Co-design with affect stories and applied ethics for health technologies
- 1GRESEC, Grenoble Alpes University, Grenoble, France
- 2Ethics and AI Chair, Multidisciplinary Institute in Artificial Intelligence (MIAI), Grenoble Alpes University, Grenoble, France
- 3IPHIG, Grenoble Alpes University, Grenoble, France
The integration of digital health technologies in clinical practices and everyday lives of patients raises several issues. Some of them are related to applied ethics. Co-design with patients and, more generally, participatory approaches are increasingly seen as a way to tackle these issues early in the innovation process. This opens the way to an “ethics by co-design.” In this article, we will present the high ambitions of this approach and discuss three challenges raised by ethics by co-design. We will argue that a co-design approach based on affect stories is a way to address these challenges. Then we will focus on a concrete example of a European research project, to discuss the gap between these ethical and theoretical ambitions and what can be achieved in practice. This project aimed at developing an implantable connected device for the monitoring of heart failure, while addressing the ethical, legal and social issues raised by this new technology. However, co-design with patient representatives was in fact limited to a small part of the project: the design of an information module. Based on 18 meetings with a team of 4 patient partners, and 26 additional interviews with patients, we were able to better understand patients’ experiences and priorities in terms of ethics. Together, we co-designed an information module that embodies a vision of the device negotiated between the patients and the technology designers.
1 Introduction
The development of new digital technologies (including the so-called artificial intelligence technologies) is causing major upheavals in the medical field and raising several concerns related to practices, actors, and institutions. Examples include the privacy risk posed by monitoring and self-tracking devices (Shankar et al., 2011; Lupton, 2016; Nissenbaum and Patterson, 2016; Smit et al., 2022), the existence of biases in datasets, that are likely to discriminate against marginalized groups (DeCamp and Lindvall, 2020; Vokinger et al., 2021; Lin and Chen, 2022), and also the fear of medical dehumanization, with the computer tool coming between physicians and their patients, or even, in some cases, replacing physicians in a context of cost reduction and staff shortages (Pols and Moser, 2009; Dorsey and Ritzer, 2016).
In recent years, ethics has been called upon to address these issues. Numerous articles and conferences were published on this subject and various ethical frameworks and methodologies emerged to take ethical risks into account (Jobin et al., 2019; World Health Organization, 2021). Yet current approaches of ethics in innovation have also been widely criticized. Instead of a philosophical reflection based on moral philosophy, “ethics” is frequently understood as a compliance to a set of preset moral principles, that are often “too vague and toothless” to bring about real changes in practices and organizations (Green, 2021; Munn, 2023). Worse still, ethics is accused of being instrumentalized by tech industries and research institutions to defuse criticism by absorbing it on their own terms (Guchet, 2016; Hunyadi, 2017; Lobet-Maris et al., 2019; Green, 2021; Tessier, 2021; Zacklad and Rouvroy, 2022).
At the same time, co-design with patients is presented as a fruitful approach to applied ethics of innovations. The aim is to work not only for the benefit of patients (patient centricity), but with them (patient partnership) (Sanders, 2002). The importance of patient participation has already been underlined in the field of Health Technology Assessment (Ten Have, 2004; Lehoux and Williams-Jones, 2007; Sacchini et al., 2009; Kiran et al., 2015). It is increasingly regarded as an important part of healthcare and health innovation, notably in the vision of “P4 medicine” (Flores et al., 2013). For instance, in the United Kingdom, the watchword is “patient and public involvement” (Ocloo and Matthews, 2016; Greenhalgh et al., 2019; Locock and Boaz, 2019), while in the European Union, one of the pillar of the research & innovation program includes “widening participation” (European Commission, 2021a).
Co-design can be defined as a type of collaborative research aiming at designing a socio-material assembly, that is a “thing” and the “context” in which it is situated (Zamenopoulos and Alexiou, 2018). Ideally, co-design differs from other participatory approaches in two ways. First, end-users should be involved at all stages of the process, including the planning phase, in order to define research issues and goals (Slattery et al., 2020). Second, all stakeholders should participate: researchers, patients, medical and paramedical staff, but also, where relevant, caregivers, receptionists, cleaners, and so on (Locock and Boaz, 2019). In fact, from one study to the next, there is a significant variation in the targeted objectives, the implemented activities, and the participant selection and involvement (Muller and Kuhn, 1993; Almirall et al., 2012; Boyd et al., 2012; Slattery et al., 2020). Just like ethics is subject to criticism for not going far enough, co-design may be accused of tokenism when patient participation is only superficial (Ocloo and Matthews, 2016; Hahn et al., 2017).
In this article, we will discuss how co-design represents a form of applied ethics in health innovation, in other words, an “ethics by co-design.” This expression drifts from the concept of “ethics by design” which was first used by Stephanie L. Moore in the context of organizations (Moore, 2010; Fischer, 2019), and is now frequently used in the field of artificial intelligence with the idea that automatic systems must embed ethics (European Commission, 2021b). While “ethics by design” focuses on the incorporation of ethical principles and requirements during the design process, “ethics by co-design” focuses on the production of norms by the stakeholders involved.
We will start by presenting the ambitions of ethics by co-design and the challenges at stake. Then, we will propose a co-design method based on affect stories, and illustrate it with a case study carried out within the framework of a European project aiming at developing a connected implantable device for the monitoring of patients with heart failure. We will discuss the success and limits of this experience in regard to our initial ambitions. Indeed, due to project governance and large number of stakeholders involved, only partial co-design was in fact possible.
2 The ambitions of ethics by co-design
The relationship between co-design and ethics is neither simple nor obvious. Indeed, co-design concerns a design activity while ethics refers to the philosophical discipline that deals with what is morally good and bad and morally right and wrong (Singer, 2024).
Steen already discussed the “inherent ethical qualities” of co-design from the perspective of Dewey’s philosophical pragmatism (Steen, 2013). Dewey held that philosophy and ethics are not abstract reasoning detached from everyday life. On the contrary, people need to cope with moral questions in each experience, decision, and interaction. In this regard, the participants of a co-design process continuously engage in ethics, because they cooperate, reflect jointly on their practices and experiences, and use their moral imagination to bring about positive change. Donia and Shaw, however, proposed a critical review of the myths associated with co-design in health and stressed the specific challenges raised by artificial intelligence technologies (Donia and Shaw, 2021). Based on critical data studies and critical digital health studies, they hold that co-design can be ethical in process, and unethical in its consequences when looking at the big picture.
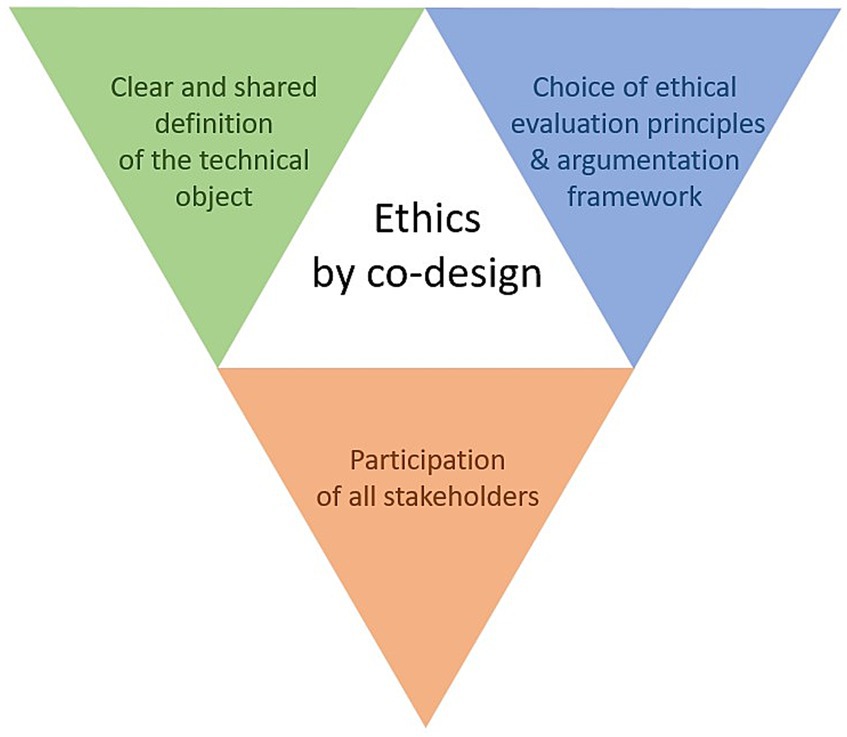
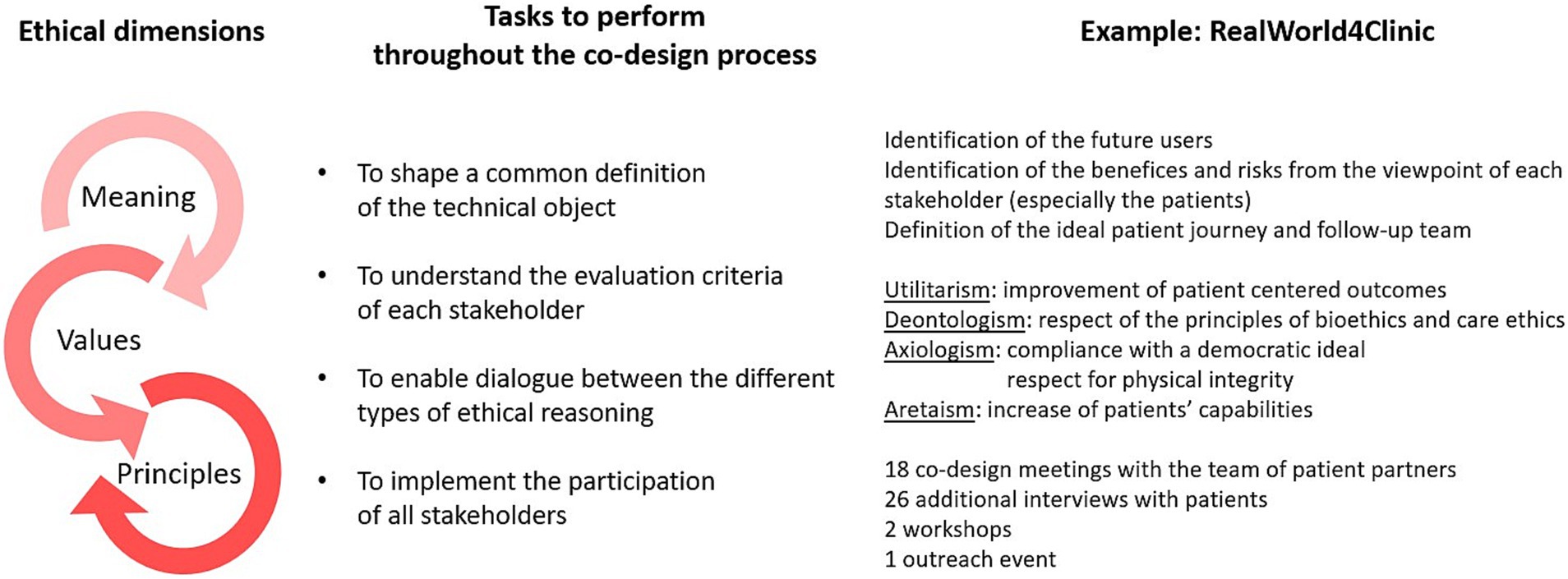
In this paper, we argue that the project of implementing an ethics by co-design raises three complementary philosophical challenges: the search for a clear and shared definition of the technical object under investigation, the choice of ethical evaluation principles and argumentation framework, and the participation of all stakeholders. These challenges are represented in Figure 1 and discussed in the following section.
