Multidomain Intervention for Reversal of Cognitive Frailty, Towards a Personalized Approach (AGELESS Trial): Study Design
Abstract
Background:
Cognitive frailty (CF) is identified as one of the main precursors of dementia. Multidomain intervention has been found to delay or prevent the onset of CF.
Objective:
The aim of our present study is to determine the effectiveness of a comprehensive, multidomain intervention on CF; to evaluate its cost effectiveness and the factors influencing adherence toward this intensive intervention.
Methods:
A total of 1,000 community dwelling older adults, aged 60 years and above will be screened for CF. This randomized controlled trial involves recruitment of 330 older adults with CF from urban, semi-urban, and rural areas in Malaysia. Multidomain intervention comprised of physical, nutritional, cognitive, and psychosocial aspects will be provided to participants in the experimental group (n = 165). The control group (n = 165) will continue their usual care with their physician. Primary outcomes include CF status, physical function, psychosocial and nutritional status as well as cognitive performance. Vascular health and gut microbiome will be assessed using blood and stool samples. A 24-month intensive intervention will be prescribed to the participants and its sustainability will be assessed for the following 12 months. The effective intervention strategies will be integrated as a personalized telerehabilitation package for the reversal of CF for future use.
Results:
The multidomain intervention developed from this trial is expected to be cost effective compared to usual care as well as able is to reverse CF.
Conclusion:
This project will be part of the World-Wide FINGERS (Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability) Network, of which common identifiable data will be shared and harmonized among the consortia.
INTRODUCTION
Globally, the number of aging population is increasing rapidly. Similarly, in Malaysia the number of older adults has tripled from 550 thousand to 1.45 million during the last three decades; and by the year 2035, older adults will represent 15%of the Malaysian population [1]. Frailty has been one of the major concerns pertaining to aging [2]. Labelled as a ‘geriatric syndrome’, frailty is defined by five phenotype models which include unintentional weight loss, fatigue, weakness, decreased gait speed, and physical inactivity [3]. Frailty is associated with increased risk of falls, functional disability, hospitalization, poor quality of life, and death [2, 4, 5]. Frailty has been reported as a ‘costly syndrome’, of which 40 to76%of total health care cost was provided for older adults with frailty [6].
Another vital component for healthy and successful aging is cognitive function. Deterioration in cognition among the aged population is often caused by neurodegenerative diseases such as Alzheimer’s diseases (AD), which is the leading causes of dementia [7]. Early detection and intervention in individuals with mild cognitive impairment (MCI)—a phenotype associated with increased risk of dementia—is deemed crucial in the prevention or delaying of dementia [8]. The interrelationship between physical frailty and cognitive impairment has been highlighted through underlying mechanisms that are common for both conditions [9]. The causative mechanisms of physical frailty comprise of systemic inflammation, hormonal changes, and mitochondrial dysfunction that contribute to depletion of homeostasis maintenance [10, 11]. Noteworthy, these mechanisms also act as catalyst in cognitive decline and dementia due to neurodegenerative and vascular damages [12]. In Malaysia, the co-existence of both physical frailty and cognitive impairment has been demonstrated to be high among institutionalized older adults [13].
The simultaneous presence of both physical frailty and MCI is termed ‘cognitive frailty’ [14]. Cognitive frailty (CF) is a newly identified medical condition coined by the International Academy on Nutrition and Aging (I.A.N.A) and the International Association of Gerontology and Geriatrics (I.A.G.G) [15]. It is found to be one of the main precursors to dementia [14], associated with disability and increased mortality rate [16, 17]. The prevalence of CF was reported to be between 1.0%to 12.0%in the community setting globally [18, 19]. In a recent study, it was found that 37.4%of community-dwelling older adults in Malaysia were cognitively pre-frail and 2.2%had CF [20]. Increased age, vitamin D deficiency, co-existence of depression as well as frailty, declined functional mobility, and processing speed have been identified as the predictors of CF [21]. The adverse health effects caused by CF calls for effective preventive measures. However, most of the preventive interventions tested so far have been focused on either physical frailty or MCI, but rarely for CF. Our earlier pilot study using a multidomain intervention for the potential reversal of CF [22] is showing promising results, which need further validation.
Physical exercise is effective in improving physical and cognitive function among older adults with physical frailty and cognitive impairment [14, 23]. Although intervention for physical frailty is monopolized by exercise, greater improvement in physical function was observed when exercise was administered in combination with nutritional counselling [24]. Similarly, cognitive training delivered together with physical exercise was more effective in increasing cognitive function [25]. In the study by [26], it was reported that a multidomain intervention comprised of nutritional, physical, and cognitive intervention was demonstrated to be superior in reversing physical frailty in older adults compared to a single component intervention [26]. Older adults with CF were shown to have improvement in cognitive and physical performance following 16 weeks of high-speed resistance exercise training [23]. Nevertheless, nutritional and psychological domains were not assessed in this study, which is also crucial to provide a holistic approach in order to improve the wellbeing and quality of life among older adults with CF [15]. The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) is a large, long-term trial in which a multidomain program comprised of cognitive training, physical activity, nutritional intervention, and control of vascular and metabolic risk factors improved cognition and reduced the risk of cognitive decline in older adults at increased risk of dementia [27–29]. The aforementioned studies emphasize the need to incorporate several domains of interventions for a more comprehensive approach for significant physical and cognitive outcomes but none of these studies addressed reversal of CF. Also, psychosocial aspects are overlooked in these interventions trial. Older adults with frailty are reported to be four times more likely to be socially isolated, with less social engagement and participation [30]. Therefore, interventions targeting psychosocial aspects may benefit older adults to a great extent. Psychosocial interventions mainly targeting social support and participation in social activities have shown to improve mental health, life satisfaction, quality of life as well as improved depressive symptoms in older adults with and without MCI [31, 32]
In addition, in most of the studies multidomain interventions were conducted over a short period of time; and little is known about factors influencing adherence towards multidomain intervention. During the current COVID-19 pandemic, virtual or online intervention, including telemedicine and telerehabilitation, has been adopted as an effective approach for clinicians and health care professionals to virtually meet their patients [33]. Telerehabilitation for neurodegenerative disease is comparable to conventional, in-person rehabilitation, of which 68.1%participants are in agreement that telerehabilitation is a significant alternative and are as good as face-to-face assessment [34–36]. Others have reported telerehabilitation to be feasible and effective in musculoskeletal pain management and in falls prevention in older adults with chronic diseases and at increased risk of falls [37, 38]. In comparison to face to face rehabilitation, telerehabilitation is more ideal for pain control and functional recovery [39, 40]. Though telerehabilitation has shown to have a significant impact among individuals with physical impairment (pain, functional disability) and cognitive impairment, but such evidence is lacking for the reversal of CF. Further, telemedicine application in certain age groups such as older adults is a challenge due to technical illiteracy, lack of desire, and cost. In this age group, the barriers need to be identified and eliminated in order to increase the prevalence of telehealth use [41, 42]. High cost and cultural resistance have also been identified as main barriers for implementing telemedicine in developing countries [43].
Mitigating factors that cover gut microbiome, physiological, nutritional status, psychosocial, and environmental aspects have rarely been considered in such intensive intervention. It is essential to determine the influence of these factors to model a personalized rehabilitation program to reverse CF. The aim of this article is to present and explain in depth the study protocol of the ‘Multidomain Intervention to Reverse Cognitive Frailty among Community Dwelling Older Adults (AGELESS Trial)’. In AGELESS Trial, we aim to determine the effect of a comprehensive multidomain intervention (nutrition, exercise, management of vascular and metabolic risk factors, cognitive training, and psychosocial support) on CF; and to determine its cost effectiveness as well as the factors influencing adherence toward the intensive intervention. Further, the feasibility of implementing the intervention using telerehabilitation approach will also be evaluated.
METHODOLOGY
Study design
The AGELESS Trial is a multicenter, longitudinal, double-blind randomized controlled trial (RCT) recruiting participants around the Central of Malaysia, i.e., Kuala Lumpur, with the Centre of Healthy Aging and Wellness, National University of Malaysia, Kuala Lumpur (HCARE) as the urban setting and two Senior Citizen Centres known locally as “Pusat Aktiviti Warga Emas” (PAWE) in a semi-urban and a rural area of Malaysia (PAWE Bangi, Selangor and PAWE Rembau, Negeri Sembilan, respectively). Ethical approval has been obtained from the Universiti Kebangsaan Malaysia Medical Research Ethics Committee (UKM PPI/111/8/ JEP-2020-347).
