Transcatheter closure of a ruptured sinus of valsalva: a systematic review of the literature
- Cardiology Department, Tehran Heart Center, Tehran University of Medical Sciences, Tehran, Iran
Background: Ruptured sinus of Valsalva (RSOV) is a rare pathology, and current data regarding its symptoms, anatomy, associated pathologies, and appropriate therapeutic approaches are scarce. Transcatheter closure (TCC) has been performed in multiple cases; however, the information on its success rate and complications is limited.
Methods: Two independent reviewers performed an advanced search based on inclusion criteria on Scopus, PubMed, and Embase from January 1985 through July 2022. The main search terms were “Sinus of Valsalva”, “Rupture/Aneurysm”, and “Transcatheter/Catheter/Device”.
Results: Totally, 1,017 relevant articles from the 3 databases were retrieved. After the final review and appraisal, 94 articles describing 407 patients who underwent the TCC of RSOV were included. Males comprised 65% of the studied patients, and the average age was 34.5 years. The total success rate of TCC was 95.6%. Forty-nine patients (12%) developed complications, the most significant of which were sustained residual shunts in 7 patients (1.7%), substantial new onset or progression of aortic insufficiency in 6 (1.5%), and RSOV recurrence in 6 (1.5%). Post-interventional mortality was reported in only 2 patients (0.5%).
Conclusions: The present study is the first systematic review of available data regarding the TCC of RSOV principally comprising case series and case reports. Although TCC seems a good option, precise patient selection is mandatory.
Introduction
Sinus of Valsalva aneurysm (SOVA) is an uncommon heart defect with an estimated prevalence of 0.2%–0.9% in cardiac surgery patients (1). SOVA can be divided into congenital and acquired categories based on its etiology. Congenital SOVA, which is more prevalent in male Asians (2), arises from the aberrant development of the bulbus cordis (3). Accompanying anomalies, such as ventricular septal defect, aortic insufficiency, and bicuspid aortic valve, are also frequently detected in congenital SOVA. Acquired SOVA can be associated with previous surgeries, atherosclerosis, endocarditis, syphilis, and other injuries (3, 4).
High-pressure flow in the proximal aorta, accompanied by the congenital or acquired weakness of the aortic wall, can form SOVA. The aneurysmal sinus can then rupture into an adjacent heart chamber, creating ruptured sinus of Valsalva (RSOV). The right, left, and non-coronary sinuses are, respectively, adjacent to the interventricular septum, the left ventricular free wall, and the interatrial septum (5). These proximities can explain the detection of each rupture root based on the SOVA origin.
SOVA predominantly occurs in the right coronary sinus (70%). SOVA usually remains asymptomatic prior to a rupture into adjacent structures. The rupture results in communication between the aorta and a heart chamber, leading to progressive heart failure (6). If left untreated, patients with RSOV have poor prognoses and high mortality rates, necessitating prompt interventions to close the ruptured fistula (7, 8).
The standard treatment for RSOV has been surgical repair. Nonetheless, increasing evidence suggests that the transcatheter closure (TCC) of RSOV is a viable, less invasive alternative (9). Studies regarding the TCC of RSOV are limited to case reports and case series, and large-scale clinical trials have yet to be performed (6). Conducting a systematic review of the existing evidence on the TCC of RSOV is crucial to attaining a comprehensive understanding of this treatment, and it should encompass patient characteristics, anatomic features of the lesion, types of devices employed, and potential complications. Such knowledge can enhance patient selection and confer deeper insights into potential outcomes.
The present study is a review of the current literature on the TCC of RSOV through an assessment of a summary of all relevant case series and case reports.
Methods
Search profile
This systematic review was conducted according to the latest Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (10). On July 12, 2022, we performed a broad systematic search in the Scopus, PubMed, and Embase electronic databases. The main search terms were “Sinus of Valsalva”, “Rupture/Aneurysm”, and “Transcatheter/Catheter/Device”. The search syntax of each database is reported in Supplementary Table S1. Our search was limited to articles in the English language. All clinical studies, composed of original articles, case series, case reports, and letters to the editor, were retrieved. Additionally, references were searched for further related studies.
Study selection
The investigations selected were clinical studies on pediatric or adult patients with RSOV or SOVA and case reports or case series with TCC as the treatment strategy.
The investigations excluded were animal studies, review articles, commentaries, editorials, and conference articles. Also excluded were studies with overlapping patients. (Newer investigations with more patients were included in this case, and previous studies were excluded.) Additionally, studies where the intervention attempt was unsuccessful in the cath lab resulting in referral for surgery and investigations where RSOV was caused by previous interventions or endocarditis were excluded.
Data collection
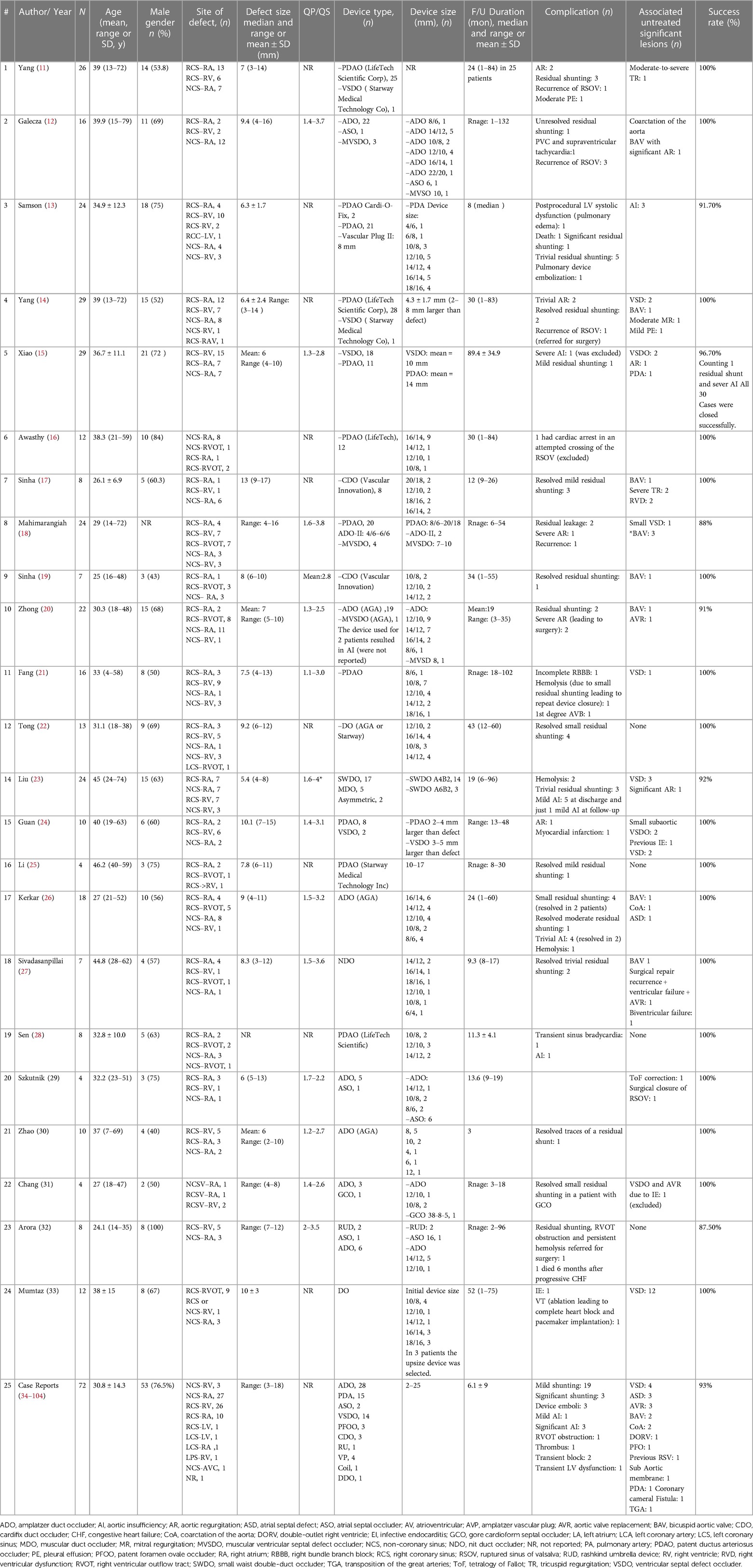
The search results were screened based on the relevance of their abstracts and titles. The full text of the selected studies was obtained. Two independent authors (AA and NT) further assessed the included studies based on the inclusion criteria. The reviewers consulted a senior author (AH) to achieve a consensus in the event of differing opinions. The studies that seemed to report overlapping cases were excluded. The selected articles are sorted in Table 1 based on study type and year. The authors identified 15 main variables from the final articles: the name of the author, the year of publication, the type of study, the location of the study, the number of studied patients, the study population's mean age, the studied patients' gender, defect sizes and defect sites, occluder device types and sizes, follow-up durations, complications, accompanying lesions, and success rates.