2.1 Philosophy of technologies and the common definition of technical objects
A first challenge for ethics by co-design is to define or characterize the technology at hand. To succeed, participatory experiences require a “philosophy of technics” that is clear to the participants and relatively shared between them.
The difficulty is accentuated by what may be called “the false evidence of technical objects.” Technical objects are most often proposed by their designers with a particular design, dominated by functionality: they are seen as artefacts defined by their function. This representation can be found in the initial definition of “ethics by design,” which stresses on the designer’s intentions (Fischer, 2019). In practice, health innovation (and even co-design) is frequently focused on the optimization of technical characteristics, at the risk of neglecting social and organizational aspects (Papoutsi et al., 2020). For example, Liljeroos et al. (2020) reported that in the context of remote monitoring of patients with implantable cardioverter-defibrillators, nurses’ work on documenting alerts have been overlooked.
The careless application of a techno-centered representation can be described as “techno-deterministic” and “techno-solutionist.” Techno-determinism means that the uses and social impacts of technologies are considered to be easily predictable, since they are the direct result of designers’ choices (Lehoux and Williams-Jones, 2007). Techno-solutionism is the belief that technology is able to solve any societal issue, including those it has itself caused (Morozov, 2014; Sætra, 2023). These two frameworks, dominate the training of French engineers. Indeed, student selection in engineering courses is highly selective and relies mainly on their performance in mathematics (Quéré, 2019). Engineers are trained to solve problems rationally, regardless of the human context (Roby, 2017; Travadel and Guarnieri, 2021). This encourages a “positivist” epistemology, which sees scientific knowledge as purely objective, and not the fruit of a social construction involving power relationships and conflicting interests (Greenhalgh and Russell, 2010; Bouzin, 2021).
On the contrary, standpoint epistemology developed by feminist philosophers outlined that knowledge is always situated: it depends on the observer’s perspective (Fee, 1981; Haraway, 1988; Harding, 2013). This does not mean that all knowledge and views are equal (which is the claim of relativism), but that real objectivity requires taking into account the researchers’ place in society and their blind spots. Involving various stakeholders broaden perspectives, and makes it possible to change representations of technologies, from “technical objects” to “sociotechnical devices.”
The shift in representations has several consequences. On the one hand, technologies are no longer considered as merely technical objects and greater importance is given to their social and moral dimension. This philosophy of techniques, which focuses on the mediating role of technical artefacts, is called post-phenomenology (Ihde, 1990; Latour, 2002; Verbeek, 2005). On the other hand, users acquire a central role in the innovation process and its assessment (Donnet-Descartes and Dujardin, 2012).
However, this user-centered framework does not guarantee a shared representation of socio-technical devices by all participants. These devices are always a complex aggregate that includes technological objects, software, and human organizations (in our case: an implant, a communication box, and a telemonitoring service). Achieving a shared representation is essential to allow a real ownership of the devices. This is possible by confronting diverse views on values and representations that are associated with these technologies. Indeed, no technology is ever neutral, but rather the bearer of implicit values (Habermas, 1971). The heart of co-design work concerns the discussion of these values, which must be debated among participants. This brings co-design closer to participatory technology assessment procedures, especially when these are explicitly related to ethical questions (Palm and Hansson, 2006; Kiran et al., 2015). Such an approach may seem general, but it is inherently ethical, since ethical issues may arise from a lack of familiarity with technology, as well as from a lack of understanding of what is at stake (Chardel and Reber, 2011). Establishing to what extent and in what ways technical devices induce social behaviors (i.e., revealing the moral influence carried by technical normativity), can be said to be fully ethical. The issue is to move from an external approach to ethics (based on predefined principles and rules) to an ethics “from within,” accompanying all stages of the design process (Verbeek, 2008; Kiran et al., 2015).
2.2 Moral philosophy and choice of ethical evaluation principles
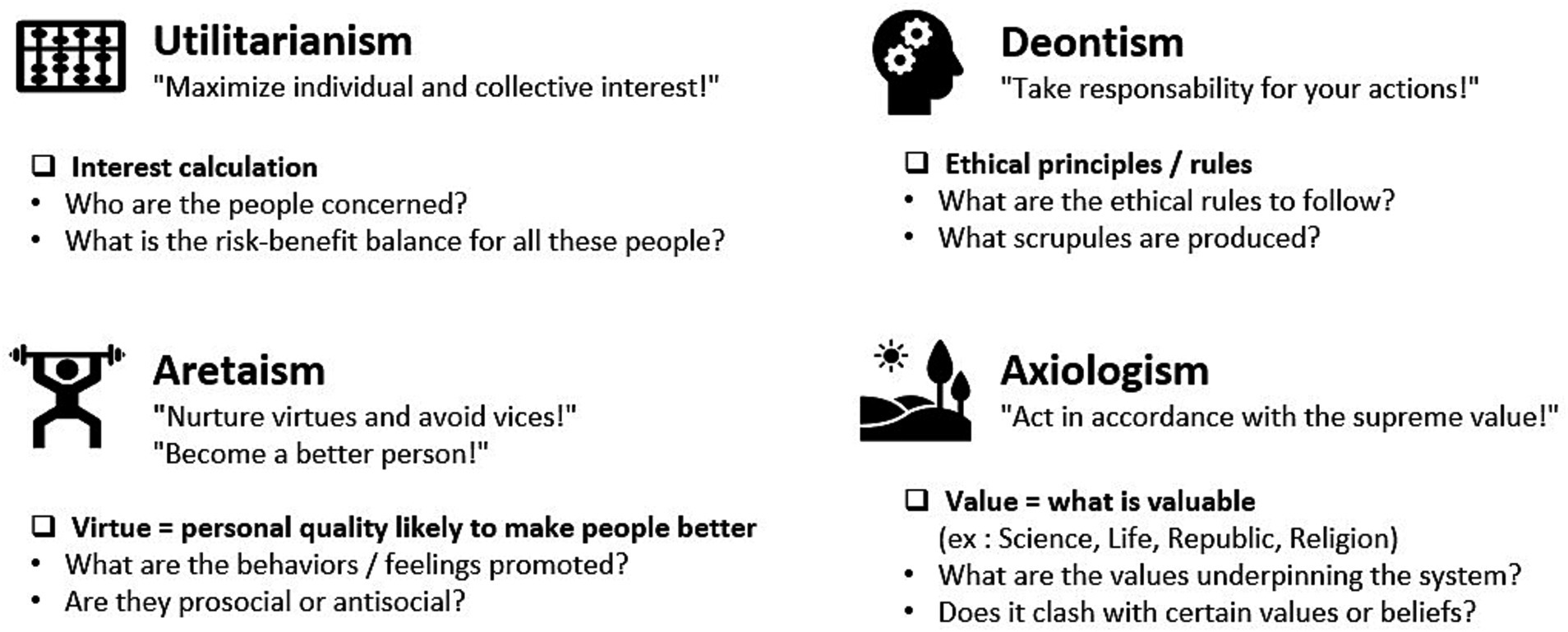
Any ethical approach appears to have multiple dimensions, because it is likely to borrow from various forms of evaluation, that are irreducible to each other. Broadly defined, ethics refers to an undertaking that coordinates three dimensions: (1) the definition of a meaning that is enlightening for human action or activity, (2) the choice of values that are considered good, and (3) the formulation of principles and rules that can guide specific action and orient general activity. The relationship between these elements produces the ethically justified evaluation of a decision. The reasoning leading to such an evaluation can be split into four types of argumentations (see Figure 2).
The consequentialist argumentation examines the relationship between the causes and consequences of the action. The deontological one emphasizes the respect of certain rules. The axiological one privileges justification based on values considered as supreme. Finally, the aretaic one aims at the pursuit for virtues, i.e., dispositions likely to make people ethically better. The consequentialist argumentation is often referred to utilitarianism (Mill, 1863), the deontological one to Kant (2002), the aretaic one to ancient tradition (Aristotle, 350) but also to a modern tradition of virtue ethics, named moral perfectionism (Foot, 1985; Cavell, 2013), finally the axiological one to value theory (Orsi, 2015).
In the context of health technology co-design, the four types of ethical reasoning are likely to be mobilized. Medical and care devices may indeed integrate the interest of the participants (utilitarian ethics). They may be accompanied by precise rules of use (deontological ethics). Their use may refer to specific values (axiological ethics). Finally, they may offer the person who benefits from them the possibility of moral improvement (aretaic ethics). One could argue in a maximalist perspective that ethics of technology will only be complete if all four types of reasoning are discussed.
In the case of health technology co-design experiments, the ethical approach also involves two other ways of practicing ethics: the care theory (Gilligan, 1993) and the capabilities theory (Nussbaum, 1999, 2020). These are difficult to classify in the previous panorama because they have renewed scientific discussion by defining themselves as original and revolutionary.
First, the care ethics devotes a central place to empathy (Gilligan, 1993), a dimension that is essential in the case of health technology assessment. Indeed, the capacity of the participants to be affected by the situation of others is mobilized at least as much as their personal ethical faculties, classically stimulated by the types of reasoning mentioned above (i.e., autonomy of personal judgment or ability to formulate one’s own interest; ability to identify preferable values, to distinguish them from others and to rank them; ability to improve oneself morally). One might add that the empathic dimension of the care ethics represents a condition of possibility for the co-design of health technologies.
Second, co-design constitutes a situated ethical practice in that it favors the empowerment of participants. This is where another ethical theory is called upon, that of capabilities, developed by Nussbaum (1999). In the healthcare field, patients involved in co-design process acquire specific skills such as health literacy and the ability to explain the patient’s perspectives (Goodrich, 2018). They are encouraged to master the conditions of use of the technologies and acquire a practical understanding of the consequences of these uses. By temporarily interacting with the professional circles of technology, health and care, they develop the ability to debate and deliberate on these subjects as quasi-experts on par with the specialists (Zheng and Stahl, 2011; Donetto et al., 2015). One might add that the implementation of a capabilities ethics is a central element of the co-design process, both as a precondition and as a result of co-design (Coeckelbergh, 2011).
2.3 Ethics of discussion and implementation of participation
Finally, the third difficulty is linked to the qualification of the participation which is at the heart of co-design procedures. The notion of participation appeared in theories that have enriched democratic practices from the 1990s (Fishkin, 1991; Cohen, 2005). These theories renewed the idea of public deliberation, by defining rules to manage conflicts during debates on sensitive issues. The notion of participatory democracy raises specific issues that distinguish it from any other known democratic practice (Chambers, 2009). These issues concern the inclusiveness of the panel participants, the definition of the “knowledge base” that allows them to become quasi-experts of the topic of debate, the appropriation of a common language, and finally, the “diplomacy” effort between the various stakeholders in the evaluation process.
If patients’ decision-making power in health innovation is still very limited or inexistant, co-design in health partly inherits this democratic ambition. The Scandinavian participatory design model clearly aimed at democratizing the work place (Ehn, 1993; Bødker et al., 2000), while people-centered care appeared after calls for health care governance democratization and patient empowerment (Millenson, 2011; Rajan and Koch, 2020).
