Percutaneous snare-retrieval of intracardiac thrombus under fluoroscopic and transesophageal echocardiography guidance: case report and systematic review
- 1Department of Vascular Surgery, The NO.1 People’s Hospital of Pinghu, Jiaxing, China
- 2Department of Vascular Surgery, The First Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China
Intracardiac foreign bodies (IFB) are rare clinical conditions. There are now several reports on the percutaneous retrieval of IFB under fluoroscopy. However, some IFB are not radiopaque, and retrieval requires combined fluoroscopic and ultrasound guidance. We report the case of a bedridden 23-year-old male patient with T-lymphoblastic lymphoma treated with long-term chemotherapy. Ultrasound examination diagnosed a huge thrombus in the right atrium near the opening of the inferior vena cava which affected the patency of his PICC line. Ten days of anticoagulant therapy did not modify the thrombus size. Open heart surgery was not feasible because of the patient clinical condition. Snare-capture of the non-opaque thrombus was done from the femoral vein under fluoroscopic and ultrasound guidance with excellent outcomes. We also present a systematic review of IFB. We found out that percutaneous removal of IFBs is a safe and effective procedure. The youngest patient who received percutaneous IFB retrieval was 10 days old and weighed only 800 g, while the oldest patient was 70 years old. Port catheters (43.5%) and PICC lines (42.3%) were the most commonly found IFBs. Snare catheters and forceps were the most commonly used instruments.
Introduction
Intracardiac foreign bodies (IFB) can result from invasive medical procedures or trauma (1, 2), and can cause infection, embolism, arrhythmia, and other complications (3, 4). Depending on their type, IFBs are diagnosed typically with x-ray, CT-scan, or ultrasound. The treatment is either conservative, surgical, or percutaneous removal (5, 6). In 1964, Thomas et al. reported the first percutaneous IFB retrieval without thoracotomy (7). Since then, there have been many case reports on the different modalities of IFB removals (8–11). Herein, we report an interesting case of percutaneous snare-retrieval of a non-radiopaque intracardiac thrombus under fluoroscopic and transesophageal echocardiography guidance and we present a comprehensive literature review.
Case report
A severely ill 23-year-old male patient, diagnosed with T-lymphoblastic lymphoma, was receiving chemotherapy over his PICC line at our institution for 8 months.
Transthoracic ultrasound was done for chest pain that cannot be relieved by thoracic puncture and drainage of a pleural. It showed a flocculent echo mass near the inferior vena cava in the right atrium. Transesophageal echocardiography (TOE) showed the thrombotic nature of the mass and described the IFB as a cord-shape formation in front of the caudal end of the PICC line with the tail floating into the right atrium, near the tricuspid valve (Figure 1). Anticoagulation therapy with low molecular weight heparin was started but no change in the size of the thrombus was observed after 10 days. A multidisciplinary team meeting was held to discuss the case, and it was decided that open-heart surgery is very risky for the patient. It was then decided to attempt a percutaneous retrieval under fluoroscopic and TOE guidance.
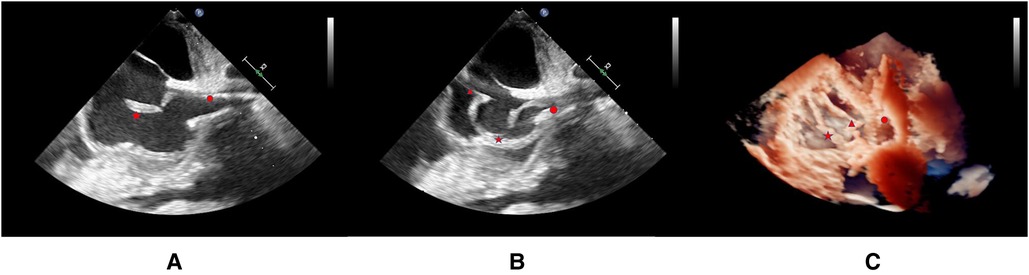
Figure 1. **The locations of the floating thrombus, gooseneck catcher, and PICC are indicated in the image by the five-pointed star, triangle, and circle, respectively. (A) Location of thrombus under transesophageal ultrasound (B) Location of thrombus and snare under transesophageal ultrasound (C) 3D reconstruction after endovascular treatment.
Under general anesthesia, the right femoral vein was accessed with a 10-Fr introducer (Terumo Corp.) and heparin was given. Baseline caval angiographies showed the PICC line in place but we were unable to delineate the location of the IFB. A Gooseneck snare catheter (LifeTech Scientific Corp.) was advanced to the right atrium (Supplementary Video S1). The snare and the thrombus were both localized on TOE. The operator performed repeated gentle grabs until the sonographer confirmed that the thrombus was captured (Supplementary Video S2). The thrombus was carefully exteriorized under fluoroscopic and TOE guidance. We did not identify a filling deficiency in the lumen of either pulmonary artery. TOE did not show residual thrombus at the caudal end of the PICC line and no thromboembolism occurred. Access hemostasis was obtained with manual compression. Anticoagulation therapy was maintained for 24 h. Postoperative pathology showed that the foreign body was old thrombus (Figure 2). The next day ultrasound showed PICC line patency and chemotherapy was restored. After 3 months, the patient had a bone marrow transplant and recovered well.