Data collection will be conducted by a multidisciplinary team consisting of trained fieldworkers from health sciences education background. This study will be conducted according to the extended Medical Research Council Framework for the development and evaluation of RCT for complex interventions to improve health (Fig. 1). This framework emphasizes systematic development of interventions based on available evidence and theory. Prior to implementation, a series of pilot tests will be executed to evaluate the feasibility of the interventions developed.
Fig. 1
Study model developed and adapted from the UK Medical Research Council (MRC) framework.
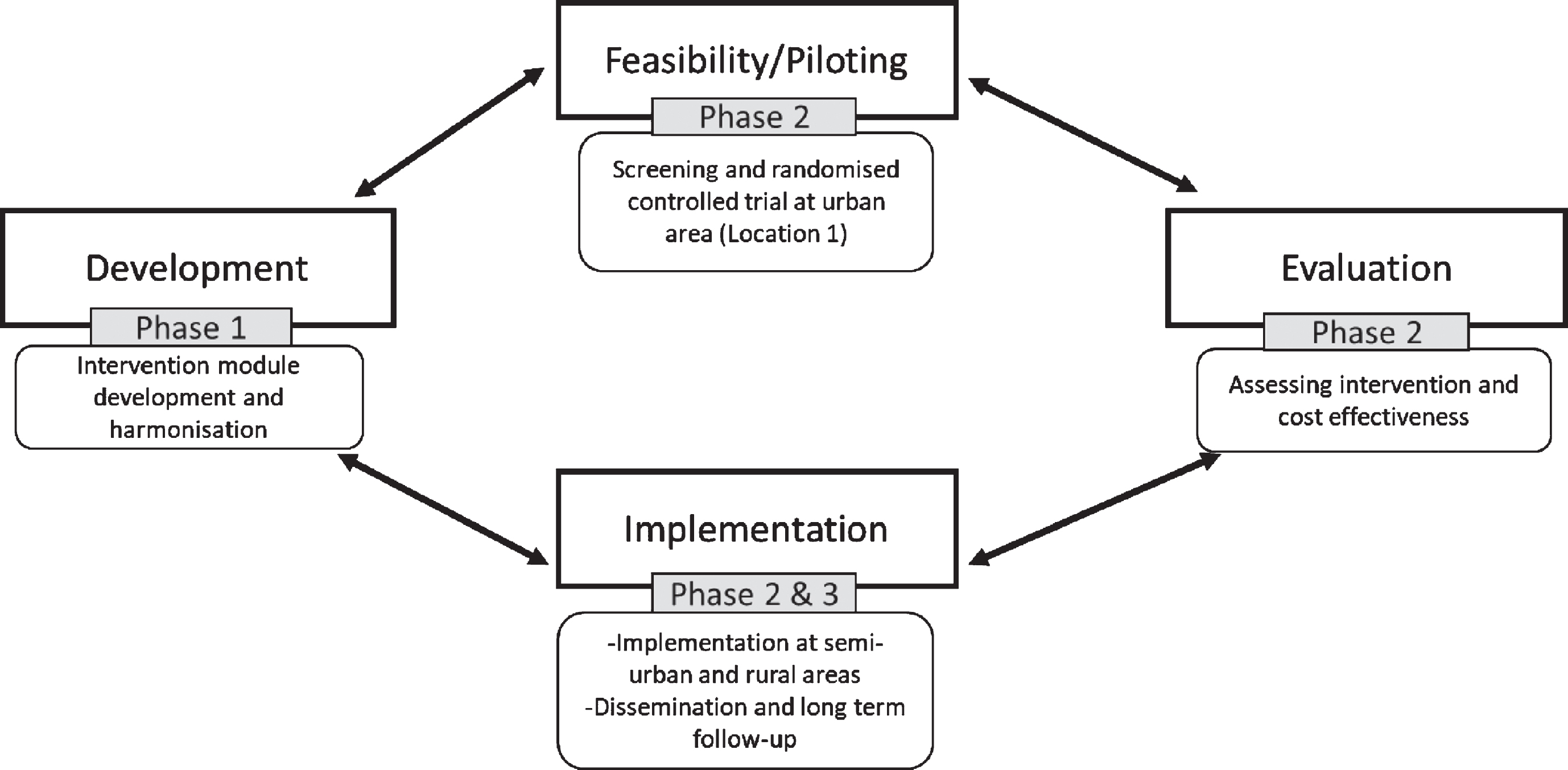
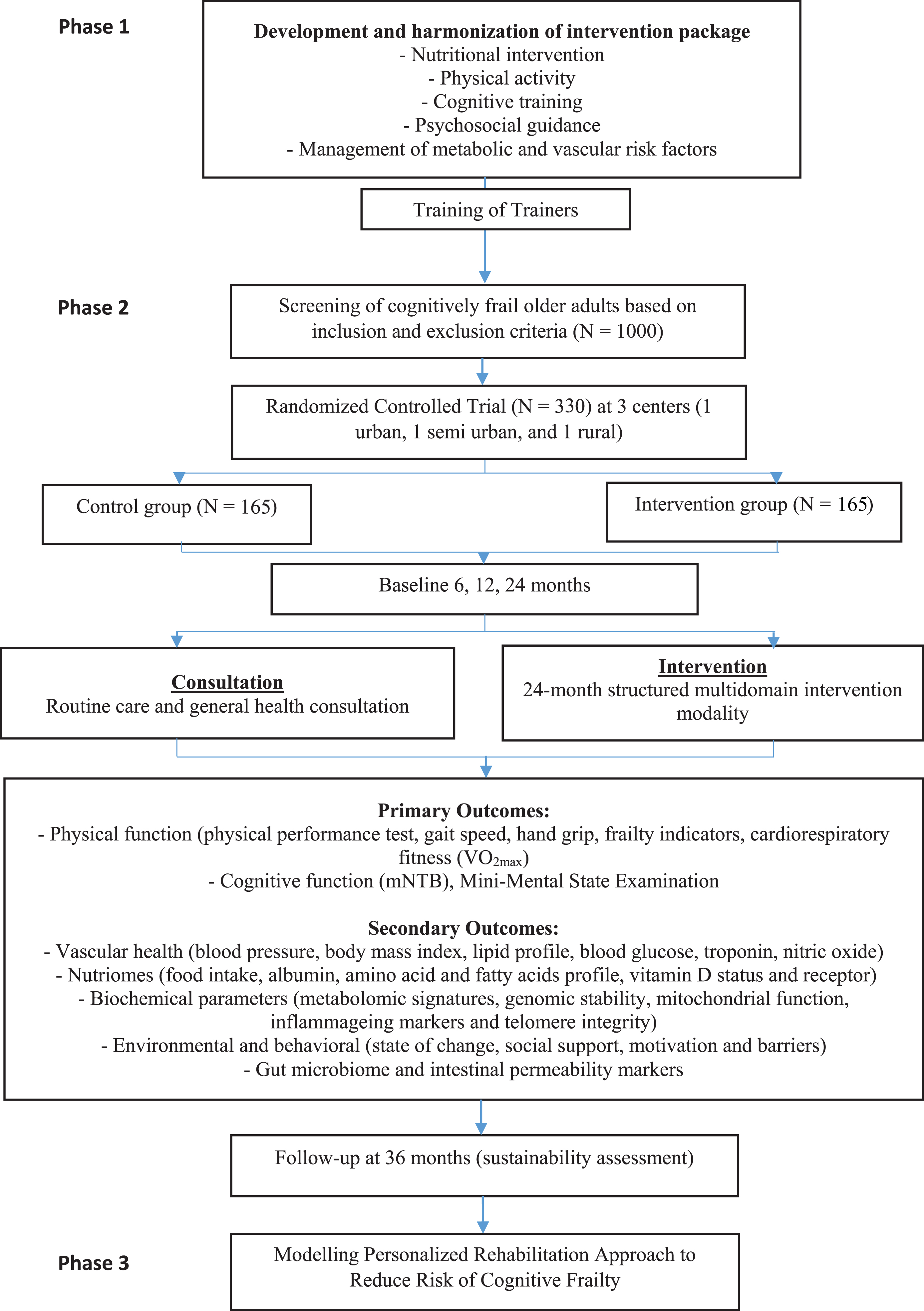
As illustrated in Fig. 2, this study will be conducted in three phases. Phase 1 is the development of the intervention package and Phase 2 is the screening, baseline assessment, and randomization of the participants, as well as the execution of the multidomain intervention. Lastly, Phase 3 would be the personalized rehabilitation approach modelling.
