Abstract
Diabetic foot syndrome is common in uncontrolled diabetes and is a constellation of symptoms and signs that include neuropathy, infection, and ischaemia. It has become a global concern and a frequent cause of hospitalisation among diabetics. In this study, the authors’ objective was to assess the knowledge, practices, and risk of diabetic foot syndrome among diabetic patients seeking outpatient care at a tertiary hospital in Bengaluru, India. A cross-sectional study involving 198 patients with diabetes aged ≥18 years was conducted using a structured questionnaire, followed by examination using Inlow’s 60-second diabetic foot screen tool. The results were based on the International Working Group on the Diabetic Foot (IWGDF) risk classification system. The knowledge regarding diabetic foot syndrome was inadequate for fungal infections (23.5%), shoe bites (26.5%), and changes in foot colour and temperature. Footcare practices were satisfactory, with the exception of wearing footwear indoors (25.0%) and applying moisturiser to feet (19.0%). Lack of education, diabetic neuropathy, peripheral vascular disease, history of foot ulcer, and a lack of knowledge regarding dry skin, special footwear, and inappropriate footwear were important risk factors. The researchers concluded that the knowledge level of the subjects was relatively poor. Foot practices, such as inspecting and washing feet every day, were followed by the majority of subjects. Lack of education, complications such as neuropathy, peripheral vascular disease, dry skin, and lack of information obtained on foot care practices were significantly associated with diabetic foot syndrome.
INTRODUCTION
India has been called the ‘diabetic capital of the world’ because of the predominant Westernisation of its inhabitants, which includes people of different age groups, from adolescents to the elderly, in all sections of society. According to the World Health Organization (WHO), the global prevalence of diabetes in the 2014 among individuals aged >18 was 422 million.1 In a study done in 2001 in India to assess the prevalence of diabetes and impaired glucose tolerance in six major cities, covering all the regions of the country, it was found that the age-standardised prevalence of diabetes and impaired glucose tolerance were 12.1% and 14.0%, respectively, with no gender difference.2 The study also showed that diabetes and impaired glucose tolerance had an increasing trend with age.2 The International Diabetes Federation (IDF), India, states that approximately 37.2% of the Indian urban population has diabetes.3
Some of the long-term complications of diabetes include retinopathy, nephropathy, and peripheral neuropathy, which are linked to the development of foot ulcers and amputations, Charcot joints, and autonomic neuropathy. Diabetes also contributes to lipid metabolism dysfunction, as well as hypertension.4
A common, but most often undetected, complication of diabetes is diabetic foot syndrome (ICD 20 code: E11.621). Diabetic foot syndrome can be defined as a constellation of signs and symptoms in which neuropathy, ischaemia, and infection are the main pathological mechanisms.5 It is often associated with minor trauma, foot deformity, and peripheral vascular disease.6
Diabetic foot syndrome is the most common cause of hospitalisation in diabetic patients7 and is a common cause of lower limb amputation.8 According to a study carried out involving diabetic foot ulcer patients in north India, the overall amputation rate was 28.4%.9
The symptoms suggestive of neuropathy are pain, paraesthesia, and sensory loss.10 The major risk factors for diabetic foot include previous foot ulcers, improper footwear, old age, tobacco use, chronic kidney disease, and low socioeconomic status. Increased risk for diabetes and its various complications are primarily associated with age, ethnicity, family history of diabetes, smoking, obesity, and physical inactivity.11
The global prevalence of diabetic foot ulcer is approximately 6.3% and is higher in males compared to females.12 In America, 5.0% of diabetics develop foot ulcers and 1.0% of them require amputation, thereby indicating that diabetic foot syndrome is the major cause of nontraumatic lower limb amputation.13 In a study completed in north India, 14.3% of diabetic patients had foot ulcers.14 In a similar study from south India, recurrence of foot infections was as prevalent as 52.0% in diabetic patients.15
The knowledge and practices among the diabetics regarding foot care is poor. This was substantiated in a study completed in a tertiary medical centre in Malaysia.16 Some of the factors associated with poor knowledge were male sex, low education, and shorter duration of diabetes.17 Illiteracy also invoked significant challenges to diabetic attentiveness and imposed increased foot complications.18 A perfect correlation exists between knowledge and practice regarding foot care among diabetic patients.19 Risk factor recognition is vital in helping clinicians predict, and hopefully prevent, the occurrence of diabetic foot ulcers.