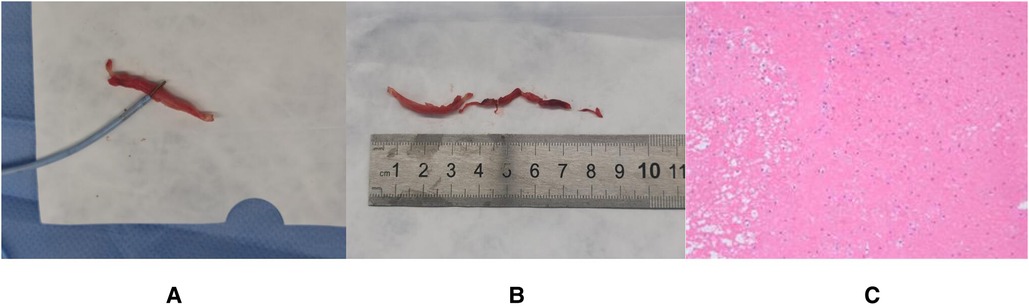
Figure 2. (A) Removed thrombus. (B) The size of the removed thrombus (C) Pathological findings of thrombus (mixed thrombus).
Literature review
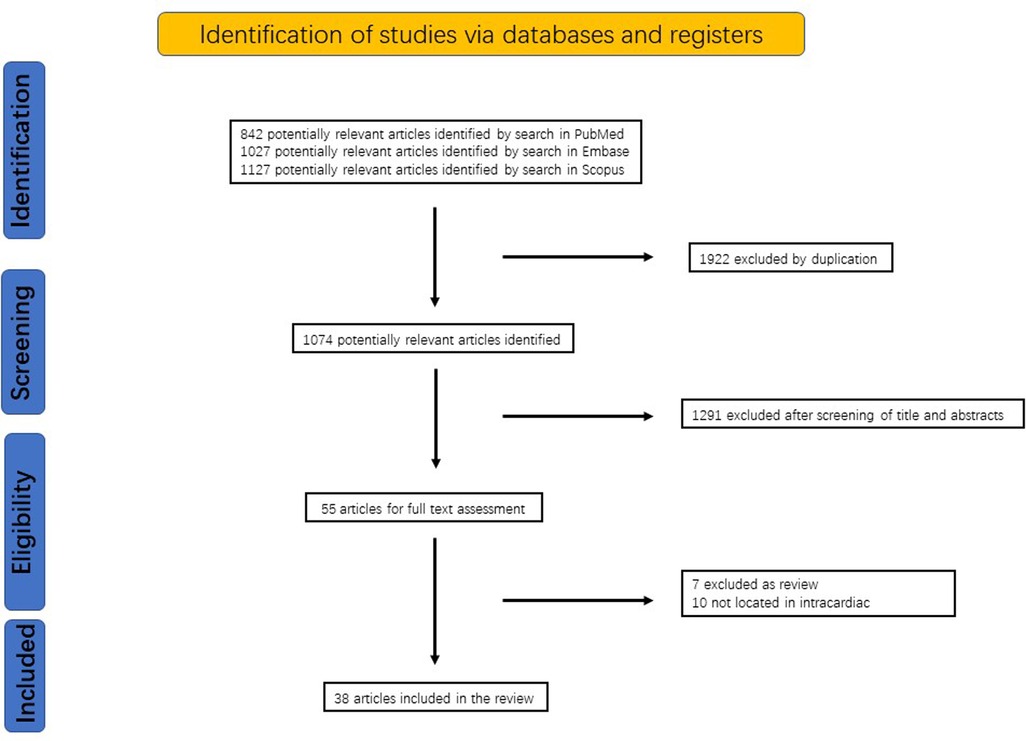
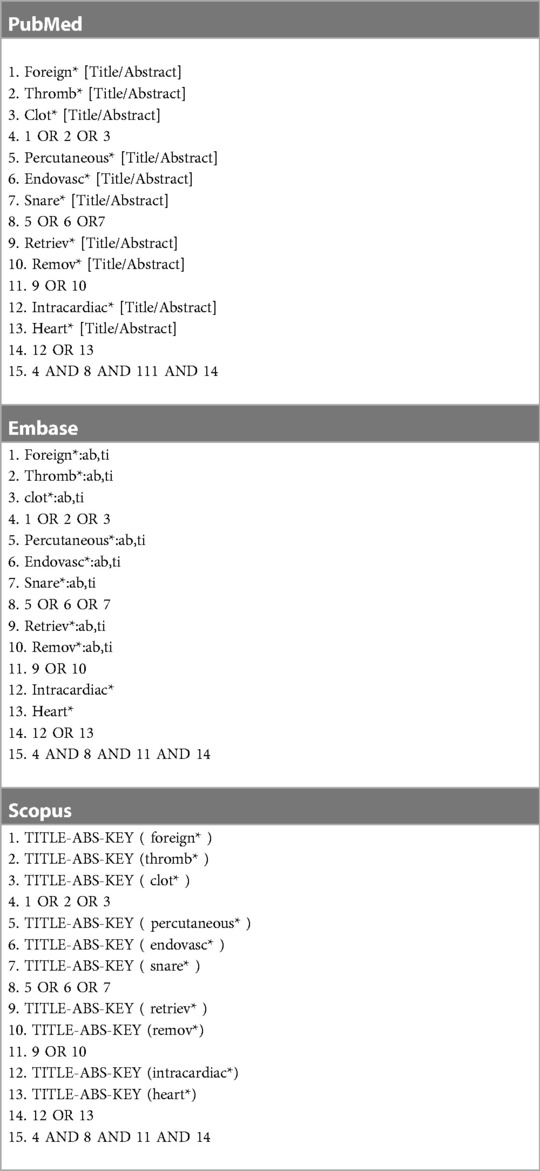
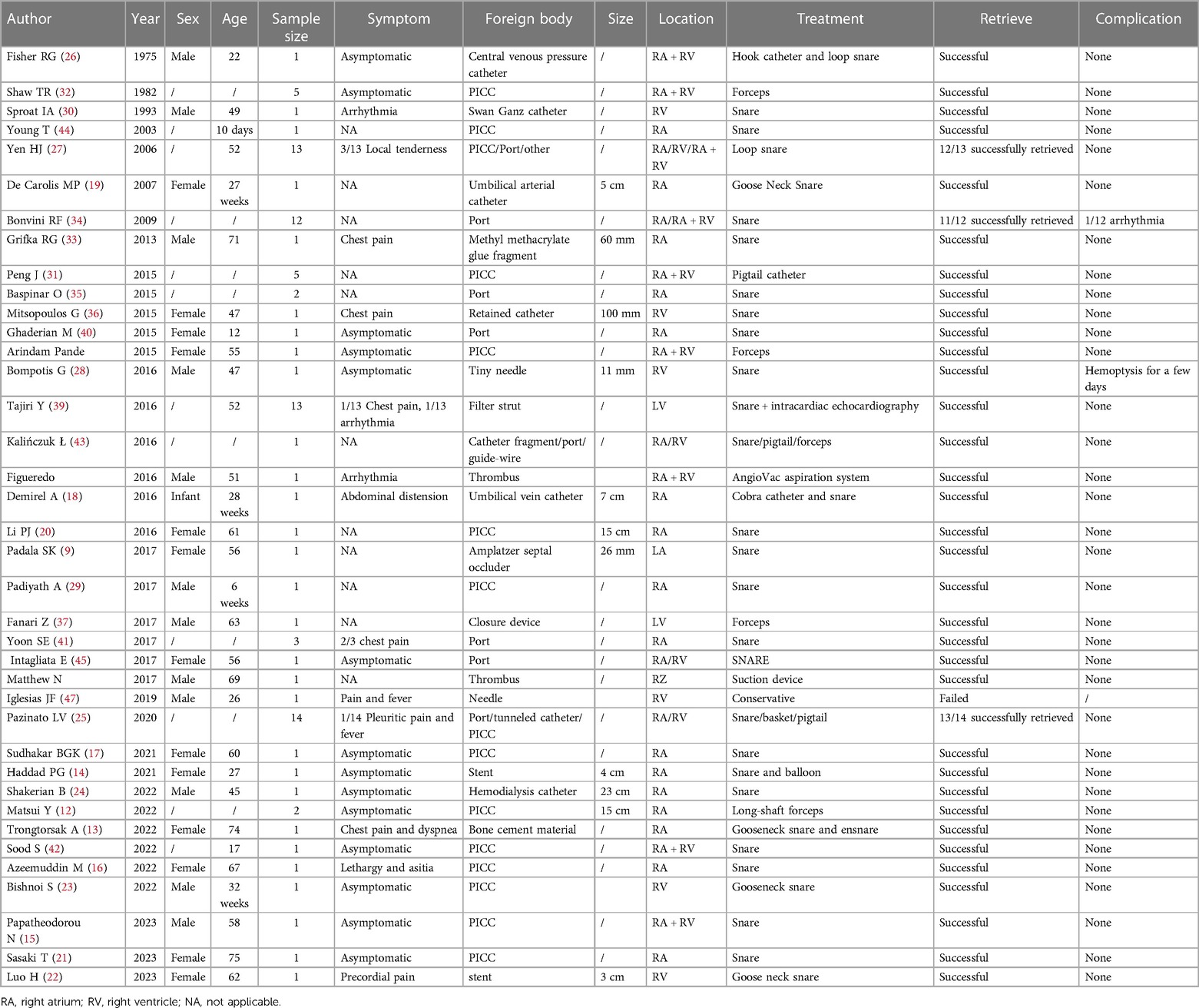
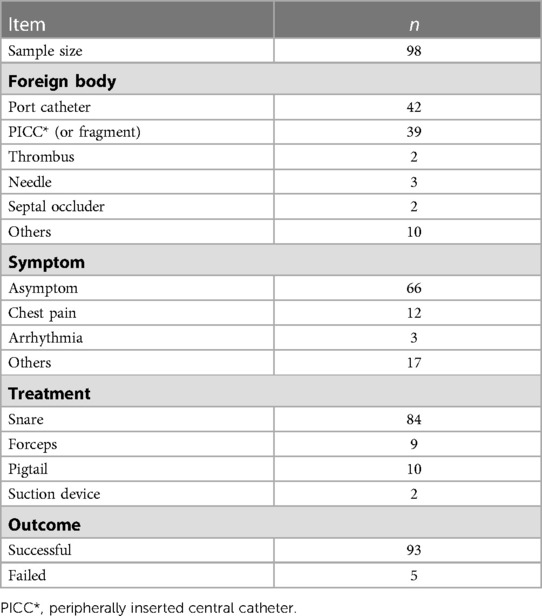
We performed a systematic literature review in PubMed, Embase, and Scopus to identify English articles on endovascular treatment for IFBs from the inception of each database to the 8th of April 2023. Variations of the following search terms were used: percutaneous, retrieval, snare, intracardiac, etc. (Table 1). References of the selected articles was hand searched to look for more studies. Studies were selected for full-text review if their abstracts indicated that the IFB was intracardiac and treated percutaneously. Two independent investigators (B.W., and C.Q.) performed the study selection and data extraction. The search strategy identified 1,074 articles, of which 55 studies were selected for full-text review on the basis of the screening of title and abstract. Seventeen articles were excluded after the full-text review. In the end, a total of 38 reports (8, 9, 11–46) were published from 1975 to 2023 were selected and are comprehensively summarized in Table 2. The identification of studies was summarized in Figure 3.
