Prevalence of 25-hydroxyvitamin D deficiency in the acute rehabilitation population following traumatic brain injury
Abstract
OBJECTIVE:
To determine the prevalence of vitamin D deficiency among individuals with traumatic brain injury (TBI) undergoing acute inpatient rehabilitation.
SETTING:
Inpatient rehabilitation.
PARTICIPANTS:
Participants were admitted from November 1st, 2010 through June 30th, 2015 with diagnosis of mild-severe TBI and had serum 25 OH vitamin D levels checked upon admission. 369 out of 845 met inclusion.
DESIGN:
Retrospective cohort.
MAIN MEASURES:
25 OH vitamin D, vitamin D treatment.
RESULTS:
The majority of patients were male (67%), Caucasian (89%) with private insurance (61%) and a mean age of 43.5±21.0 years. 25 OH vitamin D levels were categorized: deficient (<20 ng/mL), insufficient (20–29.9 ng/mL), and sufficient (≥30 ng/mL). There were 95 (26%) patients that were deficient, 131 (36%) that were insufficient, and 143 (39%) that were sufficient. Race/ethnicity was found to be significant (p = 0.0145) with the largest percentage of Hispanics found in the insufficient and deficient categories, and the largest percentage of Blacks in the deficient category. Most patients with deficient or insufficient vitamin D levels were prescribed vitamin D replacement during their rehab stay (p < 0.0001).
CONCLUSION:
The majority of patients undergoing acute inpatient rehabilitation were found to have insufficient or deficient vitamin D levels, therefore it should be routinely screened and treated as indicated.
The acute and chronic effects of traumatic brain injury (TBI) represent a significant health concern in the United States (Centers for Disease Control and Prevention, 2014; Faul, Xu, Wald, & Coronado, 2010), that may lead to deficits in motor function, memory, executive function, mood, sleep, and fatigue (Centers for Disease Control and Prevention, 2014; Jamall et al., 2016). The acute inpatient rehabilitation setting provides the opportunity and environment to begin the rehabilitation process, which includes medical, physical and cognitive treatment. Assessment of nutritional status following injury is also critical during inpatient rehabilitation. Vitamin D is one of the nutrients that may be monitored as it plays a unique role in facilitating cognitive and physical functioning in healthy individuals (Gloth & Tobin, 1995; Houston et al., 2007; Van der Schaft et al.,2013).
Vitamin D is a fat-soluble secosteroid that aids intestinal absorption of calcium, iron, magnesium, phosphate and zinc. Additionally, it plays a vital role in muscle function (Boonen et al., 2006), cardiovascular health (Muscogiuri et al., 2016), cancer prevention (Shan et al., 2016), and reducing risk for diabetes (Grammatiki, Rapti, Karras, Ajjan, & Kotsa, 2017). Specifically, vitamin D aids protein synthesis in muscles, helps protect against myocardial infarction and cardiovascular disease, regulates cancer stem-like cells, and may improve glycemic control and prevent complications in diabetes (Boonen et al., 2006; Grammatiki et al., 2017; Holick et al., 2011; Muscogiuri et al., 2016; Shan et al., 2016). Within the brain, vitamin D supports neural protection through antioxidant mechanisms, calcium regulation, enhanced nerve conduction, and detoxification mechanisms (Buell & Dawson-Hughes, 2008). As adequate neural functioning and protection play such a large role in recovery from TBI (Povlishock & Katz, 2005), these vitamin D mediated protection mechanisms may be especially important in a rehabilitation population.
The rate of vitamin D deficiency, defined as serum 25 OH vitamin D level less than 20 ng/ml, is estimated to be between 25% and 57% in the general U.S. population (Holick et al., 2011). Vitamin D deficiency may affect physical and cognitive health, is a risk factor for osteoporosis, osteopenia and bone fractures, and has been associated with musculoskeletal pain and impaired physical function (Boonen et al., 2006; Holick et al., 2011; Muscogiuri et al., 2016). Insufficient (20–29.9 ng/mL) and deficient levels (<20 ng/mL) of 25 OH vitamin D have also been associated with poor performance on cognitive tasks, and may also be correlated with dementia diagnosis and related cognitive decline (Van der Schaft et al., 2013).