Search results
A report of the search results based on the PRISMA guideline is presented in Figure 1. Our search in the 3 databases yielded 437, 273, and 307 articles from PubMed, Scopus, and Embase, respectively. The removal of duplicates left 668 articles. Another 530 studies were excluded based on our title and abstract relevance criterion. Afterward, the full texts of the remaining 138 articles were obtained, and their reference lists were searched for further related studies, leading to the addition of 2 new articles. Despite multiple attempts to contact both the author and the journal, obtaining the full text of 1 article proved impossible. Then, full-text reviews of the selected articles excluded another 46 investigations based on our inclusion criteria (Supplementary Table S2).
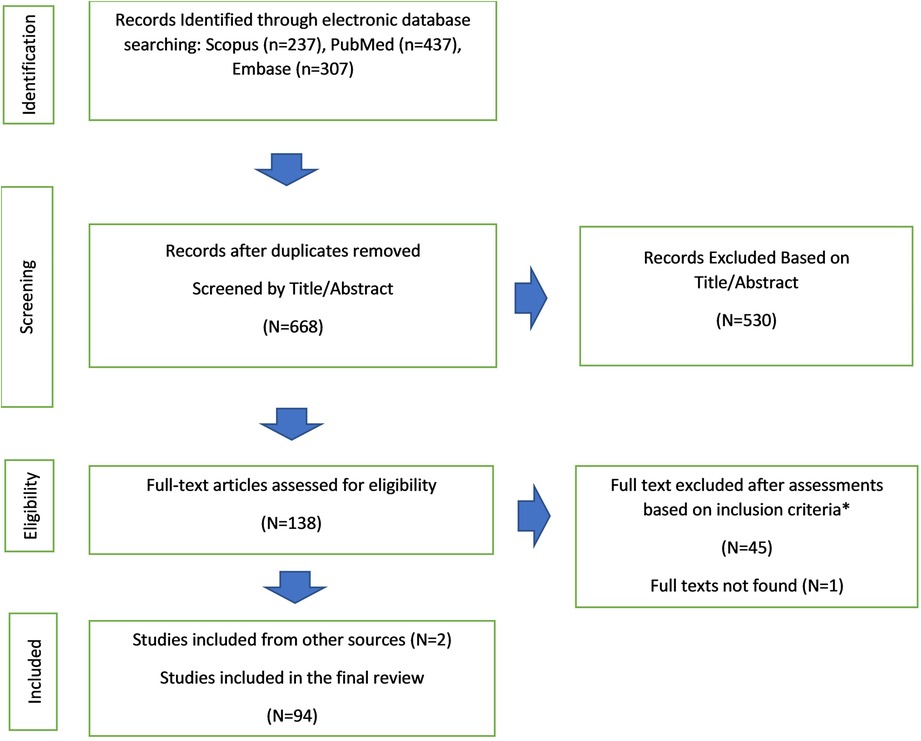
Figure 1. The image depicts the present study's systematic review PRISMA flow diagram describing database searches, title/abstracts screenings, and full-text assessments.
Ultimately, the current review was conducted on 94 articles: 23 case series and 71 case reports. The included articles are summarized in Table 1, with the case report combined in the last row. A complete list of the included case reports is available in (Supplementary Table S3).
Results
The current study reviewed 94 articles presenting 407 cases, 377 adults, and 30 pediatric patients (<18 y/o). Males accounted for about 65% of the studied patients, with an average age of 34.5 years.
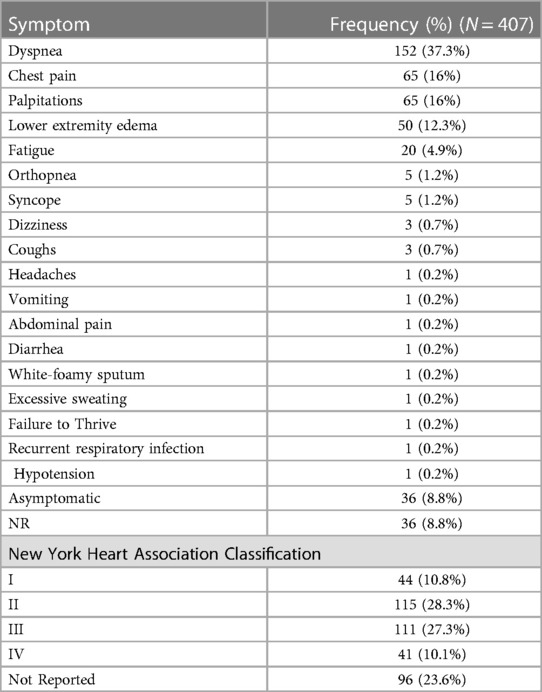
A summary of the patients' symptoms is presented in Table 2. Totally, 368 patients (90.2%) reported symptoms, the most prevalent of which were dyspnea [n = 150 (37.3%)], chest pain [n = 65 (16%)], palpitations [n = 65 (16%)], lower extremity edema [n = 50 (12.3%)], and fatigue [n = 20 (4.9%)]. Ruptures were unexpectedly discovered during imaging in 36 asymptomatic individuals (8.8%). Records of the New York Heart Association functional class were available on 311 patients: class I in 44 patients (10.8%), class II in 115 (28.3%), class III in 111 (27.3%), and class IV in 41 (10.1%).
The origin and insertion sites of the RSOV fistula are depicted in Figure 2. Most ruptures [n = 251 (61.7%)] originated from the right coronary sinus, and 152 ruptures (37.3%) originated from the non-coronary sinus. The left coronary sinus was rarely the origin [n = 4 (1.0%)]. A wide range of defect sizes was reported in the literature, from 3 mm to 17 mm (aortic opening size). The most common opening site of ruptures was the right atrium [n = 211 (51.8%)], followed by the right ventricle [n = 189 (46.4%)].
