Assessing the influence of gastrocnemius reconstruction on stress distribution of femoral tumor rotating hinge knee prosthesis via finite element analysis
- 1Department of Musculoskeletal Tumor, People’s Hospital, Peking University, Beijing, China
- 2Beijing Key Laboratory of Musculoskeletal Tumor, Beijing, China
Background: After femoral oncological knee arthroplasty, some patients suffer from rotating axis fracture, which significantly impacts the life span of the rotating hinge knee (RHK) prosthesis. This research aimed to analyze the biomechanical response of anatomical gastrocnemius reconstruction and assess whether it could reduce the risk of rotating axis breakage by finite element (FE) analysis.
Methods: A femur-prosthesis-tibia FE model was established using the data from CT scans. The mechanical properties of the RHK implant were quantitatively compared before and after gastrocnemius reconstruction at 6 angles: 10°, 20°, 30°, 40°, 50°, and 60°.
Results: Our results showed that gastrocnemius reconstruction effectively altered the stress distribution around the rotating axis, considerably relieving the stress in the fracture-prone region. In addition, the peak stress in the rotating axis, bending axis, prosthesis stem, and femoral condyles decreased variably.
Conclusion: In distal femoral resection knee arthroplasty, the rebuilding of gastrocnemius substantially improved the stress distribution within the prosthesis, thereby having the potential to reduce the risk of prosthetic fracture and prolong the overall durability of the prosthesis.
Introduction
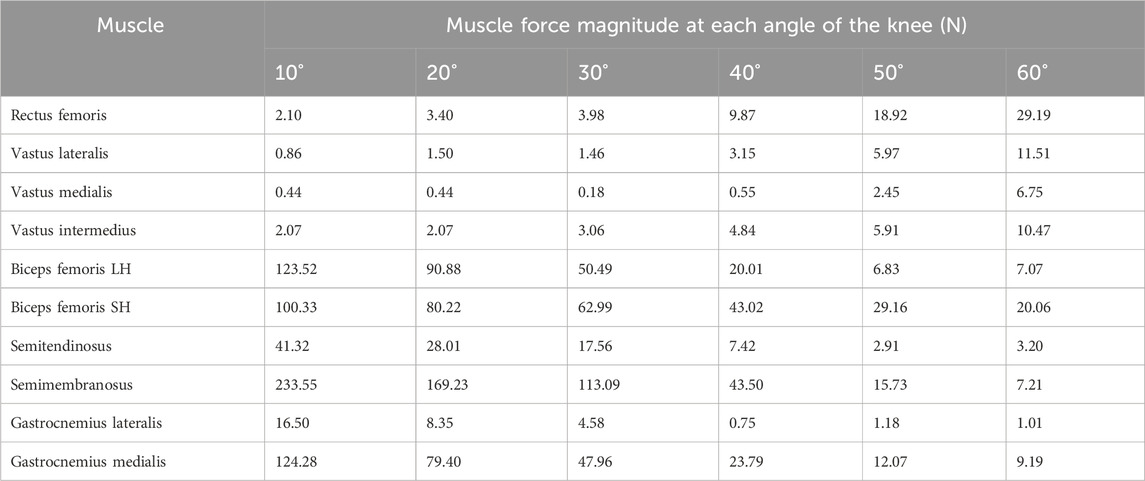
Malignant bone tumors frequently occur in the knee joint, especially the distal femur (Ritter and Bielack, 2010). Over the past 30 years, with advances in medical imaging technology, chemotherapy, and surgery, limb salvage has replaced amputation as the standard treatment for malignant bone tumors (Grimer, 2005; Bielack et al., 2009; Beird et al., 2022). Currently, oncoplastic joint prostheses are widely used to reconstruct large bone defects after tumor resection. They provide immediate postoperative stability, early weight-bearing ambulation, and better long-term function (Plötz et al., 2002; Frink et al., 2005). However, endoprosthetic failures remain a significant concern, consisting of structural failure, soft-tissue failure, aseptic loosening, infection, and tumor progression (Henderson et al., 2011; Haijie et al., 2018). In some cases, we have noted prosthetic rotating axis fractures, which occur primarily in the spacer-wrapped area of the axis, greatly affecting the longevity of the prosthetic implants (Figure 1). This may be related to anterior shear forces exerted on the proximal tibia by quadriceps contraction (Carter et al., 2017). Rotating axis breakage belongs to structural prosthesis failure, but its injury mechanism and improvement methods have been rarely described in the medical literature.
