Perception and Performance on a Virtual Reality Cognitive Stimulation for Use in the Intensive Care Unit: A Non-randomized Trial in Critically Ill Patients
- 1Gerontechnology and Rehabilitation Group, University of Bern, Bern, Switzerland
- 2Department of Intensive Care Medicine, University Hospital Bern (Inselspital), University of Bern, Bern, Switzerland
- 3Department of Neurology, University Neurorehabilitation, University Hospital Bern (Inselspital), University of Bern, Bern, Switzerland
- 4ARTORG Center for Biomedical Engineering Research, University of Bern, Bern, Switzerland
Background: Newly acquired long-term cognitive impairments are common among survivors of critical illness. They have been linked to the stressful situation that patients experience in the intensive care unit (ICU). In this paper we use virtual reality (VR) technology to comfort critically ill patients and reduce stress during their ICU stay. We investigate the acceptance, comfort, recollection, and visual perception of VR stimulation and how it affects physiological parameters.
Methods: A VR head-mounted display was used to present immersive nature scenes to 33 critically ill cardiac surgery patients [mean age 63 years (range 32–83)]. Data was collected with an eye tracker fitted inside the VR head-mounted display to measure eye movements (250 Hz) and sensors to record physiological parameters (240 Hz). Patients received VR stimulation (for 5 min.) prior to ICU admission, during ICU stay, and 3 months after discharge. Acceptance, recollection and comfort were assessed with validated questionnaires.
Results: The number of gazed meaningful objects per minute was significantly lower during the ICU session compared to pre- and follow-up sessions, whereas mean duration of fixation on meaningful moving objects did not differ between the sessions. While respiratory rate decreased significantly during VR stimulation, heart rate and blood pressure remained constant. Post-ICU rating of VR acceptance during ICU stay was moderate to high and discomfort low. Recollection of VR was high [28/33 patients (84.8%)], while recollection of ICU stay was low [10/33 patients (30.3%)].
Conclusion: Eye movements indicate that patients were able to perceive and process cognitive stimulation during their ICU stay. VR was recalled better than the rest of the ICU stay and well accepted. Decreased respiratory rate during stimulation indicate a relaxing effect of VR.
Introduction
The intensive care unit (ICU) is a noisy and stressful environment in which critically ill patients are exposed to psychological stress factors, including sensory overload and deprivation, isolation, temporal disorientation and a feeling of lack of control (1, 2). After ICU stay, ~50–75% of all critically ill patients will suffer from newly acquired long-term cognitive impairment (3–5). These cognitive long-term effects were linked to the stressful situation that patients experience during their ICU stay (4, 6). They negatively affect health-related quality of life after ICU discharge and reduce the effectiveness of intensive care (7–9).
We therefore embarked to develop a novel strategy using virtual reality (VR)-based cognitive stimulation technology to comfort critically ill patients during their stay in the ICU. When wearing a head-mounted VR display, patients do not hear or see the ICU and they are virtually “taken out” of the ICU and moved into a pleasant virtual environment. The virtual environment can be designed to the needs of immobile critically ill patients and applied directly in bed.
We decided to present pleasant nature scenes to critically ill patients because others have shown the beneficial effects of exposure to nature scenes. A study with 38 healthy participants described the cognitive benefits (i.e., directed attention) arising from the interaction with nature (10). In another study, Gamble et al. found that looking at nature pictures improves executive attention in older adults (11). There are two complementary theories related to the restorative effects of natural environments i.e., positive emotional state, reduced physiological activity level and increased cognitive functions. The first theory, called the Attention Restoration Theory, states that directed (i.e., high-effort) and voluntary (i.e., low-effort) attention, which influences cognitive performance, is a limited resource and can be depleted over a prolonged period of time. Directed and voluntary attention can be restored by interacting with nature environments (11–13). In rather stressful environments like the ICU, however, one must be vigilant, causing cognitive functions to decline. The second theory, the Stress Recovery Theory, postulates that nature environments reduce fear and anger, and have a stimulating effect on the parasympathetic nervous system shown in physical markers of stress (e.g., decreasing respiratory rate) (14). An established line of research suggests that exploring nature in VR has a restorative effect, similar to being outside in nature (13).
The state-of-the-art therapy provided to critically ill patients focuses on physical rehabilitation, and there is currently no consensus on how to prevent cognitive impairments after ICU discharge (15, 16). However, Turon et al. showed that training of cognitive functions presented on a television screen is feasible and may be beneficial for critically ill patients (17).
In a previous study, we demonstrated that healthy participants stimulated by nature videos through immersive VR in the ICU were more relaxed after the stimulation. Additionally, visual attention was not depleted during the course of the VR stimulation (18). Our finding suggests that participants were highly immersed and able to ignore the actual surroundings and restore their visual attention. To our knowledge, it remains unclear whether VR stimulation in critically ill patients would produce physiological and psychological restorative effects comparable with those observed in healthy participants.
The aim of this feasibility study in critically ill patients was to investigate the acceptance, comfort, recollection, visual perception and processing of immersive nature-related VR stimulation, and how VR affects physiological parameters. We hypothesized the following: firstly, that VR stimulation using the new proposed method offers high usability, immersion and satisfaction, is recollected and does not promote discomfort; secondly, that patients would be able to perceive and process the VR stimulation (i.e., visual attention) before and during their stay in the ICU; thirdly, that VR stimulation will reduce physiological markers of stress.