We found out that the youngest patient who received percutaneous IFB retrieval was 10 days old and weighed only 800 g (44), while the oldest patient was 71 years old (33). Port catheters (42.9%) and PICC lines (39.8%) were the most commonly found IFB (34, 38, 46). There are also some reports of intracardiac needles and metal pieces due to drug use or trauma (47). In only 6 (5.1%) patients, percutaneous IFB removal was not successful (25, 27, 34, 43, 47). Snare catheters and forceps were the most commonly used instruments (25, 27, 46) Table 3.
Discussion
IFBs can develop in situ or usually enter the heart via the circulatory system (48), most usually into the right chambers (49). IFBs can be asymptomatic (50), or they can cause infection, embolism, arrhythmia, and other issues (51, 52). In recent years, the increase of patients with chronic diseases requiring long-term use of drugs has led to more frequent use of long-term venous access systems (53, 54), with a subsequent increase in the incidence of IFB occurrence.
Nowadays, open thoracotomy, endovascular therapy, and conservative treatment are the 3 therapeutic alternatives for IFBs (5, 40, 55). Surgery is a more aggressive procedure, more expensive, and requires long recovery periods. On the other side, the endovascular procedure avoids certain major difficulties and has a claimed success rate of 87%–98% (7, 56, 57). Nowadays, endovascular approach is widely accepted as the first-line treatment for retrieving IFBs, while surgery is usually proposed as a second option (57–59). However, for certain foreign items (such as needles), the success rate cannot be guaranteed and is largely dependent on the doctor's experience and ability (48). There is no consensus regarding conservative treatment. It may rely on the patient's symptoms, the size of the foreign body, and the patient's willingness to undergo surgery.
Since 1964, several endovascular techniques and instruments have been developed and used to retrieve IFBs, including baskets, balloon catheters, grasping forceps, and tip-deflecting wires (7, 60, 61). According to the review, it is evident that the device most commonly used is a snare, which has been created for years by folding a guide wire of a tiny diameter into a loop. However, this stiff loop is vulnerable to damaging the vessel wall. A nondestructive soft metal ring that is welded to the distal end of a wallpaper wire is the modern trap (62). Balloon refers to the use of a flexible catheter with an expandable balloon at the head end. The angioplasty balloon catheter technique is used for cylindrical IFBs, with an inner lumen and a free edge (such as a stent) (57). The balloon is first inserted into the foreign body, and then inflated to form a grip with the foreign body. Baskets are devices that consists of two Nitinol wires looped together to form a basket shape (59). It is utilized to extract brief, tiny IFBs from smaller, tortuous, and distal vessels. Intravascular grasping forceps consist of two distally tapered metallic jaws (58). The proximal handle can be manually operated to adjust the bite force of the pliers. Nonetheless, this device must be operated by an experienced surgeon, as it is easy to cause vascular wall injury or perforation during the process of dragging foreign bodies (62).
X-rays and ultrasounds are typically used to detect IFBs. Fluoroscopy is typically used to perform percutaneous retrieval procedures because it makes it possible to see most metallic foreign bodies (56, 63, 64). However, there are additional reports of IFB retrieval paired with ultrasound guidance because the IFB is not radiopaque and it is challenging to pinpoint the IFB spatial location in the heart due to the heart's pounding (29, 30, 65). In this paper, the IFB was an ancient thrombus that had not responded to anticoagulant therapy and was not visible on fluoroscopy. Therefore, intraoperative TOE was helpful to locate the thrombus and guide the snare retrieval intervention.
