More Information
Submitted: 13 January 2020 | Approved: 05 March 2020 | Published: 06 March 2020
How to cite this article: Almira MC, Morejón AEG, Ricardo GS, Rodríguez TRG. Clinical relevance linked to echocardiography diagnosis in Bland, White and Garland syndrome. J Cardiol Cardiovasc Med. 2020; 5: 051-055.
DOI: 10.29328/journal.jccm.1001086
ORCiD: orcid.org/0000-0002 5609 4806
Copyright License: © 2020 Almira MC, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Bland; White y Garland syndrome; Clinical relevance; Incidence
Clinical relevance linked to echocardiography diagnosis in Bland, White and Garland syndrome
Mariela Céspedes Almira1*, Adel Eladio González Morejón2, Giselle Serrano Ricardo2 and Tania Rosa González Rodríguez1
1Specialist, Pediatric and Cardiology, Professor and Researcher, Pediatric Cardiocenter William Soler, University of Medical Sciences of Havana, Cuba
2Specialist, Cardiology, Professor and Researcher, Echocardiography Cardiocenter William Soler, University of Medical Sciences of Havana, Cuba
3Specialist, Pediatric and Cardiology, Professor Pediatric Cardiocenter William Soler, University of Medical Sciences of Havana, Cuba
*Address for Correspondence: Mariela Céspedes Almira, Cardiocentro Pediátrico “William Soler”. Ave 100 y Perla, Altahabana, Boyeros, 11800, La Habana, Cuba, Tel: 76476791; Email: marielacespedes@infomed.sld.cu
Introduction: Bland, White and Garland syndrome is a coronary anomaly with high mortality without treatment. Its clinical presentation is varied which makes epidemiological documentation difficult. Echocardiography is a useful non-invasive tool for diagnosis.
Objective: To determine the echocardiographic variables that lead to the diagnosis of Bland, White and Garland syndrome and their clinical relevance.
Material: Observational, prospective and cross-sectional study in 31 patients of the “William Soler” Pediatric Cardiocenter, from 2005 to 2018. To check the association of echocardiographic variables with the diagnosis of Bland, White and Garland syndrome, an effectiveness study was carried out that included the analysis of the incidence of echocardiographic variables that lead to the diagnosis of this entity. The clinical relevance was estimated according to the minimum importance limit. The statistical validation of the research results adopted a significance level of less than 5% (p < 0.05).
Results: The variables that facilitate the echocardiographic diagnosis of Bland, White and Garland syndrome were the echocardiographic visualization of the anomalous connection and the reversed flow in the anomalous left coronary artery. These echocardiographic measures have clinical relevance according to the quantification of risk estimators (incidence) the echocardiographic visualization of the anomalous connection, RR 39.00 and the reversed flow in the anomalous coronary artery, RR 26.31. LIM´s calculation value amounted to 6.31 and coincided with the risk estimators (incidence).
Conclusion: The echocardiographic visualization of the anomalous origin of the left coronary artery from the pulmonary arterial trunk and the detection of the local intracoronary reversed flow instituted as factors to be considered for the effective diagnosis of the disease. The documentation of the diagnostic aspects of the syndrome through echocardiography contains high statistical value and clinical relevance.
Bland, White and Garland syndrome is define as the origin of the left coronary artery from the pulmonary arterial trunk. Non-exclusive disease of pediatric age and with high mortality without detection and timely treatment [1,2].
The clinical method, which persists as a fundamental weapon of diagnostic suspicion in these times of technological explosiveness and precision, has limitations to contribute to the achievement of the adequate detection rate in this anomaly. The occasional silent nature, clinical mimicry and the various forms of expression present according to the age of the afflicted individuals induce the conception, because of epidemiological knowledge, new clinical and complementary strategies as facilitating elements for detection and successful confrontation of the ailment. Echocardiography is non-invasive diagnostic method be able to identifying the presence of Bland, White and Garland syndrome [3-6].