Materials and Methods
Participant Recruitment
This study was approved by the Ethics Committee of the Canton of Bern, Switzerland (KEK no. 2016-01652) and was registered at Clinicaltrails.gov (no. NCT03025373). The required sample size was calculated using the G*Power 3 software (19) based on a power of 80 and alpha error of 0.5. The effect size was estimated as medium-large according to the classification by Cohen, on the basis of our previous experience with VR stimulation in the ICU (relaxing effect of the VR stimulation, i.e., physiological measures), which was resulting in a sample size of 50 patients (18). Inclusion criteria were age >18 years, no neurological disorder, including delirium and planned elective open-heart surgery. Patients were recruited on admission to the ICU between 17 April 2017 and 13 March 2018.
Procedure
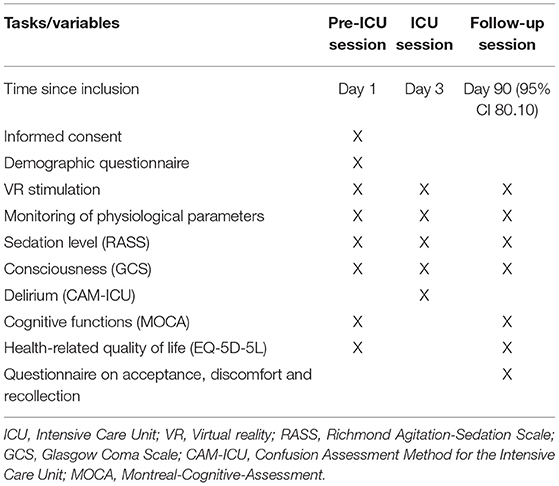
The study was split into three phases (Table 1): (i) An initial session 1 day prior to ICU admission (pre-ICU session), (ii) a second session the day after surgery (ICU session), and (iii) a follow-up session ~3 months after ICU discharge (follow-up session). In the initial session, patients were briefed, signed the informed consent, filled out questionnaires on demographics, and health-related quality of life (EQ-5D-5L) (20) and cognitive functions [Montreal-Cognitive-Assessment (MoCA) (21)] were assessed. Patients were then prepared for the VR stimulation by a study nurse, i.e., lying on the bed and monitoring of physiological parameters. After 10 min of rest, patients were stimulated with the nature VR environment for 5 min. Patients were stimulated in the ICU the morning after surgery the second time. Sedation level RASS, GCS, and delirium [Confusion Assessment Method for the ICU, CAM-ICU (22)] were assessed by trained ICU nurses. In the follow-up sessions, patients were stimulated again and questioned about their memories of the intensive care experience and acceptance, comfort and memories of the VR stimulation. The assessment of cognitive functions compared to the registered clinical trial a deviation exists. Since the Consortium to Establish a Registry for Alzheimer's Disease (CERAD) (23) was too time consuming for patients and had a too high workload instead the MoCA was used. There is evidence that the MoCA assess cognitive functions at a comparable level but is much shorter in time and needs less workload (24).
Cognitive VR Stimulation
All measurements were conducted in a two to four-bed ICU cubicle (Figure 2). The setup to stimulate patients consisted of several elements: (i) a computer, a head-mounted display with a built-in eye-tracker and noise canceling headphones, (ii) the equipment to measure the physiological parameters, (iii) a noise-signal monitor -positioned directly next to the patient- to register noise >50 dB. The setup was audited by the Medical Technology Department of the University Hospital of Berne for hygiene and medical eligibility requirements and was approved thereafter for use in ICU patients.
The VR stimulation consisted of a video presenting aquatic worlds and landscapes for 5 min. In addition, complementary classical music was played through noise-canceling headphones. The VR stimulation device (HTC Vive, High Tech Computer Corporation, Taoyuan, Taiwan) is a head-mounted display and was powered by a graphic card (NVIDIA GTX980, Nvidia, Santa Clara, USA). Eye movements were sampled as fixation points at a frequency of 250 Hz inside the head-mounted display by an eye tracker (SensoMotoric Instruments, Teltow, Germany). During VR stimulation sessions, eye movements were streamed to a second screen monitored by the investigators.
In all three sessions, heart and respiratory rates were continuously monitored by five-lead electrocardiography at a frequency of 240 Hz (Carescape Monitor B650, GE Healthcare, Little Chalfont, United Kingdom). In the pre-ICU and follow-up sessions, the blood pressure was measured every 2 min by a cuff-based blood pressure monitor. After surgery, blood pressure was continuously measured by an invasive intra-arterial blood pressure monitor.
In the follow-up session the questionnaire on a 5-point scale (from zero to four, Table 2) was used to assess acceptance, comfort and recollection of the VR method during the ICU session. Acceptance and, thus the sub domain immersion, was assessed by questions from the Igroup Presence Questionnaire (IPQ) (25), whereas usability and satisfaction were assessed by questions from the System Usability Scale (SUS) (26). The Simulator Sickness Questionnaire (SSQ) was used to assess the level of discomfort during VR stimulation (27), and the ICU Memory tool to assess recollection (28).