Hematoma at the puncture site and intraoperative arrhythmias are the most prevalent consequences of percutaneous retrieval (66). However, such arrhythmias are typically self-limiting and may be connected with intraoperative instrument contact with heart-related tissues (67). From the review of the published reports, intravascular interventional therapy is safe and has a high success rate for retrieval IFBs. Its minimally invasive nature increases indications for even more vulnerable patients (68).
Conclusion
Percutaneous retrieval of IFBs is a low-risk procedure. Intraoperative transesophageal echocardiography guidance can be helpful to determine the IFB spatial structure.
Author contributions
Conception and design: HZ, DL, HZ and ZW. Administrative support: DL and HZ. Provision of study materials or patients: All authors. Collection and assembly of data: HZ, BW, XY, YH and QZ. Data analysis and interpretation: HZ, BW, JP and CQ. All authors manuscript writing and final approval of manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1127131/full#supplementary-material.
References
1. Actis Dato GM, Arslanian A, Di Marzio P, Filosso PL, Ruffini E. Posttraumatic and iatrogenic foreign bodies in the heart: report of fourteen cases and review of the literature. J Thorac Cardiovasc Surg. (2003) 126(2):408–14. doi: 10.1016/S0022-5223(03)00399-4
2. Howanitz EP, Murray KD, Galbraith TA, Myerowitz PD. Peripheral venous bullet embolization to the heart. Case report and review of the literature. J Vasc Surg. (1988) 8(1):55–8. doi: 10.1016/0741-5214(88)90244-3
3. Mainar V, Picó Aracil F, Bordes P, Ruiz Ros JA, Campos Peris JV, Marín F. Percutaneous extraction of intravascular foreign bodies: a series of 38 cases. Rev Esp Cardiol. (1996) 49(1):41–7. 8685511.8685511
4. Decker P, Höfler HR, Decker D, Schnarkowski P, Hansis M. Traumatic foreign body embolism from the basilic vein. Unfallchirurg. (1994) 97(7):372–4. 7939740.7939740
5. Gandhi SK, Marts BC, Mistry BM, Brown JW, Durham RM, Mazuski JE. Selective management of embolized intracardiac missiles. Ann Thorac Surg. (1996) 62(1):290–2. doi: 10.1016/0003-4975(96)00097-5
6. Marshall CD, Ma MR, Park J, Sheckter CC, Massoudi RA, Ligman CM, et al. Recovery of a missile embolus from the right ventricle. Ann Thorac Surg. (2017) 103(1):e69–e71. doi: 10.1016/j.athoracsur.2016.06.107
7. Thomas J, Sinclair-Smith B, Bloomfield D, Davachi A. Non-surgical retrieval of a broken segment of steel spring guide from the right atrium and inferior vena cava. Circulation. (1964) 30:106–8. doi: 10.1161/01.CIR.30.1.106
8. Marcello P, García-Bordes L, Méndez López JM. Peripheral venous embolized intracardiac foreign body. Interact Cardiovasc Thorac Surg. (2009) 9(6):1043–4. doi: 10.1510/icvts.2009.213579
9. Padala SK, Saini A, Gertz ZM, Morano GS, Ellenbogen KA, Koneru JN. A novel percutaneous technique using lasso catheters for retrieval of an embolized amplatzer atrial septal occluder device. JACC Cardiovasc Interv. (2017) 10(3):e25–6. doi: 10.1016/j.jcin.2016.11.052
10. Goel PK, Kapoor A, Batra A, Khanna R. Transcatheter retrieval of embolized AMPLATZER septal occluder. Tex Heart Inst J. (2012) 39(5):653–6. 23109760.23109760
11. Sharma AK, Ganatra S, Hansen J, Yager N, Piemonte T, Gadey G, et al. A dual-snare percutaneous retrieval of venous stent embolization to the right heart. JACC Cardiovasc Interv. (2017) 10(12):e111–3. doi: 10.1016/j.jcin.2017.03.043
12. Matsui Y, Asai T, Oishi A, Kamikawa Y, Amano A, Tabata M. Minimally invasive extraction of a catheter from the heart without thoracotomy. Ann Thorac Surg. (2022) 114(6):e451–3. doi: 10.1016/j.athoracsur.2022.02.019
13. Trongtorsak A, Saad E, Mustafa A, Won KS, Haery C, Hamblin MH, et al. Incidental detection of an intracardiac cement embolism complicating percutaneous vertebroplasty during cardiac catheterization: a case report. J Cardiol Cases. (2022) 26(2):151–3. doi: 10.1016/j.jccase.2022.04.003
14. Haddad PG, Mohamed A, Peden EK. Novel technique of stent retrieval after migration to the right heart. J Vasc Surg Cases Innov Tech. (2021) 7(4):781–4. doi: 10.1016/j.jvscit.2021.09.008
15. Papatheodorou N Sr, Argyriou C, Botaitis S, Diamantidis DE, Georgiadis G. Endovascular retrieval of a detached and dislocated venous port catheter in the right heart chamber using a triple-loop snare device. Cureus. (2023) 15(1):e33681. doi: 10.7759/cureus.33681
