Extracorporeal cardiopulmonary resuscitation in adults and children: A review of literature, published guidelines and pediatric single-center program building experience
- 1Pediatric Critical Care Medicine, Children's National Hospital, Washington, DC, United States
- 2Department of Pediatrics, Baylor College of Medicine, Houston, TX, United States
- 3Pediatric Critical Care Medicine, Texas Children's Hospital, Houston, TX, United States
- 4ECMO, Texas Children's Hospital, Houston, TX, United States
- 5Department of Surgery, Baylor College of Medicine, Houston, TX, United States
- 6Congenital Heart Surgery, Texas Children's Hospital, Houston, TX, United States
Extracorporeal cardiopulmonary resuscitation (ECPR) is an adjunct supportive therapy to conventional cardiopulmonary resuscitation (CCPR) employing veno-arterial extracorporeal membrane oxygenation (VA-ECMO) in the setting of refractory cardiac arrest. Its use has seen a significant increase in the past decade, providing hope for good functional recovery to patients with cardiac arrest refractory to conventional resuscitation maneuvers. This review paper aims to summarize key findings from the ECPR literature available to date as well as the recommendations for ECPR set forth by leading national and international resuscitation societies. Additionally, we describe the successful pediatric ECPR program at Texas Children's Hospital, highlighting the logistical, technical and educational features of the program.
Introduction
Extracorporeal cardiopulmonary resuscitation (ECPR) as an adjunct to conventional cardiopulmonary resuscitation (CCPR) employs veno-arterial extracorporeal membrane oxygenation (ECMO) in the setting of refractory cardiac arrest. CCPR provides 25–30% of normal cardiac output, while extracorporeal perfusion techniques provide optimized circulatory support and end organ perfusion (1–3). The utilization of ECPR has grown dramatically over the last two decades in both adult and pediatric populations (4–9). The Extracorporeal Life Support Organization (ELSO) is an international non-profit consortium of health care institutions, researchers, and industry partners that maintains a data registry of ECMO patients from more than 450 centers. More than 154,000 patients have been reported to ELSO, with ECPR cases representing 12% of ECMO cases. Of the 18,000 ECPR cases, 12% are neonatal, 31% pediatric, and 57% adult, representing 5, 18, and 13% of all neonatal, pediatric, and adult ECMO cases respectively (4). The uptake and expansion of ECPR has been exponential, with fewer than 100 adult cases reported to ELSO per year before 2009 and more than 1,500 cases per year after 2018 (4).
ECPR is a resource-intensive resuscitation modality with logistical and technical challenges, availability limitations and an unclear economic impact. However, there is growing evidence suggesting potential benefit on patient outcomes. This review paper aims to summarize key findings from the ECPR literature available to date as well as the recommendations for ECPR set forth by national and international leading resuscitation societies. Additionally, we describe the successful pediatric ECPR program at Texas Children's Hospital, highlighting the logistical, technical and educational features of the program.
Adult ECPR
Epidemiology
In the United States, the annual incidence of adult in-hospital cardiac arrests (IHCA) is an estimated 292,000 per year with 12–26% survival (10–15). Additionally, there are nearly 350,000 adult out-of-hospital cardiac arrests (OHCA) per year, accounting for one in five deaths in the United States (15–17). OHCA survival ranges from 8 to 15% and is influenced by a multitude of pre-hospital factors including arrest location, bystander presence, cardiopulmonary resuscitation (CPR) quality, etiology of cardiac arrest, initial cardiac rhythm, emergency medical services response time, time to defibrillation, time to return of spontaneous circulation (ROSC), as well as post-resuscitation care (11, 15, 17–25).
Despite advancements in resuscitation science, outcomes for adult IHCA and OHCA remain poor. Attempts to improve these outcomes, coupled with broadened availability and increased uptake of ECMO technology have resulted in the development of ECPR for refractory cardiac arrest. The use of ECPR is growing, with a tenfold increase from 2003 to 2014 and more than 10,000 adult ECPR cases reported to ELSO with a contemporary survival rate of 30% (4, 26).
Adult extracorporeal cardiopulmonary resuscitation
Naturally, the ECPR literature has investigated superiority over CCPR, including several meta-analyses as well as smaller, retrospective and prospective observational studies. Overall, these data support the use of ECPR, with largely positive reported effects on survival and neurologic outcome (27–35). For example, the meta-analysis by Ouweneel et al. (29) analyzed over 3,000 IHCA and OHCA patients receiving ECPR and CCPR and found an increase in 30-day survival and favorable neurologic outcome with ECPR, findings which were upheld on propensity analysis of over 400 patients, adjusting for likelihood of receiving ECPR. However, there are inherent challenges in comparing these modalities in a non-controlled manner with high risk of bias due to fundamental group differences in type of arrest and patient comorbidities, as well as potential for heterogeneity across studies. Study heterogeneity was cited as the primary reason precluding meta-analysis in the work performed by Holmberg et al. (36) for the International Liaison Committee on Resuscitation (ILCOR) 2019 consensus statement.
Despite its growing use, ECPR is employed in <1% of adult IHCA, with use influenced by patient age, comorbidities, cardiac diagnoses and time and location of arrest (37). ECPR for adult IHCA is investigated by multiple studies (6, 27, 30, 38–68). Meta-analyses reveal promising pooled survival rates ranging from 30 to 38%, with 84% of survivors achieving favorable neurologic outcome (7, 69). However, meta-analyses comparing ECPR to CCPR in IHCA alone demonstrate mixed results, with improved ECPR outcomes noted by Chen et al. (30) but no significant difference reported by Wang et al. (27).
As a result of evolving technology and deployment efficiency, ECPR is utilized more frequently in OHCA settings as well (31, 35, 48, 66, 67, 70–99). A recent, large retrospective study by Bougouin et al. (84) analyzed 13,000 cases of OHCA from 2011 to 2018 in the Paris region, with 4% of patients receiving ECPR, and demonstrated no survival benefit for ECPR (8%) compared to CCPR (9%). However, several single center prospective and retrospective studies demonstrated improved survival with ECPR up to 43% (48, 72, 82, 83, 88, 96, 97). Similarly, a recent meta-analysis by Downing et al. of 44 studies inclusive of 3,097 patients identified an ECPR survival rate of 24%, with 18% of all patients having a good neurological outcome, consistent with previous meta-analyses (31, 35).
Currently there are only two published randomized controlled trials directly comparing ECPR and CCPR for OHCA, the “Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST)” trial and “Effect of Intra-arrest Transport, Extracorporeal Cardiopulmonary Resuscitation, and Immediate Invasive Assessment and Treatment on Functional Neurologic Outcome in Refractory Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial” (8, 9). As for the ARREST trial, the authors report 43% survival to hospital discharge in patients treated with ECPR compared to 7% with CCPR. After enrollment of only 30 patients, the study was terminated at the first interim analysis given that the posterior probability of ECMO superiority exceeded the prespecified monitoring boundary. Of note, all patients in the ARREST trial had an initial shockable rhythm and benefited from a streamlined process for ECPR initiation (8). The other randomized trial by Belohlavek et al. evaluated 256 OHCA patients, including all presenting rhythms (ventricular fibrillation, asystole and pulseless electrical activity), and reported 32% survival with good neurological outcome at 180 days in the ECPR group compared to 22% in the CCPR group (p = 0.09) (9). Of note, the trial was stopped prematurely when prespecified criteria for futility were met, however, the authors note that the trial was possibly underpowered to detect a clinically relevant difference (9).
Available data suggest that ECPR survival and neurologic outcome are impacted by various clinical and patient specifics. Favorable predictors include age (43, 68, 99), IHCA (48, 51, 67, 100, 101), shockable rhythm (28, 55, 68, 78, 84, 97–99, 102, 103), temporary ROSC (68, 84, 104), witnessed arrest with bystander CPR (104), shorter CCPR duration or time from arrest to ECMO (28, 43, 51, 64, 67, 68, 83, 86, 87, 94, 96, 102–104), higher baseline pH (93, 98, 99, 102, 103), lower baseline lactate (51, 86, 98, 102, 103) and percutaneous coronary intervention (43, 48, 91, 102). Pre-hospital cannulation for OHCA ECPR may have additional benefits on survival and neurologic outcome by reducing low-flow time for patients with longer anticipated transport times (83, 84, 91, 95, 105).
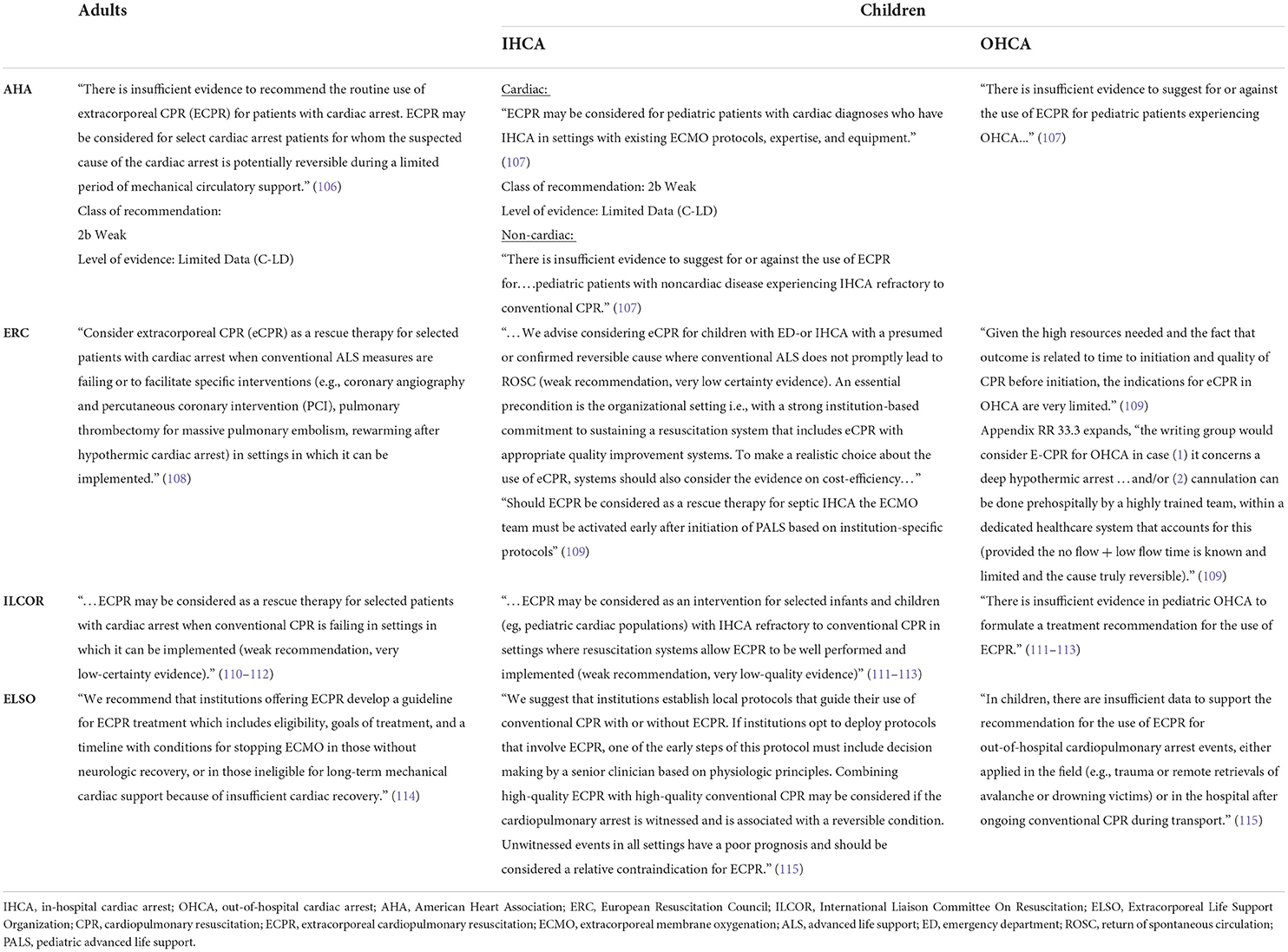
In light of the available literature, leading national and international resuscitation societies have set forth guidelines on the use of ECPR in adults. Table 1 summarizes the recommendations from the American Heart Association (AHA), European Resuscitation Council (ERC), ILCOR (106, 108, 110), and ELSO (114, 115). Of note, ILCOR commissioned a systematic review of ECPR in 2018 which informed the published 2019 Consensus on Science with Treatment Recommendations (CoSTR) (36, 111, 112).
