European Union Regulation on clinical trials and Regulation on medical devices: A common soil for future development
- 1Department of Experimental Medicine, University of Rome Tor Vergata, Rome, Italy
- 2Department of Neuroscience, Psychology, Drug Research and Child Health, NEUROFARBA—Section of Pharmacology and Toxicology, University of Florence, Florence, Italy
The recent European Union (EU) Regulations on clinical trial on medicinal products (MPs) (2014/536) and on medical devices (MD) (2017/745) represent potential improvement for the European health system and may offer advantages to the citizens. As Regulations, they are immediately applicable in Member States overruling national laws, being an advantage for stakeholders (e.g. sponsors and investigators) and Europe becomes de facto one homogeneous place for research and development of medicines and medical devices. This perspective commentary focuses on the most relevant methodological and regulatory aspects of the recent Regulation on clinical trials for drug development and how it may indirectly impact on substance-based medical devices (SBMD). The article highlights the innovations associated with the 2017/745 Regulation, especially to the area of SBMD, which represent a novelty among MDs. Since SBMDs share some aspects of medicines, they will increasingly undergo research in the future related to the performance and safety claims, via post-marketing surveillance. Importantly, SBMD’s Consumers are rapidly increasing due to their usage to treat some common symptoms, which not necessarily need conventional medicines. “Frontiers in Drug Safety and Regulation” created a section to reflect this rapidly-changing scenario and host reports on SBMD in a scientific environment. This initiative is also a reflection of the recent regulation on SBMDs. Thus, the improvement of clinical research through the new EU Regulation on clinical trials may become useful also to the new requirements for SBMD. A novel editorial initiative will further contribute to implement the EU Regulation providing adequate scientific dissemination.
Introduction
The European Union (EU) Regulation 2014/536 on clinical trial on Medicinal Products (MPs) for human use (European Commission, 2014) and the EU Regulation 2017/745 on Medical Devices (MDs) (Eur-lex, 2018) represent two very important novel improvements for the European health system and for all European citizens under many aspects.
First they are both Regulations and not Directives: a “Regulation” is a binding legislative act, that is immediately and fully applicable in all Member States overruling the national laws. On the contrary, a “Directive” is a legislative act setting objectives that all EU countries must reach and implement into their national legislation within a defined timeframe (European Union, 2022). Thus, the Regulations represent the fastest way to modify the legislation in all European countries, representing a big advantage for all the stakeholders (sponsors, and clinical investigators for the clinical trials Regulation; manufacturers, Notified Bodies, and all the other actors for the medical device Regulation). Consequently, they will operate under the same rules in all the EU nations, making de facto Europe a big and homogeneous country for clinical research in the field of MPs and for the whole sector of MDs including research and development.
Such a condition will likely turn into a relevant advantage also for the EU citizens, who will benefit of new and effective treatments that will be likely available in a faster way.
The objective of this perspective commentary is double: 1) To focus on the most relevant methodological and regulatory aspects of the Regulation on clinical trials on medicinal products (MPs) in the EU and how it may indirectly impact on the sector of Substance-Based Medical Devices (SBMDs) and 2) To highlight the innovations that the EU Regulation 2017/745 could specifically bring to the field of SBMDs.
The possible advantages that can be expected for the health of the individual citizen, either as consumer of SBMDs or as patient will be briefly summarized.
The emerging and relevant problem associated with the pollution caused by pharmaceuticals, given that the emissions of substances used for therapeutic purposes into the environment occur during their whole lifecycle, i.e., from production through consumption to disposal (European Commission, 2013; COM, 2019), will not be discussed in this paper even if a positive impact of MDs that are based on natural substances could be expected.
The European Union Regulation on clinical trials: Methodological and regulatory aspects
The EU Regulation 2014/536 on Clinical Trials on medicinal products for human use has entered into application on 31 January 2022. A work plan has been recently released (EMA, 2022) to complete its implementation.
