General Public’s knowledge, awareness, and perception of Cardiometabolic diseases: data from a Singapore study population
- 1Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, Singapore
- 2Yong Loo Lin School of Medicine, National University Singapore, Singapore, Singapore
- 3Division of Gastroenterology and Hepatology, Department of Medicine, National University Hospital, Singapore, Singapore
- 4National University Polyclinics, National University Health System, Singapore, Singapore
- 5Division of Family Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 6Nursing Department, National University Heart Centre, Singapore, Singapore
- 7Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University Singapore, Singapore, Singapore
- 8Faculty of Science, Monash University, Melbourne, VIC, Australia
- 9Department of Endocrinology, National University Hospital, Singapore, Singapore
- 10Department of Cardiology, National University Heart Centre, National University Health System, Singapore, Singapore
- 11Division of Cardiology, Department of Medicine, Ng Teng Fong General Hospital, Singapore, Singapore
- 12National University Centre for Organ Transplantation, National University Health System, Singapore, Singapore
Background: Health literacy and illness perception play crucial roles in tackling the cardiometabolic disease epidemic. We aim to compare the attitudes, knowledge, self-perceived risks and actions taken, between individuals with and without metabolic risk factors (MFs).
Methods: From 5 June to 5 October 2022, participants of the general public were invited to complete a self-administered questionnaire. MF status was defined as the presence of hypertension, hyperlipidemia, diabetes mellitus and/or current/previous smoking. Participants were assessed based on four categories (knowledge-based, attitude-based, perceived risk, and action-based) of questions pertaining to four cardiometabolic diseases – diabetes mellitus, hypertension, hyperlipidemia, and non-alcoholic fatty liver disease.
Results: A total of 345 participants were enrolled, of whom 34.5% had at least one MF. Compared to those without MFs, participants with MFs had lower knowledge scores, but higher perceived risk scores across all cardiometabolic diseases. The largest knowledge gap pertained to hypertension-related questions. After adjustment, linear regression demonstrated that the presence of MFs (β:2.752, 95%CI: 0.772–4.733, p = 0.007) and higher knowledge scores (β:0.418, 95%CI: 0.236–0.600, p < 0.001) were associated with higher perceived risk. Despite increased perceived risk in those with MFs, this translated to only few increased self-reported preventive actions, when compared to those without MFs, namely the reduction in red meat/processed food consumption (p = 0.045) and increase in fruits/vegetables consumption (p = 0.009).
Conclusion: This study identified a vulnerable subpopulation living with MFs, with high perceived risks, and discordant levels of knowledge and preventive actions taken. Nationwide efforts should be channeled into addressing the knowledge-to-action gap.
1. Introduction
The rising cardiometabolic disease epidemic is a global health concern, with worrisome trends of disease burden and morbidity over the past decades (1–3). In Asia, nearly a fifth of the adult population is affected by cardiometabolic diseases (4). Based on the National Population Health Survey 2021 (5), the prevalence of hypertension and hyperlipidemia in Singapore was 15.7 and 13.9% respectively, while the prevalence of diabetes mellitus and was 6.9%. Cardiometabolic diseases exist in tandem with one another, often sharing similarities in underlying pathomechanisms including insulin resistance and metabolic dysregulation. In the later stages, they can manifest as clinically identifiable pre-disease states of metabolic syndrome and prediabetes, eventually resulting in cardiovascular diseases and diabetes mellitus (6). In contrast to Western populations, there is a higher prevalence of metabolic dysfunction at relatively lower levels of obesity in Asian populations, which makes the identification and management of these silent metabolic disorders even more challenging (7–10). Increasingly, the individual’s own illness perception and understanding of their medical condition have been shown to have significant effects on readmission rates and recovery for many diseases (11, 12). This has been attributed to higher medication compliance (13, 14) and adherence to lifestyle changes (15) in individuals with better disease knowledge and positive illness perceptions. With multi-disciplinary approaches to managing cardiometabolic disease often hinging on lifestyle modifications and medication adherence as the cornerstone of primary prevention (16–19), there is an urgent need to understand the public’s knowledge and illness perception that can prove useful for important stakeholders in healthcare policymaking in the concerted efforts to derail the incoming metabolic wave (20–23).
While the current literature has explored the perception of cardiometabolic disease in the Western population (24), there is limited data on the knowledge and perception of cardiometabolic diseases within the Singaporean population (25, 26). Given the unique cultural and socio-economic factors that influence risk perception and actions (27), this study aims to provide insights into the perception of cardiometabolic diseases the Singapore population by exploring the general public’s attitudes and knowledge of the disease, self-perceived risks and actions taken to improve metabolic health, stratified by the presence of metabolic risk factors (MFs). These unique perspectives can help inform policy makers on the vital components of cardiometabolic diseases that needs to be addressed, as well as the identification of vulnerable population subgroups that may benefit from targeted interventions.
2. Materials and methods
2.1. Study design and population
This cross-sectional study was conducted from 5 June 2022 to 5 October 2022. Participants were recruited through convenience sampling. The online survey was disseminated to personal contacts, via social media and through mailing lists, and participants forwarded the survey link to other individuals that met the eligibility criteria. The study was open to all participants aged 21 years and above, residing in Singapore.
2.2. Data collection
All participants willing to participate in the study filled in an online self-administered English questionnaire secured by FormSg. Implied consent was indicated through the voluntary completion of the online questionnaire. Baseline characteristics such as age, sex, ethnicity, and anthropometric variables were recorded. Participants were stratified into two groups, participants with MFs and those without. The presence of MFs was defined as the self-reported presence of hypertension, hyperlipidemia, diabetes mellitus and current or ex-smoking.
2.3. Instrument
The questionnaire was developed and adapted for the use in our Singaporean cohort, based on previous validated psychometric tools (28–32). It is sectioned into four main categories – knowledge-based, attitude-based, risk perception, and action-based questions. Knowledge-based questions evaluated participants’ understanding of the metabolic diseases including their awareness of the disease, perception of the risk factors, reversibility, and complications of the disease. Attitude-based questions examined the perceived importance of factors including lifestyle modifications and medications in improving the course of the disease. Risk perception questions measured both the cognitive and affective aspect of patients’ perception of susceptibility to developing complications of cardiometabolic diseases. Action-based questions evaluated participants’ willingness in taking action toward mitigating cardiometabolic risks. These questions were raised in the survey in relation to each of the four cardiometabolic diseases that were being studied, namely hypertension, hyperlipidemia, diabetes mellitus and non-alcoholic fatty liver disease (NAFLD). The study was approved by the local institutional review committee in accordance with the revised Declaration of Helsinki (National Healthcare Group Domain Specific Review Board Ref: 2022/00097).
2.4. Statistical analysis
The study outcomes included participants’ knowledge and attitude toward cardiometabolic diseases, their perceived risk of cardiometabolic complications, and actions taken to mitigate these risks, based on the individual’s MF status.