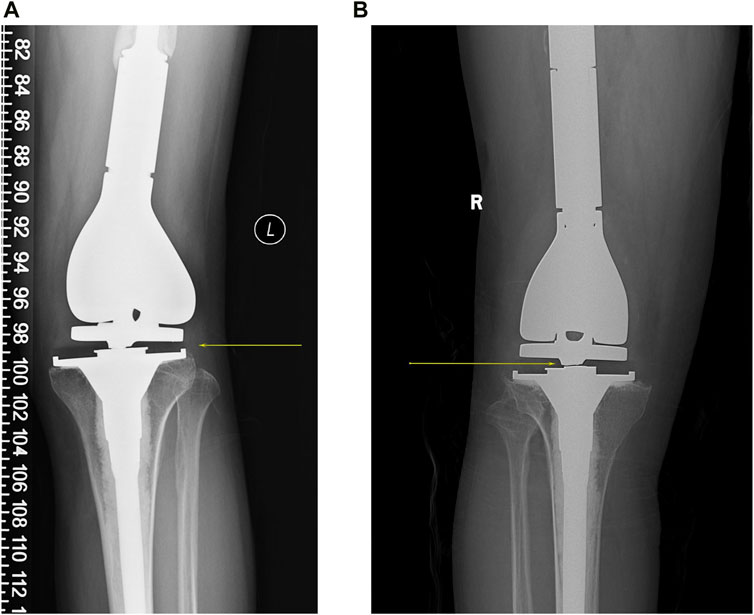
Figure 1. Two cases of rotating axis fractures of the tumor knee prosthesis, with yellow arrows showing the fracture sites. (A) A 36-year-old man had a prosthesis inserted for an undifferentiated sarcoma of the distal left femur. Subsequent to 5 years, the rotating axis fractured, requiring a comprehensive knee revision. (B) A 42-year-old man underwent the replacement of an artificial prosthesis due to the giant cell tumor of bone in his right knee. After 6 years, a rotating axis fracture within the prosthesis led him to a revision of the knee prosthesis.
The gastrocnemius is a biarticular muscle with multiple functions for the knee and ankle (Winter, 1980). Heads of the gastrocnemius originate from the medial and lateral femoral condyles, travel downward to form the Achilles tendon with the soleus, and terminate at the calcaneal tuberosity. As a knee flexor, the gastrocnemius antagonizes the quadriceps in synergy with the hamstrings to maintain knee stability. Previous studies have shown that co-contraction of the gastrocnemius with the quadriceps can effectively increase joint compression and reduce anterior tibial translation (Durselen et al., 1995; Sherbondy et al., 2003; Ali et al., 2014; Morgan et al., 2014). Therefore, we hypothesized that it would be feasible to reconstruct the gastrocnemius anatomically to relieve rotating axis stress concentration in distal femoral tumor surgery. In this research, a finite element (FE) model of the lower limb, including a rotating hinge knee (RHK) prosthesis and bone, was established to quantify the impact of gastrocnemius reconstruction on the rotating axis and other prosthesis components during gait.
Materials and methods
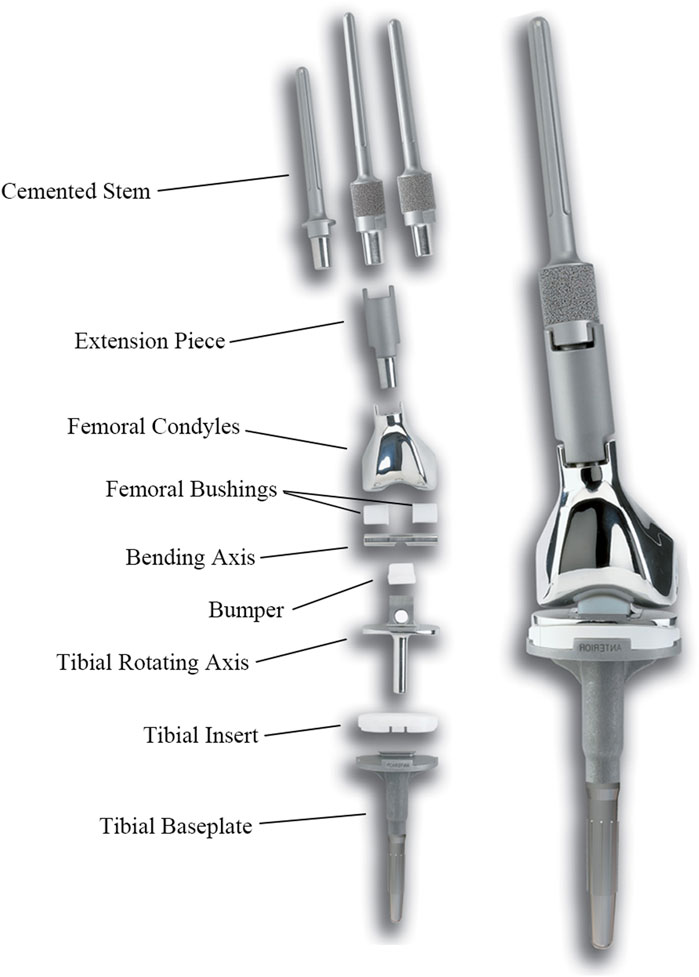
The femoral tumor RHK prosthesis was obtained from Beijing Lidakang Company and comprised several components, including the femoral stem, bending axis, rotating axis, tibial baseplate, and UHMWPE spacers (Figure 2). This semi-restrictive prosthesis provides two movable surfaces of flexion/extension and internal/external rotation. The bending axis aligns with the femoral internal and external condylar lines, while the rotating axis is on the line through the middle axis of the tibia. The UHMWPE spacers isolate the intermetallic friction area of the prosthesis, thereby effectively diminishing rotational stress between the components. The clinical outcomes of this prosthesis have been observed to be notably satisfactory, underscoring its efficacy in clinical practice.