Fig. 2
AGELESS trial flowchart.
The AGELESS Trial is built on the FINGER trial model and is part of the World-Wide FINGERS network of multidomain trials for dementia risk reduction and prevention [44]. The common key feature of the RCTs participating in the network, including AGELESS, is the use of a multidomain approach focused on management of vascular conditions, lifestyle, exercise and physical activity, cognitive training, and nutrition guidance, delivered through a combination of individually tailored counselling sessions and group-based activities. Additionally, the AGELESS clinical outcomes are harmonized to those of the FINGER trial, to ensure comparability of findings. It should be noted that in the AGELESS Trial, individuals with CF will be recruited, while FINGER involved older adults with cognitive impairment. Both conditions are predementia states of which the intervention components are similar. At the same time, local adaptations are implemented to account for geographical, ethnic, and cultural differences, and thus facilitate adherence to the intervention. Specifically, for this study, exosome (gut microbiome) and mediators (physiological, vascular, nutritional status, environmental, and psychosocial) influencing intervention adherence will be assessed to model personalized rehabilitation for reversing cognitive frailty.
Calculation of sample size
Sample size calculation was done based on objectives of the study. For Phase 2 study, sample size was computed using G-Power software with effect size (f = 0.15), obtained from previous study [45], while the intervention effect was computed based on global cognition (Mini-Mental State Examination, MMSE). A total of 242 participants was found to be sufficient. However, considering a 35% drop out rate (85); total sample to be recruited is approximately 330 (rounded to the nearest ten) with 165 participants in each group.
Selection of study participants: inclusion and exclusion criteria
Approximately 1,000 individuals aged 60 to 80 years old will be screened for CF. The participants will be informed about the study through distribution of flyers in PAWE and through social media advertisements. Participants will be invited for the screening in order to determine their eligibility for AGELESS Trial. In addition to age, inclusion criteria for the screening includes ‘free living in the community’ and absent of severe physical and mental disabilities. Non-permanent residents and those who resided less than 6 months in a particular study site will be excluded. Participants will have to meet the following inclusion criteria in order to be recruited in the RCT; MMSE ≥19 and < 26 points [46], Clinical Dementia Rating Scale (CDR) = 0.5 [13] and fulfils at least three of Fried’s frailty criteria [3]. Exclusion criteria include those conditions that affects engagement in the interventions such as major depression, dementia, other major psychiatric disorders, severe cognitive impairment, malignant diseases or other conditions preventing safe participation and cooperation as judged by the study staff and coincident participation in any intervention trial.
A total of 330 (110 participants from each location) individuals with CF, classified based on criteria tabulated in Table 1 [15], will be recruited and randomly assigned to the intervention (n = 165) or the control group (n = 165). The randomization sequence will be conducted by the clinical trial manager through a computer program; the Research Randomizer by trial manager [47]. Concealed envelopes will be used to assign group status and group allocation will be actively disclosed to participants, but they will be advised not to discuss the intervention during the assessment sessions. In order to achieve double blind design, all assessors involved in the baseline and follow up assessments as well as the participants will not be aware of the treatment arms of the participants. A list of validated questionnaires will be utilized for screening, including Malay version of the MMSE [48], CDR [49], Beck Depression Inventory [50], and Physical Activity Scale for the Elderly (PASE) [51]. In addition, literacy toward Information and Communication Technologies (ICT) will also be examined during screening [52]. The ICT questionnaire is meant to address questions pertaining to smartphones and internet availability as well as accessibility at their respective homes and within their family circle.
Baseline measurement
Information on sociodemographic and medical status, lifestyle as well as anthropometric and body composition measurements will be taken. Based on the assessment, each participant will receive a written information on the assessed parameters and will be advised to consult their doctor for cases that require medication initiation such as high blood pressure or hyperglycemia. As tabulated in Table 2, several parameters will be included for the baseline assessment of included participants. Functional magnetic resonance imaging (fMRI) will also be performed at resting state for 30 of the trial participants and 30 from the control group. fMRI is a functional neuroimaging technique that is non-invasive in studying patients with neurodegenerative disorders and can be repeated many times in longitudinal study [67]. In the present study, fMRI is used to examine the effect of multidomain intervention on brain activation. This would allow understanding on the pathological processes of cognitive decline and what are the effects of intervention. Sample size for fMRI was computed using G-Power software with effect size (f = 0.5), obtained from a previous study, for intervention effect on brain MRI [68]. A total of 38 participants was found to be sufficient. However, considering a 35%drop out rate (total sample to be recruited is 59 with approximately 30 participants in each group. These participants will be selected from two centers, Kuala Lumpur (urban) and Selangor (semi-urban), according to the availability of MRI facilities and resources.
Table 2
The parameters collected at baseline
| Parameters | |
| Primary Outcomes | |
| Cognitive function | Modified Neuropsychological Tests Battery (mNTB) [53], Mini-Mental State Examination, Clinical Dementia Rating |
| Physical fitness | Fried’s Frailty Criteria, 2-min Step Test, Grip Strength Test, Chair Stand Test, Chair Sit-and-Reach Test, Timed Up-and-Go Test, Back Scratch Test [54], Exercise Self-Efficacy Scale (ESES) [55], maximum oxygen uptake (VO2max) [56]. |
| Secondary Outcomes | |
| Body composition | Weight, height, arm span, mid-upper arm circumference, waist circumference, hip circumference, calf circumference, fat mass, muscle mass |
| Psychosocial and functional status | Medical Outcome Social Support (MOSS) [57], BRIEF-Cope [58], De Jong Gierveld Loneliness Scale [59], Resilience scale [60], General Self-Efficacy Scale (GSES) [61], University of Rhode Island Change Assessment (URICA) Psychotherapy version [62] |
| Dietary intake | Diet History Questionnaire (DHQ) [63] |
| Vascular Health | 30 ml blood for biochemical analysis (metabolic profile, troponin, nitric oxide, nutriomes, albumin, amino acid and fatty acid profile, vitamin D receptor, vitamin B12, folic acid, vitamin E, homocysteine), genomic stability and oxidative damage, mitochondrial function, inflammatory markers, metabolomics analysis, gene related pathway analysis [20] |
| Fecal sample | Gut microbiome [64] |
| Brain Activation | Structural, task-based and resting state functional magnetic resonance imaging (fMRI) data will be acquired using 3.0 Tesla scanner [65, 66] |
Intervention program
The multidomain intervention package will be developed and consolidated based on the FINGER trial protocol; with adaptation to the local context using a few prototypes to promote wellness, exercise, physical activity, and prevention of cognitive decline [22, 69, 70]. To facilitate adherence, each component of the multidomain intervention will be initiated in a stepwise manner (Fig. 3). Due to the COVID-19 pandemic, the intervention will be administered using hybrid method with both physical and virtual sessions. During the physical sessions, strict standard operating procedures (SOP) will be adhered to reduce risk of infections. Body temperature and travel history (if any) of each participant will be taken prior to the intervention. In addition, physical distancing of at least 1 meter apart will be implemented and with the intervention provider using personal protective equipment.
The intervention package will begin with nutritional guidance based on Malaysian Dietary Guidelines for Older Adults [71] and Malaysian Recommended Nutrient Intake for individuals aged 60 years and above [72]. It consists of three individual sessions and nine group sessions that will be conducted within 30 min up to 1 h for a stretch of 24 months. The calorie intake will be calculated using formula of Mifflin St Jeor or Modified Schofield equation [73] while for protein, it is advisable to recommend 1.2 to 1.5 g per kg body weight per day [74]. Meanwhile, group counselling sessions will include discussions that covers topics such as Malaysian Healthy Plate, importance of intake of macronutrient and fiber, menu planning, and how to read food and nutrient information. Each session will be carried out interactively through virtual session that includes online games, slide and video presentation, gardening and cooking demonstration. During individual counselling sessions, a dietitian and nutritionist will provide personalized nutritional needs to participants. The dietitian and nutritionist will count recommended calorie intake for each participant and will provide each participant with a menu plan based on recommended calorie intake that consist of 10 to 20%of daily energy from proteins, 25 to 30%daily energy from fat, and 50 to 65%from carbohydrates. This menu plan will be taught using household measurement.