There are many reasons for developing this Regulation in the EU. Certainly, a major driver was to make EU attractive and favorable for performing large interventional trials with high standards of public transparency and safety for their participants. In other words, Europe has been trying to set the stage to be competitive and attractive to host large, homogeneous and innovative clinical research and development as a whole country, as opposed to nations as China or Brazil for example, which due to their population size represent major competitors.
Leading quality in clinical research is central to the proper growth of the health system as a whole, and it is a driver for the economic development of each EU country. Thus, by supporting and regulating the conduct of large clinical trials in all EU member States, Europe aims at attracting large investments. At the same time, promoting medical innovation would benefit all patients by increasing the number of new and innovative available medicines.
Randomized clinical trials (RCTs), possibly based on a hypothesis of superiority, are indeed necessary and required to generate the highest quality of the evidence regarding the efficacy and safety of all healthcare interventions. Both the Food and Drug Administration (FDA) and European Medicines Agency (EMA) rely on RCTs to reach a decision on the authorisation of new medicines. Although the use of placebo has long been debated, placebo as control in RCTs can establish the assay sensitivity, i.e., the ability to discriminate whether a treatment is really effective (Temple and Ellenberg, 2000). However, RCTs may also need to compare efficacy and safety of new treatments against existing active alternative of care proved to be effective by previous studies against placebo. Since high quality RCTs provide the best evidence for developing international guidelines worldwide, it seems important to increase the use of the best active or gold standard comparator(s), when available, for the specific disease treated in the specific RCT dealing with medicinal products (Naci et al., 2020). The new EU Regulation may endorse quality in RCTs, supporting RCTs of superiority of new treatments versus the available standard of care, rather than versus placebo.
Without doubts, patients are the fundamental partners in the generation and appraisal of relevant and trustworthy evidence from RCTs (Greenhalgh et al., 2019); their recruitment and retention during the entire RCT have become a major challenge for those running RCTs, likely because of a reduced confidence or poor awareness of patients in the cornerstone value of clinical research. Thus improving the quality of RCTs may help increasing patient’s participation. In fact, the Regulation 2014/536 clearly states that in a clinical trial the rights, safety, dignity and wellbeing of subjects should be protected and the data generated should be unbiased, reliable and robust. The interests of the subjects should always be the main priority overcoming all other interests.
The COVID-19 pandemic has made this issue even more important and other ways to run RCTs have been suggested such as Decentralized (Goodson et al., 2022) or in silico (Pappalardo et al., 2019) RCTs.
A major aim of the Regulation is to foster innovation capacity of the European medical research, at the same time protecting public health and recognizing the legitimate economic interests of the sponsors. Thus, it clearly appears that a significant advantage of the clinical trial Regulation is for the patients who would prefer to be recruited in relevant RCTs and for the citizens at large who could benefit of new, safe and more effective medicines. This may contribute to ameliorate the health system due to a better investment of public and private resources.
The new Regulation on clinical trials on medicinal products for human use will likely positively impact on the clinical investigations involving medical devices and particularly those on medical devices based on substances as described below. Better conduct of clinical trials for MPs will be a reference quality in supporting the research for the claims of performance of many SBMDs used in common functional symptoms. In fact the Regulation on MDs has taken up many aspects of the regulatory framework on pharmaceuticals in relation, for example, to ethical aspects and to the quality of studies.
The European Regulation on medical devices: Focus on substance-based medical devices
The definition of Medicinal Product (MP) and of Medical Device (MD) is reported in one of the other three Perspective Articles that have been invited and published for the Research Topic: Medical Devices made of substances for human health: a challenge in terms of efficacy, safety and sustainability (Leone, 2022).
Basically, Medical Devices are products or equipment intended for a medical purpose. If they are composed of substances or combination of substances, they are defined as substance-based medical devices (SBMD).