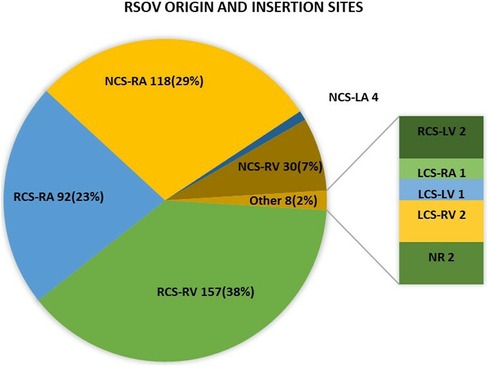
Figure 2. The image illustrates the prevalence of the origin and insertion sites of the ruptured fistula in RSOV patients who underwent TCC. RSOV, ruptured sinus of valsalva; TCC, Transcatheter closure; RCS, (right coronary sinus; LCS, left coronary sinus; NCS, non-coronary sinus; RA, right atrium; RV, right ventricle; LA, left atrium; PA, pulmonary artery; NR, not reported.
The selection criteria for TCC were reported in 256 cases. The most common criterion reported for 77% of the cases was the lack of associated cardiac anomalies (other than RSOV) requiring surgery. All the studied patients underwent the TCC of RSOV with a total success rate of 95.6%. Multiple device types were utilized for RSOV closure (Table 3). Patent ductus arteriosus (PDA) occluders were the devices most frequently utilized for the intervention [n = 172 (41.7%)], followed by the Amplatzer Ductal Occluder [n = 85 (20.6%)]. Device size was based on the size of the defect assessed by transesophageal echocardiography (TEE) or other imaging modalities.
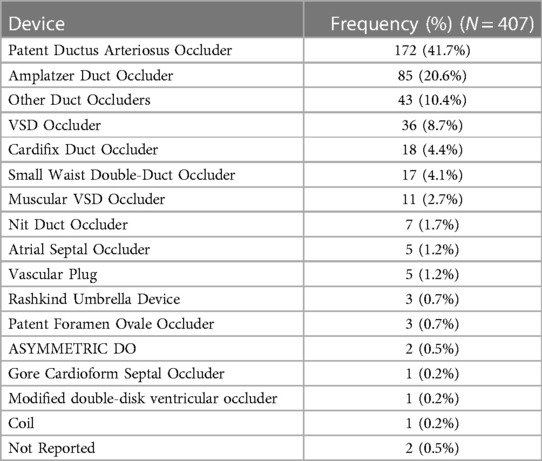
Table 3. Frequency and prevalence of device types utilized in the transcatheter closure of ruptured sinus of valsalva.
Significant complications were reported in 49 patients (12%) (Table 4). Residual shunts were reported in 61 patients (15%); still, they were resolved in most cases, with only 6 patients having significant remaining shunts. A new onset or progression of aortic insufficiency, followed by device embolization, was reported in 22 patients (5.4%); nevertheless, only 7 patients (1.7%) had moderate or severe insufficiency. Other notable complications were recurrence [n = 6 (1.5%)], hemolysis [n = 5 (1.2%)], and device embolization [n = 4 (1%)]. Post-intervention mortality was reported in only 2 patients.
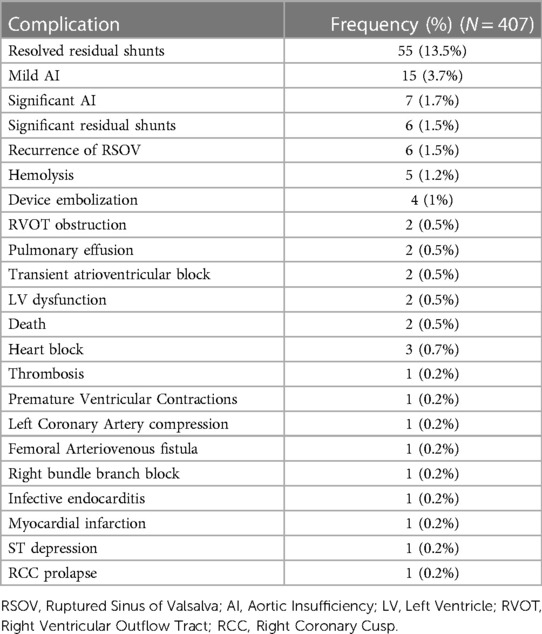
Table 4. Prevalence of reported complications in the transcatheter closure of ruptured sinus of valsalva.
Discussion
Performing the TCC of RSOV rather than surgical treatment has been dramatically favored since its introduction in 1994. However, a comprehensive guideline on the indications, patient selection, choice of imaging modalities, device selection, and complication prevention is still lacking.
Our current review of the literature on TCC yielded 407 patients undergoing the TCC of RSOV at a mean age of 34.5 years old. The most reported symptoms were dyspnea, chest pain, and palpitations. Most SOVA cases originated from the right coronary sinus, and the right atrium was the most common rupture insertion site. PDA occluders were utilized for almost one-third of the studied patients. Complications were reported in only 12% of the cases, with aortic insufficiency and residual shunting accounting for the majority of these complications.
Signs and symptoms
Patients with unruptured SOVA are often symptom-free, whereas a rupture into a heart chamber can significantly change hemodynamics and create severe symptoms (15). Dyspnea, palpitations, chest pain, fatigue, and peripheral edema are the most frequently reported symptoms after SOVA rupture. The onset of these symptoms can be acute or gradual (3, 101).
The pressure difference between the aorta and the low-pressure heart chamber causes continuous machinery murmurs, frequently heard in patients with RSOV. The murmurs become more intense when a fistula grows more prominent (102).
TCC vs. Surgical Closure
Since the first reported case of the TCC of RSOV in 1994, mounting evidence (mostly case reports and a small number of case series) has indicated the effectiveness of TCC as a potential alternative to surgical intervention. TEE proves its effectiveness during the intervention by providing live visualization of cardiac structures, especially the aortic valve. Multiple imaging modalities have made percutaneous approaches a more feasible treatment option than open-heart surgery. Still, surgical intervention is unavoidable in RSOV cases with accompanying heart defects, infections, arrhythmias, or outflow tract obstruction. Moreover, prompt surgery might become necessary when TCC results in major complications, such as significant residual shunts, aortic insufficiency, and device embolization.
Patient selection for TCC
Precise patient selection criteria are critical before TCC. Xiao et al. (15) considered patients to have TCC if they have a body weight exceeding 10 kg, if the non-coronary sinus or the right coronary sinus is the origin of the defect rupturing into the right ventricle or the right atrium, if the defect size is less than 10 mm, if RSOV does not affect the aortic valve and has more than a 7 mm distance from the annulus of the aortic valve, if a gap of more than 5 mm exists between the ostium of the right coronary sinus and the ruptured site, and if surgery is needed in the absence of other cardiac anomalies.
Lui et al. (22) also suggested that RSOV patients with a European System for Cardiac Operative Risk Evaluation II (EuroSCORE II) score exceeding 20% would benefit from TCC. Nevertheless, controversy remains over the indications for TCC in patients with RSOV since this method is new and the prevalence of RSOV is low. Further studies are, therefore, required to validate the indications or contraindications of TCC in patients with RSOV (11).
Imaging
Although there are no stringent guidelines on RSOV imaging modalities, recent studies have proposed a multimodality imaging approach to RSOV (103, 104).
Transthoracic echocardiography (TTE) is the first-line modality for diagnosing RSOV (104). A primary TTE examination can detect aortic root dilation at the level of the Valsalva sinus (7) and assess the RSOV dimension.
Color Doppler echocardiography can visualize the blood flow through the RSOV fistula from the aorta into a heart chamber (105).
TEE provides higher-resolution images due to its proximity to the heart and the thoracic aorta. During corrective interventions, TEE can visualize RSOV (106). Further, the relative accuracy of TEE in defect sizing has reduced the need for balloon occlusive diameter methods during TCC (107).
