-Tel education vs. control group, (B) Web-Tel education vs. group education, and (C) group education vs. control group.
Discussion
According to our results, the web-based education was more effective in reducing HbA1c level than group education or the control group. It was compatible with the results of another study conducted on 40 patients with T2DM for 6 months which showed that applying a web-based education system could be more effective than traditional education for glycemic control in patients with diabetes (17). Also, in agreement with the cost-effectiveness results of the present study, Li et al. (13) (in the United Kingdom), compared a 1-year web-based self-management training method with usual care for 374 patients with T2DM. The results showed that the web-based training was considered as a cost-effective method, equal to £20,000 to 30,000 per unit of quality of life (13). Another study in 2014 assessed the cost-effectiveness of an American community-based educational program for patients with type 2 diabetes. They found that the intervention improved HbA1c and QALY significantly by 0.056 per person (per unit of quality of life equivalent to $ 355) compared to the control group (12). Conversely, a 1-year randomized clinical trial (in 2015) on the cost-effectiveness of group education in patients with diabetes showed that the clinical outcome was reduced significantly in the intervention group compared to the control group who received usual care. The quality of life was also improved by 0.067, equal to 1,862 US dollars per person (11).
The observed controversy between the findings of the present study and previous ones can be justified by the following facts. In the present study, the problems reported by patients who attended in group education classes were lack of time and distance problem. Moreover, because of the COVID-19 pandemic and its high pathogenicity among the elderly and those with weak immune system, the group education method was not welcomed by the patients with diabetes. Although the groups were small, the patients were still concerned about the high transmissibility of the virus, especially in a situation where minority of the population got the first dose of vaccine, and the vast majority of the population was unvaccinated. Another reason that group education dominated the other groups/methods is probably the fact that the educational content was not accessible at any time. Therefore, virtual education such as Web-Tel education, with lower cost and higher effectiveness, can be a suitable alternative for group education to meet the needs of patients with T2DM. The Web-Tel method enables the participants to access information at any time and without the stress of participating in group classes. Moreover, based on the participants' opinion, this method was simple, comfortable, and time-saving.
Considering the fact that a considerable part of the costs of patients with diabetes is related to direct costs, which account for 2.5 to 15% of the total health budget in different countries (18), the present study aimed to investigate the direct medical costs of patients with diabetes. In Iran, a significant amount of costs of patients with diabetes are covered by health insurance. Also, education of patients with diabetes is performed in health centers and is covered by healthcare providers for free. However, three issues must be considered to justify the patients' perspective in the present study. First, previous studies have shown that despite health insurance coverage, the cost that have to be paid directly by patients is still high in Iran and other developing countries, which have faced the healthcare system with serious challenges (19, 20). Second, nutrition education in health centers does not cover many special nutrition concepts such as counting carbohydrates or traffic light labels of foods (21). In addition, the education of patients with diabetes in health centres has been limited due to the COVID-19 pandemic. In fact, many centres refused to provide these services for patients with diabetes as a high-risk population for Corona virus. The last two issues forced people with diabetes to refer to nutrition clinics to get nutrition education where the entire cost was covered by the patients. So, in the present study the patients' perspective was selected to investigate the cost-effectiveness of nutrition education in patients with diabetes, that the costs are totally or to a large extent covered by the patients.
The present study has some strengths. This is the first study that assessed the effectiveness and cost-effectiveness of two different nutrition educational methods in patients with T2DM, especially in Iran. The other two strengths include, creating active environment and using text-messages/calls during trial, to become aware of receiving educational contents by the participants and minimizing their lost to follow up. On the other hand, it has some limitations. First, because of the COVID-19 pandemic, group education was held with few participants in each class (maximum of six), so the limited number of participants decreased the interactions and class discussions. Second was the short duration of the study of about 3 months. Third was detection of a large amount of uncertainty associated with the results according to the sensitivity-analysis. Fourth and last is the generalizability of the findings. Nutrition education in Iran is used for the treatment of patients with T2DM, and its price is the same throughout the country, so the results of this study can be generalized to the whole country. However, because of differences in thresholds and prices, the results may not be comparable to other parts of the world; thus, the results should be interpreted with caution.