Co-design shows point in common with participatory democracy experiences in two major aspects. First, they both require the constitution of “consensus conferences” or “mini-publics” (Goodin and Dryzek, 2006; Fung, 2007). At the heart of the participatory experience, participants feel progressively “empowered” and this empowerment transforms ordinary people into “quasi-experts” of a subject capable of informed deliberation, and thus of providing an argued decision on a specific topic (Van Hees, 2013). Secondly, there can be no ethical evaluation, unless the participatory process is perfectly defined and supported by participatory tools, such as those developed in participatory democracy. The participatory process management is a particularly important point of vigilance if one wishes to ensure the quality of debates between stakeholders. In particular, the organizers have to carefully consider the independence of the experts who contribute to the participants’ competence acquisition. Under these conditions, co-design processes, like participatory experiences, provide additional legitimacy to the collective decision (Lafont, 2015). Co-design however implies negotiation between the stakeholders, while participatory democracy implies deliberation.
It is worth noticing that these three challenges cannot be addressed once and for all during an ethical technology assessment. On the contrary, they must always and with each new experimentation be considered. Each of these challenges asks a specific question, all of which necessitate answers, and these responses relate to the particular device at stake. This approach is typical of the ethics of user-experience in artificial intelligence technologies, or UX AI Ethics (Ménissier, 2023).
In the next section, we will explain how affect stories could be a fruitful approach to address these challenges in a sociotechnical and situated perspective.
3 A co-design approach based on affect stories
Narrative interviews are a classic tool in participatory approaches, particularly those who referred to Experience-Based Co-design (EBCD) (Bate and Robert, 2007; Donetto et al., 2015; Goodrich, 2018; Dimopoulos-Bick et al., 2019; Gaborit et al., 2021; Sendra et al., 2022). The objective is to draw on the stakeholders’ experience to create space for dialogue and reflection.
Our approach is inspired by EBCD, with a focus on affects (a general term that includes emotions, feelings, sensations, attachments, and moods). We use affects to reveal the issues, concerns, and values of each stakeholder. The underlying assumption is that affects are a way to bring out embodied knowledge (such as those concerning ethical values or the emotional relationship to the illness and its signs) that is usually difficult to express. This method is in line with theoretical contributions of the grounded theory developed by Glaser and Strauss (1967) the pragmatist philosophy of Dewey (1939) (Petit and Ballet, 2023). The aim is to explore the value systems of those involved, regardless of their communication skills, health literacy or ethical knowledge, by asking them about the major negative and positive emotions they feel in relation to technology and the care ecosystem (Dumas and Martin-Juchat, 2022). Note that we do not consider these affects from a psychological perspective, but from a social perspective: they are seen as performative acts, and not as cues of the inner life of the interviewees. For example, in the case study described below, patients were invited to tell their care journey and experience of chronic illness. They were asked to emphasize the major emotions they felt in connection with their medical care, and to describe their relations with each actors involved, including human actors (caregivers, family, collegues) and non-human actors (medicines, monitoring tools, technological environments). After this first spontaneous speech, the interview was deepened with questions focused on affective experiences, such as: What had the greatest emotional impact on you? Who do you trust most among your healthcare professionals? What did you felt when your cardiologist suggested that you should get a defibrillator?
This comprehensive approach to patients’ experiences has several advantages. First, it promotes inclusiveness: the emotional approach allows those who are not comfortable with language to speak. This ties in with the participation issues mentioned in the previous section. Second, the affect stories reveal the problems encountered during the patient journey, as well as the patient’s priorities. The emotions highlight the tacit, implicit, and sensitive interactions and activities between the network of non-human agents and human actors involved in medical care. This research process favors the expression of patients’ perspectives (Dourish, 2001; Schön, 2017). It starts with the practices, to grab a knowledge that is embodied in non-verbalized action rituals (Geertz, 1983), and a cognition that involves embedded technology and transforms the way patients think about illness (Kirsh, 2013).
This work promotes the qualification of the complex influence of interaction relationships between humans (the patient’s ecosystem) and non-humans (medications, prescriptions, and other artefacts that accompany the patient) that are conditioned by communicative and organizational dynamics (Grosjean et al., 2019). This diagnosis aims to collectively assess the place that digital health technology could take in improving the care process. It is a fundamental step in a co-design process which is a matter of ethics: beyond prototyping the technical object, the stakeholders need to agree on a meaning, values and principles associated with the sociotechnical device.
In the following section, we will show how this co-design approach was used in a research project.
4 Use case: co-design of an information module for an implantable health monitoring device
The use case presented in the following section helped us to better understand the challenges of ethics by co-design.
4.1 Context of the study
RealWorld4Clinic is a European consortium funded from 2020 to 2022 by EIT Health (European Institute of Innovation and Technology) and bringing together around fifteen public and private partners. Its aim was to support the development of MyHeartSentinel, a connected health monitoring implant resulting from research carried out in the TIMC laboratory of the University of Grenoble Alpes (Dopierala et al., 2019). This implant is intended to remotely record and transmit cardio-respiratory data, that can be used to remotely monitor patients with heart failure. The ambition of this project was to design this device and to “help resolve the ethical, legal and social issues involved with buying and using AI to maximize heart health data”.1 To achieve this, the consortium brought together physicians, engineers, but also researchers in the humanities and social sciences (including philosophy and information and communication sciences).
The project was divided in 9 work packages:
WP1 – Project management, dissemination & exploitation
WP2 – Specifications and requirements
WP3 – Technical development & CE mark
WP4 – Biocompatibility and safety
WP5 – Clinical validation
WP6 – Telemedical remote monitoring
WP7 – Education and training
WP8 – Business Creation
WP9 – Ethical, legal & social issues.
Each work package was relatively independent, and all their representants met only for the annual consortium meeting. We belonged in WP7 and mainly interacted with WP9. Members of WP9 included a business school (Grenoble Ecole de Management), a Living Lab (Madopa) and the start-up developing the implant (SentinHealth). Our role in WP7 was to co-design an information, education and training module for future patients. At the same time, the members of WP9 conducted two citizen panel consultations (Grenoble Ecole de Management), a Living Lab study (Madopa), and a GDPR Compliance analysis (SentinHealth). These works are not yet published, but we organized together an outreach event in November 2022. Records of the event with live English translations are available online.2
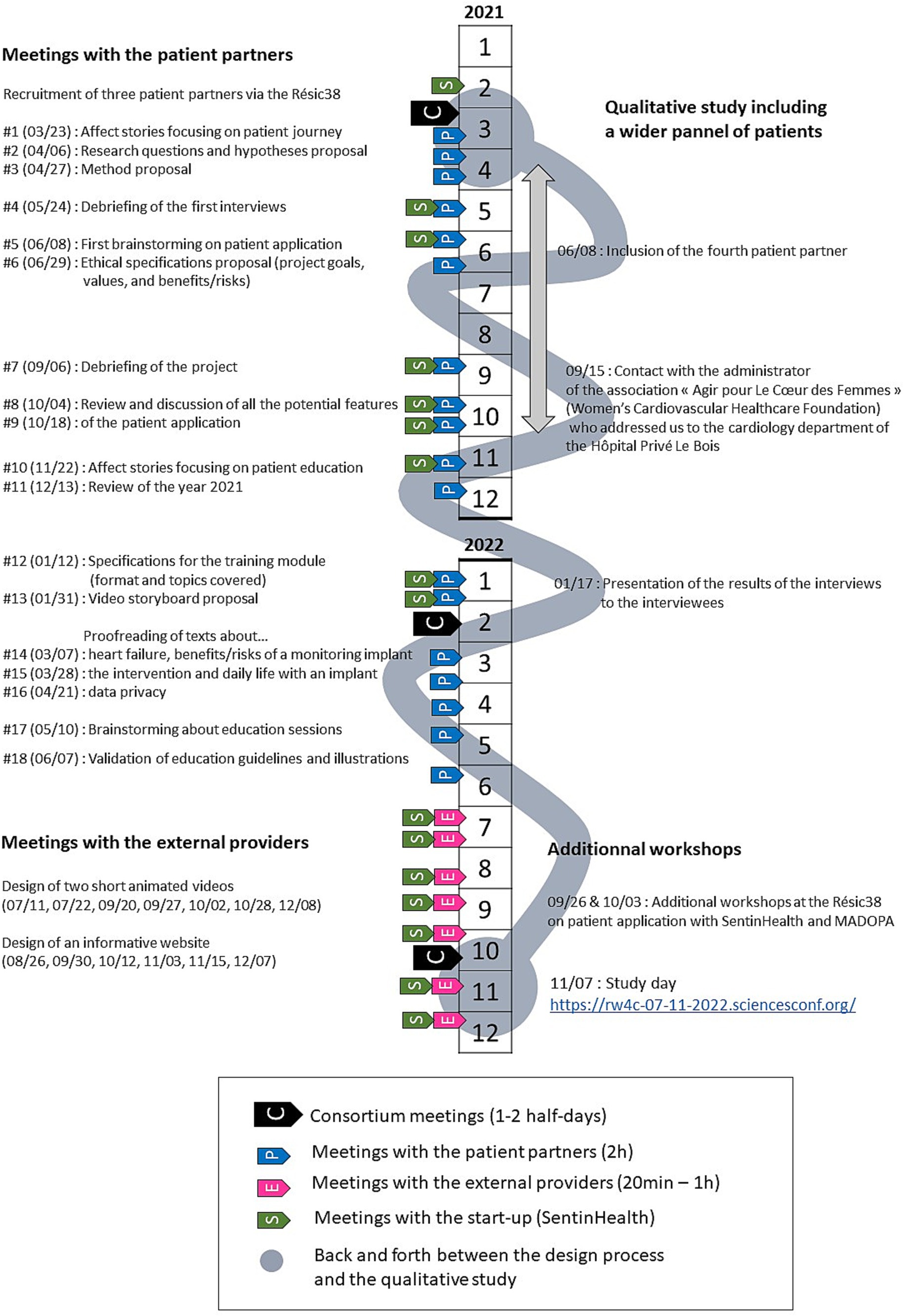
From January 2021 to the end of 2022, we conducted research to develop the information module in collaboration with patients. This research timeline is shown in Figure 3: we represented the annual meetings with the entire consortium, as well as the regular interactions with the patients, project partners (the start-up SentinHealth and the living lab Madopa), and external providers.
A first important observation is that, despite the ethical ambitions of the project, co-design was in fact restricted from the very start. In the deliverables written in 2020 that structured the project, only communication tools were included, not the implantable device itself. Moreover, co-design and ethics were separated in two different work packages. The pivotal study of WP9 (citizen panel consultation) consisted in an online survey of the general population, focusing on the likelihood of implanted device acceptance. This shows the coexistence of two complementary approaches to ethics: one focusing on the experience of people directly concerned by heart failure, the other on mainstream concerns and prior representations.
Yet, our co-design approach has revealed and provided answers to ethical questions that were essential to design the information module: What is the meaning of a monitoring implant for patients with heart failure? What would be a good/bad use of this technology? What information should they have before deciding whether or not to be implanted?
4.2 Methods
4.2.1 Recruitment of four patient partners to follow the project
A small group of patients (3 men and 1 woman) was recruited from March 2021 to work with us throughout the project. Three of them are active members of the Résic38, a health network dedicated to heart failure at Grenoble University Hospital. They were selected by the director of the Résic38, who considered them suitable candidates for our project because of their social skills. They received our call for participation and chose willingly to contact us for more information. After a first telephone call to present the project and answer their questions, they agreed to participate. The fourth participant was spotted shortly after on Instagram for her posts related to heart failure and contacted via private message. After an interview, we proposed her to join the co-design group to bring a fresh perspective and she accepted. The ages of these four patients range from 50 to 76, and their experience of the disease is very diverse: one of them has moderate symptoms, two are equipped with a defibrillator, and the last one received a heart transplant and is therefore cured of heart failure after reaching an advanced stage of the disease. There was no broad call for participation in this project, because the major patient associations were very busy at this time with other partnerships and required funding to participate in research. No financial compensation was paid to either the Résic38 or the participants. All meetings were held in videoconferencing.