Multidetector computed tomography and cardiac magnetic resonance imaging (CMR) can assess the aorta fully by forming a 3D reconstruction. Multidetector computed tomography or CMR are also capable of determining the dimensions, morphology, and complications of RSOV.
Electrocardiogram-gated CT or CMR can augment imaging accuracy by controlling motion artifacts (108, 109).
Invasive transcatheter angiography is occasionally necessary to differentiate RSOV from other coronary disorders (7).
Transcatheter occluder devices
The first case of the TCC of RSOV was performed utilizing a Rashkind Umbrella via an arterial approach (110). However, the transvenous approach has been performed more frequently because of its higher maneuverability and easier access to the Valsalva sinus. Recent decades have seen the use of other devices, including Amplatzer ductal occluders, PDA occluders, muscular ventricular septal defect occluders, septal occluders, and coils, depending on the anatomy of the defect.
Amplatzer-type ductal occluder devices have been in frequent use due to the conformity of their shape with RSOV morphology (20). Some studies have reported a preference for PDA occluder use. Other than the characteristics of the defect, the interventionist's familiarity with the device, the availability of the device, and financial concerns are taken into consideration in device selection (111).
Summary of the procedure
TCC involves creating an arteriovenous loop by passing a Judkins right coronary catheter from the ascending aorta through the defect into the right atrium or the right ventricle with the aid of an angled-tip guidewire (25, 110). The guidewire is, then, exchanged for a long guidewire, and a gooseneck snare is introduced through venous access to snare the long guidewire in the right atrium or the pulmonary artery with a view to avoiding entrapment and damage to the chordae tendineae of the tricuspid valve, which could result in postprocedural tricuspid regurgitation. Subsequently, a long wire is exteriorized from venous access to form a stable arteriovenous loop crossing the RSOV. Thereafter, a delivery sheath is introduced through the femoral vein and is negotiated from the RSOV to the ascending aorta while precaution is taken to avoid damage to the surrounding tissues, causing heart blocks or defect dilation (111). In the next step, an appropriate-sized device is selected and connected to a delivery cable. The device is inserted through this sheath, and the aortic disk is opened in the aorta. Next, the delivery sheath and the delivery cable are pulled back so that the disk closes the aortic side of the RSOV. After the confirmation of the appropriate placement, the other disk is deployed in the associated right chamber (110, 112).
It is essential to assess all the steps of the procedure with intraprocedural TEE for the confirmation of the complete blockade of the shunt. Possible residual shunting, aortic regurgitation, tricuspid regurgitation, and other possible procedural complications should also be assessed following complete device emplacement.
Complications
Although shown to be effective, the TCC of RSOV can be associated with severe complications on rare occasions. Possible complications can be prevented or readily addressed through efficient measures. A summary of reported complications is presented in Table 4.
The new onset or progression of an existing aortic regurgitation is the most critical complication in the TCC of RSOV. Aortic insufficiency can be due to traction on the aortic valve annulus or an aortic valve injury during the procedure. In cases of severe aortic insufficiency, surgical intervention is unavoidable.
Compression of the coronary arteries after device insertion can also be a life-threatening complication, which can be avoided by visualizing coronary artery flow during the intervention via angiography. A new-onset ST depression after device implantation can also be due to coronary artery compression. If left undetected, the condition could cause myocardial infarction (109). Embolization of the occluder device can also be a possible complication. Glaceza et al. (109) reported the embolization of undersized devices in 3 cases; they were, however, able to retrieve the migrated devices percutaneously.
Hemolysis is also a rare complication of TCC caused by the inserted device (46).
In rare situations, disturbances in the conduction pathways might result in arrhythmias, including atrioventricular or bundle branch blocks. These blocks are caused by possible traction or compressions on conductive pathways. Later inflammations could also be a cause of these arrhythmias (112).
As with any percutaneous intervention, complications associated with catheterization sites, including atrioventricular fistulae, hematoma, and bleeding events, are also possible.
Limitations
The lack of large-scale studies and clinical trials was the principal limitation of the present study.
Conclusions
RSOV is a rare pathology, and scarce data are available in the literature. The TCC of RSOV is a practical approach with acceptable safety and a high success rate. Most of the data reviewed in the present study were based on expert opinion, case reports, and case series. Hence, large-scale clinical trials/cohorts with extended follow-up periods are needed for elucidation.
Author contributions
Original Draft: AA and FM; Review and Editing: AA and AH; Data Collection: NT, AH, and AA; Supervision: AH and KH; Conceptualization: AH, KH and NT. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1227761/full#supplementary-material
References
1. Chu S-H, Hung CR, How SS, Chang H, Wang SS, Tsai C-H, et al. Ruptured aneurysms of the sinus of valsalva in oriental patients. J Thorac Cardiovasc Surg. (1990) 99(2):288–98. doi: 10.1016/S0022-5223(19)37013-8
2. Chang C-W, Chiu SN, Wu ET, Tsai SK, Wu MH, Wang JK. Transcatheter closure of a ruptured sinus of valsalva aneurysm. Circ J. (2006) 70(8):1043–7. doi: 10.1253/circj.70.1043
3. Ott DA. Aneurysm of the sinus of valsalva. Seminars in thoracic and cardiovascular surgery. Pediatr Card Surg Annu. (2006):165–76. doi: 10.1053/j.pcsu.2006.02.014
4. Van Son JA, Danielson GK, Schaff HV, Orszulak TA, Edwards WD, Seward JB. Long-term outcome of surgical repair of ruptured sinus of valsalva aneurysm. Circulation. (1994) 90:II-20.
5. Silver MA, Roberts WC. Detailed anatomy of the normally functioning aortic valve in hearts of normal and increased weight. Am J Cardiol. (1985) 55(4):454–61. doi: 10.1016/0002-9149(85)90393-5
6. Weinreich M, Yu PJ, Trost B. Sinus of valsalva aneurysms: review of the literature and an update on management. Clin Cardiol. (2015) 38(3):185–9. doi: 10.1002/clc.22359
7. Serban AM, Batrâna N, Cocoi M, Ianoş R, Moț Ş, Kovacs E, et al. The role of echocardiography in the diagnosis and management of a giant unruptured sinus of valsalva aneurysm. Med Ultrason. (2019) 21(2):194–6. doi: 10.11152/mu-1741
8. Bass D, Tivakaran VS. Sinus of valsalva aneurysm. In: Statpearls. Treasure Island (FL): StatPearls Publishing (2023).
9. Kuriakose EM, Bhatla P, McElhinney DB. Comparison of reported outcomes with percutaneous versus surgical closure of ruptured sinus of valsalva aneurysm. Am J Cardiol. (2015) 115(3):392–8. doi: 10.1016/j.amjcard.2014.11.013
10. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. (2009) 151(4):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
11. Yang K, Luo X, Tang Y, Hu H, Sun H. Comparison of clinical results between percutaneous closure and surgical repair of ruptured sinus of valsalva aneurysm. Catheter Cardiovasc Interv. (2021) 97(3):E354–61. doi: 10.1002/ccd.29216
12. Galeczka M, Glowacki J, Yashchuk N, Ditkivskyy I, Rojczyk D, Knop M, et al. Medium- and long-term follow-up of transcatheter closure of ruptured sinus of valsalva aneurysm in central Europe population. J Cardiol. (2019) 74(4):381–7. doi: 10.1016/j.jjcc.2019.03.012
13. Samson N, Varghese L, George O, Joseph G, George P, Roshan J. Trans-catheter device closure of ruptured sinus of valsalva aneurysms using PDA occluder devices. J Clin Diagn Res. (2019) 13(10):OC01–4.