Knowledge scores were computed in accordance to the latest guideline recommendations (33, 34), with the objective of gaging participants’ understanding of specific cardiometabolic diseases. The knowledge-based point system was developed with reference to a study (35) by Al-Hanawi et al. For knowledge questions on a Likert scale, scores were assigned based on the following: “Strongly Disagree,” “Disagree” and “Neutral” were assigned 0 points, while “Agree” and “Strongly Agree” were assigned 1 point. For the remaining questions, correct responses were assigned a score of 1, and incorrect or uncertain answers were assigned a score of 0. Perceived risk scores comprising of both the affective and cognitive component were developed to evaluate the extent of the participants’ perceived susceptibility to cardiometabolic diseases and the complications (32). The cognitive aspect was assessed on the following scale (“Very High Risk” = 5 points, “High Risk” = 4 points, “Neutral” = 3 points, “Low Risk” = 2 points, “Very Low Risk” = 1 point). Higher perceived risk scores signified that the individual perceives their own risk of developing an adverse event to be increased. The affect aspect, participants’ level of concern was evaluated on a scale (“Not Worried at All” = 1 point, “A Little Worried” = 2 points, “Somewhat Worried” = 3 points, “Worried” = 4 points and “Very Worried” = 5 points). Based on the cumulated perceived risk score, a multivariable linear regression model was constructed to examine independent predictors of increased perceived risk, which included covariates such as age, sex, ethnicity, marital status, education levels, presence of MFs, and knowledge-based score (36).
The analysis was conducted using IBM SPSS statistics 25 (SPSS Inc., Chicago, IL) and RStudio (Version 4.2.2). Categorical variables were expressed as numbers (percentages) and continuous variables were expressed as mean (standard deviation). Pearson’s chi-square test was used to compare categorical variables, 2-sample T test (or Mann–Whitney U test, where appropriate) for the comparison of continuous and ordinal variables. A p <0.05 was deemed statistically significant for this study.
3. Results
3.1. Baseline characteristics
A total of 345 participants were recruited for this study, of whom 226 (65.5%) were participants without MFs and 119 (34.5%) were participants with MFs. Individuals with MFs tended to be older (55 ± 11 years) and more likely to be male (44.5%), compared to those without MFs (37 ± 12 years, 35.8% male). Ethnicity did not vary significantly between the groups, with the majority being Chinese (89.0%), followed by Malay (5.8%), and Indian (2.6%) within the overall population. Of the study cohort, 7.0% of participants had the diagnosis of diabetes mellitus, 3.8% had prediabetes, 16.8% had hypertension, 26.8% had hyperlipidemia, and 10.5% were current/ex-smokers. The demographics and clinical characteristics of participants are appended in Table 1. All participants completed the surveys without any missing data.
3.2. Knowledge and attitude
3.2.1. Hypertension
The majority of the population had heard of hypertension (89.6%), with a higher percentage of those with MFs being aware of hypertension (95.8%) compared to those without MFs (86.3%, p = 0.006). Of the study population, 68.7% agreed that hypertension is a lifelong disease. The large proportion of participants strongly agreed (52.8%) and agreed (38.3%) that hypertension will increase the risk of coronary artery disease and stroke; however, a substantial proportion of participants chose “neutral” (44.3%) when asked if hypertension will increase the risk of fatty liver disease.
Majority of participants felt that lifestyle changes (diet and exercise) were “very important” (74.2%) with regards to the control of blood pressure. Approximately two-thirds of participants found that being compliant to blood pressure medications was “very important” (67.2%) in managing hypertension. There was no difference in responses between those with and without MFs.
3.2.2. Hyperlipidemia
Almost all participants had heard of hyperlipidemia (95.4%). While participants strongly agreed (33.0%) and agreed (43.2%) that hyperlipidemia will increase the risk of fatty liver disease, there was a higher proportion of those without MFs who strongly agreed (35.8%) compared to those with MFs (27.7%, p = 0.024). The majority of participants strongly agreed (58.0%) or agreed (33.0%) that hyperlipidemia will increase the risk of coronary artery disease and stroke, with no differences between the two groups (p = 0.099). Most participants felt that lifestyle changes were “very important” (72.8%) in controlling hyperlipidemia, with no difference in responses between those with and without MFs (p = 0.824).
3.2.3. Diabetes Mellitus
Majority of the population had heard of diabetes mellitus (95.4%), with 78.6% of the population agreeing that it is a lifelong disease. The large proportion of participants strongly agreed (40.0%) and agreed (35.7%) that diabetes mellitus will increase the risk of coronary artery disease and stroke; however, more than a third of participants (36.2%) answered “neutral” when asked if diabetes mellitus will increase the risk of fatty liver disease. Almost all participants felt that lifestyle changes (84.9%) and adherence to prescribed medications (79.1%) were “very important” in controlling diabetes mellitus. There was no difference in responses between those with and without MFs.
3.2.4. Non-alcoholic fatty liver disease
Most participants had heard of NAFLD (90.7%) and agreed that it can be reversed in its early stages (76.8%). A large proportion of participants agreed that fat in liver can cause serious health problems (90.4%) and liver failure (81.8%). There were no differences in responses between those with and without MFs. Majority of the participants either strongly agreed (45.8%) or agreed (35.9%) that excessive alcohol intake would increase the risk of NAFLD and agreed (42.3%) that NAFLD will increase the risk of coronary artery disease and stroke (37). Those without MFs were more likely to agree that family history of NAFLD (46.9% vs. 34.5% respectively, p = 0.030), smoking (36.3% vs. 26.9% respectively, p = 0.043), obesity (42.9% vs. 34.5% respectively, p = 0.024) and physical inactivity (49.1% vs. 32.6% respectively, p = 0.010) will increase the risk of NAFLD, compared to those with MFs.
Many of the participants felt that lifestyle factors were “very important” (72.8%) in treating NAFLD, with a larger proportion of those with MFs choosing “very important” (74.8%) compared to those without MFs (71.7%, p = 0.019). However, while most participants felt that compliance to medications for metabolic diseases was “very important” (53.9%) in the treatment NAFLD, a larger proportion of participants without MFs chose this option (56.6%) than those with MFs (48.7%, p = 0.034).
Overall, participants had good knowledge of cardiometabolic diseases, answering 78.6% of all questions correctly. Participants demonstrated the best knowledge for hyperlipidemia (87.6% of questions answered correctly) and the biggest gaps in knowledge for hypertension (73.8% of questions answered correctly). Participants without MFs had higher knowledge scores on cardiometabolic diseases (80.8% of questions answered correctly) compared to those with MFs (74.4% of questions answered correctly) across all four cardiometabolic diseases. The biggest discrepancy in knowledge scores between participants with and without MFs was pertaining to NAFLD. There is no difference in knowledge scores across the income tiers apart from hyperlipidemia, with a trend toward higher knowledge scores with increasing levels of income. Knowledge scores improved as education level increased from secondary school education (74.8% questions answered correctly) to post-graduate (81.5% questions answered correctly) (Figure 1; Table 2).