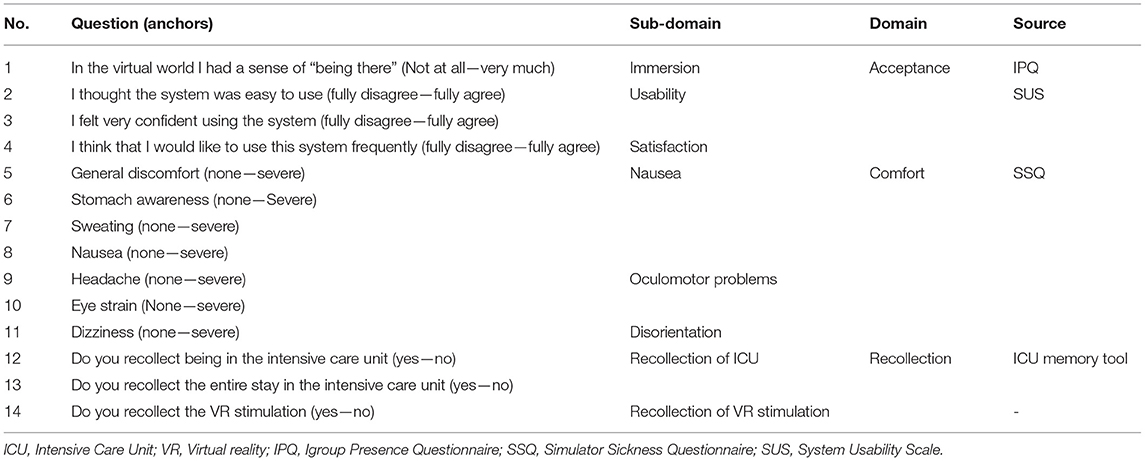
Table 2. Questionnaire on acceptance, discomfort, and recollection of the virtual reality stimulation during intensive care unit session.
Statistical Analysis
Analyses were performed at the individual level, whereas eye movements were measured as a collection of fixation points (i.e., gaze data), where a fixation had a minimum duration of 100 ms and dispersed around 2 degrees (29). The number of gazed moving objects outside the region of interest (e.g., dolphin) was calculated. To analyze the time effect (visual attention over time), the difference between the beginning of stimulation (first 15 s) and the last 15 s of stimulation was used and tested with one sample t-test against zero for significance (two-sided). The differences in eye movement (i.e., mean fixation duration, number of fixations, number of gazed meaningful moving objects and time fixated on one moving object) between the three sessions were analyzed by one-way analysis of variance (ANOVA) and Bonferroni adjustment as a post hoc analysis. The same analysis was used to examine health-related quality of life (i.e., EQ-5D-5L), cognitive functions (i.e., MoCA) and whether VR stimulation had a relaxing effect (decreasing physiological signs during stimulation). A one-sided t-test (i.e., directed hypotheses) was used based on the findings of our previous VR study (18) and the assumption that the relaxing effect always involves a reduction in physiological signs. For the questionnaire ratings, a one-sided t-test was used to test whether the majority was above or below the midpoint of the score scale. The data was analyzed using R (30) and Matlab18b (31).
URL
A video of the immersive nature VR stimulation and a video including the region of interest used in the analysis can be found on our website http://www.artorg.unibe.ch/research/ger/group_members/persons/gerber_stephan/index_eng.html#pane482606.
Results
Demographics
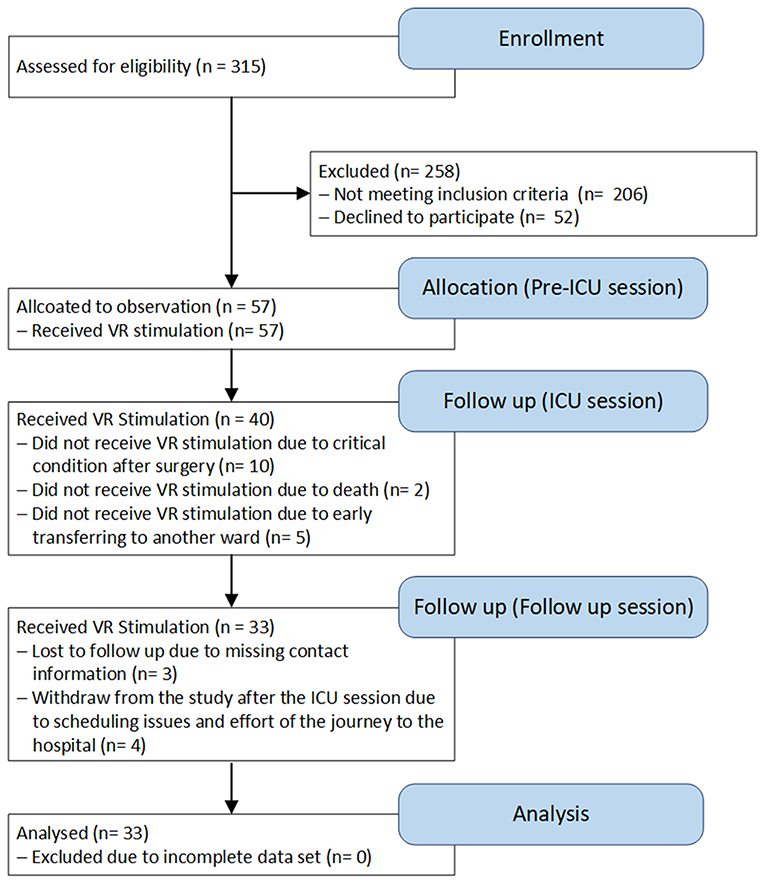
A total of 57 patients undergoing heart surgery participated in the study (Figure 1), and 33 patients (26 male) completed all the sessions (Pre-ICU, ICU, and Follow up sessions). The mean age of patients completing all the sessions was 63 years (range 32–83 years). In all the VR stimulation sessions, patients had a Glasgow Coma Score (GCS) (32) of 15 and a Richmond Agitation-Sedation Score (RASS) (33) of 0. In the second VR treatment during the ICU stay, patients had, on average, an APACHE II score of 22.3 (95% CI 20.3–24.2) and a SAPS II of 53.4 (95% CI 48.1–58.6), and all were extubated [on average within 8.1 h (95% CI 6.4–9.8)]. ICU length of stay was 0.9 days (95% CI 0.8–0.9). In the pre-ICU and follow-up sessions, 54.6 and 66.7%, respectively, of the patients received medication influencing blood pressure, while 33.3 and 69.7%, respectively, received medication influencing heart rate. During the ICU session all patients received medication influencing the heart rate, blood pressure and respiratory rate (i.e., antihypertensives or catecholamines, analgesics, sedatives). Patients who did not participate in all sessions were not considered in the final analysis and were considered as drop-outs. All dropouts were unrelated to the VR stimulation.
