- Department of Otolaryngology-Head and Neck Surgery, The Second Affiliated Hospital of Anhui Medical University, Hefei, China
Objectives: Sudden sensorineural hearing loss (SSNHL) is a common otology emergency in the practice. Its severe hearing impairment and prognosis impair the quality of life. Given that cochlear hair cell vulnerability is not consistent across frequencies, this study aims to investigate the impact of frequency-specific hearing loss on prognosis in SSNHL.
Methods: The study included 255 patients with full-frequency SSNHL. The baseline, clinical, and hearing characteristics, as well as possible cardiovascular predictors in blood, were collected for analysis.
Results: The 4,000 and 8,000 Hz hearing levels in the responder group were significantly lower than those in the non-responder group (p = 0.008, p < 0.001), while the average hearing was not (p = 0.081). Logistic regression showed that only vertigo (OR, 95% CI, 0.265, 0.102–0.684, p = 0.006) and 8,000 Hz hearing level (OR, 95% CI, 0.943, 0.916–0.971, p < 0.001) were strongly associated with treatment outcome.
Conclusions: Compared with other frequencies, 8,000 Hz hearing level was closely related to prognosis in SSNHL. In an adjusted model, our study did not find an effect of mean hearing on prognosis in SSNHL. However, further multicenter prospective studies are needed for validation.
Introduction
Sudden sensorineural hearing loss (SSNHL) is characterized by rapid hearing loss of at least 30 dB on at least three consecutive frequencies on an audiogram within 3 days (1). SSNHL affects 5–27 per 100,000 people annually, with 6,600 new cases reported annually in the United States (2, 3). The pathological mechanism of SSNHL is unknown, and previous studies have shown that microcirculatory disturbance, prethrombotic susceptibility, and chronic inflammation are associated with its occurrence and prognosis (4–6). The etiology of SSNHL usually varies according to its audiogram, and it is currently believed that full-frequency hearing loss has a poor prognosis and is related to the mechanism of hemodynamic disturbance (7, 8). The cochlea is a single terminal artery supplying blood, and blood circulation disorders can easily affect the function of the inner ear (9, 10). The hair cells at the base of the cochlea sense the highest sound frequencies (11), Studies have shown that the base of the cochlea is highly vulnerable and is more susceptible to ischemia and hypoxia, oxidative stress, trauma, and poisoning (12–14). Although some studies suggest that the average degree of hearing loss may affect the prognosis of SSNHL (15, 16), it is unclear whether hearing thresholds at different frequencies have a significant impact on the prognosis of SSNHL.
Given the anatomical specificity of the cochlea and the possible pathogenesis of SSNHL, in this study, we observed the clinical data of SSNHL patients to explore whether hearing thresholds at different frequencies were associated with the prognosis of SSNHL.
Materials and methods
Patients
We reviewed the clinical data of full-frequency SSNHL patients admitted to the head and neck surgery department of a university hospital between January 2018 and May 2022. Patients included in the study had their first visit within 14 days of the onset of SSNHL. All patients underwent a detailed physical examination, audiometry, computed tomography, and magnetic resonance imaging of the inner ear. Patients with conductive hearing loss, chronic otitis media, Meniere's disease, or retrocochlear lesions that might interfere with the diagnosis of SSNHL were excluded. At the same time, patients with recent fever and previous comorbidities such as malignant disease, mental illness, heart failure, stroke, and diabetes were excluded. To exclude the influence of the hearing level of the unaffected ear, patients with hearing loss in the unaffected ear were not included in the inclusion criteria of this study.
Data collection
Baseline characteristics [age, sex, height, weight, body mass index (BM)], clinical characteristics (audiogram, affected side, tinnitus, ear fullness, dizziness, treatment delay), and pure-tone average (PTA) of impaired frequencies (7, 8, 17–19). The maximum value of air conductance at each frequency measured by our equipment is 100 dB. Considering the predictive role of some blood parameter markers in cardiovascular and SSNHL, we collected the pretreatment blood test results of the patients.
Treatment and evaluation
According to the Chinese SSNHL guidelines (8), all included patients received systemic steroids (dexamethasone 10 mg/day for 5 days), ginkgo biloba, and batroxobin (10 U batroxobin for the first time and then reduced to 5 U batroxobin, once every other day, discontinue use when fibrinogen is <1 g/L). Patients were divided into two groups according to their hearing recovery after 2 weeks of treatment: responder (PTA improvement ≥30 dB, or returned to normal) and non-responder (PTA improvement <30 dB at damaged frequencies) (8).
Statistical analysis
Statistical analysis was performed using SPSS 26.0. Continuous data are expressed as mean ± standard deviation, or median (interquartile range). Categorical data are presented as numbers (percentages), and statistical analysis used the chi-square test. Data were surveyed using the Kolmogorov-Smirnov test to determine distribution patterns. Two-sample t-tests were used for normally distributed quantitative data comparisons; Mann-Whitney U tests were used for non-normal quantitative data. Linear correlation to assess the association between different frequency hearing thresholds and hearing recovery. Receiver operating characteristic (ROC) curve analysis was used to assess the relationship between pre-treatment hearing thresholds at different frequencies and prognosis in SSNHL. Odds ratios (OR) and 95% confidence intervals (CI) for associations between admission hearing and SSNHL outcomes were calculated using logistic regression models. A variance inflation factor was used to check for collinearity among variables before performing multivariate logistic regression. p < 0.01 was considered significant for all tests. The figures were generated using GraphPad Prism 8.0.