These four patients are referred to as “partners” because they were not only interviewed for their expertise in the disease (Gross and Gagnayre, 2013; Hejoaka et al., 2020), but considered as full members of the research team. We started by defining together the major areas of questioning and hypotheses of a qualitative research, aiming at better understanding the experience of patients living with heart failure and their needs related to the information module. First, we collected the affect stories of the patient partners. Based on a thematic analysis of these stories and a literature search, we suggested a list of questions and hypotheses that we improved and validated together. The full list is presented in Supplementary Table S1.
Our research questions focused on four main themes:
• the profile of the patients for whom the implant would be indicated;
• the factors determining the acceptability of the device;
• the sources of anxiety related to the device;
• the impact of the device on heart failure monitoring.
These questions cover two aspects of co-design ethics previously defined: the definition of the monitoring system (What does the implant do?) and the choice of an ethical framework to evaluate it (What are the values preferred by the patients?).
The information module was developed based on this qualitative research (see $4.2.2), as well as several meetings with the patient partners (see $4.2.3).
4.2.2 Qualitative research to broaden the perspectives of the study
Between April and October 2021, we carried out 26 interviews with patients who experienced heart failure. The aim was to gather the perspectives of a wider and more diverse panel of patients, by broadening our call for participation. More details on this part of the study (including participant quotes) can be found in Davat and Martin-Juchat (2023).
These patients were recruited from Résic38 (8), from the Hôpital Privé Le Bois in Lille (11), and via the internet (small patient associations and social media) (7). They are 16 men and 10 women aged between 21 and 89 (65 on average). Most of them (19) had already been implanted with a medical device with remote-monitoring capabilities (pacemaker or defibrillator), and/or were part of a remote follow-up program using connected objects (12).
Our interview guide is presented in Supplementary Table S2. It was constructed to answer the research questions co-designed with the patient partners. The interviews were conducted by phone or videoconferencing and lasted about 1 hour. We interviewed all the people who accepted to answer our call for participation and stopped recruitment after reaching saturation. Each interview was recorded with the consent of the participant, then summarized by the interviewer. The parts mentioning affects were transcribed verbatim. Information which could be used to identify the patients was either generalized (e.g., city names were replaced by brief socio-demographic information), or anonymized (e.g., physicians’ names). We performed a thematic analysis, based on the research questions and hypotheses co-defined with the patient partners (Braun and Clarke, 2006; Vaismoradi et al., 2013). The aim of these additional interviews was not to perform an acceptability test of the medical device or training module (still in development at this time of the project), but to collect affect stories and patient experiences in order to better understand the context and issues related to the development of an implantable monitoring device. So instead of asking patients to project into the future use of a new medical device, we wanted them to share their experiential knowledge of living with heart failure. The underlying assumption is that envision the future of heart failure care is a much more difficult task, that requires a deep understanding of the health care system and its actors, while sharing affect stories is something anyone can do.
We also had the opportunity to interview 4 healthcare professionals working with heart failure patients (the director of the Résic38, a nurse at the Hôpital Privé Le Bois, and two acquaintances of our patient partners). We prepared questions about their organization and daily work to clarify the patient’s journey. The interview guide is presented in Supplementary Table S3.
In January 2022, a videoconference was organized to present the results of this research to the interviewees. 6 out of 26 joined the meeting. We reminded them the context and objectives of the project. Then, we presented the results of our research, hypothesis by hypothesis, as detailed in Davat and Martin-Juchat (2023).
The results of this study were also discussed during the meetings with the patient partners and allowed us to put into perspective their vision of the project. We could compare their experiences with those of other patients, often less involved in their disease management and less familiar with technologies. In particular, we found that the question of data access and privacy was more important to the patient partners than to the interviewees, which guided the design of the information module: these questions were addressed, but not highlighted as much as they could have been if we had followed the patient partners’ opinions alone.
4.2.3 Design of the information module in collaboration with the patient partners
From March 2021 to December 2022, a total of 18 sessions were organized with the four patient partners and the authors of this article at the rate of approximately one two-hour videoconference meeting per month. The topic of each meeting is indicated in Figure 3. On several occasions, the product owner of the start-up SentinHealth (which will eventually market the implant) was invited to keep the team informed with the evolution of the project.
AD and FMJ planned each session. They prepared the agenda and preparatory documents. Each session was recorded and replayed once by AD to write the minutes, which were sent to all participants. These minutes contained the agenda of the meeting, a topic-by-topic summary of discussions and eventually questions to address for the next time. Two representative examples are available in Supplementary Table S4. Looking back, the design of the information module can be summarized in four phases:
March–May 2021: co-design of the qualitative study with the patient partners
June – December 2021: brainstorming on the specifications of the information module
January – June 2022: prototyping of the information module
July – December 2022: creation of the information module with providers and SentinHealth.
During the first three phases, patients participated fully in the design process. During brainstorming, they were asked individually to answer open-ended questions, then to share their viewpoint and discuss together to define priorities or make decisions. They regularly corrected the minutes of sessions when they saw missing elements or spontaneously shared additional information between sessions (such as news on heart failure). They were able to make strong proposals concerning the information module, that were not planned in the initial deliverables (see $4.4). During prototyping, we proposed them texts and images, based on their specifications, that we proofread and amended together in an interactive way. On the other hand, the last phase was carried out without patient intervention, but in collaboration with SentinHealth. This was mostly due to time constraints because the module had to be delivered before the end of 2022 to validate the financing of the EIT Health. We will analyze the consequences of these constraints in section 5.
4.3 Ethical permission
According to French legislation, this study did not require ethical permission, because our aim was not to develop biological or medical knowledge. We nonetheless asked an approval from the CERGA, the multidisciplinary ethics committee of the Université Grenoble Alpes (CERGA-Avis-2021-24). It checked the compliance of our protocol with research ethics guidelines and with the European General Data Protection Regulation (GDPR).
4.4 Results: description of the co-designed information module
Initially, WP7 was tasked with the creation of one realistic video describing the implantation of the medical device for the healthcare team, and one information website for the general public. Co-design with the patient partners led us to update this format and to adapt the content to their concerns.
4.4.1 Short animated videos
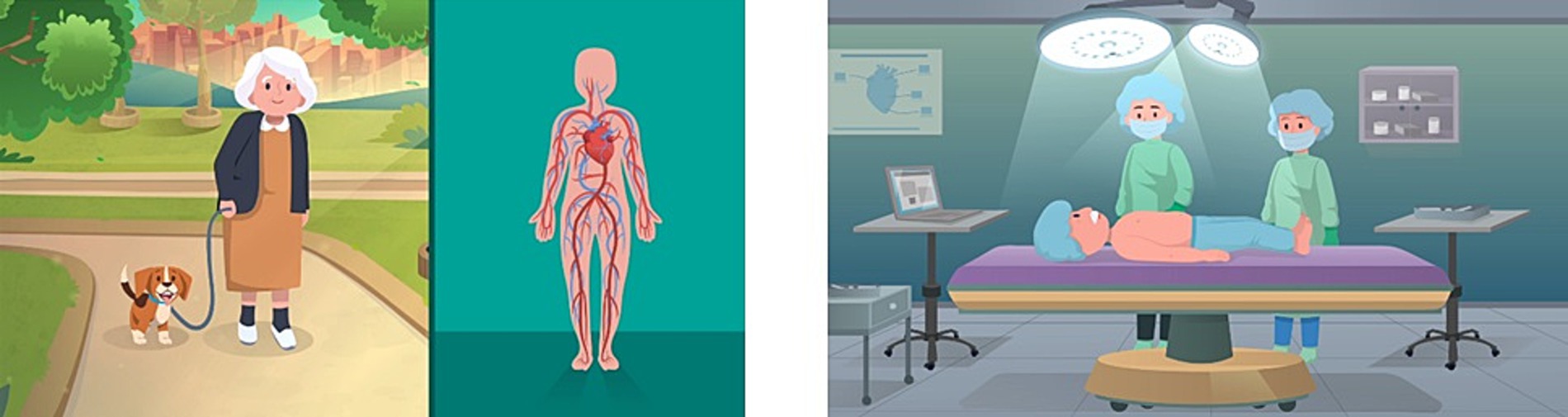
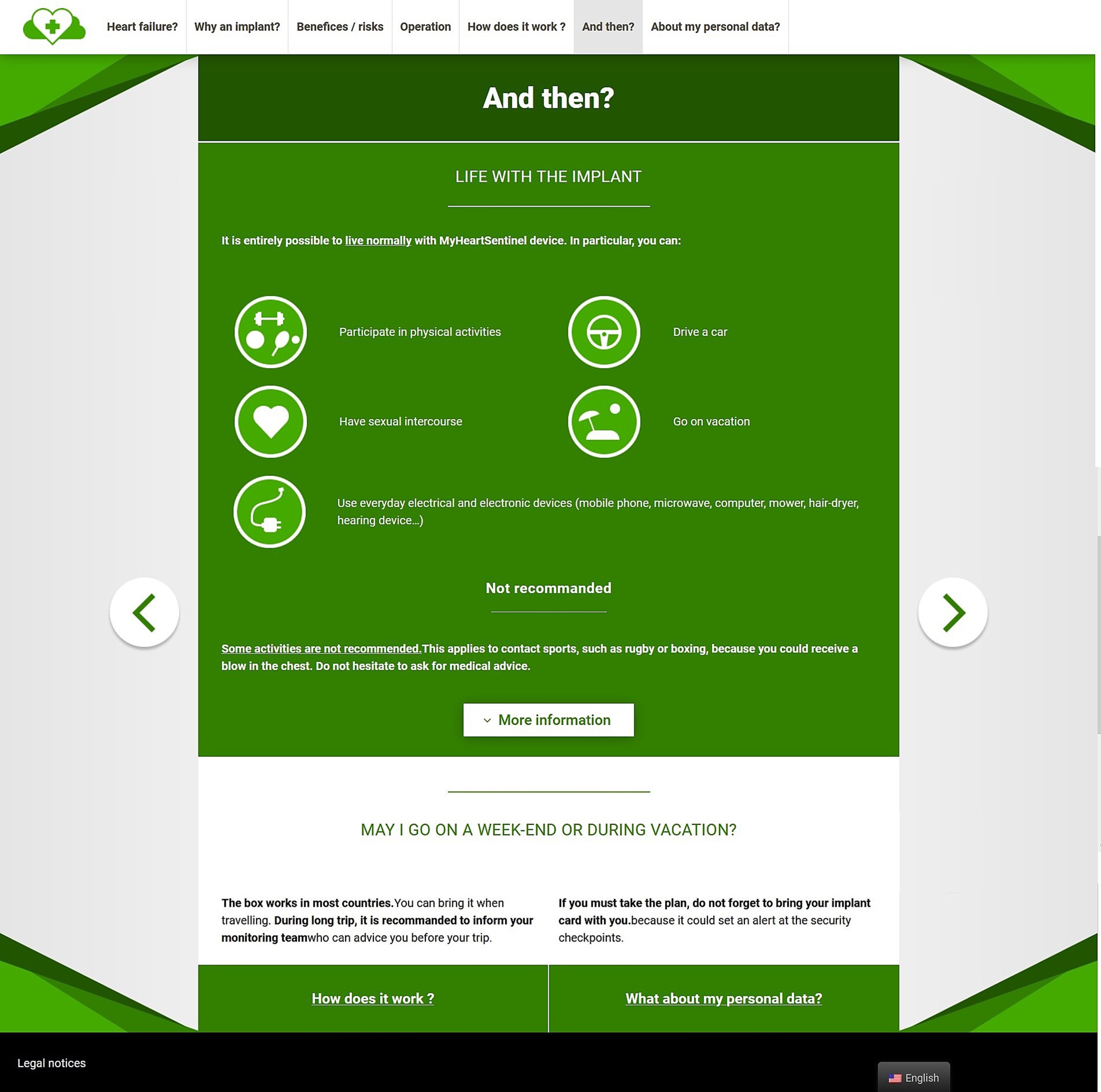
During session 12, we decided to create an animated video, as medical images could be disturbing for non-medical audience. We prepared a first storyboard with SentinHealth, that we presented to the patient partners and discussed in session 13. They recommended changing the word “operation” for “procedure” because they considered it less aggressive. We also realized that we needed to take into accounts the patients’ diversity of expectations: some wish to know in detail the technical gestures to prepare themselves, while other prefer to know as little as possible so as not to worry before the operation. Therefore, we decided to create two short animated videos. The first one (2 min) explains the patient journey and the function of MyHeartSentinel monitoring device. The second one (1 min 40 s) focuses on the implantation procedure. It is intended for the patients who want to know precisely what will happen during the operation. Screenshots of both videos can be found in Figure 4.