14. Yang K, Wei MD, Geng WL, Hu HB, Xu ZY, Zhang GJ, et al. Safety and efficacy of percutaneous closure of ruptured sinus of valsalva aneurysm. EuroIntervention. (2018) 14(12):e1288–94. doi: 10.4244/EIJ-D-18-00294
15. Xiao JW, Wang QG, Zhang DZ, Cui CS, Han X, Zhang P, et al. Clinical outcomes of percutaneous or surgical closure of ruptured sinus of valsalva aneurysm. Congenit Heart Dis. (2018) 13(2):305–10. doi: 10.1111/chd.12572
16. Awasthy N, Tomar M, Radhakrishnan S, Shrivastava S. Unconventional uses of septal occluder devices: our experience reviewed. Indian Heart J. (2015) 67(2):128–35. doi: 10.1016/j.ihj.2015.02.028
17. Sinha SK, Khanna NN, Razi M, Krishna V, Jha MJ, Mishra V, et al. Safety and feasibility of transcatheter interruption of ruptured sinus of valsalva aneurysm using the cocoon duct occluder: immediate results and mid-term follow-up. Cardiol Res. (2017) 8(4):154–60. doi: 10.14740/cr568w
18. Mahimarangaiah J, Chandra S, Subramanian A, Srinivasa KH, Usha MK, Manjunath CN. Transcatheter closure of ruptured sinus of valsalva: different techniques and mid-term follow-up. Catheter Cardiovasc Interv. (2016) 87(3):516–22. doi: 10.1002/ccd.26107
19. Sinha SC, Sujatha V, Mahapatro AK. Percutaneous transcatheter closure of ruptured sinus of valsalva aneurysm: immediate result and long-term follow-up. Int J Angiol. (2015) 24(2):99–104. doi: 10.1055/s-0034-1396948
20. Tong S, Zhong L, Liu J, Yao Q, Guo Y, Shu M, et al. The immediate and follow-up results of transcatheter occlusion of the ruptured sinus of valsalva aneurysm with duct occluder. J Invasive Cardiol. (2014) 26(2):55–9.24486661
21. Fang ZF, Huang YY, Tang L, Hu XQ, Shen XQ, Tang JJ, et al. Long-term outcomes of transcatheter closure of ruptured sinus valsalva aneurysms using patent ductus arteriosus occluders. Circ J. (2014) 78(9):2197–202. doi: 10.1253/circj.CJ-14-0106
22. Liu S, Xu X, Zhao X, Chen F, Bai Y, Li W, et al. Percutaneous closure of ruptured sinus of valsalva aneurysm: results from a multicentre experience. EuroIntervention. (2014) 10(4):505–12. doi: 10.4244/EIJV10I4A87
23. Guan L, Zhou D, Zhang F, Pan W, Dong L, Chen H, et al. Percutaneous device closure of ruptured sinus of valsalva aneurysm: a preliminary experience. J Invasive Cardiol. (2013) 25(10):492–6.24088421
24. Li Y, Wang GY, Wang ZF, Guo L. Preliminary experience using transthoracic echocardiography guiding percutaneous closure of ruptured right sinus of valsalva aneurysm. Chin Med J. (2011) 124(10):1477–82. doi: 10.3760/cma.j.issn.0366-6999.2011.10.007
25. Kerkar PG, Lanjewar CP, Mishra N, Nyayadhish P, Mammen I. Transcatheter closure of ruptured sinus of valsalva aneurysm using the amplatzer duct occluder: immediate results and mid-term follow-up. Eur Heart J. (2010) 31(23):2881–7. doi: 10.1093/eurheartj/ehq323
26. Sivadasanpillai H, Valaparambil A, Sivasubramonian S, Mahadevan KK, Sasidharan B, Namboodiri N, et al. Percutaneous closure of ruptured sinus of valsalva aneurysms: intermediate term follow-up results. EuroIntervention. (2010) 6(2):214–9. doi: 10.4244/EIJV6I2A34
27. Sen S, Chattopadhyay A, Ray M, Bandyopadhyay B. Transcatheter device closure of ruptured sinus of valsalva: immediate results and short term follow up. Ann Pediatr Cardiol. (2009) 2(1):79–82. doi: 10.4103/0974-2069.52817
28. Szkutnik M, Kusa J, Glowacki J, Fiszer R, Bialkowski J. Transcatheter closure of ruptured sinus of valsalva aneurysms with an amplatzer occluder. Rev Esp Cardiol. (2009) 62(11):1317–21. doi: 10.1016/S0300-8932(09)73084-2
29. Zhao SH, Yan CW, Zhu XY, Li JJ, Xu NX, Jiang SL, et al. Transcatheter occlusion of the ruptured sinus of valsalva aneurysm with an amplatzer duct occluder. Int J Cardiol. (2008) 129(1):81–5. doi: 10.1016/j.ijcard.2007.06.022
30. Arora R, Trehan V, Rangasetty UM, Mukhopadhyay S, Thakur AK, Kalra GS. Transcatheter closure of ruptured sinus of valsalva aneurysm. J Interv Cardiol. (2004) 17(1):53–8. doi: 10.1111/j.1540-8183.2004.01714.x
31. Mumtaz ZA, Sagar P, Rajendran M, Sivakumar K. Transcatheter versus surgical closure of acute ruptured Sinus of valsalva aneurysms with associated ventricular septal defects. Pediatr Cardiol. (2022) 43(7):1494–501. doi: 10.1007/s00246-022-02873-5
32. Abidin N, Clarke B, Khattar RS. Percutaneous closure of ruptured sinus of valsalva aneurysm using an amplatzer occluder device. Heart. (2005) 91(2):244. doi: 10.1136/hrt.2004.041046
33. Agrawal G, Agarwal M, Chintala K. Transcatheter closure of ruptured sinus of valsalva aneurysm in a pregnant woman. J Cardiol Cases. (2015) 12(6):183–7. doi: 10.1016/j.jccase.2015.08.001
34. Ahmed K, Munawar M, Chakraborty R, Hartono B, Yusri A. Device sizing for transcatheter closure of ruptured sinus of valsalva as per echocardiography color Doppler turbulent flow jet diameter. Cardiovasc Intervention Ther. (2015) 30(1):92–6. doi: 10.1007/s12928-014-0257-5
35. Al-Senaidi KS, Al-Farqani A, Maddali M, Al-Maskary S. Transcatheter closure of ruptured sinus of valsalva aneurysm: report of two cases. Sultan Qaboos Univ Med J. (2016) 16(4):e511–5. doi: 10.18295/squmj.2016.16.04.020
36. Altekin ER, Yilmaz H, Küçük M, Demir I. Percutaneous treatment of a ruptured sinus valsalva aneurysm with double orifices. Turk Kardiyol Dern Ars. (2013) 41(1):59–63. doi: 10.5543/tkda.2013.58812
37. Altekin RE, Serkan Karakas M, Er A, YanIkoglu A, Ozbek S, Yilmaz H. Percutaneous closure of ruptured sinus of valsalva aneursym with amplatzer ductal occluder. Acta Cardiol. (2011) 66(5):657–60. doi: 10.1080/AC.66.5.2131095
38. Ari H, Çamci S, Ari S, Kinik M, Melek M. Percutaneous transcatheter closure of ruptured sinus of valsalva aneurysm. Turk Kardiyol Dern Ars. (2019) 47(6):498–502. doi: 10.5543/tkda.2018.80170
39. Aroney N, Putrino A, Scalia G, Walters D. 3D Printed cardiac fistula: guiding percutaneous structural intervention. Catheter Cardiovasc Interv. (2018) 92(7):E478–80. doi: 10.1002/ccd.27786