16. Azeemuddin M, Khan A, Ansari I, Shahid J, Khan F, Haq TU, et al. Percutaneous endovascular removal of a broken port-a-catheter from right atrium using manual made snare. Radiol Case Rep. (2022) 17(7):2437–40. doi: 10.1016/j.radcr.2022.01.066
17. Sudhakar BGK, Teja BR. Successful recovery of central venous catheter fragment from coronary venous sinus and right ventricle: a case report. Radiol Case Rep. (2021) 16(8):2261–5. doi: 10.1016/j.radcr.2021.03.064
18. Demirel A, Güven G, Okan F, Saygılı A. Successful percutaneous removal of broken umbilical vein catheter in a very low-birth-weight preterm infant. Turk Kardiyol Dern Ars. (2016) 44(8):700–2. doi: 10.5543/tkda.2016.49376.28045419
19. De Carolis MP, Costa S, Polimeni V, Di Stasi C, Papacci P, Romagnoli C. Successful removal of catheter fragment from right atrium in a premature infant. Eur J Pediatr. (2007) 166(6):617–8. doi: 10.1007/s00431-006-0275-0
20. Li PJ, Liang ZA, Fu P, Feng Y. Removal of a fractured tunneled cuffed catheter from the right atrium and inferior vena cava by percutaneous snare technique. J Vasc Access. (2016) 17(3):e42–3. doi: 10.5301/jva.5000497
21. Sasaki T, Fujioka Y, Hikichi H, Yokota D, Ueki S. Endovascular retrieval of a fractured tunneled hemodialysis central venous catheter using the loop snare technique. Cureus. (2023) 15(2):e35617. doi: 10.7759/cureus.35617
22. Luo H, Sun J, Fu J. Endovascular retrieval of a dislocated stent in the right ventricle of a patient with nutcracker syndrome. Int Heart J. (2023) 64(1):100–4. doi: 10.1536/ihj.22-236
23. Bishnoi S, Banerji N, Champaneri B, Deodhar S. Transcatheter retrieval of embolised fractured peripherally inserted central catheter: a nightmare in very low birth weight preterm neonate. Cardiol Young. (2022):1–4. doi: 10.1017/S1047951122002761
24. Shakerian B, Karbalai Saleh S. Percutaneous removal of intracardiac retained hemodialysis catheter: a rare complication of a commonly used procedure. Clin Med Insights Case Rep. (2022) 15:11795476221078650. doi: 10.1177/11795476221078650
25. Pazinato LV, Leite TFO, Bortolini E, Pereira OI, Nomura CH, Motta-Leal-Filho JMD. Percutaneous retrieval of intravascular foreign body in children: a case series and review. Acta Radiol. (2022) 63(5):684–91. doi: 10.1177/02841851211006904
26. Fisher RG, Romero JR. Extraction of an embolized central venous catheter using percutaneous technique. Radiology. (1975) 116(3):735–6. doi: 10.1148/116.3.735
27. Yen HJ, Hwang B, Lee PC, Meng CC. Transcatheter retrieval of different types of central venous catheter fragment: experience in 13 cases. Angiology. (2006) 57(3):347–53. doi: 10.1177/000331970605700311
28. Bompotis G, Karkanis G, Chatziavramidis A, Konstantinidis I, Dokopoulos P, Lazaridis I, et al. Percutaneous removal of a tiny needle fracture from the right ventricle of the heart in a drug abuser. Vasc Endovascular Surg. (2016) 50(8):575–8. doi: 10.1177/1538574416680979
29. Padiyath A, Fontenot EE, Abraham BP. Removal of a retained intracardiac radiolucent guidewire fragment using an atrieve™ vascular snare using combined fluoroscopy and transesophageal echocardiography guidance in an infant. Ann Pediatr Cardiol. (2017) 10(1):65–8. doi: 10.4103/0974-2069.197068
30. Sproat IA, Bielke D, Crummy AB, Rahko P. Transthoracic 2D echocardiographic guidance for percutaneous removal of a nonopaque intracardiac catheter fragment. Cardiovasc Intervent Radiol. (1993) 16(1):58–60. doi: 10.1007/BF02603041
31. Peng J, Zhang XM, Yang L, Xu H, Miao ND, Ren YJ, et al. A novel two-step technique for retrieving fractured peripherally inserted central catheter segments migrating into the heart or the pulmonary artery. Biomed Res Int. (2016) 2016:7814529. doi: 10.1155/2016/7814529
32. Shaw TR. Removal of embolised catheters using flexible endoscopy forceps. Br Heart J. (1982) 48(5):497–500. doi: 10.1136/hrt.48.5.497
33. Grifka RG, Tapio J, Lee KJ. Transcatheter retrieval of an embolized methylmethacrylate glue fragment adherent to the right atrium using bidirectional snares. Catheter Cardiovasc Interv. (2013) 81(4):648–50. doi: 10.1002/ccd.24333