4.4.2 Information website
The list of topics to present on the website were first brainstormed with the patients in session 12 and organized in 7 sections:
• What is heart failure?
• What is the purpose of MyHeartSentinel?
• What are the benefits and risks?
• What happens during the intervention?
• How does MyHeartSentinel work?
• And then… (impact on everyday life)
• About my personal data (based on the GDPR module developed by Grenoble Ecole de Management)
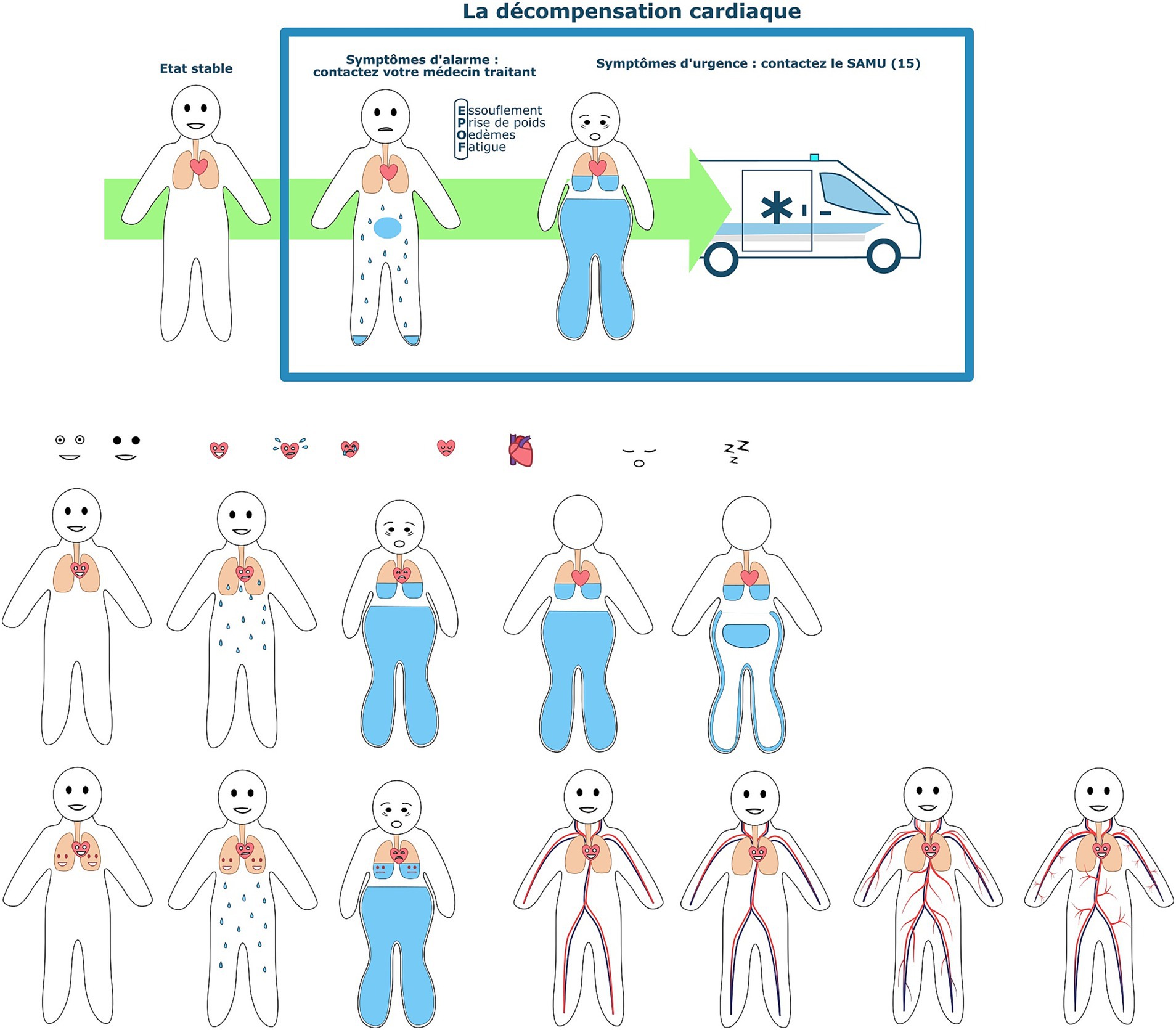
Our aim was to follow the patient-journey and address practical issues, while avoiding an overly pessimistic tone on heart failure. AD wrote the contents, that were proofreaded in sessions 14, 15 and 16. A screenshot of the website is shown in Figure 5. One of the patient partners suggested to add an implant 3D view to allow the visitors to manipulate the device. AD also proposed illustrations, that were amended by the patient partners in session 18. Only one illustration describing heart failure symptoms was retained. It is shown at the top of Figure 6. The rest of the figure shows preparatory drawings that were discussed with the patient partners.
4.4.3 Guidelines for therapeutic education sessions
In addition to the website and videos, that can be consulted individually, the patient partners asked to have access to collective education sessions. They argued that future patients should be able to exchange about their experiences and concerns with their peers, while remaining under the supervision of healthcare professionals. We therefore designed together the guidelines for 2 collective education training sessions. These guidelines should be provided to each hospital where MyHeartSentinel is proposed and adapted to fit in the local education program. We were inspired by the session “Defibrillator and pacemaker in everyday live” organized by the Résic38 as part of its Therapeutic Patient Education program.
We defined together the topics covered by these sessions as well as their timeline in session 17. Indeed, one of the major issues raised by our study is to identify the right time to engage the patients in their disease management. It is easier to organize collective education sessions for patients in rehabilitation because they are well identified and remained in the hospital for several days. However, this time is not ideal, because the patients are often stunned by their recent life-threatening emergency and eager to go home. Moreover, places are rare and usually reserved for the younger patients. It would be better to propose education sessions sometime later, during a consultation with the general practitioner or with the cardiologist. Ideally, patients who accept to be implanted with MyHeartSentinel should engage to participate in these sessions. Otherwise, there is a risk that many patients delegate entirely their disease management to the monitoring team.
The two guidelines proposed focused only on MyHeartSentinel. They should be part of a wider education program, dealing with heart failure, medications, physical activity, daily life, travels etc. The first session focuses on prior information on MyHeartSentinel. It is intended for patients who could be part of the monitoring program but are not yet implanted. The main topics focused on are:
• Patients’ expectations and fears (notably: operation, visibility of the implant, privacy, sexuality, sport, travels)
• What is MyHeartSentinel? How does it work? (monitoring devices & follow-up team)
• Which is its impact on everyday life? (Dos & don’ts)
• Who to contact in case of emergency, technical or medical questions?
The second session consists in experience feedback after implantation, further information about the patient application, and how to engage more in disease management. One of the patient partners also proposed an evaluation grid to evaluate the sessions and learning of the participants.
5 Discussion
In this last section, we will present the contributions and limits of our co-design study. It should be read in conjunction with the ethical challenges identified in section 2, as summarized in Figure 7.
5.1 Shaping a common definition of the socio-technical device
5.1.1 Identification of the care team
This participatory approach first allowed us to better identify the main players in heart failure monitoring. Indeed, MyHeartSentinel was initially conceived as a clinical research tool, an “implantable stethoscope” that would allow hospital cardiologists (both physicians and researchers) to access reliable and high quality “real-life data.” The first cardiologists associated with the project were therefore hospital rhythmologists. They are specialized in data on pacemakers and other cardiac prostheses, but not usually involved in routine care.
It was clear for the patient partners that if MyHeartSentinel was to be used as a monitoring device, then additional actors should be involved. They suggested general practitioners, private cardiologists, and nurses. In particular, the general practitioner appears to be an essential player in ongoing follow-up of chronic heart failure (at least for patients who are lucky enough to have one). The patient partners praised their holistic view of illness, opposed to the cardiologists’ view, often restricted to a single organ. According to them, the role of the general practitioner is to adapt the recommendations of specialists on a case-by-case basis so that these recommendations are applicable and tolerable in daily life.
Furthermore, the patient partners suggested that neither cardiologists nor general practitioners have currently the time nor the training required to provide therapeutic education for their patients. They suggested that this education should be provided by nurses and recommended two existing programs. The Asalée protocol created in 2004 allows general practitioners to build partnerships with nurses and entrust them with some medical acts (Fournier et al., 2018). Since 2018, nurses have also an opportunity for further training in a medical specialty (such as cardiology) to become “nurses in advanced practice.” However, the emergence of this new profession is currently the subject of strong opposition from the Order of Doctors and unions of doctors, who denounce the rise of a substandard medicine (Schwingrouber et al., 2021; Dupuis and Tranthimy, 2023).
Thus, instead of a patient-cardiologist duo, we were able to identify an ideal care team, whose main actors are the cardiologist, the general practitioner and the nurse specialized in therapeutic education. This initial hypothesis was then confirmed by our interviews, by comparing the narratives of the patients who have access to such care team, and those who do not.
5.1.2 Accessing experiential and situated knowledge
Thanks to our qualitative research and regular meetings with the patient partners, we were able to collect valuable insight on living with heart failure.
During the prototyping phase, the patient partners helped us choose the vocabulary and information to be used when writing the texts of the website and the first storyboards for the videos. It is well documented that heart failure is frequently associated with anxiety and depression, especially among patients with cardiac prostheses (Figueroa et al., 2016), and that these disorders affect the evolution of the disease (Celano et al., 2018). However, the patient partners complained repeatedly that mainstream communication on heart failure contributes to this anxiety. Regardless of their age, stage of the disease or medical treatment, newly diagnosed patients with heart failure learn, when looking for information on their disease, that their likelihood of dying within 5 years is 50%. Such communication may sound useful to alert the general public but seems detrimental to the patients. An alternative communication suggested by our patient partners consists in highlighting the possibilities of living better with the disease, by tailoring the medical treatment to their everyday life. For example, the side effects of diuretics and betablockers can be reduced by adapting the dose and time of medication; but this subject is rarely discussed with the physicians, because it requires time and training of healthcare professionals.