ECPR candidacy
ECPR patient selection is a crucial determination as it relates to ECPR program building as well as research trial design. Data that definitively identify the patients most likely to benefit from ECPR are still needed, and thus candidacy determinations will be ECPR center or trial dependent. In general, ECPR is thought to provide a bridge to process reversal (e.g., myocardial infarction requiring percutaneous coronary intervention), other definitive management (e.g., ventricular assist device or organ transplantation), or further information seeking (106, 108, 114). Informed, patient-tailored institutional decisions about ECPR candidacy should occur as early as possible (114). The 2021 ELSO Interim Guideline Consensus Statement on ECPR in adults proposes the following inclusion criteria: age <70 years, witnessed arrest, arrest to CPR time <5 min, initial rhythm ventricular fibrillation, ventricular tachycardia, or pulseless electrical activity, arrest to ECMO time <60 min, end tidal carbon dioxide >10 mmHg during CCPR prior to cannulation, intermittent ROSC or recurrent ventricular fibrillation, “signs of life” during CCPR, absence of greater than mild aortic valve incompetence, and absence of significant end-stage organ failures or comorbidities (114). However, the majority of contemporary ECPR programs do not have formalized inclusion and exclusion criteria (116).
Post-ECPR care
Mortality after ROSC can be at least partially attributed to the complex pathophysiologic state following cardiac arrest involving the initial ischemic insult as well as reperfusion and post-reperfusion injuries and their effect on organ systems, referred to as “post-cardiac arrest syndrome” (117). Post-resuscitation care is a resource-intensive multidisciplinary undertaking that requires critical monitoring and tailored management strategies to prevent additional injury, as well as investigation of the precipitating cause and reversal or treatment if necessary.
Recommendations for post-resuscitation care are set forth by AHA, informed most recently by an ILCOR 2020 systematic review and CoSTR for advanced life support (106, 110). These recommendations highlight avoidance of hypotension using crystalloid, inotropes, or mechanical support as needed (goal systolic blood pressure ≥90 mmHg; mean arterial blood pressure ≥65 mmHg), avoidance of hypoxemia and hyperoxemia (target oxygen saturation of 92–98%), and maintenance of normocapnia (arterial partial pressure of carbon dioxide 35–45 mmHg) (106, 110). Other components of care include maintenance of euglycemia and timely diagnosis and treatment of seizures. Prophylactic use of anti-seizure medications, antibiotics and steroids are not advised (106, 110). Lastly, while hyperthermia prevention and management are universally accepted, targeted temperature management (TTM) is an area of ongoing research and relative controversy. TTM was recommended between 32 and 36°C for at least 24 h for comatose adults following ROSC after IHCA or OHCA with any initial rhythm, based on landmark studies by Bernard et al. and Hypothermia after Cardiac Arrest Study Group (118, 119). However, a recent large, open-label trial comparing targeted hypothermia and normothermia found no difference in 6-month survival or functional outcome following OHCA (120). In light of this and other evidence, the ERC revised their guidelines on temperature control, advising continuous temperature monitoring and preventing fever (>37.7°C) for 72 h, but there was insufficient evidence to recommend for or against temperature control at 32–36°C (121).
While additional data is needed to inform best practices for post-ECPR care, providers should consider general post-resuscitation care recommendations as well as the ELSO Interim Guideline Consensus Statement on ECPR in adults (114). After ECMO blood flow of 3–4 L/min is achieved, providers should target mean arterial blood pressure ≥60 and <80 mmHg (114). Unintended hyperoxia and hypocapnia should be avoided, as they have been associated with worse outcomes for patients receiving ECPR (122, 123). Prompt and frequent measurements of oxygenation and ventilation are needed, with adjustments to ECMO oxygen gas and sweep flow to target arterial oxygen saturation of 92–97% and normocarbia (114). With respect to temperature control, the circuit warmer can be programmed as desired, and early intervention for hyperthermia is similarly feasible using the circuit warmer and heat exchanger. Lastly, patients exhibiting signs of left ventricular hypertension and pulmonary edema should be considered for left ventricular unloading and/or venting (114).
Pediatric ECPR
Epidemiology
There are over 15,000 pediatric in-hospital cardiac arrests requiring CPR per year in the United States, with several studies documenting an increase in survival over time (10, 11, 124, 125). Pediatric IHCA occurs in 2–6% of intensive care admissions, and the majority of arrests occur in intensively monitored patients (90%) with a secured airway (80%) (11, 126–128). Survival rates for pediatric IHCA are 40–49% with 34–90% of survivors achieving favorable neurological outcome depending on the study (11, 15, 128, 129). Additionally, over 5,000 children experience non-traumatic OHCA annually (130). In contrast to adult OHCA, pediatric OHCA is more commonly attributed to non-cardiac etiologies (131). Survival rates are ~11–13%, with favorable neurological outcomes occurring in 85–90% of survivors (11, 15).
Pediatric extracorporeal cardiopulmonary resuscitation
Pediatric ECPR, like adult ECPR, aims to optimize cardiac output and end organ perfusion with the goal of improving arrest survivability and neurological outcomes. The most recent ELSO Registry International Summary Report, comprising data from inception through 2020, identifies 5,682 pediatric ECPR cases (4). ECPR cases account for 18% of all pediatric ECMO cases, which has markedly increased from 5% in 2004 (4, 132). The survival rate to discharge for pediatric ECPR is 42% per the ELSO Registry, with over 70% of cases performed for an indication of cardiac disease (4, 133). Similarly, a recent systemic review and meta-analysis of 28 studies and 1,300 pediatric ECPR patients (excluding registry patients) demonstrated 30% survival with favorable neurological outcome (134). A secondary analysis of the IHCA “Therapeutic Hypothermia After Pediatric Cardiac Arrest” (THAPCA) trial demonstrated that ECPR survivors had similar long term neurobehavioral outcomes to other post-arrest survivors, with one third of ECPR patients alive with good functional status at 1 year (135, 136). Despite the steady growth of ECPR utilization over time in pediatric patients, the pediatric ECPR literature lacks randomized studies and the majority of data is focused on IHCA in cardiac patients (4, 5, 134, 137–149).
In a landmark paper, Lasa et al. performed a large systematic comparison of ECPR and CCPR for pediatric patients with IHCA requiring >10 min resuscitation using the Get With the Guidelines-Resuscitation Registry (GWTG-R), a large multicenter national registry. Their analysis demonstrated improved survival and survival with favorable neurological outcome for the ECPR group compared to the CCPR group even after adjusting for illness type, pre-existing conditions, and arrest features. Their findings were further confirmed on propensity score-matched analysis (150).
Analyses of the GWTG-R and the National Registry of Cardiopulmonary Resuscitation demonstrated use of ECPR in 3–7% of IHCA, with the most frequent utilization for cardiac surgical patients (150–153). In fact, ECPR was used in 27% of arrests between 2014 and 2016 according to the Pediatric Cardiac Critical Care Consortium registry (154). Use of ECPR for refractory IHCA has increased threefold in the last two decades according to the National Inpatient Sample dataset (128). Overall, registry analyses show ECPR survival is 27–44% for IHCA with neurologically favorable outcomes in 56–73% of survivors (150–152, 155). Several studies demonstrated improved ECPR survival (32–48%) for patients with cardiac disease compared to non-cardiac patients (151, 152, 156–159). A meta-analysis including 762 patients by Joffe et al. (155) described overall ECPR survival of 49%, with favorable neurological outcomes occurring in 79% of survivors and non-cardiac disease associated with increased risk of mortality. Other retrospective single, multicenter, and database studies describe 25–73% overall survival and 50–100% of survivors having good neurologic outcome (137, 145, 147, 149, 156, 159–176).
The literature is scarce regarding the use of ECPR for pediatric OHCA, which comprises only 3% of ECPR cases reported to ELSO (138). From 2010 to 2019, 33 patients (7 survivors) reported to ELSO experienced arrest during emergency medical services transport and received ECPR by the receiving institution (Bilodeau and McMullan, personal communication). ECPR in pediatric patients reported to ELSO Registry (Unpublished raw data). Additionally, ECPR for pediatric OHCA is described by infrequent single center reports (177, 178). Likewise, there is only one case report of out-of-hospital cannulation in a pediatric patient (179).
Aside from preexisting non-cardiac disease, patient factors associated with ECPR outcomes include pre-ECPR pH, lactate and renal injury as well as post-ECPR lactate and pH (133, 135, 146, 147, 149–151, 157–160, 163, 164, 168, 171–173, 175, 180, 181). In a secondary analysis of ECPR within the IHCA THAPCA trial, receipt of open-chest cardiac massage was associated with shorter CPR duration, survival and good neurological outcome at 1 year, while open-chest cardiac massage is a negative predictor in other studies (135, 164). Increasing CPR interruptions during cannulation have been associated with worse outcomes (145). Additionally, several studies have described an association between CPR duration and survival (145, 147–149, 158, 160, 162, 164, 165, 168, 172, 174, 175). Meanwhile, other studies have not upheld this finding, and moreover, some authors have recognized the ability of ECPR to rescue patients with very prolonged arrest times such as 60–95 min (146, 156, 158, 166, 169–171, 180). Arrest rhythm has also been inconsistently associated with outcomes (124, 135, 149, 158, 182). Complications while on ECMO portend a worse prognosis (133, 157–159, 168, 171, 173).
In light of the available literature, leading national and international resuscitation societies have set forth guidelines on the use of ECPR in children. Table 1 summarizes the recommendations from AHA, ERC, ILCOR and ELSO (107, 109, 113, 115).
ECPR candidacy
Data are currently insufficient to definitively identify appropriate pediatric ECPR candidates. A recent survey of pediatric critical care physicians demonstrated that ECPR activation decisions are complex and heterogeneous, but most consistently influenced by patient diagnosis (cardiac vs. non-cardiac), CPR duration, arrest location, witnessed arrest, and blood pH (183). ECPR consideration is currently advised by AHA for patients with cardiac diagnoses when CCPR is failing, but should be reserved to experienced institutions (107). There are insufficient data to advise uniform application in other pediatric subgroups (107).
Post-ECPR care
Following the application of ECPR, optimal post-resuscitation care for children is critical. Post-cardiac arrest syndrome in children mimics that in adults, involving brain injury, myocardial dysfunction, systemic ischemia and reperfusion injury, and unresolved inciting pathology (184). AHA recommendations for pediatric post-resuscitation care include optimizing hemodynamics (systolic blood pressure >5th percentile for age) utilizing crystalloid and/or vasopressor agents as needed, targeting normoxemia (oxygen saturations 94–99%) and limiting exposure to severe hypercapnia or hypocapnia. Oxygenation and ventilation targets may be modified in the context of a patient's underlying condition (107, 184). With respect to TTM following pediatric cardiac arrest, the AHA recommends continuous measurement of core temperature and targeting either normothermia (36–37.5°C) for 5 days or hypothermia (32–34°C) for 2 days followed by normothermia (36–37.5°C) for 3 days (107, 184, 185). Evaluated robustly by the multicenter randomized controlled THAPCA study, TTM at 32–34°C when compared to TTM at 36–37.5°C had no effect on survival or neurologic outcome (136, 186). Additionally, hyperthermia is common, and if persistent, is associated with worse neurological outcomes and should therefore be aggressively treated (107, 184, 187).