The EU Regulation 2017/745 (Eur-lex, 2018) on medical devices (MDR) has introduced several relevant novelties, reducing the gap of information necessary at the time of their CE mark in comparison with the data requested for the marketing authorization of pharmaceuticals. It also requires to promote post-marketing clinical follow up studies in order to increase availability of data supporting their performance and safety. Overall MDR increases the clinical informations necessary to obtain the CE mark from the Notified Bodies and promotes post-marketing studies to confirm the positive benefit-risk balance over time during marketing.
By introducing a new international Unique Device Identification (UDI) system and a publicly accessible European database (EUDAMED), traceability and transparency of MDs will be likely increased (Antich-Isern et al., 2021). The MDR mirrors the regulatory scenario of medicinal products for some relevant aspects, such as the continuous evaluation process of the post-marketing benefit-risk profile. The pre- and post-marketing clinical research of MDs will certainly indirectly benefit from the Regulation on clinical trials of medicinal products in terms of quality of the studies and comparative approach. An increase in studies versus active-comparator rather than versus placebo can be foreseen.
This is particularly true for the sector of SBMDs, whose existence is formally acknowledged by MDR (rule 21).
At a first glance of the MDR, SBMD may appear handled similarly to medicinal products (MPs) since their claim is to have a therapeutic effect and the formulations are similar to those of MPs. In particular, the definition of risk class III SBMD as reported in the Rule 21 first and second indents of the Regulation (EU) (Eur-lex, 2018), states that the intended use of MDs is very similar to MPs (Leone, 2022):
Devices that are composed of substances or of combinations of substances that are intended to be introduced into the human body via a body orifice or applied to the skin and that are absorbed by or locally dispersed in the human body are classified as:
1) class III if they, or their products of metabolism, are systemically absorbed by the human body in order to achieve the intended purpose;
2) class III if they achieve their intended purpose in the stomach or lower gastrointestinal tract and they, or their products of metabolism, are systemically absorbed by the human body.
As recently reviewed (Fimognari et al., 2022; Leone, 2022), MPs and SBMDs however differ in their mechanism of action: MPs have a demonstrated pharmacological mechanism of action while SBMDs must have “any mechanism, that is, not pharmacological”. The definition of a “non pharmacological” mechanism of action for a therapeutic product represents a big challenge for preclinical and clinical research.
Moreover the reference to Annex I of Directive 2001/83/EEC increased the level of preclinical and clinical data for SBMD as reported in the MDR: Devices that are composed of substances or of combinations of substances that are intended to be introduced into the human body, and that are absorbed by or locally dispersed in the human body shall comply, where applicable and in a manner limited to the aspects not covered by this Regulation, with the relevant requirements laid down in Annex I to Directive 2001/83/EC for the evaluation of absorption, distribution, metabolism, excretion, local tolerance, toxicity, interaction with other devices, medicinal products or other substances and potential for adverse reactions, as required by the applicable conformity assessment procedure under this Regulation.
It must be noted that the regulatory marketing process of MDs is different in the EU and United States as reported in Table 1, with a different role of regulatory agencies.
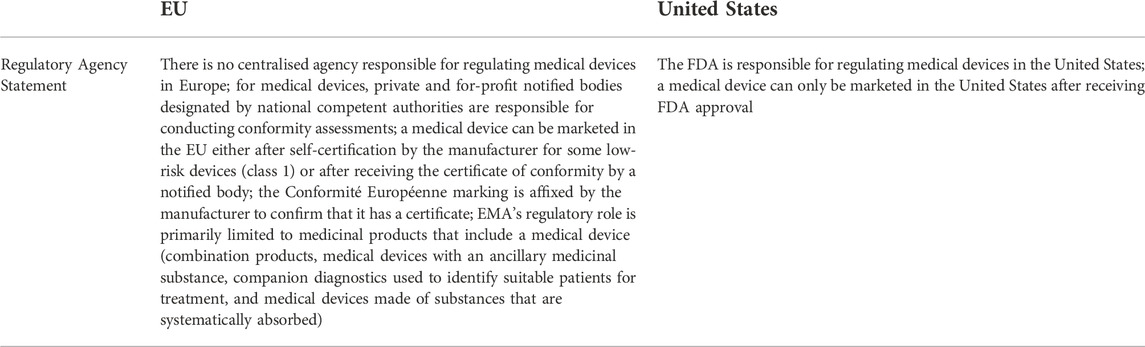
TABLE 1. Medical device regulation in the EU and in the United States (modified from Naci et al., 2020).