34. Bonvini RF, Rastan A, Sixt S, Noory E, Beschorner U, Leppanen O, et al. Percutaneous retrieval of intravascular and intracardiac foreign bodies with a dedicated three-dimensional snare: a 3-year single center experience. Catheter Cardiovasc Interv. (2009) 74(6):939–45. doi: 10.1002/ccd.22074
35. Baspinar O, Sulu A, Sahin DA. Transcatheter removal of embolized port catheters from the hearts of two children. Case Rep Cardiol. (2015) 2015:973196.26064697
36. Mitsopoulos G, Hanna RF, Brejt SZ, Goldstein GE, Sheynzon V, Weintraub JL, et al. Retrieval of a dislodged catheter using combined fluoroscopy and intracardiac echocardiography. Case Rep Radiol. (2015) 2015:610362. doi: 10.1155/2015/610362
37. Fanari Z, Goel S, Goldstein JA. Successful percutaneous retrieval of embolized transcatheter left atrial appendage closure device (watchman) using a modified vascular retrieval forceps. Cardiovasc Revasc Med. (2017) 18(8):616–8. doi: 10.1016/j.carrev.2017.05.019
38. Cheng CC, Tsai TN, Yang CC, Han CL. Percutaneous retrieval of dislodged totally implantable central venous access system in 92 cases: experience in a single hospital. Eur J Radiol. (2009) 69(2):346–50. doi: 10.1016/j.ejrad.2007.09.034
39. Tajiri Y, Makino K, Hara H, Nakamura M. Transcatheter retrieval of fractured inferior vena cava filter strut penetrating the interventricular septum under intracardiac echocardiography and fluoroscopy. J Vasc Interv Radiol. (2016) 27(11):1727–30. doi: 10.1016/j.jvir.2016.09.008
40. Ghaderian M, Sabri MR, Ahmadi AR. Percutaneous retrieval of an intracardiac central venous port fragment using snare with triple loops. J Res Med Sci. (2015) 20(1):97–9. 25767529.25767529
41. Yoon SE, Lee CH. Successful removal of embolized chemoport catheter within the heart and pericardium: 3 case reports. J Thorac Dis. (2017) 9(8):E718–22. doi: 10.21037/jtd.2017.07.15
42. Sood S, Srinivasan S. Retrieving embolized peripherally inserted central catheter - a novel two step technique. Radiol Case Rep. (2022) 17(3):531–6. doi: 10.1016/j.radcr.2021.11.044
43. Kalinczuk L, Chmielak Z, Debski A, Kepka C, Rudzinski PN, Bujak S, et al. Percutaneous retrieval of centrally embolized fragments of central venous access devices or knotted Swan-Ganz catheters. Clinical report of 14 retrievals with detailed angiographic analysis and review of procedural aspects. Postepy Kardiol Interwencyjnej. (2016) 12(2):140–55. doi: 10.5114/aic.2016.59365
44. Young T, Shaddy RE. Successful percutaneous retrieval of an intracardiac catheter fragment in an 800-g premature infant. J Perinatol. (2003) 23(1):67–8. doi: 10.1038/sj.jp.7210822
45. Intagliata E, Basile F, Vecchio R. Totally implantable catheter migration and its percutaneous retrieval: case report and review of the literature. G Chir. (2017) 37(5):211–5. doi: 10.11138/gchir/2016.37.5.211
46. Wang PC, Liang HL, Wu TH, Huang JS, Lin YH, Huang YL, et al. Percutaneous retrieval of dislodged central venous port catheter: experience of 25 patients in a single institute. Acta Radiol. (2009) 50(1):15–20. doi: 10.1080/02841850802524493
47. Iglesias JF, Qanadli SD, Godin G, Degrauwe S. An unusual intracardiac foreign body. Cardiol J. (2019) 26(6):814–5. doi: 10.5603/CJ.2019.0125
48. Bloomfield DA. Techniques of nonsurgical retrieval of iatrogenic foreign bodies from the heart. Am J Cardiol. (1971) 27(5):538–45. doi: 10.1016/0002-9149(71)90417-6
49. Turner DD, Sommers SC. Accidental passage of a polyethylene catheter from cubital vein to right atrium; report of a fatal case. N Engl J Med. (1954) 251(18):744–5. doi: 10.1056/NEJM195410282511806
50. Cadeddu C, Nocco S, Secci E, Deidda M, Pirisi R, Mercuro G. Echocardiographic accidental finding of asymptomatic cardiac and pulmonary embolism caused by cement leakage after percutaneous vertebroplasty. Eur J Echocardiogr. (2009) 10(4):590–2. doi: 10.1093/ejechocard/jep030
51. Di Carlo I, Cordio S, La Greca G, Privitera G, Russello D, Puleo S, et al. Totally implantable venous access devices implanted surgically: a retrospective study on early and late complications. Arch Surg. (2001) 136(9):1050–3. doi: 10.1001/archsurg.136.9.1050
52. Biswas S, McNerney P. Ventricular tachycardia from a central line fracture fragment embolus: a rare complication of a commonly used procedure-a case report and review of the relevant literature. Case Rep Crit Care. (2015) 2015:265326. doi: 10.1155/2015/265326