Psychosocial interventions will be implemented along with nutritional interventions and will follow the Transtheoretical Model (also called the Stages of Change Model) [75]. This model is comprised of five stages: precontemplation, contemplation, preparation, action, and maintenance. Intervention will be divided into two parts, individual and group sessions, where participants in experimental group will be exposed to psychosocial intervention such as social support, resilience, self-efficacy, reminiscing, and coping strategies [31, 76, 77]. Talks led by medical practitioner will be held to create awareness on the importance of healthy aging. Psychologists will conduct sessions to empower intervention group on healthy behavior and coping mechanism to manage their stress that occurs due to reduced health capacity, poor quality of life that arises from material and cognitive aspects as well as lack of emotional relationships or loss of loved ones [78, 79]. Coping strategies are believed to help an individual to use an adjustable mechanism to manage his or her preferences according to the available options such as accepting a disease and managing to live with it [78, 80]. Session for social support will involve participation of the respondents as well as their caregivers during which they will be given a chance to communicate and express their feelings and emotions to their caregivers. Improvement of health-related behaviors among older adults is greatly affected and promoted by good social support from family, friends, and even neighbors [81, 82]. Sharing sessions among the participants will involve individual stories of their own lives biggest challenge and how they overcame it to boost self-efficacy and resilience. Participation in intergenerational programs and meaningful cross-age relationships may decrease social isolation and increase older adults’ sense of belonging, self-esteem, and well-being [83]. For this purpose, activities such as visit to a kindergarten will be organized to enable interactive group session between older adults and children. As a whole, numerous group meetings of all intervention components is expected to stimulate social participation among the participants. Also, two reward sessions will be implemented, intended to support and maintain the new healthy behavior.
Following that, physical activity training will be implemented based on a modified version of the Dose Responses to Exercise Training (DR’s EXTRA) study protocol [84]. The exercise prescription is individually tailored based on the maximum oxygen uptake (VO2max) and repetition maximum (RM) for cardiovascular and muscular components respectively. Participants will undergo treadmill test using Balke Ramp protocol for VO2max assessment. With this, participants will be required to perform 2-min warm up at 1.7 mph and 0%grade followed by walking at 3.0 mph with a gradual increase of 1%per minute until volitional fatigue in another 8 to 10 min [85]. This multi-component group exercise routine will consist of strength, aerobic, postural balance, and stretching training. The intensity of strength training will be progressed based on RM measurements. The number of exercise sessions will be progressive and increased from one to five times a week over a period of 21 weeks. Engagement in more leisure time physical activity will be encouraged and a diary will be provided for the participants to record their activities.
Cognitive training will be guided practice tasks to train global cognition and cognitive domains mainly targeting memory, executive function, visuospatial and language abilities, attention as well as processing speed. Training will be done in individual sessions three times a week for 20 months. The training will make use of the ‘pencil and paper’ cognitive exercises such as crossword puzzle, memory game, word search, maze, and tower of Hanoi. The training module will be culturally adapted to the local context and conducted in Malay to ensure the training is at ease for the older adults as well as fun [86]. Cognitive training administered via ‘paper and pencil’ have been shown to be effective [87, 88]. Efficacy of the training can be preserved by implementing comfortable methods for older adults and for that reason the aforementioned method will be implemented prior to computerized training [86]. The participants will then be sufficiently trained by researchers to engage in mobile-based training before they are expected to independently use their mobiles for the mentioned training.
Whereas for the metabolic and vascular risk factors management, the national evidence-based guidelines [89] will be set as the guideline. Participants will be advised to do follow up with their current physician to monitor and continue their ongoing medical interventions for existing medical conditions.
In order to validate this multidomain intervention module, a panel of healthcare professionals will be recruited to evaluate the suitability of each component in this newly developed module. Then a telerehabilitation module of this multidomain intervention will be programmed, and its feasibility will be tested in location 3 of the study, a rural area of Malaysia. The need assessment of ICT literacy among older adults will be carried out in order to identify the facilitators and barriers to technology use and adoption as well as guide the design of devices. It will be designated with interactive ICT platform comprising of infographics to convey comprehensive information. A videoconference will be included to provide two-way communication between participants and multidisciplinary professionals. A training of the trainer session will be conducted with local volunteers and officers in charge of the care of older adults in the rural area. The acceptance of telerehabilitation module will then be determined based on Technology Acceptance Module (TAM) that assess the content suitability, graphics and design among older adults with cognitive frailty, their caregivers and the stakeholders [90, 91].
Intervention and follow up
The AGELESS study includes 24-month intervention plus 12-month extended follow-up. The outcome measures will be assessed at baseline, on the 6th, 12th, 24th, and 36th month. Interventions will be conducted in individual and group sessions for a stretch of two years, while the extended 12-month follow-up will be allocated to determine the sustainability and long-term effects of the implemented intervention module. During this phase, the respondents will not have to attend any sessions with the researchers. They will be provided home-based education materials according to each domain of the intervention that comes in the form of booklet (nutritional counselling, psychosocial and vascular management), sandbags and exercise booklet (physical training), and cognitive training materials (e.g., puzzles and maze). The multidomain interventions will be continued independently by the participants.
Project timeline and consideration related to the COVID-19 pandemic
The framework for the project was developed in March 2020, when intervention module development and discussion on their implementation had started. This trial has been registered under ISRCTN registry (ISRCTN75429638). The primary investigators along with the research committee will regularly check the study site to ensure the protocol of each intervention is followed carefully.
It is anticipated that participant recruitment and screening will begin in May 2021 in urban area and the intervention is expected to begin in July 2021. With the current COVID-19 pandemic situation, every session will take place using SOP ensuring the safety of the study participants and the research staff. A hybrid approach of recruitment, i.e., minimal face to face and telephone interview will be conducted to optimize recruitment during the COVID-19 pandemic. Each session will be limited to a maximum of ten older adults and physical distancing will be practiced. In person assessments will be minimized by assigning participants with tasks to be completed at home. Empowering and monitoring will be conducted through phone calls, commonly used group messaging; WhatsApp groups and social media platform; Facebook. A recent local study highlighted that ‘senior-friendly’ computer-based interventions and programs are well accepted by older adults [93, 94]. In rural areas, the availability and prevalence of computer usage has increased through computer-buying scheme enforced by the government [95]. Nevertheless, information on readiness and preferences towards this medium of communication will be determined during enrolment of participants.
Control group
The control group will undergo regular health monitoring that includes blood pressure and anthropometry measurements as well as blood testing (cholesterol, glucose HbA1C, troponin, nitric oxide). They will also receive group counselling sessions, health talks, and advice based on standard public health pamphlets from Ministry of Health during the 6th, 12th, 24th, and 36th month follow up.
Cost effectiveness analysis
The cost effectiveness analysis is conducted to measure the cost effectiveness of the multi domain intervention comparing two groups namely control and intervention groups for each intervention. The cost analysis of each intervention group will be calculated using top down and activity-based costing [96]. The cost estimated in this study is only from the provider cost. The effectiveness or outcomes variables of each intervention as described above will be selected from the bivariate analysis findings and also from the experts’ team for the cost effectiveness analysis.
The cost effectiveness ratio (CER) and incremental cost effectiveness ratio (ICER) will be the secondary outcomes for this study. The CER is the ratio between cost and effect for both groups. The ICER is used in cost-effectiveness analysis to explain the cost-effectiveness of a health care intervention. The formula is defined by the difference in cost between two possible interventions, divided by the difference in their effect. It represents the average incremental cost associated with 1 additional unit of the measure of effect [97].