Different health centers of all latitudes have published their experiences about the diagnostic method useful for diagnostic of Bland, White and Garland syndrome, including echocardiography [7]. Other studies show the challenge of ultrasound diagnosis due to the presence of artifacts, transverse sinus effect, interventricular communication, arterial duct or pulmonary hypertension secondary to mitral regurgitation that can prevent seeing abnormal flow in the pulmonary artery [5,8,9]. However, echocardiography is considered the preferred method even when the coronary origin is not observed [4,5], affirm that it is an imaging modality with well-established criteria for diagnosis in patients with Bland, White and Garland syndrome [4,8,10].
There are statistically significant research that is not useful when applied in daily practice; the medical field knows this condition as clinical relevance.
The early diagnosis of this syndrome determines the prognosis of the disease and allows the modification of its natural history through surgical intervention with increased chances of recovery of cardiac functionality [11].
Evidence-based Medicine (MBE) aimed to obtain and apply the best scientific evidence in the exercise of daily medical practice. For this careful, reflexive and explicit use of scientific arguments is required to solve the problems posed by daily medical practice [12,13], practicing MBE means integrating individual clinical competence with the best external clinical evidence available from of systematic research [14].
The present investigation was carried out with the purpose of determining the echocardiographic variables that lead to the diagnosis of Bland, White and Garland syndrome and their clinical relevance.
An analytical, observational, prospective and cross-sectional study of all patients with echocardiography diagnosis of Bland, White and Garland syndrome was performed, with tomographic, surgical or necropsy confirmation, referred to the Pediatric Cardiocenter “William Soler” in the period from November 2005 to June 2018. The hospital where the research was conducted is a national reference center for the diagnosis, treatment and monitoring of patients with congenital heart disease, which allowed the study of all subjects.
Echocardiographic examinations of all patients were performed by a single observer. In bias prevention, the masking method was adopted consisting of the encrypted reception and processing of the information obtained, of echocardiographic origin, according to the conditions necessary for a blind study by third parties [15].
The research was based on the analysis of various variables that were conceptually defined.
The diagnosis of Bland, White and Garland syndrome was considered the dependent variable. The independent variables were: Echocardiographic visualization of the abnormal connection, detection of reversed flow in the anomalous coronary artery, location of the anomalous left coronary artery, coronary artery dilation and increased collateral coronary vascularization.
All patients with Bland, White and Garland syndrome diagnosed by echocardiography and based on tomographic, hemodynamic, surgical or necropsy confirmation were included. Patients with positive echocardiographic diagnosis of Bland, White and Garland syndrome with presented negative tomographic, hemodynamic, surgical or necropsy diagnosis; patients with positive echocardiographic diagnosis of Bland, White and Garland syndrome without confirmation by other diagnostic means, surgery or necropsy and patients suffering from other congenital coronary anomalies were excluded. Patients incorporated into the study population who abandoned the research by voluntary personal or family decision was exit.
The information was obtained from clinic history, physical examination and echocardiographic research.
For the evaluation of clinical relevance, the tools of Evidence-Based Medicine (MBE) [16] were used in order to carry out the necessary effectiveness study that included the evaluation of the incidence, through the assessment of risk estimators, corresponding to the diagnosis echocardiographic syndrome.
The analysis of the incidence was based on the investigation of the following risk estimators: [17,18].
• Absolute incidence (Ie): probability of an event or phenomenon occurring. The present investigation indicated the proportion corresponding to individuals with certain echocardiographic quantification in which the event (nE) was observed with respect to the total of subjects that integrated said quantification (nP). It wascalculated using the formula: Ie = nE / nP.
• Relative risk (RR): reason established between absolute incidents, with respect to a given event, belonging to two groups of known elements. Indicates how much more likely to develop a phenomenon has a group of subjects in relation to another. RR is a measure of causal associations and therapeutic efficacy. In the present investigation, it illustrated the reason between the absolute incidences of the echocardiographic diagnostic event of Bland, White and Garland syndrome, corresponding to the group of patients where a certain echocardiographic parameter under study (Ie) was measured and to the group of individuals in whom they were evaluated the rest of the echocardiographic measurements (Io) according to the equation RR = Ie / Io.
• Absolute risk reduction (RAR): Difference observed between the absolute incidents, with respect to a known fact, of two groups of elements. In this investigation, it indicated the difference between the absolute incidences of the echocardiographic diagnostic event of White, Bland and Garland syndrome, adjusted to the measurement of a certain echocardiographic parameter under study (Ie) and to the group of individuals in whom the rest of the echocardiographic measures (Io). Its calculation was made using the formula RAR = Io + Ie.