53. Cahill AM, Ballah D, Hernandez P, Fontalvo L. Percutaneous retrieval of intravascular venous foreign bodies in children. Pediatr Radiol. (2012) 42(1):24–31. doi: 10.1007/s00247-011-2150-z
54. Surov A, Wienke A, Carter JM, Stoevesandt D, Behrmann C, Spielmann RP, et al. Intravascular embolization of venous catheter–causes, clinical signs, and management: a systematic review. JPEN J Parenter Enteral Nutr. (2009) 33(6):677–85. doi: 10.1177/0148607109335121
55. Tutar E, Aypar E, Atalay S, Yavuz G, Doğu F. Percutaneous transcatheter retrieval of intracardiac central venous catheter fragments in two infants using amplatz goose neck snare. Turk J Pediatr. (2009) 51(5):519–23. 20112614.20112614
56. Motta Leal Filho JM, Carnevale FC, Nasser F, Santos AC, Sousa Junior Wde O, Zurstrassen CE, et al. Endovascular techniques and procedures, methods for removal of intravascular foreign bodies. Rev Bras Cir Cardiovasc. (2010) 25(2):202–8. doi: 10.1590/S0102-76382010000200012
57. Woodhouse JB, Uberoi R. Techniques for intravascular foreign body retrieval. Cardiovasc Intervent Radiol. (2013) 36(4):888–97. doi: 10.1007/s00270-012-0488-8
58. Sheth R, Someshwar V, Warawdekar G. Percutaneous retrieval of misplaced intravascular foreign objects with the dormia basket: an effective solution. Cardiovasc Intervent Radiol. (2007) 30(1):48–53. doi: 10.1007/s00270-005-0297-4
59. Jud P, Portugaller R, Bohlsen D, Gary T, Brodmann M, Hackl G, et al. Successful retrieval of an embolized vascular closure device (Angio-Seal®) after peripheral angioplasty. Cardiovasc Intervent Radiol. (2017) 40(6):942–6. doi: 10.1007/s00270-017-1565-9
60. Carroll MI, Ahanchi SS, Kim JH, Panneton JM. Endovascular foreign body retrieval. J Vasc Surg. (2013) 57(2):459–63. doi: 10.1016/j.jvs.2012.01.092
61. Koseoglu K, Parildar M, Oran I, Memis A. Retrieval of intravascular foreign bodies with goose neck snare. Eur J Radiol. (2004) 49(3):281–5. doi: 10.1016/S0720-048X(03)00078-0
62. Ayx I, Goessmann H, Hubauer H, Uller W, Wiesinger I, Uhl C, et al. Interventional removal of intravascular medical devices: methods and technical success. Rofo. (2016) 188(6):566–73. doi: 10.1055/s-0042-104204
63. Holmes PJ, Miller JR, Gutta R, Louis PJ. Intraoperative imaging techniques: a guide to retrieval of foreign bodies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2005) 100(5):614–8. doi: 10.1016/j.tripleo.2005.02.072
64. Chang RS, Liang HL, Huang JS, Wang PC, Chen MC, Lai PH, et al. Fluoroscopic guidance of retrograde exchange of ureteral stents in women. AJR Am J Roentgenol. (2008) 190(6):1665–70. doi: 10.2214/AJR.07.3216
65. Pathak K, Yadav D. Percutaneous removal of intracardiac and intravascular foreign bodies. Med J Armed Forces India. (2011) 67(4):367–9. doi: 10.1016/S0377-1237(11)60088-9
66. Karanikas ID, Polychronidis A, Vrachatis A, Arvanitis DP, Simopoulos CE, Lazarides MK. Removal of knotted intravascular devices. Case report and review of the literature. Eur J Vasc Endovasc Surg. (2002) 23(3):189–94. doi: 10.1053/ejvs.2001.1591
67. Munck A, Malbezin S, Bloch J, Gerardin M, Lebourgeois M, Derelle J, et al. Follow-up of 452 totally implantable vascular devices in cystic fibrosis patients. Eur Respir J. (2004) 23(3):430–4. doi: 10.1183/09031936.04.00052504
Keywords: intracardiac foreign body, transesophageal echocardiography, percutaneous retrieval, thrombus, snare retrieval
Citation: Zhou H, Wang B, Pan J, Qiu C, Yu X, He Y, Zhu Q, Yu L, Wu Z, Li D and Zhang H (2023) Percutaneous snare-retrieval of intracardiac thrombus under fluoroscopic and transesophageal echocardiography guidance: case report and systematic review. Front. Cardiovasc. Med. 10:1127131. doi: 10.3389/fcvm.2023.1127131
Received: 19 December 2022; Accepted: 24 April 2023;
Published: 9 May 2023.
Edited by:
Enyi Shi, China Medical University, ChinaReviewed by:
Raymond N. Haddad, Assistance Publique-Hôpitaux de Paris (AP-HP), FranceDing Yuan, Sichuan University, China
© 2023 Zhou, Wang, Pan, Qiu, Yu, He, Zhu, Yu, Wu, Li and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huaji Zhou siyuange_1983@163.com Donglin Li lidonglin@zju.edu.cn Hongkun Zhang 1198050@zju.edu.cn
†These authors contributed equally to this work and share first authorship
 Huaji Zhou1,2*†
Huaji Zhou1,2*†  Jun Pan
Jun Pan Xinyu Yu
Xinyu Yu Yangyan He
Yangyan He Ziheng Wu
Ziheng Wu Hongkun Zhang
Hongkun Zhang