The CER and ICER formula as shown below:
CER = Cost / Effect
ICER = Ca –Cb / Ea– Eb
Where;
Ca = cost of intervention among control group
Cb = cost of multi domain intervention among intervention group
Ea = effect of intervention among control group
Eb = effect of multi domain intervention among intervention group
Costs are in monetary units, effects measured in terms of health status and outcome from expert team
Modelling personalized rehabilitation approach to reduce risk of cognitive frailty
In Phase 3, the personalized rehabilitation module to reverse CF will be remodeled based on the analysis of Phase 1 and 2. Feasibility study and implementation in an urban area as well as semi urban area and feasibility of telerehabilitation in a rural area of Malaysia will be conducted. The significant strategies from Phase 1 and 2 will be integrated into a module in the hope for implementation for the reversal of CF in the future through an ICT platform (Apps, web). This model is an expansion from established prototypes from an ongoing project ‘Warga Emas Sihat’ (WE Sihat) which means healthy senior citizens [93]. The model will include element and strategy for personalized rehabilitation including screening, program or activities, monitoring and alert system to be used mainly by stakeholders involved in the care of older adults (policy makers, public health strategists, health care professionals, local volunteers, and care givers). Such application will provide standardized protocol and easy to use treatment guidelines to support as well as monitor the prevention and management of older adults with risk of cognitive frailty.
Upon completion of the model, a round table and focus group discussion will be conducted among 30 stake holders as mentioned above to determine the acceptance using formative and summative proforma.
Statistical analysis
Statistical Package for Social Sciences (SPSS) software, version 23.0 will be used for all the statistical analysis in this study. An alpha level of (0.05) will considered for all the statistical tests. Two-sided p values of (0.05) and (80%) power will be statistically significant. Results of Phase 2 (RCT) will be analyzed through repeated measures analysis of variance for pre-test (Baseline Scores) and post-test (3rd month, 6th month, 12th month, 24th month, and 36th month) for intervention and active control group. All the nutritional, psychosocial, cognitive, vascular, and physical outcomes measures will be used for statistical analysis. The Benferonni correction will be used for post-hoc analysis.
Relevance to government policy
The project is in-line with the National Plan of Action for Older Persons and the National Health Policy and Action Plan for Older Persons (11th Malaysian Plan) under the Ministry of Women and Family Development. Outcomes of this project is also valuable for updating the National Non-Communicable Diseases Strategic Plan under the Ministry of Health Malaysia.
Data management
The study will be executed in accordance with Good Clinical Practice (GCP). This project will be part of the Worldwide FINGER Trials, of which common identifiable data will be shared among the consortia. Therefore, we will, as much as the current research infrastructure available to us, adhere to two basic principles: 1) Data Protection: to ensure the anonymity and privacy of our participants; 2) Data Sharing: to ensure that data from publicly funded research is publicly available We will ensure that all institutional Data Protection requirements are followed. Potentially identifiable personal data will be stored only within secure locations and electronic data in local secure servers, as stipulated within the Personal Data Protection Act 2010. We would be anonymizing data and enlisting our institutional librarians to assist with data curation before then depositing our data in an open data repository within 12 months of completion of the project.
All physical materials such as consent forms, completed questionnaires, and demographic details will be secured in a locked cabinet at the research center within UKM. To respect participants’ privacy, they will each be assigned a numerical code. Participant names or other identifying features will not appear in any form of data reporting. The coding system will be stored digitally and manually at UKM and will only be accessible to members of the research team.
Ethics and dissemination
Written informed consent will be obtained from all participants. Every participant has the right to withdraw from the study at any time and participation is solely on voluntary basis. Findings of this study will be disseminated through conference presentations and peer-reviewed publications. The results will be shared with the World FINGERS network for comparison purposes as well as to add novel local evidence on CF.
DISCUSSION
This study is to identify if multidomain intervention can reverse or delay CF in older populations, similar to the ongoing FINGER study [23, 24]. The Worldwide FINGERS network is the first global network of multidomain trials for prevention of dementia involving over 25 countries [23]. Most RCTs target people in the at-risk spectrum of dementia, but the AGELESS Trial is one of the few studies that includes physical frailty. Nevertheless, none of the studies targeted dual outcome of CF and assessed the sustainability for a longer period of time.
Also, the key strength of the current study in comparison to other ongoing projects is the involvement of psychosocial domain as part of the intervention. Psychological distress has been reported to be associated with cognitive impairment as well as physical frailty in a recent study [98]. However, this study was focused only on the rural population [98]. Therefore, the findings from our current study are expected to fill the literature gap by involving older adults from both rural and urban areas. Without addressing the psychosocial wellbeing of an older adult, the likelihood of participation in an intervention would be less than optimal [99]. In addition, this study is in line with World Health Organization (WHO) Global action plan on the public health response to dementia 2017–2025, the WHO guidelines for risk reduction of cognitive decline and dementia [100, 101] as well as the recommendations from the latest report of the Lancet Commission on dementia prevention, intervention, and care [102]. The study provides much needed knowledge and data on risk factors for dementia as this information is lacking in evidence, and is at the forefront of local efforts for integrative and innovative approaches to develop effective and sustainable preventive interventions for the Malaysia population and countries with similar cultural geographical and societal settings
Besides that, the key deliverables include novel understanding of physiological, environmental, and psychosocial variabilities in response to intervention, leading to personalized rehabilitation reversing CF. Findings of environmental and psychosocial factors influencing adherence toward intervention may lead to better formulation of public health strategies involving older adults. The multidomain intervention is considered as a possible strategy to contain the health care cost for older adults [6]. The integrated intervention consolidated in an ICT application has the potentials to be up scaled as a nationwide program, in particular during this COVID-19 pandemic, providing innovative examples to other developing countries which are aging population. On the downside, conducting this study during the pandemic is rather challenging considering the target population are the most vulnerable group for infectious diseases. In order to reduce the risk of spread of infections between participants, this current study will emphasize virtual training sessions. Other strategies to ensure the success in recruitment and participants’ retention throughout the study during this pandemic are to involve and train local managers at each study cites. Although the training modules will be mainly in Malay language, bilingual (Malay and English) modules for generalization of the module globally will be available.
ACKNOWLEDGMENTS
We thank researchers from AGELESS Project, in particular Prof Tan Maw Pin for taking the lead in obtaining fund for the program; staffs from the Centre for Healthy Aging and Wellness (HCare), Faculty of Health Sciences, Universiti Kebangsaan Malaysia for technical assistance; and the World Wide FINGERS Trial Network for sharing methodology and experiences in conducting multidomain intervention. Funding of this study was obtained from the Ministry of Higher Education of Malaysia under the Long Term Research Grant Scheme (LRGS/1/2019/UM-UKM/1/4).
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/20-1607r1).