Results
Baseline characteristics of SSNHL patients
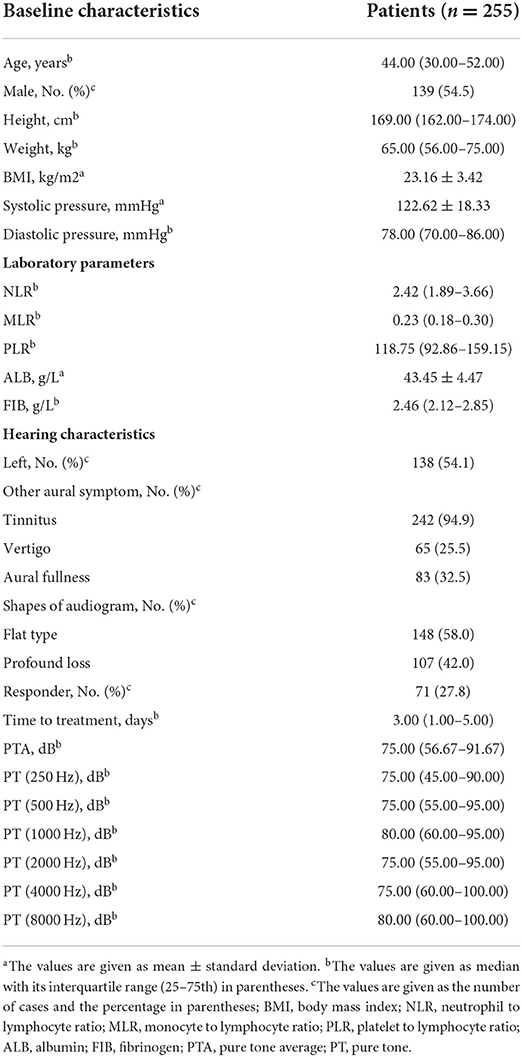
After excluding 41 patients with hearing loss in the unaffected ear, a total of 255 patients with full-range SSNHL were included, as shown in Table 1. The median age of patients was 44.00 (30.00–52.00) years, and 54.5% were male. The accompanying probability of tinnitus, aural fullness, and vertigo were 94.9, 32.5, and 25.5%, respectively. The PTA of the affected ear before treatment was 75.00 (56.67–91.67) dB, and 42.0% of the patients had total deafness hearing loss. The time from onset to treatment was 3.00 (1.00–5.00) days. Averages for 0.25, 0.5, 1, 2, 4 and 8 kHz hearing are 75.00 (45.00–90.00), 75.00 (55.00–95.00), 80.00 (60.00–95.00), 75.00 (55.00–95.00), 75.00 (60.00–100.00) and 80.00 (60.00–100.00) dB, respectively. The response rate after treatment was 27.8%.
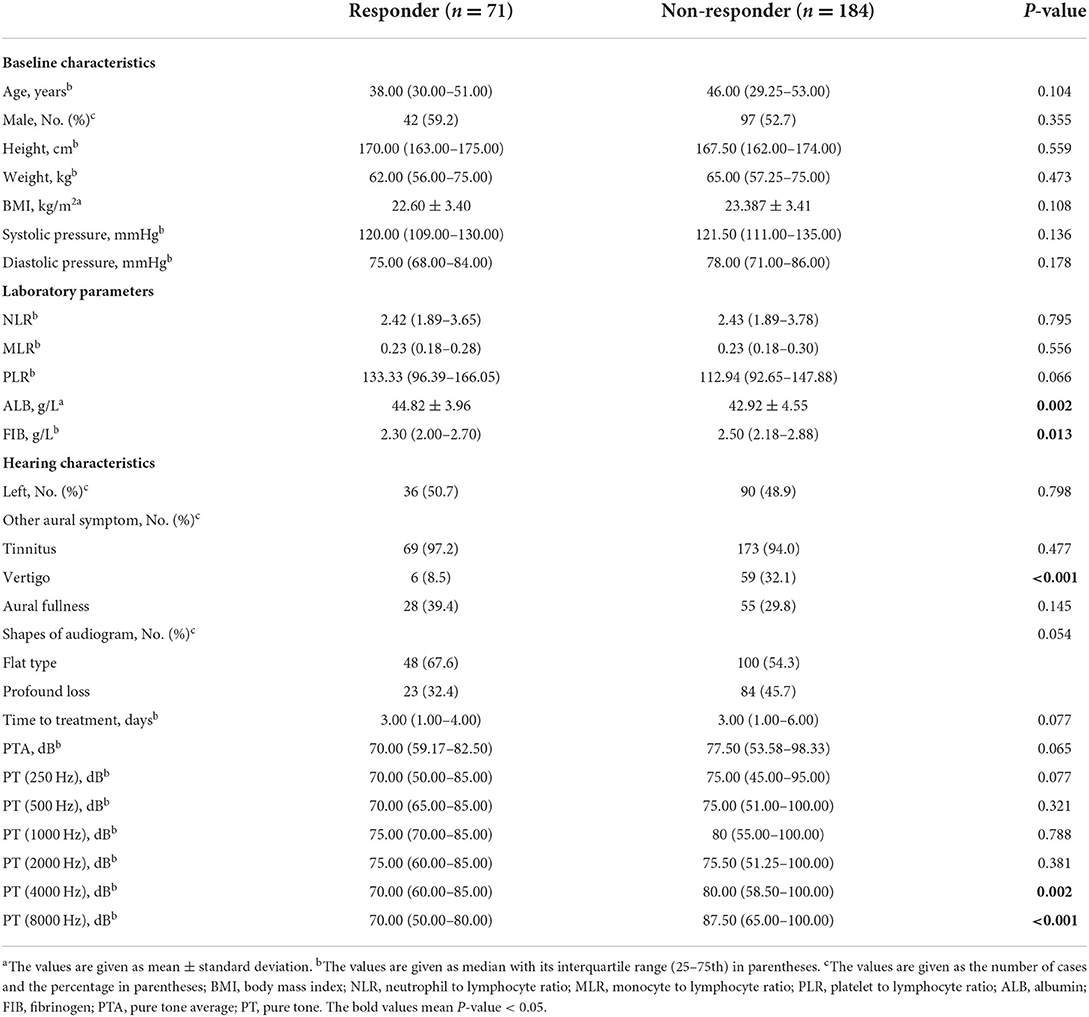
Comparison of different frequency characteristics of responder and non-responder groups
Hearing recovery patients were divided into Responder (n = 71) and Non-responder (n = 184), as shown in Table 2. There were no significant differences in baseline characteristics between the two groups (all p > 0.05). There was no significant difference in the affected side, audiogram, accompanying tinnitus, aural fullness, and treatment time after the onset between the two groups (all p > 0.05). The number of vertigo patients in the responder was significantly lower than that in the non-responder (p < 0.05). In terms of hearing at various frequencies, the hearing loss levels of the non-responder at 4,000 and 8,000 Hz were 80.00 (58.50–100.00) and 