While there is no literature specific to post-ECPR care in children, management should at minimum uphold the recommendations for general post-resuscitation care. As is true for adults upon ECPR initiation, ECMO circuit flows in conjunction with fluids and vasopressors should be titrated to optimize hemodynamics. Extracorporeal support has the potential to mitigate post-arrest hypotension which is common, and associated with worse outcomes (188). In addition, institution of extracorporeal support should prompt attention to oxygenation (risk of hyperoxia), ventilation and ECMO sweep gas flow (risk for hypocapnia), and desired temperature management (programmed temperature control with circuit warmer and heat exchanger).
Neonatal ECPR
There are 2,261 cases of neonatal ECPR reported to the ELSO Registry with an overall survival to discharge of 42% (4). Approximately half of ELSO neonatal ECMO centers report performing neonatal ECPR (189). Neonatal cases are included within GWTG-R studies, representing 21% of pediatric ECPR cases with 38% survival and 46% of survivors having favorable neurological outcome (150). Post-cardiotomy ECPR cases for neonates with congenital heart disease predominate (181, 190, 191). Additionally, neonates may require ECPR in the setting of respiratory disease, which carries a favorable prognosis (133). Other positive prognostic indicators identified by the literature include greater gestational age, weight, and cardiac arrhythmia causing arrest (190). Unfavorable factors include lower pre-ECPR arterial oxygenation, delayed lactate clearance, ECMO duration and complications (181, 190).
ECPR program building
ECPR is a complex multi-disciplinary resuscitation modality that involves substantial resources and strong institutional commitment. Successful ECPR programs require maintenance of expertise and equipment, as well as integrated quality improvement mechanisms to assess important program metrics (114).
A successful ECPR program has been established at Texas Children's Hospital since 2005. Figure 1 details an example ECPR deployment algorithm. ECPR candidacy is discussed preemptively in high-risk patients. All cardiac patients are ECPR candidates, except for those with significant comorbidities or vascular access limitations. Certain non-cardiac patients are considered on a case-by-case basis, including but not limited to patients with pulmonary hypertension, drug overdose, and pulmonary embolism. Candidate patients experiencing a witnessed arrest in pre-defined locations may receive ECPR, including the emergency department (ED), intensive care units (ICU), cardiac catheterization lab, or operating room (OR). Activation can be triggered by either cardiac intensive care physician or congenital heart surgeon, when high-quality CPR fails to achieve sustainable ROSC after two cycles. A staff member calls in to the operator requesting ECPR activation and system page out, which notifies congenital heart surgeon, operating room staff, cardiovascular anesthesia, perfusionists, and pharmacy as to the patient location and weight. The congenital heart surgery attending and fellow are available on-call 24/7. During regular business hours, the team is in-house, however, after-hours, it is expected that they are within a 20-min distance from the hospital should ECPR activation be needed. The assisting operating room team, bedside team, and ECMO technical team are in-house 24/7 and would start preparing before the arrival of the surgical team. Each team member adheres to their protocol that includes equipment gathering. Bundled surgical cannulation carts and crystalloid-primed ECMO circuits are pre-prepared and maintained in key locations dedicated to rapid deployment. ECPR cannulation takes place in specific hospital locations including the OR, cardiac catheterization lab, or ICU. Thus, candidate patients experiencing arrest in the ED will be transported. The optimal ECPR cannulation strategy is dependent upon patient anatomy, size, operative status, and pathophysiology. For example, a post-sternotomy patient with open chest may be cannulated centrally given ease of access, while closed-chest, pre-operative, medical cardiac, or non-cardiac patients are more appropriate for initial peripheral cannulation.
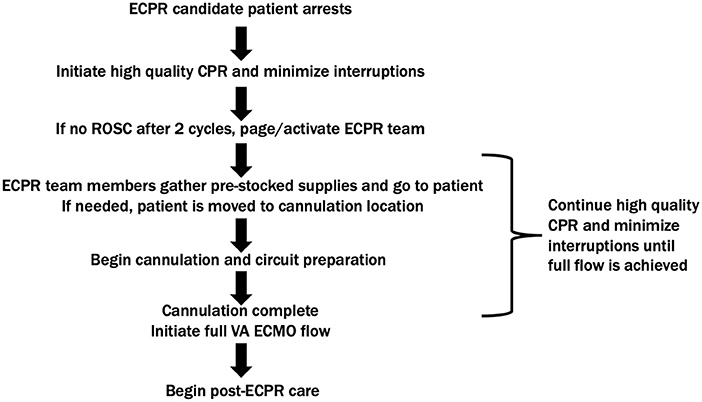
Figure 1. ECPR deployment algorithm. ECPR, extracorporeal cardiopulmonary resuscitation; CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation; VA ECMO, veno-arterial extracorporeal membrane oxygenation.
Laussen and Guerguerian (192) review the critical components for establishing and sustaining an ECPR program. They describe four time intervals of importance: cardiac arrest to CCPR (interval 1), start of CCPR to ECPR activation (interval 2), ECPR activation to ECMO flow (interval 3), and ECMO flow to post-resuscitation care (interval 4). Interval 1 should not exceed 1 min in the event of witnessed IHCA. Interval 2 can be minimized by early ECPR activation by designated team members. Interval 3 may be reduced when ECPR occurs in familiar, well-controlled, protocol-driven environments. Many centers utilize preassigned roles, flowcharts and job aides to enhance staff preparedness and decrease deployment time (177, 191, 193–195). Protocolized, rapid response ECMO programs have proven successful in reducing neurologic complications in both ECPR and general ECMO patients (196).
A key quality initiative for our ECPR program is our clinical event debriefings conducted after all ECPR cases. Started in 2014, these debriefs aim to improve team dynamics and patients' outcome. The structured approach investigates the teams' clinical performance, resources, facilities, including process or system problems to improve. Table top simulations and live simulation based system testings are frequently used to optimize any identified paucities.
Team training and simulation
Simulation has been widely regarded as beneficial for ECMO team training, technical skills, provider confidence, communication and collaboration, improving deployment times and adherence to ECPR protocols (174, 191, 194, 195, 197–205). Moreover, simulation can be used to develop, test, and/or adapt an ECPR protocol (195, 198, 206).
At Texas Children's Hospital, ECMO team members participate in a structured education and simulation program with competency benchmarks covering all aspects of ECMO delivery (Figure 2). A series of didactic sessions reviews basic fundamentals, including respiratory and cardiac pathophysiology potentially necessitating ECMO support. Didactics further explore ECMO candidacy, cannulation strategies and complications. Subsequently, providers engage in progressively complex wet lab trainings. Wet lab trainings reinforce important processes: setting up a dry circuit (<15 min), priming with crystalloid (<8 min), priming with blood (<5 min), and pump, oxygenator, and circuit exchanges. Wet lab exercises are repeated and timed until proficiency is demonstrated. Next, trainees transition to actively assisting other trained ECMO providers and are evaluated in that capacity. Direct feedback and debriefing sessions provide continuing education.
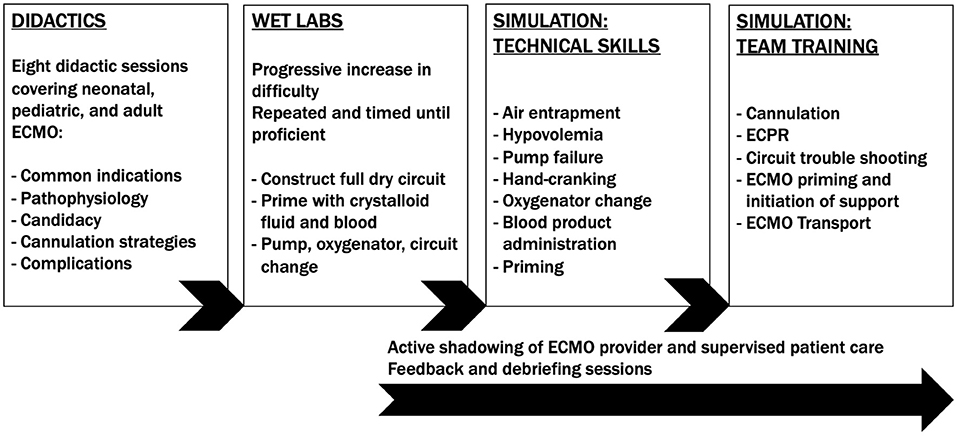
Figure 2. Texas children's hospital ECMO training program. ECMO, extracorporeal membrane oxygenation; ECPR, extracorporeal cardiopulmonary resuscitation.
Multi-disciplinary ECPR simulation sessions are held regularly at Texas Children's Hospital to enhance interprofessional team performance, communication, and technical skills. Scenarios reinforce key components of patient encounters, from deterioration and arrest through ECPR activation, patient transport, cannulation, and circuit management. Additionally, we utilize a surgical simulation model for ECMO cannulation (Image 1; RediStik™ ECMO Cannulation Trainer, Sawbones, Vashon, WA, USA). The model aims to improve procedural skills with ECMO neck cannulation, highly pertinent to ECPR deployment in pediatric patients. Alternate models have been employed by other ECPR simulation programs (199, 207).
Conclusion
ECPR has the potential to rescue selected patients when conventional resuscitation efforts are failing. There is growing evidence that ECPR improves survival and neurological outcomes in adult OHCA and IHCA. Further well-designed, randomized clinical trials are needed to identify the most appropriate ECPR candidates, as well as optimal pre-ECPR and post-ECPR practices. Additional research is needed to explore the utility of ECPR in pediatric and neonatal populations, with a focus on understanding the role in non-cardiac illness and OHCA. Effective application of ECPR requires substantial health care resources and strong institutional commitment. Institutions should develop a systematic approach, utilizing team training, simulations, and quality improvement mechanisms in order to establish a successful ECPR program.
Author contributions
PB, MA, and TO contributed to conception, design of the study, wrote the first draft of the manuscript, and edited the final draft to the manuscript submitted. PB, TO, MA, AS, and CB wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was funded by Michael Pickett MSN, APRN, PNP-BC and Texas Children's Hospital Heart Center Innovation Award 2020, $5k.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.935424/full#supplementary-material
Supplementary Image 1. RediStik™ ECMO Cannulation Trainer. ECMO: extracorporeal membrane oxygenation (https://www.youtube.com/watch?v=UwCJNP94g30&list=PLvWZmgauEkKKcGfI99fYOV9viFyTu03f1&index=2).
References
1. Lurie KG, Nemergut EC, Yannopoulos D, Sweeney M. The physiology of cardiopulmonary resuscitation. Anesth Analg. (2016) 122:767–83. doi: 10.1213/ANE.0000000000000926
2. Barsan WG, Levy RC. Experimental design for study of cardiopulmonary resuscitation in dogs. Ann Emerg Med. (1981) 10:135–7.
3. Kennedy JH. The role of assisted circulation in cardiac resuscitation. JAMA J Am Med Assoc. (1966) 197:615–8.
4. Extracorporeal Life Support Organization. ELSO Registry Report International Summary. (2021), 1–40. Available online at: https://www.elso.org/Portals/0/Files/Reports/2021_April/International%20Report%20April_page1.pdf (accessed April 3, 2022).
5. Nido PJ, Dalton HJ, Thompson AE, Siewers RD. Extracorporeal membrane oxygenator rescue in children during cardiac arrest after cardiac surgery. Circulation. (1992) 86:II300–4.