In addition, our 26 interviews revealed that the issues are not quite the same depending on age, gender, professional activity, geographical location or even comorbidities. In particular, the risk related to health data, central from a legal viewpoint, is very rarely identified by patients (with a few exceptions). The interviewees were more concerned with the surgery and the impact of the implant on daily life: management of the visibility/invisibility of the disease vis-à-vis of their family, possibility of traveling or continuing to practice physical activities, and need for medical and technical support. This helped us to define the questions that should be answered by the information module.
The reading grid provided by the hypotheses co-designed with the patient partners proved invaluable in analyzing the contradictions observed between and inside interview reports. For example, we observed that the perceived effectiveness of telecardiology depends directly on the relationship established between the patients and the staff in charge of telemonitoring. Thus, telecardiology was judged to be effective by two groups of patients. One group (12/29) is lucky enough to be part of a coordinated follow-up program, within the framework of which they are regularly contacted by nurses. The second group (2/29) is made up of cardiac prosthesis wearers who have been contacted urgently by the hospital as part of an alert related to a material malfunction of their prosthesis. In contrast, other patients (4/29) strongly doubt the effectiveness of telecardiology, because they have never been called, even in the event of sudden resuscitated death or non-transmission of their data for several days.
These results confirmed the need for a personalized approach to health information. We upgraded the information module (initially envisaged as a website) to offer more collective and interactive formats, allowing patients and their caregivers to exchange directly with their peers and healthcare professionals. Inspired by the educative workshops offered by Résic38 and the importance of psychosocial support reported in the interviews, we co-designed the guidelines for two therapeutic education sessions related to the implant. The first session is intended to inform patients before the operation about how the device works and to answer their questions. The second session was devoted to post-implant patient feedback, training on the patient application, and an invitation to enhance their involvement in their disease management.
5.2 Limits of participation
5.2.1 Failing to bring all stakeholders together
The main limitation of our study concerns the recruitment of participants, in particular among healthcare teams. Co-design, aimed at co-writing and co-creation, is by definition time-consuming, so it is difficult to put these approaches at the heart of the priorities of caregivers, who already lack the time and means to take care of their patients. In all, we were able to interview only four people working with patients with heart failure. These interviews were brief and focused on the patient’s journey, rather than on the healthcare professionals’ experience. However, it is certainly these professionals, rather than the patients, who will determine the adoption of the device.
Contrary to what was expected, the involvement of patients in the research design did not help us to diversify the recruitment for the interviews, which was done mainly with two medical structures, and by directly soliciting people who contributed to raise awareness about heart failure online. It should also be noted that our group of patient partners is not representative of all patients with heart failure, which is one of the limitations regularly raised in work dedicated to patient-centered approaches. In the case of heart failure in particular, a recent French study estimates that a third of the people concerned are unable to name their disease (and this is without counting those who are not diagnosed) (Beauvais et al., 2021). However, patient partners do have a role of “interpreters” in the anthropological sense of the term. They operate as ventriloquists of the patients absent from the dialogue, and their words are in turn translated by the researchers (Cooren, 2012).
5.2.2 An unequal dialogue
The second limitation concerns the extent of co-design. Although the technical device (implant and box) was still under development at the time of the study, it could not be co-designed with the patients. The choice of service providers (therefore of the graphic charter) for the development of the website and the videos was also left to the start-up. This notably had an impact on the choices of representations: while the patient partners (especially the younger ones) preferred “ageless” characters to highlight the diversity of people with heart failure, those in the video are obviously elderly, as evidenced by their white hair and clothing. They, thus, correspond more to the target of patients envisaged by the start-up. In fact, these videos have already been used to explain to future shareholders (in the context of fundraising) the health issues related to aging population and the principle of their system.
Furthermore, the ideal vision of the device held by the patient partners during the prototyping phase was toned down in the final version of the information module. Several questions identified as important for the patients remained unanswered (in particular the cost of the device and its reimbursement by health insurance), and a section initially validated was deleted from the version delivered at the end of 2022, because it claimed too early that therapeutic education was central in the follow-up. Guidelines for the organization of two therapeutic patient education sessions have been co-designed, but their implementation will depend on the economic model of the start-up, linked to the funding of the regional health agencies.
It should also be noted that some implicit values and ethical issues were never questioned. The environmental impact of the device, for example, has never been mentioned. Similarly, the management of end-of-life patients has been insufficiently discussed, even though it will eventually concern all implanted patients. Only the sociologist of Madopa mentioned during a consortium meeting the risk of overmedicalizing the last moments of life: indeed, patients who would perhaps prefer to die at home risk dying in hospital, following an alert from their implant.
5.3 Acculturation issues in innovation assessment
Beyond the question of the information module co-design, we were able to observe the difficulty to integrate the voice of patients in a health innovation project.
If patient participation is recognized as a major ethical and social issue (even as an added value compared to the competition according to the start-up SentinHealth), the development of health technologies must meet very strict specifications, which focus on purely technical and regulatory issues (such as biocompatibility of the device). The increasingly systematic use of patient-centered outcomes is a step in the right direction, but is not enough to take into account the diversity of patient experiences and expectations (Blom et al., 2015). Patients most often remain confined to the role of informant and adviser: they have no decision-making power over the development of the project, in which they participate on a voluntary basis. The strict framework of deliverables defined over several years, as well as the large number of stakeholders involved, with varying values, objectives, and priorities, also limit freedom of action.
The MyHeartSentinel project is particularly ambiguous in this regard. Indeed, by looking at the presentation documents of the project, we see that the choice of an implantable device responds first to a techno-centric objective: the goal is to improve the quality of the data available for clinical research and patient follow-up. The possible reduction in patient workload and mental burden associated with chronic disease is only a side effect of the device, which was only conceptualized during the project. Similarly, the choice of subcutaneous rather than gastric implantation (as initially planned) is the result of the reluctance of insurers rather than patients’ request.
What is mobilized here is a utilitarian argumentation, based on a cost–benefit calculation. During the interviews with the patients, another kind of argumentation appeared fundamental: an axiological one, that values the respect of physical integrity. Indeed, four patients who already had prosthetic hearts mentioned their initial concerns about having an electronic “foreign body” inside them. We conclude from our interviews that the decision to have an implant or not depends mainly on the relationship of trust with the referring doctor, and not on a utilitarian calculation of the patients. Not to mention the frequent cases where the procedure takes place in an emergency, when the patients do not really have the possibility of making a decision that opposes the medical norm and must rely on the healthcare professionals. This last example is characteristic of care ethics.
The recognition and integration of these different issues and visions of the world require an acculturation of the different stakeholders, as well as the organization of a real negotiation of priorities through an ethics of discussion. We believe that the role of the researcher is to facilitate the different discussion loops that are to be orchestrated between the different stakeholders, to model the main arguments of each and to bring them collectively into discussion. This is where the added value of co-design lies: succeeding in collectively writing the ethics that the collective will decide to mobilize within the framework of the development of technological innovation (Provencher et al., 2022; Sendra et al., 2022). It is a question of moving away from a techno-determinist vision according to which the impact of a health device and its uses derive directly from the technologies developed, to recognize that these are in reality the fruit of a complex construction between the different stakeholders that is highly dependent on the context (Lehoux and Williams-Jones, 2007; Greenhalgh et al., 2017). This process takes time and is sensitive to changes in actors, which are recurrent in this type of project.
6 Conclusion
In this article, we wanted to discuss the possibility of an ethics by co-design in health innovation. We presented three theoretical challenges raised by this approach and illustrated them with the example of a European project aiming at developing an implantable device for heart failure monitoring. We showed that the maximalist definition of co-design is difficult to integrate in a complex and multi-partner project.
In our case, co-design was not initially conceived as a matter of ethics by the project partners. Its role was to synthetize the contributions of other work packages to produce an information module, that would be accessible to the future patients. The implantable device itself was designed inside the consortium, without direct patient involvement. We used affect stories to co-design a qualitative study with a team of patient partners, and to partially co-design an information module. To return to our initial definition of co-design, we focused on the “context” of the implant, but not on the “thing.” Although this approach was limited, it allowed the participants and the consortium to reflect on the values and meaning of the project.
We have seen that at the heart of the co-design process is the search for a definition of the technical object relevant to all participants. In our example, the central questions concerned the identification of the future users, both health professionals and patients; the evaluation of the benefits/risks from the patient perspective; and the possibility of setting up collective therapeutic education sessions to support the deployment of the device. The information module delivered at the end of 2022 is a testimony to this philosophy, at this stage of the project. It should be supplemented by a discussion of the roles assigned to each stakeholder in the overall care of patients. In particular, should the start-up position itself as a simple technology provider, or should it become more involved in the therapeutic support of patients (which requires new skills and collaborations at a local scale)?
In addition, co-design enables the discussion of different forms of ethical reasoning. From the viewpoint of the project promoters, the technology first addresses utilitarian issues: it is expected to reduce hospital costs linked to heart failure, and to improve the life expectancy and quality of life of patients. Our participatory approach allowed us to complete this overview by emphasizing the importance of considering patients as fully-fledged players in their health, and not simply recipients of care. This demand refers to other forms of ethics: deontological ethics (respect for the principle of autonomy and care ethics), axiological ethics (compliance with the participatory ideal and respect for physical integrity), and aretaic ethics (increase of patients’ capabilities). One of the main ethical conflicts is the competition between the ethics of care, paired by utilitarian health technologies, and ethics of the environment respectful of all living things.
Finally, a health innovation project raises a multitude of technical, scientific, legal, economic, and organizational issues. An ethics of discussion is necessary to negotiate with all the participants, especially since not all of them have the same legitimacy nor the same decision-making power. Co-design and participatory methodologies are tools for implementing this process and keeping track of it. One of the challenges is to document the priorities and hierarchies of values of the various stakeholders, the evolutions of the socio-technical device, the design choices, and the alternatives, to move away from a techno-determinist and techno-solutionist vision.
Beyond the production of communication materials, the main contribution of our participatory approach lies probably in the training and empowerment of the different actors. Moving from this small involvement of patients to a complete “ethics by co-design” will require significant evolutions in project writing and management.
Data availability statement
The datasets presented in this article are not readily available because the dataset consists of interview reports with patients. They agreed on the use of short extracts of their interviews, but not full disclosure. Requests to access the datasets should be directed to fabienne.martin-juchat@univ-grenoble-alpes.fr.
Ethics statement
The studies involving humans were approved by CERGA – Comité d’éthique pour la recherche Grenoble Alpes. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AD: Investigation, Writing – original draft, Writing – review & editing. FM-J: Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. TM: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was part of RealWorld4Clinic, an activity that has received funding from EIT Health. EIT Health is supported by the European Institute of Innovation and Technology (EIT), a body of the European Union. This work has been partially supported by the “Ethics & AI” Chair, MIAI@Grenoble Alpes (ANR-19-P3IA-0003).
Acknowledgments
The authors would like to thank each contributor to RealWorld4Clinic’s education and training package: Daniel Pagonis, Philippe Cinquin, Charles-Clemens Rüling, Annabelle Drault and Raphaël Koster. This study would not have been possible without the help of Baptiste Barjhoux and Murielle Salvat from the Résic38, as well as Jessica Dayez and Frédéric Mouquet from the Hôpital Privé Le Bois. The authors are also very grateful to all the study participants, especially our patient partners. Many thanks to Dakota Root and Maryame Ichiba for their proofreading.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2024.1327711/full#supplementary-material
Footnotes
References
Almirall, E., Lee, M., and Wareham, J. (2012). Mapping living labs in the landscape of innovation methodologies. Technol. Innov. Manag. Rev. 2, 12–18. doi: 10.22215/timreview603
Aristotle. (350). Nicomachean ethics. Translated by D. W. Ross. Available at: http://classics.mit.edu/Aristotle/nicomachaen.html.