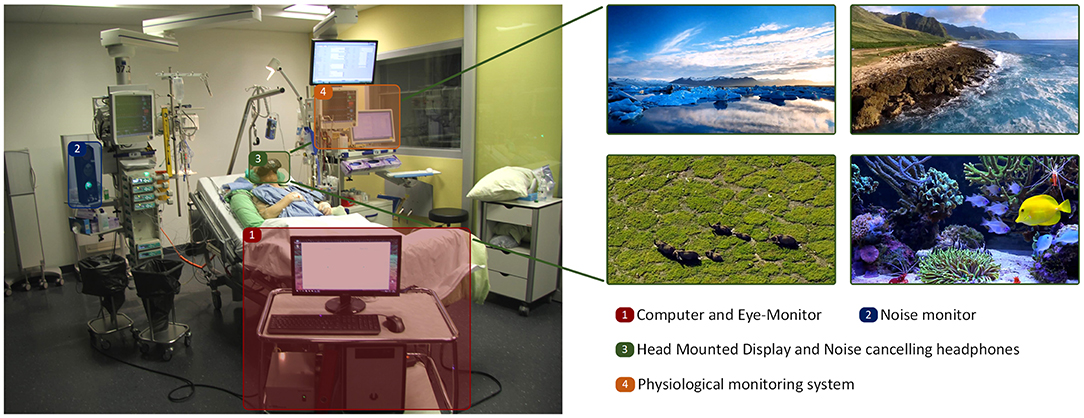
Figure 2. Patient during the stimulation in the ICU session, including setup and stimulation examples.
Acceptance, Discomfort, and Recollection
Questionnaire findings (range zero to four, Figure 3) revealed that the VR stimulation was well accepted, easy to use and appreciated by patients, as shown in the scores for high usability 3.57 (95% CI 3.3 to Inf., t(29) = 10.78, p < 0.001), immersion 2.70 (95% CI 2.3 to Inf., t(29) = 3.34, p < 0.001), and satisfaction 3.13 (95% CI 2.8 to Inf., t(29) = 5.32, p < 0.001). Symptoms of discomfort during stimulation, such as disorientation 0.03 (95% CI -Inf. to 0.09, t(29) = −59.00, p < 0.001), oculomotor problems 0.15 (95% CI -Inf. to 0.24, t(29) = −34.00, p < 0.001), and nausea 0.04 (95% CI -Inf. to 0.04, t(29) = −72.46, p < 0.001) were rated low on the score scale.
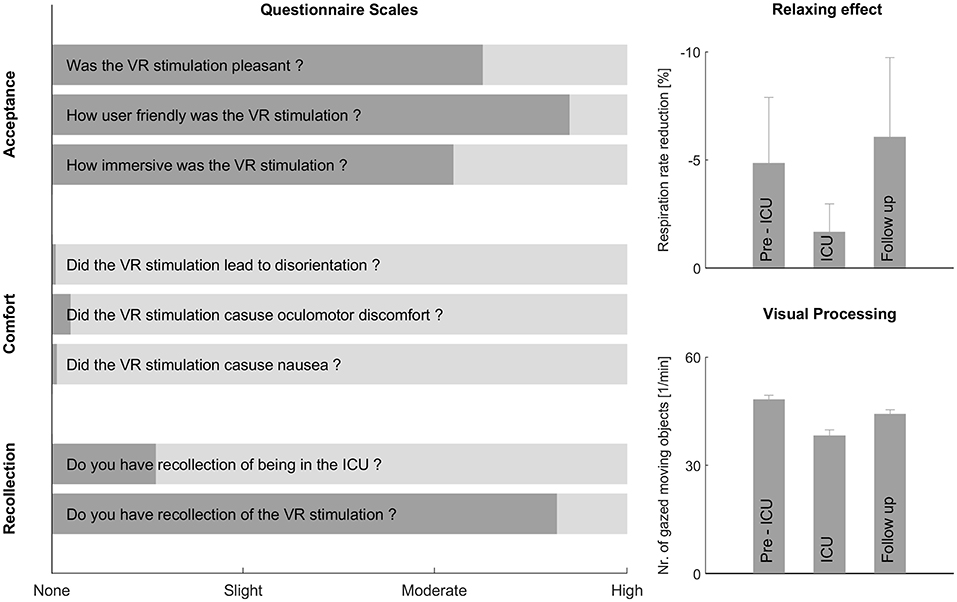
Figure 3. The questionnaire scales on the left show the perception of the virtual reality (VR) stimulation by critically ill patients during their Intensive Care Unit (ICU) stay. The relaxing effect and visual processing are shown on the right. Acceptance, discomfort and recollection were assessed in the follow-up session, whereas visual processing and the relaxing effect were measured in all three sessions. Overall, the new method was well accepted, did not trigger any discomfort, produced a decreasing respiratory rate during stimulation, and the patients were able to process the stimulation.