While numerous studies have investigated vitamin D insufficiency or deficiency in the general population, limited data is available in those undergoing rehabilitation. In a study of rehabilitation patients admitted for brain, spinal cord, and musculoskeletal injuries, Shinchuk and colleagues found that 83% were vitamin D insufficient or deficient (Shinchuk et al., 2006). Further, in an examination of the functional impact of vitamin D deficiency in rehabilitation populations (e.g., stroke, orthopedic injuries), Kiebzak reported that patients with deficient or insufficient vitamin D levels correlated with significantly lower Functional Independence Measure (FIM) efficiency scores (Kiebzak, Moore, Margolis, Hollis, & Kevorkian, 2007). These results highlight both increased prevalence of vitamin D deficiency in rehabilitation populations and the functional impact of this deficiency.
While early investigational results highlight the potential issues surrounding insufficient vitamin D in rehabilitation patients, no study has thus far examined the prevalence and functional implications of insufficient or deficient vitamin D among TBI patients undergoing acute inpatient rehabilitation. This is important as inpatient rehabilitation provides an opportunity to treat nutritional imbalances that exist, and vitamin D may have implications for physical and cognitive recovery. Therefore, the present study sought to identify vitamin D prevalence rates in a TBI rehabilitation sample and investigate the association between vitamin D levels and select functional outcomes. A retrospective chart review was performed on patients admitted to a large urban rehabilitation hospital over a four-and-a-half-year span. All patients were diagnosed with a mild to severe TBI.
1Methods
1.1Participants
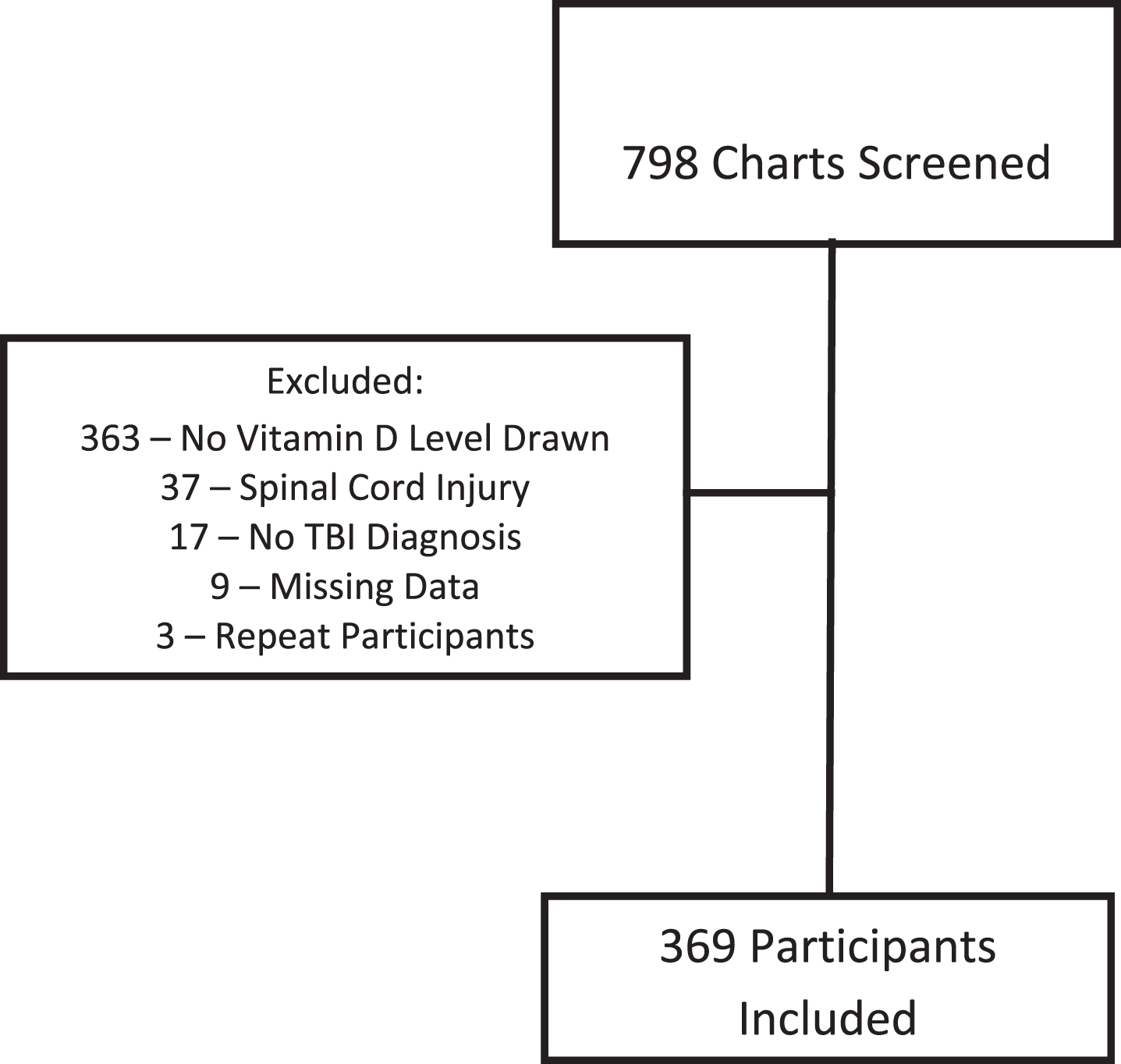
Seven hundred and ninety-eight medical charts for patients with etiological diagnosis of TBI were obtained from the eRehabData® admissions data portal at a large rehabilitation hospital located within an urban metropolitan area between May 1st, 2011 and June 30th, 2015. Charts were further reviewed for inclusion which were diagnosis of traumatic brain injury and completed vitamin D screening during inpatient rehabilitation via serum 25-hydroxy upon rehabilitation admission. Patients were excluded from the study due to a comorbid or primary diagnosis of spinal cord injury, no etiological diagnosis of TBI, or incomplete chart data. Of the 798 charts initially reviewed, 369 (46.2%) had vitamin D screening and were eligible for the study (see Fig. 1).