REFERENCES
[1] | Tengku AH , Nurizan Y ((2008) ) National policy for the elderly in Malaysia: Achievements & challenges. Aging in Southeast and East Asia. 1st Edition. Institute of Southeast Asian Studies, Singapore. |
[2] | Sourdet S , Rouge-Bugat ME , Vellas B , Forette F ((2012) ) Frailty and aging. J Nutr Health Aging 16: , 283–284. |
[3] | Fried LP , Tangen CM , Walston J , Newman AB , Hirsch C , Gottdiener J , Seeman T , Tracy R , Kop WJ , Burke G , McBurnie MA , Cardiovascular Health Study Collaborative Research Group ((2001) ) Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56: , 146–157. |
[4] | Fried LP , Ferrucci L , Darer J , Williamson JD , Anderson G ((2004) ) untangling the concepts of disability, frailty and comorbidity: Implications for improved targeting and care. J Gerontol 59: , 255–263. |
[5] | Gobbens RJJ , van Assen MALM ((2017) ) Associations between multidimensional frailty and quality of life among Dutch older people. Arch Gerontol Geriatr 73: , 69–76. |
[6] | Alkhodary AA , Aljunid SM , Ismail A , Nur AM , Shahar S ((2020) ) The economic burden of frailty among elderly people: A review of the current literature. Malaysian J Public Health Med 20: , 224–232. |
[7] | Morley JE , Morris JC , Berg-weger M , Borson S , Carpenter BD , del Campo N , Dubois B , Fargo K , Fitten LJ , Flaherty JH , Ganguli M , Grossberg GT , Malmstorm TK , Petersen RD , Rodriguez C , Saykin AJ , Scheltens P , Tangalos EG , Verghese J , Wilcock G , Winblad B , Woo J , Vellas B ((2015) ) Brain health: The importance of recognizing cognitive impairment: An IAGG consensus conference. J Am Med Dir Assoc 16: , 731–739. |
[8] | Chen W , Wang H ((2013) ) Mild cognitive impairment: A concept useful for early detection and intervention of dementia. Shanghai Arch Psychiatry 25: , 119–120. |
[9] | Sargent L , Brown R ((2016) ) Assessing the current state of cognitive frailty: Measurement properties. J Nutr Health Aging 21: , 152–160. |
[10] | Franceschi C , Campisi J ((2014) ) Chronic inflammation (Inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci 69: , 4–9. |
[11] | Ferrucci L , Fabbri E ((2018) ) Inflammageing: Chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol 15: , 505–522. |
[12] | Haaksma ML , Vilela LR , Marengoni A , Caldero A , Leoutsakos J S , Rikkert MGMO ((2017) ) Comorbidity and progression of late onset Alzheimer’s disease: A systematic review. PLoS One 15: , e0177044. |
[13] | Murukesu RR , Singh DKA , Subramaniam P , Tan XV , Mohamd Izhar IA , Ponvel P , Rasdi HFM ((2019) ) Prevalence of frailty and its association with cognitive status and functional fitness among ambulating older adults residing in institutions within west coast of Peninsular Malaysia. Int J Environ Res Public Health 16: , 4716. |
[14] | Panza F , Lozupone M , Solfrizzi V , Sardone R , Dibello V , Di Lena L , D’Urso F , Stallone R , Petruzzi M , Giannelli G , Quaranta N , Bellomo A , Greco A , Daniele A , Seripa D , Logroscino G ((2018) ) Different cognitive frailty models and health-and cognitive-related outcomes in older age: From epidemiology to prevention. J Alzheimers Dis 62: , 993–1012. |
[15] | Kelaiditi E , Cesari M , Canevelli M , van Kan GA , Ousset PJ , Gillette-Guyonnet , Ritz P , Duveau F , Soto ME , Provencher V , Nourhashemi F , Salva A , Robert P , Andrieu S , Rolland Y , Touchon J , Fitten JL , Vellas B ((2013) ) Cognitive frailt: Rational and definition from an (I.A.N.A./I.A.G.G.) International Consensus Group. J Nutr Health Aging 17: , 726–734. |
[16] | Ng TP , Feng L , Shwe M , Nyunt Z , Larbi A ((2014) ) Frailty in older persons: Multisystem risk factors and the Frailty Risk Index (FRI). J Am Med Dir Assoc 15: , 635–642. |
[17] | Esteban-Cornejo I , Rodriguez-Ayllon M , Verdejo-Roman J , Cadenas-Sanchez C , Mora-Gonzalez J , Chaddock-Heyman L , Raine LB , Stillmnan CM , Kramer AF , Erickson KI , Catena A , Ortega FB , Hillman CH ((2019) ) Physical fitness, white matter volume and academic performance in children: Findings from the ActiveBrains and FITKids2 Projects. Front Psychol 10: , 208. |
[18] | Feng L , Nyunt MSZ , Gao Q , Feng L , Lee TS , Tsoi T , Chong MS , Lim WS , Collinson S , Yap P , Yap KB , Ng TP ((2017) ) Physical frailty, cognitive impairment, and the risk of neurocognitive disorder in the Singapore Longitudinal Ageing Studies. J Gerontol 72: , 369–375. |
[19] | Solfrizzi V , Scafato E , Seripa D , Lozupone M , Imbimbo BP , D’Amato A , Tortellu R , Schilardi A , Galluzo L , Gandin C , Baldereschi M , Di Carlo A , Intizari D , Daniele A , Sabba C , Logroscino G , Panza F , Italian Longiutudinal Study on Aging Working Group ((2016) ) Reversible cognitive frailty, dementia, and all-cause mortality. The Italian longitudinal study on aging. J Am Med Dir Assoc 18: , 89.e1–89.e8. |
[20] | Rivan NFM , Shahar S , Rajab NF , Singh DKA , Din NC , Hazlina M , Hamid TATA ((2019) ) Cognitive frailty among Malaysian older adults: Baseline findings from the LRGS TUA cohort study. Clin Interv Aging 14: , 1343–1352. |
[21] | Rivan NFM , Shahar S , Rajab NF , Singh DKA , Din NC , Mahadzir H , Sakian NIM , Ishak WS , Rahman MHA , Mohammed Z , You YX ((2020) ) Incidence and predictors of cognitive frailty among older adults: A community-based longitudinal study. Int J Environ Res Public Health 6: , 1547. |
[22] | Murukesu RR , Singh DKA , Shahar S , Subramaniam P ((2020) ) A Multi-domain intervention protocol for the potential reversal of cognitive frailty: “WE-RISE” randomized controlled trial. Front Public Health 8: , 471. |
[23] | Yoon DH , Lee JY , Song W ((2018) ) Effects of resistance exercise training on cognitive function and physical performance in cognitive frailty: A randomized controlled trial. J Nutr Health Aging 22: , 944–951. |
[24] | Guyonnet S , Secher M ((2015) ) Nutrition, frailty, cognitive frailty and prevention of disabilities with aging. Nestle Nutr Inst Workshop Ser 82: , 143–152. |
[25] | Ge S , Zhu Z , Wu B , Mcconnell ES ((2018) ) Technology-based cognitive training and rehabilitation interventions for individuals with mild cognitive impairment: A systematic review. BMC Geriatr 18: , 213. |
[26] | Ng TP , Feng L , Nyunt MSZ , Feng L , Niti M , Tan, BY , Chan G , Khoo SA . Chan SM , Yap P , Yap KB ((2015) ) Nutritional, physical, cognitive and combination interventions and frailty reversal among older adults: A randomized controlled trial. Am J Med 128: , 1225–1236. |
[27] | Kivipelto M , Solomon A , Ahtiluoto S , Ngandu T , Lehtisalo J , Antikainen R , Backman L , Hanninen T , Jula A , Laatikainen T , Lindstrom J , Mangialasche F , Nissinen A , Paajanen T , Pajala S , Peltonen M , Rauramaa R , Stigsdotter-Neely A , Strandberg T , Tuomilehto J , Soininen H ((2013) ) The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER): Study design and progress. Alzheimers Dement 13: , 657–665. |
[28] | Ngandu T , Lehtisalo J , Levälahti E , Laatikainen T , Lindström J , Peltonen M , Solomon A , Ahtiluoto S , Antikainen R , Hanninen T , Jula A , Mangialasche F , Paajanen T , Pajala S , Raurama R , Strandberg T , Tuomihelto J , Soinene H , Kivipelto M ((2014) ) Recruitment and baseline characteristics of participants in the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER)—A randomized controlled lifestyle trial. Int J Environ Res Public Health 11: , 9345–9360. |
[29] | Ngandu T , Lehtisalo J , Solomon A , Levalahti E , Ahtiluoto S , Antikainen R , Backman L , Hannien T , Jula A , Laatikainen T , Lindstrom J , Mangialasche F , Paajanen T , Pajala S , Peltonen M , Rauramaa R , Stigsdotter-Neely A , Strandberg T , Tuomihelto J , Soininen H , Kivipelto M ((2015) ) A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 385: , 2255–2263. |