Finite element model construction
This research included a healthy male volunteer (height = 180 cm, weight = 80 kg) after rigorous evaluation and screening parameters, which excluded other knee-related conditions, such as knee deformity and trauma. Signed informed consent was acquired from the volunteer before the experimental program.
Subsequently, the volunteer’s knee joints were carefully scanned through a spiral CT machine in a straightened position, covering the entire length of both lower limbs. For this experiment, the right knee joint data was utilized, and the medical modeling software Mimics (Materialise, Leuven, Belgium) was used to extract the detailed geometric characteristics of the femur and tibia. Furthermore, the data was further refined and smoothed via the engineering software Geomagic (Raindrop Company, United States), which provided comprehensive and accurate solid geometry models of the femur and tibia for later analyses.
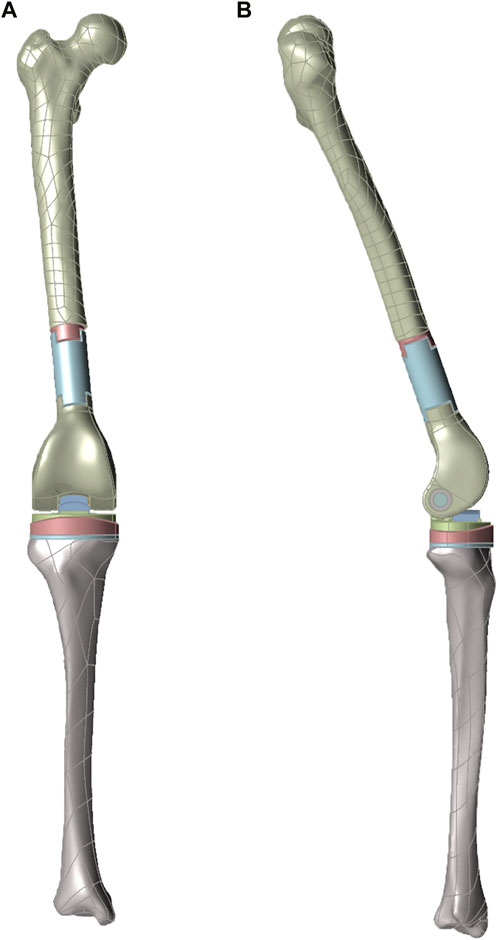
Following the principle of distal femur tumor resection arthroplasty, the femur segment was removed from a plane about 3–5 cm away from the tumor boundary to prevent tumor recurrence, and the tibia osteotomy was perpendicular to its mechanical axis. Within the model, the midpoint of the knee and ankle joints were marked, and the line connecting the two points was identified as the tibial mechanical axis. For assembling the tumor knee prosthesis, the force line of the lower end of the prosthesis was parallel to the tibial mechanical axis. The acquired 3D model was then imported into ABAQUS 6.14 (Simulia, Providence, RI, United States) for adaptive meshing, and the geometry was divided with a target cell size of 2 mm. Lastly, the mesh file was subjected to static simulation (Figure 3).
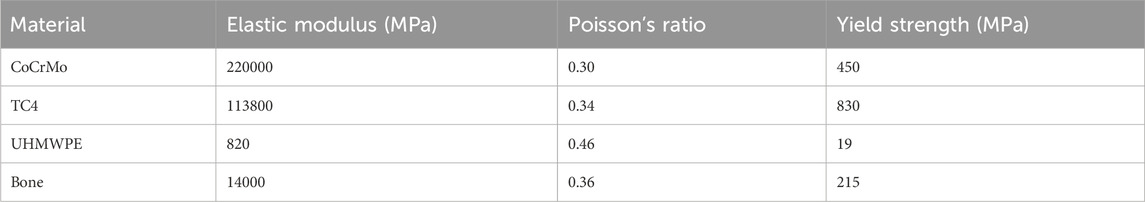
Material properties
The femoral condyles, tibial plateau, bending, and rotating axis of the prosthesis were made of CoCrMo, while the femoral end prosthesis stem and extension were made of TC4 alloy. Table 1 lists the materials used, assigned based on the previous literature (Zhang et al., 2020). The normal and tangential behaviors were set as hard and punishing contacts, respectively. The friction coefficient between CoCrMo and UHMWPE was set at 0.04 during the simulation (Yang and Lin, 2001).