6. Chen YS, Lin JW Yu HY, Ko WJ, Jerng JS, Chang WT, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support vs. conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. (2008) 372:554–61. doi: 10.1016/S0140-6736(08)60958-7
7. Gravesteijn BY, Schluep M, Disli M, Garkhail P, dos Reis Miranda D, Stolker RJ, et al. Neurological outcome after extracorporeal cardiopulmonary resuscitation for in-hospital cardiac arrest: a systematic review and meta-analysis. Critical Care. (2020) 24:1–12. doi: 10.1186/s13054-020-03201-0
8. Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. (2020) 396:1807–16. doi: 10.1016/S0140-6736(20)32338-2
9. Belohlavek J, Smalcova J, Rob D, Franek O, Smid O, Pokorna M, et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. (2022) 327:737–47. doi: 10.1001/jama.2022.6548
10. Holmberg MJ, Ross CE, Fitzmaurice GM, Chan PS, Duval-Arnould J, Grossestreuer AV, et al. Annual incidence of adult and pediatric in-hospital cardiac arrest in the United States. Circ Cardiovasc Qual Outcomes. (2019) 12:e005580. doi: 10.1161/CIRCOUTCOMES.119.005580
11. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics-−2022 update: a report from the American heart association. Circulation. (2022) 145:e153–639. doi: 10.1161/CIR.0000000000001052
12. Ofoma UR, Basnet S, Berger A, Kirchner HL, Girotra S, Abella B, et al. Trends in survival after in-hospital cardiac arrest during nights and weekends. J Am Coll Cardiol. (2018) 71:402–11. doi: 10.1016/j.jacc.2017.11.043
13. Chan PS, Spertus JA, Kennedy K, Nallamothu BK, Starks MA, Girotra S. In-hospital cardiac arrest survival in the United States during and after the initial novel coronavirus disease 2019 pandemic surge. Circ Cardiovasc Qual Outcomes. (2022) 15:e008420. doi: 10.1161/CIRCOUTCOMES.121.008420
14. Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14 720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. (2003) 58:297–308. doi: 10.1016/S0300-9572(03)00215-6
15. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American heart association. Circulation. (2019) 139:e56–e528. doi: 10.1161/CIR.0000000000000659
16. Milan M, Perman SM. Out of hospital cardiac arrest: a current review of the literature that informed the 2015 American heart association guidelines update. Curr Emerg Hosp Med Rep. (2016) 4:164–71. doi: 10.1007/s40138-016-0118-x
17. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-−2015 update: a report from the American heart association. Circulation. (2015) 131:e29–e322. doi: 10.1161/CIR.0000000000000152
18. Girotra S, van Diepen S, Nallamothu BK, Carrel M, Vellano K, Anderson ML, et al. Regional variation in out-of-hospital cardiac arrest survival in the United States. Circulation. (2016) 133:2159–68. doi: 10.1161/CIRCULATIONAHA.115.018175
19. Bray J, Howell S, Ball S, Doan T, Bosley E, Smith K, et al. The epidemiology of out-of-hospital cardiac arrest in Australia and New Zealand: a binational report from the Australasian resuscitation outcomes consortium (Aus-ROC). Resuscitation. (2022) 172:74–83. doi: 10.1016/j.resuscitation.2022.01.011
20. Stiell IG, Nichol G, Wells G, de Maio V, Nesbitt L, Blackburn J, et al. Health-related quality of life is better for cardiac arrest survivors who received citizen cardiopulmonary resuscitation. Circulation. (2003) 108:1939–44. doi: 10.1161/01.CIR.0000095028.95929.B0
21. Kilgannon JH, Kirchhoff M, Pierce L, Aunchman N, Trzeciak S, Roberts BW. Association between chest compression rates and clinical outcomes following in-hospital cardiac arrest at an academic tertiary hospital. Resuscitation. (2017) 110:154–61. doi: 10.1016/j.resuscitation.2016.09.015
22. Balian S, Buckler DG, Blewer AL, Bhardwaj A, Abella BS. Variability in survival and post-cardiac arrest care following successful resuscitation from out-of-hospital cardiac arrest. Resuscitation. (2019) 137:78–86. doi: 10.1016/j.resuscitation.2019.02.004
23. Centers for Disease Control and Prevention. Cardiac Arrest Registry to Enhance Survival (CARES) National Summary Report (2013).
24. Daya MR, Schmicker RH, Zive DM, Rea TD, Nichol G, Buick JE, et al. Out-of-hospital cardiac arrest survival improving over time: results from the resuscitation outcomes consortium (ROC). Resuscitation. (2015) 91:108–15. doi: 10.1016/j.resuscitation.2015.02.003
25. Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. (2020) 24:1–13. doi: 10.1186/s13054-020-2773-2
26. Richardson ASC, Schmidt M, Bailey M, Pellegrino VA, Rycus PT, Pilcher DV, et al. cardio-pulmonary resuscitation (ECPR), trends in survival from an international multicentre cohort study over 12-years. Resuscitation. (2017) 112:34–40. doi: 10.1016/j.resuscitation.2016.12.009
27. Wang G, Chen X, Qiao L, Mei Y, Lv J, Huang X, et al. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: a meta-analysis of 2 260 patients with cardiac arrest. World J Emerg Med. (2017) 8:5. doi: 10.5847/wjem.j.1920-8642.2017.01.001
28. Twohig CJ, Singer B, Grier G, Finney SJ, A. systematic literature review and meta-analysis of the effectiveness of extracorporeal-CPR vs. conventional-CPR for adult patients in cardiac arrest. J Intensivs Care Soc. (2019) 20:347–57. doi: 10.1177/1751143719832162
29. Ouweneel DM, Schotborgh JV, Limpens J, Sjauw KD, Engström AE, Lagrand WK, et al. Extracorporeal life support during cardiac arrest and cardiogenic shock: a systematic review and meta-analysis. Intensive Care Med. (2016) 42:1922–34. doi: 10.1007/s00134-016-4536-8
30. Chen Z, Liu C, Huang J, Zeng P, Lin J, Zhu R, et al. Clinical efficacy of extracorporeal cardiopulmonary resuscitation for adults with cardiac arrest: meta-analysis with trial sequential analysis. BioMed Res Int. (2019) 2019:6414673. doi: 10.1155/2019/6414673
31. Ortega-Deballon I, Hornby L, Shemie SD, Bhanji F, Guadagno E. Extracorporeal resuscitation for refractory out-of-hospital cardiac arrest in adults: a systematic review of international practices and outcomes. Resuscitation. (2016) 101:12–20. doi: 10.1016/j.resuscitation.2016.01.018
32. Beyea MM, Tillmann BW, Iansavichene AE, Randhawa VK, van Aarsen K, Nagpal AD. Neurologic outcomes after extracorporeal membrane oxygenation assisted CPR for resuscitation of out-of-hospital cardiac arrest patients: a systematic review. Resuscitation. (2018) 130:146–58. doi: 10.1016/j.resuscitation.2018.07.012
33. Karve S, Lahood D, Diehl A, Burrell A, Tian DH, Southwood T, et al. The impact of selection criteria and study design on reported survival outcomes in extracorporeal oxygenation cardiopulmonary resuscitation (ECPR): a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med. (2021) 29:1–9. doi: 10.1186/s13049-021-00956-5
34. Miraglia D, Miguel LA, Alonso W. Extracorporeal cardiopulmonary resuscitation for in- and out-of-hospital cardiac arrest: systematic review and meta-analysis of propensity score-matched cohort studies. J Am Coll Emerg Phys Open. (2020) 1:342–61. doi: 10.1002/emp2.12091
35. Downing J, Al Falasi R, Cardona S, Fairchild M, Lowie B, Chan C, et al. How effective is extracorporeal cardiopulmonary resuscitation (ECPR) for out-of-hospital cardiac arrest? A systematic review and meta-analysis. Am J Emerg Med. (2022) 51:127–38. doi: 10.1016/j.ajem.2021.08.072
36. Holmberg MJ, Geri G, Wiberg S, Guerguerian AM, Donnino MW, Nolan JP, et al. Extracorporeal cardiopulmonary resuscitation for cardiac arrest: a systematic review HHS public access. Resuscitation. (2018) 131:91–100. doi: 10.1016/j.resuscitation.2018.07.029
37. Tonna JE, Selzman CH, Girotra S, Presson AP, Thiagarajan RR, Becker LB, et al. Patient and institutional characteristics influence the decision to use extracorporeal cardiopulmonary resuscitation for in-hospital cardiac arrest. J Am Heart Assoc. (2020) 9:e015522. doi: 10.1161/JAHA.119.015522
38. Blumenstein J, Leick J, Liebetrau C, Kempfert J, Gaede L, Groß S, et al. Extracorporeal life support in cardiovascular patients with observed refractory in-hospital cardiac arrest is associated with favourable short and long-term outcomes: a propensity-matched analysis. Eur Heart J Acute Cardiovasc Care. (2016) 5:13–22. doi: 10.1177/2048872615612454
39. Cho YH, Kim WS, Sung K, Jeong DS, Lee YT, Park PW, et al. Management of cardiac arrest caused by acute massive pulmonary thromboembolism: importance of percutaneous cardiopulmonary support. ASAIO J. (2014) 60:280–3. doi: 10.1097/MAT.0000000000000063
40. Chou TH, Fang CC, Yen ZS, Lee CC, Chen YS, Ko WJ, et al. An observational study of extracorporeal CPR for in-hospital cardiac arrest secondary to myocardial infarction. Emerg Med J. (2014) 31:441–7. doi: 10.1136/emermed-2012-202173
41. Lin JW, Wang MJ Yu HY, Wang CH, Chang WT, Jerng JS, et al. Comparing the survival between extracorporeal rescue and conventional resuscitation in adult in-hospital cardiac arrests: propensity analysis of 3-year data. Resuscitation. (2010) 81:796–803. doi: 10.1016/j.resuscitation.2010.03.002
42. Shin TG, Choi JH, Jo IJ, Sim MS, Song HG, Jeong YK, et al. Extracorporeal cardiopulmonary resuscitation in patients with in-hospital cardiac arrest: a comparison with conventional cardiopulmonary resuscitation. Crit Care Med. (2011) 39:1–7. doi: 10.1097/CCM.0b013e3181feb339
43. Shin TG, Jo IJ, Sim MS, Song YB, Yang JH, Hahn JY, et al. Two-year survival and neurological outcome of in-hospital cardiac arrest patients rescued by extracorporeal cardiopulmonary resuscitation. Int J Cardiol. (2013) 168:3424–30. doi: 10.1016/j.ijcard.2013.04.183
44. Chen YS Yu HY, Huang SC, Lin JW, Chi NH, Wang CH, et al. Extracorporeal membrane oxygenation support can extend the duration of cardiopulmonary resuscitation. Crit Care Med. (2008) 36:2529–35. doi: 10.1097/CCM.0b013e318183f491
45. Park SB, Yang JH, Park TK, Cho YH, Sung K, Chung CR, et al. Developing a risk prediction model for survival to discharge in cardiac arrest patients who undergo extracorporeal membrane oxygenation. Int J Cardiol. (2014) 177:1031–5. doi: 10.1016/j.ijcard.2014.09.124
46. Dennis M, McCanny P, D'Souza M, Forrest P, Burns B, Lowe DA, et al. Extracorporeal cardiopulmonary resuscitation for refractory cardiac arrest: a multicentre experience. Int J Cardiol. (2017) 231:131–6. doi: 10.1016/j.ijcard.2016.12.003
47. Kagawa E, Dote K, Kato M, Sasaki S, Nakano Y, Kajikawa M, et al. Should we emergently revascularize occluded coronaries for cardiac arrest? Rapid-response extracorporeal membrane oxygenation and intra-arrest percutaneous coronary intervention. Circulation. (2012) 126:1605–13. doi: 10.1161/CIRCULATIONAHA.111.067538
48. Stub D, Bernard S, Pellegrino V, Smith K, Walker T, Sheldrake J, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation. (2015) 86:88–94. doi: 10.1016/j.resuscitation.2014.09.010
49. Ryu JA, Cho YH, Sung K, Choi SH, Yang JH, Choi JH, et al. Predictors of neurological outcomes after successful extracorporeal cardiopulmonary resuscitation. BMC Anesthesiol. (2015) 15:1–8. doi: 10.1186/s12871-015-0002-3
50. Park BW, Seo DC, Moon IK, Chung JW, Bang DW, Hyon MS, et al. Pulse pressure as a prognostic marker in patients receiving extracorporeal life support. Resuscitation. (2013) 84:1404–8. doi: 10.1016/j.resuscitation.2013.04.009
51. Haneya A, Philipp A, Diez C, Schopka S, Bein T, Zimmermann M, et al. A 5-year experience with cardiopulmonary resuscitation using extracorporeal life support in non-postcardiotomy patients with cardiac arrest. Resuscitation. (2012) 83:1331–7. doi: 10.1016/j.resuscitation.2012.07.009