Figure 1. Radar figure of knowledge scores (presented as percentages) for each cardiometabolic disease stratified by (A) metabolic factors, (B) education level, and (C) income tiers.
3.3. Perceived risk
In the study cohort, the majority estimated their risk to be “low risk” (25.4%) or “neutral” (51.0%) for coronary artery disease, stroke, NAFLD, and chronic kidney disease. However, those with MFs were more likely to choose “very high risk” (4.4%) or “high risk” (25.9%) for all cardiometabolic complications compared to those without MFs (0.9% very high risk, 10.1% high risk). Similarly, majority of participants were only “somewhat worried” (25.3%) or “a little worried” (28.6%) about their risk of developing cardiometabolic diseases and complications. They were most worried about developing strokes (31.0% worried or very worried) and least concerned about incident NAFLD (22.9% worried or very worried). Those with MFs were generally more worried about developing coronary artery disease, stroke, NAFLD and chronic kidney disease compared to those without MFs (Figure 2; Table 3).
Multivariable linear regression demonstrated that the presence of MFs (adjusted β: 2.752, 95%CI: 0.772 to 4.733, p = 0.007) was significantly associated with increased perceived risk after adjusting for age, sex, race, education, and marital status. Higher knowledge scores of cardiometabolic diseases (adjusted β: 0.418, 95%CI: 0.236 to 0.600, p < 0.001) were also associated with higher perceived risk, after adjusting for important confounders (Table 4).
3.4. Actions taken
Only a minority adhered to the recommended guidelines of more than 150 min of moderate intensity exercise (14.8%) and more than 75 min of vigorous-intensity exercise per week (10.1%). Most participants made a conscious effort in cutting down sugar (70.1%), dietary fat (55.7%), red and processed meat (50.1%) in their diet. However, less than half of participants made a conscious effort to reduce salt in their diet (48.4%) or to limit their daily caloric intake (31.6%). Only 35.1% of participants followed the healthy plate recommendations for at least one meal daily. Nevertheless, those with MFs were more likely to agree or strongly agree with making a conscious effort in reducing red and processed meat consumption (p = 0.009), as well as having at least 2 servings of fruits and vegetables a day (p = 0.045), compared to those without MFs (Figure 3, Table 3).
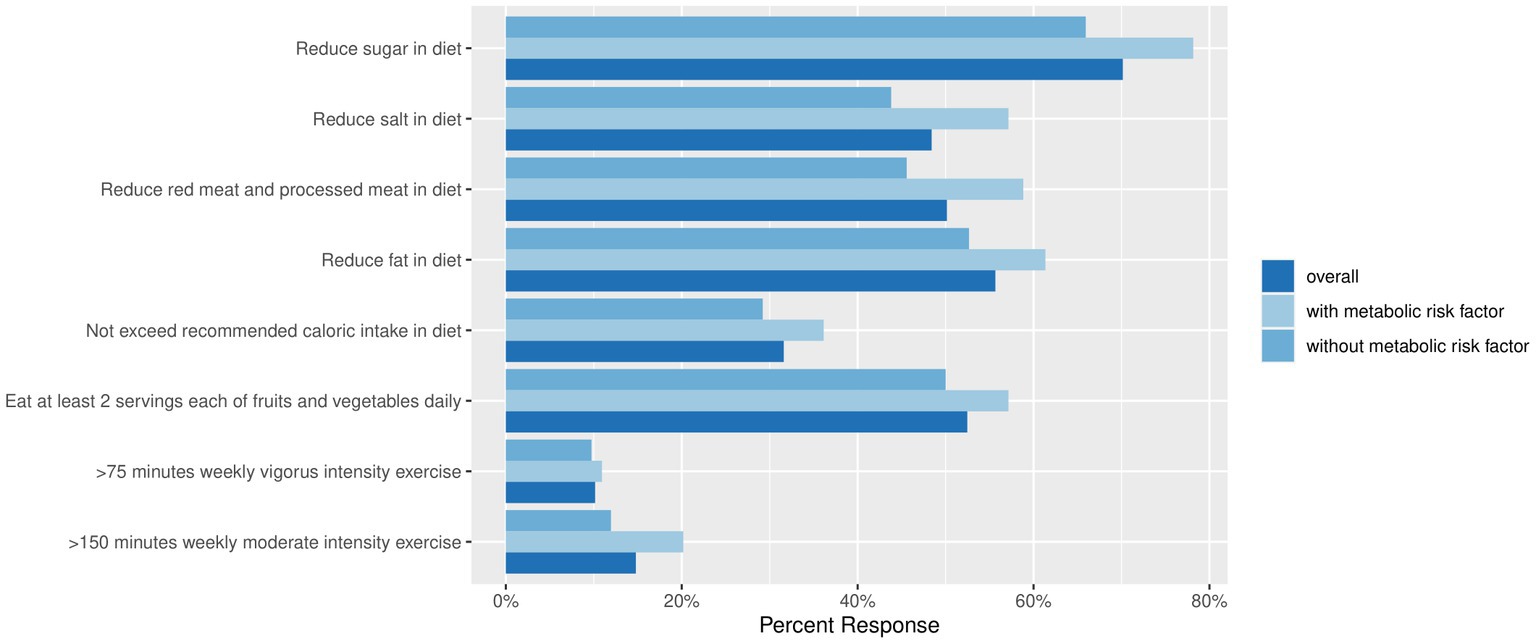
Figure 3. The percentage of study population undertaking actions to improve metabolic health, stratified by the presence of metabolic risk factors.
4. Discussion
Our findings are concordant with current literature, showing heterogeneity in the knowledge across various cardiometabolic diseases and subgroups of the population (38). In recent years, cardiometabolic diseases have been on the rise across the globe (39), especially in Asia, attributed to globalization, socioeconomic changes, technological advancements, and sedentary living (5, 40–42). The study extends the current literature by providing a comprehensive overview of the associations between knowledge, attitudes, perceived risk, and actions taken toward cardiometabolic health in a multi-ethnic Singaporean population. There are several pertinent findings: (1) knowledge on cardiometabolic diseases and the presence of MFs are closely linked to an individual’s perception of disease; (2) The largest knowledge gap among all the cardiometabolic diseases pertains to hypertension. However, when comparing to individuals without MFs, those with MFs had lower knowledge scores on all cardiometabolic domains with the largest discrepancy demonstrated in knowledge scores related to NAFLD; (3) Despite the increased perceived risk in those with MFs, this translated to only a few increased self-reported actions taken to address metabolic health, compared to those without MFs – namely red meat and processed food reduction, and adequate fruits/vegetables intake. The lowest adherence to preventive recommendations pertained to those related with physical activity. The study highlights a vulnerable group of individuals living with cardiometabolic disease, with lower levels of knowledge scores and self-reported action plans, that appear discordant to the self-perceived risk of cardiometabolic complications.