[30] | Makizako H , Shimada H , Doi T , Tsutsumimoto K , Hotta R ((2018) ) Social frailty leads to the development of physical frailty among physically non-frail adults: A four-year follow-up longitudinal cohort study. Int J Environ Res Public Health 15: , 490–499. |
[31] | Chow G , Gan JKE , Chan JKY , Wu XV , Yobas PK (2020) Effectiveness of psychosocial interventions among older adults with mild cognitive impairment: A systematic review and meta-analysis. Aging Ment Health, doi: 10.1080/13607863.2020.1839861 |
[32] | Bier N , Grenier S , Brodeur C , Gauthier S , Gilbert B , Hudon C , Lepage E , Ouellet MC , Viscogliosi C , Belleville S ((2015) ) Measuring the impact of cognitive and psychosocial interventions in persons with mild cognitive impairment with a randomized single-blind controlled trial: Rationale and design of the MEMO+study. Int Psychogeriatr 27: , 511–525. |
[33] | Maggio MG , de Luca R , Manuli A , Salvatore R ((2020) ) The five “W” of cognitive telerehabilitation in the Covid-19 era. Expert Rev Med Devices 17: , 473–475. |
[34] | Cotelli M , Manenti R , Brambilla M , Gobbi E , Ferrari C , Binetti G , Cappa SF ((2019) ) Cognitive telerehabilitation in mild cognitive impairment, Alzheimer’s disease and frontotemporal dementia: A systematic review. J Telemed Telecare 25: , 67–79. |
[35] | Jansson MM , Rantala A , Miettunen J , Puhto A , Pikkarainen M (2020) The effects and safety of telerehabilitation in patients with lower-limb joint replacement: A systematic review and narrative synthesis. J Telemed Telecare, doi: 10.1177/1357633X20917868. |
[36] | Peterson S , Kuntz C , Roush J ((2018) ) Use of a modified treatment-based classification system for subgrouping patients with low back pain: Agreement between telerehabilitation and face-to-face assessments. Physiother Theory Pract 35: , 1078–1086. |
[37] | Turolla A , Rossettini G , Viceconti A , Palese A , Geri T ((2020) ) Musculoskeletal physical therapy during the COVID-19 pandemic: Is telerehabilitation the answer? Phys Ther 100: , 1260–1264. |
[38] | Bernocchi P , Giordano A , Pintavalle G , Galli T , Ballini E , Baratti D , Scalvini S ((2019) ) Feasibility and clinical efficacy of a multidisciplinary home-telehealth program to prevent falls in older adults: A randomized controlled trial. J Am Med Dir Assoc 20: , 340–346. |
[39] | Jiang S , Xiang J , Gao X , Guo K ((2018) ) The comparison of telerehabilitation and face-to-face rehabilitation after total knee arthroplasty: A systematic review and meta-analysis. J Telemed Telecare 24: , 257–262. |
[40] | Shukla H , Nair SR , Thakker D ((2017) ) Role of telerehabilitation in patients following total knee arthroplasty: Evidence from a systematic literature review and meta-analysis. J Telemed Telecare 23: , 339–346. |
[41] | Kruse SC , Karem P , Shifflett K , Vegi L , Ravi K , Brooks M ((2018) ) Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare 24: , 4–12. |
[42] | Kruse C , Fohn J , Wilson N , Nunez Patlan E , Zipp S , Mileski M ((2020) ) Utilization barriers and medical outcomes commensurate with the use of telehealth among older adults: Systematic Review. JMIR Med Inform 8: , e20359. |
[43] | Hassibian MR , Hassibian S ((2016) ) telemedicine acceptance and implementation in developing countries: Benefits, categories, and barriers. Razawi Int J Med 4: , e38332. |
[44] | Kivipelto M , Allegri R , Caramelli P , Mangialasche F , Andrieu S , Snyder HM , Baker L , Belleville S , Brodaty H , Brucki SM , Calandri I , Caramelli P , Chen C , Chertkow H , Chew E , Choi SH , Chowdhary N , Crivelli L , Torre RDL , Du Y , Dua T , Espelanmd M , Feldman HH , Hartmanis M , Hartman T , Heffernan M , Henry CJ , Hong CH , Hakansson K , Iwatsubo T , Jeong JH , Jimenez-Manggiora G , Koo EH , Launer LJ , Lehtisalo J , Lopera F , Martinenz-Lage P , Martins R , Middleton L , Molinuevo JL , Montero-Odasso M , Moon SY , Morales-Perez K , Nitrini R , Nygaard HB , Park YK , Peltonen M , Qiu C , Quiroz YT , Raman R , Rao N , Ravindranath V , Rosenberg A , Sakurai T , Salinas RM , Scheltens P , Sevlever G , Soininen H , Sosa AL , Suemoto CK , Tainta-Cuezva M , Velilla L , Wang Y , Whitmer R , Xu X , Bain LJ , Solomon A , Ngandu T , Carrillo MC ((2020) ) World-Wide FINGERS Network: A global approach to risk reduction and prevention of dementia. Alzheimers Dement 16: , 1078–1094. |
[45] | Bossers WJ , van der Woude LH , Boersma F , Hortobágyi T , Scherder EJ , van Heuvelen MJ ((2015) ) A 9-week aerobic and strength training program improves cognitive and motor function in patients with dementia: A randomized, controlled trial. Am J Geriatr Psychiatry 23: , 1106–1116. |
[46] | Folstein M , Folstein S , McHugh P ((1975) ) Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. J Psychiat Res 12: , 189–198. |
[47] | Urbaniak G , Plous S (2013) Research Randomizer (Version 4.0) (Available online at: http://www.randomizer.org/) |
[48] | Za Z , Zahiruddin O , Ah CW ((2007) ) Validation of Malay Mini Mental State Examination. Malaysian J Psychiatry 16: , 16–19. |
[49] | Morris JC ((1997) ) Clinical Dementia Rating: A reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int Psychogeriatr 9: , 173–176. |
[50] | Wan Mahmud WM , Awang A , Herman I , Mohamed MN ((2004) ) Analysis of the psychometric properties of the Malay version of Beck Depression Inventory II (BDI-II) among postpartum women in Kedah, North West of Peninsular Malaysia. Malays J Med Sci 11: , 19–25. |
[51] | Singh DKA , Najwatul NAA , Rajaratnam BS , Yi TC ((2018) ) Original article validity and reliability of Physical Activity Scale for Elderly in Malay language (PASE-M). Malays J Public Health Med 1: , 116–123. |
[52] | Gordon NP , Hornbrook MC ((2018) ) Older adults’ readiness to engage with eHealth patient education and self-care resources: A cross-sectional survey. BMC Health Serv Res 18: , 1–13. |
[53] | Harrison J , Minassian SL , Jenkins L , Black RS , Koller M , Grundman M ((2007) ) A neuropsychological test battery for use in Alzheimer disease clinical trials. Arch Neurol 64: , 1323–1329. |
[54] | Rikle RE , Jones CJ ((2001) ) Senior fitness test manual, 2nd edition. Human Kinetics, Champaign, IL. |
[55] | Hidrus A , Kueh YC , Norsa B ((2020) ) Malay version of Exercise Self-Efficacy: A confirmatory analysis among Malaysians with type 2 diabetes mellitus. Int J Environ Res Public Health 17: , 922–934. |
[56] | Slonim NB , Gillespie DG , Harold WH ((1957) ) Peak oxygen uptake of healthy young man as determined by a treadmill method. J Appl Physiol 10: , 401–404. |
[57] | Norhayati MN , Aniza AA , Hussain N , Hazlina N , Azman MY ((2015) ) Psychometric properties of the revised Malay version Medical Outcome Study Social Support Survey using confirmatory. Asia Pac Psychiatry 7: , 398–405. |
[58] | Isa SNI , Ismarulyusda I , Azriani A ((2017) ) Perceived stress and coping styles among Malay caregivers of children with learning disabilities in Kelantan. Malays J Med Sci 24: , 81–93. |
[59] | Gierveld JDJ , Tilburg Van T ((2006) ) A 6-Item Scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Res Aging 28: , 582–598. |
[60] | Connor KM , Davidson JRT ((2003) ) Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 18: , 76–82. |
[61] | Malek MA (2018) Pembinaan modul kebolehsesuaian kerjaya bagi meningkatkan kebolehsesuaian kerjaya,harapan dan efikasi kendiri dalam kalangan penghuni penjara, thesis UKM. PhD dissertation UKM. unpublished work. |
[62] | Jusoh MR (2015) The effectiveness of psychoeducational group therapy to motivate change among addicts in the early stages of change. PhD dissertation USIM. unpublished work. |
[63] | Shahar S , Earland J ((2000) ) Validation of a Dietary History Questionnaire against a 7-D weighed record for estimating nutrient intake among rural elderly Malays. Malays J Nutr 6: , 33–44. |
[64] | Novotný M , Klimova B , Valis M ((2020) ) Microbiome and cognitive impairment: can any diets influence learning processes in a positive way? Front Aging Neurosci 11: , 170. |