Boundary conditions and loading
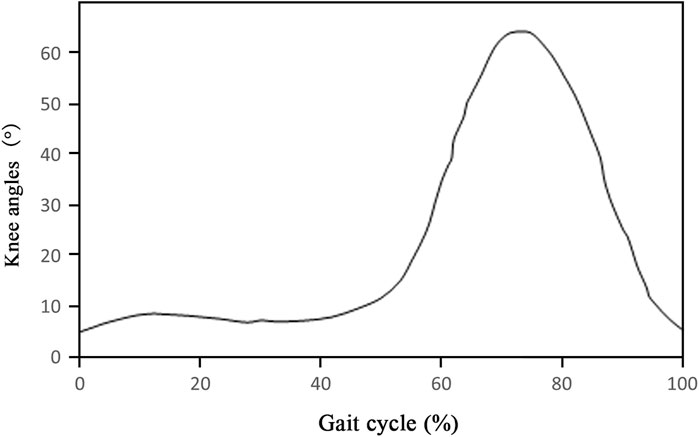
In order to accurately simulate the mechanical behavior characteristics of the knee joint during gait, the primary knee flexor and extensor muscles were considered in the model, including the quadriceps femoris, biceps femoris, semitendinosus, semimembranosus, and gastrocnemius. The knee motion angle versus gait curve after oncologic knee prosthesis replacement was evaluated according to previous literature (Figure 4), which showed that the maximal flexion reached approximately 60° (Okita et al., 2013). In this study, six angles were selected to simulate knee gait after knee prosthesis replacement. Meanwhile, the exact positions of the aforementioned muscles and the muscle force values at each angle were determined based on the anatomical atlas and relevant studies (Table 2) (White et al., 1989; Trinler et al., 2019). The peak Von Mises stress of the prosthesis and peripheral bone tissues was calculated under the loading conditions.
Results
Stress distribution of rotating axis
The FE model allowed the knee to be stretched from 60° to 10° at 10° intervals, and the stress distribution of the rotating axis before and after gastrocnemius reconstruction was quantified (Figures 5A–F). Before reconstruction, the peak stress was mainly localized in the bushing contact and tibial spacer-wrapped areas, consistent with the actual area of the rotating axis breakage in clinical cases. However, after reconstructing the gastrocnemius, stress was significantly reduced within the tibial spacer-wrapped region. Of the six angles, the unreconstructed group indicated the highest stress at 10°, reaching a peak of 75.52 MPa. Conversely, in the reconstructed group, the maximum stress occurred at 60°, with a peak value of 29.37 MPa. Comparison between the two sets of stress demonstrated that gastrocnemius restoration reduced the peak stress of the rotating axis at all angles, with the most notable reduction at 10°, from 75.52 MPa to 16.46 MPa (Figure 6A).
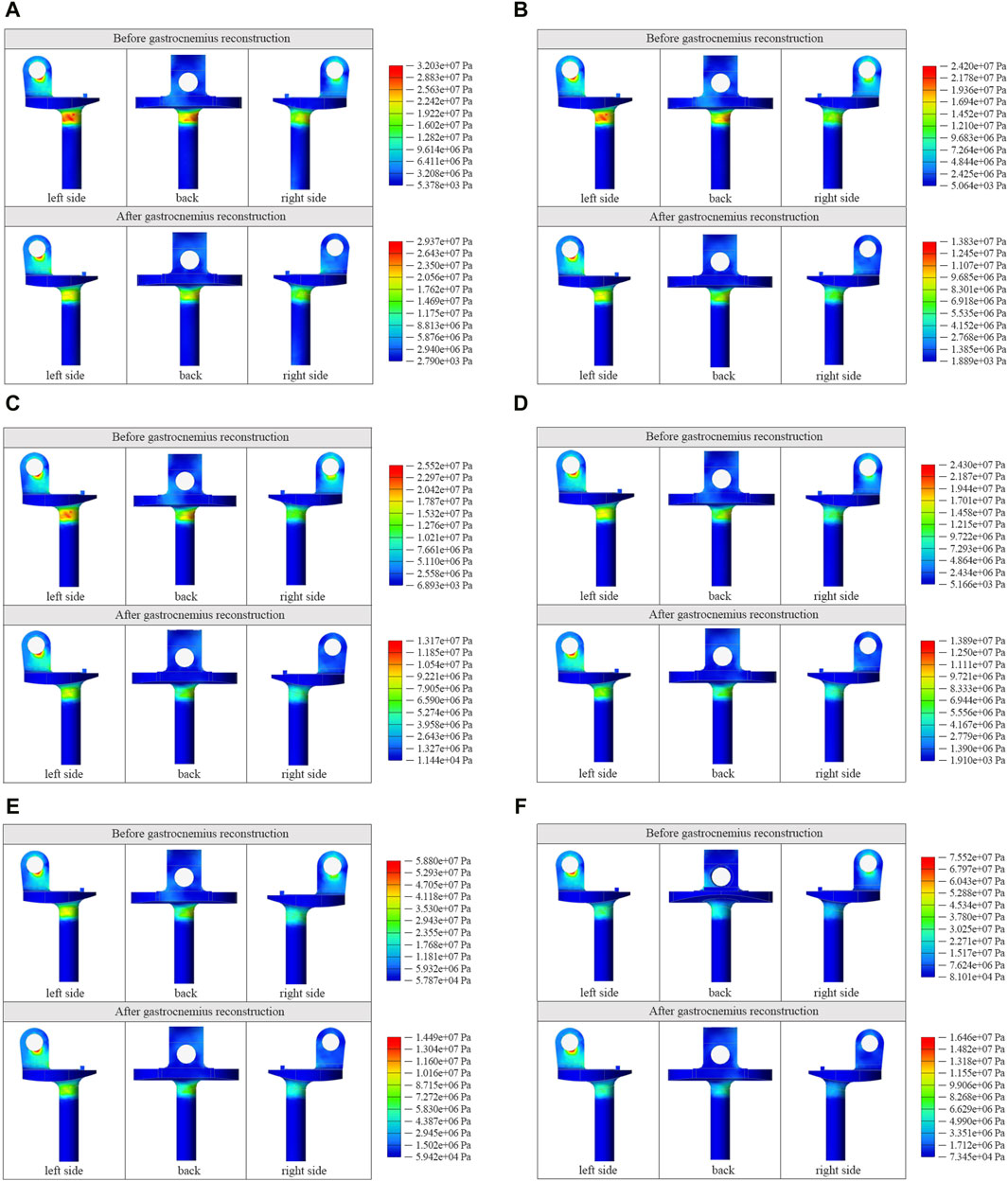
Figure 5. Cloud view of stress distribution in the rotating axis at 60° (A), 50° (B), 40° (C), 30° (D), 20° (E), and 10° (F) before and after gastrocnemius reconstruction.