Fig.1
Subject screening diagram.
1.2Procedures
IRB approval was obtained prior to beginning the retrospective chart review. Information was extracted from electronic medical records contained in the patient’s trauma and inpatient rehabilitation medical record and eRehabData®.
1.3Measures/outcomes
Demographic information was obtained for each patient, including race, ethnicity, age, gender, insurance coverage, and discharge disposition. Additionally, the following medical information was obtained from each patient’s medical record: date of injury, mechanism of injury, length of stay in the rehabilitation hospital, Glasgow Coma Scale (GCS) score at initial hospital admission, FIM scores at admission and discharge to inpatient rehabilitation, and history of vitamin D deficiency and supplementation via history and physical documentation, medication and administration chart review.
1.4Statistical analysis
Descriptive statistics were used to summarize demographic and injury characteristics. Patient data was then separated into three vitamin D groups according to vitamin D levels at admission to inpatient rehabilitation: deficient (<20 ng/mL), insufficient (20–29.9 ng/mL), or sufficient (≥30 ng/mL). Comparisons of vitamin D groups and race were made using a Fisher’s exact test. Comparisons of vitamin D groups and total FIM efficiency were made using analysis of variance. Spearman’s correlations were employed to assess the relationship between vitamin D level and acute hospital and inpatient rehabilitation stays and patient characteristics.
2Results
Demographic information for all 369 patients are summarized in Table 1. The majority of patients were male (63%), Caucasian (89%), and used private insurance (61%). Average age of participants was 43.5±21.0 years old. The most prevalent mechanisms of injury were vehicular collisions (60%), falls (25%) and acts of violence (6%). GCS at admission into the acute care hospital was missing from 40% of the inpatient rehabilitation admissions. Of the GCS scores recorded, the majority were in the severe range (37%).