OBJECTIVES
To assess the knowledge and practices regarding diabetic foot syndrome among diabetic patients attending the outpatient department of a tertiary care hospital in Bengaluru.
To assess the risk of diabetic foot syndrome among the study population.
To study the factors associated with the risk of diabetic foot syndrome in the study population.
METHODOLOGY
The authors conducted a cross-sectional study in a tertiary care hospital in Bengaluru from January 2017 to June 2017. The study population included all outpatients with diabetes seeking care at the departments of medicine and endocrinology of the selected hospital who were aged ≥18 years. Patients with gestational diabetes mellitus and Type 1 diabetes mellitus were excluded. Ethics approval was obtained from the Institutional Ethics Committee, St. John’s Medical College, Bengaluru, India, [IEC Ref No 181/2016]. The departments of medicine and endocrinology at St John’s Medical College Hospital cater to a daily outpatient load of approximately 250 patients, of whom approximately half have Type 2 diabetes mellitus. The study population was selected purposively from the patients with Type 2 diabetes mellitus attending the outpatient departments in medicine and endocrinology.
The authors estimated the sample size, basing it on a study published in the Journal of Diabetic Foot Complication in north India, which reported the prevalence of diabetic foot syndrome to be 14.3%.14 Using this as the expected prevalence, and at an absolute precision of 5% and at 95% confidence level, the authors calculated the sample size for the study to be 188 diabetics. There were not any nonresponders and therefore the authors added an additional 10 participants to the study participant number, making the final sample size 198 participants. After obtaining informed consent, the patients enrolled into the study were administered a structured interview schedule. The interview schedule included the following sections:
- Section 1: Sociodemographic details of the study population.
- Section 2: Details about diabetes.
- Section 3: Knowledge about diabetic foot syndrome.
- Section 4: Practices related to diabetic foot syndrome.
The survey was conducted by a face-to-face interview which was administered by three interviewees. The interviewees for this study were medical students who were also the investigators involved in the designing of the study and the data collection form. All the participants who were approached for the study consented to participate. The forms were checked for completeness by the interviewers themselves.
Following this, all the recruited patients were screened for risk of diabetic foot syndrome using Inlow’s 60-second diabetic foot screen tool.20 This tool was developed by the Canadian Association of Wound Care (CAWC). The tool consists of 12 elements to assess the risk of developing diabetic foot syndrome. Four elements (skin, nails, deformity, and footwear) are to be scored by inspection, three elements (temperature-hot, temperature-cold, and range of motion of the big toe) by touching, and five elements (sensation [monofilament testing, sensation] four questions, pedal pulses, dependent rubor, and erythema) to be assessed through questioning and testing. Each of these elements are scored separately for the right and left foot based on the guidelines given in the tool and the total score for each foot is calculated. Based on the value for each category, care recommendations are provided, specific to the patient’s needs. The sum of the scores for each foot will dictate the recommended follow-up. The tool has been validated and requires only a 10-g monofilament, as well as good clinical knowledge and assessment skills. Participants who scored <6 were categorised as low risk, those with scores of 7–12 were categorised as moderate risk, and those with a score of ≥13 were categorised as high risk.
This tool classifies risk of diabetic foot into six categories based on the International Working Group on the Diabetic Foot (IWGDF) risk classification system (Modified1). The six categories are as follows:
- 0: normal – no neuropathy.
- 1: loss of protective sensation.
- 2a: loss of protective sensation and deformity.
- 2b: peripheral arterial disease
- 3a: previous history of ulceration.
- 3b: previous history of amputation.
The researchers were trained on the use of this tool prior to the start of the study.
Data were entered into Microsoft-Excel and analysed using SPSS. The sociodemographic profile of the study population and details of diabetes have been outlined using descriptive statistics such as proportions and means. The risk of diabetic foot among the diabetics, knowledge pattern, and practices were computed using proportions.