40. Asmarats L, Bethencourt A, Rodríguez A, Noris M, Maristany J, Grau A, et al. Ruptured sinus of valsalva aneurysm: a reversible cause of suprasystemic pulmonary hypertension. Rev Port Cardiol. (2022) 41(2):177.e1–e4. doi: 10.1016/j.repc.2018.10.016
41. Bialkowski J, Akdeniz C, Celebi A. Transcatheter closure in two rare cases of left-to-right shunt with cardio-O-fix occluders. Cardiol Young. (2012) 22(1):96–9. doi: 10.1017/S1047951111000680
42. Bijulal S, Harikrishnan S, Ajitkumar VK. Nonsurgical closure of recurrent rupture of sinus of valsalva aneurysm in the presence of aortic prosthesis. J Invasive Cardiol. (2009) 21(3):E42–3.19258649
43. Capogrosso C, Santoro G, Giordano M, Russo M. Transcatheter closure of postsurgical ruptured sinus of valsalva with amplatzer duct occluder II AS™ device. Ann Pediatr Cardiol. (2018) 11(1):86–8. doi: 10.4103/apc.APC_38_17
44. Chen F, Li SH, Qin YW, Li P, Liu SX, Dong J, et al. Transcatheter closure of giant ruptured sinus of valsalva aneurysm. Circulation. (2013) 128(1):e1–3. doi: 10.1161/CIRCULATIONAHA.112.113365
45. Cui W, Van Bergen AH, Patel D, Javois AJ, Roberson DA. Transcatheter closure of ruptured sinus of valsalva aneurysm and secundum atrial septal defect with limited inferior rim. Echocardiography. (2008) 25(2):208–13. doi: 10.1111/j.1540-8175.2007.00563.x
46. Cullen S, Somerville J, Redington A. Transcatheter closure of a ruptured aneurysm of the sinus of valsalva. Br Heart J. (1994) 71(5):479–80. doi: 10.1136/hrt.71.5.479
47. Deore RA, Hiremath MS. Transcatheter intervention for ruptured sinus of valsalva aneurysm and coarctation of aorta with bicuspid aortic valve. IHJ Cardiovasc Case Rep. (2022) 6(2):80–2. doi: 10.1016/j.ihjccr.2022.03.006
48. Dhawan S, Tak T. Surgical correction of a massive unruptured sinus of valsalva aneurysm [1]. Cardiology. (2004) 102(2):104–5. doi: 10.1159/000077913
49. Dobarro D, Recalde ÁS, Reyes RM. Severe aortic regurgitation after the closure of a ruptured congenital aneurysm of sinus of valsalva with an amplatzer device. EuroIntervention. (2010) 6(3):426–7. doi: 10.4244/EIJV6I3A71
50. Fedson S, Jolly N, Lang RM, Hijazi ZM. Percutaneous closure of a ruptured sinus of valsalva aneurysm using the amplatzer duct occluder. Catheter Cardiovasc Interv. (2003) 58(3):406–11. doi: 10.1002/ccd.10401
51. Gaio G, Santoro G, Iacono C, Carrozza M, Cappelli Bigazzi M, Giovanna Russo M, et al. Non-surgical treatment of ruptured sinus of valsalva aneurysm. Int J Cardiol. (2006) 113(2):E44–5. doi: 10.1016/j.ijcard.2006.07.041
52. Gioia G, Zheng J, Ray A, Gioia M. Perforated Sinus of valsalva (PSOV) aneurysm closure with a muscular VSD occluder. Cardiovasc Revasc Med. (2014) 15(3):165–70. doi: 10.1016/j.carrev.2013.09.002
53. Gong X, Wang J, Wei L, Zhao T, Hu S. Case report: transcatheter closure of ruptured Sinus of valsalva with ventricular septal defect occluder in a 3-year-old child after repair of ventricular septal defect. Front Pediatr. (2021) 9:751163. doi: 10.3389/fped.2021.751163
54. Hajizeinali A, Hosseinsabet A. Percutaneous device closure of a ruptured aortic sinus of valsalva aneurysm in a patient with a mechanical bileaflet aortic valve. Turk Kardiyol Dern Ars. (2019) 47(3):243. doi: 10.5543/tkda.2018.91650
55. Ilkay E, Çelebi Ö, Kaçmaz F, Pampal K. Retrograde approach for percutaneous closure in a patient with ruptured sinus of valsalva. Turk Kardiyol Dern Ars. (2014) 42(8):759–62. doi: 10.5543/tkda.2014.45202
56. Jayaranganath M, Subramanian A, Manjunath CN. Retrograde approach for closure of ruptured sinus of valsalva. J. Invasive Cardiol. (2010) 22(7):343–5.20603510
57. Jenab Y, Hosseinsabet A, Vaskelyte L, Hosseini K. Platypnoea-orthodeoxia syndrome after percutaneous treatment of ruptured sinus valsalva complicated by SARS-cov-2 pneumonia: a case report. Eur Heart J. (2021) 5(5):1–4. doi: 10.1093/ehjcr/ytab176
58. Karlekar SM, Bhalghat P, Kerkar PG. Complete heart block following transcatheter closure of ruptured sinus of valsalva aneurysm. J. Invasive Cardiol. (2012) 24(12):E314–7.23220992
59. Kerkar P, Suvarna T, Burkule N, Panda R. Transcatheter closure of ruptured sinus of valsalva aneurysm using the amplatzer duct occluder in a critically ill post-CABG patient. J. Invasive Cardiol. (2007) 19(6):E169–71.17541141
60. Kern MC, Janardhanan R, Kelly T, Fox KA, Klewer SE, Seckeler MD. Multimodality imaging for diagnosis and procedural planning for a ruptured sinus of valsalva aneurysm. J Cardiovasc Comput Tomogr. (2020) 14(6):e139–42. doi: 10.1016/j.jcct.2019.09.018
61. Khan MA, Al Kalaf K, Al Otay AM, Momenah TS. Images of percutaneous closure of ruptured sinus of valsalva. Pediatr Cardiol. (2015) 36(6):1308–9. doi: 10.1007/s00246-015-1149-x
62. Khoury A, Khatib I, Halabi M, Lorber A. Transcatheter closure of ruptured right-coronary aortic sinus fistula to right ventricle. Ann Pediatr Cardiol. (2010) 3(2):178–80. doi: 10.4103/0974-2069.74052
63. Kumar B, Kodliwadmath A, Gore P, Chauhan G, Upadhyay AN, Darbari A, et al. Acute left ventricular systolic dysfunction following device closure of ruptured Sinus of valsalva aneurysm. JACC Case Rep. (2022) 4(3):121–7. doi: 10.1016/j.jaccas.2021.09.004
64. Kumar GA, Parimala PS, Jayaranganath M, Jagadeesh AM. Three-dimensional transesophageal echocardiography-guided transcathetar closure of ruptured non-coronary sinus of valsalva aneurysm. Ann Card Anaesth. (2017) 20(Supplement):S73–5. doi: 10.4103/0971-9784.197807
65. Kursaklioglu H, Barçin C, Baysan O, Iyisoy A, Celik T, Köse S. Transcatheter closure of a ruptured sinus valsalva via retrograde approach. Anadolu Kardiyol Derg. (2011) 11(3):271–2. doi: 10.5152/akd.2011.065
66. Mahajan K, Asotra S, Negi P, Merwaha R. Successful device closure of a ruptured sinus of valsalva aneurysm presenting with acute heart failure. BMJ Case Rep. (2015) 2015:bcr2015212883. doi: 10.1136/bcr-2015-212883
67. Mahimarangariah J, Kikkeri HS, Rai KM, Nanjappa MC. Combined transcatheter device closure of ruptured sinus of valsalva and a post-surgical residual ventricular septal defect. Catheter Cardiovasc Interv. (2013) 82(6):E803–8. doi: 10.1002/ccd.24889