Table 1
Summary of demographic and clinical information
| N = 369 | |
| Age, mean±sd | 43.5±21.0 |
| Male | 246 (67%) |
| Hispanic Ethnicity | 57 (15%) |
| Race | |
| Asian | 4 (1%) |
| Native Hawaiian/Pacific Islander | 1 (0.3%) |
| Black or African American | 27 (7%) |
| White or Caucasian | 327 (89%) |
| Unknown/Missing | 10 (3%) |
| Primary Insurance Type | |
| Private | 228 (61%) |
| Self-pay or uninsured | 3 (1%) |
| Medicaid | 7 (2%) |
| Medicare | 73 (20%) |
| Tricare | 7 (2%) |
| Other | 46 (12%) |
| Unknown/Missing | 5 (1%) |
| Discharge Disposition | |
| Private Residence | 241 (65%) |
| Nursing Home | 37 (10%) |
| Adult Home | 3 (1%) |
| Hospital | 29 (8%) |
| Other | 58 (16%) |
| Unknown/Missing | 1 (0.3%) |
| Length of Stay, median (IQR) | 20 (13–29) |
| Days from Injury to Rehab | 19.5 (11–36) |
| Mechanism of Injury | |
| Vehicular | 222 (60%) |
| Violence | 21 (6%) |
| Sports | 4 (1%) |
| Fall | 89 (24%) |
| Falling/Flying Object | 5 (1%) |
| Pedestrian | 16 (4%) |
| Other/Missing | 12 (3%) |
| GCS | |
| Mild | 58 (16%) |
| Moderate | 26 (7%) |
| Severe | 136 (37%) |
| Unknown/Missing | 149 (40%) |
| Vitamin D Level | 29.5±16.1 |
| Vitamin D Category | |
| Deficient (<20) | 95 (26%) |
| Insufficient (20–29.9) | 131 (36%) |
| Sufficient (≥30) | 142 (39%) |
25 OH vitamin D levels were labeled as deficient (<20 ng/ml), insufficient (20–29.9 ng/ml), or sufficient (≥30 ng/ml) based on Clinical Practice Guidelines (Holick et al., 2011). The average vitamin D level at admission was 29.5±16.1 ng/ml [62% of patients were insufficient (n = 131) or deficient (n = 95)].
A significant difference in vitamin D level was found based on race/ethnicity (p = 0.01) (see Table 2). While 57% of non-Hispanic White patients were vitamin D insufficient of deficient, 71% of non-Hispanic Black and 79% of Hispanic patients were insufficient or deficient. Additionally, no statistical differences emerged between FIM efficiency scores and vitamin D level categories (Table 2).
Table 2
Comparison between race/ethnicity and FIM efficiency and levels of vitamin D
| Deficient | Insufficient | Sufficient | p-value | |
| Race/Ethnicity | 0.0145 | |||
| Non-Hispanic White | 64 (23%) | 94 (34%) | 116 (42%) | |
| Non-Hispanic Black | 11 (41%) | 8 (30%) | 8 (30%) | |
| Hispanic | 18 (32%) | 27 (47%) | 12 (21%) | |
| Other | 2 (18%) | 2 (18%) | 7 (64%) | |
| FIM Efficiency | ||||
| Motor | 1.7±1.1 | 1.5±1.1 | 1.6±1.2 | 0.3976 |
| Cognition | 0.6±0.5 | 0.5±0.4 | 0.6±0.5 | 0.2267 |
| Total | 2.3±1.4 | 2±1.3 | 2.2±1.7 | 0.3942 |
365 out of 369 (99%) patients did not have documented past medical history of vitamin D deficiency per the history and physical documentation and admission medication orders. 79 out of 95 (83.2%) deficient patients and 94 out of 131 (71.8%) insufficient patients were prescribed vitamin D treatment during inpatient rehabilitation stay. There was no correlation between vitamin D level and acute hospital (r = –0.02; p = 0.7733) or inpatient rehabilitation length of stay (r = 0.002; p = 0.9692).