While in the United States a MD can be marketed only after FDA approval, in the EU the situation is more complex.
EMA opinion, which is not binding, is requested only for class III SBMDs reported in the first indent of Rule 21, i.e., those that are systemically absorbed by the human body in order to exert a therapeutic effect (or in order to achieve the intended purpose as reported in Rule 21). A proper implementation of the MDR will require harmonization and collaboration of competent authorities. For more details see Leone, 2022.
The market of SBMDs is increasing in the recent years, currently representing 10% of the total self-medication market in the European countries (Giovagnoni, 2022). With the full implementation of the MDR (Eur-lex, 2018), an increase in preclinical and clinical studies will likely occur. SBMDs largely address medical needs such as common diseases where the pharmacological treatment could be safely and effectively replaced by a SBMD. For example, in the pediatric population, a SBMD made of natural fiber complexes was shown to significantly reduce Body Mass Index, body fat, and waist circumference and to be non-inferior to metformin for glycaemic control and superior in terms of both serum lipid lowering capacity and tolerability (Guarino et al., 2022; Stagi, 2022). Thus it will necessary to produce comparative evidence of SBMDs versus the MPs used in a specific clinical setting. The comparative evidence should come from studies performed before and after CE mark. Comparative research could represent the best way to increase the public trust in clinical research and to pave the way to a more personalized medicine (Singh et al., 2020).
Conclusion
The Regulations concerning clinical research of MPs and the more general regulatory framework of MDs, and in particular SBMDs, in the EU have recently undergone parallel major revisions, in the interest of the wellbeing of the citizens, of the quality of science, and of improving feasibility and homogeneity among nations.
In particular, SBMDs which share several aspects with MPs, will increasingly undergo processes of research and development in the near future, regarding the claims of “effectiveness” and the post-marketing surveillance for safety. Both assessment of effectiveness and safety of SBMD can use the guidance developed for MD or drugs by Regulations on clinical trial on MPs (2014/536) and on MD (2017/745). Importantly, the market of class III SBMDs is undergoing a fast rise, filling some gaps and unmet medical needs in the treatment of common symptoms which not necessarily need pharmacological agents.
For all the above reasons, the section on SBMDs as a separate part of the Journal “Frontiers in Drug Safety and Regulation” has been created to reflect these rapidly changing developments and to host reports and debates on SBMDs in a scientific, high quality editorial environment. This initiative also reflects the spirit of the recent regulation on SBMDs that requires to continuously provide evidence of their safety, and to strengthen their claims of “effectiveness” with a methodologically rigorous and scientific approach. This novel editorial initiative will further contribute to implement the EU regulation at the level of the scientific dissemination.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Antich-Isern, P., Caro-Barri, J., and Aparicio-Blanco, J. (2021). The combination of medical devices and medicinal products revisited from the new European legal framework. Int. J. Pharm. 607, 120992. doi:10.1016/j.ijpharm.2021.120992
COM (2019). 128 final - approche stratégique de l’Union européenne concernant les produits pharmaceutiques dans l’environnement
EMA (2022). EU multi annual workplan. Available at: https://www.ema.europa.eu/en/documents/other/act-eu-multi-annual-workplan-2022-2026_en.pdf.
Eur-lex (2018). Regulation on medical devices. Available at: https://eur-lex.europa.eu/legal content/EN/TXT/PDF/?uri=CELEX:32017R0745.