The results of the present study suggested the use of Web-Tel education as a first priority in educating patients with T2DM to reduce the financial burden in the community. The Web-Tel education method reduced the costs and increased the clinical outcomes in comparison with the group education method or the control group. On the other hand, group education had a high cost with low effectiveness, which indicated it to be a dominated method compared with the control group or the Web-Tel method for educating patients with T2DM. It must be mentioned that the results were highly sensitive to several key inputs; therefore, they must be interpreted with caution.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by research Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran [IR.SUMS.REC.1399.1162]. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
SF helped in design conduction and coordination of the study materials. S-MD-R reviewed the literatures, designed the protocol, conducting the intervention, and wrote the manuscript. KK and DG cooperated in the protocol design, data analysis, and calculating cost-effectiveness. SF, KK, and DG revised the manuscript. SF had primary responsibility for the final content. All authors read and approved the final manuscript.
Funding
The present study sponsored by Vice Chancellor for Research, Shiraz University of Medical Sciences. Contact information: 071-32357282.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We wish to thank the participants for taking part in the project. We also appreciate our contributors form the Deputy of Health, Bushehr University of Medical Sciences, for their assistance.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.915847/full#supplementary-material
Footnotes
1. ^http://databank.worldbank.org/data/reports.aspx?source=2&series=NY.GDP.PCAP.PP.CD&country=BWWDIAf
References
1. Javanbakht M, Mashayekhi A, Baradaran HR, Haghdoost A, Afshin A. Projection of diabetes population size and associated economic burden through 2030 in Iran: evidence from micro-simulation markov model and bayesian meta-analysis. PLoS ONE. (2015) 10:e0132505. doi: 10.1371/journal.pone.0132505
2. (NCD-RisC) NRFC. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4∙ 4 million participants. Lancet Diabetes Endocrinol. (2016) 387:1513–30. doi: 10.1016/S0140-6736(16)00618-8
3. Waller K, Furber S, Bauman A, Allman-Farinelli M, van den Dolder P, Hayes A, et al. DTEXT - text messaging intervention to improve outcomes of people with type 2 diabetes: protocol for randomised controlled trial and cost-effectiveness analysis. BMC Public Health. (2019) 19:262. doi: 10.1186/s12889-019-6550-6
4. Keshavarz K, Lotfi F, Sanati E, Salesi M, Hashemi-Meshkini A, Jafari M, et al. Linagliptin versus sitagliptin in patients with type 2 diabetes mellitus: a network meta-analysis of randomized clinical trials. Daru. (2017) 25:23. doi: 10.1186/s40199-017-0189-6
5. Islam SM, Lechner A, Ferrari U, Froeschl G, Alam DS, Holle R, et al. Mobile phone intervention for increasing adherence to treatment for type 2 diabetes in an urban area of Bangladesh: protocol for a randomized controlled trial. BMC Health Serv Res. (2014) 14:586. doi: 10.1186/s12913-014-0586-1
6. Yang YS, Wu YC, Lu YL, Kornelius E, Lin YT, Chen YJ, et al. Adherence to self-care behavior and glycemic effects using structured education. J Diabetes Investig. (2015) 6:662–9. doi: 10.1111/jdi.12343
7. Reale R, Tumminia A, Romeo L, La Spina N, Baratta R, Padova G, et al. Short-term efficacy of high intensity group and individual education in patients with type 2 diabetes: a randomized single-center trial. J Endocrinol Invest. (2019) 42:403–9. doi: 10.1007/s40618-018-0929-6
8. Trento M, Passera P, Borgo E, Tomalino M, Bajardi M, Cavallo F, et al. A 5-year randomized controlled study of learning, problem solving ability, and quality of life modifications in people with type 2 diabetes managed by group care. Diabetes Care. (2004) 27:670–5. doi: 10.2337/diacare.27.3.670