52. Han SJ, Kim HS, Choi HH, Hong GS, Lee WK, Lee SH, et al. Predictors of survival following extracorporeal cardiopulmonary resuscitation in patients with acute myocardial infarction-complicated refractory cardiac arrest in the emergency department: a retrospective study. J Cardiothorac Surg. (2015) 10:1–7. doi: 10.1186/s13019-015-0212-2
53. Jung C, Janssen K, Kaluza M, Fuernau G, Poerner TC, Fritzenwanger M, et al. Outcome predictors in cardiopulmonary resuscitation facilitated by extracorporeal membrane oxygenation. Clin Res Cardiol. (2016) 105:196–205. doi: 10.1007/s00392-015-0906-4
54. Lazzeri C, Sori A, Bernardo P, Picariello C, Gensini GF, Valente S. In-hospital refractory cardiac arrest treated with extracorporeal membrane oxygenation: a tertiary single center experience. Acute Card Care. (2013) 15:47–51. doi: 10.3109/17482941.2013.796385
55. Pozzi M, Armoiry X, Achana F, Koffel C, Pavlakovic I, Lavigne F, et al. Extracorporeal life support for refractory cardiac arrest: a 10-year comparative analysis. Ann Thorac Surg. (2019) 107:809–16. doi: 10.1016/j.athoracsur.2018.09.007
56. Peigh G, Cavarocchi N, Hirose H. Saving life and brain with extracorporeal cardiopulmonary resuscitation: a single-center analysis of in-hospital cardiac arrests. J Thorac Cardiovasc Surg. (2015) 150:1344–9. doi: 10.1016/j.jtcvs.2015.07.061
57. Liu Y, Cheng YT, Chang JC, Chao SF, Chang BS. Extracorporeal membrane oxygenation to support prolonged conventional cardiopulmonary resuscitation in adults with cardiac arrest from acute myocardial infarction at a very low-volume centre. Interact Cardiovasc Thorac Surg. (2011) 12:389–93. doi: 10.1510/icvts.2010.256388
58. Mazzeffi MA, Sanchez PG, Herr D, Krause E, Evans CF, Rector R, et al. Outcomes of extracorporeal cardiopulmonary resuscitation for refractory cardiac arrest in adult cardiac surgery patients. J Thorac Cardiovasc Surg. (2016) 152:1133–9. doi: 10.1016/j.jtcvs.2016.06.014
59. Lee DS, Chung CR, Jeon K, Park CM, Suh GY, Song Y, et al. Survival after extracorporeal cardiopulmonary resuscitation on weekends in comparison with weekdays. Ann Thorac Surg. (2016) 101:133–40. doi: 10.1016/j.athoracsur.2015.06.077
60. Ellouze O, Vuillet M, Perrot J, Grosjean S, Missaoui A, Aho S, et al. Comparable outcome of out-of-hospital cardiac arrest and in-hospital cardiac arrest treated with extracorporeal life support. Artif Org. (2018) 42:15–21. doi: 10.1111/aor.12992
61. Spangenberg T, Meincke F, Brooks S, Frerker C, Kreidel F, Thielsen T, et al. “Shock and Go?” extracorporeal cardio-pulmonary resuscitation in the golden-hour of ROSC. Catheter Cardiovasc Intervent. (2016) 88:691–6. doi: 10.1002/ccd.26616
62. Avalli L, Maggioni E, Formica F, Redaelli G, Migliari M, Scanziani M, et al. Favourable survival of in-hospital compared to out-of-hospital refractory cardiac arrest patients treated with extracorporeal membrane oxygenation: an Italian tertiary care centre experience. Resuscitation. (2012) 83:579–83. doi: 10.1016/j.resuscitation.2011.10.013
63. Bednarczyk JM, White CW, Ducas RA, Golian M, Nepomuceno R, Hiebert B, et al. Resuscitative extracorporeal membrane oxygenation for in hospital cardiac arrest: a Canadian observational experience. Resuscitation. (2014) 85:1713–9. doi: 10.1016/j.resuscitation.2014.09.026
64. Wang CH, Chou NK, Becker LB, Lin JW Yu HY, Chi NH, et al. Improved outcome of extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest: a comparison with that for extracorporeal rescue for in-hospital cardiac arrest. Resuscitation. (2014) 85:1219–24. doi: 10.1016/j.resuscitation.2014.06.022
65. Fagnoul D, Taccone FS, Belhaj A, Rondelet B, Argacha JF, Vincent JL, et al. Extracorporeal life support associated with hypothermia and normoxemia in refractory cardiac arrest. Resuscitation. (2013) 84:1519–24. doi: 10.1016/j.resuscitation.2013.06.016
66. Siao FY, Chiu CC, Chiu CW, Chen YC, Chen YL, Hsieh YK, et al. Managing cardiac arrest with refractory ventricular fibrillation in the emergency department: conventional cardiopulmonary resuscitation vs. extracorporeal cardiopulmonary resuscitation. Resuscitation. (2015) 92:70–6. doi: 10.1016/j.resuscitation.2015.04.016
67. Wengenmayer T, Rombach S, Ramshorn F, Biever P, Bode C, Duerschmied D, et al. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit Care. (2017) 21:1–6. doi: 10.1186/s13054-017-1744-8
68. Tonna JE, Selzman CH, Girotra S, Presson AP, Thiagarajan RR, Becker LB, et al. Resuscitation using ECPR during in-hospital cardiac arrest (RESCUE-IHCA) mortality prediction score and external validation. JACC Cardiovasc Interv. (2022) 15:237–47. doi: 10.1016/j.jcin.2021.09.032
69. D'Arrigo S, Cacciola S, Dennis M, Jung C, Kagawa E, Antonelli M, et al. Predictors of favourable outcome after in-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation. (2017) 121:62–70. doi: 10.1016/j.resuscitation.2017.10.005
70. Agostinucci JM, Ruscev M, Galinski M, Gravelo S, Petrovic T, Carmeaux C, et al. Out-of-hospital use of an automated chest compression device: facilitating access to extracorporeal life support or non-heart-beating organ procurement. Am J Emerg Med. (2011) 29:1169–72. doi: 10.1016/j.ajem.2010.06.029
71. Cesana F, Avalli L, Garatti L, Coppo A, Righetti S, Calchera I, et al. Effects of extracorporeal cardiopulmonary resuscitation on neurological and cardiac outcome after ischaemic refractory cardiac arrest. Eur Heart J Acute Cardiovasc Care. (2018) 7:432–41. doi: 10.1177/2048872617737041
72. Choi DH, Kim YJ, Ryoo SM, Sohn CH, Ahn S, Seo DW, et al. Extracorporeal cardiopulmonary resuscitation among patients with out-of-hospital cardiac arrest. Clin Exp Emerg Med. (2016) 3:132. doi: 10.15441/ceem.16.145
73. Hase M, Tsuchihashi K, Fujii N, Nishizato K, Kokubu N, Nara S, et al. Early defibrillation and circulatory support can provide better long-term outcomes through favorable neurological recovery in patients with out-of-hospital cardiac arrest of cardiac origin. Circul J. (2005) 69:1302–7. doi: 10.1253/circj.69.1302
74. Kim SJ, Jung JS, Park JH, Park JS, Hong YS, Lee SW. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patients with out-of-hospital cardiac arrest: a propensity-matched study. Crit Care. (2014) 18:1–15. doi: 10.1186/s13054-014-0535-8
75. Lee SH, Jung JS, Lee KH, Kim HJ, Son HS, Sun K. Comparison of extracorporeal cardiopulmonary resuscitation with conventional cardiopulmonary resuscitation: Is extracorporeal cardiopulmonary resuscitation beneficial? Korean J Thorac Cardiovasc Surg. (2015) 48:318. doi: 10.5090/kjtcs.2015.48.5.318
76. Maekawa K, Tanno K, Hase M, Mori K, Asai Y. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin: a propensity-matched study and predictor analysis. Crit Care Med. (2013) 41:1186–96. doi: 10.1097/CCM.0b013e31827ca4c8
77. Poppe M, Weiser C, Holzer M, Sulzgruber P, Datler P, Keferböck M, et al. The incidence of “load&go” out-of-hospital cardiac arrest candidates for emergency department utilization of emergency extracorporeal life support: a 1-year review. Resuscitation. (2015) 91:131–6. doi: 10.1016/j.resuscitation.2015.03.003
78. Sakamoto T, Morimura N, Nagao K, Asai Y, Yokota H, Nara S, et al. Extracorporeal cardiopulmonary resuscitation vs. conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation. (2014) 85:762–8. doi: 10.1016/j.resuscitation.2014.01.031
79. Schober A, Sterz F, Herkner H, Wallmueller C, Weiser C, Hubner P, et al. Emergency extracorporeal life support and ongoing resuscitation: a retrospective comparison for refractory out-of-hospital cardiac arrest. Emerg Med J. (2017) 34:277–81. doi: 10.1136/emermed-2015-205232
80. Tanno K, Itoh Y, Takeyama Y, Nara S, Mori K, Asai Y. Utstein style study of cardiopulmonary bypass after cardiac arrest. Am J Emerg Med. (2008) 26:649–54. doi: 10.1016/j.ajem.2007.09.019
81. Venturini JM, Retzer E, Estrada JR, Friant J, Beiser D, Edelson D, et al. Mechanical chest compressions improve rate of return of spontaneous circulation and allow for initiation of percutaneous circulatory support during cardiac arrest in the cardiac catheterization laboratory. Resuscitation. (2017) 115:56–60. doi: 10.1016/j.resuscitation.2017.03.037
82. Yannopoulos D, Bartos JA, Raveendran G, Conterato M, Frascone RJ, Trembley A, et al. Coronary artery disease in patients with out-of-hospital refractory ventricular fibrillation cardiac arrest. J Am Coll Cardiol. (2017) 70:1109–17. doi: 10.1016/j.jacc.2017.06.059
83. Lamhaut L, Hutin A, Puymirat E, Jouan J, Raphalen JH, Jouffroy R, et al. A pre-hospital extracorporeal cardio pulmonary resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: an observational study and propensity analysis. Resuscitation. (2017) 117:109–17. doi: 10.1016/j.resuscitation.2017.04.014
84. Bougouin W, Dumas F, Lamhaut L, Marijon E, Carli P, Combes A, et al. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a registry study. Eur Heart J. (2020) 41:1961–71. doi: 10.1093/eurheartj/ehz753
85. Choi DS, Kim T, Ro YS, Ahn KO, Lee EJ, Hwang SS, et al. Extracorporeal life support and survival after out-of-hospital cardiac arrest in a nationwide registry: a propensity score-matched analysis. Resuscitation. (2016) 99:26–32. doi: 10.1016/j.resuscitation.2015.11.013
86. Le Guen M, Nicolas-Robin A, Carreira S, Raux M, Leprince P, Riou B, et al. Extracorporeal life support following out-of-hospital refractory cardiac arrest. Crit Care. (2011) 15:1–9. doi: 10.1186/cc9976
87. Leick J, Liebetrau C, Szardien S, Fischer-Rasokat U, Willmer M, van Linden A, et al. Door-to-implantation time of extracorporeal life support systems predicts mortality in patients with out-of-hospital cardiac arrest. Clin Res Cardiol. (2013) 102:661–9. doi: 10.1007/s00392-013-0580-3
88. Yannopoulos D, Bartos JA, Martin C, Raveendran G, Missov E, Conterato M, et al. Minnesota resuscitation consortium's advanced perfusion and reperfusion cardiac life support strategy for out-of-hospital refractory ventricular fibrillation. J Am Heart Assoc. (2016) 5:e003732. doi: 10.1161/JAHA.116.003732
89. Avalli L, Mauri T, Citerio G, Migliari M, Coppo A, Caresani M, et al. New treatment bundles improve survival in out-of-hospital cardiac arrest patients: a historical comparison. Resuscitation. (2014) 85:1240–4. doi: 10.1016/j.resuscitation.2014.06.014
90. Johnson NJ, Acker M, Hsu CH, Desai N, Vallabhajosyula P, Lazar S, et al. Extracorporeal life support as rescue strategy for out-of-hospital and emergency department cardiac arrest. Resuscitation. (2014) 85:1527–32. doi: 10.1016/j.resuscitation.2014.08.028
91. Lamhaut L, Tea V, Raphalen JH, An K, Dagron C, Jouffroy R, et al. Coronary lesions in refractory out of hospital cardiac arrest (OHCA) treated by extra corporeal pulmonary resuscitation (ECPR). Resuscitation. (2018) 126:154–9. doi: 10.1016/j.resuscitation.2017.12.017
92. Djordjevic I, Gaisendrees C, Adler C, Eghbalzadeh K, Braumann S, Ivanov B, et al. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest: first results and outcomes of a newly established ECPR program in a large population area. Perfusion. (2021) 37:249–56. doi: 10.1177/0267659121995995