Based on results of the ICU Memory tool, 28 of the 33 patients (84.8%) were able to recollect the content of the stimulation (e.g., elephant, yellow fish, ocean, dolphin, polar bear, and mountains), 23 patients had a weak recollection of their stay in ICU, and 10 patients (30.3%) had a clear recollection of the whole stay in ICU. Moreover, during the VR stimulation no noise >50 dB or adverse events were registered.
Eye Movements
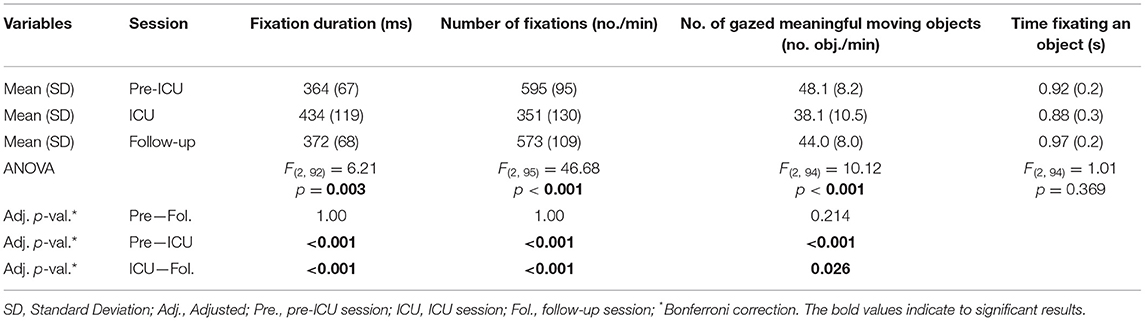
Visual fixation duration was significantly higher during the ICU session compared to the pre-ICU (p < 0.001) and follow-up sessions (p < 0.001), as seen in Table 3. The number of fixations were significantly lower during the ICU session compared to pre-ICU (p < 0.001) and follow-up sessions (p < 0.001), whereas no significant difference was found between the pre-ICU and follow-up sessions. The number of gazed meaningful moving objects per minute (Figure 3) was significantly lower in the ICU session compared to the pre-ICU (p < 0.001) and follow-up sessions (p = 0.026), whereas the time fixated on one meaningful moving object did not show any significant difference. Analysis showed that the change in visual fixation duration over time within a session was not significant in any of the three sessions and remained constant.
Physiological Parameters
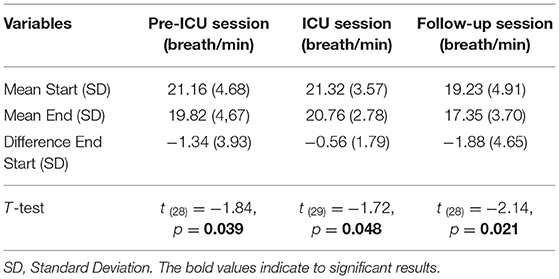
Compared to the initial measurement at the beginning of the stimulation (first 15 s) and the last 15 s of the stimulation, the respiratory rate decreased significantly in all three sessions (Figure 3 and Table 4). The significant reduction in respiratory rate by using a directed hypothesis was −1.34 breath/min in the pre-ICU session, −0.56 breath/min in the ICU session and −1.88 breath/min in the follow-up session. Analysis of variance demonstrated no significant differences between the three sessions [F(2, 84) = 0.97, p = 0.384]. No significant reduction or differences were observed during the three sessions in heart rate [F(2, 86) = 0.49, p = 0.615] and blood pressure [F(2, 77) = 0.22, p < 0.803]. Furthermore, the medication did not have any influence on the analysis.
Health-Related Quality of Life and Cognitive Functions
The health-related quality of life between the pre-ICU (M = 78.00, SD = 13.27) and follow-up sessions (M = 85.24, SD = 9.52) increased significantly by 7.03 (95% CI 1.26–12.81, t(31) = 2.48, p < 0.019). No significant differences were found in cognitive functions between the pre-ICU (M = 27.52, SD = 2.01) and follow-up sessions (M = 27.56, SD = 2.02).
Discussion
Primary Results
Consistent with our first hypothesis, our results indicate that VR stimulation was pleasant, immersive, and easy to use. Furthermore, VR stimulation did not promote discomfort. Secondly, critically ill patients were able to perceive and process VR stimulation in the ICU session, whereas on a lower level compared to the pre-ICU and follow-up sessions. Thirdly, VR stimulation decreased the respiratory rate, which can be interpreted as a sign of relaxation, produced by isolating and protecting critically ill patients from the noisy and stressful environment.