3Discussion
The present study employed a retrospective chart review to investigate the prevalence of vitamin D insufficiency and deficiency in TBI patients within inpatient rehabilitation. Overall, results revealed 63% of TBI patients were vitamin D insufficient or deficient, which is consistent with broader national prevalence estimates (Jamall et al., 2016). However, no estimates of vitamin D levels in an inpatient TBI rehabilitation population are available in the literature, thus this figure provides important information about prevalence rates in this setting.
Sufficient, insufficient, and deficient groups significantly differed in terms of race, with the largest proportion of Black and Hispanic patients presenting with insufficient or deficient levels. This result is consistent with demographic differences within the wider US population, where the highest rate of vitamin D deficiency is found in Black and Hispanic individuals (Forrest & Stuhldreher, 2011). Differences in vitamin D deficiency rates between White, Black, and Hispanic groups may have implications in terms of screening, health care access, and use of supplementation or treatment. Health care providers should therefore be aware of at-risk groups within rehabilitation settings, who may benefit most from screening and treatment.
It was predicted that insufficient and deficient vitamin D levels would be associated with poorer functional outcomes, however, no correlations were found between FIM and vitamin D status. Due to the broad nature of FIM categories, it would be difficult to use this measure as the sole indicator of vitamin D’s impact on overall health and functional improvement.
While the rate of vitamin D treatment was 76.5% for insufficient and deficient patients, it is worth noting that only 369 out of 798 (46.2%) patients had their vitamin D level screened upon rehabilitation admission. This gap in screening may be due to variability of physician practices, partially attributable to a lack of evidence-based recommendations to screen TBI patients for vitamin D deficiency. The present study adds important prevalence rates to the evidence base.
3.1Limitations and future directions
A few limitations exist for this study. First, this data represents only one institution, and vitamin D levels may vary across geographic regions (Kimlin, 2008). Additionally, data that was available for extraction was limited due to the retrospective nature, and other determinants such as premorbid vitamin D levels, injury severity (i.e., GCS), comorbidities and neuropsychological outcomes were not always available.
While evidence-based guidelines for screening and treating vitamin D in TBI patients in inpatient rehabilitation do not exist, our study finds the majority of TBI patients have deficient of insufficient vitamin D levels in the acute rehabilitation setting. Future efforts to establish an association of vitamin D and functional (motor and cognitive) status should be pursued among individuals with TBI both in the acute and post-acute setting in order to compel clinicians to routinely screen for and replace vitamin D.
4Conclusion
Ultimately, results provide an estimate of vitamin D insufficiency and deficiency rates in TBI patients admitted to inpatient rehabilitation. These rates lend support to screening 25 OH vitamin D level upon admission to inpatient rehabilitation settings. Screening may be especially important for those patients of an ethnic minority, as they are at increased risk of insufficient or deficient vitamin D levels. Finally, future research should continue to investigate prevalence of vitamin D, relationships between vitamin D levels and functional measures, and outcomes following vitamin D replacement in the TBI population. In this way, researchers can continue to inform practice and provide the best care for patients undergoing inpatient rehabilitation.
Conflict of interest
The authors have no conflicts of interest to disclose.
Acknowledgments
This work was presented as a poster at the American Congress of Rehabilitation Medicine Conference, October 2016, Chicago, IL, USA.