9. Chung LM, Law QP, Fong SS, Chung JW, Yuen PP. A cost-effectiveness analysis of teledietetics in short, intermediate-,and long-term weight reduction. J Telemed Telecare. (2015) 21:268–75. doi: 10.1186/s12877-020-01978-x
10. Franz MJ, Splett PL, Monk A, Barry B, McClain K, Weaver T, et al. Cost-effectiveness of medical nutrition therapy provided by dietitians for persons with non-insulin-dependentdiabetes mellitus. J Am Diet Assoc. (1995) 95:1018–24. doi: 10.1016/S0002-8223(95)00277-4
11. Mash R, Kroukamp R, Gaziano T, Levitt N. Cost-effectiveness of a diabetes group education program delivered by health promoters with a guiding style in underserved communities in Cape Town, South Africa. Patient Educ Couns. (2015) 98:622–6. doi: 10.1016/j.pec.2015.01.005
12. Prezio EA, Pagan JA, Shuval K, Culica D. The community diabetes education (CoDE) program: cost-effectiveness and health outcomes. Am J Prev Med. (2014) 47:771–9. doi: 10.1016/j.amepre.2014.08.016
13. Li J, Parrott S, Sweeting M, Farmer A, Ross J, Dack C, et al. Cost-effectiveness of facilitated access to a self-management website, compared to usual care, for patients with type 2 diabetes (HeLP-Diabetes): randomized controlled trial. J Med Internet Res. (2018) 20:e201. doi: 10.2196/jmir.9256
14. Kim CJ, Kang DH. Utility of a Web-based intervention for individuals with type 2 diabetes: the impact on physical activity levels and glycemic control. Comput Inform Nurs. (2006) 24:337–45. doi: 10.1097/00024665-200611000-00008
15. Marseille E, Larson B, Kazi DS, Kahn JG, Rosen S. Thresholds for the cost-effectiveness of interventions: alternative approaches. World Health Organ. (2014) 93:118–24. doi: 10.2471/BLT.14.138206
16. Tornado Diagram. New York, NY. York Health Economics Consortium (2016). Available online at: https://yhec.co.uk/glossary/tornado-diagram/
17. Noh JH, Cho YJ, Nam HW, Kim JH, Kim DJ, Yoo HS, et al. Web-based comprehensive information system for self-management of diabetes mellitus. Diabetes Technol Ther. (2010) 12:333–7. doi: 10.1089/dia.2009.0122
18. Wolf AM, Siadaty M, Yaeger B, Conaway MR, Crowther JQ, Nadler JL, et al. Effects of lifestyle intervention onhealth care costs: improving control with activity and nutrition (ICAN). J Am Diet Assoc. (2007) 107:1365–73. doi: 10.1016/j.jada.2007.05.015
19. Rashidian A. Widespread Coverage of Health, National Institute of Health Research, Iranian Health, Newspaper of United Nation's Agency Office in the Islamic Republic of Iran. (2010) 6th year, no 2.
20. Van Doorslaer E, O'Donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Garg CC, et al. Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. Lancet. (2006) 368:1357–64. doi: 10.1016/S0140-6736(06)69560-3
Keywords: diabetes, nutrition, education, cost-effectiveness, Web
Citation: Derakhshandeh-Rishehri S-M, Keshavarz K, Ghodsi D, Pishdad G and Faghih S (2022) Cost-Effectiveness Analysis of Group vs. Weblog Telecommunication (Web Tel) Nutrition Education Program on Glycemic Indices in Patients With Non-Insulin Dependent Diabetes Mellitus Type 2: A Randomized Controlled Trial. Front. Nutr. 9:915847. doi: 10.3389/fnut.2022.915847
Received: 08 April 2022; Accepted: 26 May 2022;
Published: 24 June 2022.
Edited by:
Edson da Silva, Universidade Federal dos Vales do Jequitinhonha e Mucuri, BrazilReviewed by:
Saeed Ghobadi, Alborz University of Medical Sciences, IranDedi Ardinata, Universitas Sumatera Utara, Indonesia
Copyright © 2022 Derakhshandeh-Rishehri, Keshavarz, Ghodsi, Pishdad and Faghih. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shiva Faghih, shivafaghih@gmail.com
 Seyedeh-Masomeh Derakhshandeh-Rishehri
Seyedeh-Masomeh Derakhshandeh-Rishehri Khosro Keshavarz2
Khosro Keshavarz2  Delaram Ghodsi
Delaram Ghodsi Shiva Faghih
Shiva Faghih