87.50 (65.00–100.00) dB, which were significantly higher than those of the responder [70.00 (60.00–85.00) and 70.00 (50.00–80.00) dB] (p < 0.05). In the comparison of blood parameters between the two groups, the albumin level in the responder was significantly higher than that in the non-responder, while the level of fibrinogen was the opposite (all p < 0.05). There was no significant difference between the two groups in some other possible cardiovascular validation markers (all p > 0.05).
Association between different frequencies and hearing recovery
We performed a linear correlation analysis and plotted a scatterplot of hearing thresholds at different frequencies vs. hearing improvement (Figure 1). When hearing loss was considered as a continuous variable, pre-treatment hearing thresholds at 4,000 and 8,000 Hz were negatively correlated with hearing improvement (r = – 0.189, p = 0.003, and r = – 0.314, p < 0.001, respectively), while other frequencies and PTA were not significantly correlated with hearing improvement (all p > 0.05). ROC curve analysis of SSNHL results showed that the areas under the curve at 4,000 and 8,000 Hz before treatment were 0.624 (95% CI, 0.555–0.694) and 0.700 (95% CI, 0.631–0.769), respectively (Figure 2). This suggests that high-frequency hearing, but not PTA, may be a predictor of poor prognosis in full-frequency SSNHL.
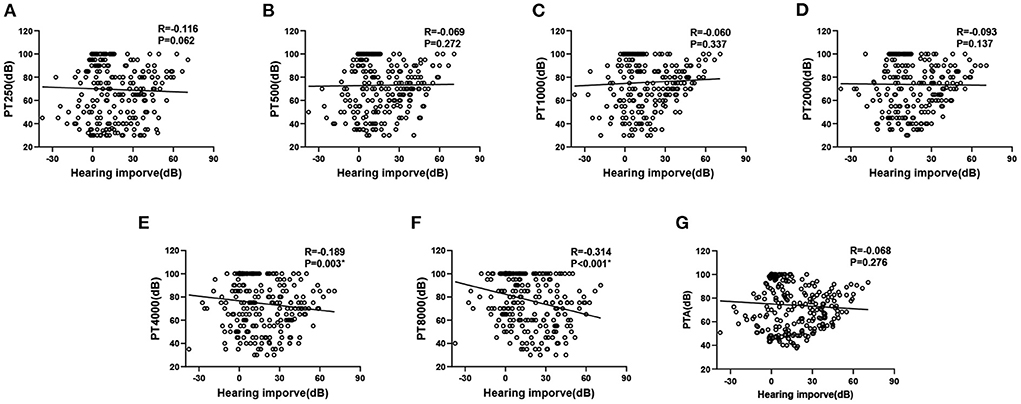
Figure 1. Hearing thresholds vs. hearing improvement. Hearing thresholds vs. hearing improvement. (A–G) represent the relationship between PT250, PT500, PT1000, PT2000, PT4000, PT8000 and PTA and hearing improve, respectively.