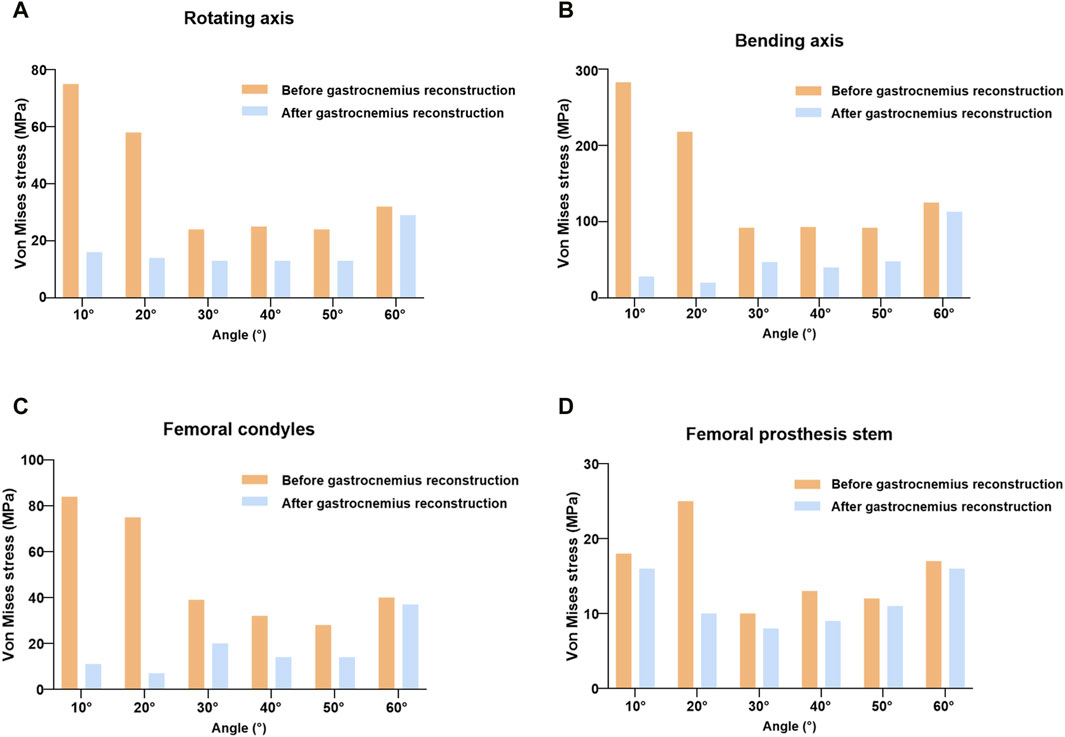
Figure 6. Comparison of peak stress in the rotating axis (A), bending axis (B), femoral condyles (C), and femoral prosthesis stem (D) before and after gastrocnemius reconstruction.
Stress distribution in other prosthetic components
Fracture rates of 5%–7% have been observed in oncoplastic knee prostheses, with the prosthesis stem and femoral condyles being common fracture sites (Morgan et al., 2006; Pala et al., 2016). We extracted and compared the peak stress in the bending axis, femoral condyles, and femoral prosthesis stem at different angles. As shown in Figures 6B–D, the trends of stress change in the bending axis and femoral condyles were similar to that observed in the rotating axis. The inclusion of gastrocnemius loading significantly reduced the peak stress levels during knee gait, with the most pronounced effect at 10°, where the bending axis and peak femoral condylar stress decreased from 283.8 to 28.33 Mpa and 84.26 to 11.95 Mpa, respectively. For the prosthesis stem, the maximum peak stress before reconstruction occurred at 20° with 25.21 Mpa and decreased to 10.9 Mpa after gastrocnemius reconstruction. The peak stress of the stem decreased to varying degrees at the other five angles.
Discussion
This study compares the mechanical environment of the RHK prosthesis before and after rebuilding gastrocnemius by the FE method. To the authors’ knowledge, this is the first to investigate gastrocnemius reconstruction in femoral tumor knee arthroplasty.