• Relative risk reduction (RRR): Reason established between the absolute reduction of the risk in the event of an event (RAR) of one group of subjects with respect to the calculated absolute incidence of another (RRR = Io + Ie / Io). The RRR is a complement to the relative risk and indicates in what proportion a certain process reduces the risk of suffering a disease or damage. The present investigation showed the reason between the RAR before an event calculated in the group of patients where a certain echocardiographic parameter was measured in study regarding the absolute incidence of similar event recorded in the group of individuals corresponding to the rest of the echocardiographic measurements.
• Number of patients that need to be treated (NNT): Estimated number of individuals from a particular group under study that should be treated with a defined therapy to obtain benefits in an additional patient or prevent an undesirable outcome compared to another known group. Together with the RRR, it is considered an impact meter in clinical epidemiology. The greater the difference in effect of the event studied between the two groups faced, the smaller the NNT, so that, as the impact of the event increases, the greater the decrease in its figures, this indicator will experience. A negative NNT means that the event analyzed has a dangerous or detrimental effect on the group under scrutiny. This situation needs to be evaluated by the so-called number of patients needed to harm (NND).
• Number of patients needed to harm (NND): Indicator that reflects the insecurity of a certain intervention. It consists of the number of people that need to be treated with a specific treatment to produce, or not avoid, an additional adverse event. The joint evaluation of NNT and NND helps to clarify the risk / benefit ratio of a fact subject to analysis. Minimum importance limit (LIM): Also called delta value. Quantification of relative risk considered clinically important effect or minimum threshold. Useful to confirm or deny the existence of relevance with respect to certain event [16,18].
To validate its results, a significance level of less than 5% (p < 0.05) was adopted for the previously established degrees of freedom. The presence of significant levels in the results attributable to the relative risk was admitted when the nullity hypothesis (Ho) was discarded since the null value (RR = 1) was not included within the confidence interval (95% CI) of that estimator of risk [19,20].
To determine the clinical relevance of the echocardiographic variables, an effectiveness study was carried out, which included the analysis of the incidence of the diagnosis of the syndrome in each echocardiographic measurement. The effectiveness study was presented according to specific estimates and the respective confidence intervals of the calculated risk estimators. The existence of clinical relevance was reaffirmed in those measured variables on patients with echocardiographic diagnosis of Bland, White and Garland syndrome whose confidence interval of relative risk exceeded the minimum importance limit value (LIM or delta) [19] set in advance according to established methodology.
Ethical considerations
The investigation was carried out in accordance with the precepts and strict compliance with the Declaration of Helsinki [21], under the ethical regulations in force at the national level, with the prior approval of the Scientific Council and the Research Ethics Committee of the Pediatric Cardiocenter “William Soler”.
Table 1 illustrate the findings obtained by establishing the relationship between echocardiographic parameters and the diagnosis of the syndrome according to the quantification of risk estimators (incidence) and the respective confidence intervals in each of the variables studied. The results obtained indicate that the echocardiographic measurements that established the highest probability for the diagnosis of the syndrome were: the echocardiographic visualization of the anomalous connection, RR (39.00; 95% CI 9.88 to 153.97) and the reversed flow in the anomalous coronary artery, RR (26.31; 95% CI 8.62 to 80.33); while the lowest incidence for the echocardiographic diagnosis of the syndrome was seen in the lateralized location of the anomalous left coronary artery, RR (1.37; 95% CI 0.86 to 2.18); increased collateral coronary vascularization, RR (1.07; 95% CI 0.67 to 1.69); and right coronary artery dilation, RR (1.35; 95% CI 0.85 to 2.21).