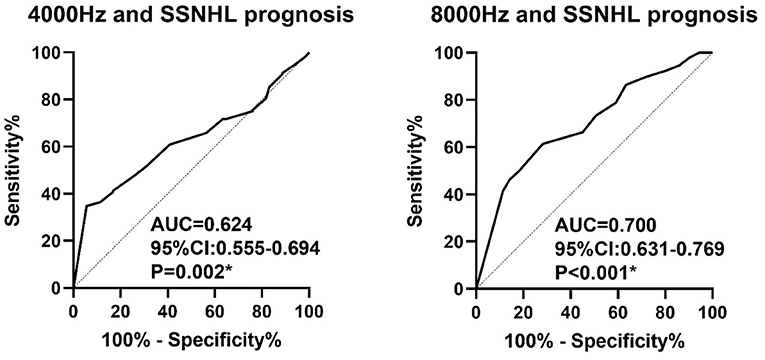
Figure 2. Receiver operating characteristic curve analysis of 4,000 and 8,000 Hz hearing levels for the prediction of the outcome of SSNHL.
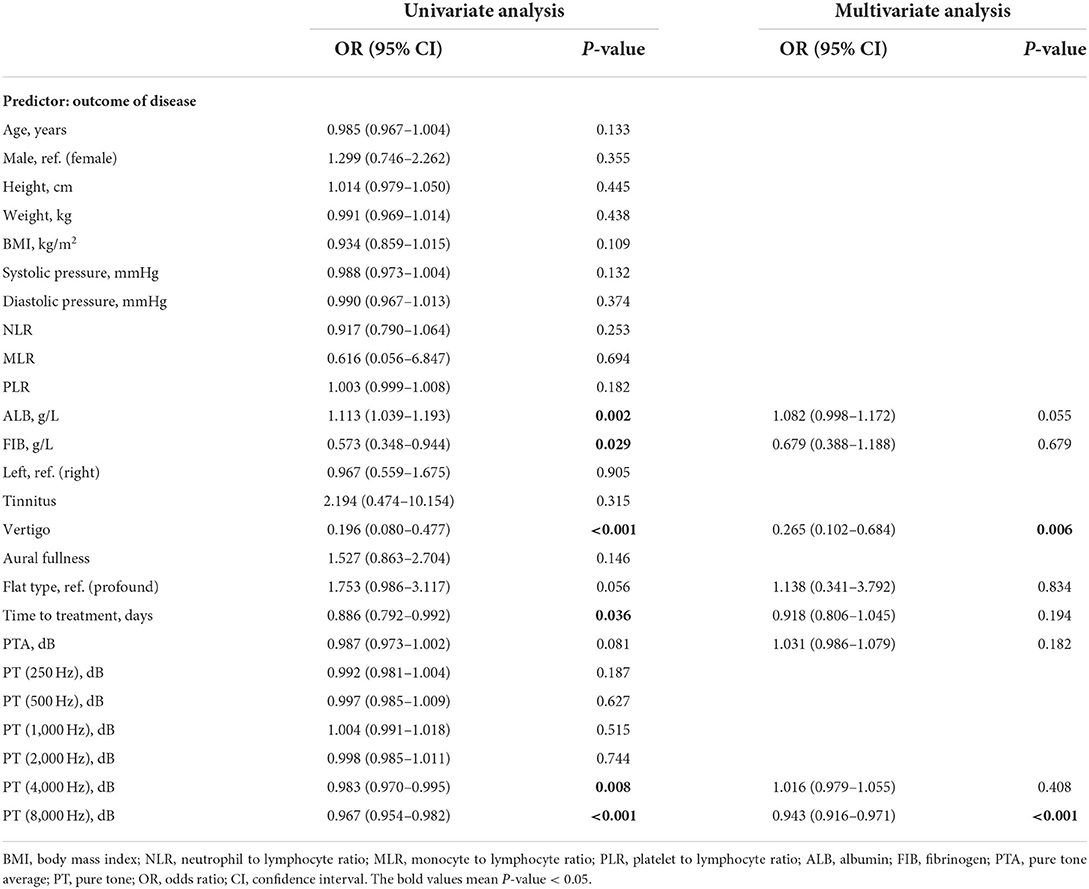
In univariate logistic regression analysis, the OR of SSNHL prognosis and parameters are shown in Table 3. We found that ALB, fibrinogen, vertigo, duration of treatment, and hearing at 4,000 and 8,000 Hz were associated with SSNHL treatment outcomes. Variables with test level < 0.1 in univariate analysis were included in multivariate logistic regression. A variance inflation factor was used to confirm that all parameters were non-collinear before multivariate analysis. After adjusting for all other significant predictors, vertigo and 8,000 Hz hearing remained independent predictors, with adjusted OR of 0.265 (0.102–0.684, p = 0.006), and 0.943 (0.916–0.971, p < 0.001), respectively. These results suggest that the presence of vertigo and higher hearing loss at 8,000 Hz are independent factors for poor prognosis in SSNHL.