[65] | Kikuchi T , Miller JM , Schneck N , Oquendo MA , Mann JJ , Parsey RV , Keilp JG ((2012) ) Neural responses to incongruency in a blocked-trial Stroop fMRI task in major depressive disorder. J Affect Disord 143: , 241–247. |
[66] | Othman EA , Yusoff AN , Mohamad M , Manan HA , Hamid AIA , Giampietro V ((2019) ) Hemispheric lateralization of auditory working memory regions during stochastic resonance: An fMRI study. J Magn Reson Imaging 51: , 1821–1828. |
[67] | Dickerson BC , Sperling RA ((2008) ) Functional abnormalities of the medial temporal lobe memory system in mild cognitive impairment and Alzheimer’s disease: Insights from functional MRI studies. Neuropsychologia 46: , 1624–1635. |
[68] | Van Dalen JW , van Charante EPM , Caan MWA , Scheltens P , Majoie CBLM , Nederveen AJ , Gool WA , Richard E ((2017) ) Effect of long-term vascular care on progression of cerebrovascular lesions. Stroke 7: , 1842–1848. |
[69] | Vanoh D , Shahar S , Razali R , Ali NM , Manaf ZA , Noah SAM , Nur AM ((2019) ) The effectiveness of a Web-Based Health Education Tool, WESIHAT 2.0, among older adults: A randomized controlled trial. J Alzheimers Dis 70: , 255–270. |
[70] | Johari SM , Shahar S , Ng TP , Rajikan R ((2014) ) A preliminary randomized controlled trial of multifaceted educational intervention for mild cognitive impairment among elderly Malays in Kuala Lumpur. Int J Gerontology 8: , 74–80. |
[71] | National Coordinating Committee on Food and Nutrition (NCCFN) (2010) Malaysian Dietary Guidelines. Putrajaya: Ministry of Health. |
[72] | National Coordinating Committee on Food and Nutrition (NCCFN) (2017). Recommended Nutrient Intakes for Malaysia. Putrajaya: Ministry of Health. |
[73] | Reidlinger DP , Willis JM , Whelan K ((2015) ) Resting metabolic rate and anthropometry in older people: A comparison of measured and calculated values. J Hum Nutr Diet 28: , 72–84. |
[74] | Bauer J , Biolo G , Cederholm T , Cesari M , Cruz-Jentoft AJ , Morley JE , Philips S , Sieber C , Stehle P , Teta D , Visvanathan R , Volpi E , Boirie Y ((2013) ) Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the PROT-AGE study group. J Am Med Dir Assoc 14: , 542–559. |
[75] | Prochaska JO , DiClemente CC ((2005) ) The transtheoretical approach. In: Handbook of psychotherapy integration, 2nd edition, Norcross JC, Goldfried MR, eds. Oxford University Press, New York, pp. 147–171. |
[76] | Forsman AK , Nordmyr J , Wahlbeck K ((2011) ) Psychosocial interventions for the promotion of mental health and the prevention of depression among older adults. Health Promot Int 26: , 85–107. |
[77] | Forsman AK , Schierenbeck I , Wahlbeck K ((2011) ) psychosocial interventions for the prevention of depression in older adults: Systematic review and meta-analysis. J Aging Health 23: , 387–416. |
[78] | Dockendorff DCT ((2014) ) Healthy ways of coping with losses related to the aging process healthy ways of coping with losses related to the aging process. Edu Gerontol 40: , 363–384. |
[79] | Skinner EA , Edge K , Altman J , Sherwood H ((2003) ) Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychol Bull 129: , 216–269. |
[80] | Ribeiro S , Borges S , Araujo TCCF , Souza MCDS ((2017) ) Coping strategies used by elderly regarding aging and death: An integrative interview. Rev Bras Geriatr Gerontol 20: , 869–877. |
[81] | Thanakwang K , Soonthorndhad K ((2011) ) Mechanisms by which social support networks influence healthy aging among Thai dwelling elderly. J Aging Health 23: , 1352–1378. |
[82] | Wu F , Sheng Y ((2019) ) Social support network, social support, self-efficacy, health-promoting behavior and healthy aging among older adults: A pathway analysis. Arch Gerontol Geriatr 84: , 103934. |
[83] | Park A ((2015) ) Do intergenerational activities do any good for older adults well-being?: A brief review. J Gerontol Geriatr Res 3: , 3–6. |
[84] | Komulainen P , Kivipelto M , Lakka TA , Savonen K , Hassinen M , Kiviniemi V , Hänninen T , Rauramaa R ((2010) ) Exercise, fitness and cognition - A randomised controlled trial in older individuals: The DR’s EXTRA study. Eur Geriatr Med 1: , 266–272. |
[85] | Petrella RJ , Koval JJ , Cunningham DA , Paterson DH ((2001) ) A self-paced step test to predict aerobic fitness in older adults in the primary care clinic. J Am Geriatr Soc 49: , 632–638. |
[86] | Alnajjar F , Khalid S , Vogan AA , Shimoda S , Nouchi R ((2019) ) Emerging cognitive intervention technologies to meet the needs of an aging population: A systematic review. Front Aging Neurosci 9: , 291. |
[87] | Bahar-Fuchs A , Martyr A , Amy G , Sabates J , Clare L ((2019) ) Cognitive training for people with mild to moderate dementia. Cochrane Database Syst Rev 7: , CD013069. |
[88] | Ng TP , Hui L , Ling A , Feng L , Shwe M , Nyunt Z , Feng L , Niti M , Tan BY , Khoo SA , Chan SM , Yap P , Yap KB ((2018) ) Cognitive effects of multi-domain interventions among pre-frail and frail community-living older persons: Randomized controlled trial. J Gerontol A Biol Sci Med Sci 73: , 806–812. |
[89] | (2017) Clinical Practice Guidelines on Primary & Secondary Prevention of Cardiovascular Disease. http://www.moh.gov.my |
[90] | Davis FD , Bagozzi RP , Warshaw PR ((1989) ) User acceptance of computer technology: A comparison of two theoretical models. Manage Sci 35: , 982–1003. |
[91] | Venkatesh V , Davis FD ((2000) ) A theoretical extension of the technology acceptance model: Four longitudinal field studies. Manage Sci 46: , 186–204. |
[92] | Malaysian Communications and Multimedia Commission (2017) Internet users survey. Malaysian Communications and Multimedia Commission, Cyberjaya. |
[93] | Vanoh D , Ishak IH , Shahar S , Manaf ZA , Ali NM , Azman S , Noah M ((2018) ) Development and assessment of a web-based intervention for educating older people on strategies promoting healthy cognition. Clin Interv Aging 17: , 1787–1798. |
[94] | Azizam NA , Ismail A , Sulong S , Nor NM ((2019) ) Cost-effectiveness analysis of psoriasis treatment modalities in Malaysia. Int J Health Policy Manag 8: , 394–402. |
[95] | Kamaruddin K , Jusoh O ((2008) ) Adult computer literacy programme in rural areas in peninsular Malaysia. J Hum Resour Adult Learn 4: , 142–153. |
[96] | Aniza I , Saperi S , Aljunid SM ((2015) ) Carta alir klinikal penjagaan dan kawalan kos rawatan. UKM Press. |
[97] | Drummond M , McGuire A ((2001) ) Economic evaluation in health care: Merging theory with practice. Int J Epidemiol 31: , 877–878. |
[98] | Jing Z , Li J , Wang Y , Ding L , Tang X , Feng Y , Zhou C ((2020) ) The mediating effect of psychological distress on cognitive function and physical frailty among the elderly: Evidence from rural Shandong, China. J Affect Disord 268: , 88–94. |
[99] | Dedeyne L , Deschodt M , Verschueren S , Tournoy J , Gielen E ((2017) ) Effects of multi-domain interventions in (pre) frail elderly on frailty, functional, and cognitive status: A systematic review. Clin Interv Aging 24: , 873–896. |
[100] | WHO (2017) Global action plan on the public health response to dementia 2017–2025, World Health Organization. |
[101] | WHO (2019) Risk reduction of cognitive decline and dementia, World Health Organization. |
[102] | Livingston G , Huntley J , Sommerlad A , Ames D , Ballard C , Banerjee S , Brayne C , Burns A , Cohen-Mansfield J , Cooper C , Costafreda SG , Dias A , Fox N , Gitlin LN , Howard R , Kales HC , Kivimäki M , Larson EB , Ogunniyi A , Orgeta V , Ritchie K , Rockwood K , Sampson EL , Samus Q , Schneider LS , Selbæk G , Teri L , Mukadam N ((2020) ) Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396: , 413–446. |

![AGELESS Trial Protocol adapted and modified from [23].](https://content.iospress.com:443/media/jad/2021/82-2/jad-82-2-jad201607/jad-82-jad201607-g003.jpg)