The study highlights that the increased knowledge on cardiometabolic diseases is closely associated with an increase in the individual’s perceived risk of cardiometabolic disease. We postulate that this observation may be attributed to public education and awareness of cardiometabolic diseases, thus equipping individuals to comprehend the modifiable lifestyle factors that can mitigate the risk of metabolic diseases. Evidence has shown that education remains the key component in primary prevention (24, 43). However, for this to be effective, the “knowledge-to-action gap” where the knowledge of individuals fails to translate to tangible behavioral change needs to be concurrently addressed (44). Based on previous studies, knowledge of a condition must be coupled with knowledge of the treatment and the reasons for treatment compliance (45–47). With a strong baseline understanding of the condition, channeling resources into helping patients understand how daily efforts to improve their diet or increase physical activity can positively impact their condition (48–50). This may be effective in bridging the gap between knowledge of a condition and actions taken. Coupled with improving health literacy in our modern-day society, there is an increasing role for active public involvement and empowering individuals to take charge of their own health. Healthier SG (51) is a national program in Singapore that focuses on empowering the public in understanding and taking initiative toward adopting preventive measures to sustain health within the community and to manage their chronic conditions proactively.
The presence of MFs can also alter the perception and knowledge of cardiometabolic diseases. Those with MFs were more likely to have higher perceived risk of metabolic disease complications. This is important as self-perceived susceptibility to cardiometabolic diseases can serve as motivation toward taking early preventive measures, which in turn modifies the course of cardiometabolic risks and their complications (52). However, the study highlights several gaps that need to be addressed. Those with MFs had lower knowledge scores on all cardiometabolic domains when compared to their counterparts without MFs. Although it is plausible that the higher baseline knowledge of cardiometabolic diseases has equipped individuals to take preemptive measures early to mitigate the risk of cardiometabolic diseases (53), this still raises concerns over the discrepancy in the knowledge gap in those living with cardiometabolic diseases (54, 55). Despite the increased perceived susceptibility of those with MFs, it is concerning that this did not appear to translate into self-reported actions taken to improve metabolic health. This may be due to the lack of knowledge on the cardiometabolic diseases, lack of self-efficacy or motivation as suggested by previous studies (52). Previous studies have also shown that an individual’s health literacy is key in the self-management of cardiometabolic diseases (56, 57). We demonstrated that the knowledge scores increased across all cardiometabolic diseases with higher levels of education, but not with higher income. This may be attributed to higher levels of health literacy (58), with education on cardiometabolic diseases playing a significant role in disease prevention. While social economic status may play a part, its role is less defined. Future studies could explore the discrepancies and the barriers that individuals with MFs may experience in trying to mitigate their cardiometabolic risks.
There were several disease-specific knowledge gaps that should be addressed in public education efforts. Knowledge on hyperlipidemia received the highest scores, while the lowest scores were observed for hypertension (59). This is concerning because hypertension is the commonest chronic condition in Singapore. Previous studies have suggested collaborative health education between patients and clinicians as a cornerstone in improving self-management of hypertension (60). Interestingly, participants shared the least concern toward the cardiometabolic complications of NAFLD (61, 62), and we postulate that the reasons for this observation may be multifactorial (63). The greatest cardiometabolic concern for participants was the chance of getting a stroke, with the least concern shown for NAFLD. We postulate that the lack of concern for NAFLD is a result of the following factors; first, there is an underdiagnosis of NAFLD by physicians across the globe (64–67), possibly contributed by the knowledge gap in the identification and diagnosis of NAFLD, as well as the limited treatment options in NAFLD (63, 68, 69). Second, less media portrayal and patient education on NAFLD, relative to that of stroke and coronary artery disease, may have been contributing factors (70, 71). Consequently, the above factors may translate to a lower level of awareness of NAFLD, its severity and consequences, among the general population.
Within the Asian community, studies have shown that the general population tend to lead sedentary lifestyles, spending a significant amount of time sitting down at work, while commuting, and during leisure activities (72, 73). Although most study participants tried to improve their diets by reducing their sugar, red meat, and processed foods intake, only a minority made conscious efforts to increase physical activity, with less than a sixth of participants achieving the Health Promotion Board recommendations of 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity per week (74). This showcases the need for greater public health messaging to incentivize individuals to adopt a more active lifestyle. One such example is the National Steps Challenge that gives participants instant rewards for clocking in steps and doing moderate-vigorous physical activities (75). While these national initiatives are promising forays in encouraging the adoption of physical activity nationwide (76), they share the common pitfalls of other similar mobile health initiatives. Leveraging on novelty and financial incentives, participants were only actively engaged in the first third of the National Steps Challenge programme (77). This highlights the need for other social, cultural and environmental factors (78) to be concurrently addressed for the benefit of lifestyle interventions to be sustainable. At present, the mindset within the population may not be completely receptive toward preventive measures, with the National Population Health Survey 2021 reporting that a substantial proportion of the public expressing that it is not necessary to go for health screenings as they are already healthy (5).
Moving forward, the findings from this study can be used to tailor appropriate healthcare policies, especially towards the Singaporean population. In the 21st century, with an increasingly obesogenic environment, coupled with poor nutrition and sedentarism (54, 79, 80), the burden of cardiometabolic diseases is expected to rise further in Asia (81, 82). It is therefore paramount that early action is taken to mitigate this public health burden. Our study emphasizes the importance of targeting the public’s knowledge on cardiometabolic diseases, which is closely associated with the perception of disease and risk. This can serve as catalysts for necessary changes to the attitudes and preventive actions taken to sustain metabolic health (83). Furthermore, the study identifies the vulnerable group of individuals living with metabolic disease, with lower levels of knowledge and action plans that is discordant to their increased perceived risk. Our findings highlight an urgent need to modify policy development in implementing more targeted preventive strategies with an emphasis on the population with metabolic diseases. Interventions should target the root causes of cardiometabolic diseases by tackling issues with knowledge, attitudes and perception, and lifestyle modifications (53, 84). As these metabolic diseases do not exist in silos, prioritizing upstream solutions can help mitigate the overall metabolic milieu of the individual, with the potential benefit of reducing downstream healthcare demands and expenditure.
4.1. Study limitations
This study is the first to explore knowledge, attitudes, and perceived risk of cardiometabolic diseases and the action taken to mitigate cardiometabolic risks in a multi-ethnic Singaporean population. However, the study has its limitations. First, as the study used convenience sampling, results may not be generalizable to the entire population, and hence the study results should be interpreted with caution. Although our preliminary results are hypothesis-generating, the findings shed light on the understudied perceptions and attitudes of the general public toward the rising metabolic epidemic. This provides an important platform for future systematic probabilistic sampling with adequately powered sample size calculations to validate the current findings. Second, due to the voluntary nature of the survey, individuals who participate in the survey may tend to have differential concerns of their health, thus introducing self-selection bias to the included study population. This selection bias may lead to an overestimation of the awareness of cardiometabolic disease in the Singapore population. Third, while the questionnaire we used was validated in other published studies, they have not been validated in a Singaporean population. Fourth, the survey was distributed in English, hence there may be a risk in response errors especially among those with limited proficiency in English.