Bate, P., and Robert, G. (2007). Bringing user experience to healthcare improvement: the concepts, methods and practices of experience-based design. London, UK: CRC Press.
Beauvais, F., Tartière, L., Pezel, T., Motet, C., Aumont, M.-C., Baudry, G., et al. (2021). First symptoms and health care pathways in hospitalized patients with acute heart failure: ICPS2 survey. A report from the heart failure working group (GICC) of the French Society of Cardiology. Clin. Cardiol. 44, 1144–1150. doi: 10.1002/clc.23666
Blom, J. W., El Azzi, M., Wopereis, D. M., Glynn, L., Muth, C., and van Driel, M. L. (2015). Reporting of patient-centred outcomes in heart failure trials: are patient preferences being ignored? Heart Fail. Rev. 20, 385–392. doi: 10.1007/s10741-015-9476-9
Bødker, Susanne, Ehn, Pelle, Sjögren, Dan, and Sundblad, Yngve. (2000). “Co-operative design — perspectives on 20 years with ‘the Scandinavian IT design model.’” Proceedings of Nordi CHI. Center for User Oriented IT Design, 22–24.
Bouzin, A. (2021). “Ce Que Le Militantisme «vert» Fait Aux Ingénieurs: Un Corps Au Service de La Cause Écologiste?” in Association française de sociologie 9e Congrès de l’AFS" Changer?", RT 21 «Mouvements Sociaux», Session 1: Se Mobiliser Dans et Par Le Travail, Entre Relais Institutionnels et Réseaux Clientélaires
Boyd, H., McKernon, S., Mullin, B., and Old, A. (2012). Improving healthcare through the use of co-design. N. Z. Med. J. 125:12.
Braun, V., and Clarke, V. (2006). Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101. doi: 10.1191/1478088706qp063oa
Cavell, S. (2013). This new yet unapproachable America: Lectures after Emerson after Wittgenstein. Chicako, USA: University of Chicago Press.
Celano, C. M., Villegas, A. C., Albanese, A. M., Gaggin, H. K., and Huffman, J. C. (2018). Depression and anxiety in heart failure: a review. Harv. Rev. Psychiatry 26, 175–184. doi: 10.1097/HRP.0000000000000162
Chambers, S. (2009). Rhetoric and the public sphere. Political Theory 37, 323–350. doi: 10.1177/0090591709332336
Chardel, P.-A., and Reber, B. (2011). Risques éthiques. Communications 88, 149–157. doi: 10.3917/commu.088.0149
Coeckelbergh, M. (2011). Human development or human enhancement? A methodological reflection on capabilities and the evaluation of information technologies. Ethics Inf. Technol. 13, 81–92. doi: 10.1007/s10676-010-9231-9
Cohen, J. (2005). “Deliberation and democratic legitimacy” in Debates in contemporary political philosophy: an anthology (London, UK: Routledge), 352–370.
Cooren, F. (2012). Communication theory at the center: ventriloquism and the communicative constitution of reality. J. Commun. 62, 1–20. doi: 10.1111/j.1460-2466.2011.01622.x
Davat, A., and Martin-Juchat, F. (2023). Patients’ information needs related to a monitoring implant for heart failure: co-designed study based on affect stories. JMIR Hum. Factors 10:e38096. doi: 10.2196/38096
DeCamp, M., and Lindvall, C. (2020). Latent Bias and the implementation of artificial intelligence in medicine. J. Am. Med. Inform. Assoc. 27, 2020–2023. doi: 10.1093/jamia/ocaa094
Dewey, J. (1939). “Theory of valuation” in International encyclopedia of unified science. (eds.) O. Neurath and T. Kuhn. Available at: https://psycnet.apa.org/record/1939-05448-001
Dimopoulos-Bick, T. L., O'Connor, C., Montgomery, J., Szanto, T., Fisher, M., Sutherland, V., et al. (2019). ‘Anyone can co-design?’: A case study synthesis of six experience-based co-design (EBCD) projects for healthcare systems improvement in New South Wales, Australia. Patient Exp. J. 6, 93–104. doi: 10.35680/2372-0247.1365
Donetto, S., Pierri, P., Tsianakas, V., and Robert, G. (2015). Experience-based co-design and healthcare improvement: realizing participatory design in the public sector. Des. J. 18, 227–248. doi: 10.2752/175630615X14212498964312
Donia, J., and Shaw, J. (2021). “Co-design and ethical artificial intelligence for health: myths and misconceptions” in Proceedings of the 2021 AAAI/ACM conference on AI, ethics, and society. (London, UK: Virtual Event USA: ACM), 77.
Donnet-Descartes, É., and Dujardin, D. (2012). “Fondements Éthiques: Donner Une Place Au Sujet” in Évaluer Avec Les Usagers. (Rennes, France: Presses de l’école des hautes études en santé publique), 33–40.
Dopierala, C., Guméry, P.-Y., Frikha, M.-R., Thiébault, J.-J., Cinquin, P., and Boucher, F. (2019). “Digital implantable gastric stethoscope for the detection of early signs of acute cardiac decompensation in patients with chronic heart failure” in Actes de l’Atelier IA & Santé Available at: https://ia-sante-2019.sciencesconf.org/data/actes_atelier_IA_Sante2019.pdf
Dorsey, E. R., and Ritzer, G. (2016). The McDonaldization of medicine. JAMA Neurol. 73, 15–16. doi: 10.1001/jamaneurol.2015.3449
Dourish, Paul. (2001). Where the action is: the foundations of embodied interaction. American Medical Association, Chicago, IL.
Dumas, A., and Martin-Juchat, F. (2022). Les Communications Affectives En Organisations. Louvain-La-Neuve, France: De Boeck Supérieur.
Dupuis, Cyrille, and Tranthimy, Loan. (2023). “Accès direct aux IPA: feu vert des députés, tollé des médecins.” Le Quotidien du Médecin, 2023. Available at: https://www.lequotidiendumedecin.fr/liberal/exercice/acces-direct-aux-ipa-feu-vert-des-deputes-tolle-des-medecins.
Ehn, P. (1993). “Scandinavian design: on participation and skill” in Participatory design: principles and practices. (eds.) D. Schuler and A. Namioka (Boca Raton: CRC Press), 41–77.
European Commission. (2021a). “#HorizonEU: Research&Innovation Programme 2021-27.” Available at: https://research-and-innovation.ec.europa.eu/system/files/2022-06/ec_rtd_he-investing-to-shape-our-future_0.pdf.
European Commission. (2021b). “Ethics by design and ethics of use approaches for artificial intelligence.” European Commission. Available at: https://ec.europa.eu/info/funding-tenders/opportunities/docs/2021-2027/horizon/guidance/ethics-by-design-and-ethics-of-use-approaches-for-artificial-intelligence_he_en.pdf.
Figueroa, C., Alcocer, L., and Ramos, B. (2016). Psychological intervention to modify anxiety, depression and quality of life in patients with an implantable pacemaker. Psychology 7, 374–381. doi: 10.4236/psych.2016.73040
Fischer, F. (2019). L’éthique by design du numérique: généalogie d’un concept. Sciences du Design 10, 61–67. doi: 10.3917/sdd.010.0061
Fishkin, J. S. (1991). Democracy and deliberation: New directions for democratic reform. Yale, USA: Yale University Press.
Flores, M., Glusman, G., Brogaard, K., Price, N. D., and Hood, L. (2013). P4 medicine: how systems medicine will transform the healthcare sector and society. Pers. Med. 10, 565–576. doi: 10.2217/PME.13.57
Foot, P. (1985). Utilitarianism and the Virtues. Mind. XCIV, 196–209. doi: 10.1093/mind/XCIV.374.196
Fournier, C., Bourgeois, I., and Naiditch, M. (2018). Action de Santé Libérale En Équipe (Asalée): Un Espace de Transformation Des Pratiques En Soins Primaires. Questions d’économie de La Santé 232, 1–8.
Fung, A. (2007). “Minipublics: deliberative designs and their consequences” in Deliberation, participation and democracy: can the people govern? 159–183. London: Palgrave Macmillan UK.
Gaborit, É., Terral, P., Génolini, J.-P., and Forté, L. (2021). Self-reporting in TPE: valuing biographies adjusted to the clinical register. Sante Publique 33, 359–368. doi: 10.3917/spub.213.0359
Gilligan, C. (1993). In a different voice: Psychological theory and Women’s development. Harvard, USA: Harvard University Press.
Glaser, Barney G., and Strauss, Anselm L.. (1967). “The discovery of grounded theory: strategies for qualitative research.” New York, Adline de Gruyter 17:364.
Goodin, R. E., and Dryzek, J. S. (2006). Deliberative impacts: the macro-political uptake of Mini-publics. Polit. Soc. 34, 219–244. doi: 10.1177/0032329206288152
Goodrich, J. (2018). Why experience-based co-design improves the patient experience. J. Health Des. 3, 84–85. doi: 10.21853/JHD.2018.45
Green, B. (2021). The contestation of tech ethics: a sociotechnical approach to technology ethics in practice. J. Soc. Comput. 2, 209–225. doi: 10.23919/JSC.2021.0018
Greenhalgh, T., A’Court, C., and Shaw, S. (2017). Understanding heart failure; explaining telehealth – a hermeneutic systematic review. BMC Cardiovasc. Disord. 17:156. doi: 10.1186/s12872-017-0594-2
Greenhalgh, T., Hinton, L., Finlay, T., Macfarlane, A., Fahy, N., Clyde, B., et al. (2019). Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot. Health Expect. 22, 785–801. doi: 10.1111/hex.12888
Greenhalgh, T., and Russell, J. (2010). Why do evaluations of eHealth programs fail? An alternative set of guiding principles. PLoS Med. 7:e1000360. doi: 10.1371/journal.pmed.1000360
Grosjean, S., Bonneville, L., and Redpath, C. (2019). The design process of an mHealth technology: the communicative constitution of patient engagement through a participatory design workshop. ESSACHESS – J. Commun. Stud. 12, 5–26.
Gross, O., and Gagnayre, R. (2013). Hypothèse d’un modèle théorique du patient-expert et de l’expertise du patient: processus d’élaboration. Rech. Qual. 15, 147–175.
Guchet, X. (2016). L’éthique Des Techniques, Entre Réflexivité et Instrumentalisation. Revue française d'éthique appliquée 2, 8–10. doi: 10.3917/rfeap.002.0008
Habermas, J. (1971). “Technology and science as ideology” in Knowledge critical concepts. (eds.) N. Stehr and R. Grundmann, vol. 4
Hahn, D. L., Hoffmann, A. E., Felzien, M., LeMaster, J. W., Jinping, X., and Fagnan, L. J. (2017). Tokenism in Patient Engagement. Fam. Pract. 34, 290–295. doi: 10.1093/fampra/cmw097
Haraway, D. (1988). Situated knowledges: the science question in feminism and the privilege of partial perspective. Fem. Stud. 14, 575–599. doi: 10.2307/3178066
Harding, S. (2013). “Rethinking standpoint epistemology: What is ‘strong objectivity’?” in feminist epistemologies, 49–82. London, UK: Routledge.
