More Information
Submitted: May 24, 2022 | Approved: June 01, 2022 | Published: June 02, 2022
How to cite this article: Chaachou A, Cherni N, Ferjaoui W, Dridi M. Ghozzi S. Ectopic adrenal tissue at the spermatic cord. J Clin Med Exp Images. 2022; 6: 001-002.
DOI: 10.29328/journal.jcmei.1001024
Copyright License: © 2022 Chaachou A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Ectopic adrenal tissue at the spermatic cord
Abdallah Chaachou1, Nizar Cherni1, Wael Ferjaoui2*, Mohamed Dridi1 and Samir Ghozzi1
1Department of Urology, Military Hospital of Tunis, Tunisia
2Department of General Surgery, Military Hospital of Tunis, Tunisia
*Address for Correspondence: Wael Ferjaoui, Department of General Surgery, Military Hospital of Tunis, Tunisia, Email: farjaouiwael4@gmail.com
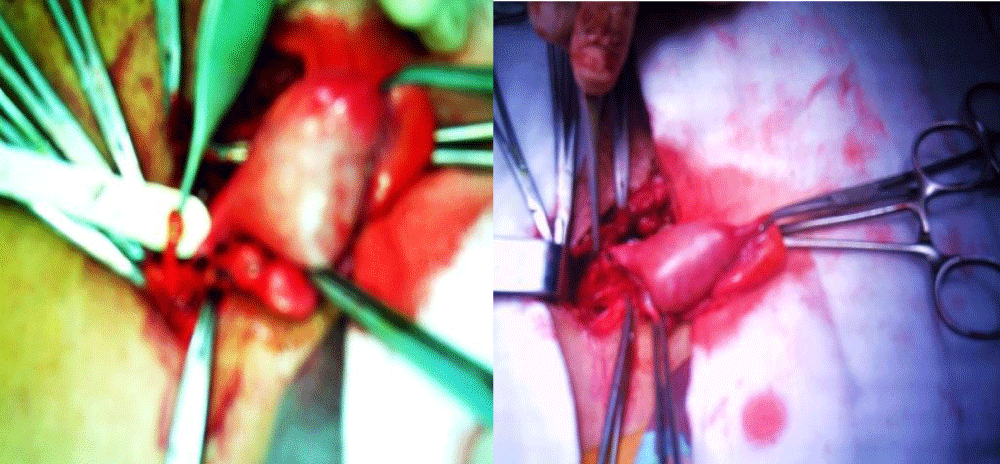
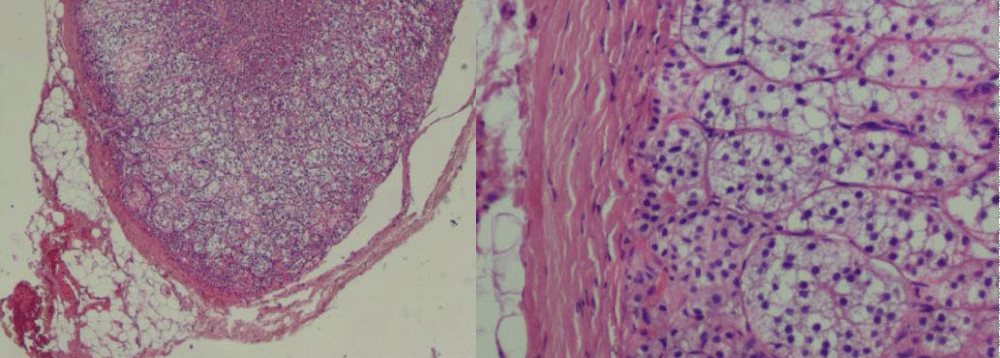
This is a 19-year-old patient. His clinical examination finds an empty bursa with a palpable left testicle at the level of the inguinal canal. The ultrasound shows a right testicle at the pelvic level and a left testicle with an average inguinal location of 30/15 mm long axis. The patient underwent a lowering of the left testicle. The right testicle was intra-abdominal with a very short vas deferens and a cord, the seat of a small buff-yellow oval nodule of 5 mm requiring its ablation, associated with orchiectomy (Figure 1). The postoperative period was uneventful. The anatomopathological examination concluded cortico-adrenal tissue at the level of the spermatic cord with hypo spermatogenesis at the level of testicular sampling (Figure 2).