In surgical management of malignant bone tumors, it is necessary to remove the involved muscles and soft tissues surrounding the diseased bone to ensure complete resection (DiCaprio and Friedlaender, 2003). Previous studies are mainly focused on the functional restoration of knee extensors and the provision of soft tissue cover (Hobusch et al., 2016; Zan et al., 2023). There is a consensus that robust extensors are critical for post-reconstruction function. On the contrary, rebuilding the flexor muscles, including the gastrocnemius, is usually neglected in distal femoral surgery.
Compared to normal knee arthroplasty, tumor knee arthroplasty presents unique challenges. The incidence of complications related to implant failure ranges from 21.6% to 61% (Bus et al., 2017; Zhang et al., 2018; Christ et al., 2023). Of these, prosthetic breakage is an important cause of revision, which could be attributed to the material used and high mechanical stress. We have noticed some cases of rotating axis breakage. The mechanism of injury may be due to excessive contraction of the quadriceps muscle during knee extension, causing the tibia to move ahead and driving the rotating axis forward. This can further engender localized stress concentrations, heightening the susceptibility to regional structural failure.
Several studies have shown that increased gastrocnemius activation contributes to decreased anterior tibial translation and anterior cruciate ligament (ACL) loading (Ali et al., 2014; Morgan et al., 2014). In musculoskeletal modeling of single-leg landings, the researchers discovered that with co-activation of the quadriceps, enhanced gastrocnemius forces led to stronger joint compression. As a result, increased friction between the knee joints caused by joint compression limited anterior tibial translation, reducing ACL strain (Morgan et al., 2014). Furthermore, another simulation study showed that elevated gastrocnemius activation decreased the peak force of anterior tibial translation, hence lowering the risk of non-contact ACL injury (Ali et al., 2014). Indirect studies have also evaluated the relationship between the gastrocnemius and ACL by detecting muscle activation in ACL-deficient patients. Lass et al. reported that gastrocnemius activity increased in ACL-deficient individuals, indirectly indicating that the gastrocnemius acts as an ACL synergist (Lass et al., 1991). Nevertheless, some investigations have demonstrated that the gastrocnemius muscle can function as an ACL antagonist (Elias et al., 2003; Adouni et al., 2016). When the gastrocnemius muscle contracts and expands in size, it pushes the tibia forward. However, at sufficient gastrocnemius stimulation level, the joint compression is expected to be enough to counter the effects of muscle expansion and restrict the anterior tibial movement (Fleming et al., 2001; Teng et al., 2021).
Consistent with the above theories, our findings suggested that gastrocnemius restoration considerably affected the mechanical environment of the prosthesis. Prior to reconstruction, the stress was concentrated in the area surrounded by the spacer in the rotating axis, which corresponded to the clinical fracture location. The regeneration of gastrocnemius greatly reduced the stress concentration in the fracture-prone region. In RHK prostheses, hinge structures such as the axis of rotating and bending replace the role of ACL, limiting the upper tibia’s anterior movement. As a consequence, gastrocnemius rebuilding provides enough joint compression as well as posterior shear force that resist the anterior tibial translation caused by the quadriceps muscle’s anterior shear force, lowering the strain on the rotating axis. Furthermore, the peak stress in other prosthetic components was reduced to varying degrees after reconstruction, which may prolong the effective period of the artificial knee joint.
Soft tissue reconstruction in endoprosthetic replacement can be accomplished in a variety of ways, including (a) direct fixation to the implant with screws or sutures, (b) synthetic materials, such as LARS ligaments and Trevira tube, and (c) biological augmentation with or without synthetic components (Ek et al., 2011). Reconstruction of the gastrocnemius can be performed in the manners described above, increasing the posterior soft tissue coverage and enhancing prosthetic joint stability.
There are some shortcomings in this study that need to be improved in subsequent experiments. Six angles (10°, 20°, 30°, 40°, 50°, and 60°) were selected to statically simulate the gait, and further refinement of gait angles is required for dynamic simulation. In addition, since the quadriceps and flexor muscles are often partially resected during knee tumor resection surgery, the changes in muscle force distribution need further confirmation.
Conclusion
This is the first study to propose gastrocnemius reconstruction in tumor knee arthroplasty and verify its feasibility by FE analysis. According to the results, anatomical gastrocnemius restoration in distal femoral arthroplasty can considerably relieve stress concentration on the rotating axis, potentially lowering the risk of prosthetic fracture.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Commttee of Peking University People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JJ: Data curation, Investigation, Writing–original draft. FZ: Investigation, Methodology, Writing–review and editing. XT: Methodology, Supervision, Validation, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The National Natural Science Foundation of China (No. 82373140).