93. Okada Y, Kiguchi T, Kitamura T, Iwami T. The association between low pH value and unfavorable neurological outcome among the out-of-hospital cardiac arrest patient treated by extra-corporeal CPR: sensitivity analysis. J Intensive Care. (2020) 8:1–9. doi: 10.1186/s40560-020-00470-3
94. Otani T, Sawano H, Natsukawa T, Nakashima T, Oku H, Gon C, et al. Low-flow time is associated with a favorable neurological outcome in out-of-hospital cardiac arrest patients resuscitated with extracorporeal cardiopulmonary resuscitation. J Crit Care. (2018) 48:15–20. doi: 10.1016/j.jcrc.2018.08.006
95. Hilker M, Philip A, Arlt M, Amann M, Lunz D, Müller T, et al. Pre-hospital cardiopulmonary resuscitation supported by ECMO: a case series of 6 patients. Thorac Cardiovasc Surg. (2013) 61(S 01):P45. doi: 10.1055/s-0032-1332685
96. Bartos JA, Grunau B, Carlson C, Duval S, Ripeckyj A, Kalra R, et al. Improved survival with extracorporeal cardiopulmonary resuscitation despite progressive metabolic derangement associated with prolonged resuscitation. Circulation. (2020) 141:877–86. doi: 10.1161/CIRCULATIONAHA.119.042173
97. Nakashima T, Noguchi T, Tahara Y, Nishimura K, Ogata S, Yasuda S, et al. Patients with refractory out-of-cardiac arrest and sustained ventricular fibrillation as candidates for extracorporeal cardiopulmonary resuscitation: Prospective multi-center observational study. Circul J. (2019) 83:1011–8. doi: 10.1253/circj.CJ-18-1257
98. Sawamoto K, Bird SB, Katayama Y, Maekawa K, Uemura S, Tanno K, et al. Outcome from severe accidental hypothermia with cardiac arrest resuscitated with extracorporeal cardiopulmonary resuscitation. Am J Emerg Med. (2014) 32:320–4. doi: 10.1016/j.ajem.2013.12.023
99. Okada Y, Kiguchi T, Irisawa T, Yamada T, Yoshiya K, Park C, et al. Development and validation of a clinical score to predict neurological outcomes in patients with out-of-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation. JAMA Netw Open. (2020) 3:e2022920. doi: 10.1001/jamanetworkopen.2020.22920
100. Kagawa E, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Kurisu S, et al. Assessment of outcomes and differences between in- and out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal life support. Resuscitation. (2010) 81:968–73. doi: 10.1016/j.resuscitation.2010.03.037
101. Lunz D, Calabrò L, Belliato M, Contri E, Broman LM, Scandroglio AM, et al. Extracorporeal membrane oxygenation for refractory cardiac arrest: a retrospective multicenter study. Intensive Care Med. (2020) 46:973–82. doi: 10.1007/s00134-020-05926-6
102. Wang J, Ma Q, Zhang H, Liu S, Zheng Y. Predictors of survival and neurologic outcome for adults with extracorporeal cardiopulmonary resuscitation: a systemic review and meta-analysis. Medicine. (2018) 97:6283197. doi: 10.1097/MD.0000000000013257
103. Debaty G, Babaz V, Durand M, Gaide-Chevronnay L, Fournel E, Blancher M, et al. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation. (2017) 112:1–10. doi: 10.1016/j.resuscitation.2016.12.011
104. Yukawa T, Kashiura M, Sugiyama K, Tanabe T, Hamabe Y. Neurological outcomes and duration from cardiac arrest to the initiation of extracorporeal membrane oxygenation in patients with out-of-hospital cardiac arrest: a retrospective study. Scand J Trauma Resusc Emerg Med. (2017) 25:1–7. doi: 10.1186/s13049-017-0440-7
105. Kippnich M, Lotz C, Kredel M, Schimmer C, Weismann D, Sommer C, et al. Venoarterielle extrakorporale Membranoxygenierung beim präklinischen Herz-Kreislauf-Stillstand. Anaesthesist. (2015) 64:580–5. doi: 10.1007/s00101-015-0058-y
106. Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2020) 142:S366–468. doi: 10.1161/CIR.0000000000000918
107. Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL, et al. Part 4: pediatric basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2020) 142:S469–523. doi: 10.1542/peds.2020-038505D
108. Soar J, Böttiger BW, Carli P, Couper K, Deakin CD, Djärv T, et al. European resuscitation council guidelines 2021: adult advanced life support. Resuscitation. (2021) 161:115–51. doi: 10.1016/j.resuscitation.2021.02.010
109. van de Voorde P, Turner NM, Djakow J, de Lucas N, Martinez-Mejias A, Biarent D, et al. European resuscitation council guidelines 2021: paediatric life support. Resuscitation. (2021) 161:327–87. doi: 10.1016/j.resuscitation.2021.02.015
110. Soar J, Berg KM, Andersen LW, Böttiger BW, Cacciola S, Callaway CW, et al. Adult advanced life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. (2020) 156:12. doi: 10.1161/CIR.0000000000000893
111. Soar J, Maconochie I, Wyckoff MH, Olasveengen TM, Singletary EM, Greif R, et al. 2019 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. (2019) 145:e826–80.
112. Soar J, MacOnochie I, Wyckoff MH, Olasveengen TM, Singletary EM, Greif R, et al. 2019 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Circulation. (2019) 140:e424–40. doi: 10.1161/CIR.0000000000000734
113. Maconochie IK, Aickin R, Hazinski MF, Atkins DL, Bingham R, Couto TB, et al. Pediatric life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. (2020) 142:S140–84. doi: 10.1542/peds.2020-038505B
114. Richardson AC, Tonna JE, Nanjayya V, Nixon P, Abrams DC, Raman L, et al. Extracorporeal cardiopulmonary resuscitation in adults. Interim guideline consensus statement from the extracorporeal life support organization. ASAIO J. (2021) 67:221. doi: 10.1097/MAT.0000000000001344
115. Guerguerian AM, Sano M, Todd M, Honjo O, Alexander P, Raman L, et al. Pediatric extracorporeal cardiopulmonary resuscitation ELSO guidelines. ASAIO J. (2021) 67:229–37. doi: 10.1097/MAT.0000000000001345
116. Tonna JE, Johnson NJ, Greenwood J, Gaieski DF, Shinar Z, Bellezo JM, et al. Practice characteristics of emergency department extracorporeal cardiopulmonary resuscitation (eCPR) programs in the United States: the current state of the art of emergency department extracorporeal membrane oxygenation (ED ECMO). Resuscitation. (2016) 107:38–46. doi: 10.1016/j.resuscitation.2016.07.237
117. Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication a consensus statement from the International Liaison Committee on Resuscitation. Circulation. (2008) 118:2452–83. doi: 10.1161/CIRCULATIONAHA.108.190652
118. Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. (2002) 346:557–63. doi: 10.1056/NEJMoa003289
119. Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. (2002) 346:549–56. doi: 10.1056/NEJMoa012689
120. Dankiewicz J, Cronberg T, Lilja G, Jakobsen JC, Levin H, Ullén S, et al. Hypothermia vs. normothermia after out-of-hospital cardiac arrest. N Engl J Med. (2021) 384:2283–94. doi: 10.1056/NEJMoa2100591
121. Sandroni C, Nolan JP, Andersen LW, Böttiger BW, Cariou A, Cronberg T, et al. ERC-ESICM guidelines on temperature control after cardiac arrest in adults. Intensive Care Med. (2022) 48:261–9. doi: 10.1007/s00134-022-06620-5
122. Tonna JE, Selzman CH, Bartos JA, Presson AP, Ou Z, Jo Y, et al. The association of modifiable mechanical ventilation settings, blood gas changes and survival on extracorporeal membrane oxygenation for cardiac arrest. Resuscitation. (2022) 174:53–61. doi: 10.1016/j.resuscitation.2022.03.016
123. Kashiura M, Yasuda H, Kishihara Y, Tominaga K, Nishihara M, Hiasa K, et al. Association between short-term neurological outcomes and extreme hyperoxia in patients with out-of-hospital cardiac arrest who underwent extracorporeal cardiopulmonary resuscitation: a retrospective observational study from a multicenter registry. BMC Cardiovasc Disord. (2022) 22:163. doi: 10.1186/s12872-022-02598-6
124. Holmberg MJ, Wiberg S, Ross CE, Kleinman M, Hoeyer-Nielsen AK, Donnino MW, et al. Trends in survival after pediatric in-hospital cardiac arrest in the United States. Circulation. (2019) 140:1398–408. doi: 10.1161/CIRCULATIONAHA.119.041667
125. Girotra S, Spertus JA Li Y, Berg RA, Nadkarni VM, Chan PS. Survival trends in pediatric in-hospital cardiac arrests an analysis from get with the guidelines-resuscitation. Circ Cardiovasc Qual Outcomes. (2013) 6:42–9. doi: 10.1161/CIRCOUTCOMES.112.967968
126. Berg RA, Sutton RM, Reeder RW, Berger JT, Newth CJ, Carcillo JA, et al. Association between diastolic blood pressure during pediatric in-hospital cardiopulmonary resuscitation and survival. Circulation. (2018) 137:1784–95. doi: 10.1161/CIRCULATIONAHA.117.032270
127. Morgan RW, Kirschen MP, Kilbaugh TJ, Sutton RM, Topjian AA. Pediatric in-hospital cardiac arrest and cardiopulmonary resuscitation in the United States: a review. JAMA Pediat. (2021) 168:110–8. doi: 10.1001/jamapediatrics.2020.5039
128. Hamzah M, Othman HF, Almasri M, Al-Subu A, Lutfi R. Survival outcomes of in-hospital cardiac arrest in pediatric patients in the USA. Eur J Pediatr. (2021) 180:2513–20. doi: 10.1007/s00431-021-04082-3
129. Berg RA, Nadkarni VM, Clark AE, Moler F, Meert K, Harrison RE, et al. Incidence and outcomes of cardiopulmonary resuscitation in PICUs. Crit Care Med. (2016) 44:798. doi: 10.1097/CCM.0000000000001484
130. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-−2020 update: a report from the American heart association. Circulation. (2020) 141:e139–596. doi: 10.1161/CIR.0000000000000746
131. Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Nadkarni VM, et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet. (2010) 375:1347–54. doi: 10.1016/S0140-6736(10)60064-5
132. Conrad SA, Rycus PT, Dalton H. Extracorporeal life support registry report 2004. ASAIO J. (2005) 51:4–10. doi: 10.1097/01.MAT.0000151922.67540.E9
133. Thiagarajan RR, Laussen PC, Rycus PT, Bartlett RH, Bratton SL. Extracorporeal membrane oxygenation to aid cardiopulmonary resuscitation in infants and children. Circulation. (2007) 116:1693–700. doi: 10.1161/CIRCULATIONAHA.106.680678
134. Farhat A, Ling RR, Jenks CL, Poon WH, Yang IX Li X, et al. Outcomes of pediatric extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care Med. (2021) 49:682–92. doi: 10.1097/CCM.0000000000004882
135. Meert K, Slomine BS, Silverstein FS, Christensen J, Ichord R, Telford R, et al. One-year cognitive and neurologic outcomes in survivors of paediatric extracorporeal cardiopulmonary resuscitation. Resuscitation. (2019) 139:299–307. doi: 10.1016/j.resuscitation.2019.02.023
136. Moler FW, Silverstein FS, Holubkov R, Slomine BS, Christensen JR, Nadkarni VM, et al. Therapeutic hypothermia after in-hospital cardiac arrest in children. N Engl J Med. (2017) 376:318–29. doi: 10.1056/nejmoa1610493
137. Lowry AW, Morales DLS, Graves DE, Knudson JD, Shamszad P, Mott AR, et al. Characterization of extracorporeal membrane oxygenation for pediatric cardiac arrest in the United States: analysis of the kids' inpatient database. Pediatr Cardiol. (2013) 34:1422–30. doi: 10.1007/s00246-013-0666-8
138. Barbaro RP, Paden ML, Guner YS, Raman L, Ryerson LM, Alexander P, et al. Pediatric extracorporeal life support organization registry international report 2016. ASAIO J. (2017) 63:60–7. doi: 10.1097/MAT.0000000000000475
139. Aharon AS, Drinkwater DC, Churchwell KB, Quisling S, Reddy VS, Taylor M, et al. Extracorporeal membrane oxygenation in children after repair of congenital cardiac lesions. Ann Thorac Surg. (2001) 72:2095–102. doi: 10.1016/S0003-4975(01)03209-X
140. Dalton HJ, Siewers RD, Fuhrman BP, del Nido P, Thompson AE, Shaver MG, et al. Extracorporeal membrane oxygenation for cardiac rescue in children with severe myocardial dysfunction. Crit Care Med. (1993) 21:1020–8.