References
1 | Boonen, S. , Bischoff-Ferrari, H. , Cooper, C. , Lips, P. , Ljunggren, O. , Meunier, P. , & Reginster, J.-Y. ((2006) ). Addressing the musculoskeletal components of fracture risk with calcium and vitamin D: a review of the evidence. Calcified tissue international, 78: (5), 257-270. |
2 | Buell, J. S. , & Dawson-Hughes, B. ((2008) ). Vitamin D and neurocognitive dysfunction: preventing “D” ecline? Molecular aspects of medicine, 29: (6), 415-422. |
3 | Centers for Disease Control and Prevention. ((2014) ). Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. Atlanta, GA. |
4 | Faul, M. , Xu, L. , Wald, M. M. , & Coronado, V. ((2010) ). Traumatic brain injury in the United States. Atlanta, GA: national Center for injury Prevention and Control, Centers for disease Control and Prevention. |
5 | Forrest, K. Y. , & Stuhldreher, W. L. ((2011) ). Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res, 31: (1), 48-54. doi:10.1016/j.nutres.2010.12.001 |
6 | Gloth, F. M. , & Tobin, J. D. ((1995) ). Vitamin D deficiency in older people. Journal of the American Geriatrics Society, 43: (7), 822-828. |
7 | Grammatiki, M. , Rapti, E. , Karras, S. , Ajjan, R. , & Kotsa, K. ((2017) ). Vitamin D and diabetes mellitus: Causal or casual association? Reviews in Endocrine and Metabolic Disorders, 1-15. |
8 | Holick, M. F. , Binkley, N. C. , Bischoff-Ferrari, H. A. , Gordon, C. M. , Hanley, D. A. , Heaney, R. P. , & Weaver, C. M. ((2011) ). Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab, 96: (7), 1911-1930. doi:10.1210/jc.2011-0385 |
9 | Houston, D. K. , Cesari, M. , Ferrucci, L. , Cherubini, A. , Maggio, D. , Bartali, B. , & Kritchevsky, S. B. ((2007) ). Association between vitamin D status and physical performance: the InCHIANTI study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 62: (4), 440-446. |
10 | Jamall, O. A. , Feeney, C. , Zaw-Linn, J. , Malik, A. , Niemi, M. E. , Tenorio-Jimenez, C. , & Scott, G. ((2016) ). Prevalence and Correlates of Vitamin D Deficiency in Adults after Traumatic Brain Injury. Clinical endocrinology, 85: (4), 636-644. |
11 | Kiebzak, G. M. , Moore, N. L. , Margolis, S. , Hollis, B. , & Kevorkian, C. G. ((2007) ). Vitamin D status of patients admitted to a hospital rehabilitation unit: relationship to function and progress. American journal of physical medicine & rehabilitation, 86: (6), 435-445. |
12 | Kimlin, M. G. ((2008) ). Geographic location and vitamin D synthesis. Molecular aspects of medicine, 29: (6), 453-461. |
13 | Muscogiuri, G. , Annweiler, C. , Duval, G. , Karras, S. , Tirabassi, G. , Salvio, G. , & Mascitelli, L. ((2016) ). Vitamin D and Cardiovascular Disease: From atherosclerosis to myocardial infarction and stroke. International Journal of Cardiology, 230: , 577-584. |
14 | Povlishock, J. T. , & Katz, D. I. ((2005) ). Update of neuropathology and neurological recovery after traumatic brain injury. The Journal of head trauma rehabilitation, 20: (1), 76-94. |
15 | Shan, N. L. , Wahler, J. , Lee, H. J. , Bak, M. J. , Gupta, S. D. , Maehr, H. , & Suh, N. ((2016) ). Vitamin D compounds inhibit cancer stem-like cells and induce differentiation in triple negative breast cancer. The Journal of Steroid Biochemistry and Molecular Biology. |
16 | Shinchuk, L. M. , Morse, L. , Huancahuari, N. , Arum, S. , Chen, T. C. , & Holick, M. F. ((2006) ). Vitamin D deficiency and osteoporosis in rehabilitation inpatients. Archives of Physical Medicine and Rehabilitation, 87: (7), 904-908. |
17 | Van der Schaft, J. , Koek, H. , Dijkstra, E. , Verhaar, H. , Van der Schouw, Y. , & Emmelot-Vonk, M. ((2013) ). The association between vitamin D and cognition: a systematic review. Ageing research reviews, 12: (4), 1013-1023. |