Acknowledgments
The authors would like to thank all the reviewers who participated in the review, as well as MJEditor (www.mjeditor.com) for providing English editing services during the preparation of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adouni, M., Shirazi-Adl, A., and Marouane, H. (2016). Role of gastrocnemius activation in knee joint biomechanics: gastrocnemius acts as an ACL antagonist. Comput. Methods Biomech. Biomed. Engin 19, 376–385. doi:10.1080/10255842.2015.1032943
Ali, N., Andersen, M. S., Rasmussen, J., Robertson, D. G. E., and Rouhi, G. (2014). The application of musculoskeletal modeling to investigate gender bias in non-contact ACL injury rate during single-leg landings. Comput. Methods Biomechanics Biomed. Eng. 17, 1602–1616. doi:10.1080/10255842.2012.758718
Beird, H. C., Bielack, S. S., Flanagan, A. M., Gill, J., Heymann, D., Janeway, K. A., et al. (2022). Osteosarcoma. Nat. Rev. Dis. Prim. 8, 77. doi:10.1038/s41572-022-00409-y
Bielack, S., Jürgens, H., Jundt, G., Kevric, M., Kühne, T., Reichardt, P., et al. (2009). Osteosarcoma: the COSS experience. Cancer Treat. Res. 152, 289–308. doi:10.1007/978-1-4419-0284-9_15
Bus, M. P. A., van de Sande, M. A. J., Fiocco, M., Schaap, G. R., Bramer, J. A. M., and Dijkstra, P. D. S. (2017). What are the long-term results of MUTARS® modular endoprostheses for reconstruction of tumor resection of the distal femur and proximal tibia? Clin. Orthop. Relat. Res. 475, 708–718. doi:10.1007/s11999-015-4644-8
Carter, J. C., Sturnick, D. R., Vacek, P. M., DeSarno, M. J., Argentieri, E. C., Slauterbeck, J. R., et al. (2017). Relationship between geometry of the extensor mechanism of the knee and risk of anterior cruciate ligament injury. J. Orthop. Res. 35, 965–973. doi:10.1002/jor.23366
Christ, A. B., Chung, B. C., Urness, M., Mayer, L. W., Gettleman, B. S., Heckmann, N. D., et al. (2023). Clinical outcomes of cemented distal femur replacements with all-polyethylene tibial components for oncologic indications. World J. Orthop. 14, 218–230. doi:10.5312/wjo.v14.i4.218
DiCaprio, M. R., and Friedlaender, G. E. (2003). Malignant bone tumors: limb sparing versus amputation. J. Am. Acad. Orthop. Surg. 11, 25–37. doi:10.5435/00124635-200301000-00005
Durselen, L., Claes, L., and Kiefer, H. (1995). The influence of muscle forces and external loads on cruciate ligament strain. Am. J. Sports Med. 23, 129–136. doi:10.1177/036354659502300122
Ek, E. W., Rozen, W. M., Ek, E. T., and Rudiger, H. A. (2011). Surgical options for reconstruction of the extensor mechanism of the knee after limb-sparing sarcoma surgery: an evidence-based review. Archives Orthop. Trauma Surg. 131, 487–495. doi:10.1007/s00402-010-1158-4
Elias, J. J., Faust, A. F., Chu, Y. H., Chao, E. Y., and Cosgarea, A. J. (2003). The soleus muscle acts as an agonist for the anterior cruciate ligament. An in vitro experimental study. Am. J. Sports Med. 31, 241–246. doi:10.1177/03635465030310021401
Fleming, B. C., Renstrom, P. A., Ohlen, G., Johnson, R. J., Peura, G. D., Beynnon, B. D., et al. (2001). The gastrocnemius muscle is an antagonist of the anterior cruciate ligament. J. Orthop. Res. 19, 1178–1184. doi:10.1016/s0736-0266(01)00057-2
Frink, S. J., Rutledge, J., Lewis, V. O., Lin, P. P., and Yasko, A. W. (2005). Favorable long-term results of prosthetic arthroplasty of the knee for distal femur neoplasms. Clin. Orthop. Relat. Res. 438, 65–70. doi:10.1097/01.blo.0000180056.84593.47
Grimer, R. J. (2005). Surgical options for children with osteosarcoma. Lancet Oncol. 6, 85–92. doi:10.1016/s1470-2045(05)01734-1
Haijie, L., Dasen, L., Tao, J., Yi, Y., Xiaodong, T., and Wei, G. (2018). Implant survival and complication profiles of endoprostheses for treating tumor around the knee in adults: a systematic review of the literature over the past 30 years. J. Arthroplasty 33, 1275–1287.e3. doi:10.1016/j.arth.2017.10.051
Henderson, E. R., Groundland, J. S., Pala, E., Dennis, J. A., Wooten, R., Cheong, D., et al. (2011). Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J. Bone Jt. Surg. Am. 93, 418–429. doi:10.2106/jbjs.J.00834
Hobusch, G. M., Funovics, P. T., Hourscht, C., Domayer, S. E., Puchner, S. E., Dominkus, M., et al. (2016). LARS® band and tube for extensor mechanism reconstructions in proximal tibial modular endoprostheses after bone tumors. Knee 23, 905–910. doi:10.1016/j.knee.2016.04.002