141. Duncan BW, Ibrahim AE, Hraska V, del Nido P, Laussen PC, Wessel DL, et al. Use of rapid-deployment extracorporeal membrane oxygenation for the resuscitation of pediatric patients with heart disease after cardiac arrest. J Thorac Cardiovasc Surg. (1998) 116:305–11.
142. Parra DA, Totapally BR, Zahn E, Jacobs J, Aldousany A, Burke RP, et al. Outcome of cardiopulmonary resuscitation in a pediatric cardiac intensive care unit. Crit Care Med. (2000) 28:3296–300. doi: 10.1097/00003246-200009000-00030
143. Thourani VH, Kirshbom PM, Kanter KR, Simsic J, Kogon BE, Wagoner S, et al. Venoarterial extracorporeal membrane oxygenation (VA-ECMO) in pediatric cardiac support. Ann Thorac Surg. (2006) 82:138–45. doi: 10.1016/j.athoracsur.2006.02.011
144. Shah SA, Shankar V, Churchwell KB, Taylor MB, Scott BP, Bartilson R, et al. Clinical outcomes of 84 children with congenital heart disease managed with extracorporeal membrane oxygenation after cardiac surgery. ASAIO J. (2005) 51:504–7. doi: 10.1097/01.mat.0000171595.67127.74
145. Anton-Martin P, Moreira A, Kang P, Green ML. Outcomes of paediatric cardiac patients after 30 min of cardiopulmonary resuscitation prior to extracorporeal support. Cardiol Young. (2020) 30:607–16. doi: 10.1017/S1047951120000591
146. Kramer P, Mommsen A, Miera O, Photiadis J, Berger F, Schmitt KRL. Survival and mid-term neurologic outcome after extracorporeal cardiopulmonary resuscitation in children. Pediatric Crit Care Med. (2020) 21:e316–24. doi: 10.1097/PCC.0000000000002291
147. Philip J, Burgman C, Bavare A, Akcan-Arikan A, Price JF, Adachi I, et al. Nature of the underlying heart disease affects survival in pediatric patients undergoing extracorporeal cardiopulmonary resuscitation. J Thorac Cardiovasc Surg. (2014) 148:2367–72. doi: 10.1016/j.jtcvs.2014.03.023
148. Erek E, Aydin S, Suzan D, Yildiz O, Altin F, Kirat B, et al. Extracorporeal cardiopulmonary resuscitation for refractory cardiac arrest in children after cardiac surgery. Anatol J Cardiol. (2017) 17:328. doi: 10.14744/AnatolJCardiol.2016.6658
149. Sperotto F, Saengsin K, Danehy A, Godsay M, Geisser DL, Rivkin M, et al. Modeling severe functional impairment or death following ECPR in pediatric cardiac patients: planning for an interventional trial. Resuscitation. (2021) 167:12–21. doi: 10.1016/j.resuscitation.2021.07.041
150. Lasa JJ, Rogers RS, Localio R, Shults J, Raymond T, Gaies M, et al. Extracorporeal cardiopulmonary resuscitation (E-CPR) during pediatric in-hospital cardiopulmonary arrest is associated with improved survival to discharge. Circulation. (2016) 133:165–76. doi: 10.1161/CIRCULATIONAHA.115.016082
151. Raymond TT, Cunnyngham CB, Thompson MT, Thomas JA, Dalton HJ, Nadkarni VM. Outcomes among neonates, infants, and children after extracorporeal cardiopulmonary resuscitation for refractory in-hospital pediatric cardiac arrest: a report from the national registry of cardiopulmonary resuscitation. Pediatric Crit Care Med. (2010) 11:362–71. doi: 10.1097/PCC.0b013e3181c0141b
152. Ortmann L, Prodhan P, Gossett J, Schexnayder S, Berg R, Nadkarni V, et al. Outcomes after in-hospital cardiac arrest in children with cardiac disease: a report from get with the guidelines-resuscitation. Circulation. (2011) 124:2329–37. doi: 10.1161/CIRCULATIONAHA.110.013466
153. Matos RI, Watson RS, Nadkarni VM, Huang HH, Berg RA, Meaney PA, et al. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation. (2013) 127:442–51. doi: 10.1161/CIRCULATIONAHA.112.125625
154. Alten JA, Klugman D, Raymond TT, Cooper DS, Donohue JE, Zhang W, et al. Epidemiology and outcomes of cardiac arrest in pediatric cardiac ICUs. Pediatric Crit Care Med. (2017) 18:935. doi: 10.1097/PCC.0000000000001273
155. Joffe AR, Lequier L, Robertson CMT. Pediatric outcomes after extracorporeal membrane oxygenation for cardiac disease and for cardiac arrest: a review. ASAIO J. (2012) 58:297–310. doi: 10.1097/MAT.0b013e31825a21ff
156. Morris MC, Wernovsky G, Nadkarni VM. Survival outcomes after extracorporeal cardiopulmonary resuscitation instituted during active chest compressions following refractory in-hospital pediatric cardiac arrest. Pediatric Crit Care Med. (2004) 5:440–6. doi: 10.1097/01.PCC.0000137356.58150.2E
157. Barrett CS, Bratton SL, Salvin JW, Laussen PC, Rycus PT, Thiagarajan RR. Neurological injury after extracorporeal membrane oxygenation use to aid pediatric cardiopulmonary resuscitation. Pediatric Crit Care Med. (2009) 10:445–51. doi: 10.1097/PCC.0b013e318198bd85
158. Bembea MM, Ng DK, Rizkalla N, Rycus P, Lasa JJ, Dalton H, et al. Outcomes after extracorporeal cardiopulmonary resuscitation of pediatric in-hospital cardiac arrest: a report from the get with the guidelines-resuscitation and the extracorporeal life support organization registries. Crit Care Med. (2019) 47:e278–85. doi: 10.1097/CCM.0000000000003622
159. Conrad SJ, Bridges BC, Kalra Y, Pietsch JB, Smith AH. Extracorporeal cardiopulmonary resuscitation among patients with structurally normal hearts. ASAIO J. (2017) 63:781–6. doi: 10.1097/MAT.0000000000000568
160. Torres-Andres F, Fink EL, Bell MJ, Sharma MS, Yablonsky EJ, Sanchez-De-Toledo J. Survival and long-term functional outcomes for children with cardiac arrest treated with extracorporeal cardiopulmonary resuscitation. Pediatric Crit Care Med. (2018) 19:451. doi: 10.1097/PCC.0000000000001524
161. Wolf MJ, Kanter KR, Kirshbom PM, Kogon BE, Wagoner SF. Extracorporeal cardiopulmonary resuscitation for pediatric cardiac patients. Ann Thorac Surg. (2012) 94:874–80. doi: 10.1016/j.athoracsur.2012.04.040
162. Sivarajan V, Best D, Brizard CP, Shekerdemian LS, D'Udekem Y, Butt W. Duration of resuscitation prior to rescue extracorporeal membrane oxygenation impacts outcome in children with heart disease. Intensive Care Med. (2011) 37:853–60. doi: 10.1007/s00134-011-2168-6
163. Shakoor A, Pedroso FE, Jacobs SE, Okochi S, Zenilman A, Cheung EW, et al. Extracorporeal cardiopulmonary resuscitation (ECPR) in infants and children: a single-center retrospective study. World J Pediatr Congenit Heart Surg. (2019) 10:582–9. doi: 10.1177/2150135119862598
164. Garcia Guerra G, Zorzela L, Robertson CMT, Alton GY, Joffe AR, Moez EK, et al. Survival and neurocognitive outcomes in pediatric extracorporeal-cardiopulmonary resuscitation. Resuscitation. (2015) 96:208–13. doi: 10.1016/j.resuscitation.2015.07.034
165. Walter EMD, Alexi-Meskishvili V, Huebler M, Redlin M, Boettcher W, Weng Y, et al. Rescue extracorporeal membrane oxygenation in children with refractory cardiac arrest. Interact Cardiovasc Thorac Surg. (2011) 12:929–34. doi: 10.1510/icvts.2010.254193
166. Burke CR, Chan T, Brogan TV, McMullan DM. Pediatric extracorporeal cardiopulmonary resuscitation during nights and weekends. Resuscitation. (2017) 114:47–52. doi: 10.1016/j.resuscitation.2017.03.001
167. Beshish AG, Baginski MR, Johnson TJ, Deatrick BK, Barbaro RP, Owens GE. Functional status change among children with extracorporeal membrane oxygenation to support cardiopulmonary resuscitation in a pediatric cardiac ICU: a single institution report. Pediatric Crit Care Med. (2018) 19:665–71. doi: 10.1097/PCC.0000000000001555
168. Alsoufi B, Awan A, Manlhiot C, Guechef A, Al-Halees Z, Al-Ahmadi M, et al. Results of rapid-response extracorporeal cardiopulmonary resuscitation in children with refractory cardiac arrest following cardiac surgery. Eur J Cardio-thorac Surg. (2014) 45:268–75. doi: 10.1093/ejcts/ezt319
169. Alsoufi B, Al-Radi OO, Nazer RI, Gruenwald C, Foreman C, Williams WG, et al. Survival outcomes after rescue extracorporeal cardiopulmonary resuscitation in pediatric patients with refractory cardiac arrest. J Thorac Cardiovasc Surg. (2007) 134:952–9. doi: 10.1016/j.jtcvs.2007.05.054
170. Prodhan P, Fiser RT, Dyamenahalli U, Gossett J, Imamura M, Jaquiss RDB, et al. Outcomes after extracorporeal cardiopulmonary resuscitation (ECPR) following refractory pediatric cardiac arrest in the intensive care unit. Resuscitation. (2009) 80:1124–9. doi: 10.1016/j.resuscitation.2009.07.004
171. Kane DA, Thiagarajan RR, Wypij D, Scheurer MA, Fynn-Thompson F, Emani S, et al. Rapid-response extracorporeal membrane oxygenation to support cardiopulmonary resuscitation in children with cardiac disease. Circulation. (2010) 122(11 SUPPL_1):S241–8. doi: 10.1161/CIRCULATIONAHA.109.928390
172. Huang SC, Wu ET, Wang CC, Chen YS, Chang CI, Chiu IS, et al. Eleven years of experience with extracorporeal cardiopulmonary resuscitation for paediatric patients with in-hospital cardiac arrest. Resuscitation. (2012) 83:710–4. doi: 10.1016/j.resuscitation.2012.01.031
173. Melvan JN, Davis J, Heard M, Trivedi JR, Wolf M, Kanter KR, et al. Factors associated with survival following extracorporeal cardiopulmonary resuscitation in children. World J Pediatr Congenit Heart Surg. (2020) 11:265–74. doi: 10.1177/2150135120902102
174. Mattke AC, Stocker CF, Schibler A, Alphonso N, Johnson K, Karl TR, et al. newly established extracorporeal life support assisted cardiopulmonary resuscitation (ECPR) program can achieve intact neurological outcome in 60 % of children. Intensive Care Med. (2015) 41:2227–8. doi: 10.1007/s00134-015-4036-2