Discussion
In this study, we found that vertigo and initial hearing at 8,000 Hz were associated with hearing recovery in patients with SSNHL. To assess the role of each frequency threshold in the prognosis of SSNHL, this study included SSNHL patients with full-frequency hearing impairment. Considering the roles of inflammation and hemodynamics in patients with full-frequency SSNHL, we included some possible blood predictors for analysis. Our results suggest that it's hearing at 8,000 Hz, but not other frequencies, that predicts full-frequency SSNHL.
There are many hypotheses about the pathogenesis of SSNHL: infectious, vascular, inflammatory, immune, degenerative, etc., (20, 21). It is known that age, vertigo, and the time to delay treatment after onset are closely related to the degree of recovery of SSNHL (22–24). In recent years, more and more studies have suggested that cardiovascular factors, hemorheology, and oxidative stress are related to the occurrence and prognosis of SSNHL (25, 26), specific inflammatory and cardiovascular markers have also been shown to be related to the outcome of SSNHL (18, 27–30). However, whether this association is directly related to SSNHL is debatable. In the present study, we included possible inflammatory and cardiovascular markers, although in univariate analysis we found that ALB and FIB but not other parameters may provide guidance on the prognosis of SSNHL. However, we did not find this correlation in multivariate analysis, which seems to further explain that vascular factors further influence the occurrence and prognosis of SSNHL by affecting inner ear hair cell function. Similarly, several studies have shown that the shorter the delayed treatment time, the better the hearing prognosis (19, 31). This study did not find that treatment time had an important effect on hearing recovery, which may be based on two aspects: 1. The population included in this study followed the guidelines for the first visit within 14 days, which is relatively loose. 2. This study defines hearing recovery as hearing improvement ≥30 dB. This study suggests that patients with vertigo may have a worse prognosis, which is consistent with previous studies (23). Vestibular dysfunction significantly associated with severe hearing loss (32). Studies have reported that the vestibule as an end-organ has better collateral vascular supply than the cochlea (33, 34), so the presence of vertigo often predicts extensive inner ear damage and a poorer prognosis.
The cochlea consists of three adjacent membranous tubes, shaped like a snail, surrounded by a bony shell (35, 36). Frequency-specific hair cell receptors transduce acoustic signals in the cochlea, and these hair cell receptors map within the cochlea, creating a tonotopic structure with the lowest frequencies at the top of the cochlea and the highest frequencies at the base of the cochlea (11, 36). As an end-organ supplied by a single arterial blood supply, the cochlea lacks collateral circulation, making it susceptible to hemodynamic effects (15). Studies have shown that various vascular injuries and oxidative stress have a more significant impact on the base of the cochlea, so cochlear damage tends to spread from the base to the top (13). Based on the penetration of the round window membrane, infections outside the inner ear may cause cochlear damage even if the infection does not enter the labyrinth. Studies have shown that middle ear infections can damage the basal corner of the cochlea (37). A prognostic analysis of SSNHL based on inflammation levels also showed that cochlear ischemic changes with high levels of inflammation can make high-frequency hearing levels more vulnerable and difficult to recover from damage (38). Therefore, the base of the cochlea is very fragile.
Audiograms are thought to correlate with prognosis in SSNHL, with low-frequency decreased SSNHL having a favorable prognosis and full-frequency hearing decreased poor prognosis (8, 39). In our study, this effect was not found in an adjusted multivariate analysis. After adjusting for possible influencing factors such as age, concomitant symptoms, cardiovascular inflammatory markers, and audiograms, we found that hearing at 8,000 Hz mainly affects the prognosis of SSNHL. Several studies have shown that when vascular, endocrine and immune dysfunction accompany hearing loss, high-frequency hearing impairment first appears, of which 8,000 is common (40–45). In a per-frequency predictive model, high-frequency hearing loss in SSNHL patients was more difficult to recover than other frequencies, and this correlation was more pronounced at 8,000 Hz (46).
To our knowledge, this is the first study that adjusted for multiple factors and used a single frequency as an influencing factor to predict SSNHL and prognosis. Based on the vulnerability characteristics of specific frequencies of the cochlea and the diagnostic criteria for SSNHL, it is logical to predict the prognosis of hearing loss by the vulnerable frequencies before treatment. This study has some limitations. First, as a preliminary study, the reproducibility of the results needs to be validated in a multicenter prospective study. Then, as an adjustment for confounders, we included only blood parameters known to have predictors in SSNHL into the analysis, and future studies should consider and incorporate other possible cardiovascular predictors. Finally, we have a short follow-up period. Although several current literatures suggest that the long-term follow-up hearing changes are 4–5 dB (47–49), which is not higher than the test error of the pure-tone hearing threshold clearly stated in the AAO-HNS guidelines (1). In other words, whether this level of hearing improvement is really clinically meaningful remains to be viewed rationally.