68. Mandel L, Gakhal M, Hopkins J. Percutaneous closure of recurrent non-coronary sinus of valsalva aneurysm rupture: utility of computed tomography in procedural planning. J. Invasive Cardiol. (2010) 22(7):336–8.20603507
69. Manuel DA, Lahiri A, George OK. Transcatheter closure of ruptured sinus of valsalva to left ventricle. Ann Pediatr Cardiol. (2016) 9(1):72–4. doi: 10.4103/0974-2069.171386
70. Mehta NK, Mishra N, Kerkar P. Percutaneous closure of ruptured sinus of valsalva aneurysm and atrial septal defect. J Invasive Cardiol. (2010) 22(5):E82–85.20440051
71. Mithani AA, Polimenakos AC, Santucci BA. Ruptured sinus of valsalva found incidentally in a patient with tetralogy of fallot. Pediatr Cardiol. (2013) 34(8):1914–7. doi: 10.1007/s00246-012-0457-7
72. Mohan Maddali M, Nasser Al-Maskari S, Al-Farqani A. Real-Time three-dimensional transesophageal echocardiography in multiple-device closure of a ruptured sinus of valsalva aneurysm. J Cardiothorac Vasc Anesth. (2015) 29(4):e45–6. doi: 10.1053/j.jvca.2014.10.025
73. Naeim HA, Khedr L, Mahmoud A, Saeed W, Taha EA, Abuelatta R. Percutaneous closure of ruptured non-coronary sinus of valsalva to right atrium causing severe right heart failure, a case report. J Cardiol Cases. (2020) 21(2):71–4. doi: 10.1016/j.jccase.2019.10.005
74. Narin N, Özyurt A, Baykan A, Üzüm K. Transcatheter closure of ruptured sinus valsalva aneurysm with retrograde approach. Turk Kardiyol Dern Ars. (2014) 42(3):299–301. doi: 10.5543/tkda.2014.94658
75. Nişli K, Karaca S, Aydoğan Ü. Transcatheter closure of ruptured sinus of valsalva aneurysm using symmetrical perimembraneous VSD device. Anatol J Cardiol. (2016) 16(5):E10. doi: 10.14744/AnatolJCardiol.2016.7044
76. O H-Icí D, Malergue MC, Garot J, Piéchaud JF. Sinus of valsalva rupture: percutaneous closure with real-time 3-dimensional echocardiography. J Am Coll Cardiol. (2010) 56(16):1351. doi: 10.1016/j.jacc.2010.01.074
77. Onorato E, Casilli F, Mbala-Mukendi M, Perlasca E, Santoro F, Bortone F, et al. Sudden heart failure due to a ruptured posterior valsalva sinus aneurysm into the right atrium: feasibility of catheter closure using the amplatzer duct occluder. Ital Heart J. (2005) 6(7):603–7.16274025
78. Pahwa JS, Verma G, Phadke MS, Lanjewar CP, Kerkar PG. Simultaneous transcatheter closure of ruptured sinus of valsalva aneurysm and stent implantation for aortic coarctation. Indian Heart J. (2015) 67:S81–4. doi: 10.1016/j.ihj.2015.09.024
79. Palma A, Silva PV, Pires A. Percutaneous management of a ruptured sinus of valsalva aneurysm in an infant. Cardiol Young. (2021) 31(8):1363–5. doi: 10.1017/S1047951121000652
80. Rao PS, Bromberg BI, Jureidini SB, Fiore AC. Transcatheter occlusion of ruptured sinus of valsalva aneurysm: innovative use of available technology. Catheter Cardiovasc Interv. (2003) 58(1):130–4. doi: 10.1002/ccd.10394
81. Rittger H, Gundlach U, Koch A. Transcatheter closure of ruptured sinus of valsalva aneurysm into the right ventricle with an amplatzer vascular plug II. Catheter Cardiovasc Interv. (2015) 85(1):166–9. doi: 10.1002/ccd.25382
82. Sabiniewicz R, Meyer-Szary J, Siondalski P, Kolaczkowska M, Galaska R. Thrombus in the aorta late complication after percutaneous closure of ruptured sinus of valsalva aneurysm. JACC Cardiovasc Interv. (2015) 8(13):e217–9. doi: 10.1016/j.jcin.2015.06.024
83. Sabiniewicz R, Wozniak L, Potaz P, Mielczarek M, Ciecwierz D. First report of transcatheter closure of a ruptured sinus of valsalva aneurysm using the nit-occlud Le VSD occluder. Kardiol Pol. (2017) 75(1):82. doi: 10.5603/KP.2017.0007
84. Santoro G, Pacileo G, Bigazzi MC, Russo MG, Caianiello G, Calabrò R. Transcatheter closure of ruptured sinus of valsalva aneurysm causing fontan circulation failure. J Cardiovasc Med. (2007) 8(6):470–2. doi: 10.2459/01.JCM.0000269713.10565.91
85. Sarupria A, Kapoor PM, Makhija N, Kiran U. Trans-esophageal echocardiography: an indispensible guide for transcatheter device closure of ruptured sinus of valsalva aneurysm. Ann Card Anaesth. (2012) 15(2):156–7. doi: 10.4103/0971-9784.95081
86. Satilmiş S, Bozbeyoglu E, Ertaş G, Yildirimtürk O, Yildirim A. Transcatheter closure of sinus of valsalva aneurysm rupture in a young patient. Postepy Kardiol Interwencyjnej. (2013) 9(4):390–1. doi: 10.5114/pwki.2013.38870
87. Schaeffler R, Sarikouch S, Peuster M. Transcatheter closure of a ruptured sinus of valsalva aneurysm (RSVA) after aortic valve replacement using the amplatzer muscular VSD occluder. Clin Res Cardiol. (2007) 96(12):904–6. doi: 10.1007/s00392-007-0573-1
88. Shen QS, Deng XX, Jing C, Li YY. Transcatheter closure of a rare ruptured giant non-coronary valsalva sinus aneurysm. Eur Heart J. (2022) 43(22):2164. doi: 10.1093/eurheartj/ehac177
89. Song J, Ascherman B, Eudailey KW, Mohar M, Argenziano M, Takayama H, et al. Long-term failure of amplatzer plugs in the treatment of aortic pathology. J Card Surg. (2017) 32(7):426–9. doi: 10.1111/jocs.13166
90. Soori R, Dixit A, Tewari P, Agarwal S. Right ventricular outflow obstruction caused by cocoon duct occluder used for closure of ruptured sinus of valsalva aneurysm. Ann Card Anaesth. (2021) 24(3):422–4. doi: 10.4103/aca.ACA_184_19
91. Srivastava A, Radha AS. Transcatheter closure of ruptured sinus of valsalva aneurysm into the left ventricle: a retrograde approach. Pediatr Cardiol. (2012) 33(2):347–50. doi: 10.1007/s00246-011-0127-1
92. Tang L, Zhou SH, Fang ZF. Transcatheter closure of ruptured sinus of valsalva aneurysm with double-disc perimembranous vsd occluder in man with mechanical aortic valve. Tex Heart Inst J. (2019) 46(3):211–4. doi: 10.14503/THIJ-17-6215
93. Vamsidhar A, Rajasekhar D, Vanajakshamma V. Transcatheter device closure of multiple defects in ruptured sinus of valsalva aneurysm. Indian Heart J. (2015) 67:S74–7. doi: 10.1016/j.ihj.2015.06.025