| Table 1: Echocardiographic diagnosis of Bland, White and Garland syndrome. Incidence study. | |||||
| Variables | Echocardiographic diagnosis of Bland, White and Garland syndrome. Risk estimators [Number + (95% CI)] |
||||
| RR | RRR | RAR | NNT | NND | |
| Echocardiographic visualization of the anomalous connection | 39.00 (9.88 a 153.97) |
- 38.00 (- 152.97 a - 8.88) |
- 0.90 (- 1.01 a -0.80) |
- | 2 |
| Lateral location of the anomalous left coronary artery | 1.37 (0.86 a 2.18) |
- 0.37 (- 1.18 a 0.14) |
- 0.13 (- 0.35 a 0.08) |
8 | - |
| Reversed flow in the anomalous coronary artery | 26.31 (8.62 a 80.33) |
- 25.31 (- 79.33 a - 7.62) |
- 0.89 (- 1.00 a -0.79) |
- | 2 |
| Increased collateral coronary vascularization | 1.07 (0.67 a 1.69) |
- 0.07 (- 0.69 a 0.33) |
0.03 (- 0.24 a 0.16) |
34 | - |
| Right coronary artery dilation | 1.35 (0.85 a 2.21) |
- 0.37 (- 1.21 a 0.15) |
- 0.13 (- 0.35 a 0.08) |
7 | - |
| RR: Relative Risk; RRR: Relative Risk Reduction; RAR: Absolute Risk Reduction; NNT: Number of patients that Need to be Treated; NND: Number of patients to Harm. | |||||
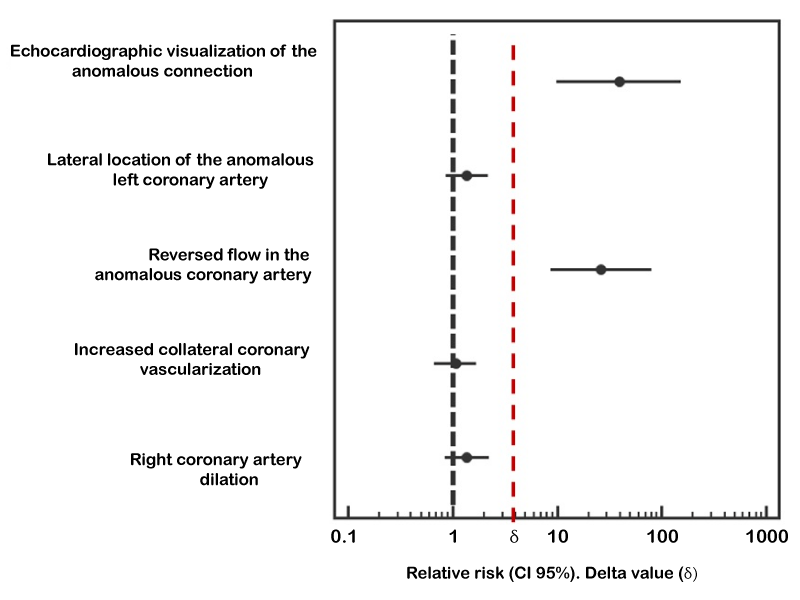
The analysis of the existing clinical relevance according to the limit value of minimum importance or δ corresponding to the echocardiographic diagnosis of Bland, White and Garland syndrome was shown in figure 1. LIM´s calculation value amounted to 6.31 and coincided with the risk estimators (incidence) that have been previously exposed.
Figure 1: Echocardiographic diagnosis of Bland, White and Garland syndrome. Analysis of the existing clinical relevance according to the minimum importance limit value (δ).
In the present study, an analysis was performed to evaluate the effect of lateralized localization of the anomalous left coronary artery, increased collateral coronary vascularization, dilatation of the right coronary artery, echocardiographic visualization of the anomalous connection and the reversed flow in the anomalous left coronary artery about the diagnosis of the disease. The echocardiographic visualization of the abnormal connection and the reversed flow in the anomalous left coronary artery evidenced as factors to be considered for the effective diagnosis of the disease.
There are statistically significant, but not clinically relevant studies; the instruments necessary to assess such situation are provided by Evidence Based Medicine (MBE). If you want to know the real effects of the phenomenon on certain diseases, the results obtained from an event under ideal and controlled conditions must be complemented with the results generated by a given event under real conditions of use [22].
By risk estimators, it is possible to know the aspects related to the incidence that lead to the evaluation of the clinical relevance in the mentioned event [23-25].
These elements lay the foundations for the estimation of clinical relevance since statistical significance does not imply clinical significance or usefulness of echocardiography as a diagnostic method for Bland, White and Garland syndrome. It is essential to establish the magnitude of the effect, as well as its degree of precision according to the confidence interval and then the interpretation of its relevance requires its comparison with the difference that is previously considered as clinically important, minimum importance limit value (LIM o δ) [13,16,19].