5. Conclusion
In the silent metabolic disease epidemic, there appears to be disparate levels of knowledge, attitude, perceived risks, and actions taken toward metabolic health in the study population living in Singapore. The preliminary study findings highlighted a vulnerable subpopulation of individuals living with metabolic risk factors, with high perceived risks, and discordant levels of knowledge and preventive actions taken. Future powered studies with systematic probabilistic sampling will be the next important step to validate the study findings. Nevertheless, our preliminary findings suggest that consolidated efforts should be channeled into addressing the knowledge-to-action gap, with the unified goal of sustaining optimal metabolic health.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by National Healthcare Group Domain Specific Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
VA and RG conceptualized, acquired, and analyzed data. BN, SK, and NC designed the work and interpreted the data. JL, NN, JC, YL, YC, BC, GK, BT, ZL, CK, LG, PL, PC, MD, MC, RF, and MM drafted the work and substantially revised it. All authors read and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
MF – Metabolic risk factor; NAFLD – Non-alcoholic fatty liver disease.
References
1. Cheng, X, Ma, T, Ouyang, F, Zhang, G, and Bai, Y. Trends in the prevalence of Cardiometabolic multimorbidity in the United States, 1999-2018. Int J Environ Res Public Health. (2022) 19:4726. doi: 10.3390/ijerph19084726
2. Ferdinand, KC. Global perspectives on cardiometabolic risk and cardiovascular disease: from basic science to bedside. Ann Transl Med. (2018) 6:290. doi: 10.21037/atm.2018.07.28
3. Chew, NW, Ng, CH, Tan, DJH, Kong, G, Lin, C, Chin, YH, et al. The global burden of metabolic disease: data from 2000 to 2019. Cell Metab. (2023) 35:414–428.e3. e3. doi: 10.1016/j.cmet.2023.02.003
4. Ranasinghe, P, Mathangasinghe, Y, Jayawardena, R, Hills, AP, and Misra, A. Prevalence and trends of metabolic syndrome among adults in the asia-pacific region: a systematic review. BMC Public Health. (2017) 17:101. doi: 10.1186/s12889-017-4041-1
5. Epidemiology & Disease Control Division and Policy RSG. National Population Health Survey 2021 (Household Interview) (2022) Available at: https://www.moh.gov.sg/docs/librariesprovider5/resources-statistics/reports/national-population-health-survey-2021-report.pdf. (Accessed January 20, 2023).
6. Kong, G, Chew, NWS, Ng, CH, Chin, YH, Lim, OZH, Ambhore, A, et al. Prognostic outcomes in acute myocardial infarction patients without standard modifiable risk factors: a multiethnic study of 8,680 Asian patients. Front Cardiovasc Med. (2022) 9:869168. doi: 10.3389/fcvm.2022.869168
7. Kurpad, AV, Varadharajan, KS, and Aeberli, I. The thin-fat phenotype and global metabolic disease risk. Curr Opin Clin Nutr Metab Care. (2011) 14:542–7. doi: 10.1097/MCO.0b013e32834b6e5e
8. Tang, A, Ng, CH, Phang, PH, Chan, KE, Chin, YH, Fu, CE, et al. Comparative burden of metabolic dysfunction in lean NAFLD vs non-lean NAFLD - a systematic review and meta-analysis. Clin Gastroenterol Hepatol. (2022). doi: 10.1016/j.cgh.2022.06.029
9. Nah, BKY, Ng, CH, Chan, KE, Tan, C, Aggarwal, M, Zeng, RW, et al. Historical changes in weight classes and the influence of NAFLD prevalence: a population analysis of 34,486 individuals. Int J Environ Res Public Health. (2022) 19:9935. doi: 10.3390/ijerph19169935
10. Lin, C, Loke, WH, Ng, BH, Chin, YH, Chong, B, Goh, RSJ, et al. Mortality, cardiovascular and medication outcomes in patients with myocardial infarction and underweight in a meta-analysis of 6.3 million patients. Am J Cardiol. (2023) 196:1–10. doi: 10.1016/j.amjcard.2023.02.023
11. Giri, P, Poole, J, Nightingale, P, and Robertson, A. Perceptions of illness and their impact on sickness absence. Occup Med. (2009) 59:550–5. doi: 10.1093/occmed/kqp123
12. Sawyer, AT, Harris, SL, and Koenig, HG. Illness perception and high readmission health outcomes. Health Psychol Open. (2019) 6:2055102919844504. doi: 10.1177/2055102919844504
13. AlShayban, DM, Naqvi, AA, Alhumaid, O, AlQahtani, AS, Islam, MA, Ghori, SA, et al. Association of Disease Knowledge and Medication Adherence among out-Patients with Type 2 diabetes mellitus in Khobar Saudi Arabia. Front Pharmacol. (2020) 11:60. doi: 10.3389/fphar.2020.00060
14. Sweileh, WM, SeH, Z, Abu Naba, RJ, Deleq, MI, Enaia, MI, Sam, N, et al. Influence of patients’ disease knowledge and beliefs about medicines on medication adherence: findings from a cross-sectional survey among patients with type 2 diabetes mellitus in Palestine. BMC Public Health. (2014) 14:94. doi: 10.1186/1471-2458-14-94
15. Alm-Roijer, C, Stagmo, M, Udén, G, and Erhardt, L. Better knowledge improves adherence to lifestyle changes and medication in patients with coronary heart disease. Eur J Cardiovasc Nurs. (2004) 3:321–17. doi: 10.1016/j.ejcnurse.2004.05.002
16. Lillich, FF, Imig, JD, and Proschak, E. Multi-target approaches in metabolic syndrome. Front Pharmacol. (2020) 11:554961. doi: 10.3389/fphar.2020.554961
17. Grundy, SM, Hansen, B, Smith, SC, Cleeman, JI, and Kahn, RA. Clinical Management of Metabolic Syndrome. Circulation. (2004) 109:551–6. doi: 10.1161/01.CIR.0000112379.88385.67
18. Wang, Q, Chair, SY, Wong, EM, Taylor-Piliae, RE, Qiu, XCH, and Li, XM. Metabolic syndrome knowledge among adults with Cardiometabolic risk factors: a cross-sectional study. Int J Environ Res Public Health. (2019) 16:159. doi: 10.3390/ijerph16010159
19. Amarasekara, P, de Silva, A, Swarnamali, H, Senarath, U, and Katulanda, P. Knowledge, attitudes, and practices on lifestyle and cardiovascular risk factors among metabolic syndrome patients in an urban tertiary Care Institute in Sri Lanka. Asia Pac J Public Health. (2016) 28:32s–40s. doi: 10.1177/1010539515612123