European Commission (2013). Pharmaceuticals and the environment. Available at: https://health.ec.europa.eu/medicinal-products/pharmaceuticals-and-environment_it.
European Commission (2014). The clinical trial regulation. Available at: https://health.ec.europa.eu/medicinal-products/clinical-trials/clinical-trials-regulation-eu-no-5362014_en.
European Union (2022). Types of legislation. Available at: https://european-union.europa.eu/institutions-law-budget/law/types-legislation_en.
Fimognari, C., Barrajón-Catalán, E., Luceri, C., Turrini, E., Raschi, E., and Bigagli, E. (2022). New regulation on medical devices made of substances: opportunities and challenges for pharmacological and toxicological research. Front. Drug Saf. Regul. 2. doi:10.3389/fdsfr.2022.1001614
Giovagnoni, E. (2022). Substance-based medical devices made of natural substances: an opportunity for therapeutic innovation. Front. Drug Saf. Regul. 2. doi:10.3389/fdsfr.2022.998114
Goodson, N., Wicks, P., Morgan, J., Hashem, L., Callinan, S., and Reites, J. (2022). Opportunities and counterintuitive challenges for decentralized clinical trials to broaden participant inclusion. NPJ Digit. Med. 5, 58. doi:10.1038/s41746-022-00603-y
Greenhalgh, T., Hinton, L., Finlay, T., Macfarlane, A., Fahy, N., Clyde, B., et al. (2019). Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot. Health Expect. 22, 785–801. doi:10.1111/hex.12888
Guarino, G., Strollo, F., Malfertheiner, P., Della Corte, T., Stagi, S., Masarone, M., et al. (2022). Efficacy and safety of a polysaccharide-based natural substance complex in the treatment of obesity and other metabolic syndrome components: a systematic review. Front. Drug Saf. Regul. 2, 844256. doi:10.3389/fdsfr.2022.844256
Leone, M. G. (2022). Medical devices made of substances: a new challenge. Front. Drug Saf. Regul. 2, 9520. doi:10.3389/fdsfr.2022.952013
Naci, H., Salcher-Konrad, M., Kesselheim, A. S., Wieseler, B., Rochaix, L., Redberg, R. F., et al. (2020). Generating comparative evidence on new drugs and devices before approval. Lancet 395, 986–997. doi:10.1016/S0140-6736(19)33178-2
Pappalardo, F., Russo, G., Musuamba Tshinanu, F., and Viceconti, M. (2019). In silico clinical trials: concepts and early adoptions. Brief. Bioinform. 20 (5), 1699–1708. doi:10.1093/bib/bby043
Singh, I., Naci, H., Miller, J., Caplan, A., and Cipriani, A. (2020). Ethical implications of poor comparative effectiveness evidence: obligations in industry-research partnerships. Lancet 395, 926–928. doi:10.1016/S0140-6736(20)30413-X
Stagi, S. (2022). Medical devices made of substances: the need for a change in approach in paediatrics. Front. Drug Saf. Regul. 2, 867143. doi:10.3389/fdsfr.2022.867143
Keywords: medical device, medicinal product, European Union Regulation, safety, performance, clinical trial, substance-based medical device
Citation: Rasi G and Mugelli A (2022) European Union Regulation on clinical trials and Regulation on medical devices: A common soil for future development. Front. Drug. Saf. Regul. 2:1071620. doi: 10.3389/fdsfr.2022.1071620
Received: 16 October 2022; Accepted: 24 November 2022;
Published: 07 December 2022.
Edited by:
Simon Ulrich Jaeger, University Hospital Tuebingen, GermanyReviewed by:
Hendrik Napierala, Institute of General Practice, GermanyMatthias Schwab, Dr. Margarete Fischer-Bosch Institut für Klinische Pharmakologie (IKP), Germany
Copyright © 2022 Rasi and Mugelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessandro Mugelli, alessandro.mugelli@unifi.it
 Guido Rasi
Guido Rasi Alessandro Mugelli
Alessandro Mugelli