By establishing the relationship between the echocardio- graphic parameters and the diagnosis of the syndrome according to the quantification of risk estimators and the respective confidence intervals in each measured echocardiographic variables, it was obtained that the echocardiographic visualization of the abnormal connection and reversed flow in the anomalous left coronary artery were the variables most likely for the diagnosis of the syndrome. Precisely in these measures the existence of reaffirmed clinical relevance is verified according to the relationship of the confidence interval pertaining to the relative risk with the minimum value limit established for the analyzed event and its results coincide with those obtained from the statistics standards descriptive.
Evidence Based Medicine (MBE) [22,26]. The MBE is a process aimed at obtaining and applying the best scientific evidence in the exercise of daily medical practice. The fulfillment of that purpose is achieved through the careful, thoughtful and explicit use of scientific arguments for the solution of the problems that medical praxis poses. The execution of the MBE means integrating the individual clinical competence with the best external evidence available from systematic research.
Using risk estimators it is possible to know the aspects related to the incidence of a certain event that lead to the evaluation of the clinical relevance in that [18,27]. The importance of estimating clinical relevance is that statistical significance does not automatically imply transcendence for the practical medical field. It is essential to establish the magnitude of each presumed risk estimator according to the confidence interval calculated and know its relevance from the relationship established with the estimated value in advance and that is considered as clinically important [12,17,19].
Risk estimators linked to the diagnostic probability by echocardiography of Bland, White and Garland syndrome, emphasized that the visualization of the anomalous connection belonging to the left coronary artery and the reversed blood flow detection inside the mentioned vessel are the only variables capable of establishing the echocardiographic diagnosis of the condition (incidence). These variables proved to have clinical relevance according to the positioning of their respective confidence intervals, pertaining to the relative risk, with respect to the limit value of minimum importance established for the investigated event.
The echocardiographic visualization of the anomalous origin of the left coronary artery from the pulmonary arterial trunk and the detection of the local intracoronary reversed flow are the factors to be considered for the effective diagnosis of the disease.
The documentation of the diagnostic aspects of Bland, White and Garland syndrome through non-invasive procedures contains high statistical value and clinical relevance.
A small sample was studied because the entity has an uncertain prevalence due to difficult epidemiological documentation.
- Ramírez RF, Bitar HP, Paolinelli GP, Pérez CD, Furnaro F. Anomalías congénitas de arterias coronarias, estudio de aquellas con importancia hemodinámica. Rev Chil Radiol. 2018; 24: 142-50.
- López LP, Centella Hernández T, López Menéndez J, Cuerpo Caballero G, Silva Guisasola J, et al. Registro de intervenciones en pacientes con cardiopatía congénita de la Sociedad Española de Cirugía Torácica-Cardiovascular 2017 y retrospectiva de los últimos 6 años. Cirug Cardiov. 2019; 26: 28-38.
- Perloff JK. Anomalous origin of the left coronary artery from the pulmonary trunk. In the clinical recognition of congenital heart disease. 4th edition. Perloff JK, editor. Philadelphia: WB Saunders Co. 1994; 546-561.
- Wen-xiu L, Bin G, Jiang W, et al. The echocardiografphy diagnosis of infantile and adult types of anomalous origin of the left coronary artery from the pulmonary artery. Chin J Evid Based Pediatr. 2014; 9: 186-189.
- Arunamata A, Buccola Stauffer KJ, Punn R, Chan FP, Maeda K, et al. Diagnosis of anomalous aortic origin of the left coronary artery in a pediatric patient. World J Pediatr Congenit Heart Surg. 2015; 6: 470-473. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26180168
- Yarrabolu TR, Ozcelik N, Quinones J, Brown MD, Balaguru D. Anomalous origin of left coronary artery from pulmonary artery-duped by 2D; saved by color Doppler: echocardiographic lesson from two cases. Ann Pediatr Cardiol. 2014; 7: 230-232. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4189245/
- Mertens LL, Rigby ML, Horowitz ES, et al. Cross sectional echocardiographic and doppler imaging. In: Anderson RH, editor. Paediatric Cardiology. Philadelphia: Churchill Livingstone Elsevier Ltd; 2010; 313 – 339.