20. Yeong, T, Mai, AS, Lim, OZH, Ng, CH, Chin, YH, Tay, P, et al. Can glucose-lowering medications improve outcomes in non-diabetic heart failure patients? A Bayesian network meta-analysis. ESC Heart Failure. (2022) 9:1338–50. doi: 10.1002/ehf2.13822
21. Chew, NWS, Ng, CH, Truong, E, Noureddin, M, and Kowdley, KV. Nonalcoholic Steatohepatitis drug development pipeline: an update. Semin Liver Dis. (2022) 42:379–17. doi: 10.1055/a-1877-9656
22. Ng, CH, Lin, SY, Chin, YH, Lee, MH, Syn, N, Goh, XL, et al. Antidiabetic medications for type 2 diabetics with nonalcoholic fatty liver disease: evidence from a network meta-analysis of randomized controlled trials. Endocr Pract. (2022) 28:223–17. doi: 10.1016/j.eprac.2021.09.013
23. Chew, NWS, Ng, CH, Muthiah, MD, and Sanyal, AJ. Comprehensive review and updates on holistic approach towards non-alcoholic fatty liver disease management with cardiovascular disease. Curr Atheroscler Rep. (2022) 24:515–2. doi: 10.1007/s11883-022-01027-5
24. Stephens, CR, Easton, JF, Robles-Cabrera, A, Fossion, R, de la Cruz, L, Martínez-Tapia, R, et al. The impact of education and age on metabolic disorders. Front Public Health. (2020) 8:180. doi: 10.3389/fpubh.2020.00180
25. Roystonn, K, AshaRani, PV, Siva Kumar, FD, Wang, P, Abdin, E, Sum, CF, et al. Factor structure of the diabetes knowledge questionnaire and the assessment of the knowledge of risk factors, causes, complications, and management of diabetes mellitus: a national population-based study in Singapore. PLoS One. (2022) 17:e0272745. doi: 10.1371/journal.pone.0272745
26. Fu, CE, Ng, CH, Chew, NWS, Heng, ZEQ, Chin, YH, Quek, J, et al. A poor perspective of self weight significantly increases adverse outcomes in non-alcoholic fatty liver disease (NAFLD). Front Med. (2022) 9:9. doi: 10.3389/fmed.2022.977552
27. Heine, M, Badenhorst, M, Van Zyl, C, De Melo Ghisi, GL, Babu, AS, Buckley, J, et al. Developing a complex understanding of physical activity in Cardiometabolic disease from Low-to-middle-income countries—a qualitative systematic review with meta-synthesis. Int J Environ Res Public Health. (2021) 18:11977. doi: 10.3390/ijerph182211977
28. Kugbey, N, Oppong Asante, K, and Adulai, K. Illness perception, diabetes knowledge and self-care practices among type-2 diabetes patients: a cross-sectional study. BMC Res Notes. (2017) 10:381. doi: 10.1186/s13104-017-2707-5
29. Oliveria, SA, Chen, RS, McCarthy, BD, Davis, CC, and Hill, MN. Hypertension knowledge, awareness, and attitudes in a hypertensive population. J Gen Intern Med. (2005) 20:219–25. doi: 10.1111/j.1525-1497.2005.30353.x
30. Wieland, AC, Mettler, P, McDermott, MT, Crane, LA, Cicutto, LC, and Bambha, KM. Low awareness of nonalcoholic fatty liver disease among patients at high metabolic risk. J Clin Gastroenterol. (2015) 49:e6–e10. doi: 10.1097/MCG.0000000000000075
31. Zelber-Sagi, S, Bord, S, Dror-Lavi, G, Smith, ML, Towne, SD Jr, Buch, A, et al. Role of illness perception and self-efficacy in lifestyle modification among non-alcoholic fatty liver disease patients. World J Gastroenterol. (2017) 23:1881–90. doi: 10.3748/wjg.v23.i10.1881
32. Stol, DM, Hollander, M, Damman, OC, Nielen, MMJ, Badenbroek, IF, Schellevis, FG, et al. Mismatch between self-perceived and calculated cardiometabolic disease risk among participants in a prevention program for cardiometabolic disease: a cross-sectional study. BMC Public Health. (2020) 20:740. doi: 10.1186/s12889-020-08906-z
33. Singapore HPB. 8 Singapore dietary guidelines you must know (2022) Available at: https://www.healthhub.sg/live-healthy/111/living_with_health_8_sets_diet_guidelines (accessed 15 November 2022).
34. Singapore HPB. How much exercise is enough? (2022) Available at: https://www.healthhub.sg/live-healthy/1820/move-more-live-longer#:~:text=Ideally%2C%20we%20should%20aim%20for,aerobic%20physical%20activity%20per%20week (accessed 15 November 2022).
35. Al-Hanawi, MK, Angawi, K, Alshareef, N, Qattan, AMN, Helmy, HZ, Abudawood, Y, et al. Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: a cross-sectional study. Front Public Health. (2020) 8:8. doi: 10.3389/fpubh.2020.00217
36. Hao, F, Wang, B, Tan, W, Husain, SF, McIntyre, RS, Tang, X, et al. Attitudes toward COVID-19 vaccination and willingness to pay: comparison of people with and without mental disorders in China. BJPsych Open. (2021) 7:e146. doi: 10.1192/bjo.2021.979
37. Tang, ASP, Chan, KE, Quek, J, Xiao, J, Tay, P, Teng, M, et al. Non-alcoholic fatty liver disease increases risk of carotid atherosclerosis and ischemic stroke: an updated meta-analysis with 135,602 individuals. Clin Mol Hepatol. (2022) 28:483–6. doi: 10.3350/cmh.2021.0406
38. Huang, Z, Yap, QV, Chan, YH, Ho, JS, Tan, SY, Koh, WP, et al. Knowledge of heart disease, preventive behavior and source of information in a multi-ethnic Asian population: a population-based survey. J Community Health. (2021) 46:31–40. doi: 10.1007/s10900-020-00838-4
39. Chong, B, Kong, G, Shankar, K, Chew, HSJ, Lin, C, Goh, R, et al. The global syndemic of metabolic diseases in the young adult population: a consortium of trends and projections from the global burden of disease 2000–2019. Metabolism. (2023) 141:155402. doi: 10.1016/j.metabol.2023.155402
40. Li, J-J, Yeo, KK, Tan, K, Ako, J, Krittayaphong, R, Tan, RS, et al. Tackling cardiometabolic risk in the Asia Pacific region. Am. J. Prevent. Cardiol. (2020) 4:100096. doi: 10.1016/j.ajpc.2020.100096
41. Huxley, RR, Hirakawa, Y, Hussain, MA, Aekplakorn, W, Wang, X, Peters, SAE, et al. Age- and sex-specific burden of cardiovascular disease attributable to 5 major and modifiable risk factors in 10 Asian countries of the Western Pacific region. Circ J. (2015) 79:1662–74. doi: 10.1253/circj.CJ-15-0661