Conclusion
In this study, we explored the relationship of individual frequencies to SSNHL hearing improvement. Unlike previous studies, our study demonstrated that initial 8,000 Hz hearing and not other frequencies were independently associated with hearing improvement. The presence of vertigo and higher hearing at 8,000 Hz may be risk factors for poor prognosis in SSNHL, and these patients may require early combination therapy to increase the likelihood of hearing recovery.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Second Hospital of Anhui Medical University: YJ-YX2019-039. The patients/participants provided their written informed consent to participate in this study.
Author contributions
CL and QF: built the models, analyzed the data, and drafted the manuscript. HC, ZW, CL, and LL: collect and filter data. HC, XQ, YL, and MC: participated in manuscript editing. JY: reviewed the manuscript and support for this assistance was funded. All authors contributed to the article and approved the submitted version.
Funding
The study was supported by funding from the Incubation Program of National Natural Science Foundation of China (Grant No. 2019GMFY06).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chandrasekhar SS, Tsai Do BS, Schwartz SR, Bontempo LJ, Faucett EA, Finestone SA, et al. Clinical practice guideline: sudden hearing loss (update). Otolaryngol Head Neck Surg Off J Am Acad Otolaryngol Head Neck Surg. (2019) 161:S1–45. doi: 10.1177/0194599819859885
2. Byl FM. Seventy-six cases of presumed sudden hearing loss occurring in 1973: prognosis and incidence. Laryngoscope. (1977) 87:817–25. doi: 10.1002/lary.5540870515
3. Alexander TH, Harris JP. Incidence of sudden sensorineural hearing loss. Otol Neurotol Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol. (2013) 34:1586–9. doi: 10.1097/MAO.0000000000000222
4. Weiss BG, Bertlich M, Bettag SA, Desinger H, Ihler F, Canis M. Drug-induced defibrinogenation as new treatment approach of acute hearing loss in an animal model for inner ear vascular impairment. Otol Neurotol Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol. (2017) 38:648–54. doi: 10.1097/MAO.0000000000001400
5. Zhang X, Weng Y, Xu Y, Xiong H, Liang M, Zheng Y, et al. Selected blood inflammatory and metabolic parameters predicted successive bilateral sudden sensorineural hearing loss. Dis Markers. (2019) 2019:7165257. doi: 10.1155/2019/7165257
6. Li C, Zhou H, Feng Y, Zhao Y, Wang J, Chen Z, et al. Coagulation states in patients with sudden sensorineural hearing loss evaluated by thromboelastography. Otolaryngol–Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. (2021) 164:1280–6. doi: 10.1177/0194599820965240
7. Michel O. Deutsche Gesellschaft für Hals-Nasen-Ohren-Heilkunde, Kopf- und Hals-Chirurgie. The revised version of the german guidelines “sudden idiopathic sensorineural hearing loss”. Laryngorhinootologie. (2011) 90:290–3. doi: 10.1055/s-0031-1273721
8. Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery; Society of Otorhinolaryngology Head and Neck Surgery Chinese Medical Association. Guideline of diagnosis and treatment of sudden deafness. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. (2015) 50:443–7.
9. Schweinfurth JM, Cacace AT. Cochlear ischemia induced by circulating iron particles under magnetic control: an animal model for sudden hearing loss. Am J Otol. (2000) 21:636–40.
10. Nakashima T, Naganawa S, Sone M, Tominaga M, Hayashi H, Yamamoto H, et al. Disorders of cochlear blood flow. Brain Res Brain Res Rev. (2003) 43:17–28. doi: 10.1016/S0165-0173(03)00189-9
11. Stakhovskaya O, Sridhar D, Bonham BH, Leake PA. Frequency map for the human cochlear spiral ganglion: implications for cochlear implants. J Assoc Res Otolaryngol JARO. (2007) 8:220–33. doi: 10.1007/s10162-007-0076-9
12. Wu PZ, Liberman LD, Bennett K, de Gruttola V, O'Malley JT, Liberman MC. Primary neural degeneration in the human cochlea: evidence for hidden hearing loss in the aging ear. Neuroscience. (2019) 407:8–20. doi: 10.1016/j.neuroscience.2018.07.053
13. Wong ACY, Ryan AF. Mechanisms of sensorineural cell damage, death and survival in the cochlea. Front Aging Neurosci. (2015) 7:58. doi: 10.3389/fnagi.2015.00058
14. Sun H, Qiu X, Hu J, Ma Z. Comparison of intratympanic dexamethasone therapy and hyperbaric oxygen therapy for the salvage treatment of refractory high-frequency sudden sensorineural hearing loss. Am J Otolaryngol. (2018) 39:531–5. doi: 10.1016/j.amjoto.2018.06.004
15. Mosnier I, Stepanian A, Baron G, Bodenez C, Robier A, Meyer B, et al. Cardiovascular and thromboembolic risk factors in idiopathic sudden sensorineural hearing loss: a case-control study. Audiol Neurootol. (2011) 16:55–66. doi: 10.1159/000312640
16. Atay G, Kayahan B, Çinar BÇ, Saraç S, Sennaroglu L. Prognostic factors in sudden sensorineural hearing loss. Balk Med J. (2016) 33:87–93. doi: 10.5152/balkanmedj.2015.15216
17. Shen Y, Zheng Z, Xiao L, Liu C, Guo J, Chen Z, et al. Association of glycosylated hemoglobin a1c level with sudden sensorineural hearing loss: a prospective study. Front Endocrinol. (2021) 12:763021. doi: 10.3389/fendo.2021.763021