Acceptance, Comfort, and Recollection
Firstly, VR stimulation was highly appreciated and accepted by critically ill patients as reflected in high usability and satisfaction scores close to the maximum of the respective scales. Immersion was also highly scored, thus indicating that patients forgot about their actual surroundings. This may underline the fact that sensory overload and deprivation (stress and noise of the ICU environment) can be reduced during VR stimulation.
Furthermore, VR stimulation did not evoke any negative reactions, but provided patients with a confident, secure, fascinating and familiar environment. Almost 85% of all critically ill patients had clear memories of the VR stimulation during the ICU stay, as indicated by remembered content. However, only one third of the patients had clear memories of their stay in the ICU. The low recollection of the ICU stay was potentially caused by the psychological phenomenon of fading affect bias, which causes memories of negative events like the ICU stay to fade faster than the pleasant VR stimulation (34–36). These results and the low withdrawal rate of four patients further confirms that VR stimulation was highly appreciated, captured patients' attention and distracted them from the stressful and noisy ICU.
Eye Movements
Visual fixation duration was significantly higher in the ICU session compared to pre-ICU and follow-up sessions. In contrast, the number of fixations was significantly lower in the ICU session, indicating that patients needed more time to process the information and had less visual exploration. This means that patients were experiencing post-surgery fatigue (i.e., reduced level of attention), potentially caused by medication (e.g., analgesics to reduce pain) and sleep-deprivation. Visual fixation duration and the number of fixations in the pre- and follow-up session were in line with VR stimulation in healthy volunteers (18) and findings when viewing dynamic natural scenes on a screen (37).
Additionally, post-surgery fatigue was also reflected in the number of gazed meaningful moving objects inside the video, which was significantly lower in the ICU session, but still at a high level of almost 40 objects a minute. It is noteworthy that there were no significant differences between the times fixating meaningful objects, confirming the second finding that patients were able to perceive, process, and follow the objects during all three sessions, although to a lesser extent during the ICU session. In line with the Attention Restoration Theory, the results suggest that critically ill patients are able to recover and restore attentional fatigue during VR nature stimulation by fostering low-effort attention (38, 39).
Physiological Parameters
The third main finding was that the respiratory rate decreased significantly during all three sessions, whereas heart rate and blood pressure were not significantly influenced by the stimulation. Consistent with the Stress Recovery Theory, the VR stimulation had a relaxing effect on the parasympathetic nervous system. The decrease in respiratory rate during stimulation may indicate that nature-related VR stimulation can reduce stress and mental fatigue in critically ill patients by sealing off and protecting them from the noisy and stressful environment (14, 40).
One explanation why the significant relaxing effect was only seen in the respiratory rate was that more than 50% of all patients received medication affecting the heart rate and blood pressure, which influenced and thus stabilized and minimized the relaxing effect. Furthermore, the smaller decrease in the respiratory rate during the ICU session was probably due to medication influencing the respiratory rate, which was not administered in the pre-ICU and follow-up sessions.
Health-Related Quality of Life and Cognitive Functions
In the follow-up session, health-related quality of life was significantly higher compared to the pre-ICU session, indicating that they profited from the surgery, whereas no significant differences were found for cognitive functions. Therefore, in line with the literature, the short stay in the ICU did not have a negative effect on long-term cognitive functions (4, 5).
Limitations and Outlook
It remains unclear whether our findings can be generalized to a general population of critically ill patients. Moreover, as patients need to be awake, VR stimulation may not be suitable for critically ill patients who are unconscious and deeply sedated. In addition, it is unclear which part of the positive relaxing effect was due to the head-mounted display and which part due to the noise-canceling headphones. If the relaxing effect was due to noise reduction, VR stimulation might additionally help distract patients from their current condition and daily routine and thus has a positive effect on well-being. Therefore, the main limitations of this study design are the lack of a control group (i.e., sham intervention), the selected patient population (i.e., no patients were included in the study with prolonged ICU stay and mechanical ventilation) and the lack of repeated VR stimulation during ICU stay (i.e., long-term effects).
In this study, we showed that patients can be protected from the noisy and stressful environment. Further randomized clinical trials should investigate whether the proposed VR stimulation reduces functional and long-term cognitive impairment and improves health-related quality of life after ICU stay. Since long-term cognitive impairment is associated with delirium, studies should also focus on whether VR stimulation can potentially reduce the incidence and the duration of delirium (5). Furthermore, it remains unclear how long and how many times a day VR stimulation should be employed. We suggest including VR stimulation at least twice in the daily routine. If applicable, Electroencephalogram monitoring should be considered as a further means of measuring the effect of VR stimulation in critically ill patients.
Conclusion
Our results indicate that the newly developed VR stimulation method was well accepted, immersive and appreciated by critically ill patients, and that VR was recollected better than the rest of the ICU stay. Furthermore, VR stimulation may have had a relaxing and calming effect, was easy to use and did not evoke discomfort. Eye movement analysis indicated that critically ill patients were able to perceive and process the stimulation in all sessions. Thus, VR stimulation has the potential of becoming a new method to reduce long-term cognitive impairment and comfort critically ill patients during a stay in ICU.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Canton of Bern, Switzerland (KEK-Nr. 2016-01652). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
SG, M-MJ, UM, RM, SJ, and TN designed the study. SG developed the set-up and stimulated all critically ill patients together with M-MJ. SG and SK analyzed the data. SG, M-MJ, SK, UM, RM, SJ, and TN wrote the manuscript. All authors approved the final manuscript.