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28: 1-39. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25559473
- Cordero L, Rodríguez J, Zuluaga J, Mendoza F, Pérez O. Utilidad de la ecocardiografía en la detección de la insuficiencia cardíaca en un adulto joven con síndrome de origen anómalo de la arteria coronaria izquierda del tronco de la arteria pulmonar y válvula mitral asimétrica similar al paracaídas. Rev Colomb Card. 2018; 25:151.
- Weigand J, Marshall CD, Bacha EA, Chen JM, Richmond ME. Repair of anomalous left coronary artery from the pulmonary artery in the modern era: preoperative predictors of immediate postoperative outcomes and long term cardiac follow‑up. Pediatr Cardiol. 2015; 36: 489-497. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25301273
- Holst LM, Helvind M, Andersen HO. Diagnosis and prognosis of anomalous origin of the left coronary artery from the pulmonary artery. Dan Med J. 2015; 62: A5125. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26324080
- Sackett DL, Rosenberg WM, Gray JA. Evidence based medicine: what it is and what it is not. BMJ. 1996; 312: 71-2. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8555924
- García Garmendia JL, Maroto Monserrat F. Interpretación de resultados estadísticos. Med Int. 2018; 42: 370-379.
- Landa Ramírez E, Martínez Basurto AE, Sánchez Sosa JJ. Medicina basada en la evidencia y su importancia en la medicina conductual. Psicología y Salud. 2013; 23: 273-282.
- Laporte JR. Principios básicos de investigación clínica. 2da. ed. Barcelona: Astra Zeneca; 2001.
- Tajer CD. Ensayos terapéuticos, significación estadística y relevancia clínica. Rev Argent Cardiol. 2010; 78: 385-390.
- Bonmatí AN, Vasallo JM. Estadística básica en Ciencias de la Salud. Univ Alicante. 2016:7-59.
- Moncho J. Estadística aplicada a las Ciencias de la Salud. Barcelona: Elsevier; 2015; 62-92.
- Ochoa Sangrador C. Evaluación de la importancia de los resultados de estudios clínicos. Importancia clínica frente a significación estadística. Evid Pediatr. 2010; 6: 40-50.
- Bilder, Christopher R. Loughin, Thomas M. Analysis of Categorical Data with R. First ed. USA: Chapman and Hall/CRC; 2014; 378-382.
- World Medical Association (WMA). World Medical Association Inc. Declaration of Helsinki-Ethical Principles for Medical Research Involving Human Subjects [homepage en Internet]; 64ª Asamblea General, Fortaleza, Brasil, octubre 2013 [citado 16 de marzo de 2019]. Disponible en: https://www.wma.net/en/30publications/10policies/b3/index.html
- Cañedo Andalia R. Medicina basada en la evidencia: un nuevo reto al profesional de la información en salud. ACIMED [serie en Internet]. 2001 [citado 16 de marzo de 2019; 9. Disponible en: http://bvs.sld.cu/revistas/aci/vol9_1_01/aci011001.htm
- Alva Díaz C, Aguirre Quispe W, Becerra Becerra Y, García Mostajo J, Huerta Rosario M, et al. La medicina científica y el programa medicina basada en evidencia han fracasado? Educ Med. 2018; 19: 198-202.
- Baptista González HA. El número necesario a tratar (NNT) y número necesario para hacer daño (NNH). Valoración de la magnitud de la relación beneficio vs. riesgo en las intervenciones médicas. Rev Invest Med Sur Mex. 2008; 15: 302-305.
- Silva Fuente-Alba C, Molina Villagra M. Likelihood ratio (razón de verosimilitud): definición y aplicación en Radiología. Rev Argent Radiol. 2017; 81: 204-208.
- Straus, Glasziou, Richardson, Haynes. Medicina basada en la evidencia: Cómo practicar y enseñar la medicina basada en la evidencia. 5e ed. España: Editorial Elsevier; 2019.
- Ortega Páez E. Sigue vigente hoy día la medicina basada en la evidencia? Rev Pediatr Aten Primaria. 2018; 20: 323-328.