The factors associated with diabetic foot syndrome were identified using the Chi squared test for association or Fischer’s exact probability test as applicable. All the factors that showed a significant association with the risk of developing diabetic foot on bivariate analysis were put into a multiple logistical regression model. Risk of developing diabetic foot (moderate or high) was considered to be the outcome variable and the variables showing significant association as co-variants. The odds ratios and the 95% confidence intervals (CI) were calculated. A p value <0.05 was considered as significant for all analysis.
RESULTS
Among the 198 diabetic subjects interviewed, the mean age of the people was 56.08 years with a standard deviation of 10.15 years, 52.0% were males, 60.5% originated from an urban background, and the majority of the patients (71.5%) were Hindus. The majority of the males were graduates (32%), followed by secondary school graduates (27%), and among the females, the majority were uneducated (32%), followed by secondary school graduates (26%). The most common occupation among males was within business (32%) while most of the females were housewives (81%). Out of the 198 participants, 102 were employed and their mean monthly family income was ₹21,332 (£245.45). Around one third of the total population belonged to upper socioeconomic status according to BG Prasad scale.21
The mean duration of diabetes was 8.6 years, with a standard deviation of 8.12 years. The majority of the study subjects (91%) had altered their diet habits and were on oral hypoglycaemic agents. Only 24.4% of the patients were on insulin, and 83.4% of the patients used to take their medications regularly. Based on the normal cut-offs of glucometer random blood sugar, fasting blood sugar, post-prandial blood sugar, and glycated haemoglobin, only 11.0% of the patients had their sugar values under control.
The most common complication was neuropathy, which occurred in 43.0% of the subjects, followed by retinopathy, observed in 39.8%. Roughly 2.5% of the subjects had a history of amputations.
Approximately 53.2% of the patients were hypertensive, of whom 57.0% were females; hypercholesterolaemia was observed in 29.0% of the patients. Tobacco had been consumed by 26.0% of the subjects. Among them, cigarette smoking was the predominant type, found in 12.5% of the patients. Alcohol had been consumed by 22.5%.
Among the 198 patients, 13% had previous history of trauma to their feet, and approximately 63% of the subjects had heaviness, tightness, pains, or cramps in their feet or legs.
Table 1 shows the knowledge and practices around foot practices among diabetic patients. The authors found that knowledge was poor regarding risk factors such as fungal infections (23.5%) and shoe bites (26.5%). Interestingly, only 12% of the patients knew about the importance of changes in colour and as few as 9% knew about that of change in temperature. Only one third of the patients knew that uncontrolled diabetes could lead to reduced blood flow to feet, reduced sensations in feet, and foot ulcers; furthermore, only half of the patients knew that calluses were a risk factor for diabetic foot ulcer formation. Similarly, knowledge regarding special diabetic footwear was present in only half of the patients. Two-thirds of the patients knew that cracked feet and trauma were risk factors. The second section of Table 1 shows practices among diabetic patients regarding foot care. This study showed that the majority of the subjects had good practices, especially for washing their feet every day (97.0%) and wearing footwear outdoors (98.5%). For practices such as applying moisturiser (19.0%) and wearing footwear indoors (25.5%), they fared poorly. Roughly 45% of the patients dried their feet in between their toes, which is a significant finding because the presence of moisture is an important predisposing factor for developing fungal infections.
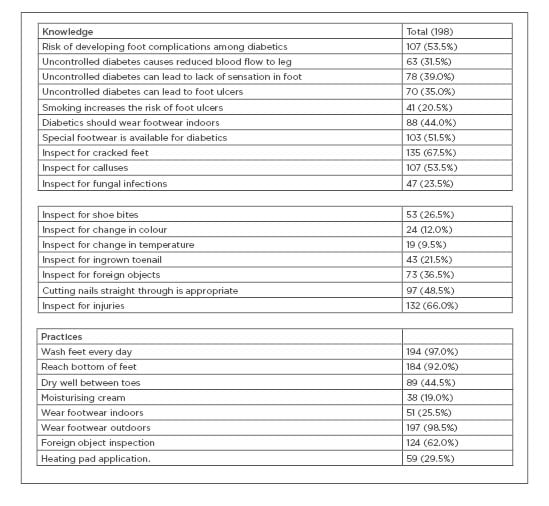
Table 1: Knowledge and practices about diabetic foot syndrome in the study sample.