Funding
This study was conducted and funded by the Gerontechnology and Rehabilitation Research Group at ARTORG Center for biomedical engineering at the University of Bern and the Department of Intensive Care Medicine at the University Hospital Bern (Inselspital).
Conflict of Interest
M-MJ and SJ report grants from Orion Pharma, Abbott Nutrition International, B. Braun Medical AG, CSEM AG, Edwards Lifesciences Services GmbH, Kenta Biotech Ltd, Maquet Critical Care AB, Omnicare Clinical Research AG, Nestle, Pierre Fabre Pharma AG, Pfizer, Bard Medica S.A., Abbott AG, Anandic Medical Systems, Pan Gas AG Healthcare, Bracco, Hamilton Medical AG, Fresenius Kabi, Getinge Group Maquet AG, Dräger AG, Teleflex Medical GmbH, Glaxo Smith Kline, Merck Sharp and Dohme AG, Eli Lilly and Company, Baxter, Astellas, Astra Zeneca, CSL Behring, Novartis, Covidien, and Nycomed outside the submitted work. The money was paid into departmental funds. No personal financial gain applied.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank all patients for their participation in the study. Furthermore, we would like to express our gratitude to the clinical medical and nursing team in the Department of Intensive Care Medicine at the University Hospital Bern (Inselspital) for their support. Our sincere thanks also go to colleagues at the Gerontechnology and Rehabilitation Research Group at the University of Bern for their insightful comments and encouragement.
References
1. Leach J. Psychological factors in exceptional, extreme and torturous environments. Extreme Physiol Med. (2016) 5:1. doi: 10.1186/s13728-016-0048-y
2. Lindenmuth JE, Breu CS, Malooley JA. Sensory overload. Am J Nurs. (1980) 80:1456. doi: 10.2307/3462693
3. Wergin R, Modrykamien A. Cognitive impairment in ICU survivors: assessment and therapy. Clevel Clin J Med. (2012) 79:705–12. doi: 10.3949/ccjm.79a.12038
4. Wilcox ME, Brummel NE, Archer K, Ely EW, Jackson JC, Hopkins RO. Cognitive dysfunction in ICU patients: risk factors, predictors, and rehabilitation interventions. Crit Care Med. (2013) 41:S81–98. doi: 10.1097/CCM.0b013e3182a16946
5. Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. (2013) 369:1306–16. doi: 10.1056/NEJMoa1301372
6. Hopkins RO, Jackson JC. Short-and long-term cognitive outcomes in intensive care unit survivors. Clin Chest Med. (2009) 30:143–53. doi: 10.1016/j.ccm.2008.11.001
7. Timmers TK, Verhofstad MJ, Moons KM, van Beeck EF, Leenen LH. Long-term quality of life after surgical intensive care admission. Arch Surg. (2011) 146:412–8. doi: 10.1001/archsurg.2010.279
8. Hofhuis JG, Spronk PE, van Stel HF, Schrijvers GJ, Rommes JH, Bakker J. The impact of critical illness on perceived health-related quality of life during ICU treatment, hospital stay, and after hospital discharge: a long-term follow-up study. CHEST J. (2008) 133:377–85. doi: 10.1378/chest.07-1217
9. Patel MB, Morandi A, Pandharipande PP. What's new in post-ICU cognitive impairment? Intensive Care Med. (2015) 41:708–11. doi: 10.1007/s00134-014-3632-x
10. Berman MG, Jonides J, Kaplan S. The cognitive benefits of interacting with nature. Psychol Sci. (2008) 19:1207–12. doi: 10.1111/j.1467-9280.2008.02225.x
11. Gamble KR, Howard JH Jr, Howard DV. Not just scenery: viewing nature pictures improves executive attention in older adults. Exp Aging Res. (2014) 40:513–30. doi: 10.1080/0361073X.2014.956618
12. Kaplan S. The restorative benefits of nature: toward an integrative framework. J Env Psychol. (1995) 15:169–82. doi: 10.1016/0272-4944(95)90001-2
13. Berto R. The role of nature in coping with psycho-physiological stress: a literature review on restorativeness. Behav Sci. (2014) 4:394–409. doi: 10.3390/bs4040394
14. Ulrich RS, Simons RF, Losito BD, Fiorito E, Miles MA, Zelson M. Stress recovery during exposure to natural and urban environments. J Env Psychol. (1991) 11:201–30. doi: 10.1016/S0272-4944(05)80184-7
15. Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med. (2013) 41:1543–54. doi: 10.1097/CCM.0b013e31827ca637
16. Brummel NE, Jackson JC, Girard TD, Pandharipande PP, Schiro E, Work B, et al. A combined early cognitive and physical rehabilitation program for people who are critically ill: the activity and cognitive therapy in the intensive care unit (ACT-ICU) trial. Phys Ther. (2012) 92:1580–92. doi: 10.2522/ptj.20110414
17. Turon M, Fernandez-Gonzalo S, Jodar M, Gomà G, Montanya J, Hernando D, et al. Feasibility and safety of virtual-reality-based early neurocognitive stimulation in critically ill patients. Ann Intensive Care. (2017) 7:81. doi: 10.1186/s13613-017-0303-4
18. Gerber SMM, -Jeitziner M, Wyss P, Chesham A, Urwyler P, Müri RM, et al. Visuo-acoustic stimulation that helps you to relax: a virtual reality setup for patients in the intensive care unit. Sci Rep. (2017) 7:13228. doi: 10.1038/s41598-017-13153-1
19. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. (2009) 41:1149–60. doi: 10.3758/BRM.41.4.1149
20. Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. (2011) 20:1727–36. doi: 10.1007/s11136-011-9903-x
21. Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. (2005) 53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x
22. Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. (2001) 286:2703–10. doi: 10.1001/jama.286.21.2703
23. Mirra SS, Heyman A, McKeel D, Sumi S, Crain BJ, Brownlee L, et al. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD): PART II. Standardization of the neuropathologic assessment of Alzheimer's disease. Neurology. (1991) 41:479–9. doi: 10.1212/WNL.41.4.479
24. McLennan SN, Mathias J, Brennan L, Stewart S. Validity of the Montreal Cognitive Assessment (MoCA) as a screening test for mild cognitive impairment (MCI) in a cardiovascular population. J Geriatr Psychiatry Neurol. (2011) 24:33–8. doi: 10.1177/0891988710390813
25. Schubert T, Friedmann F, Regenbrecht H. Embodied Presence in Virtual Environments. Visual Representations and Interpretations. Liverpool: Springer (1999). p. 269–78.