Figure 1: The right testicle was intra-abdominal with a very short vas deferens and a cord, the seat of a small buff-yellow oval nodule of 5 mm requiring its ablation, associated with orchiectomy.
Figure 2: The anatomopathological examination concluded to cortico-adrenal tissue at the level of the spermatic cord with hypo spermatogenesis at the level of testicular sampling.
In children operated on for inguinal hernia or cryptorchidism, the frequency of adrenal ectopia varies from 3.5% to 15% of cases [2]. It is reduced to 1.96% in adolescents with cryptorchidism [3].
In the majority of cases, adrenocortical ectopia is asymptomatic.
It exceptionally produced an inguinoscrotal mass requiring surgical excision.
Most often, it is a fortuitous discovery during treatment of inguinal hernia, hydrocele, or testicular ectopia as in our patient. It is distinguished by the isolated presence of adrenocortical tissue.
The absence of a medullary component confirms the congenital nature of ectopia [1].
Embryologically, the adrenal cortex arises from clusters of mesenchymal cells in the mesoderm located between the root of the dorsal mesentery and the gonadal buds.
The adrenal medulla, which derives from the neural crest, forms long after the appearance of the adrenal cortex.
The simultaneous development of gonadal buds around the sixth week of embryonic life and their early migration into the pelvis would be responsible for the anomaly.
The topography of the ectopic tissue is explained by the anatomical intimacy between the adrenal cortex and the primitive gonads during their descent into the pelvis in women (fallopian tubes and ovaries) or the scholarships in men (vas deferens, epididymis, testis) [1,4,5].
The islands of the ectopic adrenal cortex, scattered along their course, make one or more dark yellow nodules, standing out from the neighboring connective-adipose tissue. Rarely, they are confined to the retroperitoneal space, between the diaphragm and the pelvis, or remain included even in the neighboring viscera (lungs and kidneys).
Most often, ectopic tissue atrophies and disappears during childhood. Exceptionally, it persists at an advanced age as in our patient and can become functional after adrenalectomy [5].
Malignant degeneration has been reported [6].
The differential diagnosis arises with a possible metastasis of a malignant clear cell tumor, in particular that of a clear cell adenocarcinoma of the kidney.
In the absence of mass syndrome, systematic detection of adrenal ectopia is unjustified given the lack of clinical involvement.
- Ventura L, Leocata P, Hind A, Greco I, Ventura T. Ectopic adrenal tissue in the spermatic cord. Case report and review of the literature. Arch Ital Urol Androl. 1998 Feb;70(1):15-8. PMID: 9549163.
- Trías Puigsureda I, Orsola Gran I, Paga Carbonell J, Prera Villaseca A. Ectopia adrenal escrotal [Adrenal scrotal ectopy]. Arch Esp Urol. 1995 Jul-Aug;48(6):645-6. Spanish. PMID: 7661646.
- Czaplicki M, Bablok L, Kuzaka B, Janczewski Z. Heterotopic adrenal tissue. Int Urol Nephrol. 1985;17(2):177-81. doi: 10.1007/BF02082491. PMID: 4086234.
- Lorenzo Romero JG, Segura Martín M, Hernández Millán I, Salinas Sánchez AS, López García S, Ruiz Mondéjar R, Vírseda Rodríguez JA, Martínez Martín M. Tumor epididimario de restos adrenales [Epididymal ectopic adrenal tumor]. Arch Esp Urol. 2000 Apr;53(3):271-3. Spanish. PMID: 10851736.
- Sato S, Imachi H, Kobayashi T, Fukunaga K, Lyu J, Dong T, Yoshioka Y, Saheki T, Fukata Y, Ban N, Urushihara K, Kadota K, Murao K. Ectopic Cortisol-producing Adrenocortical Adenoma Detected by 131I-6β-iodomethyl-norcholesterol Scintigraphy. Intern Med. 2020 Jul 15;59(14):1731-1734. doi: 10.2169/internalmedicine.4180-19. Epub 2020 Apr 2. PMID: 32238722; PMCID: PMC7434542.