18. Zheng Z, Liu C, Shen Y, Xia L, Xiao L, Sun Y, et al. Serum albumin levels as a potential marker for the predictive and prognostic factor in sudden sensorineural hearing loss: a prospective cohort study. Front Neurol. (2021) 12:747561. doi: 10.3389/fneur.2021.747561
19. Zheng Z, Shen Y, Xia L, Xiao L, Sun Y, Wang H, et al. Thyroid-related hormone levels in clinical patients with moderately severe-to-profound sudden sensorineural hearing loss: a prospective study. Front Neurol. (2021) 12:753270. doi: 10.3389/fneur.2021.753270
20. Durmuş K, Terzi H, Karataş TD, Dogan M, Uysal IÖ, Sencan M, et al. Assessment of hematological factors involved in development and prognosis of idiopathic sudden sensorineural hearing loss. J Craniofac Surg. (2016) 27:e85–91. doi: 10.1097/SCS.0000000000002241
21. Yoshida Y, Yamauchi S, Shinkawa A, Horiuchi M, Sakai M. Immunological and virological study of sudden deafness. Auris Nasus Larynx. (1996) 23:63–8. doi: 10.1016/S0385-8146(96)80010-1
22. Cho Y, Kim J, Oh SJ, Kong SK, Choi SW. Clinical features and prognosis of severe-to-profound sudden sensorineural hearing loss. Am J Otolaryngol. (2022) 43:103455. doi: 10.1016/j.amjoto.2022.103455
23. Yu H, Li H. Association of vertigo with hearing outcomes in patients with sudden sensorineural hearing loss: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. (2018) 144:677–83. doi: 10.1001/jamaoto.2018.0648
24. Xiong W, Dai Q, Wang Y, Hou Z, Lu K, Sun X, et al. Idiopathic sudden sensorineural hearing loss in different ages: prognosis of patients with initial total hearing loss. Front Psychol. (2022) 13:818967. doi: 10.3389/fpsyg.2022.818967
25. Nakata T, Okada M, Hanari T, Takagi T, Fujiwara T, Hato N. Association of the prognosis and severity of idiopathic sudden sensorineural hearing loss with cervical ultrasonographic findings. Auris Nasus Larynx. (2021) 48:1074–80. doi: 10.1016/j.anl.2021.03.004
26. Kim JY, Hong JY, Kim DK. Association of sudden sensorineural hearing loss with risk of cardiocerebrovascular disease: a study using data from the Korea national health insurance service. JAMA Otolaryngol Head Neck Surg. (2018) 144:129–35. doi: 10.1001/jamaoto.2017.2569
27. Sancaktar ME, Agri I, Çeçen AB, Akgül G, Çelebi M. The prognostic value of circulating inflammatory cell counts in sudden sensorineural hearing loss and the effect of cardiovascular risk factors. Ear Nose Throat J. (2020) 99:464–9. doi: 10.1177/0145561320920968
28. Cavaliere M, De Luca P, Scarpa A, Ralli M, Bottiglieri P, Cassandro E, et al. SCORE risk scale as a prognostic factor after sudden sensorineural hearing loss. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg. (2020) 277:953–4. doi: 10.1007/s00405-019-05771-4
29. Guo Y, Liu J. The Roles played by blood inflammatory parameters in sudden sensorineural hearing loss. Ear Nose Throat J. (2021) 18:145561320960355. doi: 10.1177/0145561320960355
30. Cayir S, Kayabasi S, Hizli O. Predictor parameters for poor prognosis in patients with sudden sensorineural hearing loss: fibrinogen to albumin ratio vs. C-reactive protein to albumin ratio. Braz J Otorhinolaryngol. (2021) 87:457–61. doi: 10.1016/j.bjorl.2020.06.010
31. Kang WS, Yang CJ, Shim M, Song CI, Kim TS, Lim HW, et al. Prognostic factors for recovery from sudden sensorineural hearing loss: a retrospective study. J Audiol Otol. (2017) 21:9–15. doi: 10.7874/jao.2017.21.1.9
32. Korres S, Stamatiou GA, Gkoritsa E, Riga M, Xenelis J. Prognosis of patients with idiopathic sudden hearing loss: role of vestibular assessment. J Laryngol Otol. (2011) 125:251–7. doi: 10.1017/S0022215110002082
33. Wang Y, Wang L, Jing Y, Yu L, Ye F. Association between hearing characteristics/prognosis and vestibular function in sudden sensorineural hearing loss with vertigo. Front Neurol. (2020) 11:579757. doi: 10.3389/fneur.2020.579757
34. Kim JS, Lopez I, DiPatre PL, Liu F, Ishiyama A, Baloh RW. Internal auditory artery infarction: clinicopathologic correlation. Neurology. (1999) 52:40–4. doi: 10.1212/WNL.52.1.40
35. Muthu V, Rohacek AM, Yao Y, Rakowiecki SM, Brown AS, Zhao YT, et al. Genomic architecture of Shh-dependent cochlear morphogenesis. Dev Camb Engl. (2019) 146:dev181339. doi: 10.1101/665091
36. Raphael Y, Altschuler RA. Structure and innervation of the cochlea. Brain Res Bull. (2003) 60:397–422. doi: 10.1016/S0361-9230(03)00047-9
37. Hunter LL, Margolis RH, Rykken JR, Le CT, Daly KA, Giebink GS. High frequency hearing loss associated with otitis media. Ear Hear. (1996) 17:1–11. doi: 10.1097/00003446-199602000-00001
38. Seo YJ, Jeong JH, Choi JY, Moon IS. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio: novel markers for diagnosis and prognosis in patients with idiopathic sudden sensorineural hearing loss. Dis Markers. (2014) 2014:702807. doi: 10.1155/2014/702807
39. Chinese sudden hearing loss multi-center clinical study group. Prospective clinical multi-center study on the treatment of sudden deafness with different typings in China. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. (2013) 48:355–61.