Lass, P., Kaalund, S., leFevre, S., Arendt-Nielsen, L., Sinkjaer, T., and Simonsen, O. (1991). Muscle coordination following rupture of the anterior cruciate ligament. Electromyographic studies of 14 patients. Acta Orthop. Scand. 62, 9–14. doi:10.3109/17453679108993083
Morgan, H. D., Cizik, A. M., Leopold, S. S., Hawkins, D. S., and Conrad, E. U. (2006). Survival of tumor megaprostheses replacements about the knee. Clin. Orthop. Relat. Res. 450, 39–45. doi:10.1097/01.blo.0000229330.14029.0d
Morgan, K. D., Donnelly, C. J., and Reinbolt, J. A. (2014). Elevated gastrocnemius forces compensate for decreased hamstrings forces during the weight-acceptance phase of single-leg jump landing: implications for anterior cruciate ligament injury risk. J. Biomechanics 47, 3295–3302. doi:10.1016/j.jbiomech.2014.08.016
Okita, Y., Tatematsu, N., Nagai, K., Nakayama, T., Nakamata, T., Okamoto, T., et al. (2013). Compensation by nonoperated joints in the lower limbs during walking after endoprosthetic knee replacement following bone tumor resection. Clin. Biomech. (Bristol, Avon.) 28, 898–903. doi:10.1016/j.clinbiomech.2013.08.005
Pala, E., Trovarelli, G., Angelini, A., and Ruggieri, P. (2016). Distal femur reconstruction with modular tumour prostheses: a single Institution analysis of implant survival comparing fixed versus rotating hinge knee prostheses. Int. Orthop. 40, 2171–2180. doi:10.1007/s00264-016-3232-1
Plötz, W., Rechl, H., Burgkart, R., Messmer, C., Schelter, R., Hipp, E., et al. (2002). Limb salvage with tumor endoprostheses for malignant tumors of the knee. Clin. Orthop. Relat. Res. 405, 207–215. doi:10.1097/00003086-200212000-00027
Ritter, J., and Bielack, S. S. (2010). Osteosarcoma. Ann. Oncol. 21 (Suppl. 7), vii320–325. doi:10.1093/annonc/mdq276
Sherbondy, P. S., Queale, W. S., McFarland, E. G., Mizuno, Y., and Cosgarea, A. J. (2003). Soleus and gastrocnemius muscle loading decreases anterior tibial translation in anterior cruciate ligament intact and deficient knees. J. knee Surg. 16, 152–158.
Teng, P. S. P., Leong, K. F., Phua, P. Y. X., and Kong, P. W. (2021). An exploratory study of the use of ultrasound in the measurement of anterior tibial translation under gastrocnemius muscle stimulation. Res. Sports Med. 29, 103–115. doi:10.1080/15438627.2020.1840378
Trinler, U., Schwameder, H., Baker, R., and Alexander, N. (2019). Muscle force estimation in clinical gait analysis using AnyBody and OpenSim. J. Biomech. 86, 55–63. doi:10.1016/j.jbiomech.2019.01.045
White, S. C., Yack, H. J., and Winter, D. A. (1989). A three-dimensional musculoskeletal model for gait analysis. Anatomical variability estimates. J. Biomech. 22, 885–893. doi:10.1016/0021-9290(89)90072-9
Winter, D. A. (1980). Overall principle of lower-limb support during stance phase of gait. J. Biomechanics 13, 923–927. doi:10.1016/0021-9290(80)90162-1
Yang, R. S., and Lin, H. J. (2001). Contact stress on polyethylene components of a new rotating hinge with a spherical contact surface. Clin. Biomech. (Bristol, Avon) 16, 540–546. doi:10.1016/s0268-0033(01)00024-9
Zan, P., Shen, J., Liu, K., Wang, H., Cai, Z., Ma, X., et al. (2023). Custom-made semi-joint prosthesis replacement combined ligament advanced reinforcement system (LARS) ligament reconstruction for the limb salvage surgery of malignant tumors in the distal femur in skeletal immature children. Front. Pediatr. 11, 1168637. doi:10.3389/fped.2023.1168637
Zhang, C. L., Hu, J. P., Zhu, K. P., Cai, T., and Ma, X. L. (2018). Survival, complications and functional outcomes of cemented megaprostheses for high-grade osteosarcoma around the knee. Int. Orthop. 42, 927–938. doi:10.1007/s00264-018-3770-9
Keywords: bone tumor, rotating hinge knee prosthesis, gastrocnemius reconstruction, anterior tibial translation, finite element analysis
Citation: Jiang J, Zeng F and Tang X (2024) Assessing the influence of gastrocnemius reconstruction on stress distribution of femoral tumor rotating hinge knee prosthesis via finite element analysis. Front. Bioeng. Biotechnol. 12:1391298. doi: 10.3389/fbioe.2024.1391298
Received: 29 February 2024; Accepted: 08 April 2024;
Published: 19 April 2024.
Edited by:
Jingchao Liu, Peking Union Medical College, ChinaReviewed by:
Alireza Mousavian, Mashhad University of Medical Sciences, IranJun Fu, Fourth Military Medical University, China
Hao Zhang, Wuhan University, China
Copyright © 2024 Jiang, Zeng and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaodong Tang, tang15877@163.com
 Jie Jiang
Jie Jiang Fanwei Zeng1,2
Fanwei Zeng1,2  Xiaodong Tang
Xiaodong Tang