Additionally, 61% of patients checked their feet for the presence of foreign bodies.
Table 2 categorises the 198 patients into three groups based on a foot examination. The table depicts factors that show a significant association with the risk of developing diabetic foot, on bivariate analysis, with respect to the various categories. The factors related to diabetic foot were a lack of formal education, diabetic neuropathy, nephropathy, peripheral vascular disease, hyperlipidaemia, smoking, history of trauma, and foot ulcers. Among the subjects with moderate risk of developing diabetic foot, 68.9% were not educated. Of the patients who had a moderate-to-high risk of developing foot ulcers, diabetic neuropathy (77.9%), nephropathy (77.4%), peripheral vascular disease (PVD) (89.0%), and smoking (73.6%) were related risk factors.
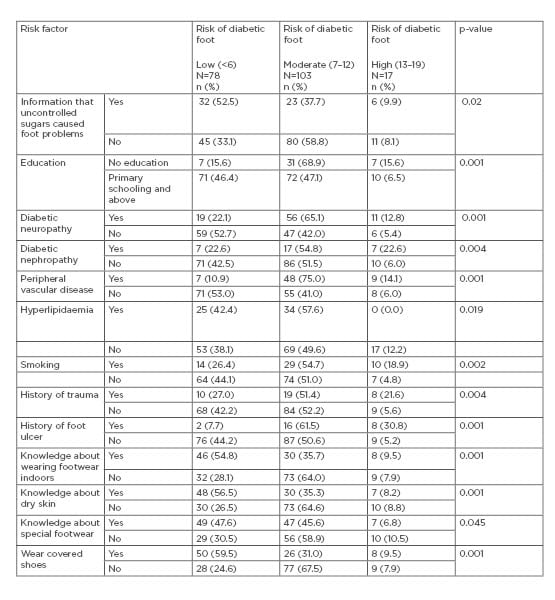
Table 2: Factors associated with risk of developing diabetic foot.
History of foot ulcers was associated with increased risk (92%) of developing diabetic foot, while history of foot trauma increased the risk by 72%. Lack of knowledge regarding diabetic complications was also a contributing factor.
Table 3 shows the independent factors associated with development of diabetic foot ulcers. All the factors that showed a significant association with the risk of developing diabetic foot on bivariate analysis (Table 2) were put into a multiple logistical regression model and the authors calculated the odds ratios (OR) and the 95% CI.
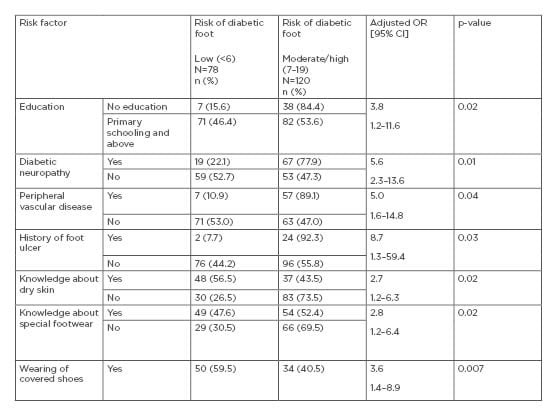
Table 3: Independent risk factors associated with diabetic foot.
Factors independently associated with a risk of diabetic foot were: lack of education (OR: 3.8; 95% CI: 1.2–11.6), diabetic neuropathy (OR: 5.6; 95% CI: 2.3–13.6), PVD (OR: 5.0; 95% CI: 1.6–14.8), history of foot ulcers (OR: 8.7; 95% CI: 1.3–59.4), lack of knowledge about application of moisturiser (OR: 2.72; 95% CI: 1.2–6.3), lack of knowledge about special footwear (OR: 2.8; 95% CI: 1.2–6.4), and practices of wearing uncovered shoes (OR: 3.6; 95% CI: 1.4–8.9).