40. Chen CK, Shen SC, Lee LA, Sun MH, Chen NH, Chuang LP, et al. Idiopathic sudden sensorineural hearing loss in patients with obstructive sleep apnea. Nat Sci Sleep. (2021) 13:1877–85. doi: 10.2147/NSS.S331880
41. Oghan F, Coksuer H. Does hyperandrogenism have an effect on hearing loss in patients with polycystic ovary syndrome? Auris Nasus Larynx. (2012) 39:365–8. doi: 10.1016/j.anl.2011.06.006
42. Sun XM, Zhuang SM, Xiao ZW, Luo JQ, Long Z, Lan LC, et al. Autoimmune thyroiditis in patients with sudden sensorineural hearing loss. Laryngoscope Investig Otolaryngol. (2022) 7:571–7. doi: 10.1002/lio2.755
43. Ak E, Harputluoglu U, Oghan F, Baykal B. Behçet's disease and hearing loss. Auris Nasus Larynx. (2004) 31:29–33. doi: 10.1016/j.anl.2003.07.006
44. Al-Sofiani M, MacLeod S, Ghanim H, Stecker N, Hall J, Lippes H. Type 1 diabetes and hearing loss: audiometric assessment and measurement of circulating levels of soluble receptor for advanced glycation end products. Diabetes Metab Res Rev. (2020) 36:e3312. doi: 10.1002/dmrr.3312
45. Esparza CM, Jáuregui-Renaud K, Morelos CMC, Muhl GEA, Mendez MN, Carillo NS, et al. Systemic high blood pressure and inner ear dysfunction: a preliminary study. Clin Otolaryngol Off J ENT-UK Off J Neth Soc Oto-Rhino-Laryngol Cervico-Facial Surg. (2007) 32:173–8. doi: 10.1111/j.1365-2273.2007.01442.x
46. Kawamura Y, Suzuki H, Nguyen TN, Ohkubo JI, Wakasugi T, Kitamura T. Frequency-specific prediction model of hearing outcomes in patients with idiopathic sudden sensorineural hearing loss. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg. (2022) 279:4727–33. doi: 10.1007/s00405-021-07246-x
47. Na G, Kim KW, Jung KW, Yun J, Cheong TY, Lee JM. Delayed recovery in idiopathic sudden sensorineural hearing loss. J Clin Med. (2022) 11:2792. doi: 10.3390/jcm11102792
48. Kang SM, Lim HW Yu H. Idiopathic sudden sensorineural hearing loss in dialysis patients. Ren Fail. (2018) 40:170–4. doi: 10.1080/0886022X.2018.1450760
Keywords: sudden sensorineural hearing loss (SSNHL), cochlea, predictive, prognostic, frequency
Citation: Liang C, Fang Q, Chen H, Wang Z, Qiao X, Liao Y, Lv C, Chen M, Li L and Yang J (2022) Vulnerable frequency as an independent prognostic factor for sudden sensorineural hearing loss. Front. Neurol. 13:962376. doi: 10.3389/fneur.2022.962376
Received: 06 June 2022; Accepted: 12 September 2022;
Published: 27 September 2022.
Edited by:
Jose Antonio Lopez-Escamez, Universidad de Granada, SpainReviewed by:
Juan Carlos Amor-Dorado, Hospital Can Misses, SpainTeru Kamogashira, The University of Tokyo, Japan
Copyright © 2022 Liang, Fang, Chen, Wang, Qiao, Liao, Lv, Chen, Li and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianming Yang, entjianming@163.com
 Chaoqun Liang
Chaoqun Liang Jianming Yang
Jianming Yang