94. Vatankulu MA, Tasal A, Erdogan E, Sonmez O, Goktekin O. The role of three-dimensional echocardiography in diagnosis and management of ruptured sinus of valsalva aneurysm. Echocardiography. (2013) 30(8):E260–2. doi: 10.1111/echo.12248
95. Wilson W, Emmanuel Y, Uren N, Northridge D. Percutaneous closure of ruptured sinus of valsalva aneurysms using a retrograde approach without formation of an arteriovenous loop. EuroIntervention. (2015) 10(12):e1. doi: 10.4244/EIJV10I12A258
96. Zhang B, Sun Y, Wu J, Zhu JY, Cao R, Liu XL, et al. Failed transcatheter closure of a giant ruptured sinus of valsalva aneurysm. Chin Med J. (2015) 128(14):1985–6. doi: 10.4103/0366-6999.160624
97. Choudhry LK, Rao VM, Gnanamuthu BR, Agrawal V, Shankar R, Prasath R. Embolization of the device to the left pulmonary artery after the interventional closure of ruptured sinus of valsalva aneurysm. Korean J Thorac Cardiovasc Surg. (2015) 48(3):202. doi: 10.5090/kjtcs.2015.48.3.202
98. Jiang K, Chen J, Zhu X, Xiao H, Ran T, Tang Y, et al. Rupture of sinus of valsalva aneurysm: a case report in a child. BMC Cardiovasc Disord. (2022) 22(1):1–5. doi: 10.1186/s12872-021-02434-3
99. Chua JH, Methangkool E, Cha CM, Mahajan A. The use of real-time three-dimensional transesophageal echocardiography for percutaneous closure of a ruptured sinus of valsalva aneurysm. J Cardiothorac Vasc Anesth. (2014) 28(1):e4–6. doi: 10.1053/j.jvca.2013.08.022
100. Cullen S, Vogel M, Deanfield JE, Redington AN. Rupture of aneurysm of the right sinus of valsalva into the right ventricular outflow tract: treatment with amplatzer atrial septal occluder. Circulation. (2002) 105(1):e1–2. doi: 10.1161/hc0102.100422
101. Foster TJ, Amin AH, Busu T, Patel K, Farjo P, Al Hallak A, et al. Aorto-cardiac fistula etiology, presentation, and management: a systematic review. Heart Lung. (2020) 49(3):317–23. doi: 10.1016/j.hrtlng.2019.11.002
102. Marroush TS, Boshara AR, Botros B, Vendittelli P, Ahmed Z, Dawood L, et al. Rupture of sinus of valsalva aneurysm: two case reports and a concise review of the literature. Heart Lung. (2018) 47(2):131–5. doi: 10.1016/j.hrtlng.2017.10.005
103. Kassab K, Kaul S, Gomez J, Delafontaine JL, Sawaqed R, Saini A. Ruptured sinus of valsalva aneurysm: use of multimodality imaging in delineating structure and function. J Investig Med High Impact Case Rep. (2021) 9:23247096211020684. doi: 10.1177/23247096211020684
104. Xu B, Kocyigit D, Betancor J, Tan C, Rodriguez ER, Schoenhagen P, et al. Sinus of valsalva aneurysms: a state-of-the-art imaging review. J Am Soc Echocardiogr. (2020) 33(3):295–312. doi: 10.1016/j.echo.2019.11.008
105. Arcario MJ, Lou S, Taylor P, Gregory SH. Sinus of Valsalva Aneurysms: A Review with Perioperative Considerations. J Cardiothorac Vasc Anesth. (2021) 35(11):3340–3349. doi: 10.1053/j.jvca.2020.12.016
106. Svensson LG, Adams DH, Bonow RO, Kouchoukos NT, Miller DC, O’Gara PT, et al. Aortic valve and ascending aorta guidelines for management and quality measures. Ann Thorac Surg. (2013) 95(6):S1–S66. doi: 10.1016/j.athoracsur.2013.01.083
107. Sadeghian H, Hajizeinali A, Eslami B, Lotfi-Tokaldany M, Sheikhfathollahi M, Sahebjam M, et al. Measurement of atrial septal defect size: a comparative study between transesophageal echocardiography and balloon occlusive diameter method. J Tehran Heart Cent. (2010) 5(2):74.23074571
108. Feuchtner GM, Spoeck A, Lessick J, Dichtl W, Plass A, Leschka S, et al. Quantification of aortic regurgitant fraction and volume with multidetector computed tomography: comparison with echocardiography. Acad Radiol. (2011) 18(3):334–42. doi: 10.1016/j.acra.2010.11.006
109. Bolen MA, Popovic ZB, Tandon N, Flamm SD, Schoenhagen P, Halliburton SS. Image quality, contrast enhancement, and radiation dose of ECG-triggered high-pitch CT versus non–ECG-triggered standard-pitch CT of the thoracoabdominal aorta. Am J Roentgenol. (2012) 198(4):931–8. doi: 10.2214/AJR.11.6921
110. Ayati A, Toofaninejad N, Hosseinsabet A, Hosseini K, Hajizeinali A. Transcatheter closure of ruptured sinus of valsalva: a report of first five cases in Tehran heart center, Iran. Clin Case Rep. (2023) 11(3):e7036. doi: 10.1002/ccr3.7036
111. Karlekar SM, Bhalghat P, Kerkar PG. Complete heart block following transcatheter closure of ruptured sinus of valsalva aneurysm. J Invasive Cardiol. (2012) 24(12):E314–7.23220992
Keywords: sinus of valsalva, percutaneous closure, ruptured sinus of valsalva aneurysm, transcatheter, aneurysm sinus of valsalva
Citation: Ayati A, Toofaninejad N, Hosseinsabet A, Mohammadi F and Hosseini K (2023) Transcatheter closure of a ruptured sinus of valsalva: a systematic review of the literature. Front. Cardiovasc. Med. 10:1227761. doi: 10.3389/fcvm.2023.1227761
Received: 23 May 2023; Accepted: 7 August 2023;
Published: 25 August 2023.
Edited by:
Pablo Codner, Rabin Medical Center, IsraelReviewed by:
Sivasankaran Sivasubramonian, Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), IndiaMaruti Haranal, U N Mehta Institute of Cardiology and Research, India
© 2023 Ayati, Toofaninejad, Hosseinsabet, Mohammadi and Hosseini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ali Hosseinsabet ali_hosseinsabet@yahoo.com
Abbreviations RSOV, Ruptured Sinus of Valsalva; SOVA, Sinus of Valsalva Aneurysm; TCC, Transcatheter Closure; VSD, Ventricular Septal Defect;, AI, Aortic Insufficiency; BAV, Bicuspid Aortic Valve; RCS, Right Coronary Sinus; LCS, Left Coronary Sinus, NCS, Non-Coronary Sinus; TEE, Transesophageal Echo, TTE, Transthoracic Echo; CMR, Cardiac Magnetic Resonance Imaging; NYHA, New York Heart Association; RA, Right Atrium; RV, Right Ventricle; LA, Left Atrium; ECG, Electrocardiography; ADO, Amplatzer Ductal Occluder; PDA, Patent Ductus Arteriosus.
†ORCID Ali Hosseinsabet orcid.org/0000-0003-2927-3742
 Aryan Ayati
Aryan Ayati Neda Toofaninejad
Neda Toofaninejad Ali Hosseinsabet
Ali Hosseinsabet Fatemeh Mohammadi
Fatemeh Mohammadi Kaveh Hosseini
Kaveh Hosseini