DISCUSSION
The study shows that knowledge about diabetic foot complications was poor among patients with Type 2 diabetes mellitus seeking outpatient care in a tertiary care hospital.
A lack of formal education and lower socioeconomic status were associated with poor knowledge in the participants.
The first step towards controlling this problem is awareness of risk factors for diabetic foot complications and the measures that should be taken to prevent them. Awareness levels were similar for men and women. Viswanathan et al.15 reported that poor knowledge and practices were slightly more common in women (78.5%) than in men (62.5%).
Approximately 79.5% of the subjects believe that smoking does not carry the risk of developing foot ulcers. In a similar study conducted by Desalu et al.,22 smoking was not considered to be a risk factor for foot ulcers by 75% of the patients, attributable to a lack of knowledge surrounding possible side effects of tobacco. This finding emphasises the need for health education campaigns towards explaining the ill effects of tobacco. Just 51.5% of the subjects were aware of the availability of special footwear for diabetics. Based on a study completed in south India, 19.1% of the diabetic patients had evidences of neuropathy.22
Despite poor awareness levels regarding diabetic foot syndrome, the study found that foot care practices were adequate with majority of the participants washing feet every day and wearing footwear outdoors. Only 25.5% of the study subjects wore footwear indoors. This may be attributable to religious sentiments in Indian settings in which footwear is typically left outside the house. Specific attention towards foot care is not shown in many of the cases, such as drying well in the web spaces, which can be the factor predisposing the feet to fungal infections, further increasing the risk of developing ulcers. Practices regarding diabetic foot care range from poor to adequate in studies from different parts of India. This could be because of differences in availability of healthcare and local cultural practices.23-25
According to a similar study to the present one by Al-Rubeaan,26 PVD (OR 14.47; 95% CI:8.99–23.31), neuropathy (OR 12.06; 95% CI: 10.54–13.80), and nephropathy (OR 2.88; 95% CI: 2.43–3.40) were independent risk factors. A history of foot ulcers was also an independent risk factor (OR 8.7; 95% CI: 1.3–59.4). In a similar study by Abbott et al.27 a history of foot ulcers showed a similar pattern (OR 3.05; 95% CI: 2.16–4.31). Furthermore, that a lack of knowledge regarding the use of special footwear was an independent risk factor for development of diabetic foot (OR 2.8; 95% CI: 1.2–6.4). However, in a study by Bus et al.,28 on the effect of custom-made footwear on foot ulcer recurrence in diabetes, adherence to the use of footwear was a more important factor than the type of footwear.
This study was completed in an outpatient setting and provides a snapshot of the awareness and practices among patients with Type 2 diabetes mellitus. A limited sample of patients from a busy hospital were studied; they were selected purposively from those attending the outpatient department. The findings of this study should be viewed with consideration of the above limitations.
CONCLUSION
In the study, the most common complication among patients was neuropathy. The knowledge level among the subjects was relatively poor. Only around half of the people were aware of the complications associated with uncontrolled diabetes such as decreased sensations in the foot and foot ulcers. Most foot care practices were satisfactory, with the exception of wearing footwear indoors and applying moisturiser to the feet. Risk factors for diabetic foot were studied. A lack of education, diabetic neuropathy, peripheral vascular disease, history of foot ulcers, lack of knowledge regarding dry skin, special footwear, and inappropriate footwear were independent risk factors. This calls for increasing awareness among the patients with Type 2 diabetes mellitus on foot care practices. In tertiary care settings, special foot counters can be established where assessment of risk and advice on foot care is provided. These counters can be manned by interns; alternatively, nurse education students can be trained to man this counter. In primary and secondary care settings, the treating physicians should perform a foot examination at every diabetes consultation and offer advice on foot care to the patient. This should be included as part of standard practice. Further research is needed to study the long-term reduction in diabetic foot complications resultant of different models of care in diverse settings across India.