42. Chongsuvivatwong, V, Phua, KH, Yap, MT, Pocock, NS, Hashim, JH, Chhem, R, et al. Health and health-care systems in Southeast Asia: diversity and transitions. Lancet. (2011) 377:429–7. doi: 10.1016/S0140-6736(10)61507-3
43. Ramôa Castro, A, Oliveira, NL, Ribeiro, F, and Oliveira, J. Impact of educational interventions on primary prevention of cardiovascular disease: a systematic review with a focus on physical activity. Eur J Gen Pract. (2017) 23:59–68. doi: 10.1080/13814788.2017.1284791
44. Hakvoort, L, Dikken, J, Derks, C, Wel, M, and Schuurmans, M. Minimizing the knowledge-to-action gap; identification of interventions to change nurses' behavior regarding fall prevention, a mixed method study. BMC Nurs. (2021) 20:80. doi: 10.1186/s12912-021-00598-z
45. Awwad, O, Akour, A, Al-Muhaissen, S, and Morisky, D. The influence of patients' knowledge on adherence to their chronic medications: a cross-sectional study in Jordan. Int J Clin Pharm. (2015) 37:504–17. doi: 10.1007/s11096-015-0086-3
46. Chin, YH, Lim, O, Lin, C, Chan, YY, Kong, G, Ng, CH, et al. Meta-analysis of the placebo and Nocebo effects associated with placebo treatment in randomized trials of lipid lowering therapy. Eur Heart J Qual Care Clin Outcomes. (2022). doi: 10.1093/ehjqcco/qcac060
47. Ng, CH, Teng, ML, Chew, NW, Chan, KE, Yong, JN, Quek, J, et al. Statins decrease overall mortality and cancer related mortality but are underutilized in NAFLD: a longitudinal analysis of 12,538 individuals. Expert Rev Gastroenterol Hepatol. (2022) 16:895–1. doi: 10.1080/17474124.2022.2119128
48. Ng, C, Xiao, J, Lim, WH, Yip Han, C, Yong, J, Tan, D, et al. Placebo effect on progression and regression in non-alcoholic Steatohepatitis. Evidence from a meta-analysis. Hepatology. (2022) 75:1647–61. doi: 10.1002/hep.32315
49. Ng, CH, Xiao, J, Lim, WH, Chin, YH, Yong, JN, Tan, DJH, et al. Placebo effect on progression and regression in NASH: evidence from a meta-analysis. Hepatology. (2022) 75:1647–61. doi: 10.1002/hep.32315
50. Quek, J, Lim, G, Lim, WH, Ng, CH, So, WZ, Toh, J, et al. The Association of Plant-Based Diet with Cardiovascular Disease and Mortality: a meta-analysis and systematic review of Prospect cohort studies. Front Cardiovasc Med. (2021) 8:756810. doi: 10.3389/fcvm.2021.756810
51. Singapore MOH. White paper on Healthier SG (2022) Available at: https://file.go.gov.sg/healthiersg-whitepaper-pdf.pdf. (Accessed January 20, 2023).
52. Jones, EJ, Appel, SJ, Eaves, YD, Moneyham, L, Oster, RA, and Ovalle, F. Cardiometabolic risk, knowledge, risk perception, and self-efficacy among American Indian women with previous gestational diabetes. J Obstet Gynecol Neonatal Nurs. (2012) 41:246–7. doi: 10.1111/j.1552-6909.2012.01339.x
53. Xu, C, and Cao, Z. Cardiometabolic diseases, total mortality, and benefits of adherence to a healthy lifestyle: a 13-year prospective UK biobank study. J Transl Med. (2022) 20:234. doi: 10.1186/s12967-022-03439-y
54. Anand, VV, Lee Cheng Zhe, E, Chin, YH, Lim, WH, Goh, RSJ, Lin, C, et al. Barriers and facilitators to engagement with a weight management intervention in Asian patients with overweight or obesity: a systematic review. Endocr Pract. (2022). doi: 10.1016/j.eprac.2022.10.006
55. Kong, G, Chew, NWS, Ng, CH, Chin, YH, Zeng, R, Foo, R, et al. Long-term outcomes in acute coronary syndrome patients without standard modifiable risk factors: a multi-ethnic retrospective cohort study of 5400 asian patients. J Thromb Thrombolysis. (2022) 54:569–8. doi: 10.1007/s11239-022-02704-7
56. Dahal, PK, and Hosseinzadeh, H. Association of health literacy and diabetes self-management: a systematic review. Aust J Prim Health. (2019) 25:526–3. doi: 10.1071/PY19007
57. Sudore, RL, Yaffe, K, Satterfield, S, Harris, TB, Mehta, KM, Simonsick, EM, et al. Limited literacy and mortality in the elderly. J Gen Intern Med. (2006) 21:806–2. doi: 10.1111/j.1525-1497.2006.00539.x
58. Teles, M, and Kaya, S. Health literacy of cardiology patients: determinants and effects on patient outcomes. Soc Work Health Care. (2021) 60:656–3. doi: 10.1080/00981389.2021.2014615
59. Ng, CH, Wong, ZY, Chew, NWS, Chan, KE, Xiao, J, Sayed, N, et al. Hypertension is prevalent in non-alcoholic fatty liver disease and increases all-cause and cardiovascular mortality. Front Cardiovasc Med. (2022) 9:942753. doi: 10.3389/fcvm.2022.942753
60. Johnson, HM, LaMantia, JN, Brown, CM, Warner, RC, Zeller, LM, Haggart, RC, et al. My hypertension education and reaching target (MyHEART): development and dissemination of a patient-centered website for Young adults with hypertension. JMIR Cardio. (2017) 1:e5. doi: 10.2196/cardio.8025
61. Ng, CH, Chan, KE, Chin, YH, Zeng, RW, Tsai, PC, Lim, WH, et al. The effect of diabetes and prediabetes on the prevalence, complications and mortality in nonalcoholic fatty liver disease. Clin Mol Hepatol. (2022) 28:565–4. doi: 10.3350/cmh.2022.0096
62. Quek, J, Ng, CH, Tang, ASP, Chew, N, Chan, M, Khoo, CM, et al. Metabolic associated fatty liver disease increases the risk of systemic complications and mortality. A meta-analysis and systematic review of 12 620 736 individuals. Endocr Pract. (2022) 28:667–2. doi: 10.1016/j.eprac.2022.03.016
63. Younossi, ZM, Ong, JP, Takahashi, H, Yilmaz, Y, Eguchi, Y, El Kassas, M, et al. A global survey of physicians knowledge about nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. (2022) 20:e1456–68. doi: 10.1016/j.cgh.2021.06.048
64. Nielsen, EM, Anderson, KP, Marsden, J, Zhang, J, and Schreiner, AD. Nonalcoholic fatty liver disease Underdiagnosis in primary care: what are we missing? J Gen Intern Med. (2022) 37:2587–90. doi: 10.1007/s11606-021-07197-3
65. Goh, GB, Kwan, C, Lim, SY, Venkatanarasimha, NK, Abu-Bakar, R, Krishnamoorthy, TL, et al. Perceptions of non-alcoholic fatty liver disease - an Asian community-based study. Gastroenterol Rep (Oxf). (2016) 4:131–5. doi: 10.1093/gastro/gov047