26. Brooke J. SUS-A Quick and Dirty Usability Scale, Usability Evaluation in Industry. Reading: Redhatch Consulting Ltd. (1996). p. 4–7.
27. Kennedy RS, Lane NE, Berbaum KS, Lilienthal MG. Simulator sickness questionnaire: an enhanced method for quantifying simulator sickness. Int J Aviat Psychol. (1993) 3:203–20. doi: 10.1207/s15327108ijap0303_3
28. Jones C, Griffiths RD, Humphris G, Skirrow PM. Memory, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Crit Care Med. (2001) 29:573–80. doi: 10.1097/00003246-200103000-00019
29. Bulling A, Ward JA, Gellersen H, Troster G. Eye movement analysis for activity recognition using electrooculography. IEEE Trans Pattern Anal Mach Intell. (2011) 33:741–53. doi: 10.1109/TPAMI.2010.86
30. R Development Core Team. A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing (2018).
32. Teasdale G, Jennett B Assessment of coma and impaired consciousness: a practical scale. Lancet. (1974) 304:81–4. doi: 10.1016/S0140-6736(74)91639-0
33. Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA. (2003) 289:2983–91. doi: 10.1001/jama.289.22.2983
34. Walker WR, Skowronski JJ, Thompson CP. Life is pleasant–and memory helps to keep it that way! Rev Gen Psychol. (2003) 7:203. doi: 10.1037/1089-2680.7.2.203
35. Ritchie TD, Skowronski JJ, Cadogan S, Sedikides C. Affective responses to self-defining autobiographical events. Self Identity. (2014) 13:513–34. doi: 10.1080/15298868.2013.863222
36. Gibbons JA, Lee SA, Walker WR. The fading affect bias begins within 12 hours and persists for 3 months. Appl Cogn Psychol. (2011) 25:663–72. doi: 10.1002/acp.1738
37. Dorr M, Martinetz T, Gegenfurtner KR, Barth E. Variability of eye movements when viewing dynamic natural scenes. J Vis. (2010) 10:28. doi: 10.1167/10.10.28
38. Berto R, Massaccesi S, Pasini M. Do eye movements measured across high and low fascination photographs differ? Addressing Kaplan's fascination hypothesis. J Env Psychol. (2008) 28:185–91. doi: 10.1016/j.jenvp.2007.11.004
39. Ohly H, White MP, Wheeler BW, Bethel A, Ukoumunne OC, Nikolaou V, et al. Attention restoration theory: a systematic review of the attention restoration potential of exposure to natural environments. J Toxicol Env Health Part B. (2016) 19:305–43. doi: 10.1080/10937404.2016.1196155
Keywords: virtual reality, critical illness, intensive care unit, cognitive dysfunction, nature, stimulation
Citation: Gerber SM, Jeitziner M-M, Knobel SEJ, Mosimann UP, Müri RM, Jakob SM and Nef T (2019) Perception and Performance on a Virtual Reality Cognitive Stimulation for Use in the Intensive Care Unit: A Non-randomized Trial in Critically Ill Patients. Front. Med. 6:287. doi: 10.3389/fmed.2019.00287
Received: 22 July 2019; Accepted: 22 November 2019;
Published: 10 December 2019.
Edited by:
Zhongheng Zhang, Zhejiang University, ChinaReviewed by:
Longxiang Su, Peking Union Medical College Hospital (CAMS), ChinaJesus Rico-Feijoo, Hospital Universitario Río Hortega, Spain
Evgenia V. Fot, Northern State Medical University, Russia
Marina Soro, Hospital Clínic Universitari de València, Spain
Copyright © 2019 Gerber, Jeitziner, Knobel, Mosimann, Müri, Jakob and Nef. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tobias Nef, tobias.nef@artorg.unibe.ch
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
 Stephan M. Gerber
Stephan M. Gerber Marie-Madlen Jeitziner2†
Marie-Madlen Jeitziner2†  Samuel E. J. Knobel
Samuel E. J. Knobel René M. Müri
René M. Müri Tobias Nef
Tobias Nef