Hejoaka, F., Simon, E., Halloy, A., and Arborio, S. (2020). Définir les savoirs expérientiels en santé: une revue de la littérature en sciences humaines et sociales. Questions de communication. Série actes 40:49.
Hunyadi, M. (2017). “Democracy beyond liberalism: for a ‘modes de vie’ politic” in The crisis conundrum: how to reconcile economy and society. ed. M. Magatti (Cham: Springer International Publishing), 219–231.
Ihde, D. (1990). Technology and the lifeworld: from garden to earth Indiana University Press Available at: https://iupress.org/9780253205605/technology-and-the-lifeworld/.
Jobin, A., Ienca, M., and Vayena, E. (2019). The global landscape of AI ethics guidelines. Nat. Mach. Intell. 1, 389–399. doi: 10.1038/s42256-019-0088-2
Kiran, A. H., Oudshoorn, N., and Verbeek, P.-P. (2015). Beyond checklists: toward an ethical-constructive technology assessment. J. Responsible Innov. 2, 5–19. doi: 10.1080/23299460.2014.992769
Kirsh, D. (2013). Embodied cognition and the magical future of interaction design. ACM Trans. Comput. Hum. Interact. 20, 1–30. doi: 10.1145/2442106.2442109
Lafont, C. (2015). Deliberation, participation, and democratic legitimacy: should deliberative Mini-publics shape public policy? J Polit Philos 23, 40–63. doi: 10.1111/jopp.12031
Latour, B. (2002). Morality and technology. Translated by Couze Venn. Theory Cult. Soc. 19, 247–260. doi: 10.1177/026327602761899246
Lehoux, P., and Williams-Jones, B. (2007). Mapping the integration of social and ethical issues in health technology assessment, vol. 9. International journal of technology assessment in health.
Liljeroos, M., Thylén, I., and Strömberg, A. (2020). Patients’ and nurses’ experiences and perceptions of remote monitoring of implantable cardiac defibrillators in heart failure: cross-sectional, descriptive, mixed methods study. J. Med. Internet Res. 22:e19550. doi: 10.2196/19550
Lin, T.-A., and Chen, P.-H. C. (2022). Artificial intelligence in a structurally unjust society. Fem. Philos. Q. 8, 1–31. doi: 10.5206/fpq/2022.3/4.14191
Lobet-Maris, C., Grandjean, N., De Vos, N., Thiry, F., Pagacz, P., and Pieczynski, S. (2019). Dealing with constraints: when ethics becomes bricolage. Revue francaise d’ethique appliquee 7, 72–88. doi: 10.3917/rfeap.007.0072
Locock, L., and Boaz, A. (2019). Drawing straight lines along blurred boundaries: qualitative research, patient and public involvement in medical research, co-production and co-design. Evid. Policy: J. Res. Debate Pract. 15, 409–421. doi: 10.1332/174426419X15552999451313
Lupton, D. (2016). The diverse domains of quantified selves: self-tracking modes and Dataveillance. Econ. Soc. 45, 101–122. doi: 10.1080/03085147.2016.1143726
Ménissier, T. (2023). Les Quatre Éthiques de l’intelligence Artificielle: Comment Se Constitue l’évaluation Éthique d’un Système Technique Global. Revue d’Anthropologie Des Connaissances 17, 1–21. doi: 10.4000/rac.29961
Mill. (1863). Utilitarianism. Available at: https://www.utilitarianism.com/mill1.htm.
Millenson, M. L. (2011). Spock, feminists, and the fight for participatory medicine: a history | journal of participatory medicine. J. Particip. Med. 3:e27
Moore, S. L. (2010). Ethics by design: Strategic thinking and planning for exemplary performance, responsible results, and societal accountability Amherst USA: Human Resource Development.
Morozov, E. (2014). To save everything, click Here: the folly of technological solutionism. J. Inf. Policy 4, 173–175.
Muller, M. J., and Kuhn, S. (1993). Participatory design. Commun. ACM 36, 24–28. doi: 10.1145/153571.255960
Munn, L. (2023). The uselessness of AI ethics. AI Ethics 3, 869–877. doi: 10.1007/s43681-022-00209-w
Nissenbaum, H., and Patterson, H. (2016). “Biosensing in context: health privacy in a connected world” in Quantified: Biosensing Technologies in Everyday Life. (ed.) D. Nafus, vol. 79 (Cambridge, Massachusetts: MIT University Press).
Nussbaum, M. (1999). Women and equality: the capabilities approach. Int’l Lab. Rev. 138, 227–245. doi: 10.1111/j.1564-913X.1999.tb00386.x
Nussbaum, M. (2020). “The capabilities approach and the history of philosophy” in The cambridge handbook of the capability approach. (eds.) E. Chiappero-Martinetti, S. Osmani, and M. Qizilbash (Cambridge, UK: Cambridge University Press), 13–39.
Ocloo, J., and Matthews, R. (2016). From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual. Saf. 25, 626–632. doi: 10.1136/bmjqs-2015-004839
Palm, E., and Hansson, S. O. (2006). The case for ethical technology assessment (eTA). Technol. Forecast. Soc. Chang. 73, 543–558. doi: 10.1016/j.techfore.2005.06.002
Papoutsi, C., Wherton, J., Shaw, S., Morrison, C., and Greenhalgh, T. (2020). Putting the social Back into sociotechnical: case studies of co-Design in Digital Health. J. Am. Med. Inform. Assoc. ocaa197, 284–293. doi: 10.1093/jamia/ocaa197
Petit, E., and Ballet, J. (2023). Valuation and emotion according to John Dewey. Camb. J. Econ. 47, 1019–1036. doi: 10.1093/cje/bead040
Pols, J., and Moser, I. (2009). Cold technologies versus warm care? On affective and social relations with and through care technologies. Alter 3, 159–178. doi: 10.1016/j.alter.2009.01.003
Provencher, V., Baillargeon, D., Abdulrazak, B., Boissy, P., Levasseur, M., Delli-Colli, N., et al. (2022). Developing a one-stop platform transportation planning service to help older adults move around in their community where, when, and how they wish: protocol for a living lab study. JMIR Res. Protoc. 11:e33894. doi: 10.2196/33894
Quéré, Pierre-Vincent. (2019). “Les mathématiques dans la formation des ingénieurs et sur leur lieu de travail: études et propositions (cas de la France).” Phdthesis, Université de Bretagne occidentale – Brest. Available at: https://theses.hal.science/tel-02281937.
Roby, C. (2017). Humanités et SHS dans les écoles d’ingénieurs en France: une approche sociohistorique. Tréma 47, 17–34. doi: 10.4000/trema.3636
Sacchini, D., Virdis, A., Refolo, P., Pennacchini, M., and de Paula, I. C. (2009). Health technology assessment (HTA): ethical aspects. Med. Health Care Philos. 12, 453–457. doi: 10.1007/s11019-009-9206-y
Sætra, H. S. (2023). Technology and sustainable development: The promise and pitfalls of techno-solutionism Taylor & Francis.
Sanders, E. B.-N. (2002). “From user-centered to participatory design approaches” in Design and the social sciences. ed. J. Frascara, vol. 20020425 (Boca Raton, USA: Contemporary Trends Institute Series. CRC Press), 1–8.
Schön, D. A. (2017). The reflective practitioner: How professionals think in action. London, UK: Routledge.
Schwingrouber, J., Loschi, A., Gentile, S., and Colson, S. (2021). Étude exploratoire de la perception des parties prenantes hospitalières vis-à-vis de l’implantation des infirmiers en pratique avancée. Rech. Soins Infirm. 145, 104–121. doi: 10.3917/rsi.145.0104
Sendra, A., Grosjean, S., and Bonneville, L. (2022). Co-constructing experiential knowledge in health: the contribution of people living with Parkinson to the co-design approach. Qual. Health Commun. 1, 101–121. doi: 10.7146/qhc.v1i1.124110
Shankar, K., Jean Camp, L., Connelly, K. H., and Huber, L. (2011). Aging, privacy, and home-based computing: development of a framework for design. IEEE Pervasive Comput 11, 46–54. doi: 10.1109/MPRV.2011.19
Singer, P. (2024). “Ethics” in Encyclopædia Britannica Available at: https://www.britannica.com/topic/ethics-philosophy
Slattery, P., Saeri, A. K., and Bragge, P. (2020). Research co-design in health: a rapid overview of reviews. Health Res. Policy Syst. 18:17. doi: 10.1186/s12961-020-0528-9
Smit, J.-A. R., Mostert, M., and van Delden, J. J. M. (2022). Protecting privacy while optimizing the use of (health)data: the importance of measures and safeguards. Am. J. Bioeth. 22, 79–81. doi: 10.1080/15265161.2022.2075973
Steen, M. (2013). Co-design as a process of joint inquiry and imagination. Des. Issues 29, 16–28. doi: 10.1162/DESI_a_00207
Ten Have, H. (2004). Ethical perspectives on health technology assessment. Int. J. Technol. Assess. Health Care 20, 71–76. doi: 10.1017/S0266462304000819
Tessier, C. (2021). “Éthique et IA: Analyse et Discussion” in CNIA 2021: Conférence Nationale En Intelligence Artificielle. HAL archive, 22–29.
Vaismoradi, M., Turunen, H., and Bondas, T. (2013). Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs. Health Sci. 15, 398–405. doi: 10.1111/nhs.12048
Van Hees, M. (2013). Rights, goals, and capabilities. Politics Philos. Econ. 12, 247–259. doi: 10.1177/1470594X12447787
Verbeek, P.-P. (2005). What things do: philosophical reflections on technology, agency, and design. State College, USA: Penn State Press.
Verbeek, P.-P. (2008). “Morality in design: design ethics and the morality of technological artifacts” in Philosophy and design: From engineering to architecture. eds. P. Kroes, P. E. Vermaas, A. Light, and S. A. Moore (Dordrecht: Springer Netherlands), 91–103.
Vokinger, K. N., Feuerriegel, S., and Kesselheim, A. S. (2021). Mitigating Bias in machine learning for medicine. Commun. Med. 1, 1–3. doi: 10.1038/s43856-021-00028-w
World Health Organization. (2021). “Ethics and governance of artificial intelligence for health: WHO guidance.” Geneva: World Health Organization. Available at: https://apps.who.int/iris/rest/bitstreams/1352854/retrieve.
Zacklad, M., and Rouvroy, A. (2022). L’éthique située de l’IA et ses controverses. Revue française des sciences de l’information et de la communication 25, 1–22. doi: 10.4000/rfsic.13204
Zamenopoulos, T., and Alexiou, K.. (2018). Co-design as collaborative research. Connected Communities Foundation Series. Bristol: Bristol University/AHRC Connected Communities Programme.
Keywords: ethics, participatory approaches, co-design, affect stories, health technologies, health innovation
Citation: Davat A, Martin-Juchat F and Ménissier T (2024) Co-design with affect stories and applied ethics for health technologies. Front. Commun. 9:1327711. doi: 10.3389/fcomm.2024.1327711
Edited by:
Maria Cherba, University of Ottawa, CanadaReviewed by:
Sana Boudhraa, Université du Québec à Montréal, CanadaJohanne Stümpel, University of Bonn, Germany
Copyright © 2024 Davat, Martin-Juchat and Ménissier. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fabienne Martin-Juchat, fabienne.martin-juchat@univ-grenoble-alpes.fr
 Ambre Davat
Ambre Davat Fabienne Martin-Juchat1,2*
Fabienne Martin-Juchat1,2*  Thierry Ménissier
Thierry Ménissier