175. de Mul A, Nguyen DA, Doell C, Perez MH, Cannizzaro V, Karam O. Prognostic evaluation of mortality after pediatric resuscitation assisted by extracorporeal life support. J Pediatr Intensive Care. (2019) 08:057–63. doi: 10.1055/s-0038-1667012
176. Kendirli T, Özcan S, Havan M, Baran C, Çakici M, Arici B, et al. Pediatric extracorporeal cardiopulmonary resuscitation: single-center study. Turk J Med Sci. (2021) 51:1733–7. doi: 10.3906/sag-2002-10
177. Tsukahara K, Toida C, Muguruma T. Current experience and limitations of extracorporeal cardiopulmonary resuscitation for cardiac arrest in children: a single-center retrospective study. J Intensive Care. (2014) 2:1–5. doi: 10.1186/s40560-014-0068-x
178. Loaec M, Himebauch AS, Kilbaugh TJ, Berg RA, Graham K, Hanna R, et al. Pediatric cardiopulmonary resuscitation quality during intra-hospital transport. Resuscitation. (2020) 152:123–30. doi: 10.1016/j.resuscitation.2020.05.003
179. Arlt M, Philipp A, Voelkel S, Graf BM, Schmid C, Hilker M. Out-of-hospital extracorporeal life support for cardiac arrest: a case report. Resuscitation. (2011) 82:1243–5. doi: 10.1016/j.resuscitation.2011.03.022
180. Kelly RB, Harrison RE. Outcome predictors of pediatric extracorporeal cardiopulmonary resuscitation. Pediatr Cardiol. (2010) 31:626–33. doi: 10.1007/s00246-010-9659-z
181. Polimenakos AC, Rizzo V, El-Zein CF, Ilbawi MN. Post-cardiotomy rescue extracorporeal cardiopulmonary resuscitation in neonates with single ventricle after intractable cardiac arrest: attrition after hospital discharge and predictors of outcome. Pediatr Cardiol. (2017) 38:314–23. doi: 10.1007/s00246-016-1515-3
182. Topjian AA, Berg RA. Pediatric out-of-hospital cardiac arrest. Circulation. (2012) 125:2374–8. doi: 10.1161/CIRCULATIONAHA.111.071472
183. Nguyen DA, de Mul A, Hoskote AU, Cogo P, da Cruz EM, Erickson S, et al. Factors associated with initiation of extracorporeal cardiopulmonary resuscitation in the pediatric population: an international survey. ASAIO J. (2022) 68:413–8. doi: 10.1097/MAT.0000000000001495
184. Topjian AA, de Caen A, Wainwright MS, Abella BS, Abend NS, Atkins DL, et al. Pediatric post-cardiac arrest care: a scientific statement from the American heart association. Circulation. (2019) 140:e194–233. doi: 10.1161/CIR.0000000000000697
185. Duff JP, Topjian AA, Berg MD, Chan M, Haskell SE, Joyner BL, et al. 2019 American heart association focused update on pediatric advanced life support: an update to the American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2019) 140:e904–14. doi: 10.1161/CIR.0000000000000731
186. Moler FW, Silverstein FS, Holubkov R, Slomine BS, Christensen JR, Nadkarni VM, et al. Therapeutic hypothermia after out-of-hospital cardiac arrest in children. N Engl J Med. (2015) 372:1898–908. doi: 10.1056/NEJMoa1411480
187. Bembea MM, Nadkarni VM, Diener-West M, Venugopal V, Carey SM, Berg RA, et al. Temperature patterns in the early postresuscitation period after pediatric in-hospital cardiac arrest. Pediatric Crit Care Med. (2010) 11:723–30. doi: 10.1097/PCC.0b013e3181dde659
188. Topjian AA, Telford R, Holubkov R, Nadkarni VM, Berg RA, Dean JM, et al. The association of early post-resuscitation hypotension with discharge survival following targeted temperature management for pediatric in-hospital cardiac arrest. Resuscitation. (2019) 141:24–34. doi: 10.1016/j.resuscitation.2019.05.032
189. Lawson S, Ellis C, Butler K, McRobb C, Mejak B. Neonatal extracorporeal membrane oxygenation devices, techniques and team roles: 2011 survey results of the United States' extracorporeal life support organization centers. J Extra-Corp Technol. (2011) 43:236.
190. McMullan DM, Thiagarajan RR, Smith KM, Rycus PT, Brogan T. Extracorporeal cardiopulmonary resuscitation outcomes in term and premature neonates. Pediatric Crit Care Med. (2014) 15:e9–e16. doi: 10.1097/PCC.0b013e3182a553f3
191. Polimenakos AC, Wojtyla P, Smith PJ, Rizzo V, Nater M, El Zein CF, et al. Post-cardiotomy extracorporeal cardiopulmonary resuscitation in neonates with complex single ventricle: analysis of outcomes. Eur J Cardio-thorac Surg. (2011) 40:1396–405. doi: 10.1016/j.ejcts.2011.01.087
192. Laussen PC, Guerguerian AM. Establishing and sustaining an ECPR program. Front Pediatrics. (2018) 6:152. doi: 10.3389/fped.2018.00152
193. Su L, Spaeder MC, Jones MB, Sinha P, Nath DS, Jain PN, et al. Implementation of an extracorporeal cardiopulmonary resuscitation simulation program reduces extracorporeal cardiopulmonary resuscitation times in real patients. Pediatric Crit Care Med. (2014) 15:856–60. doi: 10.1097/PCC.0000000000000234
194. Ueda K, Yamane T, Aguru Y, Shibata M. Establishing protocol and simulation-based learning to initiate ECPR in our institution. J Am Coll Cardiol. (2019) 73:2145. doi: 10.1016/S0735-1097(19)32751-2
195. Stoner AC, Schremmer RD, Miller MA, Davidson KL, Pedigo RL, Parson JS, et al. Simulation-based system analysis: testing preparedness for extracorporeal membrane oxygenation cannulation in pediatric COVID-19 patients. Pediatr Qual Saf. (2022) 7:e510. doi: 10.1097/pq9.0000000000000510
196. Turek JW, Andersen ND, Lawson DS, Bonadonna D, Turley RS, Peters MA, et al. Outcomes before and after implementation of a pediatric rapid-response extracorporeal membrane oxygenation program. Ann Thorac Surg. (2013) 95:2140–7. doi: 10.1016/j.athoracsur.2013.01.050
197. Sin SWC, Ng PY, Ngai WCW, Lai PCK, Mok AYT, Chan RWK. Simulation training for crises during venoarterial extracorporeal membrane oxygenation. J Thorac Dis. (2019) 11:2144. doi: 10.21037/jtd.2019.04.54
198. Sawyer T. Simulation training in extracorporeal cardiopulmonary resuscitation (ECPR). Acad Pediatrics. (2021) 21:438–9. doi: 10.1016/j.acap.2020.11.004
199. Sawyer T, Burke C, McMullan DM, Chan T, Valdivia H, Yalon L, et al. Impacts of a pediatric extracorporeal cardiopulmonary resuscitation (ECPR) simulation training program. Acad Pediatr. (2019) 19:566–71. doi: 10.1016/j.acap.2019.01.005
200. di Nardo M, David P, Stoppa F, Lorusso R, Raponi M, Amodeo A, et al. The introduction of a high-fidelity simulation program for training pediatric critical care personnel reduces the times to manage extracorporeal membrane oxygenation emergencies and improves teamwork. J Thorac Dis. (2018) 10:3409. doi: 10.21037/jtd.2018.05.77
201. Thomas F, Chung S, Holt DW. Effects of ECMO simulations and protocols on patient safety. J Extra-Corp Technol. (2019) 51:12.
202. Puślecki M, Ligowski M, Dabrowski M, Stefaniak S, Ładzińska M, Ładziński P, et al. BEST life—“bringing ECMO simulation to life”—how medical simulation improved a regional ECMO program. Artif Org. (2018) 42:1052–61. doi: 10.1111/aor.13332
203. Whitmore SP, Gunnerson KJ, Haft JW, Lynch WR, VanDyck T, Hebert C, et al. Simulation training enables emergency medicine providers to rapidly and safely initiate extracorporeal cardiopulmonary resuscitation (ECPR) in a simulated cardiac arrest scenario. Resuscitation. (2019) 138:68–73. doi: 10.1016/j.resuscitation.2019.03.002
204. Weems MF, Friedlich PS, Nelson LP, Rake AJ, Klee L, Stein JE, et al. The role of extracorporeal membrane oxygenation simulation training at extracorporeal life support organization centers in the United States. Simul Healthcare. (2017) 12:233–9. doi: 10.1097/SIH.0000000000000243
205. Lasa JJ, Jain P, Raymond TT, Minard CG, Topjian A, Nadkarni V, et al. Extracorporeal cardiopulmonary resuscitation in the pediatric cardiac population: in search of a standard of care. Pediatric Crit Care Med. (2018) 19:125. doi: 10.1097/PCC.0000000000001388
206. Ross P, Nickson C, Sheldrake J, McClure J. Using in-situ simulation for extracorporeal cardiopulmonary resuscitation (ECPR) guideline development. SSRN Elect J. (2019) 2019:21. doi: 10.2139/ssrn.3409806
Keywords: ECMO—extracorporeal membrane oxygenation, ECPR program, ECPR training, extracorporeal resuscitation, pediatric ECPR, adult ECPR
Citation: Olson T, Anders M, Burgman C, Stephens A and Bastero P (2022) Extracorporeal cardiopulmonary resuscitation in adults and children: A review of literature, published guidelines and pediatric single-center program building experience. Front. Med. 9:935424. doi: 10.3389/fmed.2022.935424
Received: 03 May 2022; Accepted: 04 November 2022;
Published: 21 November 2022.
Edited by:
Andrea Montisci, Ospedale Civile di Brescia, ItalyReviewed by:
Lakshmi Raman, University of Texas Southwestern Medical Center, United StatesWarwick Wolf Butt, Royal Children's Hospital, Australia
Fabrizio De Rita, Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom
Copyright © 2022 Olson, Anders, Burgman, Stephens and Bastero. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Patricia Bastero, pxbaster@texaschildrens.org
 Taylor Olson
Taylor Olson Marc Anders
Marc Anders Cole Burgman4
Cole Burgman4  Adam Stephens
Adam Stephens Patricia Bastero
Patricia Bastero