66. Alexander, M, Loomis, AK, Fairburn-Beech, J, van der Lei, J, Duarte-Salles, T, Prieto-Alhambra, D, et al. Real-world data reveal a diagnostic gap in non-alcoholic fatty liver disease. BMC Med. (2018) 16:130. doi: 10.1186/s12916-018-1103-x
67. Chalasani, N, Younossi, Z, Lavine, JE, Charlton, M, Cusi, K, Rinella, M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. (2018) 67:328–7. doi: 10.1002/hep.29367
68. Fu, CE, Ng, CH, Yong, JN, Chan, KE, Xiao, J, Nah, B, et al. A meta-analysis on associated risk of mortality in nonalcoholic fatty liver disease. Endocr Pract. (2023) 29:33–9. doi: 10.1016/j.eprac.2022.10.007
69. Chan, KE, Ng, CH, Fu, CE, Quek, J, Kong, G, Goh, YJ, et al. The Spectrum and impact of metabolic dysfunction in MAFLD: a longitudinal cohort analysis of 32,683 overweight and obese individuals. Clin Gastroenterol Hepatol. (2022). doi: 10.1016/j.cgh.2022.09.028
70. Tincopa, MA, Wong, J, Fetters, M, and Lok, AS. Patient disease knowledge, attitudes and behaviours related to non-alcoholic fatty liver disease: a qualitative study. BMJ Open Gastroenterol. (2021) 8:e000634. doi: 10.1136/bmjgast-2021-000634
71. Muthiah, M, Ng, CH, Chan, KE, Fu, CE, Lim, WH, Tan, DJH, et al. Type 2 diabetes mellitus in metabolic-associated fatty liver disease vs. type 2 diabetes mellitus non-alcoholic fatty liver disease: a longitudinal cohort analysis. Ann Hepatol. (2023) 28:100762. doi: 10.1016/j.aohep.2022.100762
72. Mahmood, B, Tang, TS, Afshar, R, and Ashe, MC. Objective measurement of physical activity and sedentary behavior among south Asian adults: a systematic review. PLoS One. (2020) 15:e0236573. doi: 10.1371/journal.pone.0236573
73. Lau, JH, Nair, A, Abdin, E, Kumarasan, R, Wang, P, Devi, F, et al. Prevalence and patterns of physical activity, sedentary behaviour, and their association with health-related quality of life within a multi-ethnic Asian population. BMC Public Health. (2021) 21:1939. doi: 10.1186/s12889-021-11902-6
74. Singapore HPB. Health promotion board launches national physical activity guidelines (2011) Available at: https://www.hpb.gov.sg/newsroom/article/health-promotion-board-launches-national-physical-activity-guidelines#:~:text=To%20achieve%20substantial%20health%20benefits,intensity%20physical%20activity%20a%20week. (Accessed January 9, 2023).
75. Yao, J, Tan, CS, Chen, C, Tan, J, Lim, N, and Müller-Riemenschneider, F. Bright spots, physical activity investments that work: National Steps Challenge, Singapore: a nationwide mHealth physical activity programme. Br J Sports Med. (2020) 54:1047–8. doi: 10.1136/bjsports-2019-101662
76. Chin, YH, Ng, CH, Chew, NWS, Kong, G, Lim, WH, Tan, DJH, et al. The placebo response rate and nocebo events in obesity pharmacological trials. A systematic review and meta-analysis. eClinicalMedicine. (2022) 54:101685. doi: 10.1016/j.eclinm.2022.101685
77. Yao, J, Lim, N, Tan, J, Matthias Müller, A, Martinus van Dam, R, Chen, C, et al. Evaluation of a population-wide Mobile health physical activity program in 696 907 adults in Singapore. J Am Heart Assoc. (2022) 11:e022508. doi: 10.1161/JAHA.121.022508
78. Garcia, L, Mendonça, G, Benedetti, TRB, Borges, LJ, Streit, IA, Christofoletti, M, et al. Barriers and facilitators of domain-specific physical activity: a systematic review of reviews. BMC Public Health. (2022) 22:1964. doi: 10.1186/s12889-022-14385-1
79. Stanhope, KL. Sugar consumption, metabolic disease and obesity: the state of the controversy. Crit Rev Clin Lab Sci. (2016) 53:52–67. doi: 10.3109/10408363.2015.1084990
80. Danaei, G, Ding, EL, Mozaffarian, D, Taylor, B, Rehm, J, Murray, CJL, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. (2009) 6:e1000058. doi: 10.1371/journal.pmed.1000058
81. Raji, A, Seely, EW, Arky, RA, and Simonson, DC. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab. (2001) 86:5366–71. doi: 10.1210/jcem.86.11.7992
82. Banerji, MA, Faridi, N, Atluri, R, Chaiken, RL, and Lebovitz, HE. Body composition, visceral fat, leptin, and insulin resistance in Asian Indian men. J Clin Endocrinol Metab. (1999) 84:137–4. doi: 10.1210/jc.84.1.137
83. Chew, NWS, Kong, G, Venisha, S, Chin, YH, Ng, CH, Muthiah, M, et al. Long-term prognosis of acute myocardial infarction associated with metabolic health and obesity status. Endocr Pract. (2022) 28:802–17. doi: 10.1016/j.eprac.2022.05.007
Keywords: knowledge, awareness, perception, actions, cardiometabolic disease, risk factors
Citation: Anand VV, Goh RSJ, Nah B, Koh SWC, Lim J, Neo NWS, Chew J, Lee YY, Chin YH, Chong B, Kong G, Tan B, Low Z, Khoo CM, Goh LH, Loh PH, Chai P, Dalakoti M, Chan M, Foo R, Muthiah M and Chew NWS (2023) General Public’s knowledge, awareness, and perception of Cardiometabolic diseases: data from a Singapore study population. Front. Med. 10:1193829. doi: 10.3389/fmed.2023.1193829
Edited by:
Redhwan Ahmed Al-Naggar, National University of Malaysia, MalaysiaReviewed by:
Feisul Mustapha, Ministry of Health Malaysia, MalaysiaHuan-Keat Chan, Ministry of Health (Malaysia), Malaysia
Copyright © 2023 Anand, Goh, Nah, Koh, Lim, Neo, Chew, Lee, Chin, Chong, Kong, Tan, Low, Khoo, Goh, Loh, Chai, Dalakoti, Chan, Foo, Muthiah and Chew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicholas W. S. Chew, nicholas_ws_chew@nuhs.edu.sg
†These authors have contributed equally to this work and share first authorship
‡ORCID: Nicholas W. S. Chew https://orcid.org/0000-0002-0640-0430
 Vickram Vijay Anand
Vickram Vijay Anand Rachel Sze Jen Goh2†
Rachel Sze Jen Goh2†  Jocelyn Chew
Jocelyn Chew Yip Han Chin
Yip Han Chin Bryan Chong
Bryan Chong Gwyneth Kong
Gwyneth Kong Mayank Dalakoti
Mayank Dalakoti Roger Foo2,10
Roger Foo2,10  Mark Muthiah
Mark Muthiah Nicholas W. S. Chew
Nicholas W. S. Chew